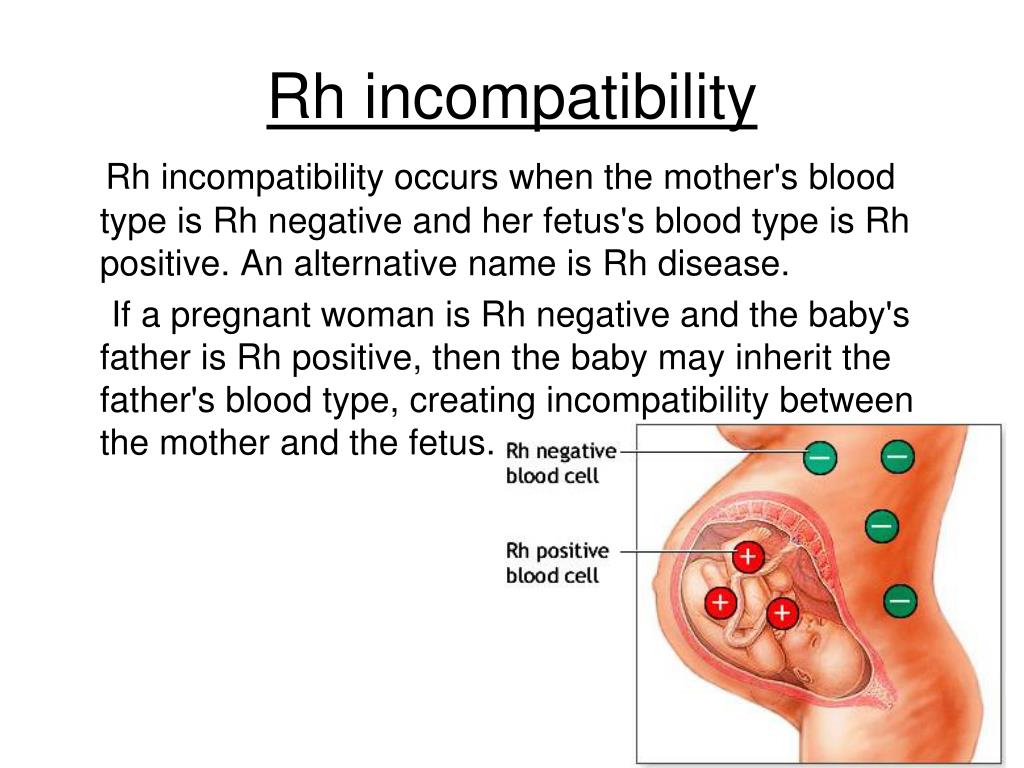
What is rhesus disease
Rhesus disease - NHS
Rhesus disease is a condition where antibodies in a pregnant woman's blood destroy her baby's blood cells. It's also known as haemolytic disease of the foetus and newborn (HDFN).
Rhesus disease doesn't harm the mother, but it can cause the baby to become anaemic and develop newborn jaundice.
Read about the symptoms of rhesus disease in a baby.
What causes rhesus disease?
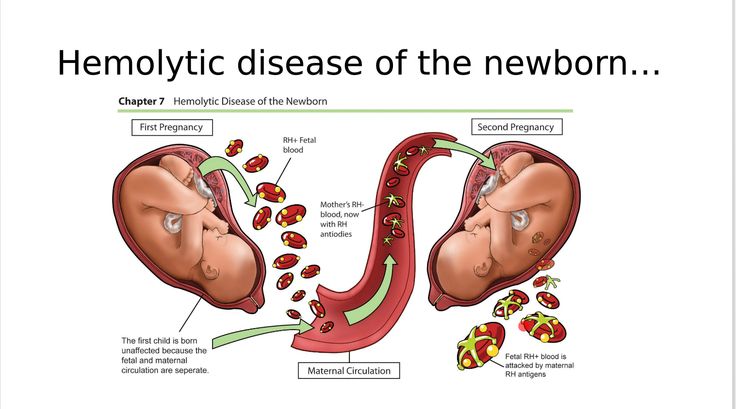
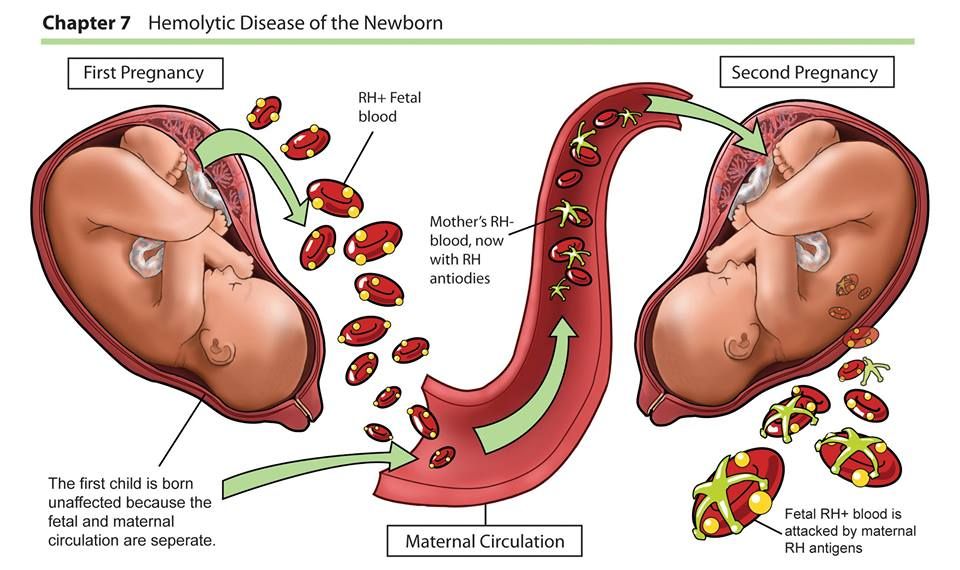
Rhesus disease only happens when the mother has rhesus negative blood (RhD negative) and the baby in her womb has rhesus positive blood (RhD positive). The mother must have also been previously sensitised to RhD positive blood.
