Hip dysplasia in newborn baby
Developmental dysplasia of the hip
Developmental dysplasia of the hip (DDH) is a condition where the "ball and socket" joint of the hip does not properly form in babies and young children.
It's sometimes called congenital dislocation of the hip, or hip dysplasia.
The hip joint attaches the thigh bone (femur) to the pelvis. The top of the femur (femoral head) is rounded, like a ball, and sits inside the cup-shaped hip socket.
In DDH, the socket of the hip is too shallow and the femoral head is not held tightly in place, so the hip joint is loose. In severe cases, the femur can come out of the socket (dislocate).
DDH may affect 1 or both hips, but it's more common in the left hip. It's also more common in:
- girls
- firstborn children
- families where there have been childhood hip problems (parents, brothers or sisters)
- babies born in the breech position (feet or bottom downwards) after 28 weeks of pregnancy
Without early treatment, DDH may lead to:
- problems moving around, for example a limp
- pain
- osteoarthritis of the hip and back
With early diagnosis and treatment, children are less likely to need surgery, and more likely to develop normally.
Diagnosing DDH
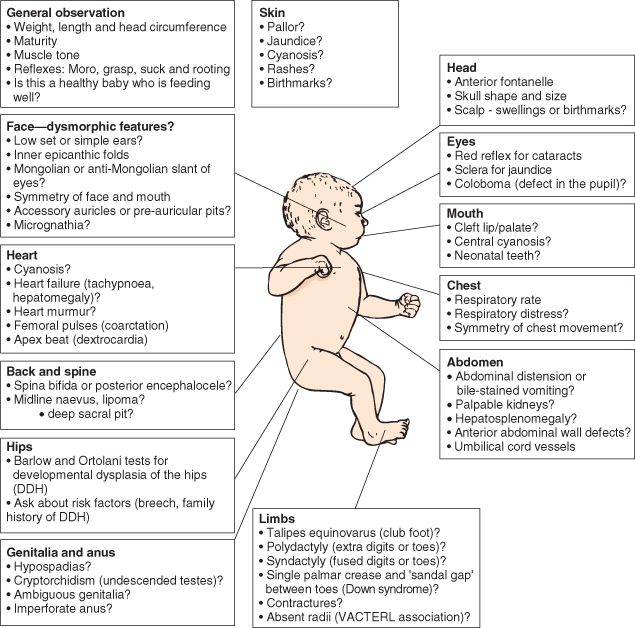
Your baby's hips will be checked as part of the newborn physical screening examination within 72 hours of being born, and again at 6 to 8 weeks of age.
The examination involves gently moving your baby's hip joints to check if there are any problems. It should not cause them any discomfort.
If a doctor, midwife or nurse thinks your baby's hip feels unstable, they should have an ultrasound scan of their hip between 4 and 6 weeks old.
Babies should also have an ultrasound scan of their hip between 4 and 6 weeks old if:
- there have been childhood hip problems in your family
- your baby was born in the breech position (feet or bottom downwards) after 28 weeks of pregnancy
If you have had twins or multiples and 1 of the babies was in the breech position, each baby should have an ultrasound scan of their hips by the time they're 4 to 6 weeks old.
Sometimes a baby's hip stabilises on its own before the scan is due, but they should still be checked to make sure.
Get help and support from the charity Steps if your baby's been diagnosed with DDH
Treating DDH
Pavlik harness
Babies diagnosed with DDH early in life are usually treated with a fabric splint called a Pavlik harness.
This secures both of your baby's hips in a stable position and allows them to develop normally.
Credit:
DR P. MARAZZI/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/729142/view
The harness needs to be worn constantly for 6 to 12 weeks and should not be removed by anyone except a health professional.
The harness may be adjusted during follow-up appointments. Your clinician will discuss your baby's progress with you.
Your clinician will discuss your baby's progress with you.
Your hospital will provide detailed instructions on how to look after your baby while they're wearing a Pavlik harness.
This will include information on:
- how to change your baby's clothes without removing the harness – nappies can be worn normally
- cleaning the harness if it's soiled – it still should not be removed, but can be cleaned with detergent and an old toothbrush or nail brush
- positioning your baby while they sleep – they should be placed on their back and not on their side
- how to avoid skin irritation around the straps of the harness – you may be advised to wrap some soft, hygienic material around the bands
Eventually, you may be given advice on removing and replacing the harness for short periods of time until it can be permanently removed.
You'll be encouraged to allow your baby to move freely when the harness is off. Swimming is often recommended.
Surgery
Surgery may be needed if your baby is diagnosed with DDH after they're 6 months old, or if the Pavlik harness has not helped.
The most common surgery is called reduction. This involves placing the femoral head back into the hip socket.
Reduction surgery is done under general anaesthetic and may be done as either:
- closed reduction – the femoral head is placed in the hip socket without making any large cuts
- open reduction – a cut is made in the groin to allow the surgeon to place the femoral head into the hip socket
Your child may need to wear a cast for at least 12 weeks after the operation.
