Dark neck in pregnancy
Skin changes during pregnancy - BabyCentre UK
In this article
- Why does my skin change in pregnancy?
- Can skin changes in pregnancy be harmful?
- Why is pregnancy giving me stretchmarks?
- Why is my skin darker now I'm pregnant?
- What’s this dark line running up my bump?
- Does "pregnancy glow" really exist?
- Why do I have red veins on my cheeks?
- Why is pregnancy giving me spots?
- Why is my skin more sensitive than normal?
Why does my skin change in pregnancy?
There are so many changes going on inside your body during pregnancy, it’s hardly surprising if changes show on the outside, too. Apart from your growing bump, that is!
During pregnancy, you may develop:
- stretch marks
- changes in skin colour (pigmentation)
- spots or acne
- broken veins
- sensitive skin
- itchy skin (Pomeranz 2018a)
Changes to hormones, your circulation, and your immune system affect your skin's appearance and sensitivity. It'll mostly get back to normal after you've had your baby (Murray and Hassall 2014, NHS 2018a, Pomeranz 2018a), though some skin changes, such as stretch marks, will fade, rather than disappear.
Stretch marks and pigmentation changes are thought to run in families (Pomeranz 2018a, Tyler 2015). So if your mum or sister had them during their pregnancies, you may be more likely to develop them too.
Your body changes in pregnancy
Our video reveals how your body changes and makes room for your developing baby. Watch the amazing process in action.More inside pregnancy videos
Can skin changes in pregnancy be harmful?
The usual skin changes that happen during pregnancy aren’t harmful to you or your baby (Pomeranz 2018a, Vaughan Jones et al 2014).
Rarely, though, skin problems can be a sign of something that needs medical treatment.
For a small number of women, severe itching is a symptom of obstetric cholestasis (OC), also known as intrahepatic cholestasis of pregnancy. OC is a complication that affects your liver, causing bile acids to build up in your body (RCOG 2011).
OC is a complication that affects your liver, causing bile acids to build up in your body (RCOG 2011).
With OC, the itching may be more noticeable on the palms of your hands and soles of your feet, and it may be worse at night (Lindor and Lee 2019a, RCOG 2011). See your doctor or midwife if you have these symptoms, so that they can test your liver function (Vaughan Jones et al 2014).
Your doctor can prescribe creams or medication to give you relief from the itching (Lindor and Lee 2019, RCOG 2011). You'll be under the care of a consultant obstetrician for the rest of your pregnancy (RCOG 2011). Read more about OC.
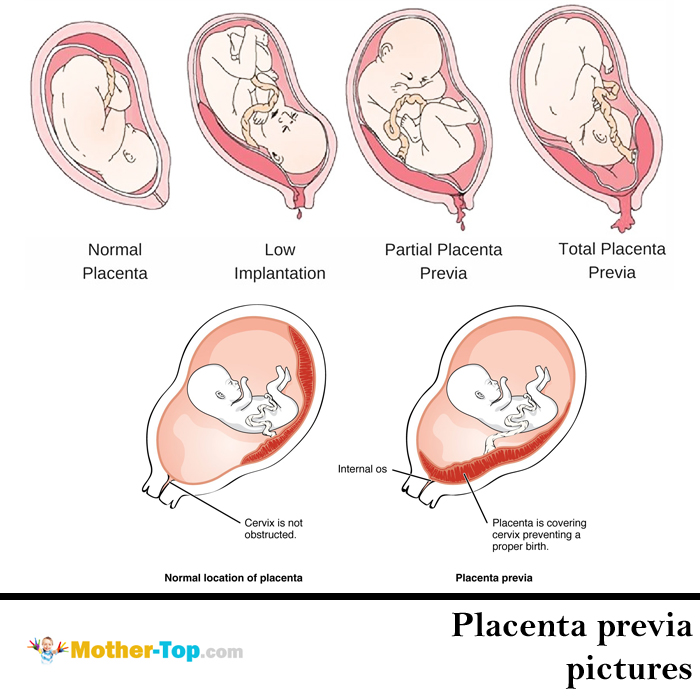
Pregnancy can also cause an extremely rare itchy red rash called pemphigoid gestationis (Vaughan Jones et al 2014). This happens when your body has an immune response, possibly triggered by traces of placenta tissues entering your bloodstream. If you have a red itchy rash, it's very unlikely to be pemphigoid gestationis, but always check any skin condition with your midwife or doctor, just in case.
