Pregnancy anatomy diagram
Anatomy of pregnancy and birth - uterus
Anatomy of pregnancy and birth - uterus | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What does the uterus look like?
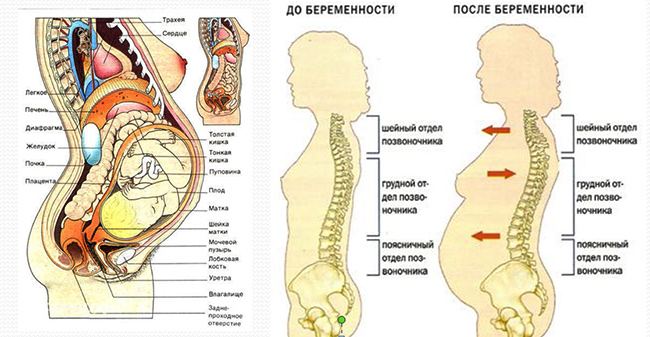
One of the most recognised changes in a pregnant woman’s body is the appearance of the ‘baby bump’, which forms to accommodate the baby growing in the uterus. The primary function of the uterus during pregnancy is to house and nurture your growing baby, so it is important to understand its structure and function, and what changes you can expect the uterus to undergo during pregnancy.
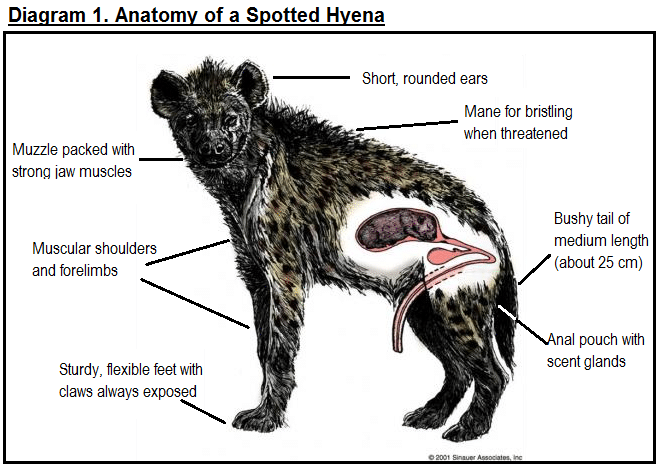
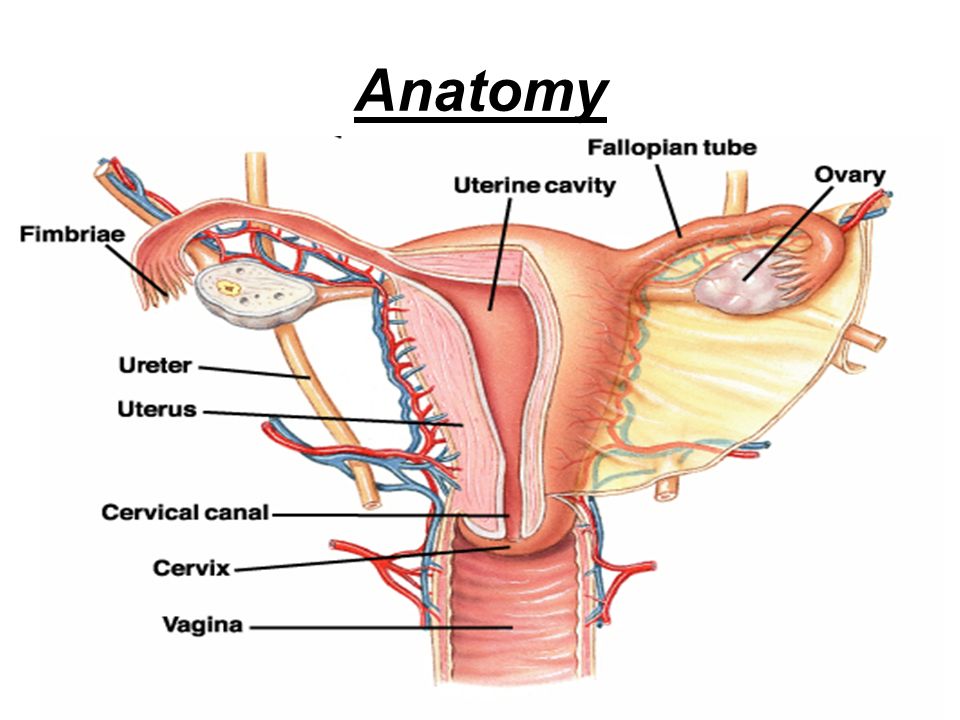
The uterus (also known as the ‘womb’) has a thick muscular wall and is pear shaped. It is made up of the fundus (at the top of the uterus), the main body (called the corpus), and the cervix (the lower part of the uterus ). Ligaments – which are tough, flexible tissue – hold it in position in the middle of the pelvis, behind the bladder, and in front of the rectum.
The uterus wall is made up of 3 layers. The inside is a thin layer called the endometrium, which responds to hormones – the shedding of this layer causes menstrual bleeding. The middle layer is a muscular wall. The outside layer of the uterus is a thin layer of cells.
Illustration showing the female reproductive system.The size of a non-pregnant woman's uterus can vary. In a woman who has never been pregnant, the average length of the uterus is about 7 centimetres. This increases in size to approximately 9 centimetres in a woman who is not pregnant but has been pregnant before. The size and shape of the uterus can change with the number of pregnancies and with age.
How does the uterus change during pregnancy?
During pregnancy, as the baby grows, the size of a woman’s uterus will dramatically increase. One measure to estimate growth is the fundal height, the distance from the pubic bone to the top of the uterus. Your doctor (GP) or obstetrician or midwife will measure your fundal height at each antenatal visit from 24 weeks onwards. If there are concerns about your baby’s growth, your doctor or midwife may recommend using regular ultrasound to monitor the baby.
Your doctor (GP) or obstetrician or midwife will measure your fundal height at each antenatal visit from 24 weeks onwards. If there are concerns about your baby’s growth, your doctor or midwife may recommend using regular ultrasound to monitor the baby.
Fundal height can vary from person to person, and many factors can affect the size of a pregnant woman’s uterus. For instance, the fundal height may be different in women who are carrying more than one baby, who are overweight or obese, or who have certain medical conditions. A full bladder will also affect fundal height measurement, so it’s important to empty your bladder before each measurement. A smaller than expected fundal height could be a sign that the baby is growing slowly or that there is too little amniotic fluid. If so, this will be monitored carefully by your doctor. In contrast, a larger than expected fundal height could mean that the baby is larger than average and this may also need monitoring.
As the uterus grows, it can put pressure on the other organs of the pregnant woman's body.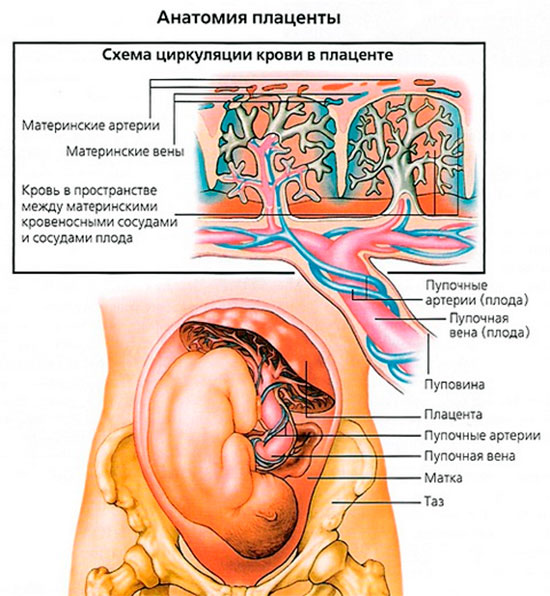 For instance, the uterus can press on the nearby bladder, increasing the need to urinate.
For instance, the uterus can press on the nearby bladder, increasing the need to urinate.
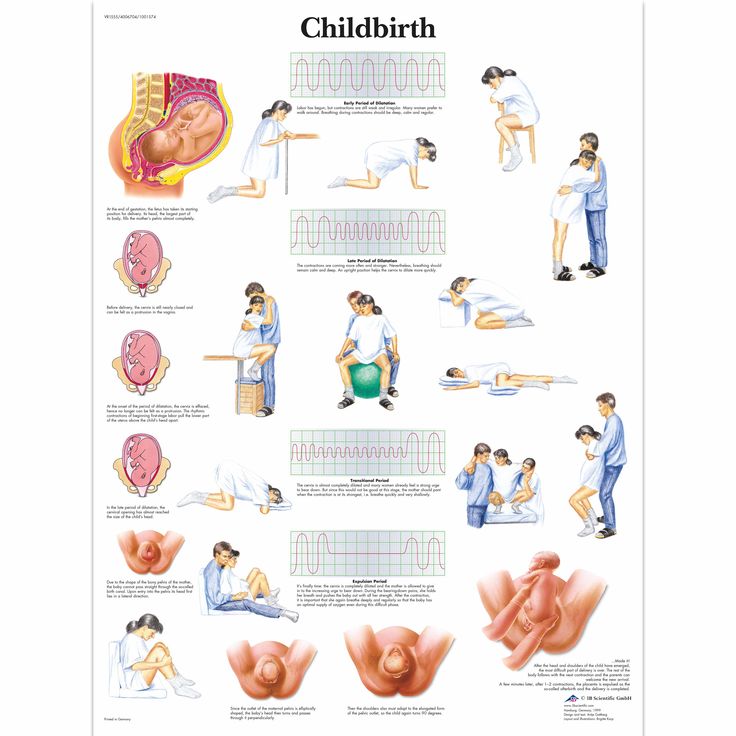
How does the uterus prepare for labour and birth?
Braxton Hicks contractions, also known as 'false labour' or 'practice contractions', prepare your uterus for the birth and may start as early as mid-way through your pregnancy, and continuing right through to the birth. Braxton Hicks contractions tend to be irregular and while they are not generally painful, they can be uncomfortable and get progressively stronger through the pregnancy.
During true labour, the muscles of the uterus contract to help your baby move down into the birth canal. Labour contractions start like a wave and build in intensity, moving from the top of the uterus right down to the cervix. Your uterus will feel tight during the contraction, but between contractions, the pain will ease off and allow you to rest before the next one builds. Unlike Braxton Hicks, labour contractions become stronger, more regular and more frequent in the lead up to the birth.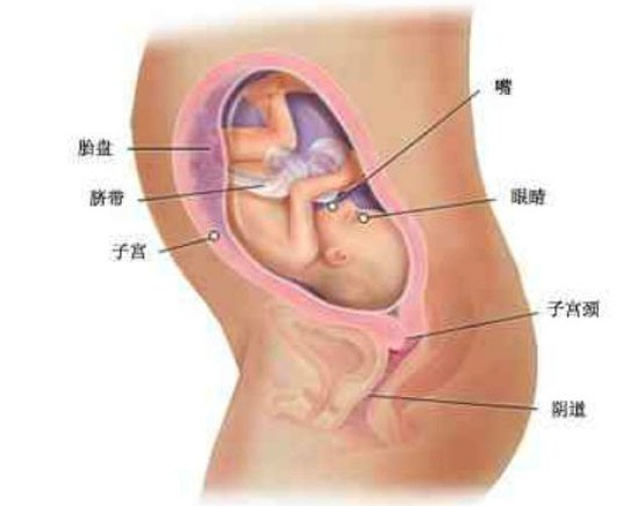
How does the uterus change after birth?