Their hip will be checked under general anaesthetic again after 6 weeks, to make sure it's stable and healing well.
After this investigation, your child will probably wear a cast for at least another 6 weeks to allow their hip to fully stabilise.
Some children may also require bone surgery (osteotomy) during an open reduction, or at a later date, to correct any bone deformities.
Late-stage signs of DDH
The newborn physical screening examination, and the infant screening examination at 6 to 8 weeks, aim to diagnose DDH early.
But sometimes hip problems can develop or show up after these checks.
It's important to contact a GP as soon as possible if you notice your child has developed any of the following symptoms:
- 1 leg cannot be moved out sideways as far as the other when you change their nappy
- 1 leg seems to be longer than the other
- 1 leg drags when they crawl
- a limp or "waddling" walk
Your child will be referred to an orthopaedic specialist in hospital for an ultrasound scan if your doctor thinks there's a problem with their hip.
Hip-healthy swaddling
A baby's hips are naturally more flexible for a short period after birth. But if your baby spends a lot of time tightly wrapped (swaddled) with their legs straight and pressed together, there's a risk this may affect their hip development.
Using hip-healthy swaddling techniques can reduce this risk. Make sure your baby is able to move their hips and knees freely to kick.
Find out more about hip-healthy swaddling on the International Hip Dysplasia Institute website
Page last reviewed: 08 August 2022
Next review due: 08 August 2025
Developmental Dysplasia of the Hip (for Parents)
What Is Developmental Dysplasia of the Hip?
Developmental dysplasia of the hip (DDH) is a problem with the way a baby's hip joint forms. Sometimes the condition starts before the baby is born, and sometimes it happens after birth, as the child grows.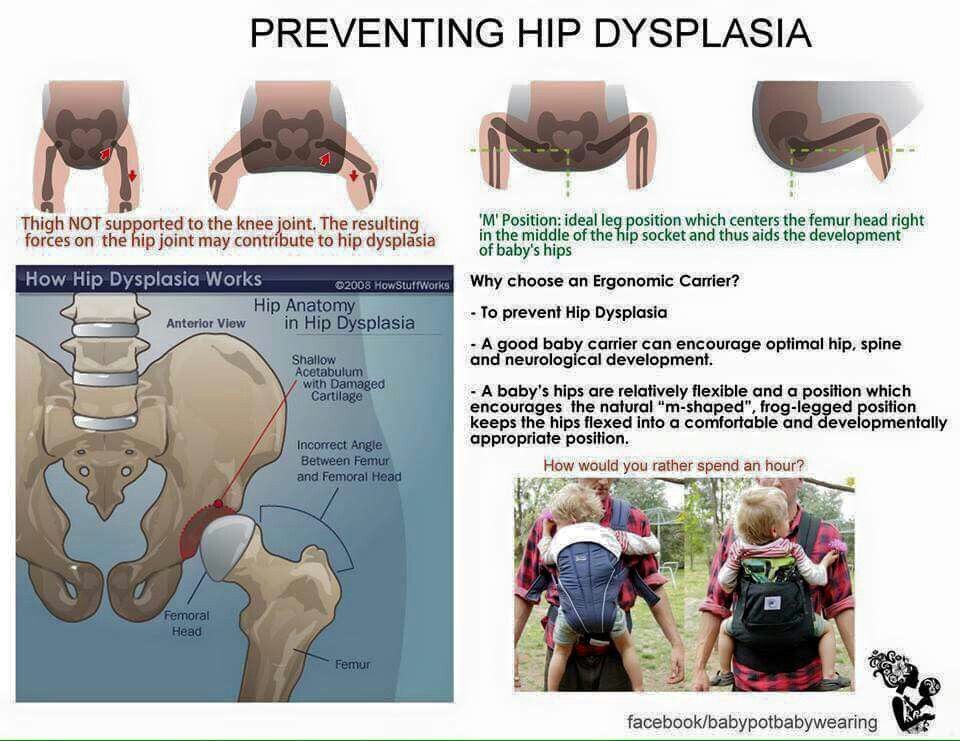 It can affect one hip or both.
It can affect one hip or both.
Most infants treated for DDH develop into active, healthy kids and have no hip problems.
What Happens in a Hip With Developmental Dysplasia?
The hip joint is a ball and socket joint. The top part of the thighbone (the ball part of the hip) sits inside a socket that's part of the pelvic bone. The ball moves around in different directions, but always stays inside the socket. This lets us move our hips front, back, and side to side. It also supports our body weight for walking and running.
In DDH, the hip does not form well. The ball part of the joint may be completely, or partly, out of the socket. Sometimes the ball part may slide in and out of the socket. Often, the socket is shallow. If this is not fixed, the hip joint will not grow well. This can lead to pain with walking and hip arthritis at a young age.