Some changes in skin colour can be caused by other conditions, which are nothing to do with pregnancy. Get medical advice if you notice any changes in the colour or size of a mole, or other birthmark (Pomeranz 2018a).
Why is pregnancy giving me stretchmarks?
Pregnancy hormones affect the middle layer of your skin so that it no longer binds as well with the other layers of your skin (NHS 2016a, Tyler 2015). That's what causes the slight ridges and lines to appear. The marks will be a different colour to your usual skin tone, ranging from pink to brown, black or purple (Pomeranz 2018a).
You may notice stretch marks on your breasts, belly and thighs as your baby grows bigger and you put on weight (Pomeranz 2018a, Tyler 2015).
There are products you can buy to try to prevent stretch marks, but there's no real evidence that they work (NHS 2016a, Pomeranz 2018a).
If your stretch marks become itchy and red, especially in your third trimester, you may have polymorphic eruption of pregnancy (PEP). It's a harmless pregnancy side-effect, but it can be irritating. Read more about PEP (Pomeranz 2018b).
It's a harmless pregnancy side-effect, but it can be irritating. Read more about PEP (Pomeranz 2018b).
After your baby's born, your stretch marks should fade slowly and become paler than your usual skin tone (Tyler 2015). It can take up to one or two years for this to happen (Pomeranz 2018a). Try to see your stretch marks as a positive. After all, you’re growing a baby!
Why is my skin darker now I'm pregnant?
Areas of your skin turning darker is often one of the first signs that you’re pregnant. You may notice that your nipples and the surrounding skin (areolas) darken (Pomeranz 2018a). Other pigmented areas, such as moles and freckles, may darken too (NHS 2018a, Pomeranz 2018a).
If you're dark-skinned, the area around your tummy button may darken, as well as your armpits and inner thighs (Pomeranz 2018a, Tyler 2015). These areas will lighten again with time, after the birth (NHS 2018a, Pomeranz 2018a, Tyler 2015), although some areas may stay slightly darker than they were before (NHS 2018a, Tyler 2015).
Darker patches of pigmentation on your forehead, cheeks, and neck are known as melasma, or chloasma, or mask of pregnancy. Melasma is caused by your body making extra melanin, the tanning pigment, which protects your skin against ultraviolet (UV) light (BAD 2018). Up to three quarters of mums-to-be are thought to experience this in pregnancy (Pomeranz 2018a, Tyler 2015). It happens because of pregnancy hormones but your family history can play a role, too (BAD 2018, Filoni et al 2019).
Being in the sun may darken your patches, making them more noticeable (BAD 2018, Tyler 2015). To protect your skin, use a sunblock (SPF30 or more), or wear a hat outside, and try to keep to the shade as much as possible (BAD 2018, Pomeranz 2018a).
It’s understandable if you feel self-conscious about your patches, but they're likely to fade within about a year of your baby’s birth (Pomeranz 2018a). In the meantime, tinted moisturiser, foundation and concealer can all help to even out skin tone (BAD 2018).
One mum in 10 finds that her patches stay (Murray and Hassall 2014, Tyler 2015) and may be worsened by using hormonal contraceptives after pregnancy (Murray and Hassall 2014). If this is the case, your doctor can prescribe treatments that you apply to your skin (BAD 2018, Pomeranz 2018a).
What’s this dark line running up my bump?
The vertical line that appears down the middle of your belly is called a linea nigra. It usually runs from the top of your pubic bone to the middle of your belly, but sometimes crosses your belly button to just below your breastbone (sternum) (Pomeranz 2018a).
A linea nigra tends to appear around the second trimester (APA 2015). Not everybody gets a linea nigra, though, so don't worry if you don't have one.
Although the linea nigra appears over your abdominal muscles, which stretch and open a little as your baby grows, it's not caused by this gap. It's caused by pigmentation of the skin, again due to hormone changes (Pomeranz 2018a, Tyler 2015).
The line should fade a few months after you’ve given birth (Pomeranz 2018a).
Does "pregnancy glow" really exist?
The "bloom" or "glow" of pregnancy is not just a saying. Your skin retains more moisture during pregnancy, which plumps it up, smoothing out any fine lines and wrinkles (Pomeranz 2018a).
The pinkish glow that makes you look so well is caused by changes in hormone levels, and by the extra blood circulating round your body (APA 2015). Your circulation will fluctuate, though. So sometimes you'll feel warm and flushed, and at other times you'll feel cooler and look paler (Pomeranz 2018a).