After the baby is born, the uterus will contract again to allow the placenta, which feeds the baby during pregnancy, to leave the woman’s body. This is sometimes called the ‘after birth’. These contractions are milder than the contractions felt during labour. Once the placenta is delivered, the uterus remains contracted to help prevent heavy bleeding known as ‘postpartum haemorrhage‘.
The uterus will also continue to have contractions after the birth is completed, particularly during breastfeeding. This contracting and tightening of the uterus will feel a little like period cramps and is also known as 'afterbirth pains'.
Read more here about the first few days after giving birth.
Sources:
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth), StatPearls Publishing (Anatomy, Abdomen and Pelvis), Department of Health (Clinical practice guidelines: Pregnancy care), Better Health Channel Victoria (Pregnancy stages and changes), Mater Mother's Hospital (Labour and birth information), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (The First Few Weeks Following Birth), Queensland Health (Queensland Clinical Guidelines – maternity and neonatal), King Edward Memorial Hospital (Fundal height: Measuring with a tape measure), Royal Hospital for Women (Fetal growth assessment (clinical) in pregnancy), MSD Manual (Female internal genital organs)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Anatomy of pregnancy and birth - perineum and pelvic floor
- Anatomy of pregnancy and birth - pelvis
- Anatomy of pregnancy and birth - cervix
- Anatomy of pregnancy and birth - abdominal muscles
- Anatomy of pregnancy and birth
Need more information?
Prolapsed uterus - Better Health Channel
The pelvic floor and associated supporting ligaments can be weakened or damaged in many ways, causing uterine prolapse.
Read more on Better Health Channel website
Uterus, cervix & ovaries - fact sheet | Jean Hailes
This fact sheet discusses some of the health conditions that may affect a woman's uterus, cervix and ovaries.
Read more on Jean Hailes for Women's Health website
Dilatation and curettage (D&C)
A D&C is an operation to lightly scrape the inside of the uterus (womb).
Read more on WA Health website
Ectopic pregnancy
An ectopic pregnancy occurs when a fertilised egg implants outside the uterus (womb)
Read more on WA Health website
Placental abruption - Better Health Channel
Placental abruption means the placenta has detached from the wall of the uterus, starving the baby of oxygen and nutrients.
Read more on Better Health Channel website
Placenta previa - Better Health Channel
Placenta previa means the placenta has implanted at the bottom of the uterus, over the cervix or close by.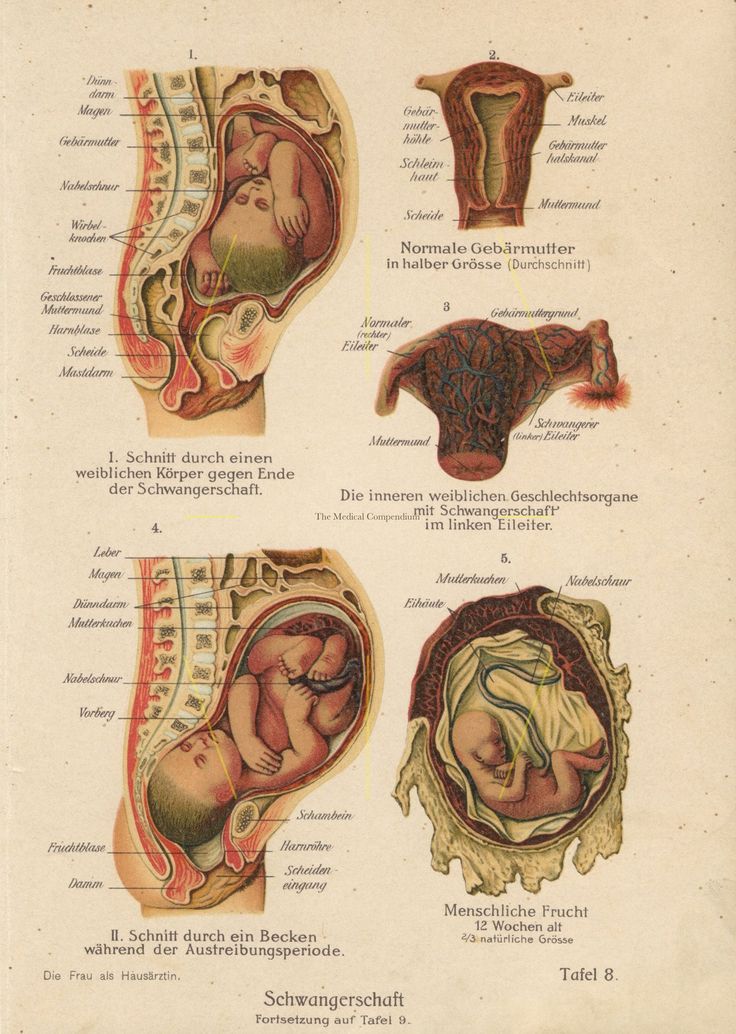
Read more on Better Health Channel website
Pelvic Floor | Family Planning NSW
The pelvic floor is a group of muscles in the pelvic area that support the bladder, bowel and uterus (womb).
Read more on Family Planning NSW website
Mirena IUD | Hormonal IUD Mirena | IUD Mirena insertion | IUD Mirena cost | Mirena IUD Melbourne - Sexual Health Victoria
The hormonal intrauterine device (IUD) is a small contraceptive device that is put into the uterus (womb) to prevent pregnancy.
Read more on Sexual Health Victoria website
Contraception - intrauterine devices (IUD) - Better Health Channel
An intrauterine device (IUD) is a small contraceptive device that is put into the uterus (womb) to prevent pregnancy.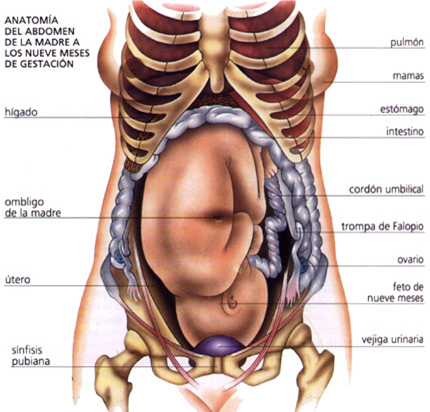
Read more on Better Health Channel website
Endometriosis | Your Fertility
Endometriosis is a condition where the tissue that lines the uterus also grows in other areas of the body
Read more on Your Fertility website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.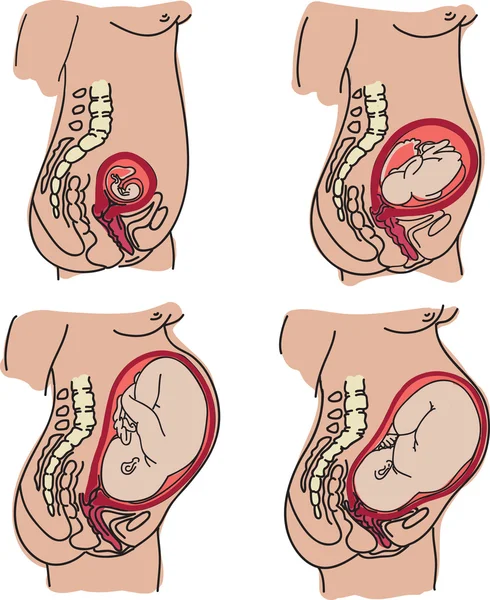
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.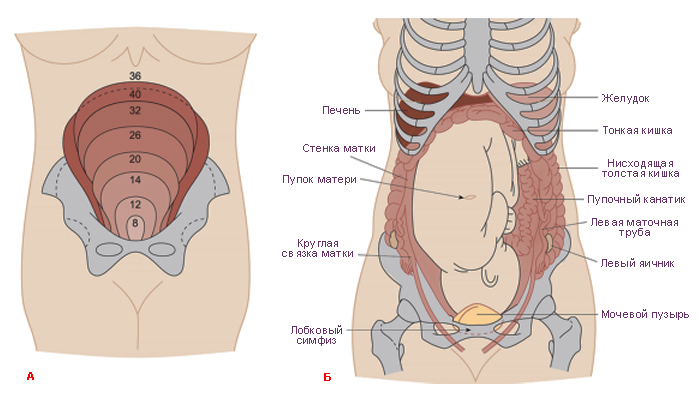
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Anatomical changes during pregnancy | Kenhub
Author: Onome Okpe • Reviewer: Uruj Zehra MBBS, MPhil, PhD
Last reviewed: November 30, 2022
Reading time: 11 minutes
The term gestation, also known as pregnancy refers to period of development of an embryo/fetus within the female reproductive system. It is mainly the period of the intrauterine life of a fetus, and includes developmental changes from conception (fertilization) to birth.
It is mainly the period of the intrauterine life of a fetus, and includes developmental changes from conception (fertilization) to birth.
Changes occur in the developing conceptus and in the pregnant mother during the gestational period, and are very important. In the developing conceptus the rate of body growth is remarkable especially during the third and fourth months, and weight gain is phenomenal during the terminal months.
This article will address the salient anatomical changes of the embryo and fetus during the gestational period and will also briefly mention the changes in the pregnant woman during the course.
Contents
- Anatomical changes in embryo and fetus
- Maternal changes
- Sources
+ Show all
[Fetus in utero]While in the uterus, the fetus is surrounded by a thin double layered membrane called the amniotic sac. The inner layer (closer to fetus) is also known as the amnion; the outer layer (closer to uterus) is also known as the chorion.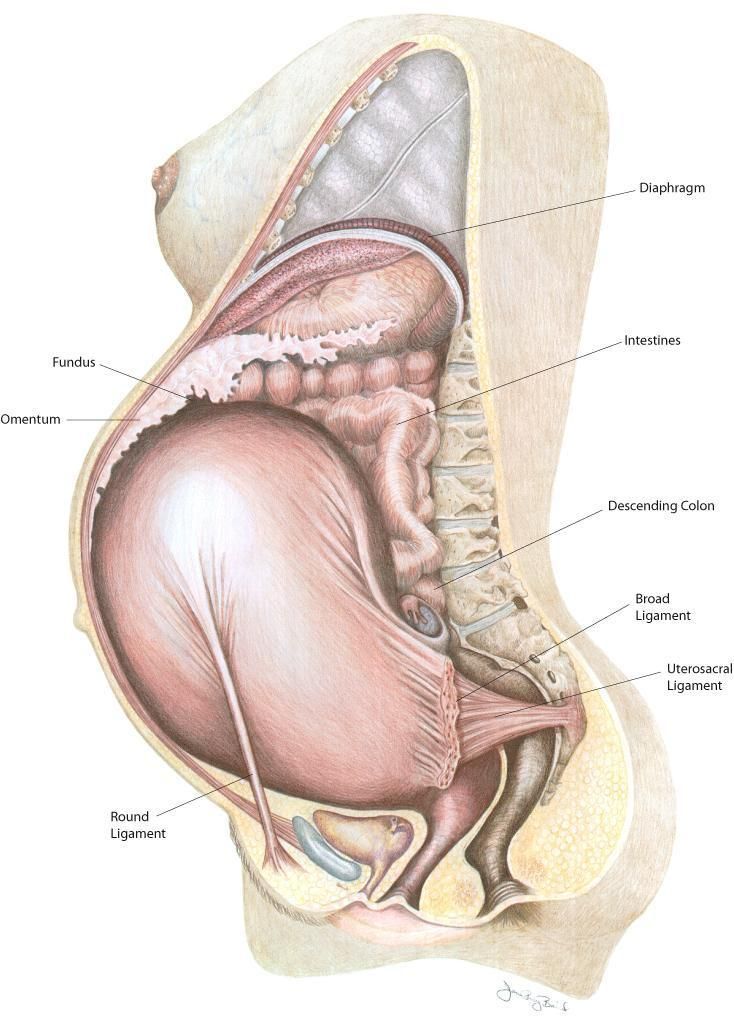 The amniotic sac is filled with amniotic fluid that surrounds and bathes the fetus during development. The fetus is connected to the placenta via the umbilical cord. The umbilical cord has two arteries that carry the deoxygenated blood from the fetus. In contrast, a single umbilical vein carries oxygenated blood, rich in nutrients from the mother to the fetus.