What Are the Signs & Symptoms of Developmental Dysplasia of the Hip?
Developmental dysplasia of the hip doesn't cause pain in babies, so can be hard to notice. Doctors check the hips of all newborns and babies during well-child exams to look for signs of DDH.
Doctors check the hips of all newborns and babies during well-child exams to look for signs of DDH.
Parents could notice:
- The baby's hips make a popping or clicking that is heard or felt.
- The baby's legs are not the same length.
- One hip or leg doesn't move the same as the other side.
- The skin folds under the buttocks or on the thighs don't line up.
- The child has a limp when starting to walk.
Babies with any of these signs should see a doctor to have their hips checked. Finding and treating DDH early usually means there's a better chance for a baby's hips to develop normally.
What Is Hip Laxity?
Many babies are born with hips that feel loose when moved around. This is called neonatal hip laxity. It happens because the bands of tissue that connect one bone to another, called ligaments, are extra stretchy. Neonatal hip laxity usually gets better on its own by 4–6 weeks of age and is not considered true DDH.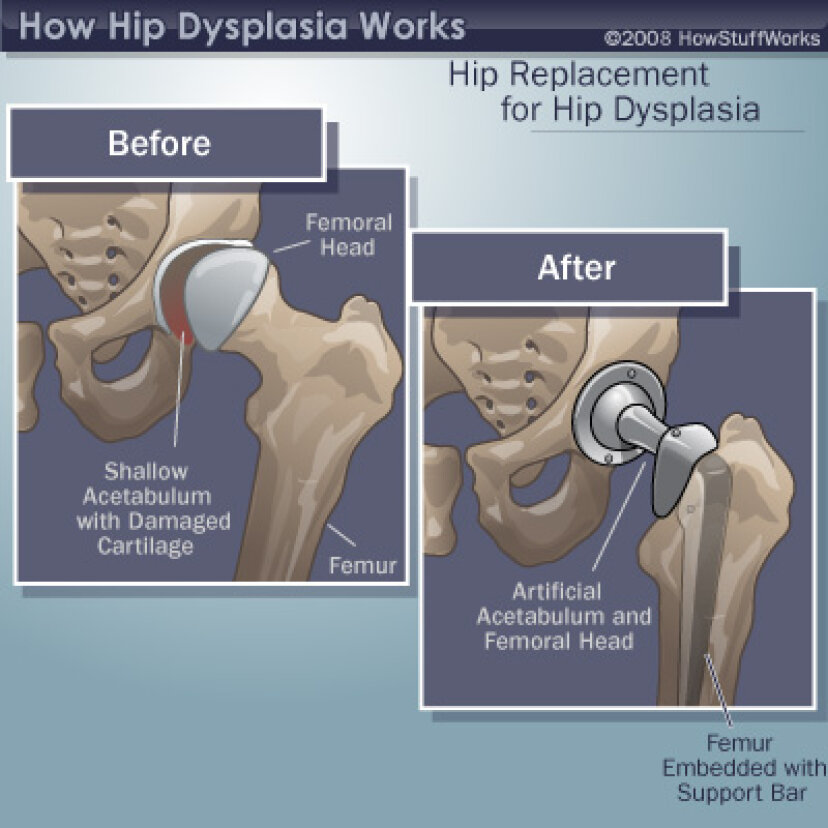
A baby's whose hip ligaments are still loose after 6 weeks might need treatment. So follow-up doctor visits for babies with hip laxity are important.
Who Gets Developmental Dysplasia of the Hip?
Any baby can have DDH. But there's a higher chance of being born with it in babies who:
- are girls
- are first-born
- were breech babies (in the womb buttocks-down instead of head-down), especially during the third trimester of pregnancy
- have a family member with the condition, such as parent or sibling
Rarely, a baby isn't born with DDH, but develops it after birth. To prevent DDH in babies who aren't born with it, don't swaddle a newborn's hips or legs tightly together. Always make sure a baby's legs have plenty of wiggle room.
How Is Developmental Dysplasia of the Hip Diagnosed?
Doctors find most cases of DDH during well-child exams. If a baby has signs of DDH or has a higher risk for it, the doctor will order tests.
Two tests help doctors check for DDH:
- An ultrasound uses sound waves to make pictures of the baby's hip joint. This works best with babies under 6 months of age. That's because most of a baby's hip joint is still soft cartilage, which won't show up on an X-ray.
- An X-ray works best in babies older than 4–6 months. At that age, their bones have formed enough to see them on an X-ray.
How Is Developmental Dysplasia of the Hip Treated?
A pediatric orthopedic surgeon (a specialist in children's bone conditions) cares for babies and kids with DDH. The goal of care is to get the ball of the hip in the socket and keep it there, so the joint can grow normally.
