When 1st trimester ends
Pregnancy | Conditions | UCSF Health
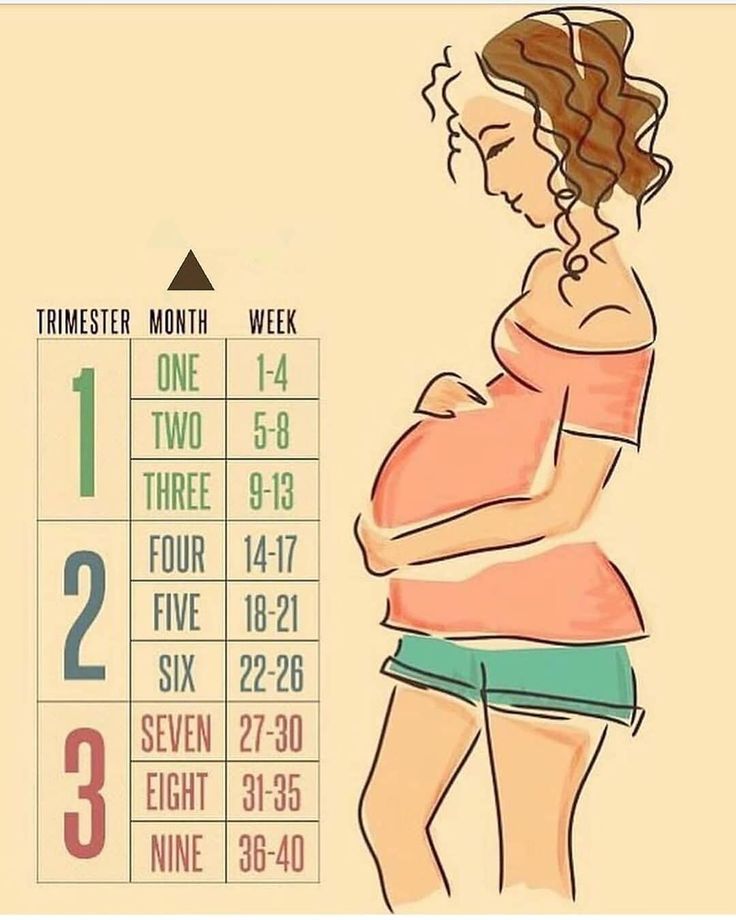
The Three Trimesters
Pregnancy has three trimesters, each of which is marked by specific fetal developments. A pregnancy is considered full-term at 40 weeks; infants delivered before the end of week 37 are considered premature. Premature infants may have problems with their growth and development, as well as difficulties in breathing and digesting.
First Trimester (0 to 13 Weeks)
The first trimester is the most crucial to your baby's development. During this period, your baby's body structure and organ systems develop. Most miscarriages and birth defects occur during this period.
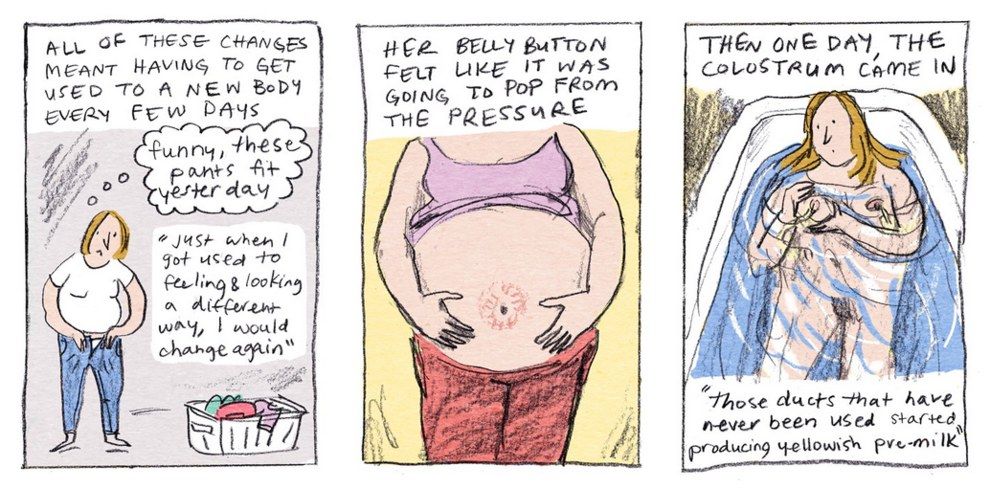
Your body also undergoes major changes during the first trimester. These changes often cause a variety of symptoms, including nausea, fatigue, breast tenderness and frequent urination. Although these are common pregnancy symptoms, every woman has a different experience. For example, while some may experience an increased energy level during this period, others may feel very tired and emotional.
Second Trimester (14 to 26 Weeks)
The second trimester of pregnancy is often called the "golden period" because many of the unpleasant effects of early pregnancy disappear. During the second trimester, you're likely to experience decreased nausea, better sleep patterns and an increased energy level. However, you may experience a whole new set of symptoms, such as back pain, abdominal pain, leg cramps, constipation and heartburn.