Sensitisation happens when a woman with RhD negative blood is exposed to RhD positive blood, usually during a previous pregnancy with an RhD positive baby. The woman’s body responds to the RhD positive blood by producing antibodies (infection-fighting molecules) that recognise the foreign blood cells and destroy them.
If sensitisation occurs, the next time the woman is exposed to RhD positive blood, her body produces antibodies immediately. If she's pregnant with an RhD positive baby, the antibodies can cross the placenta, causing rhesus disease in the unborn baby. The antibodies can continue attacking the baby's red blood cells for a few months after birth.
Read more about the causes of rhesus disease.
Preventing rhesus disease
Rhesus disease is uncommon these days because it can usually be prevented using injections of a medication called anti-D immunoglobulin.
All women are offered blood tests as part of their antenatal checks and tests to determine whether their blood is RhD negative or positive. If the mother is RhD negative, she'll be offered injections of anti-D immunoglobulin at certain points in her pregnancy when she may be exposed to the baby's red blood cells.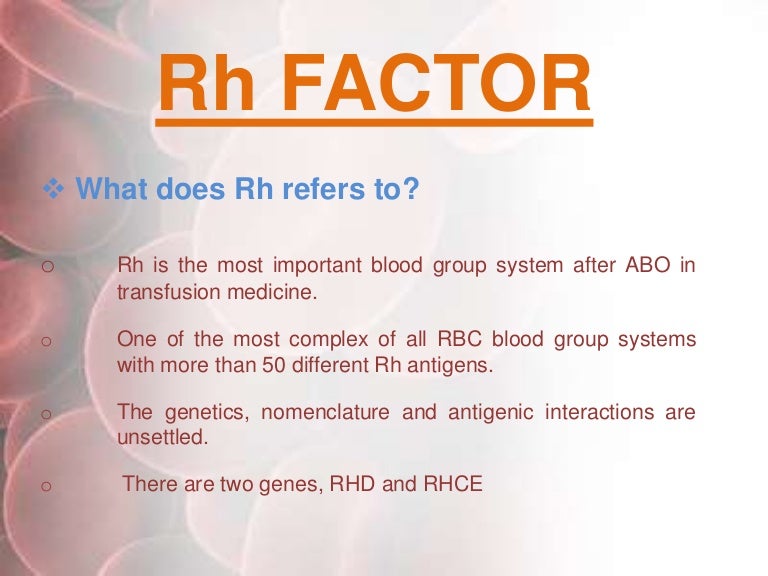 This anti-D immunoglobulin helps to remove the RhD foetal blood cells before they can cause sensitisation.
This anti-D immunoglobulin helps to remove the RhD foetal blood cells before they can cause sensitisation.
If a woman has developed anti-D antibodies in a previous pregnancy (she's already sensitised) then these immunoglobulin injections don't help. The pregnancy will be monitored more closely than usual, as will the baby after delivery.
Read more about preventing rhesus disease and diagnosing rhesus disease.
Treating rhesus disease
If an unborn baby does develop rhesus disease, treatment depends on how severe it is. A blood transfusion to the unborn baby may be needed in more severe cases. After delivery, the child is likely to be admitted to a neonatal unit (a hospital unit that specialises in caring for newborn babies).