The amniotic sac is filled with amniotic fluid that surrounds and bathes the fetus during development. The fetus is connected to the placenta via the umbilical cord. The umbilical cord has two arteries that carry the deoxygenated blood from the fetus. In contrast, a single umbilical vein carries oxygenated blood, rich in nutrients from the mother to the fetus.
Anatomical changes in embryo and fetus
Primary oocyte
1/3
Anatomically, changes due to development can be grouped into a prenatal (before birth) and postnatal (after birth) periods. However, those occurring before birth falls under the changes during gestation. Changes in these prenatal periods can further be grouped under two periods of developments, which are the first to eight week, called the embryonic period and the ninth week to birth, known as the fetal period.
Generally, development is a continuous process beginning with the formation of a zygote when an oocyte (ovum) from a female is fertilized by a sperm (spermatozoon) from a male.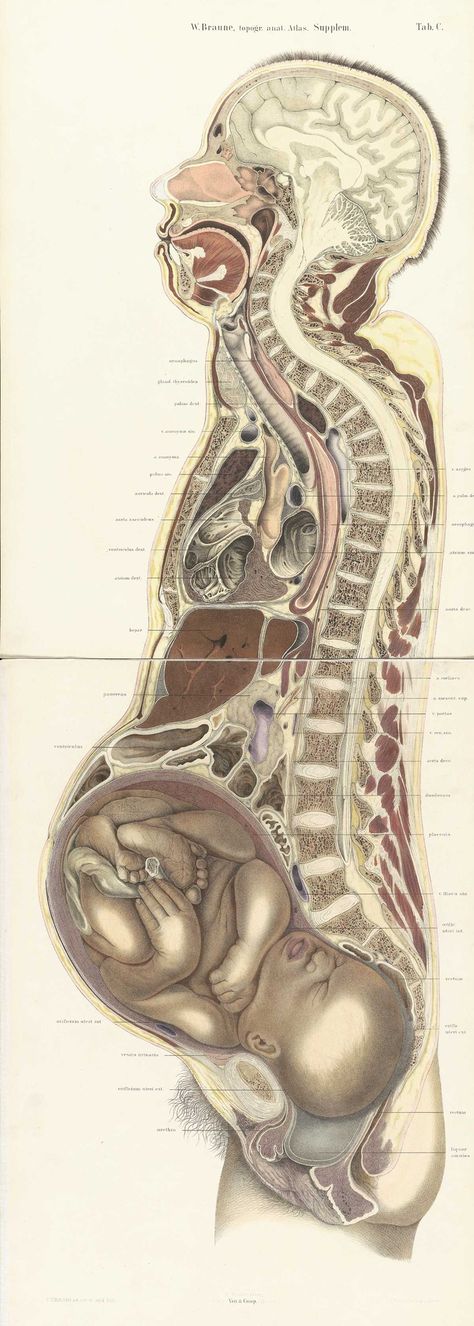 Cell division, cell migration, programmed cell death, differentiation, growth, and cell rearrangement transform the fertilized oocyte, into a zygote and finally into a multicellular human being.
Cell division, cell migration, programmed cell death, differentiation, growth, and cell rearrangement transform the fertilized oocyte, into a zygote and finally into a multicellular human being.
A major change that occur to the zygote is the multiplication of cells. This occurs due to a process called cleavage. Cleavage is the series of mitotic cell divisions of the zygote to formation of early embryonic cells, two cell stage, four cell stage, until the formation of a ball or mass of cells (sixteen to thirty-two cells stage) called morula.
Each of these cells are also referred to as blastomeres and the size of the cleaving zygote remains unchanged because at each succeeding cleavage division, the blastomeres become smaller. The blastomeres change their shape and tightly align themselves against each other to form a compact ball of cells (morula). This phenomenon, compaction, is probably mediated by cell surface adhesion glycoproteins.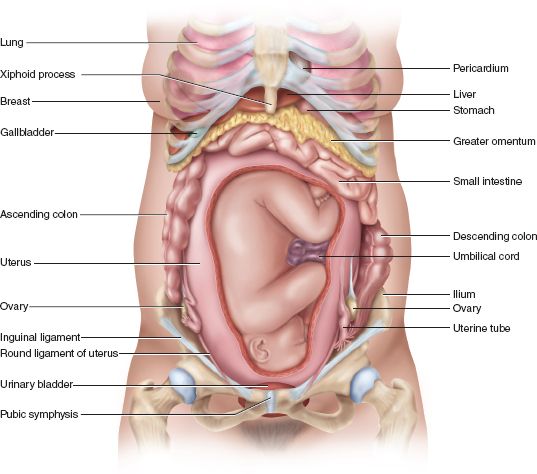 The morula stage occurs 3 to 4 days after fertilization, just as the early embryo enters the uterus.
The morula stage occurs 3 to 4 days after fertilization, just as the early embryo enters the uterus.
After the morula enters the uterus a fluid-filled cavity, the blastocele, develops inside it. This changes converts the morula into a blastocyst. The centrally located cells, the inner cell mass or embryoblast, is the embryonic part of the embryo while the outer cell mass or the trophoblast contributes to the placenta. The pre-implantaion period of embryonic development is the time between fertilization and the beginning of implantation, and the period is approximately 6 days.
From the formation of zygote at fertilization to this stage, the embryo makes its way through the fallopian tube towards to uterus where it implants. Implantation is the process by which the blastocyst attaches to the endometrium of the mother’s uterine tube, the mucous membrane or lining of the uterus, and subsequently embeds in it.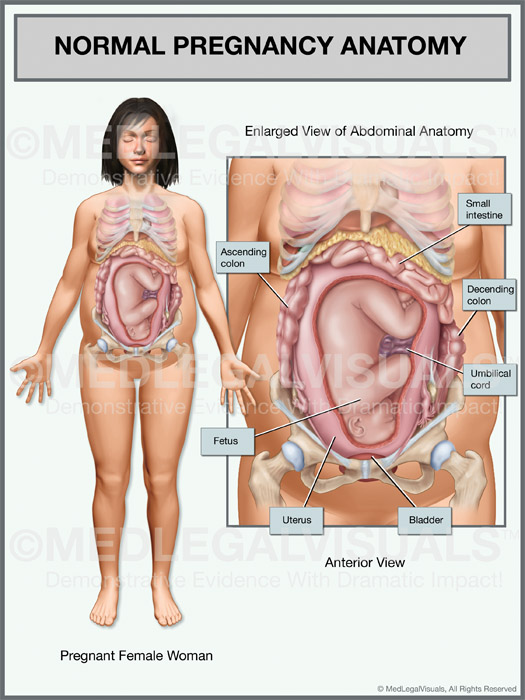
Next is the formation of a gastrula. The developing blastocyst becomes a gastrula by a process called gastrulation. During gastrulation a three layered or trilaminar embryonic disc forms. The embryonic period extends from the third to eighth weeks of development and during this period three germ layers (ectoderm, mesoderm, and endoderm) subsequently differentiate into the tissues and organs of the embryo.
The stage of neurula during the third and fourth weeks is characterised by the formation of neural tube from the neural plate. It is the first appearance of the nervous system and the next stage after the gastrula. The size of embryos is given as crown-rump length (CRL), which is measured from the vertex of the cranium (crown of head) to the rump (buttocks) on ultrasound and is used to determine the gestational age of embryo or fetus.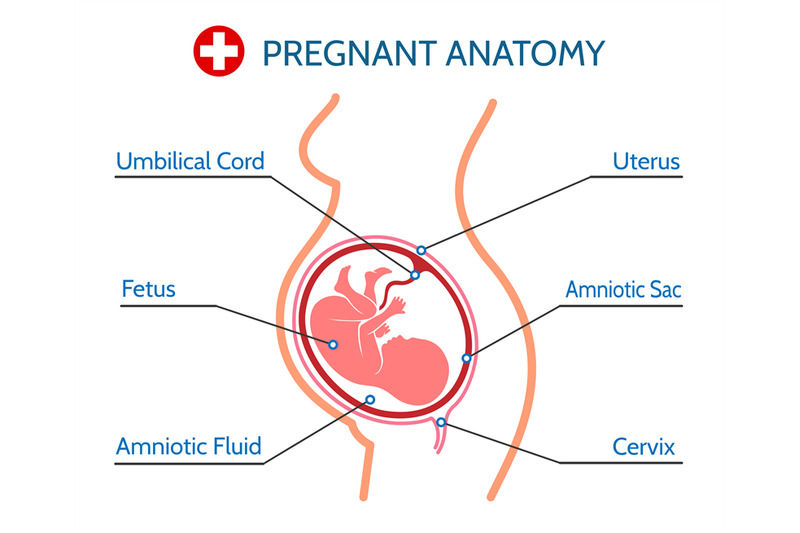
The fetal period begins on day 57 (from 9th week) and ends when the fetus is completely outside the mother (at birth). During the fetal period, differentiation and growth of the tissues and organs formed during the embryonic period occur. The anatomical changes are more gross; for example, the placenta and the umbilical cord clearly marks the connection between the developing fetus and the mother.
[Cross-section of the placenta: An overview]At the beginning of the fetal period, the placenta has two components: a fetal portion, formed by the chorion frondosum, and a maternal portion, formed by the decidua basalis. On the fetal side, the placenta is bordered by the chorionic plate. On its maternal side, it is bordered by the basal decidua. The placenta is the meeting point of two circulatory systems: fetal circulation and maternal circulation. The maternal component of the placenta contains maternal arteries and maternal veins that feed into the intervillous spaces.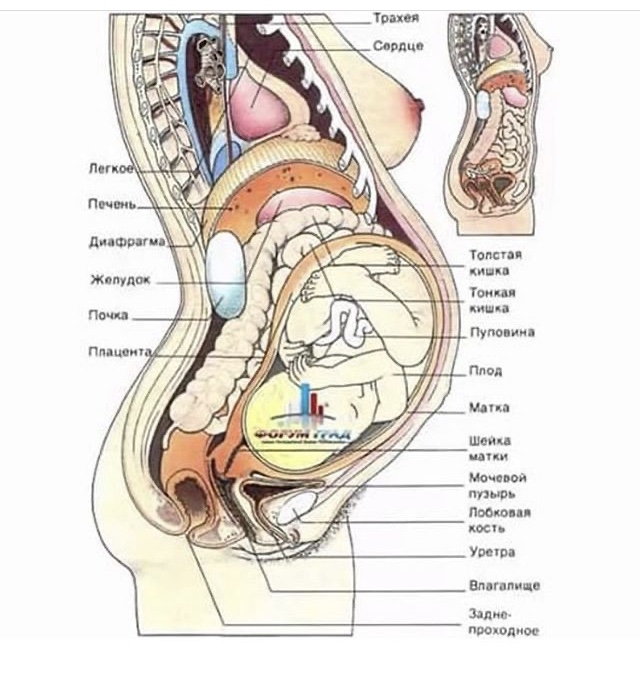 On the opposite side, the umbilical arteries and veins form a tree-like structure within the intervillous space. Here, the fetal and maternal blood comes into close contact separated only by a thin membrane, called the placental membrane.
