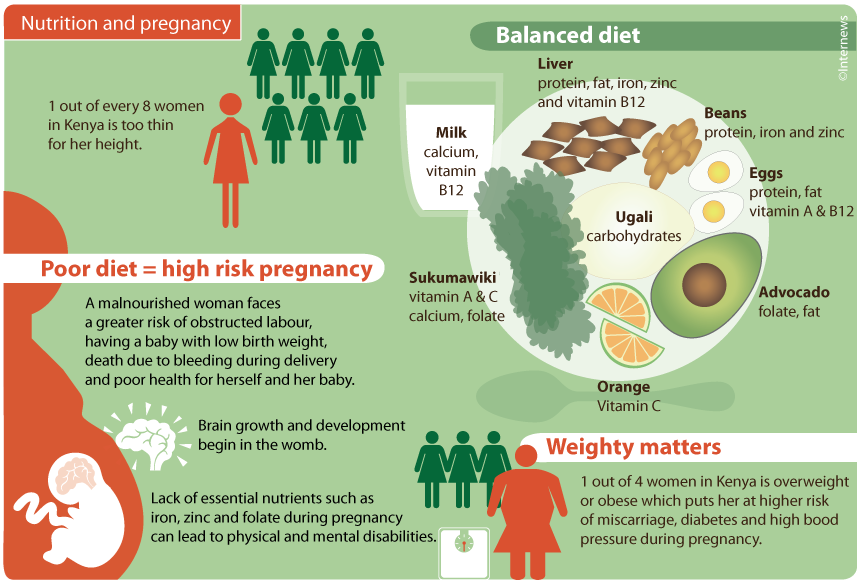
Abdominal muscles separating during pregnancy
Diastasis Recti (Abdominal Separation): Symptoms & Treatment
Overview
Diastasis recti happens when a person's abdomen stretches during pregnancy and creates a gap in the abdominal muscles.What is diastasis recti?
Diastasis recti (diastasis rectus abdominis or diastasis) is the separation of the rectus abdominis muscles during and after pregnancy. The rectus abdominis runs vertically along the front of your stomach. It's frequently referred to as someone's "six-pack abs." It's divided into left and right sides by a band of tissue called the linea alba that runs down the middle. As your uterus expands during pregnancy, the abdominals are stretched and the linea alba thins and pulls apart. This band of tissue gets wider as it's pushed outward.
Once you deliver your baby, the linea alba can heal and come back together. It's highly elastic and retracts backs (like a rubber band). When the tissue loses its elasticity from being overstretched, the gap in the abdominals will not close as much as it should. This is diastasis recti.
If you have diastasis, your belly may appear to stick out just above or below the belly button, making you appear pregnant months or years after giving birth.
Why does diastasis recti happen?
Pregnancy puts a lot of pressure on your abdomen (abs). The abdomen is made up of left and right ab muscles and a thin band of connective tissue (linea alba) in between. They are pushed outward and stretched to make room for the growing baby. Diastasis recti occurs when the linea alba is overstretched and doesn't come back together. The left and right sides of the abdominals stay separated. It's also referred to as an "ab gap" or abdominal separation.
Who gets diastasis recti?
Diastasis recti is most common in pregnant and postpartum women (it can also be seen in men and infants). Diastasis recti usually develops in the third trimester. There is increased pressure on the abdominal wall because the baby is growing quickly during this time. Most people don't notice diastasis recti until the postpartum period.
How common is diastasis recti?
Diastasis recti is extremely common in those who are pregnant and during the postpartum period. It affects 60% of people. It usually resolves itself within eight weeks of delivery. About 40% of those who have diastasis recti still have it by six months postpartum.
Symptoms and Causes
What are the symptoms of diastasis recti?
Most people don't notice signs of diastasis recti until they are postpartum. You can have diastasis recti during pregnancy, but it's hard to distinguish because your abdomen is stretched.
Common signs of diastasis recti during the postpartum period are:
- A visible bulge or "pooch" that protrudes just above or below the belly button.
- Softness or jelly-like feeling around your belly button.
- Coning or doming when you contract your ab muscles.
- Difficulty lifting objects, walking or performing everyday tasks.
- Pain during sex.
- Pelvic or hip pain.

- Low back pain.
- Poor posture.
- Urine leaking when you sneeze or cough.
- Constipation.
- Feeling weak in your abdominals.
What does diastasis recti feel like?
Diastasis recti is not painful. You may feel pain associated with some of the side effects of diastasis, but the ab separation itself doesn't hurt. You may feel weakness in your core when doing once easy tasks, like lifting a laundry basket. Some people feel a jelly-like texture in the space between the left and right abdominals when contracting the ab muscles.
How do I know if I have diastasis recti?
There are some common signs that can signal you have diastasis recti. One of the most common signs of diastasis recti is a bulge in your midsection that doesn't go away, even after exercising or losing weight gained during pregnancy. Another sign is that your belly cones or domes when you lean back on a chair or get up out of bed. You can check for diastasis recti on your own, but it is always a good idea to speak with your healthcare provider about your symptoms.
What are the risk factors for developing diastasis recti?
Several factors can increase your risk for developing diastasis recti:
- Having multiple pregnancies (especially back-to-back).
- Being over 35 years old.
- Having multiples (such as twins or triplets).
- Having a heavy or big baby.
- Being extremely petite.
- Vaginal delivery. Pushing can increase abdominal pressure.
Diagnosis and Tests
How is diastasis recti diagnosed?
Your healthcare provider will evaluate if diastasis is present, where it's located and how severe it is. Diastasis recti can occur above the belly button, below the belly button and at the belly button.
Your provider will use their hands and fingers to feel the abdominal area for gaps and muscle tone. Some providers may use ultrasound, measuring tape or a tool called a caliper for a more accurate measurement. This exam typically occurs at your postpartum appointment before being cleared for exercise.
An abdominal gap wider than 2 centimeters is considered diastasis recti. Diastasis recti is also measured in finger widths, for example, two or three fingers' separation.
Your healthcare provider may recommend movements for diastasis recti or they may refer you to a specialist for additional treatment.
How do I test myself for diastasis recti?
You can test yourself for diastasis recti:
- Lie on your back with your knees bent and feet flat on the floor.
- Lift your shoulders slightly off the ground, keeping one hand behind your head for support. Almost like you are doing a sit-up. Look down at your belly.
- Move your other hand above your belly button area, palms down and fingers towards your toes.
- Use your fingers to feel for a gap between the abs. See how many fingers can fit in the gap between your right and left abdominals.
If you feel a gap of two or more finger widths, discuss your concerns with your healthcare provider. They should confirm diastasis recti with a proper diagnosis and recommend appropriate care.
They should confirm diastasis recti with a proper diagnosis and recommend appropriate care.
Management and Treatment
How can I fix diastasis recti?