Treatment for rhesus disease after delivery can include a light treatment called phototherapy, blood transfusions, and an injection of a solution of antibodies (intravenous immunoglobulin) to prevent red blood cells being destroyed.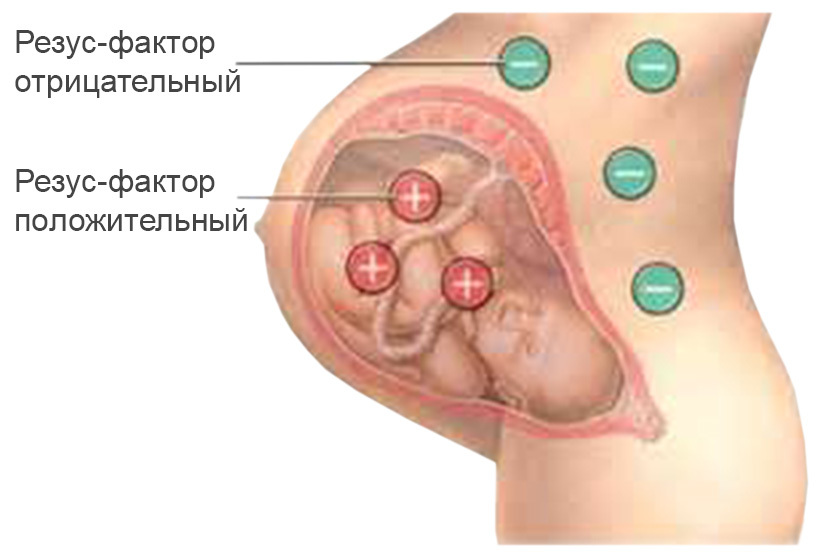
If rhesus disease is left untreated, severe cases can lead to stillbirth. In other cases, it could lead to brain damage, learning difficulties, hearing loss and blindness and vision loss. However, treatment is usually effective and these problems are uncommon.
Read more about treating rhesus disease and the potential complications of rhesus disease.
Page last reviewed: 16 November 2021
Next review due: 16 November 2024
Rhesus disease - Treatment - NHS
Treatment for rhesus disease depends on how severe the condition is. In more severe cases, treatment may need to begin before the baby is born.
Around half of all cases of rhesus disease are mild and don't usually require much treatment. However, your baby will need to be monitored regularly, in case serious problems develop.
In more severe cases, a treatment called phototherapy is usually needed and blood transfusions may help to speed up the removal of bilirubin (a substance created when red blood cells break down) from the body.
In the most serious cases, a blood transfusion may be carried out while your baby is still in the womb and a medication called intravenous immunoglobulin may be used when they're born if phototherapy isn't effective.
If necessary, the baby may be delivered early using medication to start inducing labour (induction) or a caesarean section, so treatment can start as soon as possible. This is usually only done after about 34 weeks of pregnancy.
Phototherapy
Phototherapy is treatment with light. It involves placing the newborn baby under a halogen or fluorescent lamp with their eyes covered.
Alternatively, they may be placed on a blanket containing optical fibres through which light travels and shines onto the baby's back (fibre optic phototherapy).
The light absorbed by the skin during phototherapy lowers the bilirubin levels in the baby's blood through a process called photo-oxidation.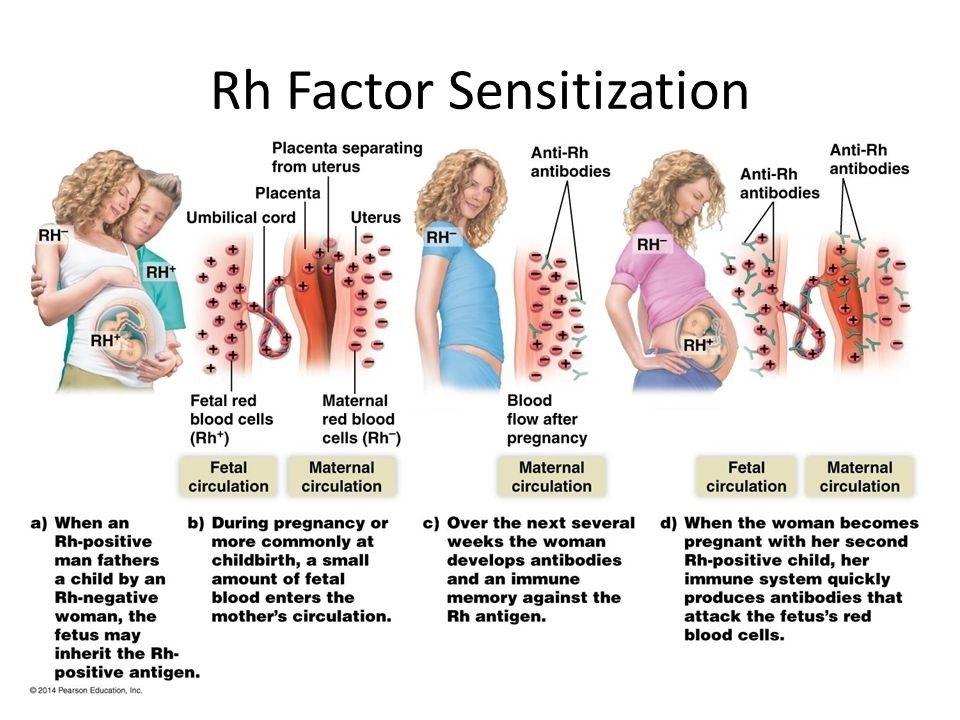 This means that oxygen is added to the bilirubin, which helps it to dissolve in water. This makes it easier for the baby's liver to break down the bilirubin and remove it from the blood.