Somewhere between 16 weeks and 20 weeks, you may feel your baby's first fluttering movements.
Third Trimester (27 to 40 Weeks)
You have now reached your final stretch of pregnancy and are probably very excited and anxious for the birth of your baby. Some of the physical symptoms you may experience during this period include shortness of breath, hemorrhoids, urinary incontinence, varicose veins and sleeping problems. Many of these symptoms arise from the increase in the size of your uterus, which expands from approximately 2 ounces before pregnancy to 2. 5 pounds at the time of birth.
5 pounds at the time of birth.
Prenatal Care
Expert prenatal care ensures that both you and your baby are as healthy as possible throughout your pregnancy.
If you think you're pregnant, contact your doctor to make an appointment and establish your prenatal care schedule. Many factors determine the number of visits you'll have, including your personal health and your doctor's preference.
At prenatal visits, we test you and your baby to identify any potential risks, treat any complications, and monitor your baby's growth and development. Additional prenatal care may be needed if you have preexisting medical conditions, such as diabetes, or if complications arise during your pregnancy.
If your pregnancy is going well, visits are planned around key pregnancy developments and tests. Visits are also a time for your doctor to give you important information as your pregnancy progresses and help you prepare for giving birth.
Here's a guide to the most common prenatal tests, including when they happen and what you can expect.
Genetic carrier screening
Timing: Before or during pregnancy
How it works: A blood test is done to see whether you're a carrier of a genetic change that could raise your baby's risk for a genetic condition. Two conditions commonly screened for are cystic fibrosis and spinal muscular atrophy.
California Prenatal Screening Program (CA PNS)
CA PNS screening is a combination of these two blood tests, performed at different stages of pregnancy:
- Cell-free DNA screening (also called noninvasive prenatal testing or NIPT) is done at 10 weeks of pregnancy or later to determine a baby's risk for Down syndrome and two other syndromes, trisomy 18 and trisomy 13. It can also predict the sex of your baby.
- A maternal serum alpha-fetoprotein (MASFP) screening is done between 15 and 21 weeks of pregnancy to assess the risk for abnormalities of the spine (neural tube defects) or abdomen (abdominal wall defects).
Nuchal translucency (NT) screening
Timing: Usually between 12 and 14 weeks of pregnancy, at the first trimester screening
How it works: An abdominal ultrasound measures the amount of fluid behind the baby's neck to look for certain genetic conditions as well as structural problems, such as heart defects. Extra fluid in that area indicates a higher risk of chromosome abnormalities, birth defects and genetic conditions.
Extra fluid in that area indicates a higher risk of chromosome abnormalities, birth defects and genetic conditions.
Chorionic villus sampling (CVS)
Timing: Usually between 10 and 13 weeks of pregnancy
How it works: A small sample of the placenta is taken and sent for testing to identify any chromosomal or genetic disorders. (Not everyone who is pregnant chooses to have CVS.)
Amniocentesis
Timing: Usually between 16 and 22 weeks of pregnancy
How it works: The doctor takes a small sample of the amniotic fluid surrounding your baby. Genetic testing of that fluid can identify chromosomal or genetic disorders as well as neural tube defects. (Not everyone who is pregnant chooses to have amniocentesis.)
Early fetal anatomy examination
Timing: Usually between 12 and 14 weeks of pregnancy
How it works: Like the level 2 anatomy ultrasound done in the second trimester, the first-trimester ultrasound examines many physical aspects of your baby's body and includes additional imaging, such as the evaluation done in a nuchal translucency ultrasound. It's usually recommended for high-risk patients, such as those who are carrying a baby with a suspected abnormality, had high-risk findings on a genetic screening test, or had a previous pregnancy with fetal abnormalities.
It's usually recommended for high-risk patients, such as those who are carrying a baby with a suspected abnormality, had high-risk findings on a genetic screening test, or had a previous pregnancy with fetal abnormalities.
Anatomy ultrasound (level 2)
Timing: Around 20 weeks of pregnancy
How it works: An "anatomic survey" examines many aspects of your baby's body, including the heart, brain, spine, limbs and certain other organs. The anatomy ultrasound visit also includes an assessment of the placenta and of your uterus and cervix.
Glucose tolerance test
Timing: Usually between 24 and 28 weeks of pregnancy
How it works: This test measures the level of sugar (glucose) in your blood. An abnormally high blood sugar level may be a sign of gestational diabetes, a type of diabetes that can develop during pregnancy and requires monitoring.
Fetal monitoring
How it works: Your doctor may want to monitor your baby's heart rate (using an ultrasound transducer) and measure uterine contractions (using a device called a toco transducer).
Group B strep testing
How it works: Doctors routinely take a sample from your vagina and rectum during pregnancy to test for group B streptococcus ("group B strep") bacteria.
Group B strep bacteria can cause infections during pregnancy and lead to complications and even death for a newborn if transmitted during delivery. Fortunately, the infection can easily be treated with antibiotics during pregnancy.