To fix diastasis recti, you'll need to perform gentle movements that engage the abdominal muscles. Before starting an exercise program, be sure it's safe for diastasis recti. Work with a fitness professional or physical therapist who has experience with diastasis recti. They can create a treatment plan to make sure you are performing the movements correctly and progressing to more challenging movements at the right time.
Certain movements will make abdominal separation worse. During the postpartum period, there are some modifications you should make:
- Avoid lifting anything heavier than your baby.
- Roll onto your side when getting out of bed or sitting up. Use your arms to push yourself up.
- Skip activities and movements that push your abdominals outward (like crunches and sit-ups).
Some people use binding devices (elastic belly bands) to help hold their belly in and support the lower back.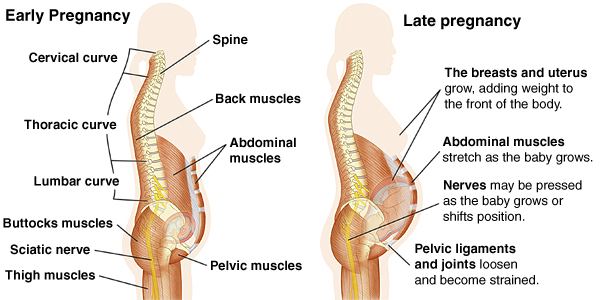 Wearing binders can't heal diastasis recti and will not strengthen your core muscles. It can be a good reminder of your diastasis recti and promote good posture.
Wearing binders can't heal diastasis recti and will not strengthen your core muscles. It can be a good reminder of your diastasis recti and promote good posture.
Can you fix diastasis recti without surgery?
Yes, it's possible to fix diastasis recti without surgery. Surgery is rarely performed to fix diastasis recti. Healthcare providers will recommend physical therapy or at-home exercises to help heal diastasis before surgical methods. Surgery is performed in cases of hernia (when an organ pushes through the linea alba) or if a woman wants diastasis recti surgery (a tummy tuck).
What are the best exercises for diastasis recti?
The best exercises for diastasis recti are those that engage the deep abdominals. Most diastasis recti exercises involve deep breathing and slow, controlled movements. Unfortunately, many of the most common ab exercises (like crunches) can worsen your diastasis. Before starting abdominal exercises, ask your healthcare provider to check you for diastasis recti.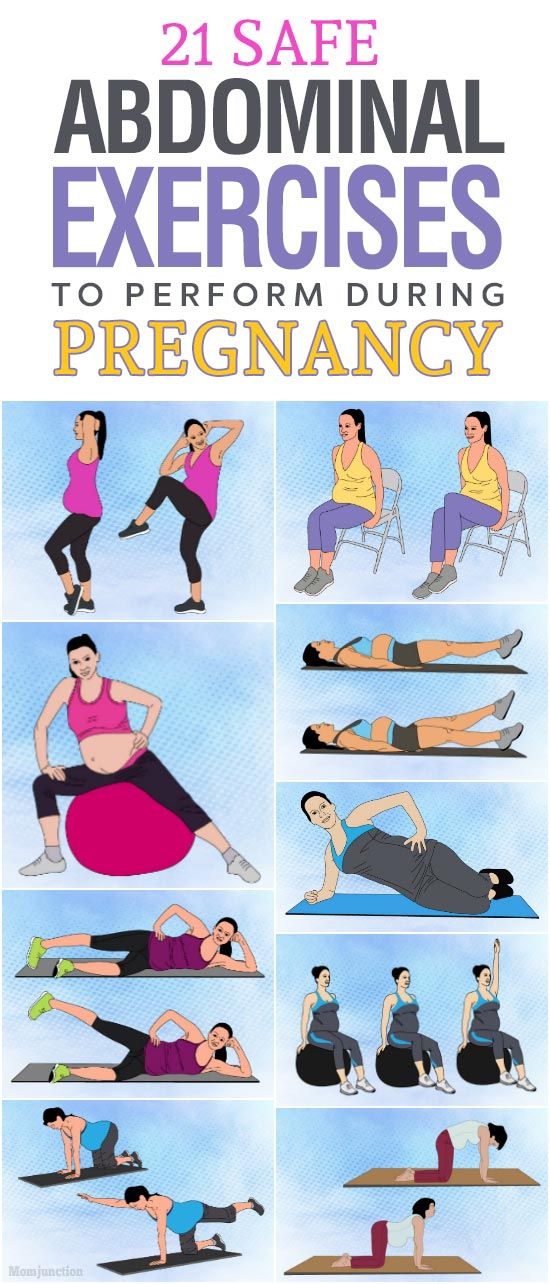
What movements make diastasis recti worse?
Any movement that bulges the abdominal wall forward can cause more damage to your diastasis recti. Everyday movements like getting out of bed or up off a chair can worsen diastasis. Try to be mindful about how you are using your abdominals as you go about your day.
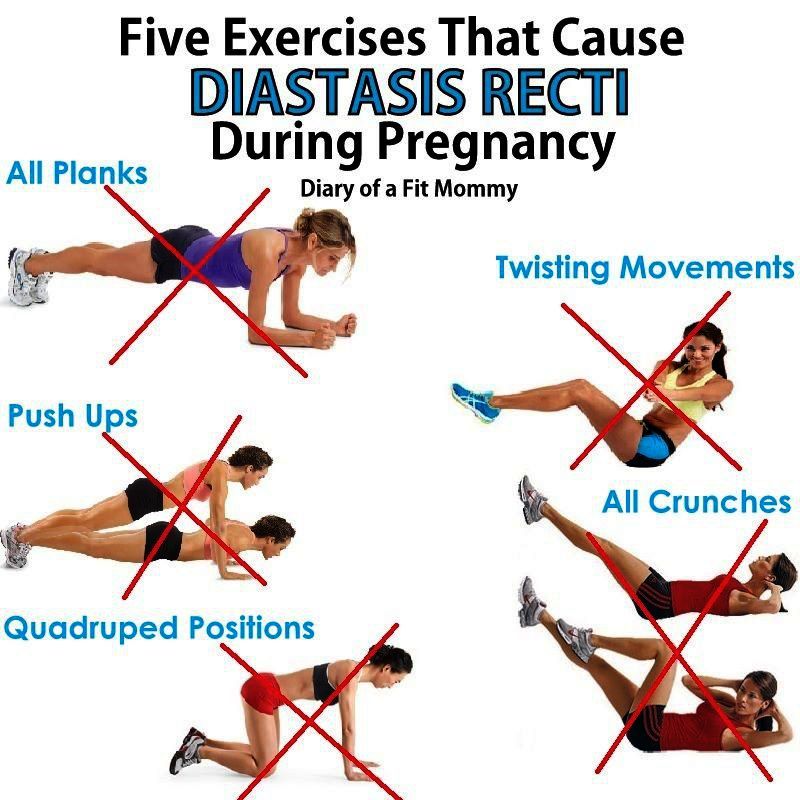
These exercise movements should be avoided if you have diastasis recti:
- Crunches or sit-ups of any kind.
- Planks or push-ups (unless using modifications).
