Why do i have acid reflux while pregnant
Indigestion and heartburn in pregnancy
Indigestion, also called heartburn or acid reflux, is common in pregnancy. It can be caused by hormonal changes and the growing baby pressing against your stomach.
You can help ease indigestion and heartburn by making changes to your diet and lifestyle, and there are medicines that are safe to take in pregnancy.
Symptoms of indigestion and heartburn
Symptoms of indigestion and heartburn include:
- a burning sensation or pain in the chest
- feeling full, heavy or bloated
- burping or belching
- feeling or being sick
- bringing up food
Symptoms usually come on soon after eating or drinking, but there can sometimes be a delay between eating and developing indigestion.
You can get symptoms at any point during your pregnancy, but they are more common from 27 weeks onwards.
Things you can do to help with indigestion and heartburn
Changes to your diet and lifestyle may be enough to control your symptoms, particularly if they are mild.
Eat healthily
You're more likely to get indigestion if you're very full.
If you're pregnant, it may be tempting to eat more than you would normally, but this may not be good for you or your baby.
Find out more about a healthy diet in pregnancy and foods to avoid.
Change your eating and drinking habits
You may be able to control your indigestion with changes to your eating habits.
It can help to eat small meals often, rather than larger meals 3 times a day, and to not eat within 3 hours of going to bed at night.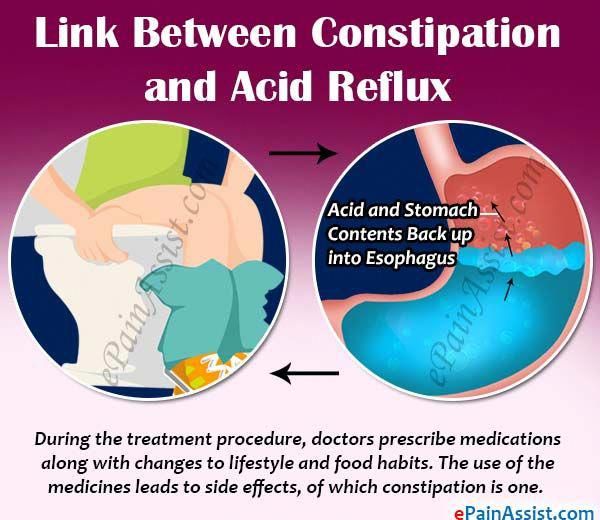
Cutting down on drinks containing caffeine, and foods that are rich, spicy or fatty, can also ease symptoms.
Keep upright
Sit up straight when you eat. This will take the pressure off your stomach. Propping your head and shoulders up when you go to bed can stop stomach acid coming up while you sleep.
Stop smoking
Smoking when pregnant can cause indigestion, and can seriously affect the health of you and your unborn baby.
When you smoke, the chemicals you inhale can contribute to your indigestion. These chemicals can cause the ring of muscle at the lower end of your gullet to relax, which allows stomach acid to come back up more easily. This is known as acid reflux.
Smoking also increases the risk of:
- your baby being born prematurely (before week 37 of your pregnancy)
- your baby being born with a low birthweight
- sudden infant death syndrome (SIDS), or "cot death"
There's lots of help available to stop smoking. Talk to your midwife or call the NHS Smokefree helpline on 0300 123 1044. Find out more about stopping smoking in pregnancy.
Talk to your midwife or call the NHS Smokefree helpline on 0300 123 1044. Find out more about stopping smoking in pregnancy.
Avoid alcohol
Drinking alcohol can cause indigestion. During pregnancy, it can also lead to long-term harm to the baby. It's safest to not drink alcohol at all in pregnancy.
Find out more about alcohol and pregnancy
When to get medical help
See your midwife or GP if you need help managing your symptoms or if changes to your diet and lifestyle do not work. They may recommend medicine to ease your symptoms.