The orthopedic surgeon chooses the treatment based on the child's age. Options include:
- bracing
- a closed reduction and casting
- an open reduction (surgery) and casting
A brace or cast will hold the hip in place and will be on both sides, even if only one hip is affected.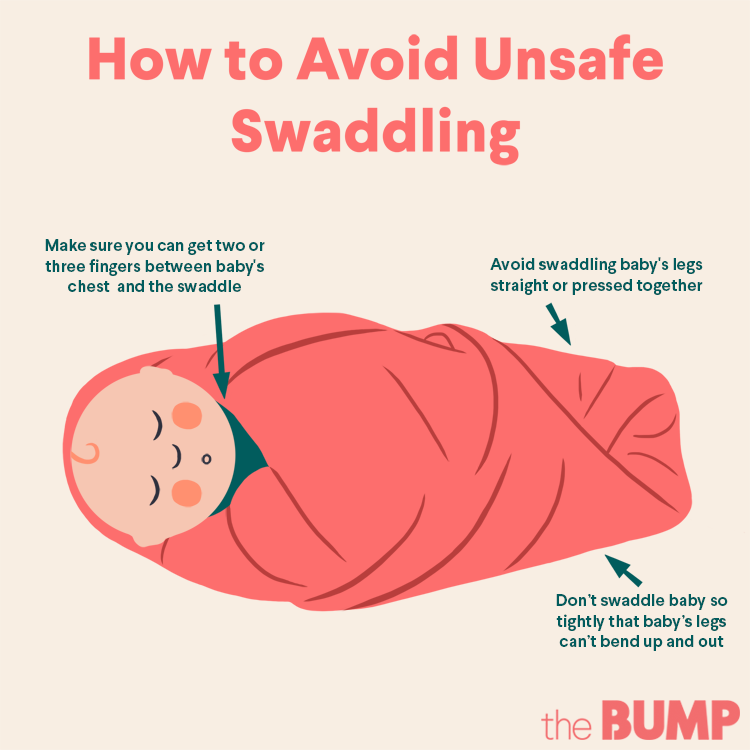
Bracing
Treatment for babies younger than 6 months old usually is a brace. The brace used most often is a Pavlik harness. It has a shoulder harness that attaches to foot stirrups. It puts the baby's legs into a position that guides the ball of the hip joint into the socket.
Treatment with the Pavlik harness often lasts about 6–12 weeks. While wearing the harness, the baby has a checkup every 1–3 weeks with hip ultrasounds and exams. During the visit, the medical team can adjust the harness if needed.
The harness (brace) usually works well to keep the hips in position. Most babies won't need other treatment.
Rarely, the harness isn't able to keep the ball of the hip in the socket. Then, doctors might do either:
- a closed reduction (manually moving the ball back into the socket) and casting
- an open reduction (surgery) and casting
Closed Reduction and Casting
A child might need a closed reduction if:
- The harness was not successful at keeping the ball of the hip in the socket.
- A baby starts care after age 6 months.
For a closed reduction, the baby gets medicine (general anesthesia) to sleep through the procedure and not feel pain. The surgeon:
- Injects contrast dye into the joint to see the cartilagepart of the ball.
- Moves the baby's thighbone so that the ball of the joint goes back into place in the socket.
- Puts on a hip spica cast to hold the hip in place. The baby wears the cast for 2–4 months.
Sometimes, the orthopedic surgeon also loosens the tight muscle in the groin during the closed reduction.
Open Reduction (Surgery) and Casting
A child might need surgery (an open reduction) if:
- The closed reduction was not successful at keeping the ball of the hip in the socket.
- The child is older than 18 months when starting treatment.
During an open reduction, the child is asleep under anesthesia. The surgeon:
- Makes a cut through the skin.

- Moves muscles out of the way to see the hip joint directly.
- Puts the ball back into place.
- Closes the surgical cut with stitches placed under the skin. These won't need to be removed.
- Puts on a hip spica cast to hold the hip in place. The child wears the cast for 6–12 weeks.
Sometimes, the orthopedic surgeon also does a surgery on the pelvic bone to deepen a very shallow hip socket, especially for a child older than 18 months.
What Else Should I Know?
Kids will have regular checkups with their orthopedic specialist until they're 16–18 years old and done growing. These help make sure the hip develops well.