- Downward dog, boat pose and other yoga poses.
- Double leg lifts, scissors and other Pilates moves.
- Any exercise that causes your abdominals to bulge, cone or dome.
Prevention
How do I prevent diastasis recti?
Some abdominal separation is normal and expected with pregnancy. There are some things you can do to lower your risk for developing diastasis recti:
- Healthy weight gain during pregnancy: Exercising and eating healthy foods to keep weight gain within a healthy range.

- Proper posture and deep breathing: Stand up straight with your shoulders back. Take deep breaths that allow your ribs to expand and not just your belly.
- Safe core exercises: Avoid exercises like sit-ups and crunches that put pressure on your abdominals after 12 weeks of pregnancy and postpartum.
- Don't strain while lifting: Certain day-to-day activities like lifting grocery bags or your children can put undue strain on your abdominals.
- Log roll when getting out of bed: If you're pregnant or postpartum, roll to one side and use your arms to push up out of bed.
Outlook / Prognosis
How long will it take to heal my diastasis recti?
The amount of time it takes to heal diastasis recti depends on the amount of ab separation and how consistent you are with strengthening exercises. After several weeks postpartum, this gap will start to close as your muscles regain strength.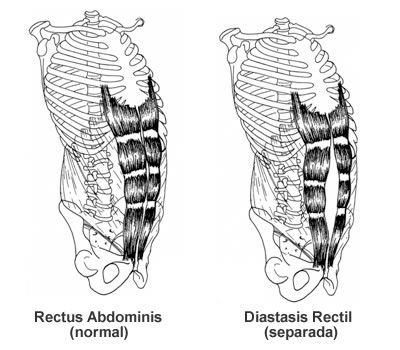 If you're making modifications to your lifestyle and performing exercises with good form, you're more likely to notice progress.
If you're making modifications to your lifestyle and performing exercises with good form, you're more likely to notice progress.
Can I get diastasis recti again?
Yes, you can heal your diastasis recti and get it again. Your risk for diastasis recti increases the more times you are pregnant. Think of the linea alba as a rubber band that is continuously stretched. Over time, the rubber band will lose its elasticity. The linea alba may not regain its original shape or form after being stretched through multiple pregnancies.
Is it too late to fix my diastasis recti?
It's never too late to repair your diastasis recti. With the proper exercises, you can fix your ab separation years after you've delivered your last baby.
Are there complications from diastasis recti?
If left untreated or in severe cases of diastasis recti, complications can include:
- Umbilical hernia.
- Increase in back pain.
- Pain during sex.
- Urinary incontinence.
- Pelvic and hip pain.
Living With
When should I see my healthcare provider?
Diastasis recti is a common and easily treated condition. If you have more than a two-finger gap between your abdominals or are experiencing pain, contact your healthcare provider for a diagnosis. They may want you to see a physical therapist or pelvic floor specialist to help strengthen your abdominal muscles.
A note from Cleveland Clinic:
Diastasis recti can make you appear pregnant years after your last baby. Discuss your concerns with your healthcare provider so they can diagnose and treat you. Getting treatment can help you feel more confident in your body and correct any pain you are experiencing.
Why Ab Separation Happens and How It's Treated
Written by Stephanie Siegel
In this Article
- Dos and Don'ts
- Treatment
“Diastasis recti” means your belly sticks out because the space between your left and right belly muscles has widened.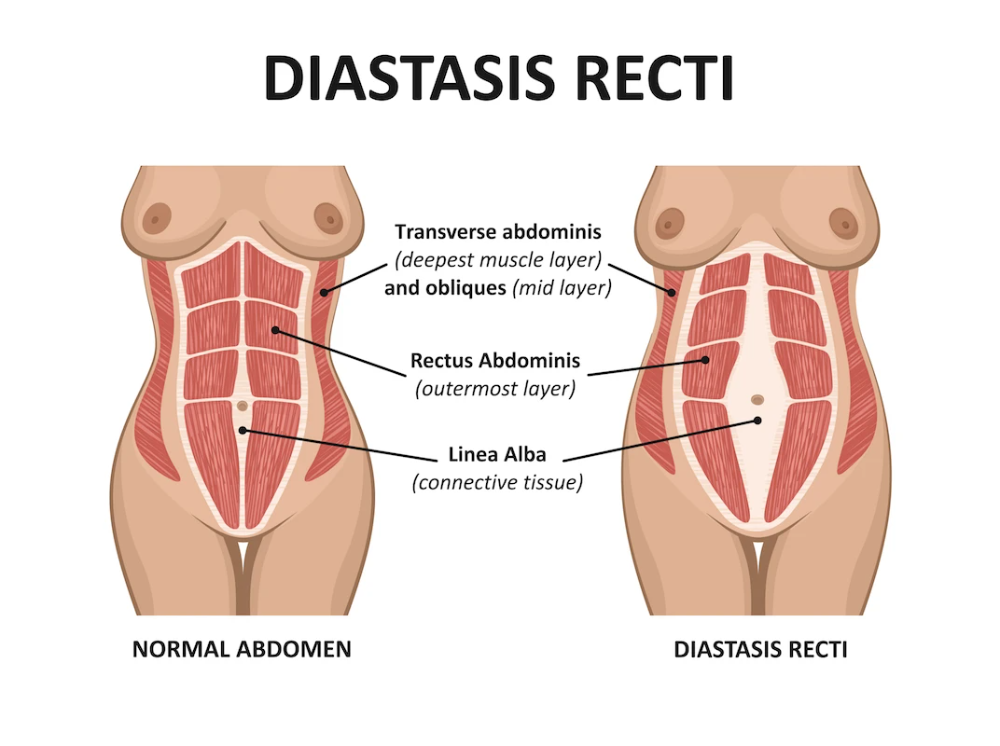 You might call it a “pooch.”
You might call it a “pooch.”
It's very common among pregnant women. About two-thirds of pregnant women have it.
Newborn babies also can have this belly spread, and it should go away on its own. Men can get it, possibly from yo-yo dieting, from doing sit-ups or weightlifting the wrong way, or from other causes.
Having more than one child makes this condition more likely, especially if they’re close in age. You’re also more likely to get it if you’re over 35 when pregnant, or if you’re having a heavy baby or twins, triplets, or more.
Pregnancy puts so much pressure on the belly that sometimes the muscles in front can’t keep their shape. "Diastasis" means separation. "Recti" refers to your ab muscles called the "rectus abdominis."