You should also see your midwife or GP if you have any of the following:
- difficulty eating or keeping food down
- weight loss
- stomach pains
Your midwife or GP may ask about your symptoms and examine you by pressing gently on different areas of your chest and stomach to see whether it's painful.
If you're taking prescription medicines
Speak to your GP if you're taking medicine for another condition, such as antidepressants, and you think it may be making your indigestion worse. They may be able to prescribe an alternative medicine.
Never stop taking a prescribed medicine unless you're advised to do so by your GP or another qualified healthcare professional who's responsible for your care.
Medicines for indigestion and heartburn
Medicines for indigestion and heartburn during pregnancy include:
- antacids – to neutralise the acid in your stomach (some are available over the counter from a pharmacist)
- alginates – to relieve indigestion caused by acid reflux by stopping the acid in your stomach coming back up your gullet
You may only need to take antacids and alginates when you start getting symptoms.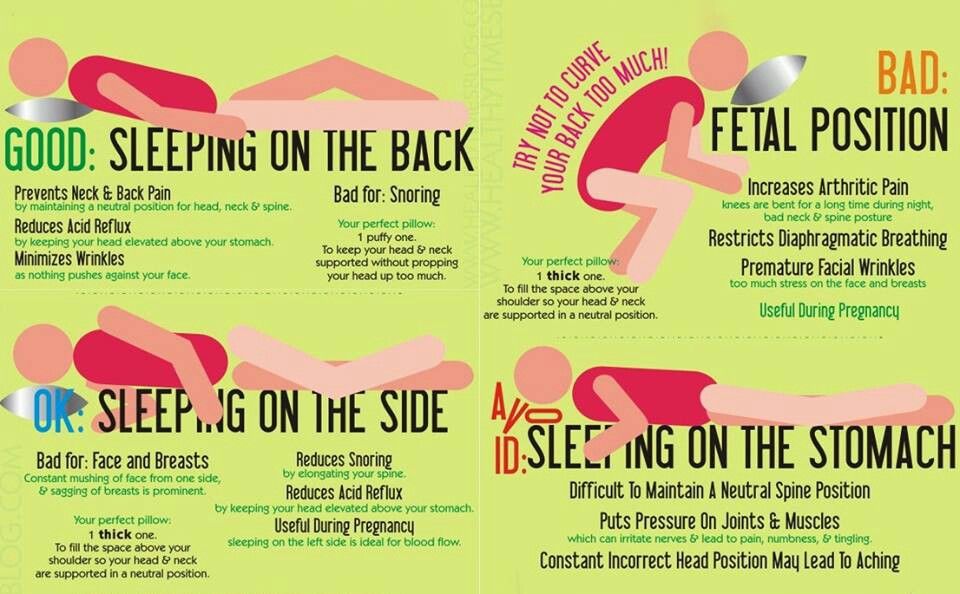 However, your GP may recommend taking them before symptoms come on – for example, before a meal or before bed.
However, your GP may recommend taking them before symptoms come on – for example, before a meal or before bed.
If you're taking iron supplements as well as antacids, do not take them at the same time. Antacids can stop iron from being absorbed by your body.
If antacids and alginates do not improve your symptoms, your GP may prescribe a medicine to reduce the amount of acid in your stomach. 2 that are widely used in pregnancy and not known to be harmful to an unborn baby are:
- ranitidine – a tablet you take twice a day
- omeprazole – a tablet you take once a day
Causes of indigestion in pregnancy
Symptoms of indigestion come when the acid in your stomach irritates your stomach lining or your gullet. This causes pain and a burning feeling.