Labor and Delivery
Labor is a series of progressive and continuous contractions of the uterus that help the cervix to open and thin, allowing the baby to travel through the birth canal. Labor usually starts within two weeks before or after your estimated delivery date. However, this can vary widely.
Labor and delivery are hard work and involve some discomfort. The level of discomfort experienced during childbirth varies from woman to woman and from pregnancy to pregnancy. Each woman chooses a different way to experience her birth — some prefer to go through it without medication, while others choose to have medication or anesthesia.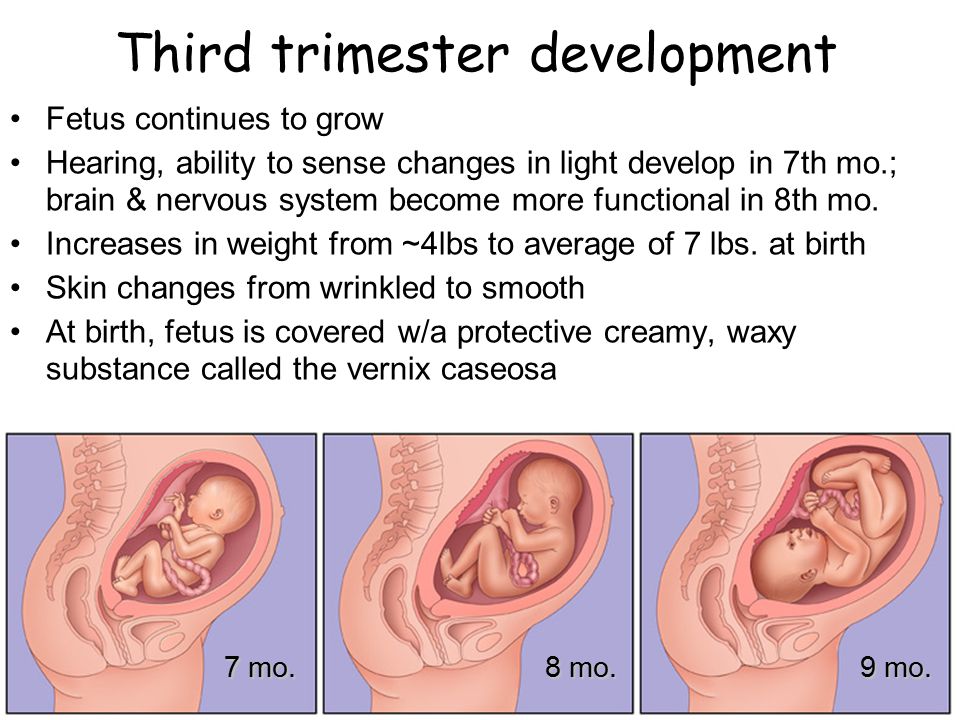 Many decide to "see how it goes" and make choices as their labor unfolds.
Many decide to "see how it goes" and make choices as their labor unfolds.
We offer a spectrum of options for managing your pain during labor and delivery. You will be assigned to your own nurse during your stay in the birthing suite. He or she will help keep you comfortable and guide you through non-drug approaches to pain management, such as whirlpool soaks and position changes.
Pain Management
Non-Medical Approaches for Labor and Vaginal Birth
The Birth Center rooms provide a number of options for comfort during labor including space to move around, tubs for soaking, rocking chairs and beds that convert into different positions.
Relaxation and breathing techniques ease the discomfort for many, as does the presence of family and friends and the support of health care providers. Comfort measures can be learned from classes, books or videos available through UCSF's Great Expectations Pregnancy Program.
Medical Approaches for Labor and Vaginal Birth
- Narcotic Injections of a narcotic can be given intravenously (through an IV) during labor.
 The narcotic works quickly and can be given every hour during labor. However, it is not given immediately before delivery to ensure that the effects will have worn off before the baby is born. For some women, this medication takes the edge off and allows them to rest and relax between contractions.
The narcotic works quickly and can be given every hour during labor. However, it is not given immediately before delivery to ensure that the effects will have worn off before the baby is born. For some women, this medication takes the edge off and allows them to rest and relax between contractions. - Nitrous oxide gas This is the same gas that is used at the dentist, and can be inhaled during contractions through a mask you hold. The gas can lessen but not eliminate the pain of labor. The effect occurs only while the gas is being inhaled and disappears rapidly when the mask is removed. It can be used through delivery.
- Epidural anesthesia An epidural offers the most complete pain relief during labor and birth. A tiny tube or catheter is placed through a needle into a space (the "epidural space") outside the spinal cord sac in the lower back. The needle is removed and the tubing is taped in place. Similar to an IV, medication is given continuously through the tube during labor and birth.
 The medication blocks the pain of contractions. Because of the numbness produced by the epidural, a woman with an epidural cannot get out of bed. Most women take the opportunity to get some rest. A "walking epidural" — also called a "combined spinal-epidural" — is a technique that allows a woman to continue to move around while receiving a lighter form of medication.
