What is the first stage of pregnancy called
The First Trimester | Johns Hopkins Medicine
What You Need to Know
- At your first prenatal visit, you will undergo a physical exam as well as certain tests and screenings to assess the health of you and your unborn baby.
- First trimester symptoms vary from woman to woman, with some experiencing all known symptoms and others only a few. Duration of symptoms can vary as well.
- After eight weeks, the embryo is referred to as a fetus.
- Although the fetus is only 1 to 1.5 inches long at this point, all major organs and systems have been formed.
- During the first trimester, the fetus is most susceptible to damage from substances, like alcohol, drugs and certain medicines, and illnesses, like rubella (German measles).
Your First Prenatal Visit
Your first prenatal visit is the most thorough. A complete medical history is taken, a physical exam is done, and certain tests and procedures are performed to assess the health of both you and your unborn baby. Your first prenatal visit may include:
-
Personal medical history. This may include taking record of any of the following:
-
Previous and current medical conditions, like diabetes, high blood pressure (hypertension), anemia and/or allergies
-
Current medicines (prescription, over-the-counter and nutritional supplements)
-
Previous surgeries
-
-
Maternal and paternal family medical history, including illnesses, intellectual or developmental disabilities, and genetic disorders, like sickle cell disease or Tay-Sachs disease
-
Personal gynecological and obstetrical history, including past pregnancies (stillbirths, miscarriages, deliveries, terminations) and menstrual history (length and duration of menstrual periods)
-
Education, including a discussion regarding the importance of proper nutrition and expected weight gain in pregnancy; regular exercise; the avoidance of alcohol, drugs and tobacco during pregnancy; and a discussion of any concerns about domestic violence
-
Pelvic exam.
 This exam may be done for one or all of the following reasons:
This exam may be done for one or all of the following reasons:-
To note the size and position of the uterus
-
To determine the age of the fetus
-
To check the pelvic bone size and structure
-
To perform a Pap test (also called Pap smear) to find the presence of abnormal cells
-
-
Lab tests, including the following:
-
Urine tests. These are done to screen for bacteria, glucose and protein.
-
Blood tests. These are done to determine your blood type.
-
All pregnant women are tested for the Rh factor during the early weeks of pregnancy. Rh incompatibility happens when the mother’s blood is Rh-negative, the father’s blood is Rh-positive and the fetus’ blood is Rh-positive.
 The mother may make antibodies against the Rh-positive fetus, which may lead to anemia in the fetus. Incompatibility problems are watched and appropriate medical treatment is available to prevent the formation of Rh antibodies during pregnancy. There are also other blood antibodies that may cause problems in pregnancy that are screened for on the first visit.
The mother may make antibodies against the Rh-positive fetus, which may lead to anemia in the fetus. Incompatibility problems are watched and appropriate medical treatment is available to prevent the formation of Rh antibodies during pregnancy. There are also other blood antibodies that may cause problems in pregnancy that are screened for on the first visit.
-
-
-
Blood screening tests. These are done to find diseases that could have an effect on the pregnancy. One example is rubella, an infectious disease that is also called German measles.
-
Genetic tests. These are done to find inherited diseases, like sickle cell disease and Tay-Sachs disease.
-
Other screening tests. These are performed to find infectious diseases, like sexually transmitted diseases and urinary tract infections.
The first prenatal visit is also an opportunity to ask any questions or discuss any concerns that you may have about your pregnancy.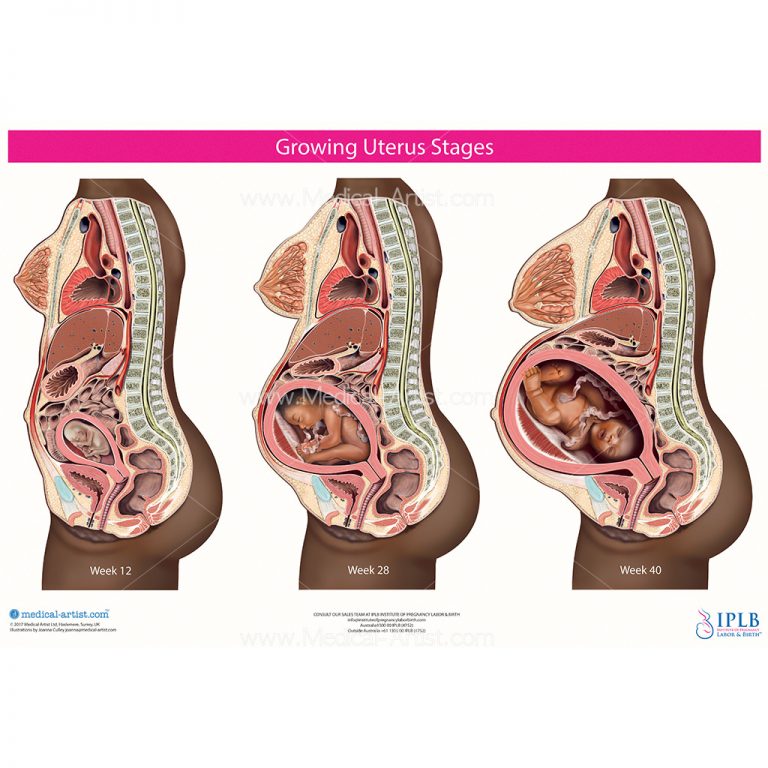
The First Trimester: What to Expect
A healthy first trimester is crucial to the normal development of the fetus. You may not be showing much on the outside yet, but on the inside, all of the major body organs and systems of the fetus are forming.
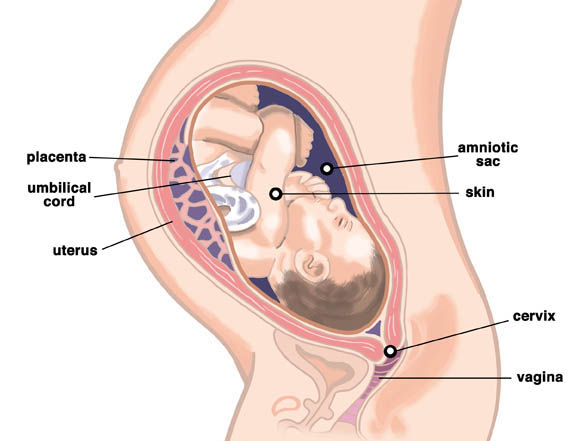
As the embryo implants itself into the uterine wall, several developments take place, including the formation of the:
-
Amniotic sac. A sac filled with amniotic fluid, called the amniotic sac, surrounds the fetus throughout the pregnancy. The amniotic fluid is liquid made by the fetus and the amnion (the membrane that covers the fetal side of the placenta) that protects the fetus from injury. It also helps to regulate the temperature of the fetus.
-
Placenta. The placenta is an organ shaped like a flat cake that only grows during pregnancy. It attaches to the uterine wall with tiny projections called villi. Fetal blood vessels grow from the umbilical cord into these villi, exchanging nourishment and waste products with your blood.
 The fetal blood vessels are separated from your blood supply by a thin membrane.
The fetal blood vessels are separated from your blood supply by a thin membrane. -
Umbilical cord. The umbilical cord is a ropelike cord connecting the fetus to the placenta. The umbilical cord contains two arteries and a vein, which carry oxygen and nutrients to the fetus and waste products away from the fetus.
It is during this first trimester that the fetus is most susceptible to damage from substances, like alcohol, drugs and certain medicines, and illnesses, like rubella (German measles).
During the first trimester, your body and your baby’s body are changing rapidly.