When you're pregnant, you're more likely to have indigestion because of:
- hormonal changes
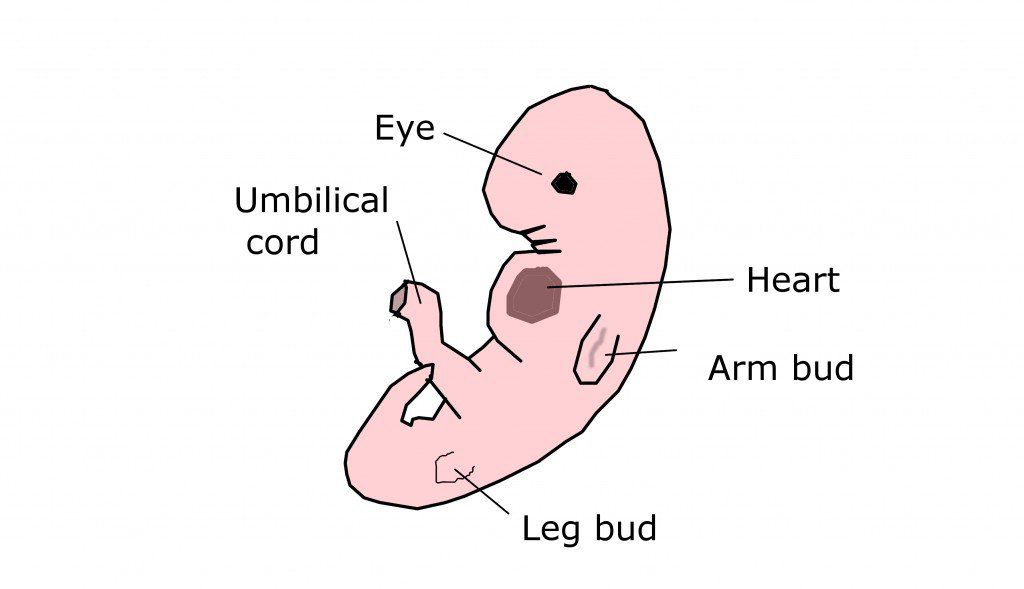
- the growing baby pressing on your stomach
- the muscles between your stomach and gullet relaxing, allowing stomach acid to come back up
You may be more likely to get indigestion in pregnancy if:
- you had indigestion before you were pregnant
- you've been pregnant before
- you're in the later stages of pregnancy
Video: Eating well on a budget
In this video, a dietitian gives advice on how to eat healthily on a budget.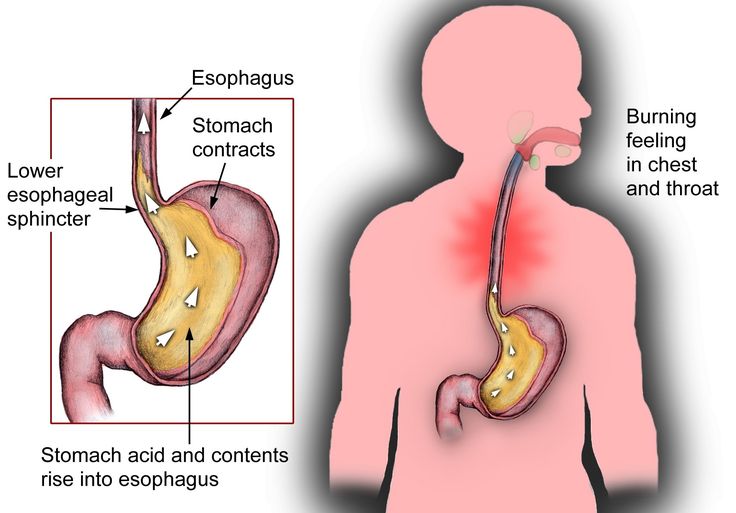
Media last reviewed: 13 January 2021
Media review due: 13 January 2024
Gastroesophageal Reflux Disease (GERD) and Heartburn During Pregnancy
Written by WebMD Editorial Contributors
Medically Reviewed by Nivin Todd, MD on August 26, 2022
In this Article
- Symptoms of Heartburn During Pregnancy
- Causes of Heartburn During Pregnancy
- Prevention of Heartburn During Pregnancy
- Treatment of Heartburn During Pregnancy
- Heartburn Medication to Avoid During Pregnancy
More than half of pregnant women get serious heartburn, particularly during their second and third trimesters. Heartburn, also called acid indigestion, is an irritation or burning sensation of the esophagus (the tube that carries food and liquid to your stomach when you swallow). It’s caused by stomach contents that reflux (come back up).