The downside of this effect is that when your body holds on to moisture it may make your ankles and legs swell (Pomeranz 2018a). Also, blood flow to your skin may make any red patches on your face, neck, or chest more visible. These will calm down within a few months of giving birth.
Drink plenty of water, as this can actually help your body to hoard less water (NHS 2018b). Your skin will also benefit if you keep well hydrated (Palma et al 2015).
Your skin will also benefit if you keep well hydrated (Palma et al 2015).
Why do I have red veins on my cheeks?
Tiny blood vessels (capillaries) that break are known as spider veins or naevi. They’re harmless and common in pregnancy (Pomeranz 2018a).
Extra blood circulating in your body, which puts pressure on capillaries, and higher levels of the hormone oestrogen, are two reasons why you may have broken veins. You’re most likely to notice them in your face, throat, neck and arms (Tyler 2015).
Spider veins will fade within a few months of giving birth (Pomeranz 2018a, Tyler 2015), once your hormone levels have settled down.
You may also notice that your palms are more reddish because the surface capillaries are widened (Pomeranz 2018a). This is called palmar erythema. It's harmless and, like spider veins, will fade after you've had your baby (Pomeranz 2018a, Tyler 2015).
Why is pregnancy giving me spots?
You may have thought you'd put the years of raging hormones behind you. But pregnancy can bring the unwelcome return of spots or acne (Bechstein and Ochsendorf 2017).
But pregnancy can bring the unwelcome return of spots or acne (Bechstein and Ochsendorf 2017).
In pregnancy, the raised levels of hormones encourage the production of sebum, the oil that keeps your skin supple (Pomeranz 2018a). Too much sebum causes pores to become blocked, resulting in greasy skin and spots (NHS 2019).
The glands that make sebum are most active in late pregnancy (Pomeranz 2018a). If you had acne before getting pregnant, you may find that it calms down in the first trimester, but flares up again in the third trimester (Vaughan Jones et al 2014).
The little bumps around the dark area of your nipple may also become more raised (Tyler 2015, Vaughan Jones et al 2014). The bumps are called Montgomery tubercles and they produce sebum to moisturise your nipple (Pomeranz 2018a). Up to half of pregnant women experience this – the bumps will go down after you've had your baby (Pomeranz 2018a).
To protect your skin:
- Don't over-cleanse, as this may dry your skin.
 Wash your face twice a day with a gentle soap, or use a fragrance-free cleanser for make-up. This will be plenty to keep your skin clean and fresh.
Wash your face twice a day with a gentle soap, or use a fragrance-free cleanser for make-up. This will be plenty to keep your skin clean and fresh. - Choose water-based, rather than oil-based products that won’t block your pores. Look for products that are labelled "noncomedogenic" or "pH-balanced".
- Resist the temptation to pick or squeeze your spots, to protect your skin from scarring.
- Eat healthily(NICE 2018).
Acne rosacea can worsen during pregnancy (Vaughan Jones et al 2014). Along with spots, rosacea can cause facial flushing and persistent redness of the skin, particularly across your cheeks, nose and chin (NICE 2018b). Possible triggers include very hot or cold weather, sunlight, and spicy food (NICE 2018b). Your doctor can prescribe a cream and a low dose of medicine that’s safe for you to take in pregnancy (NICE 2018b, Vaughan Jones et al 2014).
Don’t use acne creams or treatments unless your GP advises you to. Some acne treatments aren't suitable for pregnancy, because they could harm your unborn baby (APA 2015, DermNet NZ 2014, NICE 2018a, b).
Some acne treatments aren't suitable for pregnancy, because they could harm your unborn baby (APA 2015, DermNet NZ 2014, NICE 2018a, b).
After your baby's birth, you’ll probably find that your skin returns to its pre-pregnancy condition, as your hormone and sebum levels return to normal (Bagatin et al 2019).
Why is my skin more sensitive than normal?
Higher hormone levels, more blood flowing to your skin, and the fact that your skin has become stretched and delicate, can make it feel sensitive. Soaps, detergents and skincare products that you’ve used for months, or even years, may suddenly cause your skin to flare up.
Skin conditions that you had before you became pregnant may improve or worsen because of changes to how your immune system works.
If you have psoriasis, you may find that it improves (Lin and Huang 2016, Vaughan Jones et al 2014). This is because the immune cells that cause your psoriasis tend to decrease in pregnancy (Vaughan Jones et al 2014). However, some women find that their psoriasis gets much worse during this time and needs more intensive treatment (Vaughan Jones et al 2014).