On the opposite side, the umbilical arteries and veins form a tree-like structure within the intervillous space. Here, the fetal and maternal blood comes into close contact separated only by a thin membrane, called the placental membrane.
Structures constituting the genitalia (phallus, urogenital fold, labioscrotal fold and the perineum) are quite identifiable. The fetus attains a CRL of 45 – 61 mm on average at the tenth week, the face changes into an identifiable human profile with the ears, eyes, nose and mouth in the normal positions. Sex is fully distinguishable at week twelve, elaboration and growth of formed structure continue, and the fetus is viable at week thirty on the average, once all the structures of respiration, particularly the alveoli sacs are formed. During the last two months of gestation increase in weight is the most striking feature.
Test your knowledge on the fetus in utero with this quiz.
Maternal changes
During the development and growth of the fetus inside the womb several anatomical changes occur in the pregnant mother to accommodate the process.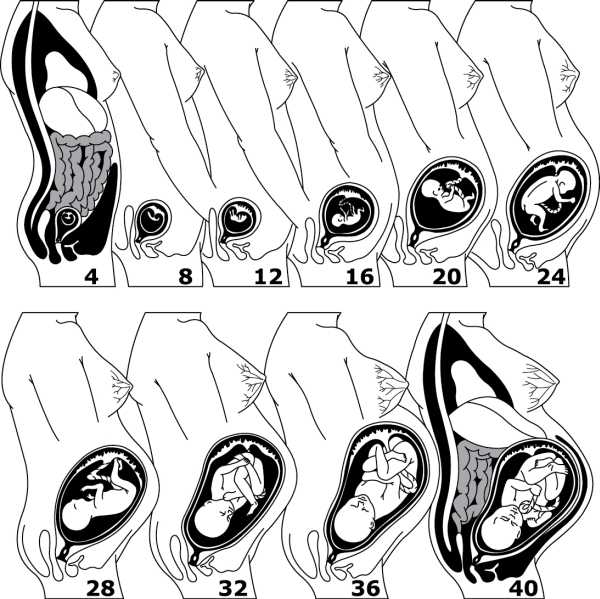 These changes are basically attributed to the hormones of pregnancy and mechanical pressure exerted by the enlarging uterus. The changes include:
These changes are basically attributed to the hormones of pregnancy and mechanical pressure exerted by the enlarging uterus. The changes include:
- Development of placenta
-
Increase in the size of uterus along with abdominal extension, weight gain, breast enlargement and some postural changes. The uterus not only increases in size but also changes its position and shape, the muscular wall of uterus strengthen and becomes more elastic.
-
Softening of the cervical tip at the beginning of sixth week may be observed.
-
The vaginal mucosa also becomes thick and prepares itself for stretching during labor and birth.
-
All the systems of the body like respiratory, cardiovascular, renal, GIT, musculoskeletal and integumentary adapt themselves to provide for maternal and fetal needs.
-
Cardiac output increases from 30% to 50% over the non pregnant rate.
But almost all of these changes and adaptations reverted to the non pregnant state after birth and lactation.
Sources
All content published on Kenhub is reviewed by medical and anatomy experts. The information we provide is grounded on academic literature and peer-reviewed research. Kenhub does not provide medical advice. You can learn more about our content creation and review standards by reading our content quality guidelines.
References:
- O. College: Maternal Changes During Pregnancy, Labor, and Birth. (accessed 07/02/2016)
- T. W. Sadler: Langman's Medical Embryology, Lippincot Williams and Wilkins, (2010), 11th edition, p. i – v, 67 – 87 and 91 – 111.
- H. B. Malakandi: Anatomical changes in pregnancy. (accessed 07/02/2016)
-
D. L. Lowdermilk, “Anatomy and physiology of pregnancy,” in Maternity Nursing, D.
 L. Lowdermilk and S. E. Perry, Eds., pp.208–230,Mosby Elsevier, St. Louis,Mo, USA, 7th edition, 2006.
L. Lowdermilk and S. E. Perry, Eds., pp.208–230,Mosby Elsevier, St. Louis,Mo, USA, 7th edition, 2006.
Illustrators:
- Body of uterus (ventral view) - Samantha Zimmerman
- Blastomere and morula formation - Photo credit: Internet Archive Book Images via Visualhunt / No known copyright restrictions
- Endometrium (ventral view) - Samantha Zimmerman
- Embryo (10 weeks) - Photo credit: lunar caustic via Visual Hunt / CC BY-SA
Anatomical changes during pregnancy: want to learn more about it?
Our engaging videos, interactive quizzes, in-depth articles and HD atlas are here to get you top results faster.
What do you prefer to learn with?
Videos Quizzes Both
“I would honestly say that Kenhub cut my study time in half.” – Read more. Kim Bengochea, Regis University, Denver
© Unless stated otherwise, all content, including illustrations are exclusive property of Kenhub GmbH, and are protected by German and international copyright laws.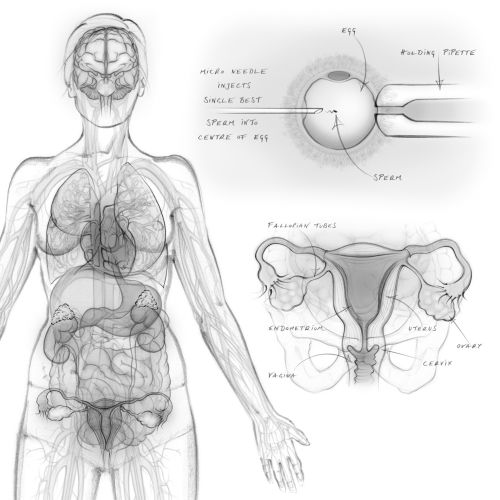 All rights reserved.
All rights reserved.Interpretation of the results of 1 pregnancy screening
Combined prenatal screening is carried out at 11-14 weeks of gestation with an embryo size of at least 45 mm and not more than 84 mm. This is a comprehensive examination of the fetus to assess the parameters of its development. Its main task is the early detection of fetal malformations, the prevention of childhood disability, and the reduction of infant and child mortality.
The first screening consists of an instrumental part - an ultrasound scan and a laboratory one - a blood test to determine the concentration of chorionic gonadotropin (βhCG) and pregnancy-associated protein A (PAPP-A). The cumulative results of these indicators allow you to plan the tactics of pregnancy management.
Why is the examination carried out at 11-14 weeks
The first trimester is the period of formation of all organs and structures of the body. By the end of the first trimester, the embryonic period ends and the fetal period of fetal development begins.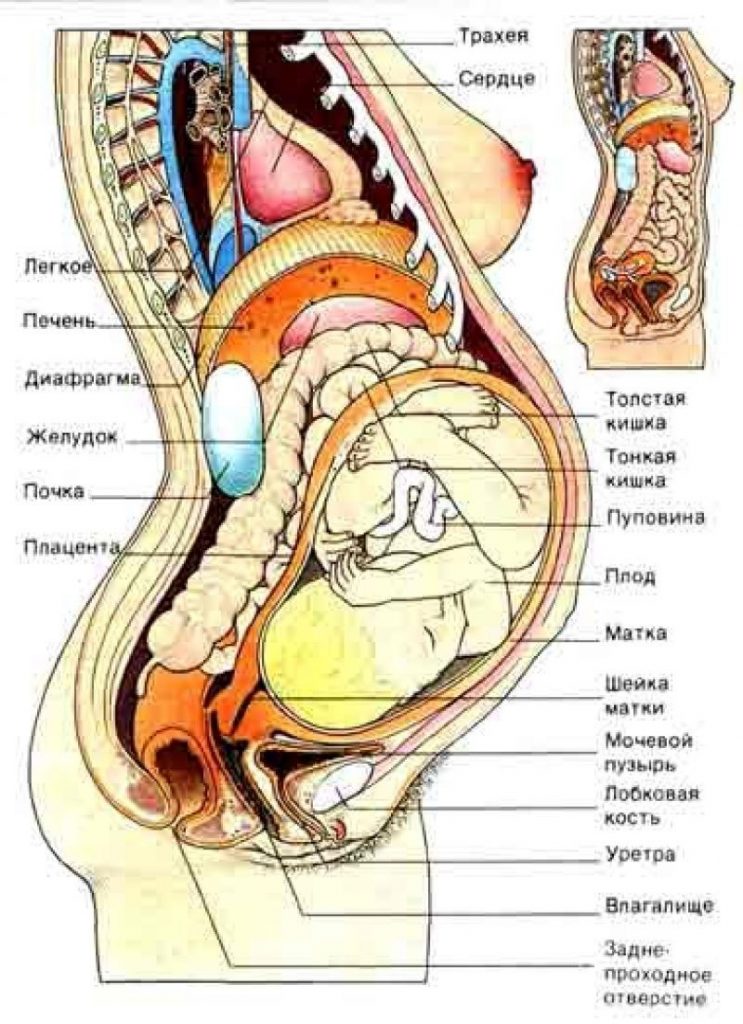 It is in the period from 11 weeks 1 day to 13 weeks 6 days of pregnancy that echographic markers of chromosomal abnormalities are best visualized.
It is in the period from 11 weeks 1 day to 13 weeks 6 days of pregnancy that echographic markers of chromosomal abnormalities are best visualized.
Who needs to be examined
According to the results of the study, it is possible to judge the risk of giving birth to children with chromosomal diseases and congenital malformations, therefore it is recommended to carefully consider the issue and examine all pregnant women. Indications for mandatory prenatal screening of the first trimester are:
- Women with a history of spontaneous abortions, ectopic and missed pregnancies, premature birth, stillbirth, birth of a child with developmental anomalies.
- Hereditary diseases in the family of the mother or father of the child
- First trimester illness treated with antibiotics or drugs contraindicated during pregnancy.
- Marriage between relatives.
- The woman is over 35 years of age.
- Presence of occupational hazards
How to prepare
Preparation for the first screening is expressed in a sparing diet.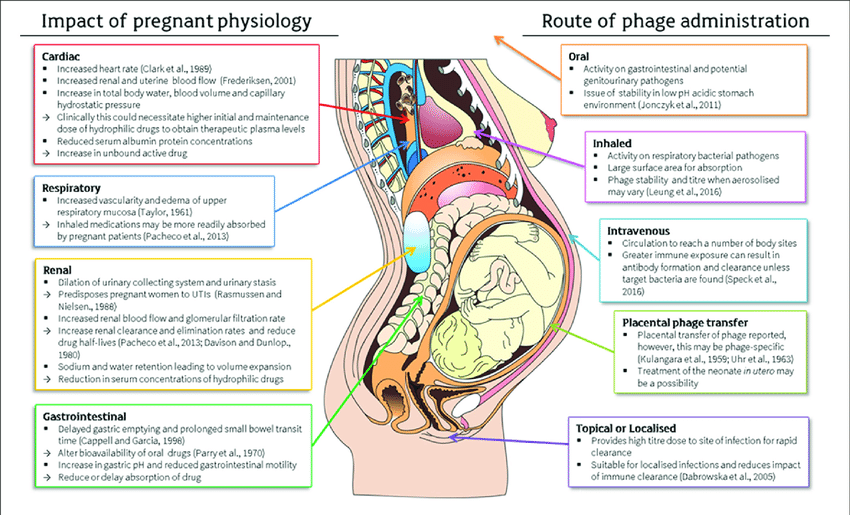 Nutritional errors can affect the general condition of a woman and reduce the accuracy of the results. One week before the examination:
Nutritional errors can affect the general condition of a woman and reduce the accuracy of the results. One week before the examination:
- Salty, spicy, fatty, fried foods should be excluded from the diet.