Symptoms of Heartburn During Pregnancy
If you have heartburn while you’re pregnant, you may:
- Feel burning or pain in your chest or throat, especially after you eat
- Have sensations of fullness, heaviness, or bloating
- Burp or belch
- Have a sour or bitter taste in your mouth
- Cough or have sore throat
Causes of Heartburn During Pregnancy
Heartburn in pregnancy may happen because of changing hormone levels, which can affect the muscles of the digestive tract.
Pregnancy hormones can cause your lower esophageal sphincter (the muscular valve between the stomach and esophagus) to relax, allowing stomach acids to flow back up into your esophagus. Also, as your baby grows, your enlarged uterus can crowd the abdomen, pushing stomach acids upward. Although it's rare, gallstones can also cause heartburn during pregnancy.
Prevention of Heartburn During Pregnancy
Some tips that may help you cut down on heartburn during your pregnancy include:
- Eat several small meals each day instead of three large ones.
- Eat slowly.
- Avoid fried, spicy, or rich (fatty) foods or any foods that seem to cause relaxation of the lower esophageal sphincter and increase the risk of heartburn.
- Don’t smoke tobacco or drink alcohol, which can make heartburn symptoms worse.
- Drink less while eating. Drinking large amounts while eating may increase the risk of acid reflux and heartburn.
- Don't lie down directly after eating.

- Keep the head of your bed higher than the foot of your bed. Or place pillows under your shoulders to help prevent stomach acids from rising into your esophagus.
- Wear loose-fitting clothing. Tight-fitting clothes can increase the pressure on your stomach and abdomen.
- Try to avoid constipation.
Treatment of Heartburn During Pregnancy
If your heartburn won’t go away, see your doctor. They may prescribe or recommend OTC medications that are safe to take during pregnancy. Heartburn usually disappears following childbirth.
Medications may include:
Over-the-counter antacids such as calcium carbonate or magnesium hydroxide. These are generally safe to use during pregnancy. You may find that liquid heartburn relievers are more effective in treating heartburn, because they coat the esophagus.
h3 blockers. These medications block chemical signals that produce stomach acid. They include cimetidine (Tagamet) and famotidine (Pepcid, Zantac 360), and they’re available in over the counter and prescription strengths.
Proton pump inhibitors (PPIs). Like h3 blockers, these drugs help cut down on stomach acid. PPIs, which include lansoprazole (Prevacid) and omeprazole (Prilosec), are available over the counter and by prescription.
If you take iron supplements, talk to your doctor before you take a PPI or h3 blocker. These medications can make the supplements less effective.
Heartburn Medication to Avoid During Pregnancy
Talk to your doctor before taking any antacids. Some contain ingredients that may harm you or your baby. Be sure to not to take these medications:
Ranitidine. In 2020, the FDA stopped sales of an h3 blocker called ranitidine (the ingredient in older Zantac products) because it was contaminated with a cancer-causing agent. If you take OTC ranitidine, stop your use. If you have a prescription for ranitidine, talk to your doctor about other options before you stop your medication.
Heartburn / GERD Guide
- Overview & Facts
- Symptoms & Complications
- Diagnosis & Tests
- Treatment & Care
- Living & Managing
Acid related diseases in pregnancy | Rassvet Clinic
Heartburn during pregnancy is a very common complaint. It is known that up to 80% of pregnant women experience symptoms characteristic of gastroesophageal reflux disease (GERD) (heartburn, dysphagia, belching, and others), and the frequency of heartburn in the first trimester is 7.2%, in the second - 18.2%, in the third - 40%.
It is known that up to 80% of pregnant women experience symptoms characteristic of gastroesophageal reflux disease (GERD) (heartburn, dysphagia, belching, and others), and the frequency of heartburn in the first trimester is 7.2%, in the second - 18.2%, in the third - 40%.