The medication blocks the pain of contractions. Because of the numbness produced by the epidural, a woman with an epidural cannot get out of bed. Most women take the opportunity to get some rest. A "walking epidural" — also called a "combined spinal-epidural" — is a technique that allows a woman to continue to move around while receiving a lighter form of medication.
Our anesthesiologists are available to the Birth Center 24 hours a day. The anesthesiologist on-call meets every woman who is admitted in labor regardless of whether she is planning anesthesia for her birth. The purpose of this visit is two-fold: To learn of any medical problems you may have in the unlikely event of an emergency, and to answer any questions you may have about the pros and cons of medical approaches to pain relief during labor.
Caesarean Birth
When a Caesarean is Needed
While most women will have a vaginal delivery, some may need abdominal surgery referred to as Caesarean section. Most often women have a Caesarean birth when labor does not progress — the cervix does not completely dilate or the baby cannot be pushed out — over a long period of time. It is a decision made by the woman and her doctor when both feel everything else has been tried and this is the only alternative.
Most often women have a Caesarean birth when labor does not progress — the cervix does not completely dilate or the baby cannot be pushed out — over a long period of time. It is a decision made by the woman and her doctor when both feel everything else has been tried and this is the only alternative.
Sometimes a Caesarean birth is planned. Situations that might require a scheduled Caesarean include:
- Breech position
- Previous Caesarean section
- Placenta previa, when the placenta is covering the cervix
Rarely, Caesarean birth is due to an emergency situation that endangers the woman's or her baby's health. In these situations, there is no time to wait for the regular process of labor and the decision to perform a Caesarean section must be made very quickly. Indications for an emergency Caesarean may include:
- Maternal bleeding
- The baby being in distress
Anesthesia for Caesarean Section
For a planned or non-emergency Caesarean, an epidural or spinal anesthesia is the anesthesia of choice.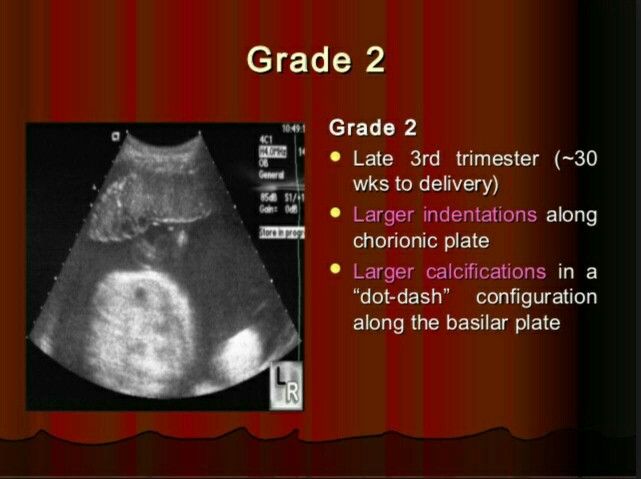 This allows the woman to be awake and able to see her baby immediately after birth. In an emergency situation, the woman would be put to sleep using general anesthesia. This is the fastest anesthesia to administer when time is of the essence.
This allows the woman to be awake and able to see her baby immediately after birth. In an emergency situation, the woman would be put to sleep using general anesthesia. This is the fastest anesthesia to administer when time is of the essence.
If the woman is awake, a support person can be with her for the birth. If general anesthesia is used and the woman is asleep, support people need to wait in the labor room or waiting room until the surgery is completed.
Caesarean Procedure and Recovery
Most often, the doctor will make a low transverse incision — a "bikini cut" — both on the skin, just above the pubic hair, and on the uterus itself. This is a preferable cut for both comfort and recovery. Occasionally an "up and down" or vertical incision is made on the skin, uterus, or both. This is a faster cut and may be used in an emergency. The size and position of your baby also may determine the need for this kind of incision.
Recovery from surgery takes longer than recovery from a vaginal birth.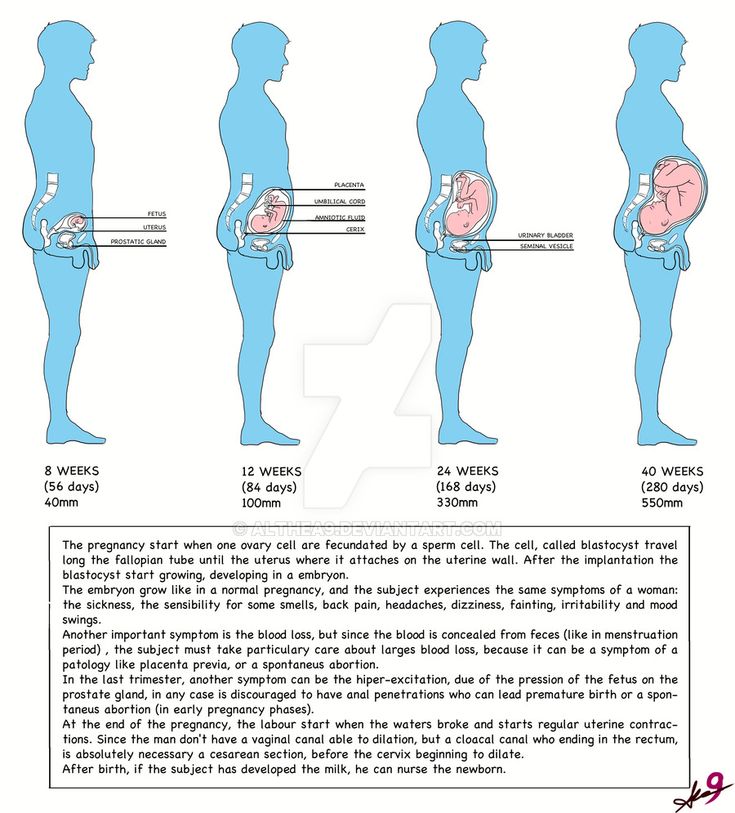 Usually it requires an extra night or two in the hospital, for a total of three to four nights, and more help at home in the first few weeks.