When the ab muscles move aside like this, the uterus, bowels, and other organs have only a thin band of connective tissue in front to hold them in place. Without the needed muscle support, a vaginal delivery could be more difficult.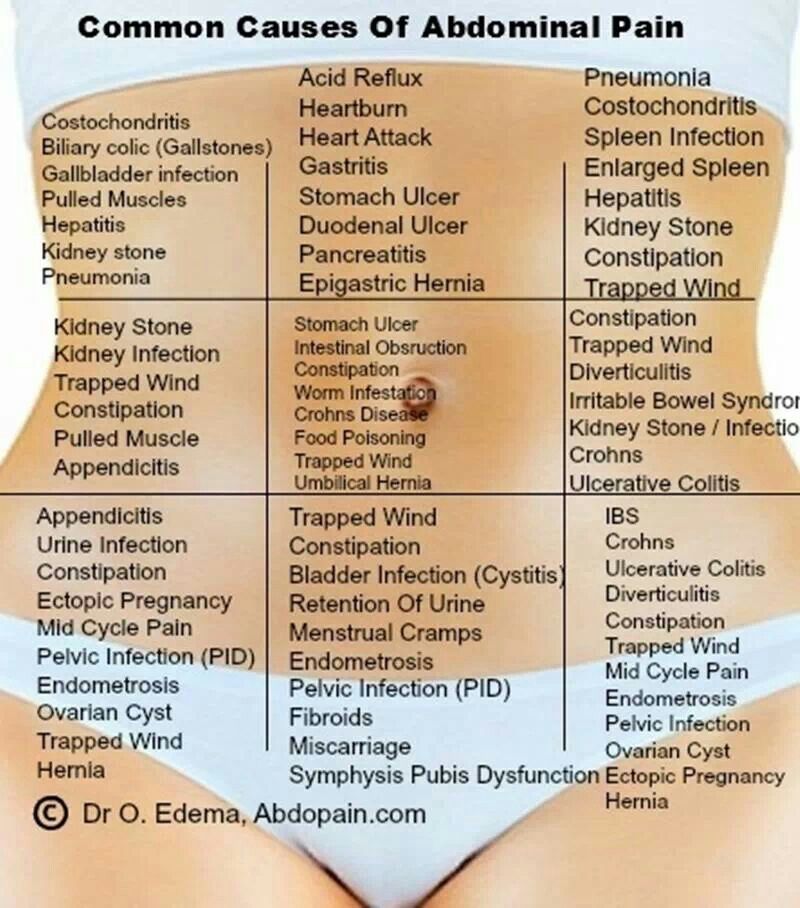
The condition also can cause lower back pain, constipation, and urine leaking. It can even make it harder to breathe and to move normally. It's rare, but in extreme cases, the tissue may tear, and organs may poke out of the opening -- that’s called a hernia.
The muscle opening often shrinks after giving birth, but in some studies of women with diastasis recti, the muscle wasn't back to normal even a year later.
Dos and Don'ts
Don't strain. It can make matters worse. Constipation and lifting heavy things, including your kids, strain that connective tissue. Standing up and sitting down also count as heavy lifting in this case, because you’re lifting your body weight.
You push down when giving birth, but if done wrong, this action puts big pressure on the weak belly tissue.
Do be careful with exercise. Some routine fitness moves, including crunches, sit-ups, pushups, press-ups, and front planks, make abdominal separation worse. So can swimming, some yoga poses (like downward dog), and doing anything on your hands and knees. Some trainers may suggest those exercises for women with abdominal separation, not knowing what could happen.
So can swimming, some yoga poses (like downward dog), and doing anything on your hands and knees. Some trainers may suggest those exercises for women with abdominal separation, not knowing what could happen.
Do heal your belly. Physical therapists don’t have one standard guideline on what moves will bring the belly muscles back into line. Some research found success with the Tupler technique. It involves certain exercises done while wearing a belly splint, which protects and holds the ab muscles together.
When the connective tissue has healed, some Pilates or other exercises may help you strengthen and rely more on your transverse (deep core) belly muscles instead of the outer ones. Not all Pilates or strengthening moves are good during pregnancy, though, so make sure you're working with a trainer who knows what "diastasis recti" means.
The best time to begin core strengthening is before you get pregnant, if you don’t already have an abdominal separation.
Before starting any exercises during or after pregnancy, be sure to ask your doctor what's OK for you to do and what's off-limits for now.
Treatment
If your abdominal separation is not too big, you may decide to live with it. But you should bring those muscles back together before you have another pregnancy.
Your doctor can measure how far apart your muscles are using finger widths, a measuring tape or instrument, or ultrasound. Then they can see whether it's getting better or worse.
Many women can close their belly gap by learning gentle movements to use while the abs are supported. Ask your doctor for advice. They may refer you to a physical therapist.
If that rehab won’t work for you, maybe surgery will. An operation to correct diastasis may be called "abdominoplasty" or "a tummy tuck." The surgeon folds and sews together the weak central ridge.
It might be possible to get laparoscopy, which is surgery done with only small cuts instead of one large one. Scarring, infection, and other side effects are possible with any operation.
Scarring, infection, and other side effects are possible with any operation.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Diastasis of the rectus abdominis muscles and diastasis of the womb. Solvable problems of pregnancy. Interview with Doctor of Medical Sciences, Professor M.A. Chechnevoy
— What is muscle diastasis and what is pubic symphysis diastasis?
— Pregnancy is an amazing and wonderful time, but it is also a period of additional loads, which undoubtedly becomes a test of strength for the female body.
The previously existing everyday point of view that pregnancy rejuvenates and gives strength is not confirmed by anything. During the bearing of a child, significant additional loads are placed on the mother's body, which often lead to the manifestation of problems that were invisible before pregnancy.
Diastasis of the rectus abdominis muscles is a divergence of the inner edges of the muscles along the white line of the abdomen (connective tissue structure) at a distance of more than 27 mm. Pubic diastasis is one of the manifestations of pregnancy-associated pelvic girdle pain. This pathology affects the entire pelvic ring, sacroiliac joints and symphysis. And they certainly have common causes for the appearance.
The formation of such problems is facilitated by a decrease in the strength of connective tissue collagen. One of the reasons is an innate predisposition, the so-called connective tissue dysplasia, when the tissues are very elastic, extensible. During pregnancy, the body of a woman increases the production of the hormone relaxin, which reduces the synthesis of collagen and enhances its breakdown. This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin.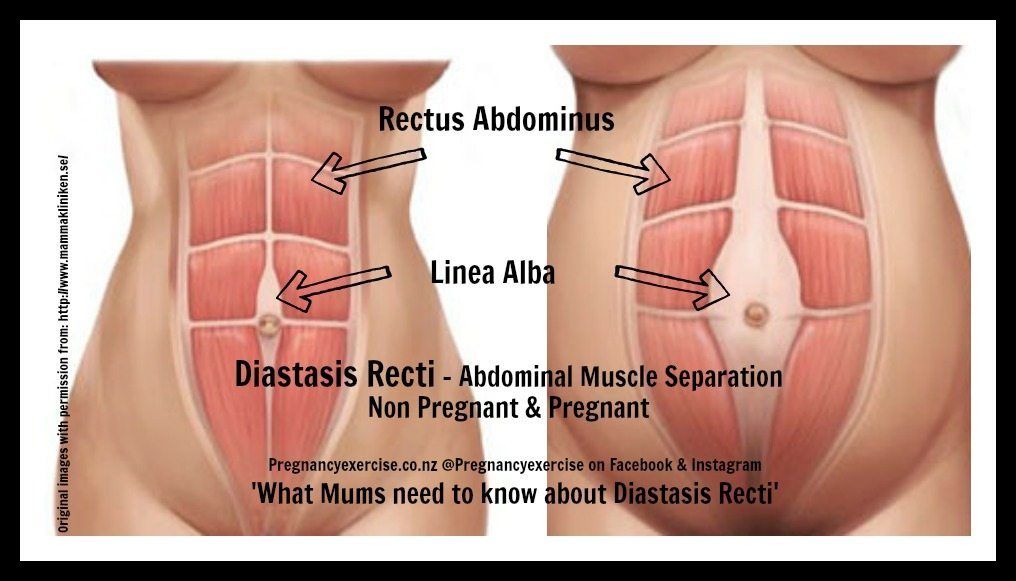
— How does diastasis of the muscles and diastasis of the pubis affect pregnancy and childbirth?