This means that oxygen is added to the bilirubin, which helps it to dissolve in water. This makes it easier for the baby's liver to break down the bilirubin and remove it from the blood.
During phototherapy, fluids will usually be given into a vein (intravenous hydration) because more water is lost through your baby's skin and more urine is produced as the bilirubin is expelled.
Using phototherapy can sometimes reduce the need for a blood transfusion.
Blood transfusions
In some cases, the levels of bilirubin in the blood may be high enough to require one or more blood transfusions.
During a blood transfusion, some of your baby's blood is removed and replaced with blood from a suitable matching donor (someone with the same blood group). A blood transfusion normally takes place through a tube inserted into a vein (intravenous cannula).
This process helps to remove some of the bilirubin in the baby's blood and also removes the antibodies that cause rhesus disease.
It's also possible for the baby to have a transfusion of just red blood cells to top up those they already have.
Blood transfusion to an unborn baby
If your baby develops rhesus disease while still in the womb, they may need to be given a blood transfusion before birth. This is known as intrauterine foetal blood transfusion.
An intrauterine foetal blood transfusion requires specialist training and is not available in all hospitals. You may therefore be referred to a different hospital for the procedure.
A needle is usually inserted through the mother's abdomen (tummy) and into the umbilical cord, so donated blood can be injected into the baby. An ultrasound scan is used to help guide the needle to the right place.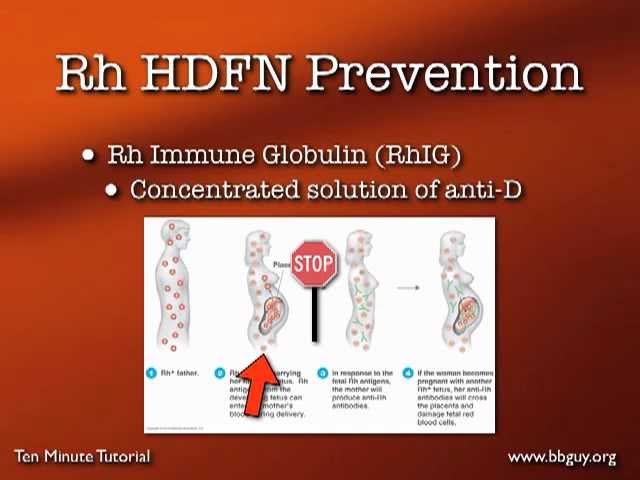
Local anaesthetic is used to numb the area, but you'll be awake during the procedure. A sedative may be given to keep you relaxed and your baby may also be sedated to help stop them moving during the procedure.
You may need more than one intrauterine foetal blood transfusion. Transfusions can be repeated every 2 to 4 weeks until your baby is mature enough to be delivered. They may even reduce the need for phototherapy after birth, but further blood transfusions could still be necessary.
There's a small risk of miscarriage during an intrauterine foetal blood transfusion, so it's usually only used in particularly severe cases.
Intravenous immunoglobulin
In some cases, treatment with intravenous immunoglobulin (IVIG) is used alongside phototherapy if the level of bilirubin in your baby's blood continues to rise at an hourly rate.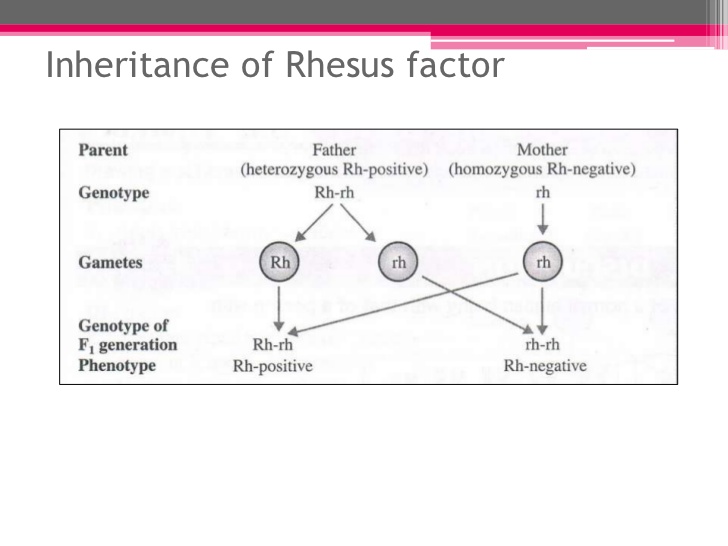
The immunoglobulin is a solution of antibodies (proteins produced by the immune system to fight against disease-carrying organisms) taken from healthy donors. Intravenous means that it's injected into a vein.