Usually it requires an extra night or two in the hospital, for a total of three to four nights, and more help at home in the first few weeks.
Many women choose to attempt a vaginal birth after Caesarean, called VBAC, and many will succeed. Every woman who has had a Caesarean will need to discuss the subject of VBAC with her provider. Many factors — including the reason for the Caesarean, the type of incision and the number of prior Caesareans — will influence the safety of VBAC.
Birth Plans
You will be provided with a Birth Plan, a form asking about your preferences for delivery. This promotes communication with your health care provider and helps them meet your individual needs. You will complete your Birth Plan and discuss it with your health care provider at your 34 to 36 week visit.
Make photocopies of your Birth Plan. Give one to your health care provider to put in your medical record, and bring one with you when you come to the hospital in labor.
A Week-by-Week Pregnancy Calendar (for Parents)
en español: Calendario del embarazo semana a semana
Reviewed by: KidsHealth Medical Experts
Want to know what to expect during your pregnancy? You've come to the right place! Our illustrated pregnancy calendar is a detailed guide to all the changes taking place in your baby — and in you.
Each week of pregnancy includes a description of your baby's development, as well as an explanation of the changes taking place in your body. You'll also find important medical info that will help keep you and your baby healthy.
A Word About Due Dates and Trimesters
After you announce your pregnancy, the first question you'll probably be asked is "When are you due?" At your first prenatal visit, your health care provider will help you determine an expected delivery date (EDD). Your EDD is 40 weeks from the first day of your last menstrual period (LMP).
It's important to remember that your due date is only an estimate — most babies are born between 38 and 42 weeks from the first day of their mom's LMP and only a small percentage of women actually deliver on their due date.
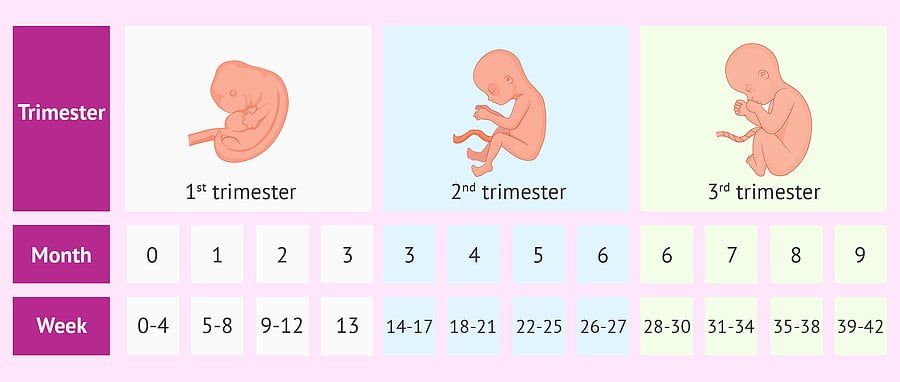
Another common term you'll hear throughout your pregnancy is trimester. A pregnancy is divided into trimesters:
- the first trimester is from week 1 to the end of week 12
- the second trimester is from week 13 to the end of week 26
- the third trimester is from week 27 to the end of the pregnancy
Getting Started
To get started, simply click below on the week of pregnancy you'd like to view. Many of the articles include links to other pregnancy and newborn articles with more information.
Many of the articles include links to other pregnancy and newborn articles with more information.
Check back every week of your pregnancy to see how your baby is developing and to find out what changes you can expect in your own body, too!