However, some women find that their psoriasis gets much worse during this time and needs more intensive treatment (Vaughan Jones et al 2014).
Other types of immune cells increase during pregnancy. So conditions that are caused by these cells, such as eczema or lupus, can get worse (Vaughan Jones et al 2014). Some women develop a red, itchy rash that looks like eczema, called atopic eruption of pregnancy (AEP).
You may find that your skin burns more easily (NHS 2018a) or that it feels prickly after you’ve been out in the sun (Pomeranz 2018a). Use a sunblock (SPF30 or higher), and try to keep out of direct sunlight as much as possible (BAD 2013, NHS 2016b).
It's also normal to be more sensitive to substances that didn't affect you before pregnancy, such as the chlorine in swimming pools. Dabbing moisturiser or lotion onto itchy areas, or using a bath emollient, should help to protect your skin (Vaughan Jones et al 2014).
Hives (urticaria or nettle rash) are common in the second half of pregnancy (Pomeranz 2018a). Hives are raised, swollen areas on your skin that are very itchy. They are caused by your body producing histamine in response to a trigger, such as temperature changes, a substance you're allergic to, or an infection (NHS 2018c).
Hives are raised, swollen areas on your skin that are very itchy. They are caused by your body producing histamine in response to a trigger, such as temperature changes, a substance you're allergic to, or an infection (NHS 2018c).
Hives may appear on any part of your body, and may come and go for anything from a few minutes to a few days (NHS 2018c). Hives can be easily treated with an oral antihistamine that’s safe to use in pregnancy (Pomeranz 2018a, Vaughan Jones et al 2014).
See your midwife or doctor if you have any concerns about a skin condition.
Find out how pregnancy affects your hair and nails.
References
APA. 2015. Skin changes during pregnancy. American Pregnancy Association. americanpregnancy.org [Accessed July 2019]
BAD. 2013. Sunscreen and sun safety factsheet. British Association of Dermatologists. www.bad.org.uk [Accessed July 2019]
BAD. 2018. Melasma. British Association of Dermatologists. www.bad.org.uk [Accessed July 2019]
www.bad.org.uk [Accessed July 2019]
Bagatin E, Preoenca de Freitas TH, Machago MCR, et al. 2019. Adult female acne: a guide to clinical practice. An Bras Dermatol 94(1):62-75. www.ncbi.nlm.nih.gov [Accessed July 2019]
Bechstein SK, Ochsendorf F. 2017. Acne and rosacea in pregnancy. Hautarzt 68(2):111-9
Bechtel MA. 2018. Pruritus in pregnancy and its management. Dematol Clin 36(3):259-65
DermNet NZ. 2014. Acne in pregnancy. www.dermnetnz.org [Accessed July 2019]Lin X, Huang T. 2016. Impact of pregnancy and oestrogen on psoriasis and potential therapeutic use of selective oestrogen receptor modulators for psoriasis. JEADV 30(7):1085-91
Lindor KD, Lee RH. 2019. Intrahepatic cholestasis of pregnancy. UpToDate. www.uptodate.com [Accessed July 2019]
Murray I, Hassall J. 2014. Change and adaptation in pregnancy. In: Marshall JE, Raynor MD. eds. Myles Textbook for Midwives. 16th ed. Edinburgh: Churchill Livingstone, 143-77
NHS. 2016a. Stretch marks in pregnancy. NHS, Health A-Z, Pregnancy and baby. www.nhs.uk [Accessed July 2019]
2016a. Stretch marks in pregnancy. NHS, Health A-Z, Pregnancy and baby. www.nhs.uk [Accessed July 2019]
NHS. 2016b. Sunscreen and sun safety. NHS, Live well, Healthy body. www.nhs.uk [Accessed July 2019]
NHS. 2016c. Itching and intrahepatic cholestasis of pregnancy. www.nhs.uk [Accessed July 2019]
NHS. 2018a. Common pregnancy problems: skin and hair changes in pregnancy. NHS, Health A-Z, Pregnancy and baby. www.nhs.uk [Accessed July 2019]
NHS. 2018b. Swollen ankles, feet and fingers in pregnancy. NHS, Health A-Z, Pregnancy and baby. www.nhs.uk [Accessed July 2019]
NHS 2018c. Hives. NHS, Health A-Z. www.nhs.uk [Accessed July 2019]
NHS 2019. Acne - causes. NHS, Health A-Z. www.nhs.uk [Accessed July 2019]
NICE. 2018a. Acne vulgaris. Scenario: management of acne vulgaris in primary care. National Institute for Health and Care Excellence, Clinical Knowledge Summaries. cks.nice.org.uk [Accessed July 2019]
NICE. 2018b. Rosacea - acne. National Institute for Health and Care Excellence, Clinical Knowledge Summaries. cks.nice.org.uk [Accessed July 2019]