Intravenous immunoglobulin helps to prevent red blood cells being destroyed, so the level of bilirubin in your baby's blood will stop rising. It also reduces the need for a blood transfusion.
However, it does carry some small risks. It's possible that your baby may have an allergic reaction (anaphylaxis) to the immunoglobulin, although it's difficult to calculate how likely this is or how severe the reaction will be.
Concerns over possible side effects, and the limited supply of intravenous immunoglobulin, mean that it's only used when the bilirubin level is rising rapidly, despite phototherapy sessions.
Intravenous immunoglobulin has also been used during pregnancy, in particularly severe cases of rhesus disease, as it can delay the need for treatment with intrauterine foetal blood transfusions.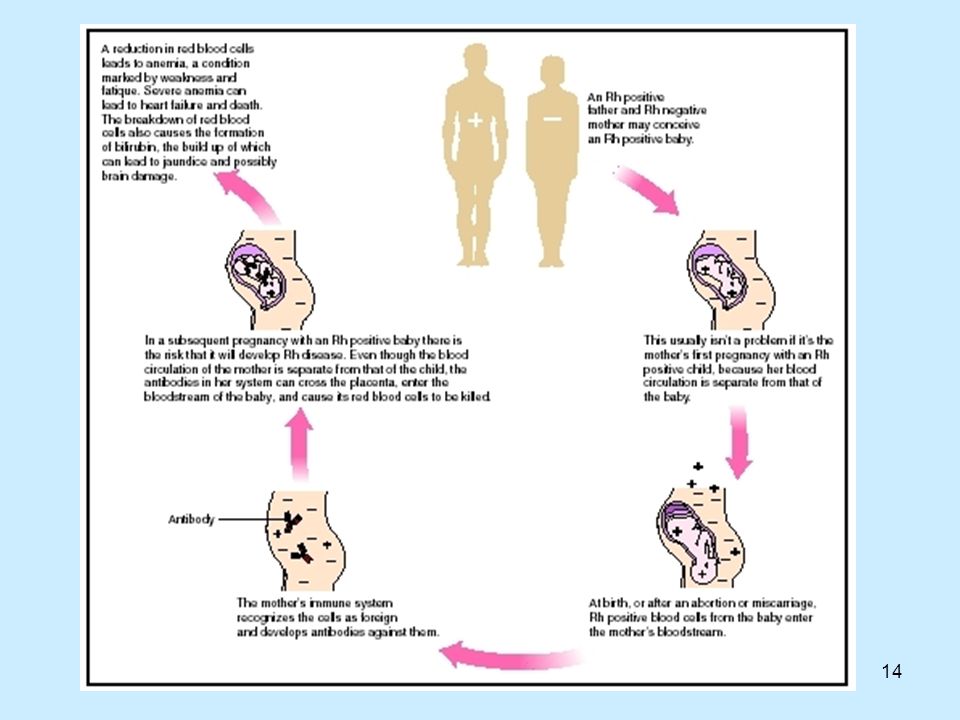
Page last reviewed: 16 November 2021
Next review due: 16 November 2024
What is Rhesus conflict? | Territory of femininity
Irma
Eagle
Rhesus conflict is an immune conflict that occurs during pregnancy between mother and fetus. If a woman has a positive Rh factor, she has nothing to fear. However, if the expectant mother has negative blood, during pregnancy she can learn from her own experience what the Rh conflict is.