PREGNANCY CALENDAR: A week-by-week guide
PREGNANCY CALENDAR: A week-by-week guide
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
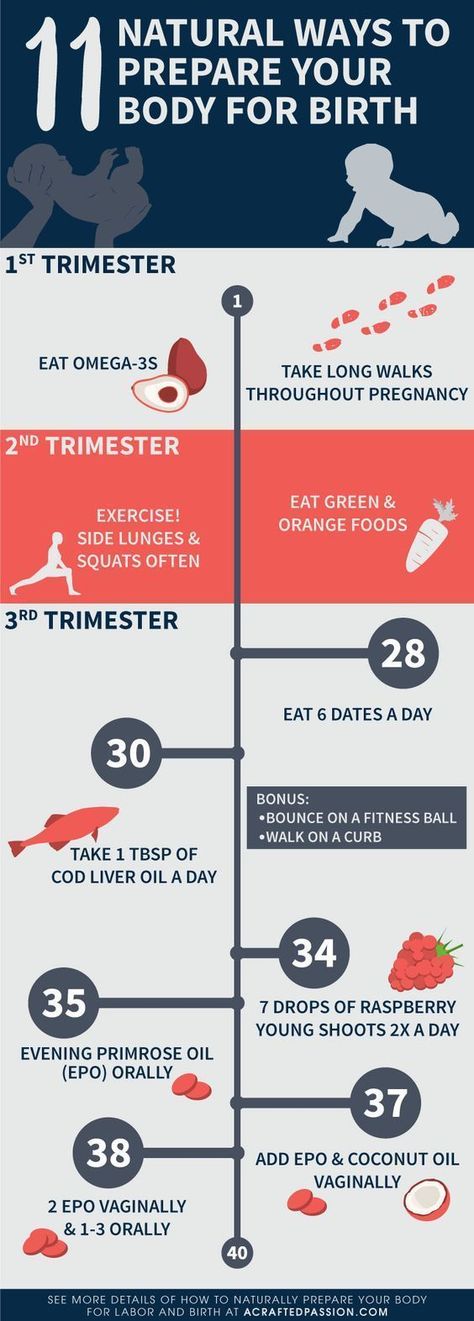
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Trimester 1
- Trimester 2
- Trimester 3
Reviewed by: KidsHealth Medical Experts
Share:
/content/kidshealth/misc/medicalcodes/parents/articles/pregnancy-calendar-intro
1st trimester of pregnancy: what happens to the fetus
1st trimester of pregnancy: what happens to the fetus - Private maternity hospital Ekaterininskaya Clinics1st trimester: 1st-12th weeks
The gestational age is calculated from the first day of the last menstruation, since it is difficult to determine the exact day of conception. Since conception usually occurs in the middle of the menstrual cycle, you are not actually pregnant during the first two weeks, but this period is counted as the beginning of pregnancy.
Since conception usually occurs in the middle of the menstrual cycle, you are not actually pregnant during the first two weeks, but this period is counted as the beginning of pregnancy.
As soon as the fertilization of the egg takes place around the 3rd week, the hormones begin to produce changes in your body little by little. As a result, you may experience some of the following symptoms:
- Morning sickness. As a result of rising levels of hormones characteristic of pregnancy, up to 80% of women in the 1st trimester experience morning sickness with symptoms such as nausea and vomiting. The idea that such malaise is observed only in the morning is a common misconception. In fact, symptoms can appear at any time of the day or night. Up to 1 in 5 women experience morning sickness in the 2nd trimester of pregnancy and can sometimes persist throughout pregnancy.
If you experience morning sickness, avoid foods that make you sick, eat little and often, avoid fatty and spicy foods, drink more water.
 If you experience severe symptoms or symptoms that bother you, see your doctor.
If you experience severe symptoms or symptoms that bother you, see your doctor. - Breast changes. The mammary glands will begin to increase in size, soreness may appear. The nipples will increase in size, become darker and more protruding.
- Fatigue. High levels of the hormone progesterone can make you feel tired and sleepy. Rest as often as possible in a horizontal position with your legs up and eat as well as possible, which is not easy if you are experiencing morning sickness!
- Increased emotionality. A higher level of emotionality, manifested as a result of an increase in hormone levels, is normal. Understanding and patience on the part of your partner and loved ones is very important here.
- Food likes and dislikes. You may find yourself intolerant of one food and addicted to another. This is usually not a problem, unless you feel like eating weird foods like chalk.
 If you are concerned about the situation, contact your doctor.
If you are concerned about the situation, contact your doctor. - Frequent urination. As your fluid levels increase and your uterus puts pressure on your bladder, you will become more likely to visit the toilet. Go to the toilet as soon as you feel the need - this minimizes the pressure on the bladder.
- Feeling of dizziness. Sometimes you may feel a little dizzy (this is due to hormonal changes). Try not to stay on your feet for a long time and slowly rise from a sitting or lying position. If you experience severe dizziness, contact your doctor immediately.
- Heartburn and constipation. Your digestive system will slow down to give you more time to digest your food. This can lead to heartburn and constipation. To help manage heartburn, try to eat small meals at regular intervals and avoid fried or spicy foods and carbonated drinks. Constipation is helped by eating a diet rich in fiber, maintaining physical activity and drinking plenty of water.
1st trimester milestones
- Approximately 7 days after fertilization, the embryo implants in the uterine wall. The placenta, umbilical cord and amniotic sac will begin to form to provide nourishment and protection to the embryo.
- By the end of the first 12 weeks of pregnancy, the uterus is palpable through the wall of the abdomen, the abdomen will begin to grow.