The main factors behind this high prevalence of GERD in pregnancy include hormonal changes such as hyperprogesteronemia (increased levels of the hormone progesterone) and hyperestrogenemia (increased levels of estrogen hormones), as well as increased intra-abdominal pressure due to uterine and fetal growth. nine0003
The action of gestational hormones in the first trimester of pregnancy is due to the fact that they, without affecting the basal tone of the lower esophageal sphincter (LES), reduce the increase in pressure of this sphincter in response to a variety of physiological stimuli, including food intake. In the second and third trimesters of pregnancy, progesterone and estrogen reduce the basal tone of the LES to 50% of the initial level, the maximum decrease occurs at 36 weeks of gestation. After a successful delivery, the tone of the LES in women who did not suffer from GERD before pregnancy, as a rule, returns to normal - in connection with this, this condition is called "pregnancy heartburn." nine0003
After a successful delivery, the tone of the LES in women who did not suffer from GERD before pregnancy, as a rule, returns to normal - in connection with this, this condition is called "pregnancy heartburn." nine0003
Pregnancy heartburn usually does not lead to the development of esophagitis, complications of GERD (strictures, ulcers, bleeding) and does not require serious medical treatment.
If a woman had GERD before pregnancy, the complaints may worsen during pregnancy and require examination and medication.
The diagnosis of GERD during pregnancy is established primarily on the basis of complaints, anamnesis data and objective examination. X-ray examination in pregnant women - due to possible damaging effects on the fetus - is not used, pH-metry and manometry can be used, but the need for its use is doubtful. nine0003
Esophagogastroduodenoscopy (EGD) is the method of choice for diagnosing GERD in pregnant women, but it should only be used for strict indications, such as a history of complications of GERD and the ineffectiveness of ongoing drug therapy.
Treatment of GERD in pregnant women should be based on changes in lifestyle and nutrition: exclusion of a horizontal position of the body immediately after meals, sleeping with the head end of the bed elevated (by 15 cm), exclusion of physical activity that increases intra-abdominal pressure (including wearing corsets, tight belts, bandages). The last meal should take place no later than 3 hours before bedtime, you need to eat in small portions, pay special attention to the normalization of the stool. nine0003
First-line drugs for the treatment of GERD in pregnant women include antacids and alginates. With the ineffectiveness of these drugs, it is permissible to prescribe prokinetics (metoclopramide), blockers of histamine h3 receptors and (according to strict indications) proton pump inhibitors (PPIs).
H2-histamine blockers are the most commonly prescribed group of drugs for pregnant women. They are classified as risk category B by the US Food and Drug Administration (FDA) ( "drugs taken by a limited number of pregnant women without evidence of their effect on the incidence of congenital anomalies or damaging effects on the fetus") . In Russian instructions, only cimetidine and ranitidine are allowed with a caveat: use during pregnancy is possible only if the expected effect of therapy outweighs the potential risk to the fetus. Famotidine and nizatidine in the Russian Federation are contraindicated for pregnant women.
In Russian instructions, only cimetidine and ranitidine are allowed with a caveat: use during pregnancy is possible only if the expected effect of therapy outweighs the potential risk to the fetus. Famotidine and nizatidine in the Russian Federation are contraindicated for pregnant women.