Johns Hopkins Hospital Designated as Baby-Friendly
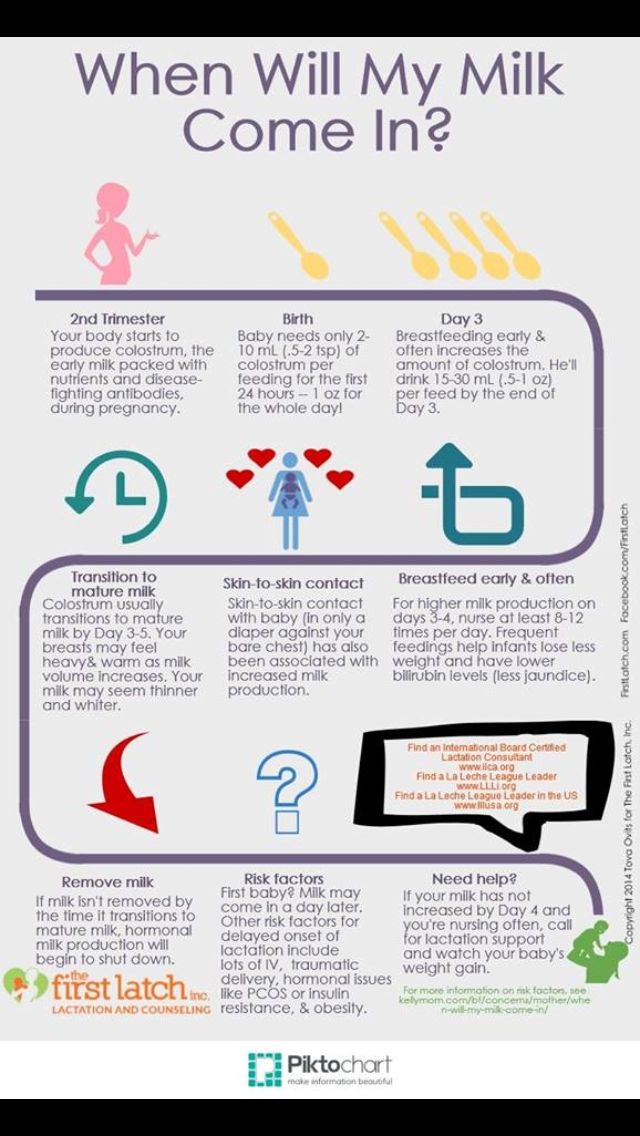
The Baby-Friendly Hospital Initiative, a global program launched by the World Health Organization and the United Nations Children’s Fund, has designated The Johns Hopkins Hospital as Baby-Friendly.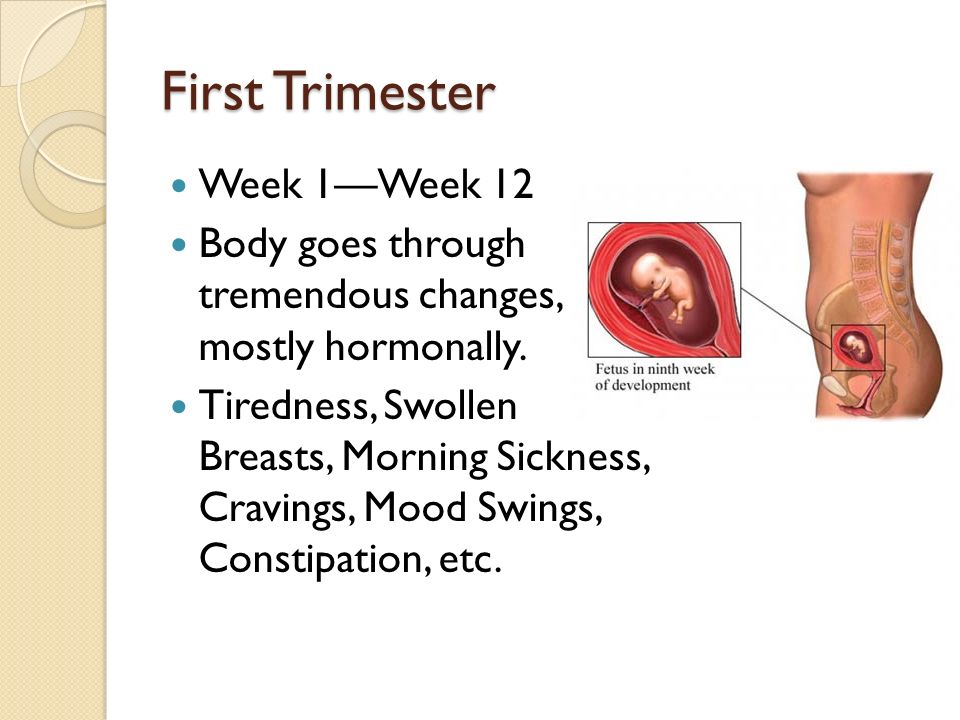 This designation is given to hospitals and birthing centers that offer an optimal level of care for infant feeding and mother-baby bonding.
This designation is given to hospitals and birthing centers that offer an optimal level of care for infant feeding and mother-baby bonding.
Learn more
The First Trimester: Changes to Your Body
During pregnancy, many changes will happen to your body to help nourish and protect your baby. Women experience these changes differently. Some symptoms of pregnancy continue for several weeks or months. Others are only experienced for a short time. Some women experience many symptoms, and other women experience only a few or none at all. The following is a list of changes and symptoms that may happen during the first trimester:
-
The mammary glands enlarge, causing the breasts to swell and become tender in preparation for breast-feeding. This is due to an increased amount of the hormones estrogen and progesterone. A supportive bra should be worn.
-
Your areolas (the pigmented areas around each breast’s nipple) will enlarge and darken.
 They may become covered with small, white bumps called Montgomery’s tubercles (enlarged sweat glands).
They may become covered with small, white bumps called Montgomery’s tubercles (enlarged sweat glands). -
Veins become more noticeable on the surface of your breasts.
-
The uterus is growing and begins to press on your bladder. This causes you to need to urinate more often.
-
Partly due to surges in hormones, you may experience mood swings similar to premenstrual syndrome, a condition experienced by some women that is characterized by mood swings, irritability and other physical symptoms that happen shortly before each menstrual period.
-
Increased levels of hormones to sustain the pregnancy may cause “morning sickness,” which causes nausea and sometimes vomiting. However, morning sickness does not necessarily happen just in the morning and rarely interferes with proper nutrition for the mother and her fetus.
-
Constipation may happen as the growing uterus presses on the rectum and intestines.
-
The muscular contractions in the intestines, which help to move food through the digestive tract, are slowed due to high levels of progesterone. This may, in turn, cause heartburn, indigestion, constipation and gas.
-
Clothes may feel tighter around the breasts and waist, as the size of the stomach begins to increase to accommodate the growing fetus.
-
You may experience extreme tiredness due to the physical and emotional demands of pregnancy.
-