Child development in the 1st trimester of pregnancy
By the end of the 1st trimester:
- All the main organs of the baby are formed, the circulatory system works.
- The development of the sexual organs has begun.
- Fingers are formed on the hands and feet, nails have appeared.
- Facial features have formed.
- The length of the baby's body is about 6 cm from the head to the lower part of the body, he is already recognizable. The baby moves in the amniotic sac, but you don't feel it move yet.
Clinic mobile app
You can make an appointment with a doctor, get tests
and much more...
Fill out the form to make an appointment or order a call back
I agree with personal data processing policy and user agreement I also give my consent to the processing of personal data.
Sign up for a consultation
I agree with personal data processing policy and user agreement I also give my consent to the processing of personal data.
By continuing to use rd.clinic23.ru, you agree to the use of cookies. How to ban the use of certain cookies can be found in Politics
Critical stages of pregnancy - why are they dangerous?
Services
Virtual tour. Clinic "ARNIKA"
The wonderful period of expecting a baby for almost every woman is far from serene: how many anxieties, worries and doubts arise in expectant mothers at this time - they simply cannot be counted.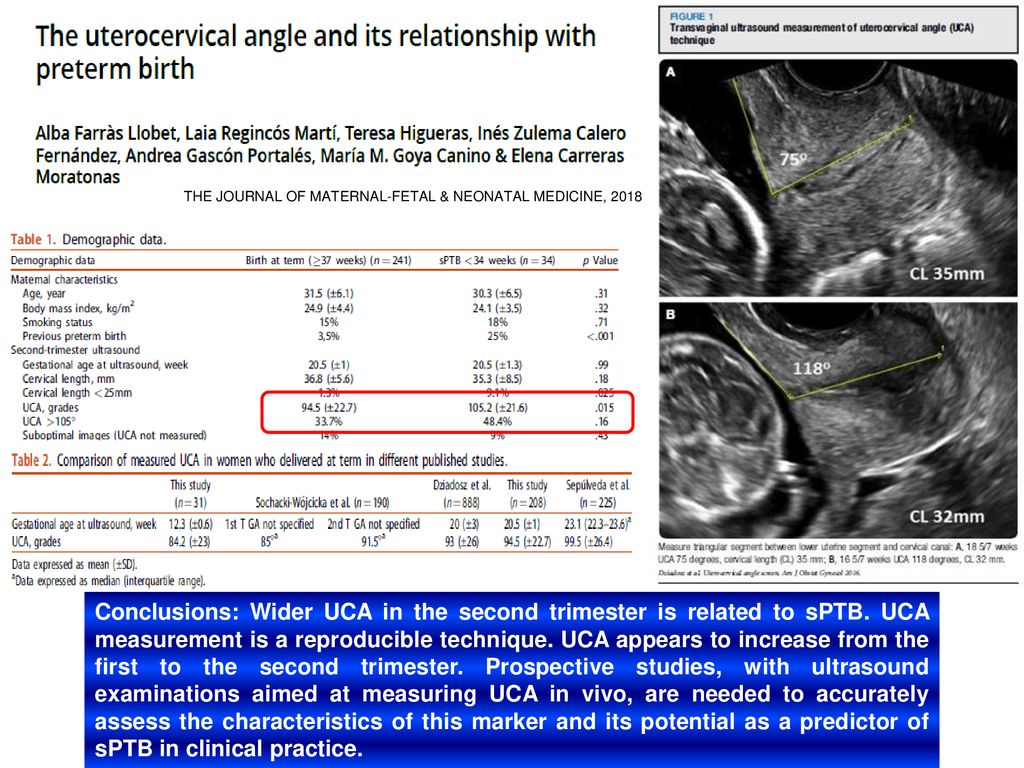 In most cases, all fears are in vain - the baby develops and grows safely. However, it must be remembered that there are also so-called critical periods of pregnancy, when inattention to oneself and one's body can lead to a disastrous result - its spontaneous termination.
In most cases, all fears are in vain - the baby develops and grows safely. However, it must be remembered that there are also so-called critical periods of pregnancy, when inattention to oneself and one's body can lead to a disastrous result - its spontaneous termination.
First trimester
The beginning of a new life in a woman's body, or 2-3 weeks of pregnancy, is considered the first critical period. This is due to the fact that the egg can be fertilized, but due to changes as a result of inflammation, hormonal imbalances, the presence of nodes, scars, fibroids or synechia on the inner mucous membrane of the uterus, implantation does not occur, the embryo dies and is removed from the mother's body during menses. However, even if implantation has occurred, the embryo may stop developing and early miscarriage , and the main reason for this course of events is chromosomal abnormalities.