Hip dysplasia in young children
At an orthopedist's appointment in the first month of a child's life, an unpleasant detail may turn out: the baby has immaturity of the pelvic bones. Most often, at the same time, the pediatrician pronounces the words “hip dysplasia”, which instantly frighten all young parents without exception. But being scared is not the right thing to do in this situation. You need to be patient and strictly follow the recommendations of the attending physician. Nevertheless, all doctors will be right when they tell you that joint dysplasia, which was left without the attention of parents and doctors in the first year of a baby’s life, can form the most severe inflammatory processes in a child by the age of two or three, painful hip dislocation and in the future - lameness for life. nine0003
But being scared is not the right thing to do in this situation. You need to be patient and strictly follow the recommendations of the attending physician. Nevertheless, all doctors will be right when they tell you that joint dysplasia, which was left without the attention of parents and doctors in the first year of a baby’s life, can form the most severe inflammatory processes in a child by the age of two or three, painful hip dislocation and in the future - lameness for life. nine0003
Hip dysplasia is a congenital disorder of the formation of the joint that can cause dislocation or subluxation of the femoral head. In this condition, either underdevelopment of the joint, or its increased mobility in combination with connective tissue deficiency, can be observed. Predisposing factors are unfavorable heredity, gynecological diseases of the mother and pathology of pregnancy. Hip dysplasia is 10 times more common in those children whose parents had signs of congenital hip dislocation and in those born with a breech presentation of the fetus, more often in the first birth. Often, dysplasia is detected during drug correction of pregnancy, during pregnancy complicated by toxicosis. The left hip joint is most often affected (60%), less often the right (20%) or both (20%). The relationship of morbidity with environmental problems has been noted. With untimely detection and lack of proper treatment, hip dysplasia can cause dysfunction of the lower limb and even disability. Therefore, this pathology must be identified and eliminated in the early period of the baby's life. nine0003
Often, dysplasia is detected during drug correction of pregnancy, during pregnancy complicated by toxicosis. The left hip joint is most often affected (60%), less often the right (20%) or both (20%). The relationship of morbidity with environmental problems has been noted. With untimely detection and lack of proper treatment, hip dysplasia can cause dysfunction of the lower limb and even disability. Therefore, this pathology must be identified and eliminated in the early period of the baby's life. nine0003
Hip dysplasia can present in a variety of ways. There are three main forms of dysplasia: acetabular dysplasia - acetabular dysplasia; dysplasia of the proximal femur; rotational dysplasia.
With timely detection and proper treatment, the prognosis is conditionally favorable.
Statistics say: up to 25% of newborn children have some form of hip dysplasia, in other words, they are born with subluxations. In most cases, under the constant supervision of an orthopedist, the joints “grow” on their own and return to the anatomical norm. For the rest, they just need a little help. nine0003
For the rest, they just need a little help. nine0003
A preliminary diagnosis can be made even in the maternity hospital. In this case, you need to contact a pediatric orthopedist within 3 weeks, who will conduct the necessary examination and draw up a treatment regimen. In addition, to exclude this pathology, all children are examined at the age of 1-4 months. Particular attention is paid to children who are at risk. This group includes all patients with a history of maternal toxicosis during pregnancy, a large fetus, breech presentation, as well as those whose parents also suffer from dysplasia. If signs of pathology are detected, the child is sent for additional studies. nine0003
To clarify the diagnosis, methods such as radiography and ultrasonography are used. In young children, a significant part of the joint is formed by cartilage, which is not displayed on radiographs, so this method is not used until the age of 2-3 months. Ultrasound diagnostics is a good alternative to X-ray examination in children during the first months of life. This technique is practically safe and quite informative.
This technique is practically safe and quite informative.
With dysplasia, the shape, relationship and size of the structures of the hip joint change significantly. The hip joint of a newborn, even in normal conditions, is an immature biomechanical structure. If the development of the joint is disturbed, the excessively elastic ligaments and the articular capsule are not able to hold the head of the femur in the articular cavity, it shifts upward and laterally (outwards). With certain movements, the femoral head can extend beyond the acetabulum. This condition of the joint is called "subluxation". In severe hip dysplasia, the head of the femur extends completely beyond the acetabulum, a condition called hip dislocation. Hip dysplasia can manifest itself not only as a violation of the acetabulum (acetabular dysplasia), but also as an abnormal development of the proximal femur. nine0003
Hip dysplasia is suspected in the presence of shortened hip, asymmetric skin folds, limited hip abduction, and Marx-Ortolani slipping. Asymmetry of the inguinal, popliteal and gluteal skin folds is usually better detected in children older than 2-3 months. During the inspection, they pay attention to the difference in the level of location, shape and depth of the folds. It should be borne in mind that the presence or absence of this symptom is not enough to make a diagnosis. With bilateral dysplasia, the folds may be symmetrical. In addition, the symptom is absent in half of the children with unilateral pathology. The asymmetry of the inguinal folds in children from birth to 2 months is of little information, since it sometimes occurs even in healthy infants. But the most important sign indicating congenital dislocation of the hip is the “click” or Marx-Ortolani symptom. Slowly abduct the hips evenly to both sides. With normal relations in the joints, both hips in the position of extreme abduction almost touch the outer surfaces of the table plane. With dislocation, the femoral head slips into the acetabulum at the moment of abduction, which is accompanied by a characteristic push - the moment when the femoral head from the dislocation position is reduced into the acetabulum.