Cardiac volume increases by about 40 to 50 percent from the beginning to the end of the pregnancy. This causes an increased cardiac output. An increased cardiac output may cause an increased pulse rate during pregnancy. The increase in blood volume is needed for extra blood flow to the uterus.
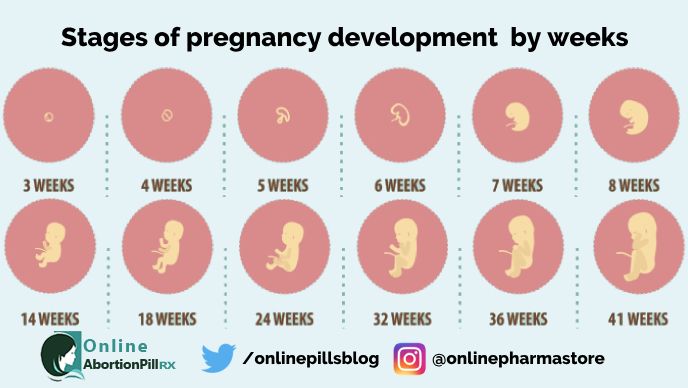
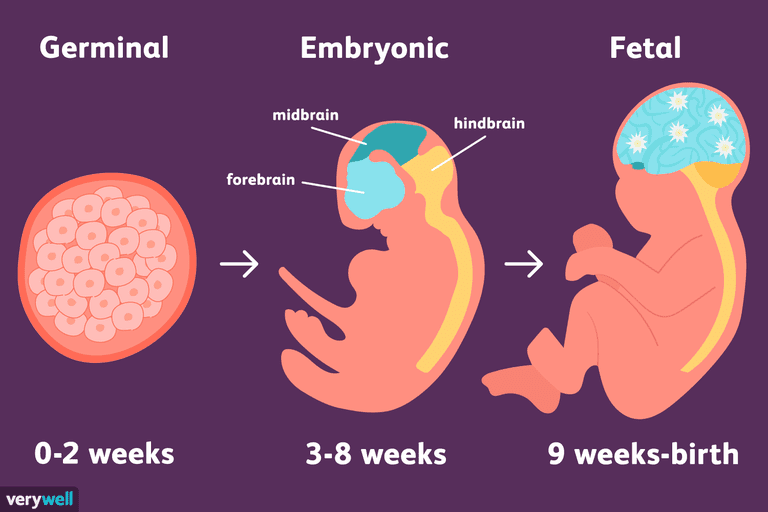
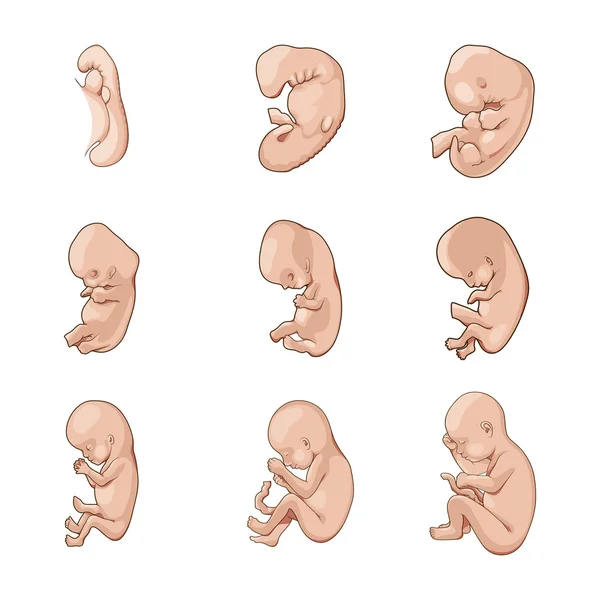
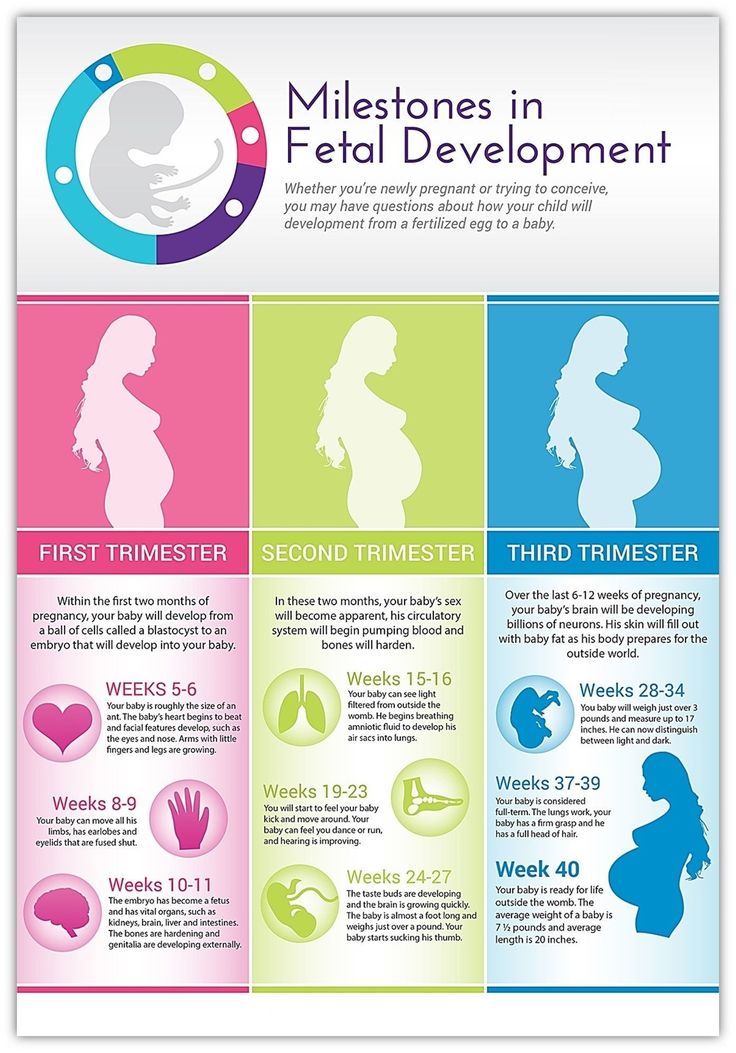
The First Trimester: Fetal Development
The most dramatic changes and development happen during the first trimester.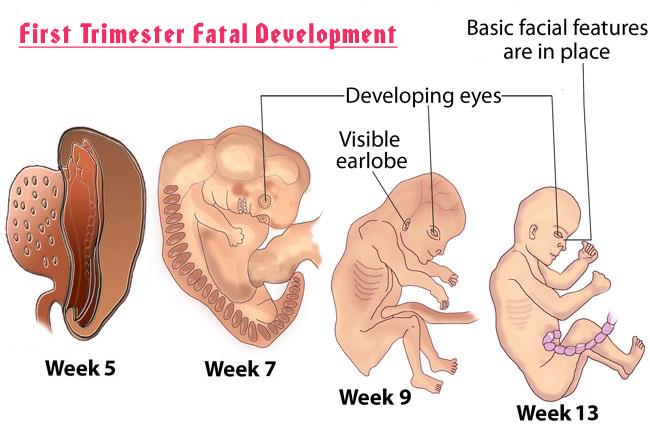 During the first eight weeks, a fetus is called an embryo. The embryo develops rapidly and by the end of the first trimester, it becomes a fetus that is fully formed, weighing approximately 0.5 to 1 ounce and measuring, on average, 3 to 4 inches in length.
During the first eight weeks, a fetus is called an embryo. The embryo develops rapidly and by the end of the first trimester, it becomes a fetus that is fully formed, weighing approximately 0.5 to 1 ounce and measuring, on average, 3 to 4 inches in length.
First Trimester Fetal Growth and Development Benchmarks
The chart below provides benchmarks for most normal pregnancies. However, each fetus develops differently.
| Timing | Development Benchmark |
|---|---|
| By the end of four weeks |
|
| By the end of eight weeks |
|
| From embryo to fetus |
|
| During weeks nine to 12 |
|
The fetus is most vulnerable during the first 12 weeks. During this period of time, all of the major organs and body systems are forming and can be damaged if the fetus is exposed to drugs, infectious agents, radiation, certain medications, tobacco and toxic substances.
Even though the organs and body systems are fully formed by the end of 12 weeks, the fetus cannot survive independently.
Fetal development: Month-By-Month Stages of Pregnancy
When does a pregnancy start?
The start of pregnancy is actually the first day of your last menstrual period. This is called the gestational age, or menstrual age. It’s about two weeks ahead of when conception actually occurs. Though it may seem strange, the date of the first day of your last period will be an important date when determining your due date. Your healthcare provider will ask you about this date and will use it to figure out how far along you are in your pregnancy.
This is called the gestational age, or menstrual age. It’s about two weeks ahead of when conception actually occurs. Though it may seem strange, the date of the first day of your last period will be an important date when determining your due date. Your healthcare provider will ask you about this date and will use it to figure out how far along you are in your pregnancy.
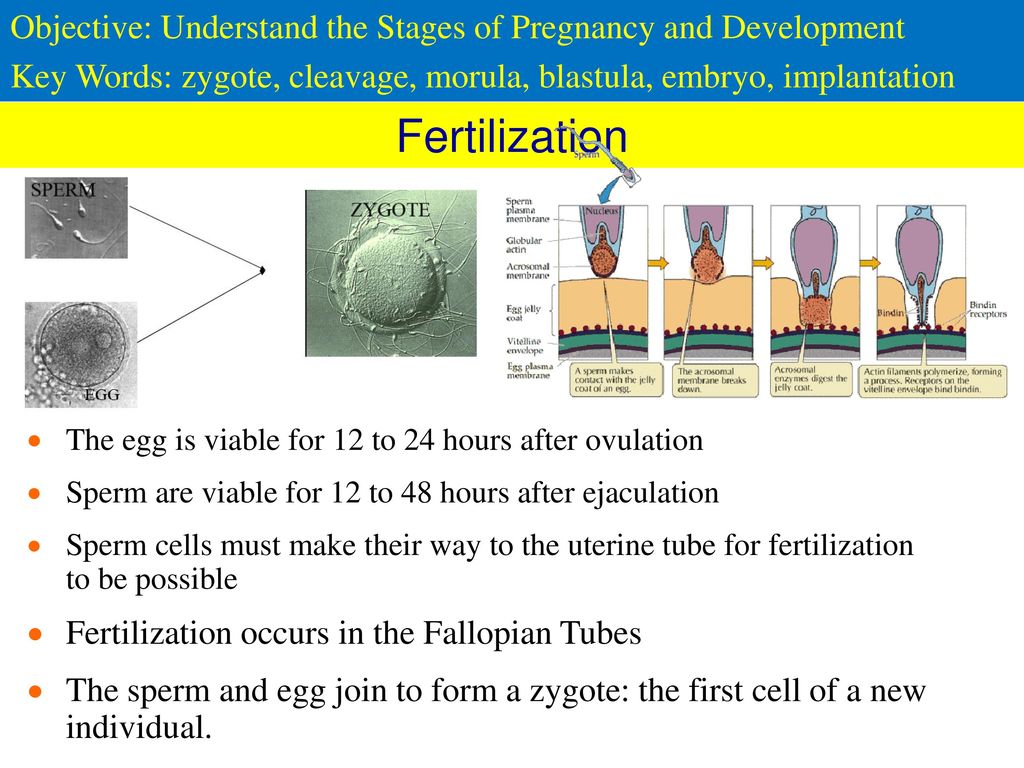
How does conception work?
Each month, your body goes through a reproductive cycle that can end in one of two ways. You will either have a menstrual period or become pregnant. This cycle is continuously happening during your reproductive years — from puberty in your teen years to menopause around age 50.