2018b. Rosacea - acne. National Institute for Health and Care Excellence, Clinical Knowledge Summaries. cks.nice.org.uk [Accessed July 2019]
Palma L, Marques LT,Bujan J et al. 2015. Dietary water affects human skin hydration and biomechanics. Clin Cosmet Investig Dermatol 8:413-421
Pomeranz MK. 2018a. Maternal adaptations to pregnancy: skin, hair, nails, and mucous membranes. UpToDate. www.uptodate.com [Accessed July 2019]
Pomeranz MK. 2018b. Dermatoses of pregnancy. UpToDate. www.uptodate.com [Accessed July 2019]
RCOG 2011. Obstetric cholestasis. Royal College of Obstetricians and Gynaecologists, Green-top guideline, 43. www.rcog.org.uk [Accessed July 2019]
Tyler KH. 2015. Physiological skin changes during pregnancy. Clin Obstet Gynecol 58(1):119-24
Vaughan Jones S, Ambros-Rudolph C, Nelson-Piercy C. 2014. Skin disease in pregnancy. BMJ 348:g3489
Show references Hide references
Does Dark Neck During Pregnancy Mean You’re Having A Boy Or A Girl? Here’s The Truth
Symptoms
Shutterstock
Is there no end to pregnancy myths?
by Lindsay E. Mack
Mack
Updated:
Originally Published:
People sometimes find meaning in the many, many ways the body changes during pregnancy. In some cases, minor differences in your complexion are said to predict the sex of your baby. So does a dark neck during pregnancy mean you’re having a boy, or is that simply an old wives’ tale? Here’s what experts have to say about this phenomenon.
During pregnancy, some people develop dark patches on the skin around their face and neck. It’s totally common. “If you develop dark splotches on your face, you could have melasma, or the mask of pregnancy. This skin condition affects up to half of the pregnant women,” Dr. Gretchen Frieling, a Boston Area board-certified dermatopathologist and mother of two young children, tells Romper. Some folks believe the appearance of dark skin on the face and neck means the person is having a boy, as noted in Baby Gaga, but experts have a different take. “There is no correlation between melasma or any skin changes and the sex of the baby,” Dr. Caitlin Szabo, OB/GYN at Taylor, Suarez, Cook, Khan, and Zertuche, tells Romper.
“There is no correlation between melasma or any skin changes and the sex of the baby,” Dr. Caitlin Szabo, OB/GYN at Taylor, Suarez, Cook, Khan, and Zertuche, tells Romper.
What causes melasma?
“Melasma on the neck does not indicate the sex of the baby. These markings are simply the result of the body producing more melanin than normal,” says Dr. Frieling. It’s the same hormone responsible for tanning, in fact. Getting melasma doesn’t mean anything in particular, other than the fact that your hormones are causing skin to darken. It’s just one of the many ways pregnancy affects your body, similar to numb, tingly hands or changes to your taste buds. Yes, pregnancy changes affect way more than the growing bump.
Will it go away on its own?
In most cases, experiencing the mask of pregnancy is a temporary thing that fades after the baby is born. But if your melasma won’t go away after pregnancy, and you’d like to get rid of the marks, then visiting a dermatologist is recommended, according to Romper. A hydroquinone-topical solution, as well as several different acid treatments, are among the things your derm can use to help melasma fade away. Just remember that there’s nothing harmful about melasma, and leaving it alone isn’t likely to cause any sort of health issue.
A hydroquinone-topical solution, as well as several different acid treatments, are among the things your derm can use to help melasma fade away. Just remember that there’s nothing harmful about melasma, and leaving it alone isn’t likely to cause any sort of health issue.
How did this idea originate?
So where does the idea even come from? It’s one of the many old wives’ tales about pregnancy and childbirth, like the idea that a full moon leads to labor, according to Romper. “There is so much folklore associated with pregnant women and people trying to determine the sex of a child,” says Dr. Frieling. “None of these are backed by science.” Before modern science, people came up with some pretty creative ways to guess the sex of the baby in the womb, and some of those ideas sill hang around today.