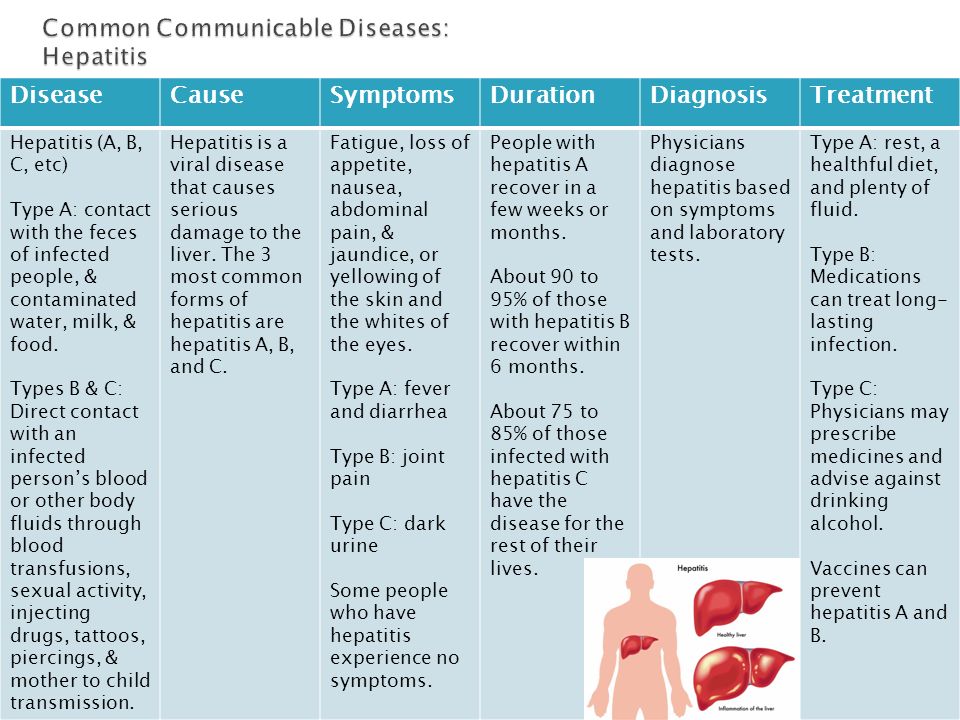
The cause of the Rh conflict is a specific protein (antigen) known as the "Rh factor" or "D factor". This antigen is found on the surface of erythrocytes (red blood cells), but not everyone has it. The blood of 85% of people contains the Rh factor, so they are considered Rh-positive. And the remaining 15% of this protein is not in the blood, so they are called Rh-negative. The absence of the Rh factor does not affect a person’s health or quality of life in any way (this is just an individual feature: the same as blue or brown eyes, straight or wavy hair).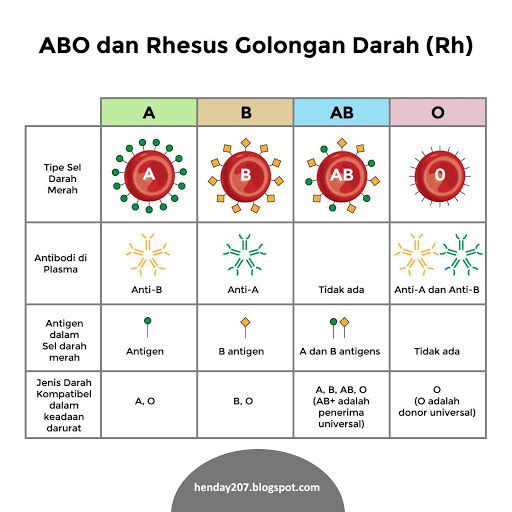 But sometimes this seemingly small thing is of great importance. Problems can arise in 2 cases: nine0003
But sometimes this seemingly small thing is of great importance. Problems can arise in 2 cases: nine0003
- An Rh-negative patient received a positive blood transfusion by mistake. If this is the first encounter with a foreign protein, the body will respond to its invasion by producing Rh antibodies, but perhaps everything will work out. If such a meeting turns out to be repeated, a state of shock will arise, accompanied by serious damage to the kidneys and liver.
- An Rh-negative woman is pregnant with an Rh-positive child, which means that there is a risk of conflict between the fetus and mother. nine0015
- First, the fetal blood does not mix with the mother's blood, which means that there are no provoking factors for the development of a Rh conflict. It is important to understand that this can happen with an “exemplary” pregnancy without any complications.
- The second option - erythrocytes (red blood cells) of the embryo enter the bloodstream of a pregnant woman. They begin to "stick together" the mother's blood. Therefore, in response to their appearance, the immune system produces antibodies. They are of two classes. During the first meeting with a positive Rh, the body forms IgM antibodies. Their size is very large, they are sluggish, so it is difficult for them to penetrate the placenta to the fetus. In this case, the probability of an Rhesus conflict is very small. nine0012
- The third option is that the woman has not had her first pregnancy or has had an erroneous positive blood transfusion in the past. The body is already familiar with the hostile protein, and upon receipt of even a small amount of Rh-positive blood, it will begin to produce another class of antibodies - IgG. They are smaller and more mobile than their predecessors, so they can easily overcome the placental barrier, enter the blood of the fetus and begin to destroy its red blood cells.