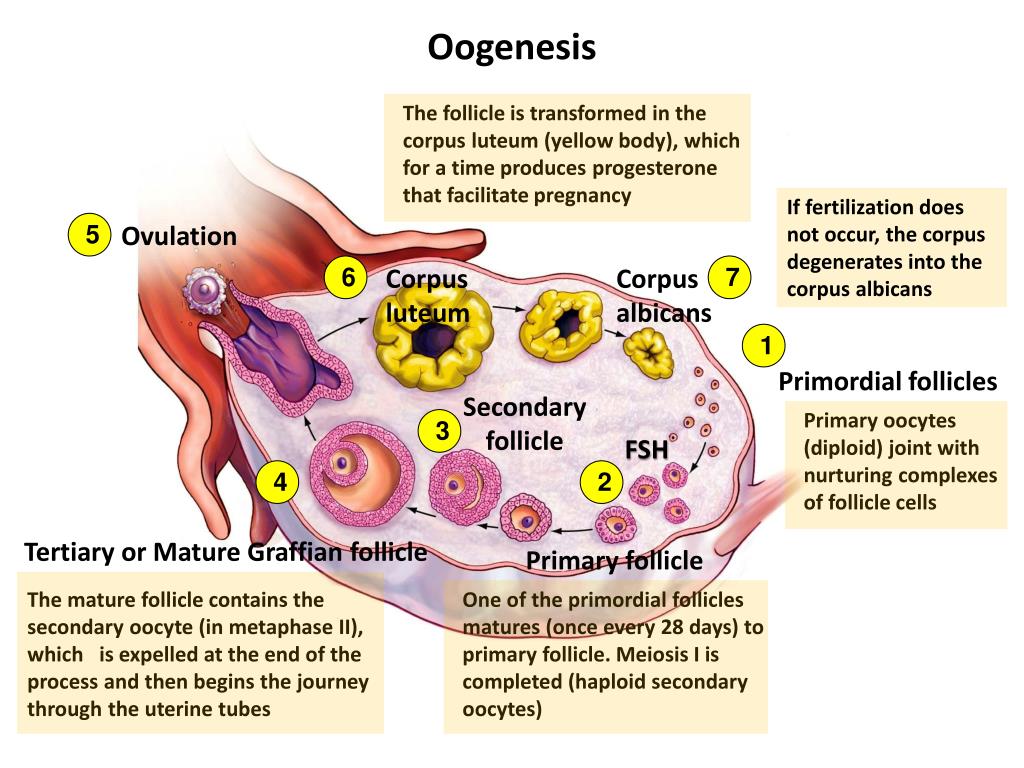
The second critical period of the first trimester begins at 8 and ends at 12 weeks of gestation. At this time, the main cause of interruption is considered to be hormonal deficiency, which disrupts the process of placental formation. This condition may be associated with reduced work of the corpus luteum of the ovaries, excessive production of androgens by the adrenal glands - male sex hormones, as well as malfunctions of the pituitary gland or thyroid gland. The threat of termination of pregnancy can be eliminated with the help of properly selected and timely prescribed hormonal treatment, which will allow the baby to live safely before the due date.
In addition, throughout the first trimester of pregnancy, the fetus may stop developing due to the following adverse environmental factors:
- harmful working conditions
- bad habits
- physical effects - radiation, vibration, intense sports training, etc.
- acute infectious diseases (influenza, cytomegalovirus, herpes, rubella and others)
- severe stressful situations
And even if the fetus develops further, the negative impact of most of these factors may appear after a few months of pregnancy or even after the baby is born: these may be anatomical disorders or severe malformations. Therefore, the entire first trimester of the development of a new life can be considered "critical".
Second trimester
The third critical period of pregnancy occurs at 18-24 weeks of gestation and is largely associated with the active growth of the uterus. At this time, spontaneous interruption most often occurs due to isthmic-cervical insufficiency (ICI), as a result of which the fetal egg descends under the influence of gravity, loses its integrity and triggers the mechanism of labor activity. However, shortening and expansion of the cervical canal, detected in time, allows suturing the cervix or installing an obstetric pessary and safely prolonging the pregnancy. Here we should also remember about infectious diseases, including intrauterine infection, which can disrupt the functions of the placenta, lead to the outflow of water from the fetal bladder and late miscarriage.
Another common reason for interrupting the process of gestation at this time is placenta previa or its low location: for various reasons, it can exfoliate, cause severe bleeding and death of the fetus. In addition, at this time, pregnancy may stop developing due to violations in the development of the brain and the most important functional systems of the baby, caused by the harmful effects of various negative factors on them in the first trimester.
Third trimester
In this trimester - at 28-32 weeks - the fourth critical period takes place. The threat of premature birth may arise due to insufficiency of the placenta, its premature detachment, severe forms of late toxicosis of pregnant women, ICI and various hormonal disorders. In addition, due to the overdistension of the uterus, most multiple pregnancies end at this time. Children born during this period are already viable, but they need long-term qualified medical care.
In addition to all the periods listed above, the critical periods for women who have had reproductive losses in the past are the days of planned menstruation, miscarriages or "fading" of pregnancies. Doctors believe that during these periods the body can “remember” the need for hormonal changes, so they carefully monitor the condition of the expectant mother and baby and prescribe treatment in a timely manner if any threat arises.