To accurately determine the sex of your baby, experts recommend taking a “wait and see” approach. “Ultrasound is the most accurate way to determine the sex of the baby,” Dr. Szabo explains, “but even ultrasounds can be wrong a very small percentage of the time, so the best way is to look after the baby is born!”
Folkloric beliefs about the mask of pregnancy don't offer any scientific guarantees. On the other hand, it can be fun to indulge in some of these old superstitions, and there's no real harm in them. So if a dear relative or friend claims to know what you're having just by looking at the pigmentation on your neck, no big deal. Whether it's revealed through an ultrasound or the birth itself, everyone will know the sex of the baby soon enough.
On the other hand, it can be fun to indulge in some of these old superstitions, and there's no real harm in them. So if a dear relative or friend claims to know what you're having just by looking at the pigmentation on your neck, no big deal. Whether it's revealed through an ultrasound or the birth itself, everyone will know the sex of the baby soon enough.
Experts:
Dr. Gretchen Frieling M.D., board-certified dermatopathologist
Dr. Caitlin Szabo M.D., OB/GYN at Taylor, Suarez, Cook, Khan, and Zertuche
This article was originally published on
Changes in the skin during pregnancy - St. Petersburg State Budgetary Institution of Healthcare "Dermatovenerological Dispensary No. 4"
During pregnancy, the female body is constantly changing.
What physiological skin changes occur during pregnancy?
During pregnancy, under the influence of hormones, the skin around the nipples, in the genital area becomes darker and a dark line (Linea nigra) appears in the middle of the abdomen.
During the period of intrauterine development of the fetus, due to the tension of the skin, lilac and pink stripes (lines), the so-called striae, may appear. nine0003
Some women develop pigment spots on the face (melasma).
Could these phenomena be temporary? Can they be treated?
Some physiological phenomena may resolve spontaneously after delivery (such as pigmentation around the nipples and a dark line on the abdomen). Others persist, although not so pronounced, for a long time (styria). Age spots can be eliminated with special whitening creams. Unfortunately, creams against the appearance of stretch marks practically do not work. There are various techniques that reduce optically visible stretch marks that can be used after childbirth (laser resurfacing, mesotherapy procedures, plasma lifting procedures). nine0003
During pregnancy, there may be some diseases that are observed only in this physiological state of the woman and usually resolve after childbirth.
polymorphic dermatitis of pregnancy.
This pruritic dermatosis develops according to various sources in 1 out of 300 pregnant women.
The rash usually begins with striae in the abdomen and may spread to other parts of the body.
This condition is not harmful to the fetus and usually resolves completely by 6 weeks postpartum. nine0003
It is extremely rare for this dermatitis to develop after the baby is born, but it resolves completely after 6 weeks.
Bullous pemphigoid of pregnancy - BPB (pregnancy herpes) - a rare autoimmune disease with the formation of blisters on the skin, observed during pregnancy and in the postpartum period. In some sources, this disease is usually described under the term "pregnancy herpes", although it has nothing to do with herpes infection. As a rule, it begins with the appearance of small bubbles in the navel area with further spread to other parts of the body. nine0003
There is no evidence for the development of a serious risk for the newborn, although skin lesions in newborns in the form of a transient urticarial and vesicular rash are noted in 5-10%, which spontaneously disappears within 3 weeks.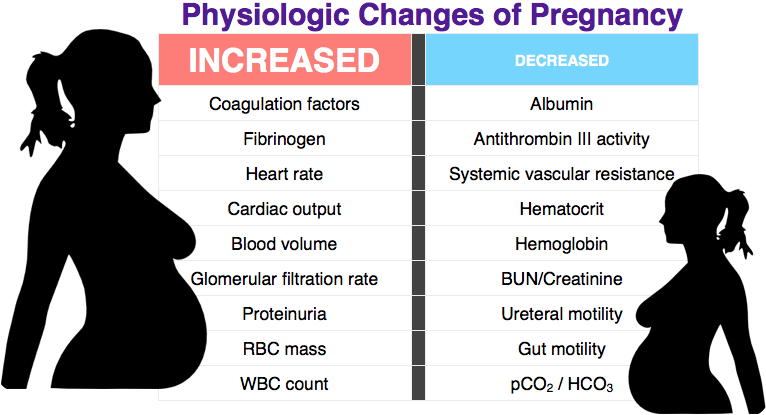
These diseases are successfully treated. The doctor selects therapy according to the standards and prescribes drugs with minimal risk to the mother and fetus.