- Do not eat allergenic foods.
- Avoid carbonated drinks.
One day before screening:
- Do not eat chocolate, seafood, fatty meat, flour, limit sweets.
- If the study is scheduled for the morning, eat a light dinner no later than 20:00 hours.
It is advisable to observe moderate physical activity, if there are no contraindications for this. Walking and proper rest are also important.
Survey
A blood test and ultrasound are performed on the same day to avoid errors due to time differences.
- Ultrasound screening is performed first, as its results allow you to determine the exact gestational age, which affects the normative values of hormone levels. The study is carried out both transabdominally and transvaginally.
 The procedure is painless, safe for women and children, has no contraindications.
The procedure is painless, safe for women and children, has no contraindications. - Blood is donated from a vein on an empty stomach or 4 hours after a meal. The material is taken on the day of the ultrasound. The study determines the concentration of hormones and compares with standard indicators.
Only by deciphering the results of ultrasound and hormone analysis, a conclusion is made about possible risks.
What ultrasound shows
At screening during pregnancy, fetometry of the fetus is performed - determination of the size of body parts and all anatomical structures are evaluated.
The results obtained are compared with a statistical table, which indicates the percentile of falling into the sample of standard values. With indicators less than 5 and more than 95 additional examinations are scheduled.
During an ultrasound examination in the 1st trimester, the following parameters are evaluated: the bones of the cranial vault and the brain, the spine, the anterior abdominal wall, the limbs of the fetus, the structures of the face, the organs of the chest and abdominal cavity, as well as the main echographic markers of chromosomal abnormalities.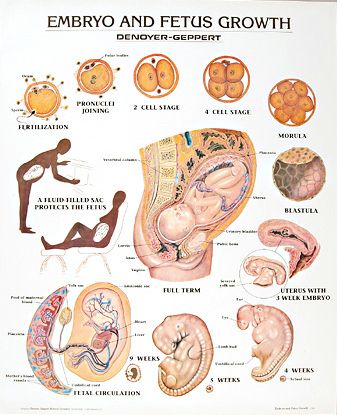
Collar space thickness (NTP)
The area between the inner surface of the skin of the fetus and the outer surface of the soft tissues covering the cervical spine. TVP is considered the most important marker of chromosomal abnormalities.
This space begins to decrease after 13 weeks, so it can only be assessed at the first screening.
| Gestational age | Collar thickness in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 0.8 | 1.6 | 2.4 | |
| 12 weeks | 0.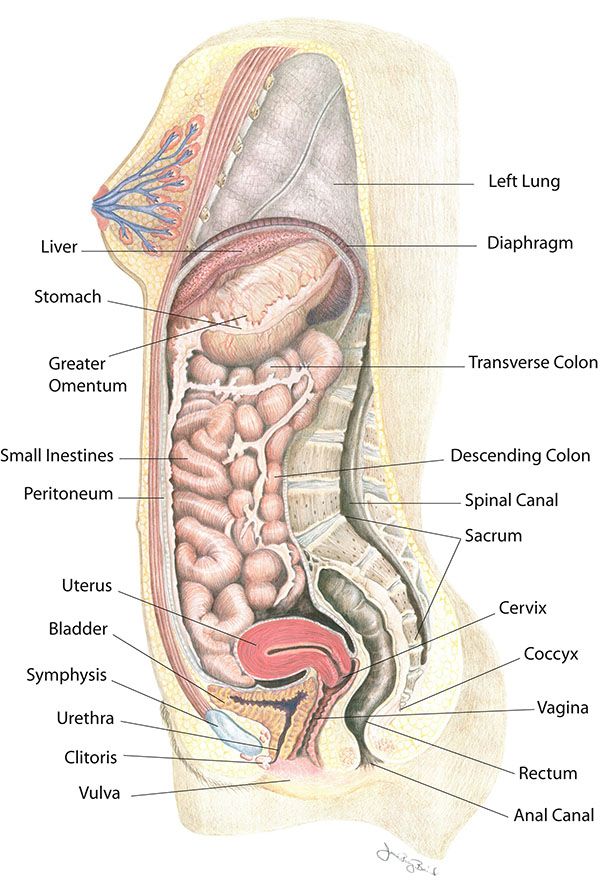 7 7 | 1.6 | 2.5 | |
| 13 weeks | 0.7 | 1.7 | 2.7 | |
The discrepancy between the results and the normative values indicates an increased risk of developing chromosomal pathologies. Depending on the formed set of chromosomes, it can be Down syndrome, Patau, Edwards, Shereshevsky-Turner. To clarify the diagnosis in this case, a biopsy of the chorion or placenta, an analysis of cord blood, and amniotic fluid may be prescribed. Only after additional research can an accurate diagnosis be made.
Coccyx-parietal size (KTR)
Shows the distance between the coccygeal and parietal bones. According to this parameter, the exact gestational age is determined on ultrasound, and the ratio of the mass of the fetus to its CTE is also established.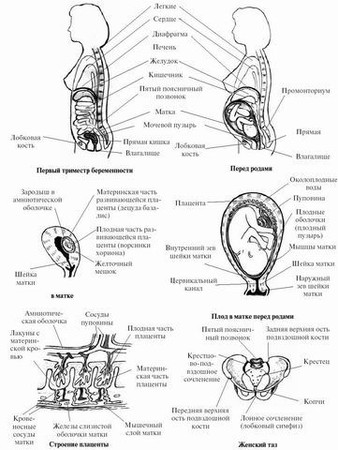
A slight deviation from the norm indicates the features of the physique and is not a cause for concern.
| Gestational age | Coccyx-parietal size in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 34 | 42 | fifty | |
| 12 weeks | 42 | 51 | 59 | |
| 13 weeks | 51 | 63 | 75 | |
If screening during pregnancy showed results that exceed the norm, this indicates that the fetus is quite large. The indicator says much less either about an incorrectly determined gestational age (in this case, a re-examination is carried out after 1-1.5 weeks), or about a slowdown in development due to intrauterine death, impaired hormonal levels or an infectious disease of the mother, genetic abnormalities.
The indicator says much less either about an incorrectly determined gestational age (in this case, a re-examination is carried out after 1-1.5 weeks), or about a slowdown in development due to intrauterine death, impaired hormonal levels or an infectious disease of the mother, genetic abnormalities.
Skull bones and brain
Already from the 11th week, ultrasound examination can detect defects in the bones of the skull, which indicates severe fetal malformations that are incompatible with life. The evaluation of the brain is based on the study of the so-called "butterfly" - the choroid plexus of the lateral ventricles. A clear visualization and its symmetry indicates the normal development of the brain.
| Gestational age | BPR, LZR in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 13.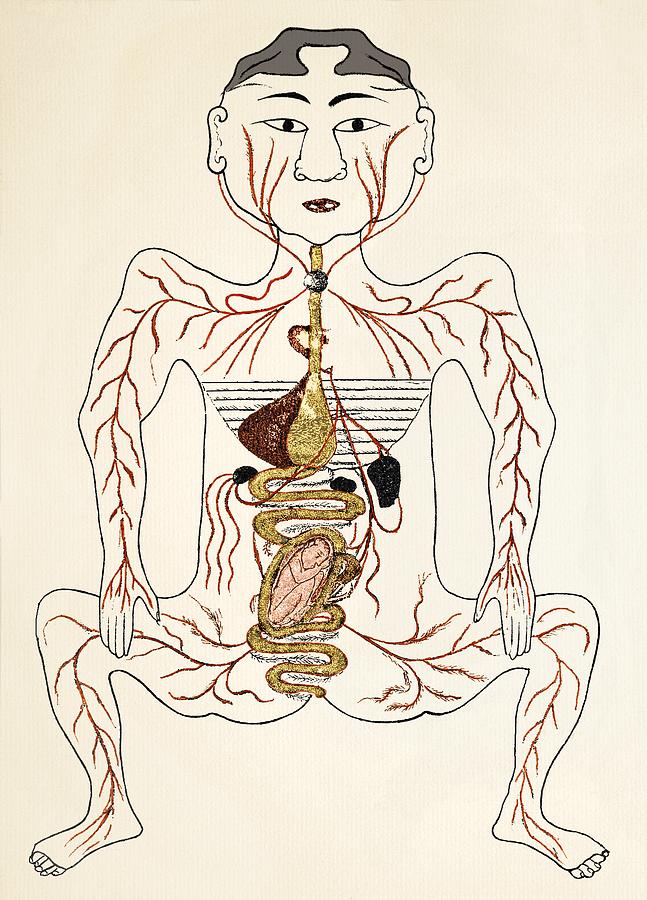 19 19 | 17.21 | 21.23 | |
| 12 weeks | 19.22 | 21.24 | 24.26 | |
| 13 weeks | 20.26 | 24.29 | 28.32 | |
Nasal bone
By the end of the trimester, it should be formed, clearly visualized.
| Gestational age | Nasal bone in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | visualized, not measured | visualized, not measured | visualized, not measured | |
| 12 weeks | 2 | 3.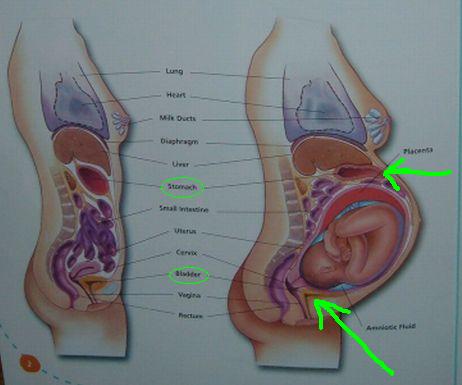 1 1 | 4.2 | |
| 13 weeks | 2 | 3.1 | 4.2 | |
The pathology of the nasal bone is its absence, hypoplasia (very small size) and a change in its echogenicity.
The diameter of the chest, the circumference of the head and abdomen, the length of the femur also make it possible to judge the proportionality of development.
Heart condition
When examining the heart, its location is assessed, the presence of four chambers of the heart is established - two atria and two ventricles, and their symmetry is assessed. The heart rate is measured.
| Gestational age | Heart rate in beats per minute | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 153 | 165 | 177 | |
| 12 weeks | 150 | 162 | 174 | |
| 13 weeks | 147 | 159 | 171 | |
The venous duct (VP) is a direct communication between the umbilical vein and the central venous system. In a normally developing pregnancy, the blood flow in the EP is a three-phase curve. The appearance of reverse blood flow may indicate the presence of fetal pathology.
In a normally developing pregnancy, the blood flow in the EP is a three-phase curve. The appearance of reverse blood flow may indicate the presence of fetal pathology.
What a blood test shows
Ultrasound results are compared with maternal plasma pregnancy-associated protein A (PAPP-A) and human chorionic gonadotropin (hCG). The values are given in the table:
| Gestational age | hCG in ng/ml | PAPP-A in mU/l |
| 11 weeks | 17.4 - 130.4 | 0.46 - 3.73 |
| 12 weeks | 13.4 - 128.5 | 0.79 - 4.76 |
| 13 weeks | 14.2 - 114.7 | 1. 03 - 6.01 03 - 6.01 |
Differences from the reference values \u200b\u200bmay indicate pathologies of the mother or fetus.
| Deviation | hCG | PAPP-A |
| Above normal |
|
|
| Below normal |
|
|
Survey interpretation
The first study is evaluated only by the totality of all indicators. A single parameter cannot be the basis for an accurate conclusion. The protocol records ultrasound data, hormone analysis, the risks of probable diseases and the complex median coefficient MoM. It indicates the cumulative deviation of the obtained results from the average values. The coefficient must be in the range from 0.5 to 2.5. It is calculated by specialized programs.