- The divergence of the rectus abdominis muscles is observed in about 40% of pregnant women. During pregnancy, it does not give serious complications that threaten the life of the mother or the condition of the fetus. However, the inferiority of the work of the rectus abdominis muscles forces the redistribution of the load on the back muscles, which can lead to lumbar-pelvic pain and, accordingly, discomfort in the back. During childbirth, the abdominal muscles are involved in attempts, and the violation of their anatomy and function can affect the birth act.
With diastasis of the pubis, things are more complicated. As already mentioned, this is only one of the manifestations of a violation of the structure and function of the pubic joint (symphysiopathy) during pregnancy. It occurs in about 50% of pregnant women in varying degrees of severity: in 25% of cases it leads to restriction of the mobility of the pregnant woman, in 8% - to severe disorders up to disability.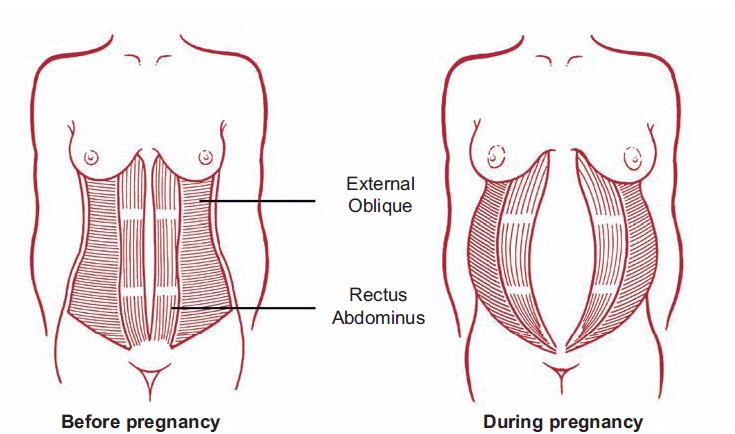
With symphysiopathy, the ligaments of the pubic articulation and the cartilages that connect the pubic bones are affected. All this leads to severe pain in the pubic joint, pelvic bones, lower back, as well as to a violation of gait and the inability to stand up or lie down without outside help. Women with pelvic girdle pain syndrome experience significant levels of discomfort, disability, and depression, with associated social and economic problems. These include impaired sexual activity during pregnancy, chronic pain syndrome, risk of venous thromboembolism due to prolonged immobility, and even seeking early induction of labor or caesarean section to stop pain.
During childbirth, this patient may experience rupture of the pubic symphysis and may require surgery to repair it.
— How to prevent the development of muscle and pelvic diastasis during pregnancy and childbirth? What factors increase the likelihood of its development?
- There is no recipe that will be one hundred percent.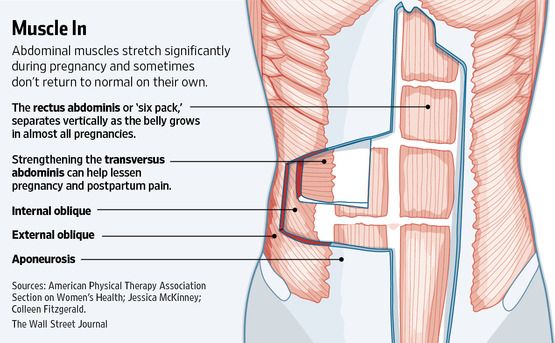 There is a wonderful term in the medical literature called "lifestyle modification". Whatever diseases we study, be it symphysiopathy, diabetes mellitus or preeclampsia, the risk group for pathology is always overweight women. You need to prepare for pregnancy, you need to be in good physical shape. During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis.
There is a wonderful term in the medical literature called "lifestyle modification". Whatever diseases we study, be it symphysiopathy, diabetes mellitus or preeclampsia, the risk group for pathology is always overweight women. You need to prepare for pregnancy, you need to be in good physical shape. During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis.
The risk factors for symphysiopathy in numerous studies are hard physical labor and previous injuries of the pelvic bones. Factors such as time elapsed from previous pregnancies, smoking, use of hormonal contraception, epidural anesthesia, mother's ethnicity, number of previous pregnancies, bone density, weight and gestational age of the fetus (post-term fetus) are not associated with an increased risk of symphysiopathy.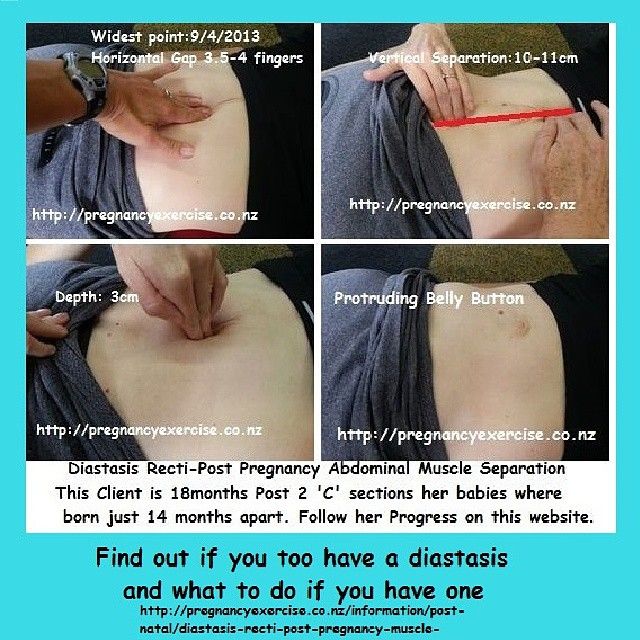
— How to diagnose diastasis recti and diastasis pubis?
— In most cases, diastasis rectus abdominis can be diagnosed clinically. It happens that inspection, palpation and simple measurements are enough.
In the standing position, you can see the divergence of the muscles when the woman does not have subcutaneous fat. In this case, diastasis is defined as a vertical defect between the rectus muscles.