Asymmetry of the inguinal, popliteal and gluteal skin folds is usually better detected in children older than 2-3 months. During the inspection, they pay attention to the difference in the level of location, shape and depth of the folds. It should be borne in mind that the presence or absence of this symptom is not enough to make a diagnosis. With bilateral dysplasia, the folds may be symmetrical. In addition, the symptom is absent in half of the children with unilateral pathology. The asymmetry of the inguinal folds in children from birth to 2 months is of little information, since it sometimes occurs even in healthy infants. But the most important sign indicating congenital dislocation of the hip is the “click” or Marx-Ortolani symptom. Slowly abduct the hips evenly to both sides. With normal relations in the joints, both hips in the position of extreme abduction almost touch the outer surfaces of the table plane. With dislocation, the femoral head slips into the acetabulum at the moment of abduction, which is accompanied by a characteristic push - the moment when the femoral head from the dislocation position is reduced into the acetabulum. nine0003
nine0003
Another symptom that indicates the pathology of the joint is limitation of movement. In healthy newborns, the legs are retracted to a position of 80-90 ° and freely placed on the horizontal surface of the table. When the abduction is limited to 50-60°, there is reason to suspect a congenital pathology. In a healthy child of 7-8 months, each leg is retracted by 60-70°, in a baby with congenital dislocation - by 40-50°.
The main method of preventing hip dysplasia is wide swaddling. As soon as at 19In 1971, the national health program promoted wide swaddling; already a few years later, only 0.2% of children over the age of one year suffered from this disease. Orthopedic devices that securely fix the baby's legs in a bent and divorced form. These devices include all kinds of splints (a kind of spacers between the legs), plastic corsets and even plaster retainers. The most popular fixing device is the so-called Pavlik stirrups. Moreover, Pavlik here is not a boy who was the first to try a miracle unit on himself, but a talented Czech orthopedic doctor who came up with the idea of fixing a baby’s legs with a special harness. Massage and gymnastics. Your attending orthopedist will teach you specific exercises and techniques for daily massage and gymnastics, since the set of manipulations strictly depends on how the joint is under-formed. Use of carriers, slings, backpacks and car seats. But only those models that allow the baby to hold freely, legs wide apart. In the countries of Asia and Africa, where women have been carrying their babies on themselves since ancient times, tying them on their backs or on their stomachs (that is, the child spends all the time in a sitting position, with legs wide apart), there is no such phenomenon as hip dysplasia in children at all. exist. nine0003
Massage and gymnastics. Your attending orthopedist will teach you specific exercises and techniques for daily massage and gymnastics, since the set of manipulations strictly depends on how the joint is under-formed. Use of carriers, slings, backpacks and car seats. But only those models that allow the baby to hold freely, legs wide apart. In the countries of Asia and Africa, where women have been carrying their babies on themselves since ancient times, tying them on their backs or on their stomachs (that is, the child spends all the time in a sitting position, with legs wide apart), there is no such phenomenon as hip dysplasia in children at all. exist. nine0003