What can affect the result
- Incorrect preparation, peculiarities of the woman's condition.
- Obsolete equipment with poor measurement accuracy and insufficient resolution.
- Qualification of the doctor of the ultrasound room, errors in decoding.
- Correctness of MoM calculation algorithms.
Modern diagnostic equipment makes it possible to evaluate more than 15 fetal parameters, build its volumetric reconstruction for examining organs in the early stages of development, and calculate possible risks with high accuracy. Contact well-equipped clinics and trust specialists with proven qualifications.
Contact well-equipped clinics and trust specialists with proven qualifications.
Non-developing pregnancy: modern possibilities of conservative management
Miscarriage still remains one of the main forms of obstetric pathology and the most important component of reproductive losses, reaching 12-15 thousand per year in the form of spontaneous miscarriages and non-developing pregnancies, and in 2-2 500 couples have repeated abortions [14]. In the structure of total reproductive losses, spontaneous abortions account for 65.3%. It is important to note that the prevalence of spontaneous abortions in recent years tends to increase: from 4.21 per 1000 women of childbearing age in 2001 to 4.63 in 2010 [19]. The greatest number of prenatal losses occurs in the early stages of pregnancy: spontaneous abortions before 12 weeks occurred in 142,859 (82.8%) women, at 12-21 weeks - in 20,034 (11.6%), at 22-27 weeks - in 9636 (5.6%) [19].
In the structure of spontaneous abortions, there is a significant increase in the proportion of non-developing pregnancy (synonym: missed abortion, English - missed abortion).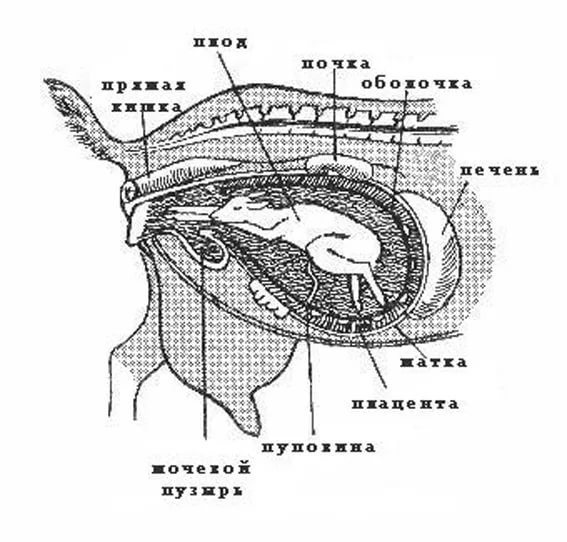 The number of her observations among all cases of spontaneous miscarriages in the early stages has increased from 10-20% to 45-88.6% in recent years and does not tend to decrease [2, 15]. The relevance of this problem is associated not only with the scale of reproductive losses, but also with an unfavorable reproductive prognosis - in 27.4% of cases, habitual miscarriage is noted after an undeveloped pregnancy [7]. This problem is not only medical, but also social in nature, since such a complication often becomes an unfavorable outcome of a desired and planned pregnancy, including after the use of assisted reproductive technologies. According to V.E. Radzinsky et al. [15], miscarriage is observed in 10-25% of all desired pregnancies.
The number of her observations among all cases of spontaneous miscarriages in the early stages has increased from 10-20% to 45-88.6% in recent years and does not tend to decrease [2, 15]. The relevance of this problem is associated not only with the scale of reproductive losses, but also with an unfavorable reproductive prognosis - in 27.4% of cases, habitual miscarriage is noted after an undeveloped pregnancy [7]. This problem is not only medical, but also social in nature, since such a complication often becomes an unfavorable outcome of a desired and planned pregnancy, including after the use of assisted reproductive technologies. According to V.E. Radzinsky et al. [15], miscarriage is observed in 10-25% of all desired pregnancies.
The causes of intrauterine retention of the dead fetus and pathological intactness of the uterus after its death have not yet been precisely established. The basis of the pathogenesis of non-developing pregnancy, regardless of the causes of occurrence, is chronic endometritis [15].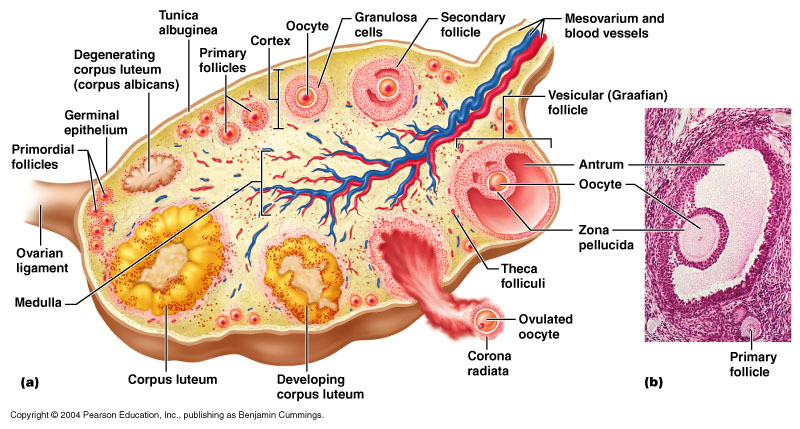 Most often, infectious diseases, hormonal and immune disorders in the mother, and chromosomal abnormalities are considered as the cause of non-developing pregnancy [7, 12, 14]. In the structure of etiological factors, a large group is made up of acute and chronic infectious diseases of the mother and a mixed viral-bacterial infection [7, 8, 23, 30]. In the abortion material and the material of the adjacent endometrium in early and late spontaneous miscarriages, signs of an infectious and inflammatory process are found, and 3–4 months after spontaneous abortion, chronic endometritis of varying degrees of activity is detected in all patients [2].
Most often, infectious diseases, hormonal and immune disorders in the mother, and chromosomal abnormalities are considered as the cause of non-developing pregnancy [7, 12, 14]. In the structure of etiological factors, a large group is made up of acute and chronic infectious diseases of the mother and a mixed viral-bacterial infection [7, 8, 23, 30]. In the abortion material and the material of the adjacent endometrium in early and late spontaneous miscarriages, signs of an infectious and inflammatory process are found, and 3–4 months after spontaneous abortion, chronic endometritis of varying degrees of activity is detected in all patients [2].
Viral diseases of the female genital organs are more often formed against the background of immunodeficiency states, and they themselves contribute to the aggravation of secondary immunodeficiencies. The main reason for the chronicity of the inflammatory process, according to modern concepts, is the inadequacy of the ongoing antibacterial treatment, associated both with polypharmacy and with the etiological structure of infectious morbidity that has changed in recent years.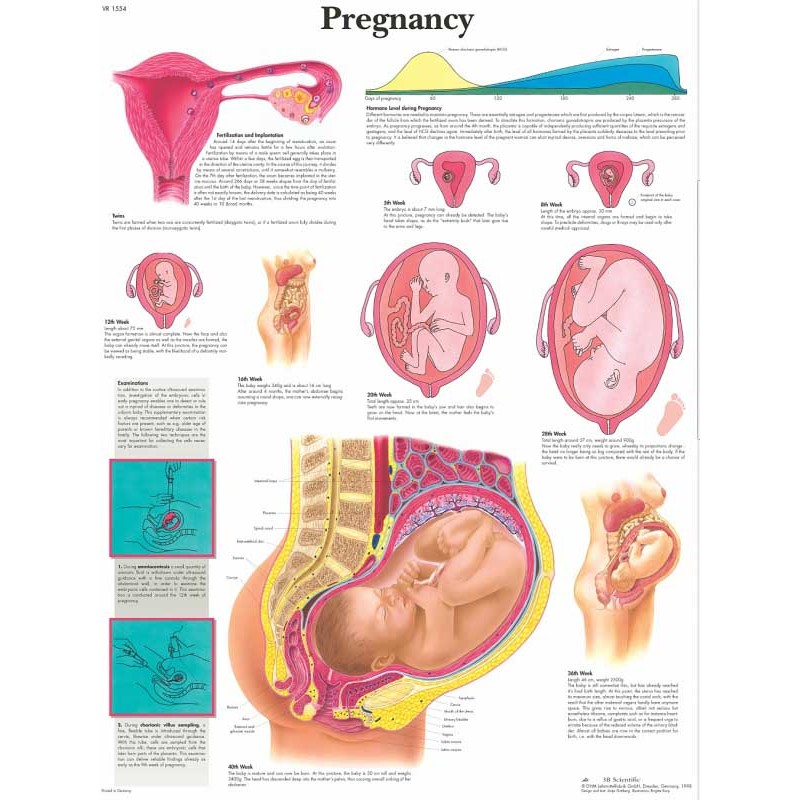 The inflammatory process can also develop as a result of the activation of the symbiotic flora of the vagina, for example, in all forms of immunodeficiency.
The inflammatory process can also develop as a result of the activation of the symbiotic flora of the vagina, for example, in all forms of immunodeficiency.
One of the main causes of non-developing pregnancy is hormonal disorders, the whole variety of which is manifested at the level of the endometrium by luteal phase insufficiency [3, 18]. The progesterone-induced blocking factor, acting on NK cells (natural killer cells), directs the mother's immune response to the embryo with the involvement of less active killer cells - large granular lymphocytes carrying CD56+, CD 16– markers. It has also been shown that progesterone stimulates the local production of proteins that bind NK cells, causing them to undergo apoptosis [18].
Among the pathogenetic factors of non-developing pregnancy, it is necessary to note the structural and functional inferiority of the endometrium in the implantation zone due to previous curettage of the mucous membrane of the walls of the uterine cavity [6].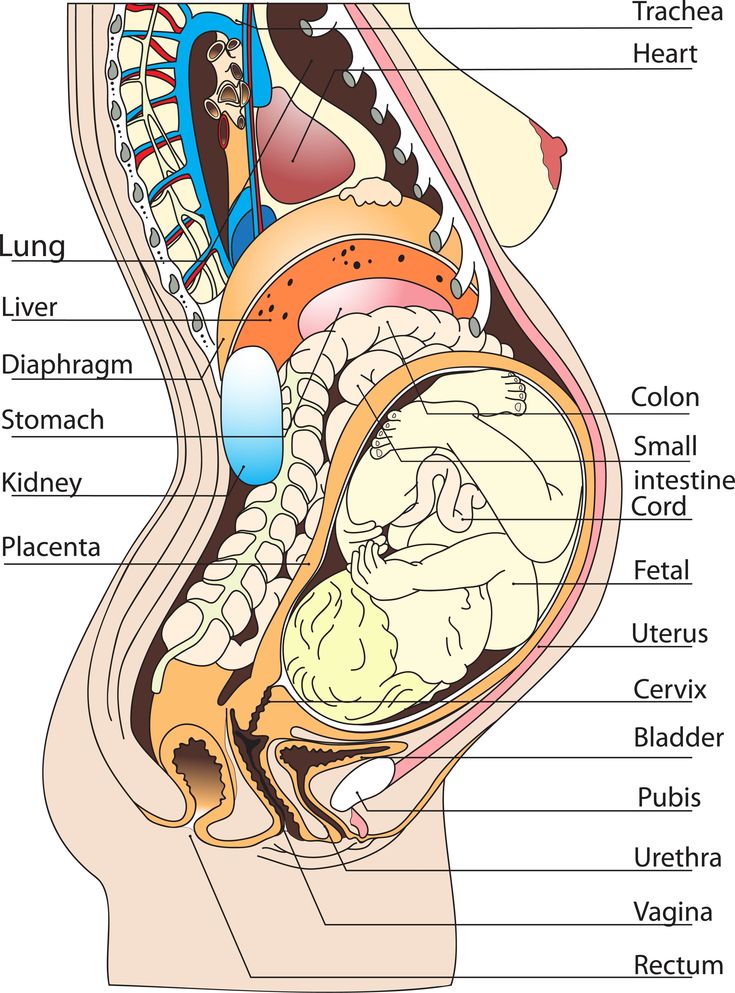 In patients of reproductive age with a burdened obstetric and gynecological history, a high frequency of sporadic abortions by the type of non-developing pregnancy is observed [11, 13].