 If the destruction of blood cells is very active, there will be an Rh conflict between the fetus and mother. It leads to oxygen starvation of the tissues and organs of the child, as well as to circulatory and metabolic disorders. As a result of the conflict of blood rhesus, premature birth, miscarriage, as well as the development of hemolytic disease of the newborn are possible. nine0012
If the destruction of blood cells is very active, there will be an Rh conflict between the fetus and mother. It leads to oxygen starvation of the tissues and organs of the child, as well as to circulatory and metabolic disorders. As a result of the conflict of blood rhesus, premature birth, miscarriage, as well as the development of hemolytic disease of the newborn are possible. nine0012 - The edematous form (dropsy) is the most severe. It occurs very rarely - in 2% of cases of Rh-conflict. The edematous form usually occurs in babies born from 5 - 7 pregnancies of an Rh-negative mother. Children are born with pale integument and large body weight.
 They have severe edema (fluid in the chest, abdomen and other body cavities), enlarged liver and spleen. The condition of these newborns is very difficult. There is a high probability of death, so emergency medical attention is needed. nine0012
They have severe edema (fluid in the chest, abdomen and other body cavities), enlarged liver and spleen. The condition of these newborns is very difficult. There is a high probability of death, so emergency medical attention is needed. nine0012 - The icteric form proceeds more easily than the edematous form. Just like with the edematous form, the child is born with an enlarged liver and spleen. His red blood cells continue to die under the influence of maternal antibodies. As a result of their decay, a lot of bile pigment - bilirubin is formed. It should be neutralized by the liver, but it has not yet coped with this task. As a result, on the first day after birth, the child rapidly turns yellow. After 2 - 3 days, its yellowness reaches a peak. The skin becomes lemon or orange-yellow. Bilirubin is highly toxic in large quantities. At critically high concentrations, it affects brain cells and kidneys. Severe (!) jaundice can lead to the death of the child or, if he survives, to further physical and mental retardation in development.
 Therefore, in the first hours after birth, the baby needs to have a blood transfusion and start his treatment. nine0012
Therefore, in the first hours after birth, the baby needs to have a blood transfusion and start his treatment. nine0012 - Anemic form - the mildest. The blood counts deviate from the norm, but this does not pose a danger to his life.
- Causes of Rh conflict
- Mechanism of development of Rhesus conflict
- Rh incompatibility symptoms
- Diagnosis of Rhesus conflict
- Treatment of Rh conflict
- Prevention of Rh conflict
- Prices for treatment
What is the probability of conceiving a child with a negative Rh factor?
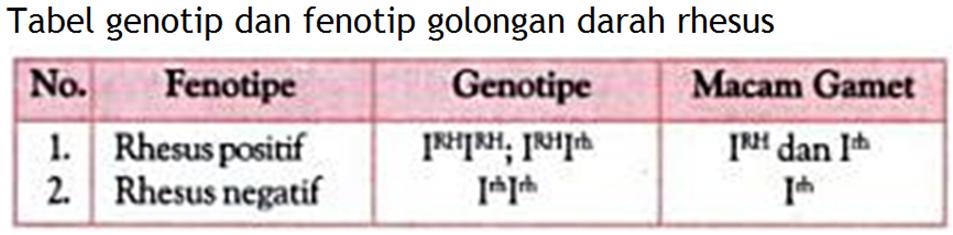
With the onset of pregnancy, an Rh-negative woman worries about what Rh factor her child has. If the father is negative, there is nothing to guess: the baby has the Rh of his parents. However, if the father is Rh positive, options are possible. Let's remember the basics of genetics.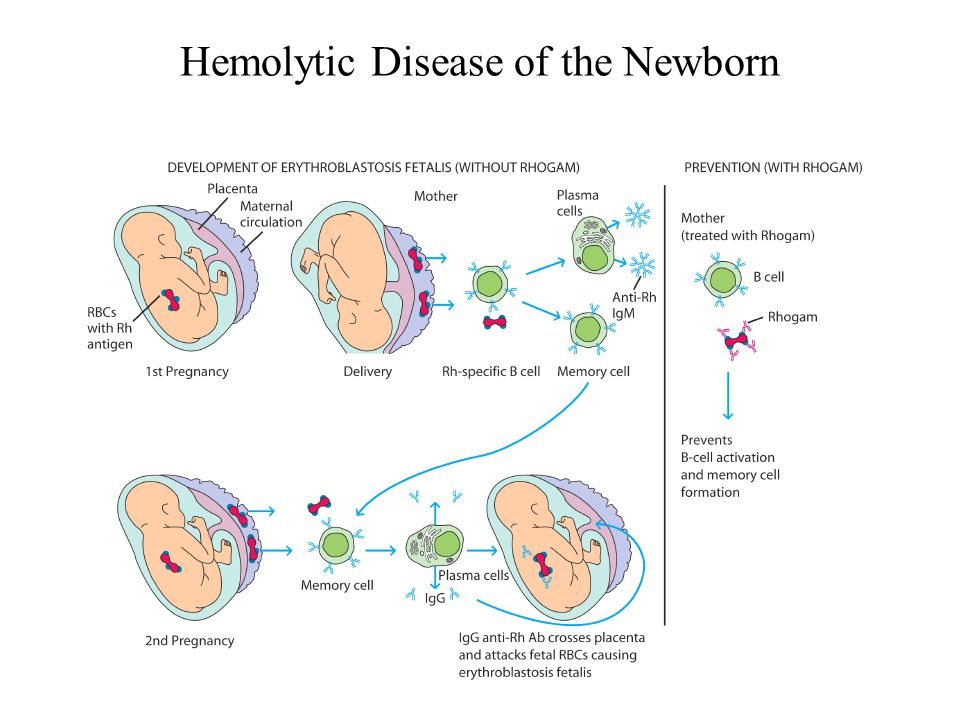
A positive Rh factor is a dominant (predominant, strong) sign. Negative Rh factor is recessive (weak). It is easily suppressed by the dominant one, but in alliance with the recessive "brother" it can be stronger. nine0003