In a cycle that ends with pregnancy, there are several steps. First, a group of eggs (called oocytes) gets ready to leave the ovary for ovulation (release of the egg). The eggs develop in small, fluid-filled cysts called follicles. Think of these follicles as small containers for each immature egg. Out of this group of eggs, one will become mature and continue on through the cycle.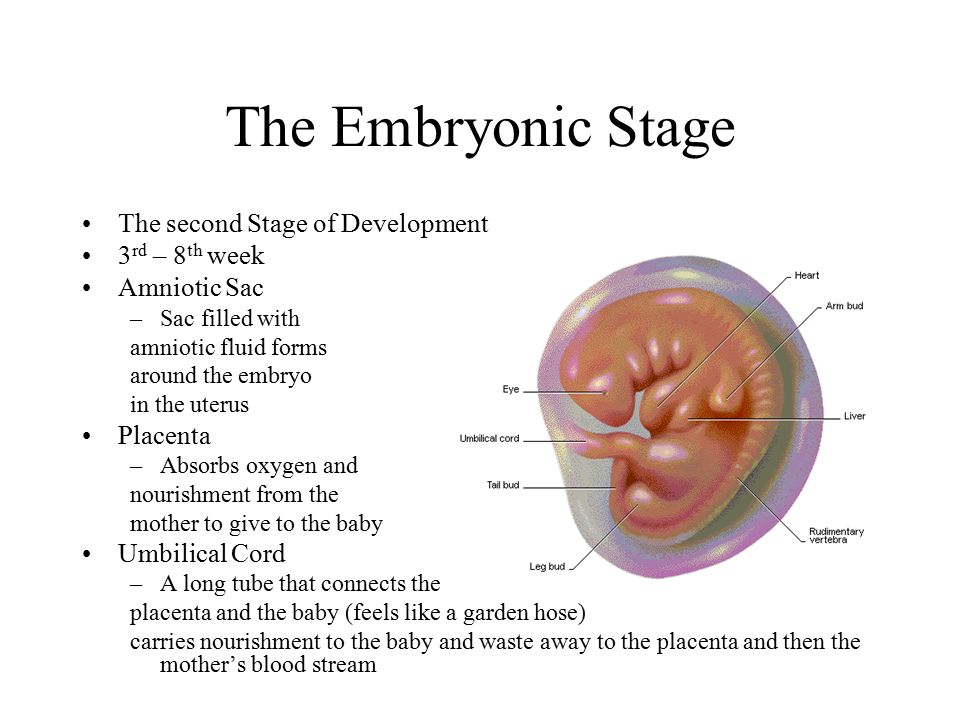 This follicle then suppresses all the other follicles in the group. The other follicles stop growing at this point.
This follicle then suppresses all the other follicles in the group. The other follicles stop growing at this point.
The mature follicle now opens and releases the egg from the ovary. This is ovulation. Ovulation generally happens about two weeks before your next menstrual period begins. It’s generally in the middle of your cycle.
After ovulation, the opened (ruptured) follicle develops into a structure called the corpus luteum. This secretes (releases) the hormones progesterone and estrogen. Progesterone helps prepare the endometrium (lining of the uterus). This lining is the place where a fertilized egg settles to develop. If you don’t become pregnant during a cycle, this lining is what is shed during your period.
On average, fertilization happens about two weeks after your last menstrual period. When the sperm penetrates the egg, changes occur in the protein coating of the egg to prevent other sperm from entering.
At the moment of fertilization, your baby’s genetic make-up is complete, including its sex. The sex of your baby depends on what sperm fertilizes the egg at the moment of conception. Generally, women have a genetic combination of XX and men have XY. Women provide each egg with an X. Each sperm can be either an X or a Y. If the fertilized egg and sperm is a combination of an X and Y, it’s a boy. If there are two Xs, it’s a girl.
The sex of your baby depends on what sperm fertilizes the egg at the moment of conception. Generally, women have a genetic combination of XX and men have XY. Women provide each egg with an X. Each sperm can be either an X or a Y. If the fertilized egg and sperm is a combination of an X and Y, it’s a boy. If there are two Xs, it’s a girl.
What happens right after conception?
Within 24 hours after fertilization, the egg begins rapidly dividing into many cells. It remains in the fallopian tube for about three days after conception. Then the fertilized egg (now called a blastocyte) continues to divide as it passes slowly through the fallopian tube to the uterus. Once there, its next job is to attach to the endometrium. This is called implantation.
Before implantation though, the blastocyte breaks out of its protective covering. When the blastocyte makes contact with the endometrium, the two exchange hormones to help the blastocyte attach. Some women notice spotting (slight bleeding) during the one or two days when implantation happens.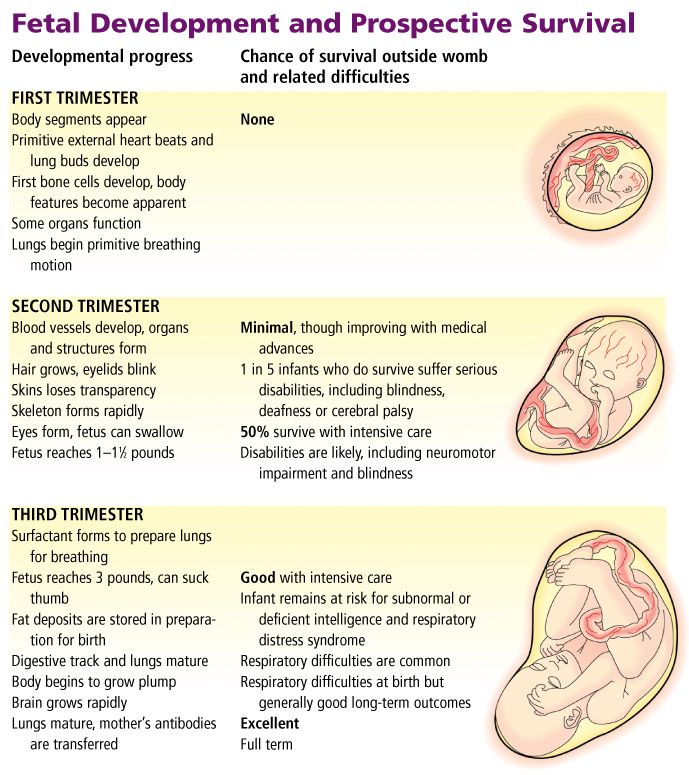 This is normal and isn’t something you should worry about. At this point, the endometrium becomes thicker and the cervix (the opening between your uterus and birth canal) is sealed by a plug of mucus.
This is normal and isn’t something you should worry about. At this point, the endometrium becomes thicker and the cervix (the opening between your uterus and birth canal) is sealed by a plug of mucus.
Within three weeks, the blastocyte cells ultimately form a little ball, or an embryo. By this time, the first nerve cells have formed.
Your developing fetus has already gone through a few name changes in the first few weeks of pregnancy. Generally, it's called an embryo from conception until the eighth week of development. After the eighth week, it's called a fetus until it’s born.
How early can I know I’m pregnant?
From the moment of conception, the hormone human chorionic gonadotrophin (hCG) will be present in your blood. This hormone is created by the cells that form the placenta (food source for the growing fetus). It’s also the hormone detected in a pregnancy test. Even though this hormone is there from the beginning, it takes time for it to build within your body.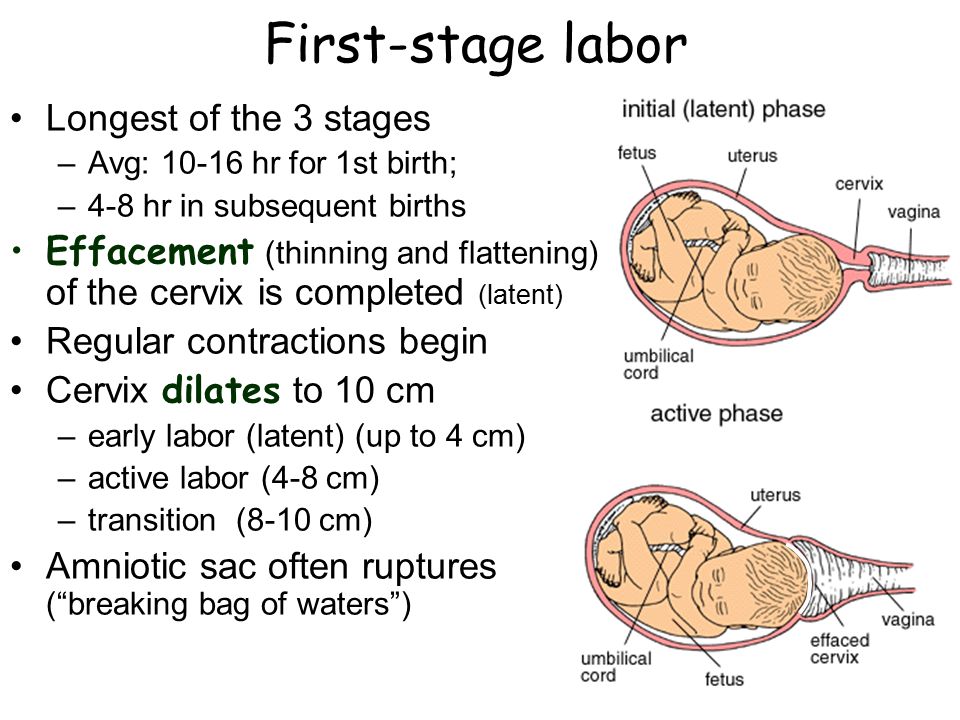 It typically takes three to four weeks from the first day of your last period for the hCG to increase enough to be detected by pregnancy tests.