In patients of reproductive age with a burdened obstetric and gynecological history, a high frequency of sporadic abortions by the type of non-developing pregnancy is observed [11, 13].
Currently, the need for immediate termination of a non-developing pregnancy at any gestational age is generally recognized, since prolonged intrauterine retention of the fetal egg against the background of inhibition of its contractile activity of the uterus is accompanied by a high risk of developing infectious and hemostasiological complications [10, 15, 17]. The traditional tactic for a non-developing pregnancy is the surgical evacuation of a dead fetal egg. Although instrumental curettage of the walls of the uterine cavity is a highly effective method of treatment and allows you to achieve results in the shortest possible time, it has its drawbacks. These include bleeding, infectious complications, trauma to the cervix and body of the uterus, Asherman's syndrome, infertility, and possible complications of anesthesia.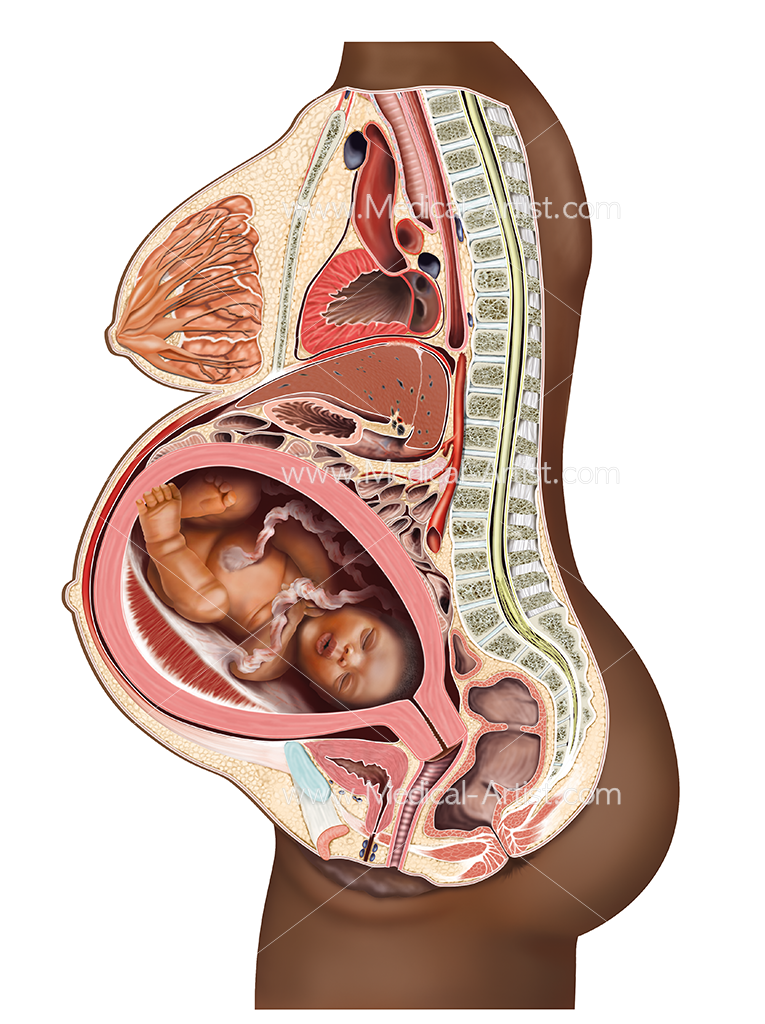 The complication rate averages 5.8% [15, 26]. After the removal of a dead fetal egg, the process of endometrial recovery is longer than after artificial abortion [2, 7, 15].
The complication rate averages 5.8% [15, 26]. After the removal of a dead fetal egg, the process of endometrial recovery is longer than after artificial abortion [2, 7, 15].
Thus, the traditional curettage of the walls of the uterine cavity contributes to additional traumatization of the endometrium and exacerbation of existing pathogenetic disorders, which can complicate the onset and course of subsequent pregnancy. Therefore, the issues of using modern methods of evacuating a dead fetal egg (fetus), which allow avoiding complications of surgical abortion, are extremely relevant.
Currently, medical termination of pregnancy using antiprogestogens, the active ingredient of which is mifepristone - synthetic 19, is being considered as a sparing method of early pregnancy termination-norsteroid, specifically blocking progesterone and glucocorticoid receptors. The mechanism of early termination of pregnancy is presumably associated with the blockade of progesterone receptors in the glandular cells of the endometrium, which alters the metabolism of prostaglandins.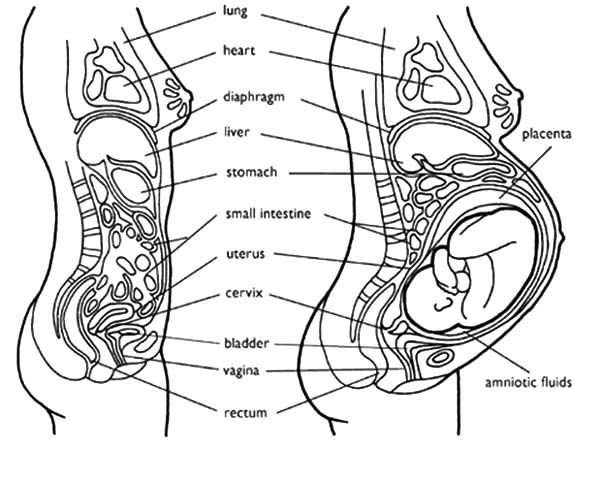 Under the influence of mifepristone, decidualization of the endometrium is prevented, structural changes occur in the capillaries of the decidua at the ultrastructural level, which leads to rejection of the implanted embryo [1, 16, 24]. Mifepristone promotes the synthesis of prostaglandins in the epithelium of the decidual glands and the inhibition of prostaglandin dehydrogenase [20, 40]. The resulting increase in prostaglandin concentrations induce uterine contractions. In some cases, this effect is enough to expel the fetal egg from the uterus. However, in most cases, the isolated use of mifepristone does not provide adequate contractility of the myometrium, so it is used in combination with a prostaglandin analogue, misoprostol [20, 29].
Under the influence of mifepristone, decidualization of the endometrium is prevented, structural changes occur in the capillaries of the decidua at the ultrastructural level, which leads to rejection of the implanted embryo [1, 16, 24]. Mifepristone promotes the synthesis of prostaglandins in the epithelium of the decidual glands and the inhibition of prostaglandin dehydrogenase [20, 40]. The resulting increase in prostaglandin concentrations induce uterine contractions. In some cases, this effect is enough to expel the fetal egg from the uterus. However, in most cases, the isolated use of mifepristone does not provide adequate contractility of the myometrium, so it is used in combination with a prostaglandin analogue, misoprostol [20, 29].
Mifepristone 600 mg with a prostaglandin analog administered 36-48 hours later is recommended for early medical abortion. Since the approval of this method in most countries, where the use of mifepristone for early termination of pregnancy is allowed, clinical studies have been focused mainly on finding the optimal scheme for this procedure.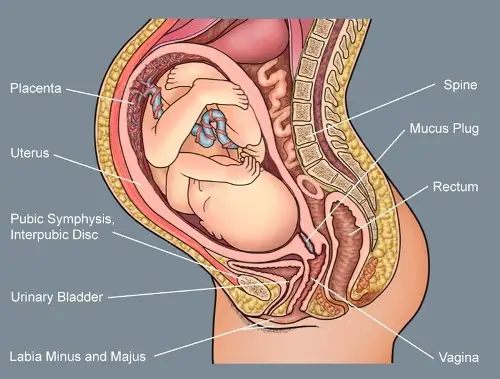 Studies have not revealed a relationship between the dose of mifepristone and the effectiveness of abortion in the early stages: when performing an abortion in the first trimester of pregnancy, the effectiveness of a dose of mifepristone 600 mg and a single dose of 200 mg followed by the introduction of prostaglandin is the same [4, 9, 32].
Studies have not revealed a relationship between the dose of mifepristone and the effectiveness of abortion in the early stages: when performing an abortion in the first trimester of pregnancy, the effectiveness of a dose of mifepristone 600 mg and a single dose of 200 mg followed by the introduction of prostaglandin is the same [4, 9, 32].
However, the use of these drugs to empty the uterine cavity during non-developing pregnancy has not yet been widely used in our country due to insufficient data on their efficacy and safety. At the all-Russian seminar "Reproductive potential of Russia: from safe abortion and contraception to safe childbirth", held in Kazan in 2010, V.E. Radzinsky called for finding the possibility of using medical abortion technology for non-developing pregnancies.
We conducted a review of foreign literature on this issue. To date, there have been several randomized and prospective trials using mifepristone and misoprostol to terminate a miscarriage. Some of them are presented in table. Studies vary in quality and methodology, selection criteria, drug dosages, schedules, and evaluation of outcomes.
Some of them are presented in table. Studies vary in quality and methodology, selection criteria, drug dosages, schedules, and evaluation of outcomes.
H. El-Refaey et al. at 1992 g. in 60 women with non-developing pregnancy in a period of less than 13 weeks, mifepristone at a dose of 600 mg was used, followed after 36-48 hours by misoprostol at a dose of 600 mcg in two stages (400 mcg, after 2 hours 200 mcg). Complete abortion occurred in 92% of cases. Similar results were obtained by C. Lelaidier et al. (1993), who used mifepristone 600 mg orally without prostaglandins in 23 women with non-progressive pregnancies. According to them, mifepristone was effective in 82% of cases compared with 8% in the placebo group.
In order to determine the optimal dose of mifepristone, L. Coughlin et al. [27] compared the results of medical termination of non-developing pregnancy using 200 mg (in 60 women) and 600 mg (in 44 women) of mifepristone in combination in both groups with 400 μg of misoprostol taken 48 hours later in two divided doses. 200 mcg with an interval of 2 hours. In the 1st group of patients, a positive result was achieved in 82% of cases, in the 2nd group - in 84% of cases. The authors concluded that the use of mifepristone at a lower dose does not reduce its effectiveness, but is better tolerated by patients.
200 mcg with an interval of 2 hours. In the 1st group of patients, a positive result was achieved in 82% of cases, in the 2nd group - in 84% of cases. The authors concluded that the use of mifepristone at a lower dose does not reduce its effectiveness, but is better tolerated by patients.