Although most PPIs are also classified by the FDA as risk category B, in Russia there are more stringent restrictions on the use of this group of drugs in pregnant women. So, lansoprazole is contraindicated in the first trimester, in the second and third trimesters it can be used only if the expected benefit of therapy outweighs the potential risk to the fetus. The use of pantoprazole and esomeprazole is possible only under strict indications, when the benefit to the mother outweighs the potential risk to the fetus. Rabeprazole during pregnancy is contraindicated. nine0003
Pregnancy has a beneficial effect on the course of peptic ulcer disease: 75-80% of women experience remission of the disease, and it does not have a noticeable effect on its outcome.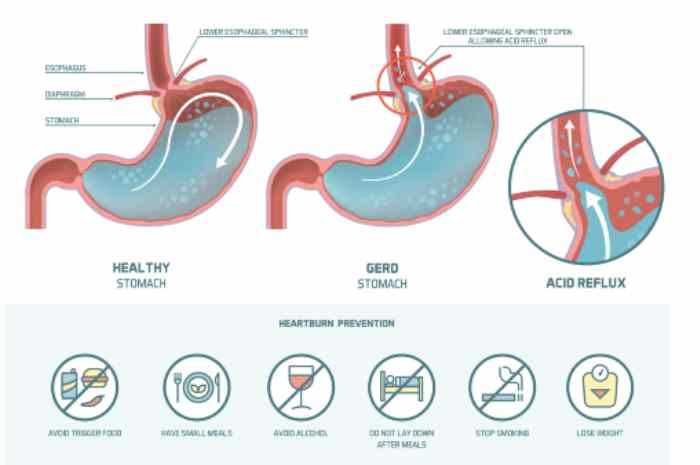 However, some patients may experience an exacerbation. This is most often observed in the first trimester of pregnancy (14.8%) and the third trimester (10.2%), as well as 2-4 weeks before the due date or in the early postpartum period. Uncomplicated peptic ulcer does not adversely affect the development of the fetus.
However, some patients may experience an exacerbation. This is most often observed in the first trimester of pregnancy (14.8%) and the third trimester (10.2%), as well as 2-4 weeks before the due date or in the early postpartum period. Uncomplicated peptic ulcer does not adversely affect the development of the fetus.
Treatment of peptic ulcer in pregnant women includes adherence to generally accepted "regime" measures and diet; taking in the usual therapeutic doses of non-absorbable antacids (1 sachet 3 times a day 1 hour after meals and adsorbents 1 sachet 3 times a day 1 hour after meals). If there is no effect, h3-blockers are prescribed (ranitidine 150/300 mg once a night), in case of their insufficient effectiveness, as well as with the development of complications, we can take PPIs (omeprazole 20-40 mg, lansoprazole 30-60 mg, pantoprazole 40 mg). mg in the morning before the first meal). Bismuth preparations are contraindicated for pregnant women. Eradication therapy for H. pylori infection in pregnant women is not carried out. nine0003
pylori infection in pregnant women is not carried out. nine0003