It typically takes three to four weeks from the first day of your last period for the hCG to increase enough to be detected by pregnancy tests.
When should I reach out to my healthcare provider about a new pregnancy?
Most healthcare providers will have you wait to come in for an appointment until you have had a positive home pregnancy test. These tests are very accurate once you have enough hCG circulating throughout your body. This can be a few weeks after conception. It’s best to call your healthcare provider once you have a positive pregnancy test to schedule your first appointment.
When you call, your healthcare provider may ask you if you are taking a prenatal vitamin. These supplements contain folic acid. It’s important that you get at least 400mcg of folic acid each day during a pregnancy to make sure the fetus's neural tube (beginning of the brain and spine) develops correctly. Many healthcare providers suggest that you take prenatal vitamins with folic acid even when you aren’t pregnant. If you weren’t taking prenatal vitamins before your pregnancy, your provider may ask you to start as early as possible.
If you weren’t taking prenatal vitamins before your pregnancy, your provider may ask you to start as early as possible.
What’s the timeline for fetal development?
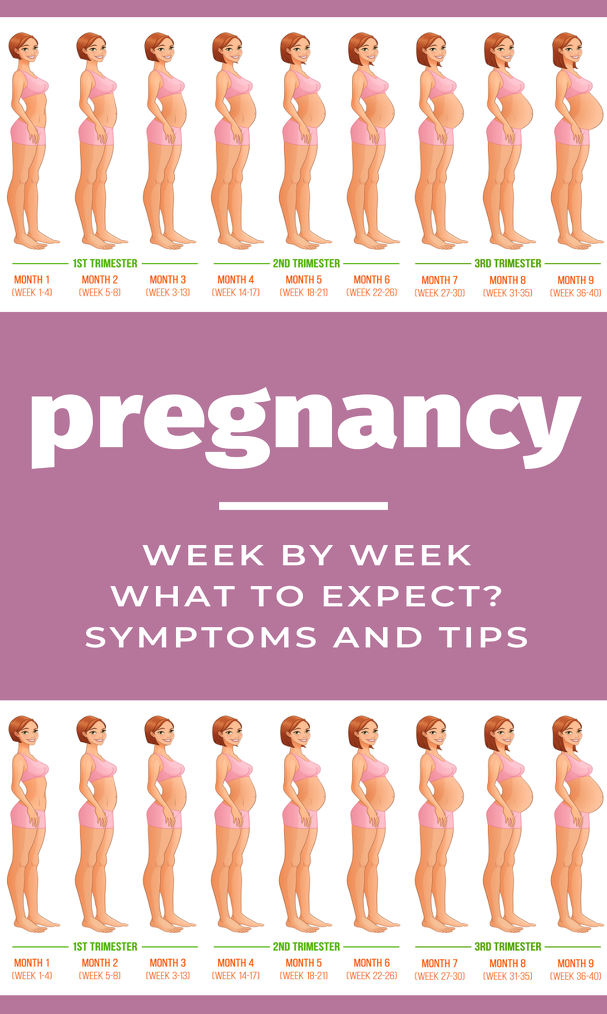
The fetus will change a lot throughout a typical pregnancy. This time is divided into three stages, called trimesters. Each trimester is a set of about three months. Your healthcare provider will probably talk to you about fetal development in terms of weeks. So, if you are three months pregnancy, you are about 12 weeks.
You will see distinct changes in the fetus, and yourself, during each trimester.
Traditionally, we think of a pregnancy as a nine-month process. However, this isn’t always the case. A full-term pregnancy is 40 weeks, or 280 days. Depending on what months you are pregnant during (some are shorter and some longer) and what week you deliver, you could be pregnant for either nine months or 10 months. This is completely normal and healthy.
Once you get close to the end of your pregnancy, there are several category names you might hear regarding when you go into labor.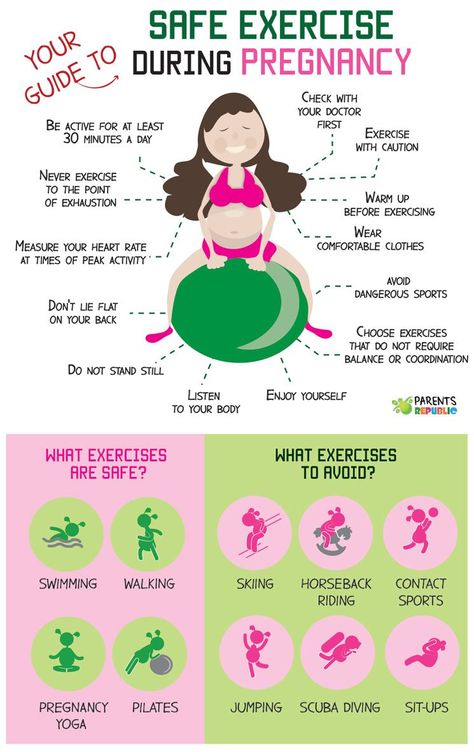 These labels divide up the last few weeks of pregnancy. They’re also used to look out for certain complications in newborns. Babies that are born in the early term period or before may have a higher risk of breathing, hearing or learning issues than babies born a few weeks later in the full term time frame. When you’re looking at these labels, it’s important to know how they’re written. You may see the week first (38) and then you’ll see two numbers separated by a slash mark (6/7). This stands for how many days you currently are in the gestational week. So, if you see 38 6/7, it means that you are on day 6 of your 38th week.
These labels divide up the last few weeks of pregnancy. They’re also used to look out for certain complications in newborns. Babies that are born in the early term period or before may have a higher risk of breathing, hearing or learning issues than babies born a few weeks later in the full term time frame. When you’re looking at these labels, it’s important to know how they’re written. You may see the week first (38) and then you’ll see two numbers separated by a slash mark (6/7). This stands for how many days you currently are in the gestational week. So, if you see 38 6/7, it means that you are on day 6 of your 38th week.
The last few weeks of pregnancy are divided into the following groups:
- Early term: 37 0/7 weeks through 38 6/7 weeks.
- Full term: 39 0/7 weeks through 40 6/7 weeks.
- Late term: 41 0/7 weeks through 41 6/7 weeks.
- Post term: 42 0/7 weeks and on.
Talk to your healthcare provider about any questions you may have about gestational age and due date.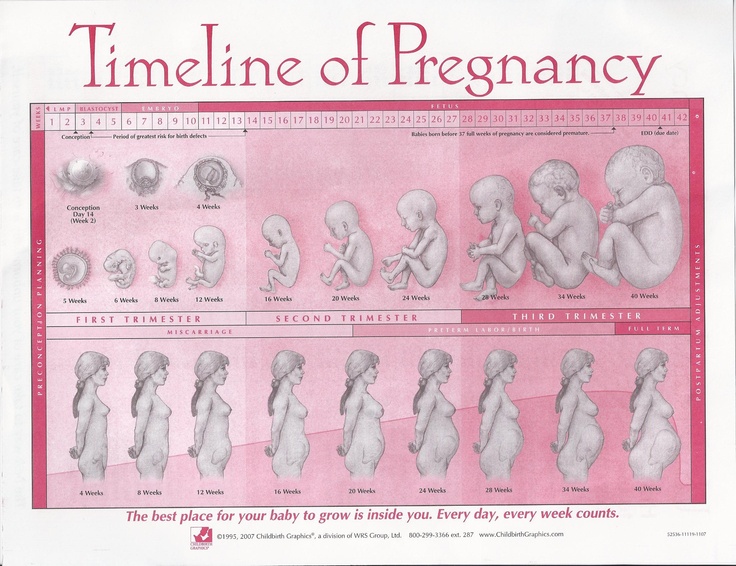
Stages of Growth Month-by-Month in Pregnancy
First trimester
The first trimester will span from conception to 12 weeks. This is generally the first three months of pregnancy. During this trimester, the fertilized egg will change from a small grouping of cells to a fetus that is starting to have a baby’s features.
Month 1 (weeks 1 through 4)
As the fertilized egg grows, a water-tight sac forms around it, gradually filling with fluid. This is called the amniotic sac, and it helps cushion the growing embryo.
During this time, the placenta also develops. The placenta is a round, flat organ that transfers nutrients from the mother to the fetus, and transfers wastes from the fetus. Think of the placenta as a food source for the fetus throughout your pregnancy.
In these first few weeks, a primitive face will take form with large dark circles for eyes. The mouth, lower jaw and throat are developing. Blood cells are taking shape, and circulation will begin. The tiny "heart" tube will beat 65 times a minute by the end of the fourth week.