Treatment should begin as soon as possible. Alas, the treatment of dysplasia is not a quick matter. As a rule, it takes several months, sometimes - a year and a half. This is understandable: the hip joint cannot take the correct position and acquire reliable ligaments in a couple of days. But believe me, your efforts and patience are worth it! Of course, it’s not too pleasant to “hobble” your baby with orthopedic stirrups every day, and swaddle him with a pillow between his legs or “shackle” him in a plastic corset at night.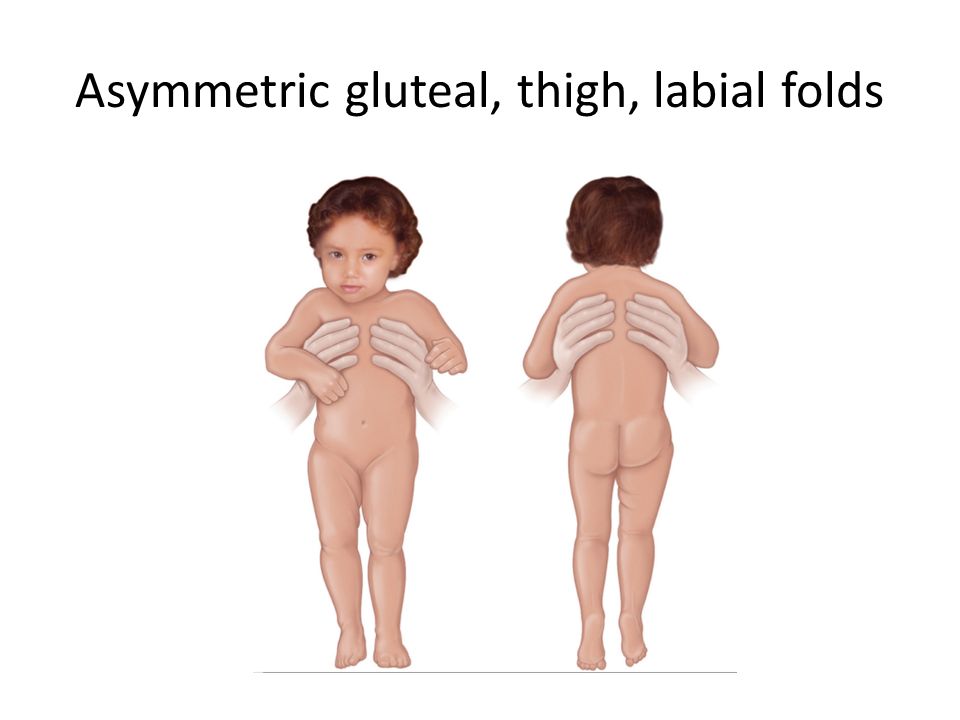 But it’s better to be a little sad before he is even a year old, so that later you can see how famously he dances at his 17-18 years old at the prom. The opposite is true: to be touched by crooked legs now and do nothing, and then reap the terrible consequences of your carelessness ... Isn't it? nine0003
But it’s better to be a little sad before he is even a year old, so that later you can see how famously he dances at his 17-18 years old at the prom. The opposite is true: to be touched by crooked legs now and do nothing, and then reap the terrible consequences of your carelessness ... Isn't it? nine0003
Radiologist ME "3rd City Children's Clinical Clinic"
Krasovsky Vyacheslav Fedorovich
Dysplasia in a child: the main thing is to start treatment on time
Young parents often meet such a diagnosis in a baby as hip dysplasia. This is a congenital inferiority of the joint, which is due to its underdevelopment and can lead to subluxation or dislocation of the hip.
Traumatologist-orthopedist of the first qualification category of the Chelyabinsk Regional Children's Clinical Hospital Alexander Semenov tells about the signs of dysplasia, methods of treatment and the main mistakes of parents. nine0003
- Alexander Vladimirovich, why does dysplasia occur?
- One of the reasons leading to disruption of the normal development of the joint is its abnormal development already in utero.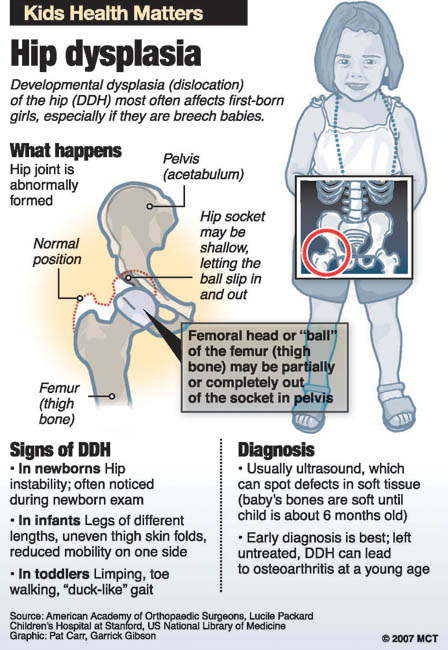 The disease begins to develop at 5-6 weeks of gestation.
The disease begins to develop at 5-6 weeks of gestation.
Genetic and hormonal factors have an influence. Hip dysplasia is 10 times more common in children whose parents had signs of congenital hip dislocation. It is worth noting that in girls, hip dysplasia occurs twice as often and is especially difficult. nine0003
- Can a woman learn about the disease during pregnancy through ultrasound and avoid its development?
- During ultrasound, as a rule, this diagnosis is not revealed. In this case, nothing depends on the woman. Here the main thing is timely diagnosis in a child and proper treatment.
- What should parents pay attention to first of all?
- For the asymmetry of the folds on the legs and buttocks, during gymnastics - restriction of movement in the joint. Parents often complain that one leg is shorter than the other in a child, but most often this symptom is misinterpreted. Factors such as breech presentation of the fetus, large fetus, pregnancy toxemia should alert a pregnant woman in terms of possible congenital joint pathology in a child. The risk in these cases increases tenfold. nine0003
The risk in these cases increases tenfold. nine0003
- Is there an asymptomatic course of dysplasia?
- It happens. Sometimes parents cannot suspect dysplasia on their own when there is no restriction of movement in the hip joint. In this case, only a doctor detects the disease. Therefore, in one month, the child must be examined by an orthopedist.
- But orthopedists are not available in all areas of the Chelyabinsk region. What about families from the outback?