Author:
Kaibysheva Valeria Olegovna
Gastroenterologist Ph.D.
Article "Pregnancy and heartburn"
Hormonal changes that the body undergoes during pregnancy is the root cause of heartburn. In early pregnancy, the ovaries, and then the placenta, produce the hormone progesterone, one of the main functions of which is to relax the smooth muscles of the body, including the muscles of the uterus. Similarly, progesterone acts on other smooth muscles in our body, for example, the muscles of the esophagus, stomach, and intestines. Progesterone also has a relaxing effect on the sphincters (circular muscles), the main task of which is to separate the various organs of the gastrointestinal system from each other. Relaxation of the esophageal-gastric sphincter leads to the fact that in pregnant women its lumen is open, and hydrochloric acid, which is produced by the stomach, can be thrown into the esophagus, which causes an unpleasant sensation of pain and burning - heartburn.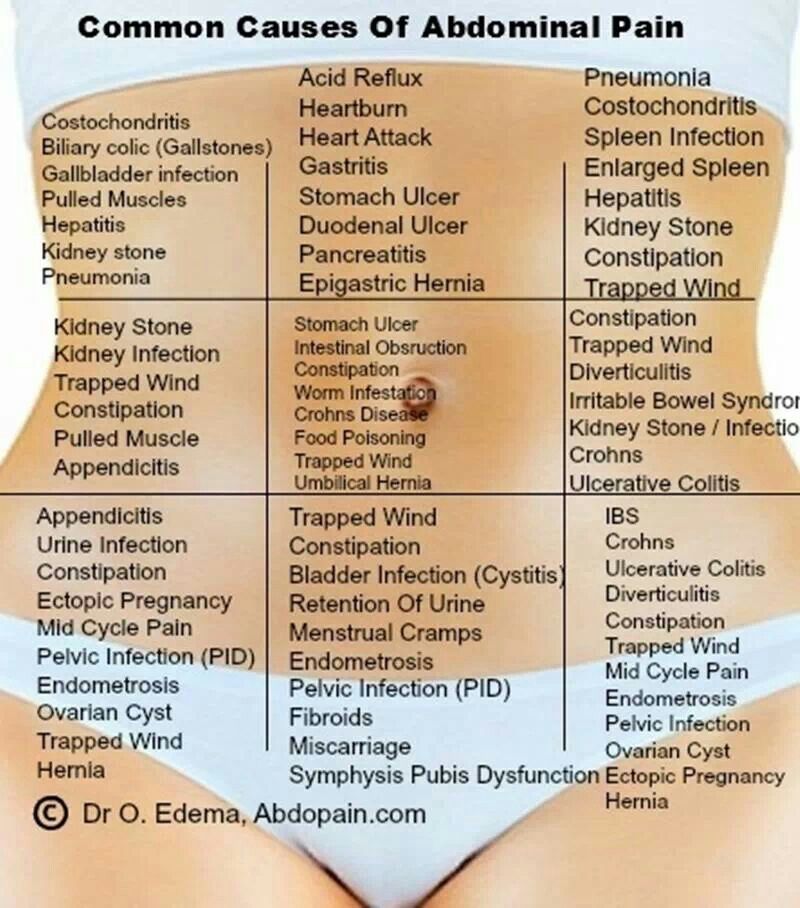 nine0003
nine0003
Another cause of heartburn in pregnant women is the weakening of motility - the wave-like movement of the gastrointestinal tract, slowing down the processes of digestion. Food passes through the digestive tract more slowly, lingering in the stomach. Heartburn in pregnant women is also provoked by the large size of the uterus, which increases intra-abdominal pressure and increases pressure on all the internal organs of the pregnant woman - the stomach and intestines as well. The stomach changes its location during pregnancy, pushed up and to the side by the uterus - all these factors also contribute to the violation of the motility of the esophagus, stomach and intestines and create conditions for the occurrence of heartburn. nine0003
Heartburn can start at any stage of pregnancy, but is most common in the second and third trimesters. As a rule, discomfort occurs after 24 weeks, when the uterus rises above the navel, and becomes especially severe after 30 weeks. Especially intense heartburn can be in a woman if she had an increased acidity of gastric juice before pregnancy.
Especially intense heartburn can be in a woman if she had an increased acidity of gastric juice before pregnancy.