The tiny "heart" tube will beat 65 times a minute by the end of the fourth week.
By the end of the first month, the fetus is about 1/4 inch long – smaller than a grain of rice.
Month 2 (weeks 5 through 8)
Facial features continue to develop. Each ear begins as a little fold of skin at the side of the head. Tiny buds that eventually grow into arms and legs are forming. Fingers, toes and eyes are also forming.
The neural tube (brain, spinal cord and other neural tissue of the central nervous system) is well formed now. The digestive tract and sensory organs begin to develop too. Bone starts to replace cartilage.
The head is large in proportion to the rest of the body at this point. At about 6 weeks, a heartbeat can usually be detected.
After the 8th week, healthcare providers refer to it as a fetus instead of an embryo.
By the end of the second month, the fetus is about 1 inch long and weighs about 1/30 of an ounce.
Month 3 (weeks 9 through 12)
The arms, hands, fingers, feet and toes are fully formed.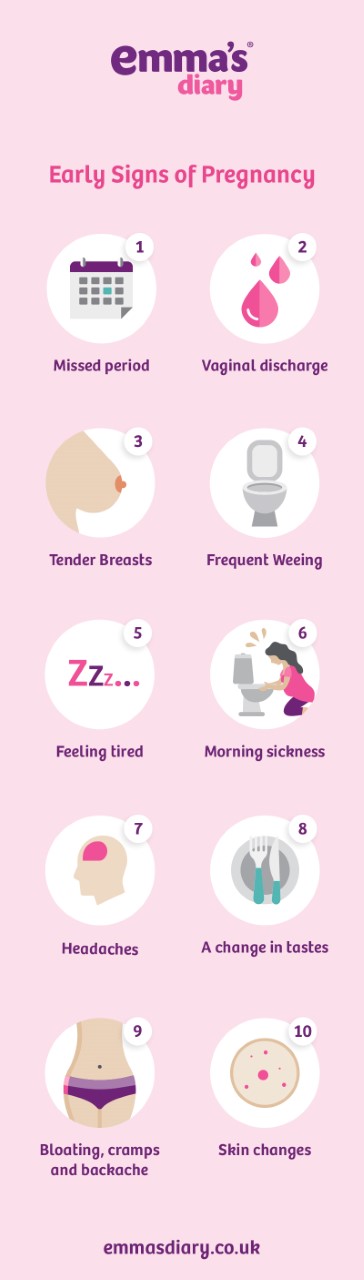 At this stage, the fetus is starting to explore a bit by doing things like opening and closing its fists and mouth. Fingernails and toenails are beginning to develop and the external ears are formed. The beginnings of teeth are forming under the gums. The reproductive organs also develop, but sex is still difficult to distinguish on ultrasound.
At this stage, the fetus is starting to explore a bit by doing things like opening and closing its fists and mouth. Fingernails and toenails are beginning to develop and the external ears are formed. The beginnings of teeth are forming under the gums. The reproductive organs also develop, but sex is still difficult to distinguish on ultrasound.
By the end of the third month, the fetus is fully formed. All the organs and limbs (extremities) are present and will continue to develop in order to become functional. The circulatory and urinary systems are also working and the liver produces bile.
At the end of the third month, the fetus is about 4 inches long and weighs about 1 ounce.
Since the most critical development has taken place, your chance of miscarriage drops considerably after three months.
Second trimester
This middle section of pregnancy is often thought of as the best part of the experience. By this time, any morning sickness is probably gone and the discomfort of early pregnancy has faded. The fetus will start to develop facial features during this month. You may also start to feel movement as the fetus flips and turns in the uterus. During this trimester, many people find out whether their baby will be designated male or female at birth. This is typically done during an anatomy scan (an ultrasound that checks physical development) around 20 weeks.
The fetus will start to develop facial features during this month. You may also start to feel movement as the fetus flips and turns in the uterus. During this trimester, many people find out whether their baby will be designated male or female at birth. This is typically done during an anatomy scan (an ultrasound that checks physical development) around 20 weeks.
Month 4 (weeks 13 through 16)
The fetal heartbeat may now be audible through an instrument called a doppler. The fingers and toes are well-defined. Eyelids, eyebrows, eyelashes, nails and hair are formed. Teeth and bones become denser. The fetus can even suck his or her thumb, yawn, stretch and make faces.
The nervous system is starting to function. The reproductive organs and genitalia are now fully developed, and your doctor can see on ultrasound if the fetus will be designated male or female at birth.
By the end of the fourth month, the fetus is about 6 inches long and weighs about 4 ounces.
Month 5 (weeks 17 through 20)
At this stage, you may begin to feel the fetus moving around. The fetus is developing muscles and exercising them. This first movement is called quickening and can feel like a flutter.
Hair begins to grow on the head. The shoulders, back and temples are covered by a soft fine hair called lanugo. This hair protects the fetus and is usually shed at the end of your baby's first week of life.
The skin is covered with a whitish coating called vernix caseosa. This "cheesy" substance is thought to protect fetal skin from the long exposure to the amniotic fluid. This coating is shed just before birth.
By the end of the fifth month, the fetus is about 10 inches long and weighs from 1/2 to 1 pound.
Month 6 (weeks 21 through 24)
If you could look inside the uterus right now, you would see that the fetus's skin is reddish in color, wrinkled and veins are visible through translucent skin. The finger and toe prints are visible. In this stage, the eyelids begin to part and the eyes open.
In this stage, the eyelids begin to part and the eyes open.
The fetus responds to sounds by moving or increasing the pulse. You may notice jerking motions if the fetus hiccups.
If born prematurely, your baby may survive after the 23rd week with intensive care.
By the end of the sixth month, the fetus is about 12 inches long and weighs about 2 pounds.
Month 7 (weeks 25 through 28)
The fetus continues to mature and develop reserves of body fat. At this point, hearing is fully developed. The fetus changes position frequently and responds to stimuli, including sound, pain and light. The amniotic fluid begins to diminish.
If born prematurely, your baby would be likely to survive after the seventh month.
At the end of the seventh month, the fetus is about 14 inches long and weighs from 2 to 4 pounds.
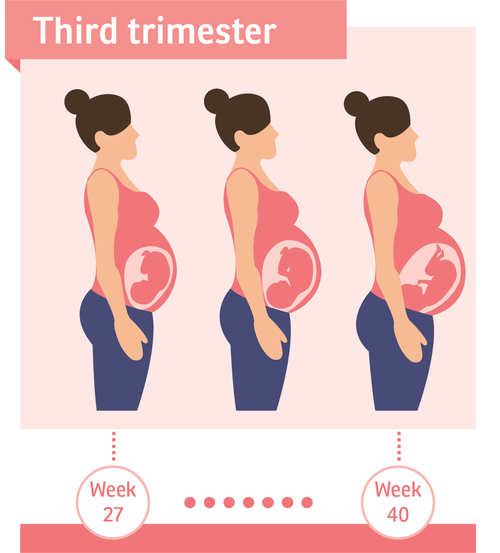
Third trimester
This is the final part of your pregnancy. You may be tempted to start the countdown till your due date and hope that it would come early, but each week of this final stage of development helps the fetus prepare for birth.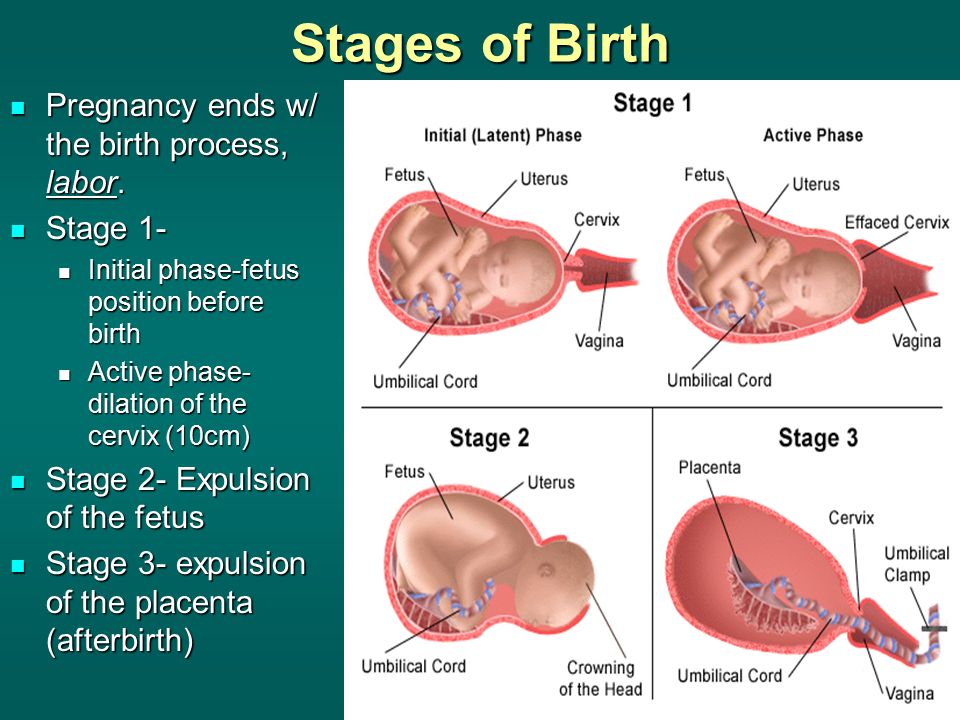 Throughout the third trimester, the fetus gains weight quickly, adding body fat that will help after birth.