- Currently, about 18 orthopedists are being treated in the Chelyabinsk region, two of them - in the regional hospital, three - in the region - in Kopeysk, Miass and Zlatoust, about 13 - in the city of Chelyabinsk. The orthopedist must necessarily examine the child within the decreed terms (1 month, 6 months, 12 months), so if there is no doctor in the area, you need to take a referral to our children's regional clinic. We are ready to accept all children from the Chelyabinsk region.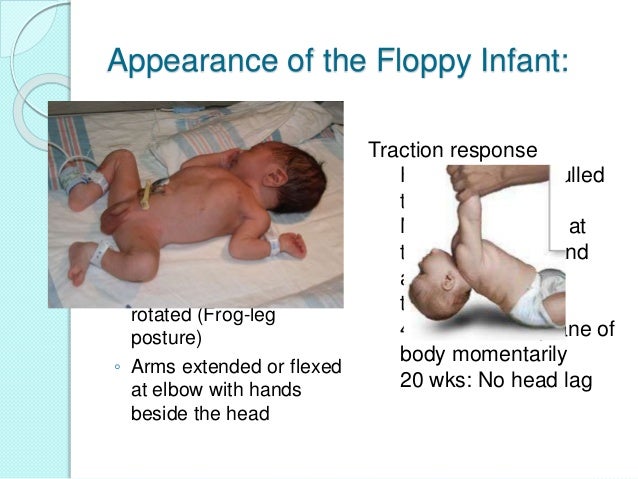 nine0045
nine0045
In addition, in some maternity hospitals in the region, a screening ultrasound of the hip joints is performed on the 5-7th day of the newborn to exclude dysplasia. If the disease is detected, then the baby is discharged already with recommendations and a referral to an orthopedist.
- What are the treatments for dysplasia?
- The main principles of treatment are early onset, the use of orthopedic devices for long-term retention of the legs in the position of abduction and flexion, active movements in the hip joint. nine0045 The main thing in the treatment is gymnastics, which parents should perform with their children. The task of exercise therapy is to strengthen the muscles of the hip joint and organize the child's motor activity, sufficient for full physical development. It usually includes five types of exercises. In addition, complex treatment should include massage and physiotherapy. In more severe cases (severe dysplasia, subluxation, dislocation of the hip), we use various orthopedic aids - Pavlik's stirrups at an earlier age, spacer splints for older children.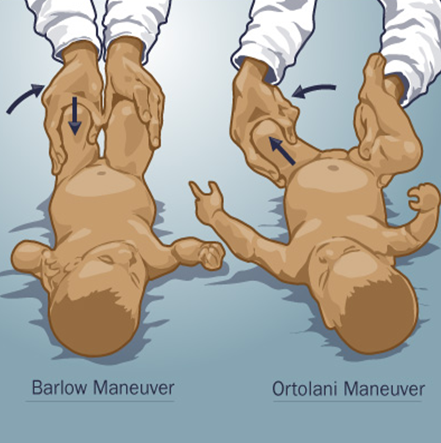 nine0003
nine0003
- Where is the child being treated?
- We send patients for treatment at their place of residence. The main responsibility in this case lies with the parents, they must perform a set of exercises daily. And massage and physiotherapy can be obtained in polyclinics at the place of residence.
- Who can massage a child?
- Massage can only be done by a specially trained massage therapist, certified and preferably specialized in baby massage. nine0003
- How does swaddling a baby affect treatment?
- Previously, tight swaddling was used, now it has already been abandoned, because in this case the joint is in a non-physiological position. Now experts recommend either wide swaddling or a free position for the legs.
- If a child is prescribed orthopedic products, then his movements are limited for a long time. How will this affect his future development?
- Nothing.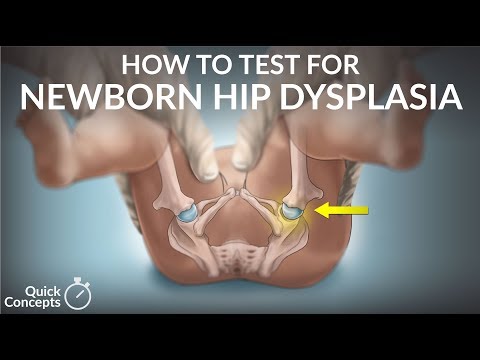 The fact is that there is no particular restriction on movement. If parents follow the orthopedic regimen, then in 80% of cases we cancel Pavlikama's stirrups after 3 months. Even if a child wears a spacer splint for six months, this only has a positive effect on the formation of his joints. In the future, this will not affect the overall development of the child.
The fact is that there is no particular restriction on movement. If parents follow the orthopedic regimen, then in 80% of cases we cancel Pavlikama's stirrups after 3 months. Even if a child wears a spacer splint for six months, this only has a positive effect on the formation of his joints. In the future, this will not affect the overall development of the child.
- Is it possible to completely get rid of dysplasia?
- The leading role is played by early recognition of this defect and timely treatment. With timely treatment and compliance with the orthopedic regimen by parents, about 70% of children recover completely, but 30% develop gait disturbance at an older age. nine0045 If we talk about congenital dislocation of the hip, then there is a high probability of developing arthrosis of the hip joint in a few years. But still, in most children, the disease goes away without a trace if it is detected in time and treated.
- How many children in the Chelyabinsk region suffer from dysplasia?
- Every day 4-5 people from all over the region come to our regional polyclinic with this diagnosis.