To avoid heartburn during pregnancy, first of all, you need to review your menu and exclude fatty, fried, spicy, salty foods from it, you must give up coffee and carbonated drinks. Include cereals, dairy products, lean meats and mashed vegetables in the diet. It is advisable to eat often and in small portions every 1.5-2 hours. Spend more time eating, remember to chew food thoroughly so that it is digested properly. Drink water between meals, not with meals. After a meal, it is not recommended to sit or lie down, but take a walk for some time (about 30-40 minutes). Try to avoid sharp torso bending after eating. Do not eat at night, the last meal is desirable 2-3 hours before going to bed. Remember to put an extra pillow under your head, sometimes this helps to cope with heartburn. And if heartburn still appears, you need to try to reduce it. nine0003
At the first signs of heartburn, you can drink a small amount of alkaline mineral water without gas or take a few sips of low-fat milk.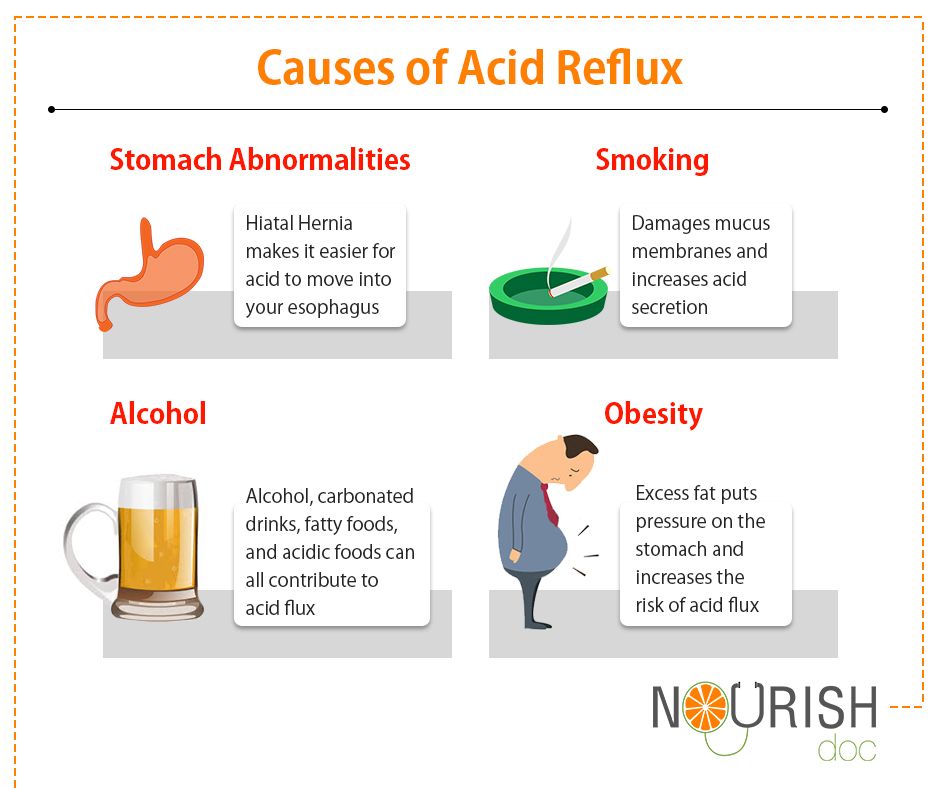 Drink should be in small sips. Kissels work well. They envelop the esophagus and thus reduce burning sensation. The safest in the treatment of heartburn in pregnant women are antacids containing sodium bicarbonate, calcium carbonate, preparations containing magnesium and other substances. Antacids neutralize gastric acid, are not absorbed into the bloodstream and cannot affect the developing fetus. Caution should be taken only to antacids that contain aluminum - because of the theoretical risk of absorption of aluminum ions into the body of a pregnant woman and their penetration into the tissues of the fetus. The effect of medicinal herbs on a pregnant woman and fetus, their effectiveness, and most importantly, safety have not been sufficiently studied, therefore it is better to avoid the use of herbal remedies for this purpose during pregnancy. Many herbs have a relaxing effect on the smooth muscles of the gastrointestinal tract and thus, on the contrary, can provoke heartburn attacks.
Drink should be in small sips. Kissels work well. They envelop the esophagus and thus reduce burning sensation. The safest in the treatment of heartburn in pregnant women are antacids containing sodium bicarbonate, calcium carbonate, preparations containing magnesium and other substances. Antacids neutralize gastric acid, are not absorbed into the bloodstream and cannot affect the developing fetus. Caution should be taken only to antacids that contain aluminum - because of the theoretical risk of absorption of aluminum ions into the body of a pregnant woman and their penetration into the tissues of the fetus. The effect of medicinal herbs on a pregnant woman and fetus, their effectiveness, and most importantly, safety have not been sufficiently studied, therefore it is better to avoid the use of herbal remedies for this purpose during pregnancy. Many herbs have a relaxing effect on the smooth muscles of the gastrointestinal tract and thus, on the contrary, can provoke heartburn attacks.