With tension of the abdominal press, a longitudinal protrusion is observed in the diastasis zone. Such a protrusion is especially noticeable if the patient in the supine position is asked to raise her head and legs. If necessary, you can measure the width of the defect simply with a ruler.
Ultrasound may be the most accurate diagnostic method. With ultrasound, the inner edges of the rectus muscles are clearly visible and the distance between them at different levels can be measured.
Computed tomography is used in the diagnosis of diastasis extremely rarely, mainly in scientific research.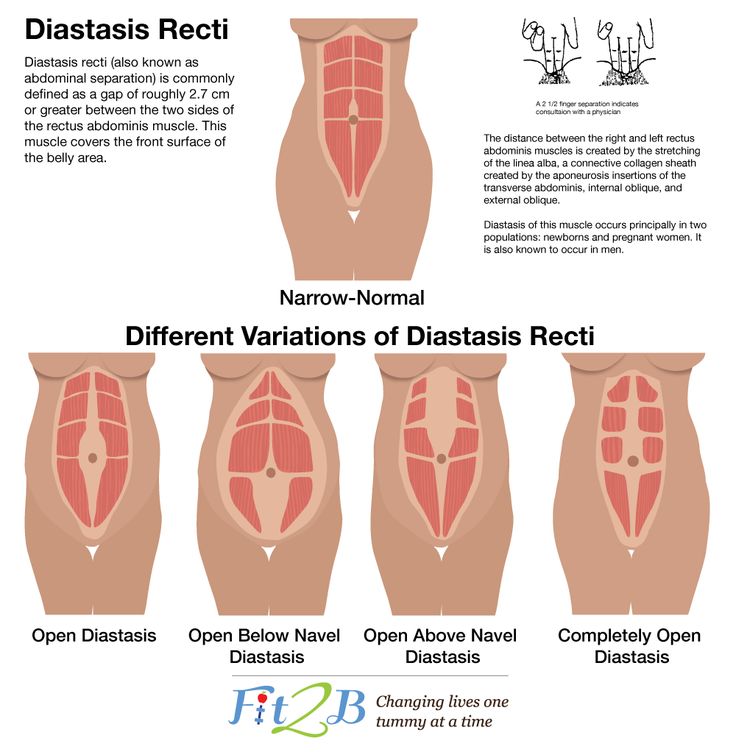
For the diagnosis of symphysiopathy and diastasis pubis there is no one test as a "gold standard".
The first place, of course, is the questioning and examination of the patient. We pay attention to the gait of the pregnant woman, to how she sits down, lies down and how she gets up. Symphysiopathy is characterized by a “duck gait”, when a pregnant woman rolls from foot to foot. On palpation in the area of the womb, pain and swelling are noted. The so-called pain provocative tests are used, for example, a mat-test (pulling up an imaginary rug, mat with your foot towards you).
The following questionnaires are used to assess quality of life, pain and disability: Health-Related Quality of Life (HRQL), Oswestry Disability Index (ODI), Disability Rating Index (DRI), Edinburgh Postpartum Depression Scale (EPDS), Pregnancy Mobility Index (PMI), and Pelvic Ring Score (PGQ).
Of the instrumental methods, ultrasound is the most widely used, less often computed or magnetic resonance imaging.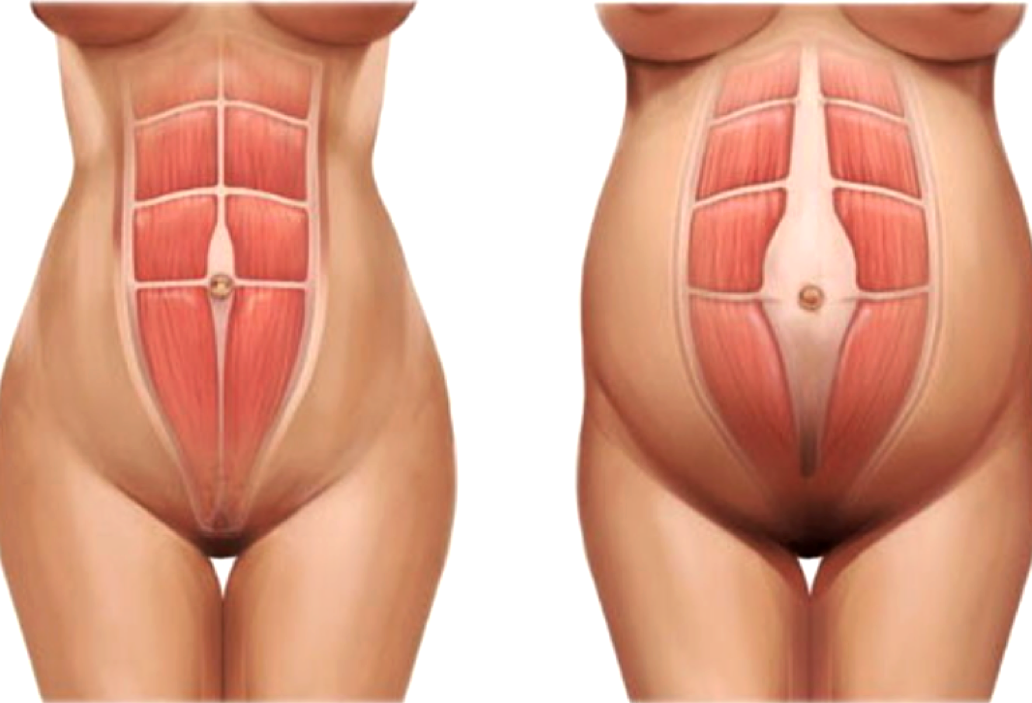 Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth.
Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth.
— What is the treatment for diastasis recti or pubis?
— Primary prevention: when planning and during pregnancy, it is necessary to strengthen all muscle groups of the pelvic girdle, as well as the pelvic diaphragm.