Methods of administration of misoprostol have been widely discussed by investigators [21, 22, 25, 31, 33, 37, 38, 43, 44], with preference given to the vaginal route of administration due to greater efficacy and better tolerability. With oral administration, the maximum concentration of the drug in the blood is reached after 15-30 minutes, with vaginal administration - after 60 minutes and remains in the blood longer, this explains a longer clinical effect [43, 44]. It is promising to study the effectiveness of sublingual administration of misoprostol [20].
G. Ara et al. [22] in 2009 published the results of vaginal use of misoprostol in 300 women with non-developing pregnancy up to 12 weeks: after 24 hours, uterine emptying occurred in 84% of cases, after 48 hours - in 91% of cases, after 7 days - in 92 % of patients. According to the authors, expectant management improves the results of the drug.
According to the authors, expectant management improves the results of the drug.
N. Ncog et al. [34] compared the efficacy of oral (n=100) and vaginal (n=98) misoprostol 800 mcg in non-progressive pregnancies. Complete expulsion of the ovum from the uterine cavity with vaginal misoprostol occurred at 92.9% of cases, with oral administration - in 89%. The average duration of abortion from the moment of taking the drug to complete emptying of the uterine cavity with the oral route of administration (21.04 hours) was significantly longer than with the vaginal route (13.47 hours; p=0.041).
An interesting work by R. Machtinger et al. [33] in which they compared the efficacy of two doses of misoprostol 400 mcg given vaginally followed by oral administration 24–72 h apart in 220 patients with spontaneous non-pregnancy (n=167) and after assisted reproductive technologies (n= 53). Treatment success was 72.5 and 92.4% respectively.
A number of studies have investigated the efficacy of misoprostol without prior administration of mifepristone in non-progressive pregnancies. The authors suggested that due to abnormal implantation of the ovum and low progesterone levels, the use of an antiprogestogen was not necessary. At the same time, there were no significant differences in the results of medical termination of non-developing pregnancy using misoprostol in combination with mifepristone and without its prior administration. So, according to A. Gronlund et al. [31], who used mifepristone 600 mg orally 48 hours later and misoprostol 400 mcg (200 mcg every 2 hours) vaginally (n=54) and two doses of misoprostol 200 mcg vaginally every 2 hours (n=73), effectiveness amounted to 74 and 71%, respectively. In the study by D. Stockheim et al. [42] in 115 women with missed abortions less than 9weeks compared the efficacy and safety of two different regimens: taking mifepristone 600 mg + misoprostol 800 mcg and taking two doses of misoprostol 800 mcg with an interval of 48 hours. Efficiency was 65.5 and 73.6%, respectively.
The authors suggested that due to abnormal implantation of the ovum and low progesterone levels, the use of an antiprogestogen was not necessary. At the same time, there were no significant differences in the results of medical termination of non-developing pregnancy using misoprostol in combination with mifepristone and without its prior administration. So, according to A. Gronlund et al. [31], who used mifepristone 600 mg orally 48 hours later and misoprostol 400 mcg (200 mcg every 2 hours) vaginally (n=54) and two doses of misoprostol 200 mcg vaginally every 2 hours (n=73), effectiveness amounted to 74 and 71%, respectively. In the study by D. Stockheim et al. [42] in 115 women with missed abortions less than 9weeks compared the efficacy and safety of two different regimens: taking mifepristone 600 mg + misoprostol 800 mcg and taking two doses of misoprostol 800 mcg with an interval of 48 hours. Efficiency was 65.5 and 73.6%, respectively.
According to a number of authors [22, 31, 33, 36], the factors determining the success of medical management of non-developing pregnancy include low parity and a short gestational age. It is known that repeated mechanical trauma to the endometrium causes its morphological and functional inferiority, damage to the receptor apparatus, the development of chronic endometritis, and can cause the ineffectiveness of medical abortion [22, 36]. The risk of failure is significantly higher in patients who have had at least five previous pregnancies (of which 3 abortions or more) than in patients with a history of one or two pregnancies, as well as in a pregnancy that occurred in a natural cycle, compared with pregnancy after ovulation induction [33].
It is known that repeated mechanical trauma to the endometrium causes its morphological and functional inferiority, damage to the receptor apparatus, the development of chronic endometritis, and can cause the ineffectiveness of medical abortion [22, 36]. The risk of failure is significantly higher in patients who have had at least five previous pregnancies (of which 3 abortions or more) than in patients with a history of one or two pregnancies, as well as in a pregnancy that occurred in a natural cycle, compared with pregnancy after ovulation induction [33].
Of note, none of the studies reported cases of severe bleeding requiring a blood transfusion following medical termination of a miscarriage. So, A. Davis et al. [28] studied the duration and volume of bleeding in 80 women with a missed pregnancy of less than 11 weeks with vaginal misoprostol 800 mcg. The duration of bleeding, according to their data, was 12-14 days, according to H. El-Refaey et al. in 1992 - 2-22 days (average 7 days).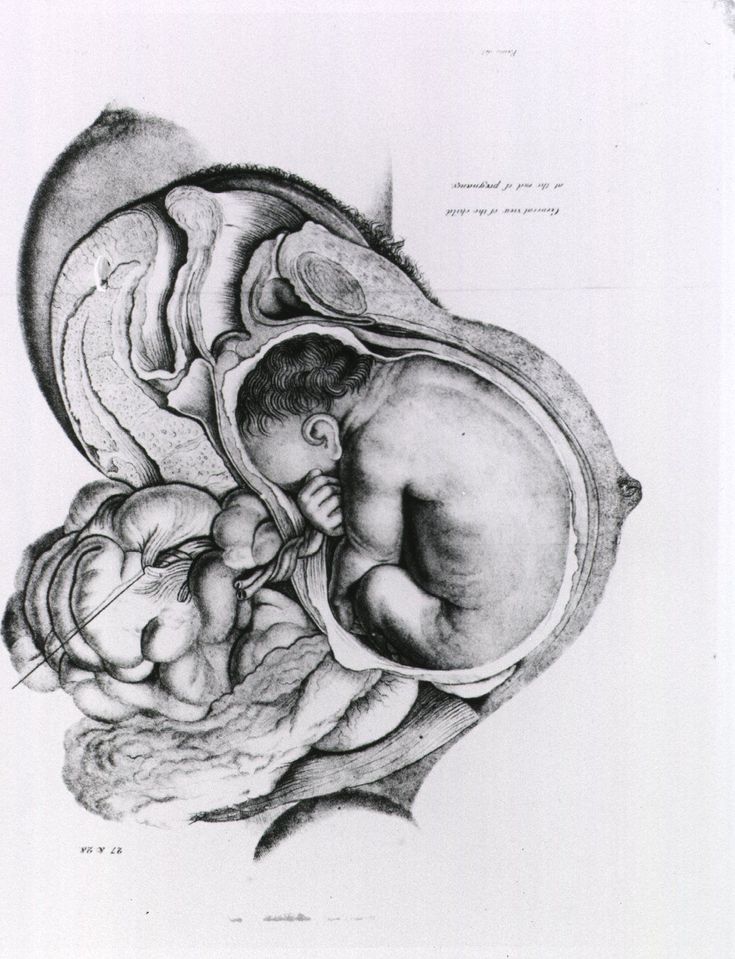 The volume of blood loss was determined by the number of pads used - an average of 30.5 pieces (from 2 to 125) for 2 weeks. There was no significant difference in hemoglobin levels before abortion and 14 days after it [28, 33].
The volume of blood loss was determined by the number of pads used - an average of 30.5 pieces (from 2 to 125) for 2 weeks. There was no significant difference in hemoglobin levels before abortion and 14 days after it [28, 33].
The incidence of infectious complications when using mifepristone in combination with misoprostol in women with non-developing pregnancy, according to A. Gronlund et al. [31], is 1.9%, while when using misoprostol without mifepristone and surgical evacuation, it was the same and amounted to 1.4%. It should be noted that G.B. Dicke and D.M. Kochev [5], in their work on the complications of artificial termination of an unwanted pregnancy in the first trimester, indicate the frequency of this complication after medical termination of a progressing pregnancy is less than 1%.
Several randomized controlled trials in a sufficient number of subjects have compared the options for medical and surgical treatment of incomplete miscarriage and non-developing early pregnancy.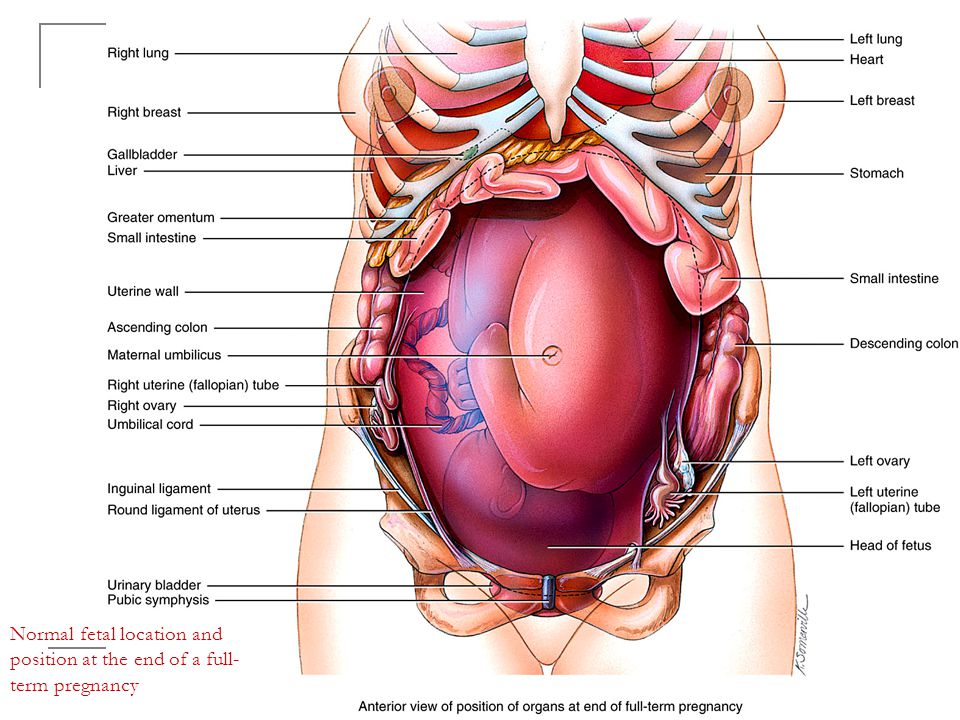 The MIST study (miscarriage treatment - treatment of spontaneous abortion) showed a significantly higher incidence of emergency hospitalization and unscheduled procedures for surgical curettage of the walls of the uterus during expectant management and after medical abortion than after surgical treatment, although the risk of infection was low and amounted to 2-3% , regardless of the method of treatment [45].
The MIST study (miscarriage treatment - treatment of spontaneous abortion) showed a significantly higher incidence of emergency hospitalization and unscheduled procedures for surgical curettage of the walls of the uterus during expectant management and after medical abortion than after surgical treatment, although the risk of infection was low and amounted to 2-3% , regardless of the method of treatment [45].
A. Sotiriadis et al. [39] presented the results of a meta-analysis of works devoted to the quantitative assessment of the relative benefits and risks of various methods of managing spontaneous abortion in the first trimester. The authors report a higher efficacy of surgical treatment compared to expectant management and medical abortion, but note the low methodological quality of most of the analyzed studies.
Thus, the analysis of the literature on the problem of terminating a non-developing pregnancy indicates the advantage of using medical abortion in early pregnancy over traditional surgical treatment.