There is also diffuse hair loss during and after pregnancy - Telogen effluvium (telogen effluvium), which usually lasts from 3 to 12 months after childbirth and resolves on its own without any treatment. Such hair loss after the birth of a child is normal and according to the European Association of Dermatology, treatment with special shampoos or other preparations during this period is not effective. nine0003
It is very important to tell the doctor about any changes in the skin during pregnancy and not to self-medicate, because in addition to the usual and expected changes in the skin during pregnancy, a rash can be a manifestation of dangerous diseases for mother and child (syphilis, rubella, chickenpox , genital, herpes simplex and herpes zoster).
Khramtsova Yu.S.
Pigmentation during pregnancy: how to get rid of it - Parents.
 ru
ru Pregnancy
- Photo
- DiMedia/Shutterstock
Pigmentation is the darkening or, conversely, lightening of skin areas, which occurs due to failures in the production of melanin, the pigment responsible for the color of the skin. The appearance of such signs suggests that a woman is pregnant. Whether the spots appear dark or light, depends on the original skin color. Such marks, characterized by clear edges and irregular shape, are called melasma or chloasma by doctors. nine0003
During pregnancy, they can appear both on the face (on the forehead, chin, around the eyes, on the upper part of the cheeks, on the upper lip), and on other parts of the body: on the inside of the thighs, areolas of the mammary glands, on the abdomen.
"Pregnancy mask" on the face: what is it
In some areas, the skin begins to darken in the very early stages of pregnancy. Sometimes the manifestation of this particular symptom prompts a woman to think about pregnancy. First, the nipples and areolas around them, the area of the labia and the clitoris darken. nine0003
Sometimes the manifestation of this particular symptom prompts a woman to think about pregnancy. First, the nipples and areolas around them, the area of the labia and the clitoris darken. nine0003
In the second trimester, pigmentation becomes brighter and some expectant mothers get the so-called “pregnancy mask” - pigmentation occurs on the face during pregnancy. The spots appear on the cheeks, on the nose, on the forehead, cheekbones, under the eyes, above the upper lip and on the chin and can be arranged symmetrically. If a woman is prone to the appearance of freckles, then you need to be prepared for the fact that during the bearing of the baby they will become brighter, and their number will increase.
Pigmentation during pregnancy on the abdomen appears at about the same time. This brown stripe, which stretches from the navel to the pubis, the so-called Alba stripe, exists in every woman, it just becomes more noticeable during the bearing of the baby. nine0003
Why pigmentation occurs
Human skin color depends on many circumstances, but the most important is the concentration of coloring substances, or pigments, one of which is melanin. It accumulates in special molecules called "melanosomes", which act as a natural filter that protects the top layer of the skin from the harmful effects of ultraviolet rays.
It accumulates in special molecules called "melanosomes", which act as a natural filter that protects the top layer of the skin from the harmful effects of ultraviolet rays.
During pregnancy, the production of melanin changes, because the adrenal glands begin to synthesize more estrogens, progesterone and melanocyte-stimulating hormone. Because of this, more melanin is released, which is concentrated in certain areas of the skin. As a result, the woman develops hyperpigmentation. nine0003
Occasionally, chloasma is caused by oral contraceptives taken before pregnancy or a lack of folic acid. Pigmentation can also indicate problems in the functioning of the liver, pituitary gland, ovaries, incorrect cosmetic procedures, the use of low-quality cosmetics or perfumes. Stress also plays an important role in the appearance of spots on the skin.
Genetics also matter. If the mother had such a problem during pregnancy, then it is possible that age spots during the period of bearing the baby will appear in her daughter. nine0003
nine0003
Expectant mothers often ask how pregnancy pigmentation affects the baby. If its cause is not an exacerbation of chronic ailments, then age spots will not have any effect on the unborn child.
- Photo
- Konstantin Aksenov/Shutterstock
Age spots during pregnancy: a boy or a girl?
There is a popular belief that age spots during pregnancy appear more often in expectant mothers of girls. This is justified: a girl developing in her stomach takes estrogens from her future mother, and their level in the woman's body decreases. But how then to explain that age spots appear in expectant mothers of boys? In a word, than to guess according to folk signs, it is better to do an ultrasound. It definitely won't go wrong. nine0003
How to reduce the risk of age spots
Age spots are a temporary phenomenon, but not so pleasant. What rules should the expectant mother follow in order to reduce the likelihood of their occurrence?