Throughout the third trimester, the fetus gains weight quickly, adding body fat that will help after birth.
Remember, even though popular culture only mentions nine months of pregnancy, you may actually be pregnant for 10 months. The typical, full-term pregnancy is 40 weeks, which can take you into a tenth month. It’s also possible that you can go past your due date by a week or two (41 or 42 weeks). Your healthcare provider will monitor you closely as you approach your due date. If you pass your due date, and don’t go into spontaneous labor, your provider may induce you. This means that medications will be used to make you go into labor and have the baby. Make sure to talk to your healthcare provider during this trimester about your birth plan.
Month 8 (weeks 29 through 32)
The fetus continues to mature and develop reserves of body fat. You may notice more kicking. The brain developing rapidly at this time, and the fetus can see and hear. Most internal systems are well developed, but the lungs may still be immature.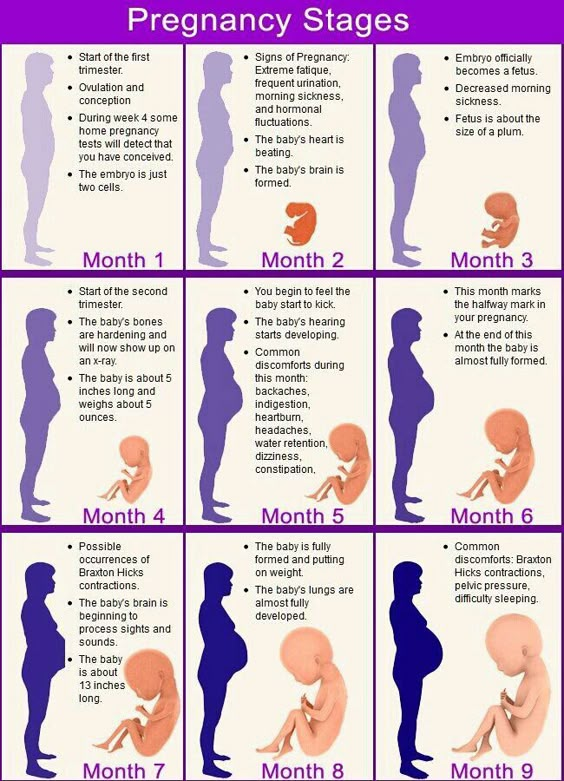
The fetus is about 18 inches long and weighs as much as 5 pounds.
Month 9 (weeks 33 through 36)
During this stage, the fetus continues to grow and mature. The lungs are close to being fully developed at this point.
The fetus has coordinated reflexes and can blink, close the eyes, turn the head, grasp firmly, and respond to sounds, light and touch.
The fetus is about 17 to 19 inches long and weighs from 5 ½ pounds to 6 ½ pounds.
Month 10 (Weeks 37 through 40)
In this final month, you could go into labor at any time. You may notice that less movement because space is tight. At this point, The fetus's position may have changed to prepare for birth. Ideally, it's head down in your uterus. You may feel very uncomfortable in this final stretch of time as the fetus drops down into your pelvis and prepares for birth.
Your baby is ready to meet the world at this point. They are about 18 to 20 inches long and weigh about 7 pounds.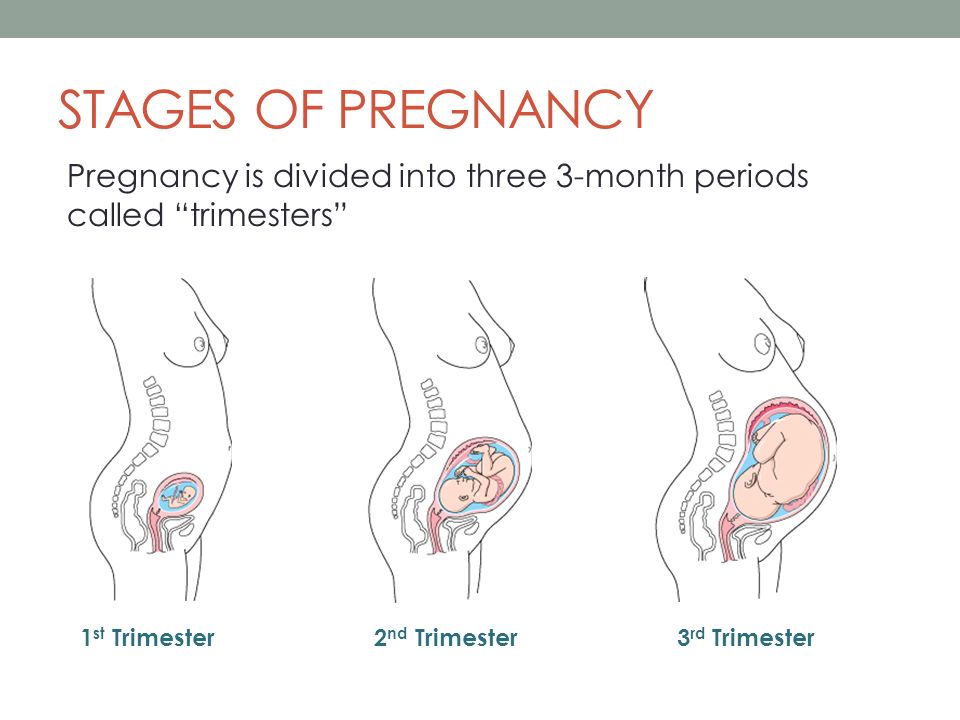
Important to know - Petersburger's health
The total duration of childbirth and their course
The total duration of childbirth depends on many factors: age, physique and physical condition of the woman, her psychological mood, the speed of cervical dilatation, first pregnancy or repeated, the size of the child, the type of presentation and a number of other points.
Labor activity proceeds differently for all women, but the main periods of childbirth are clearly distinguished: 1st period - the period of contractions, the longest and most intense, 2nd period - the direct birth of a baby, 3rd period - the birth of the afterbirth (placenta).
First stage of labor (opening period)
As the name implies, during this period there is a gradual opening of the cervix as a result of regular contractions of the uterine muscles. Contractions occur with a decreasing interval, while they themselves become longer and more frequent.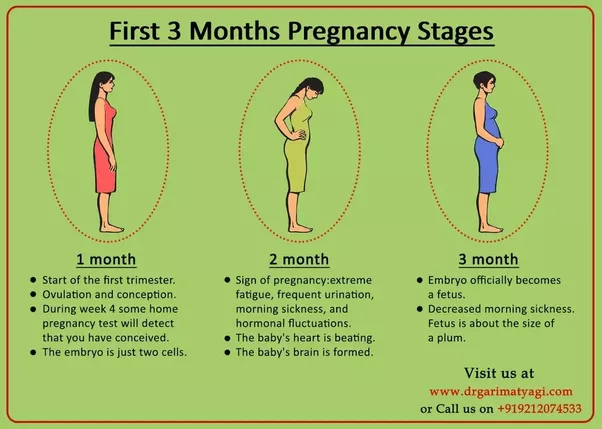
The dilation period is the time elapsed from the onset of regular contractions until the cervix is fully dilated. During this period, the birth canal is prepared for the passage of the fetus through them with all the fetal formations.
Cervical dilatation occurs gradually: at first the cervix is smoothed out, then the pharynx opens up to 3-4 cm and at the end of the first stage of labor up to 10 cm. This is already a complete dilatation of the cervix. With it, during contractions, the fetal bladder becomes tense and bursts at the height of one of them, the anterior portion of amniotic fluid is poured out.
The first stage of labor is the longest and consists of three phases:
1. Latent phase (lasts 5-6 hours). It is characterized by the establishment of regular contractions, with an interval between them of 10-15 minutes. Latent, or hidden, this phase is called because the contractions of the uterus during it are painless or slightly painful. By the end of the phase, the cervix is definitively flattened and opens about 4 cm.
2. Active phase (lasts 3-4 hours). Contractions become more intense, last at least 20 seconds, and the interval between them is reduced to 5-6 minutes. Normally, during the active phase, amniotic fluid is poured out, which contributes to a more rapid full disclosure of the uterine pharynx. By the end of the phase, the uterus opens by 8 cm. This phase is not always clearly manifested, but it is nevertheless distinguished due to the usual weakening of contractions during disclosure from 8 to 10 cm. The child's head descends and stands in the narrow part of the small pelvis, which necessitates a slower and smoother process. Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
Second stage of labor (exile period)
The period of exile is the time from the moment of full opening of the pharynx until the birth of the fetus.