More often, diastasis of the rectus muscles disappears on its own during the first months after childbirth. Special physical exercises to correct the work of muscles, to tone them and restore their basic functions should be performed under the guidance of a competent instructor. There are types of physical exercises that can, on the contrary, worsen the situation with diastasis of the rectus abdominis muscles. In some cases, when there is no effect from physiotherapy exercises, it is necessary to resort to surgical correction of the defect. Currently, both endoscopic and open surgery are practiced.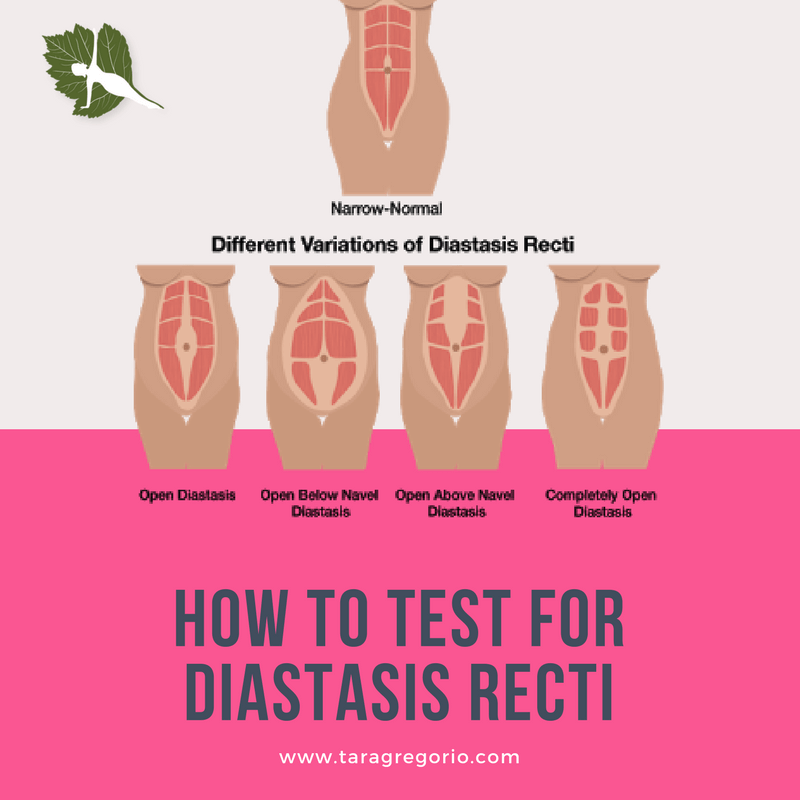 The choice of method depends on the size and localization of the defect.
The choice of method depends on the size and localization of the defect.
With symphysiopathy, therapeutic exercises reduce lumbar and pelvic pain. Acupuncture and wearing a pelvic bandage have a positive effect on symphysiopathy.
Initial treatment of pubic symphysis should be conservative even if symptoms are severe. Treatment includes bed rest and the use of a pelvic brace or corset that tightens the pelvis. Early appointment of physiotherapy with dosed therapeutic exercises will help to avoid complications associated with prolonged immobilization. Walking should be done with assistive devices such as walkers.
In most cases (up to 93%), the symptoms of dysfunction of the pelvic ring, including the pubic joint, progressively subside and completely disappear six months after birth. In other cases, it persists, becoming chronic. However, if the diastasis exceeds 40 mm, then surgical treatment may be required. Most studies recommend surgery only after failure of conservative treatment, inadequate enlargement of diastasis, or its recurrence.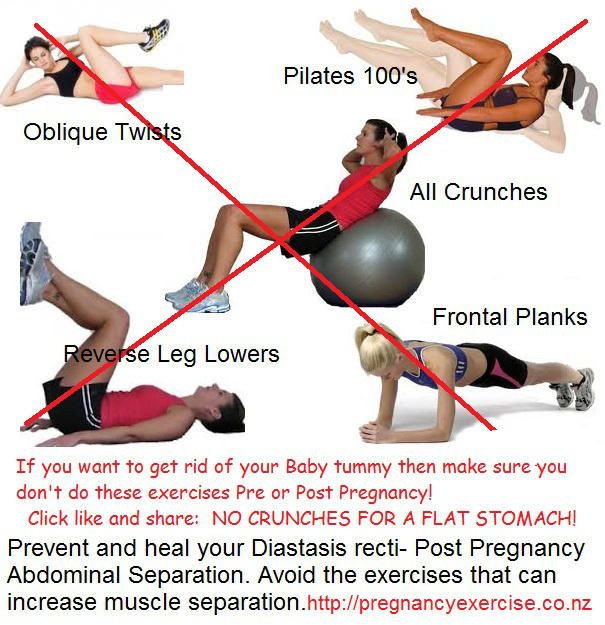 Several procedures have been described, including external fixation and open reduction of the pubic bones with internal fixation.
Several procedures have been described, including external fixation and open reduction of the pubic bones with internal fixation.
The best advice for prevention, diagnosis and treatment: ask a competent doctor all the questions that worry you. Only the joint efforts of the doctor and the patient can overcome all problems and find the best solutions.
Diastasis of abdominal muscles after childbirth in women in Moscow
Diastasis is a divergence to the sides of the rectus abdominis muscles. At the same time, the white line of the abdomen becomes thinner and stretched - a connective tissue structure that connects the muscles that form the very desired "press cubes".
If its width is more than 20 mm, we are talking about the presence of diastasis of the rectus muscles.
Diastasis itself is not a disease, but rather a physiological condition. This is not a hernia: there is no defect in the white line, so there is no risk of infringement of internal organs.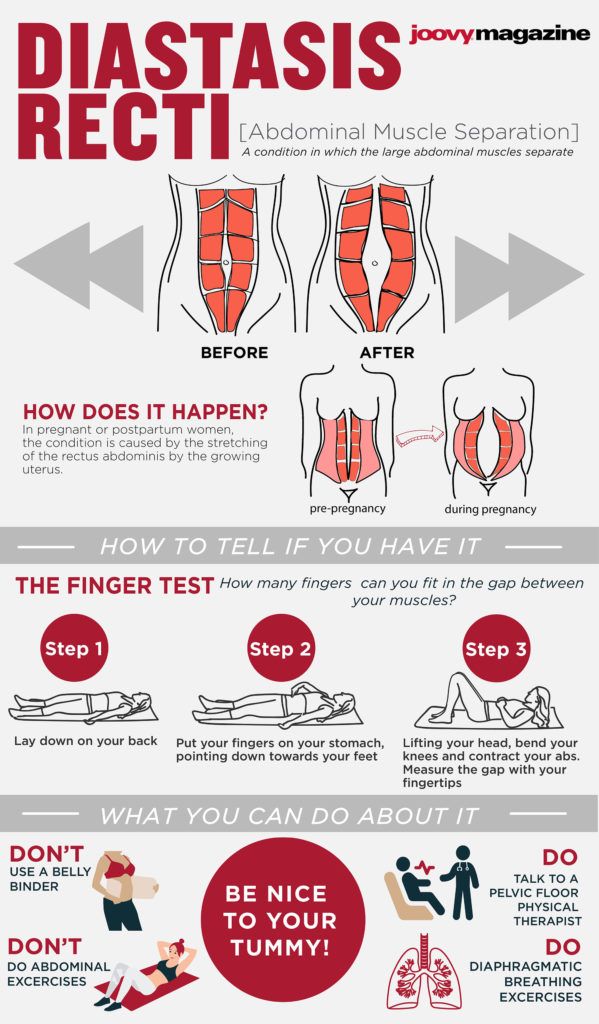 At the same time, the expansion and thinning of the white line increases the potential risk of developing true hernias.
At the same time, the expansion and thinning of the white line increases the potential risk of developing true hernias.
Causes of diastasis
Most often, diastasis appears in the third trimester of pregnancy. This is one of the manifestations of physiological changes in the connective tissue of a woman during this period under the influence of hormones - the anterior abdominal wall is stretched due to connective tissue structures (and primarily the white line) - otherwise the uterus with a growing child would simply not fit in the abdominal cavity. In this case, the center of gravity of the body shifts anteriorly, the bend of the spine increases, the pressure on the anterior abdominal wall increases. The second reason for the appearance and increase in diastasis is an increase in pressure in the abdominal cavity, including during certain physical exercises.