What rules should the expectant mother follow in order to reduce the likelihood of their occurrence?
-
Since pigmentation becomes more noticeable under the influence of ultraviolet rays, protect the skin from the sun: in summer, wear wide-brimmed hats, sunglasses, use sunscreen intended for children;
-
Carefully read the ingredients list of cosmetic products and choose those that do not contain vitamin A, which stimulates the formation of age spots: : green leafy vegetables, cabbage, quality vegetable oil, cereals, fish, liver and beets;
-
But fatty foods are best avoided, because they make the liver work in an enhanced mode, and this threatens with hyperpigmentation. nine0003
-
Do not disregard the recommendation of the gynecologist to visit an endocrinologist. This is necessary to check the functioning of the thyroid gland.
Will we be treated?
Many experts believe that during pregnancy you should not take any drastic measures to combat hyperpigmentation, and advise you to calmly wait until it disappears by itself some time after childbirth.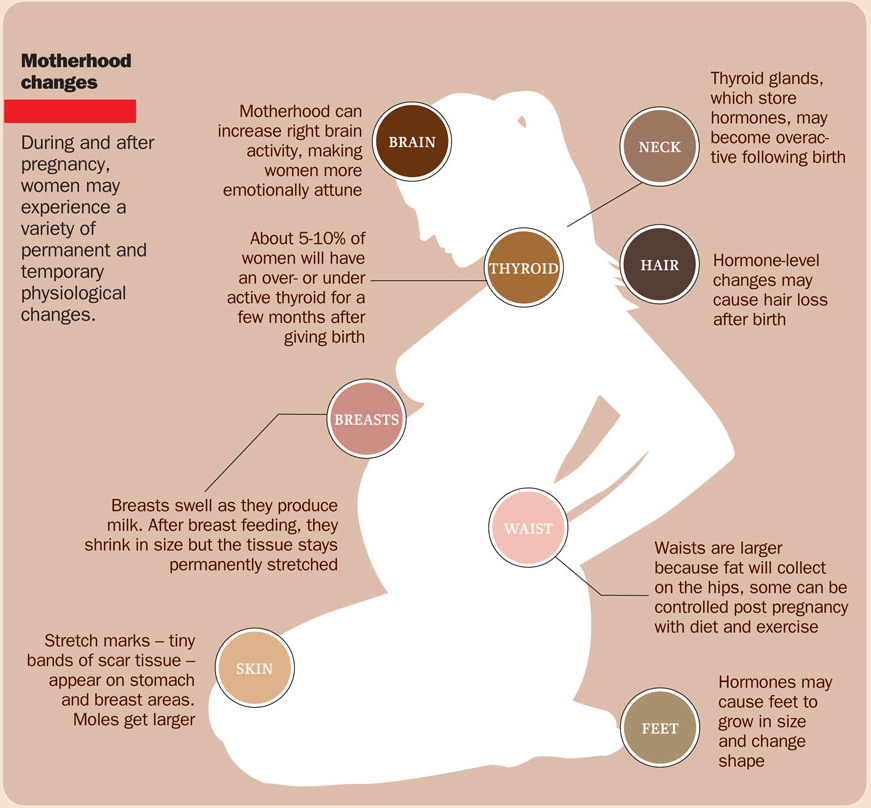 But among the doctors there are those who do not mind the use of traditional medicine. In that case , the expectant mother should understand that it is unlikely that it will be possible to completely get rid of this problem during the bearing of the baby, the pigmentation will only become less noticeable. And most importantly, before using any remedy, you must always consult a doctor.
But among the doctors there are those who do not mind the use of traditional medicine. In that case , the expectant mother should understand that it is unlikely that it will be possible to completely get rid of this problem during the bearing of the baby, the pigmentation will only become less noticeable. And most importantly, before using any remedy, you must always consult a doctor.
These tips, of course, do not apply to cases where chloasma is caused by an exacerbation of chronic diseases. If this is the reason, serious attention should be paid to the treatment of the disease and strictly follow the recommendations of the attending doctor. nine0003
- Photo
- And-One/Shutterstock
Do Home Remedies Work? You can moisten a cotton pad with freshly squeezed juice of parsley, cranberries, cucumber, onions, strawberries, red currants, raspberries, sweet peppers and lubricate the stains with it.