It is the second stage of childbirth that is their culmination, because for a short time (compared to contractions) the long-awaited birth of the baby takes place.
After the discharge of amniotic fluid, contractions temporarily stop. The volume of the uterine cavity decreases, the uterine cavity and vagina appear as a single birth canal. Contractions reappear and become more intense. They are joined by attempts - contractions of the muscle press (abdominal wall, diaphragm and pelvic floor). The frequency and intensity of contractions and attempts are constantly increasing. The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts.
Pushing is a lot of physical work. During attempts, a woman experiences maximum physical stress (blood pressure rises, pulse and respiration become more frequent). During the attempts, the woman holds her breath, and in the intervals between them she rests and "gathers her strength for a new attempt. "
"
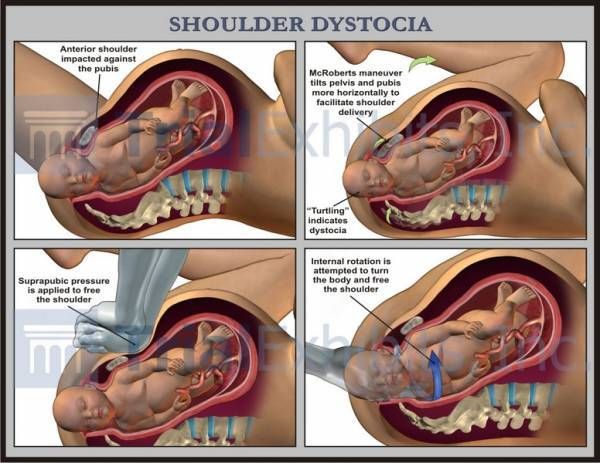
In the process of one of the attempts, the head is born. Next, the shoulders are born (first the front, then the back) and the torso. Following the fetus, the posterior amniotic fluid is poured out with an admixture of cheese-like lubricant.
A woman in labor, having experienced severe fatigue, rests after hard work (pulse and respiration rate decrease).
Third stage of labor (postpartum period).
The afterbirth period is the time from the birth of the fetus to the birth of the placenta. During this period, the placenta separates from the walls of the uterus and the birth of the placenta (placenta with membranes and umbilical cord).
In the process of separation of the placenta from the walls of the uterus, the uteroplacental vessels are damaged, which is normally accompanied by blood loss in the amount of 100-200 ml, without adversely affecting the woman's condition. After the birth of the placenta, the uterus contracts sharply, becomes dense, which is necessary to stop bleeding in the area of the placental site; its bottom is in the middle between the womb and the navel.
During this period, the woman's pulse and respiration normalize. Her demeanor is calm. Sometimes chills can be observed (as a reaction to the transferred strong physical stress).
The third period is no longer as exciting and tense as the previous two. The child was born and the matter remains for the small - the separation of the placenta, or placenta. Nature provides for the resumption of contractions a few minutes after the birth of the baby, which is necessary for effective exfoliation from the uterus of the tissues that nourished the fetus during pregnancy (placenta, membranes, umbilical cord).
Three periods of physiological labor - the natural end of a nine-month wait. Most likely, during the birth process itself, the woman in labor will not care what the period or phase of childbirth is now, but it is still desirable to know about them, at least for greater certainty before going to the hospital.
Critical stages of pregnancy - why are they dangerous?
Services
Virtual tour.
 Clinic "ARNIKA"
Clinic "ARNIKA"
The wonderful period of waiting for a baby for almost every woman is far from serene: how many anxieties, worries and doubts arise in expectant mothers at this time - they simply cannot be counted. In most cases, all fears are in vain - the baby develops and grows safely. However, it must be remembered that there are also so-called critical periods of pregnancy, when inattention to oneself and one's body can lead to a disastrous result - its spontaneous termination.
First trimester
The beginning of a new life in a woman's body, or 2-3 weeks of pregnancy, is considered the first critical period. This is due to the fact that the egg can be fertilized, but due to changes as a result of inflammation, hormonal imbalances, the presence of nodes, scars, fibroids or synechia on the inner mucous membrane of the uterus, implantation does not occur, the embryo dies and is removed from the mother's body during menses. However, even if implantation has occurred, the embryo may stop developing and early miscarriage , and the main reason for this course of events is chromosomal abnormalities.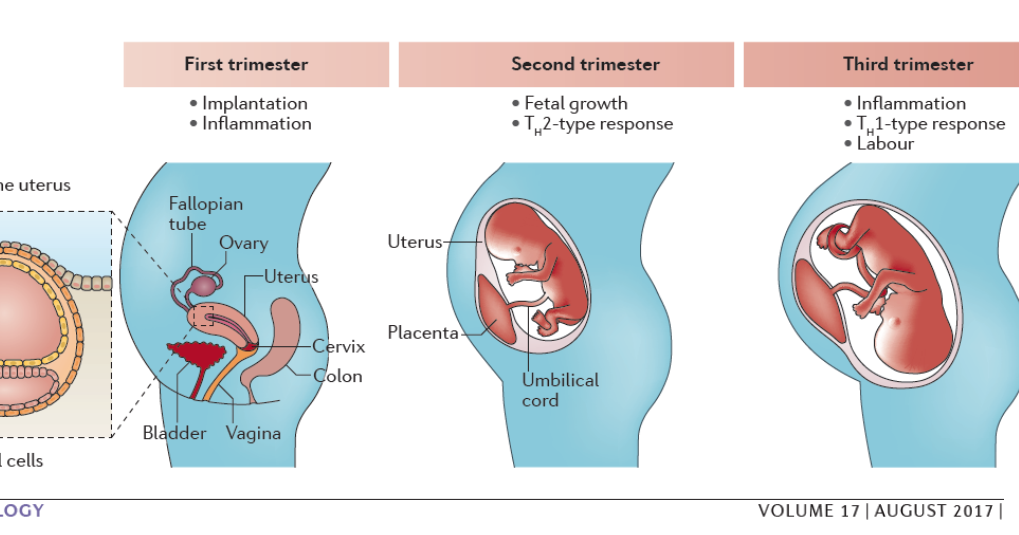
The second critical period of the first trimester begins at 8 and ends at 12 weeks of gestation. At this time, the main cause of interruption is considered to be hormonal deficiency, which disrupts the process of placental formation. This condition may be associated with reduced work of the corpus luteum of the ovaries, excessive production of androgens by the adrenal glands - male sex hormones, as well as malfunctions of the pituitary gland or thyroid gland. The threat of abortion can be eliminated with the help of properly selected and timely prescribed hormonal treatment, which will allow the baby to safely reach the due date.
In addition, throughout the first trimester of pregnancy, the fetus may stop developing due to the following adverse environmental factors: And even if the fetus develops further, the negative impact of most of these factors may appear after a few months of pregnancy or even after the baby is born: these may be anatomical disorders or severe malformations. The third critical period of pregnancy occurs at 18-24 weeks of gestation and is largely associated with the active growth of the uterus. At this time, spontaneous interruption most often occurs due to isthmic-cervical insufficiency (ICI), as a result of which the fetal egg descends under the influence of gravity, loses its integrity and triggers the mechanism of labor activity. However, shortening and expansion of the cervical canal, detected in time, allows suturing the cervix or installing an obstetric pessary and safely prolonging the pregnancy. Here we should also remember about infectious diseases, including intrauterine infection, which can disrupt the functions of the placenta, lead to the outflow of water from the fetal bladder and late miscarriage. Another common reason for interrupting the process of gestation at this time is placenta previa or its low location: for various reasons, it can exfoliate, cause severe bleeding and death of the fetus. In this trimester - at 28-32 weeks - the fourth critical period takes place. The threat of premature birth may occur due to insufficiency of the placenta, its premature detachment, severe forms of late toxicosis of pregnant women, ICI and various hormonal disorders. In addition, due to the overdistension of the uterus, most multiple pregnancies end at this time. Children born during this period are already viable, but they need long-term qualified medical care. In addition to all the periods listed above, the critical periods for women who have had reproductive losses in the past are the days of planned menstruation, miscarriages or “fading” of pregnancies. Doctors believe that during these periods the body can “remember” the need for hormonal changes, so they carefully monitor the condition of the expectant mother and baby and prescribe treatment in a timely manner if any threat arises. Therefore, the entire first trimester of the development of a new life can be considered "critical".
Therefore, the entire first trimester of the development of a new life can be considered "critical". Second trimester
 In addition, at this time, pregnancy may stop developing due to violations in the development of the brain and the most important functional systems of the baby, caused by the harmful effects of various negative factors on them in the first trimester.
In addition, at this time, pregnancy may stop developing due to violations in the development of the brain and the most important functional systems of the baby, caused by the harmful effects of various negative factors on them in the first trimester. Third trimester