In the postpartum period, the distance between the muscles decreases, but this process takes about a year.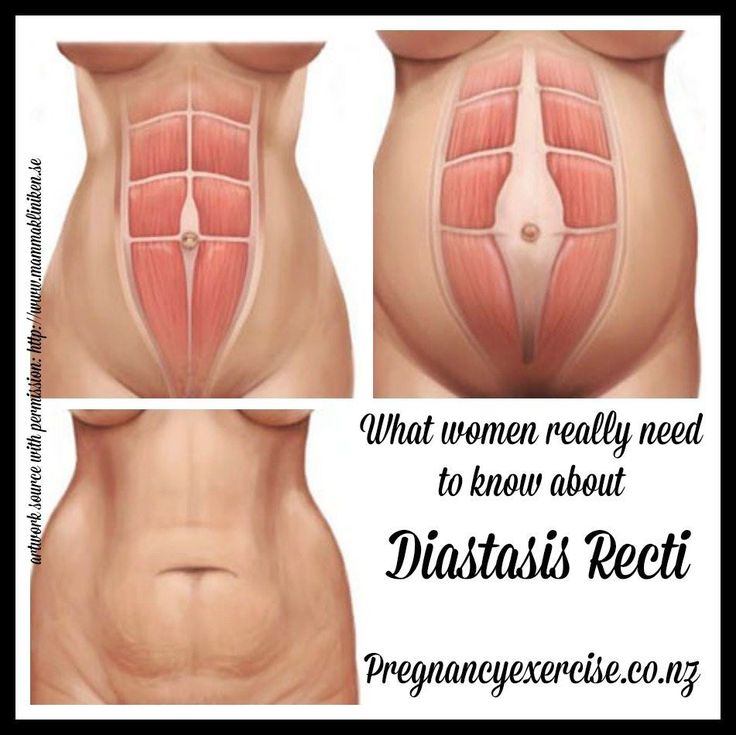 A survey of 300 women conducted by our Norwegian colleagues showed that 6 weeks after birth, diastasis persists in 60% of women, and after 12 months - only in 33%. That is why we do not recommend considering the issue of surgical treatment of diastasis earlier than a year after childbirth.
A survey of 300 women conducted by our Norwegian colleagues showed that 6 weeks after birth, diastasis persists in 60% of women, and after 12 months - only in 33%. That is why we do not recommend considering the issue of surgical treatment of diastasis earlier than a year after childbirth.
Classification of diastasis
There are several classifications of diastasis. Back at 1990 Ranney proposed to define diastasis as small with a width of up to 3 cm, moderate - 3-5 cm and large - if the distance between the rectus muscles is 5 cm or more.
Today, we most often use the classification of Reinpold et al. (2019), which is similar to the hernia classification of the European Society of Herniology. We also note the number of pregnancies, skin condition, clinical symptoms and a number of other parameters that help us to carefully describe the situation in each case and choose the best way to correct diastasis.
Symptoms of diastasis
Often diastasis is visible to the naked eye. For its clearer definition, we ask patients in the supine position to raise their heads and shoulders. At the same time, the rectus abdominis muscles contract and a protrusion becomes visible, or vice versa, a deepening along a line running from the sternum to the pubis. Palpation allows you to more accurately identify the presence and degree of diastasis.
For its clearer definition, we ask patients in the supine position to raise their heads and shoulders. At the same time, the rectus abdominis muscles contract and a protrusion becomes visible, or vice versa, a deepening along a line running from the sternum to the pubis. Palpation allows you to more accurately identify the presence and degree of diastasis.
Diastasis can also be manifested by clinical symptoms. The loss of a strong “foothold” for the muscles of the anterior abdominal wall leads to a redistribution of the static load, which in turn can lead to pelvic and lumbar pain, and in some, fortunately rare, cases, dysfunction of the pelvic organs.
Diastasis diagnostics
We routinely use ultrasound to accurately determine the presence, length and width of diastasis, white line defects and hernias. Ultrasound is included in the consultation and is performed by the surgeon, who determines the tactics of treatment. This approach, in our opinion, is optimal and allows you to obtain reliable additional information that affects the adoption of a tactical decision.
In some cases, usually with severe diastasis and the presence of a hernia, we perform computed tomography, which gives us an understanding of the state of the anterior abdominal wall and allows us to determine and model the optimal method for diastasis plasty.
How can diastasis be treated?
As we said above, diastasis is not a disease, but rather a postpartum condition leading to an aesthetic and functional defect of the anterior abdominal wall. Accordingly, we prefer to replace "treatment" with "correction".
A properly selected set of exercises can often correct external manifestations. It must be remembered that not all exercises can be performed with diastasis. All types of exercises that can contribute to an increase in diastasis are prohibited - these are all basic exercises with weights (deadlift, squats), many exercises for the abdominal muscles - twisting, hanging leg raises, etc. The classic "bar" is also not recommended for patients with diastasis.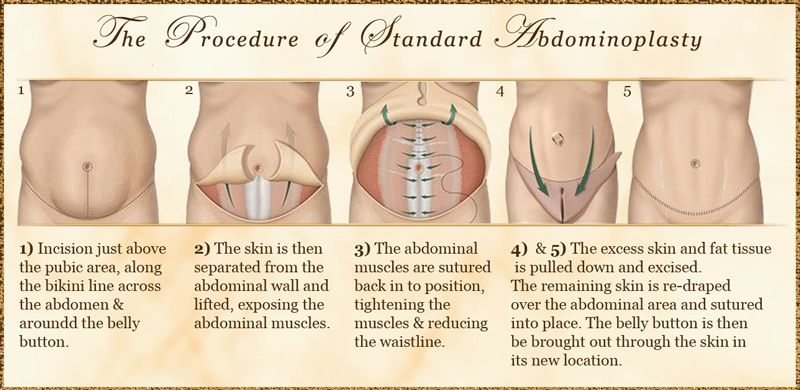
What exercises do we recommend for diastasis? Anything that strengthens the “deep core muscles”: side plank, tummy tuck, cat, Kegel exercises.
They cannot reduce the width of the white line (we remember that this is not a muscle, but a connective tissue that cannot be “pumped up”), but they can often improve the appearance of the abdomen and the quality of life of its owner, as a recent study by Thabet and Alshehri showed, although the level The evidence for this thesis is low. However, we recommend a training program for at least 6 months before considering diastasis surgery.
NB! This does not apply to situations where diastasis is combined with hernias - umbilical or white line. It is impossible to eliminate hernias with physical exercises, we immediately move on to the surgical treatment option (here, it is the treatment).
Diastasis surgical treatment
Surgery for diastasis is a rather extensive topic: there are several options for operations: laparoscopic (at least three fundamentally different methods) and open (also at least three), with or without implants, various suture materials, etc.