If an Rh-negative woman gets pregnant by an Rh-positive man, in whose genes the Rh-negative gene is dormant, he can win. The probability of having an Rh-negative child in this case is 50%!
If the father's genotype does not have this "sleeping" gene, then with one hundred percent certainty it can be said that a child with a positive Rh factor will be conceived.
How will the pregnancy of an Rh-negative mother proceed if the child is Rh-positive? nine0017
Several variants of the course of pregnancy are possible.
What is hemolytic disease of the newborn?
Hemolytic disease of the newborn occurs in 20-25% of cases of conflict between the fetus and mother. This disease is accompanied by increased breakdown of red blood cells and poisoning of the body by their decay products. Hemolytic disease is always accompanied by anemia (anemia) and can occur in three forms:
How to prevent Rh conflict?
The more pregnancies (including those with subsequent termination of pregnancy and miscarriages) - the higher the risk of a conflict between the Rhesus of the fetus and the mother. Therefore, a girl who begins sexual activity and does not plan to give birth to a child, first of all, should think about protection. Reliable contraceptive effect (99%) can be achieved with combined oral contraceptives. Also, in case of unprotected sex and a high risk of pregnancy, you can use emergency contraception, for example, Levonorgestrel at a dosage of 1.5 mg. It is used within three days after sexual intercourse. The effectiveness of the drug reaches 95%. It is also possible to minimize possible problems associated with termination of pregnancy or miscarriages with the help of anti-Rhesus immunoglobulin. It is also recommended as a prevention of Rh conflict during pregnancy and after childbirth. nine0003
It is also recommended as a prevention of Rh conflict during pregnancy and after childbirth. nine0003
Topics:
health Rh factor Rhesus conflict blood rhesus conflict immune conflict pregnancy miscarriage anti-rhesus immunoglobulin
Rhesus conflict. What is Rhesus conflict?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0003
Rh-conflict - immunological incompatibility of the blood Rh factor of the Rh-negative mother and the Rh-positive fetus, characterized by sensitization of the mother's body. The cause of the Rh conflict is the transplacental penetration of fetal erythrocytes carrying a positive Rh factor into the bloodstream of an Rh-negative mother. Rhesus conflict can cause intrauterine fetal death, miscarriage, stillbirth and hemolytic disease of the newborn. nine0003
nine0003
General
Rh-conflict can occur in women with a negative Rh during pregnancy or during childbirth, if the child has inherited a positive father's Rh. The Rh factor (Rh) of human blood is a special lipoprotein (D-agglutinogen) in the Rh system, located on the surface of red blood cells. It is present in the blood of 85% of the human population who are Rh-positive Rh (+), and 15% of those without Rh factor belong to the Rh-negative Rh (-) group. nine0003
Rhesus conflict
Causes of Rh conflict
Isoimmunization and Rh-conflict are caused by the entry of Rh-incompatible blood of the child into the mother's bloodstream and largely depend on the outcome of the first pregnancy in Rh (-) women. Rhesus conflict during the first pregnancy is possible if a woman has previously had a blood transfusion without taking into account Rh compatibility. The occurrence of the Rhesus conflict is facilitated by previous abortions: artificial (abortions) and spontaneous (miscarriages). nine0003
Rhesus conflict during the first pregnancy is possible if a woman has previously had a blood transfusion without taking into account Rh compatibility. The occurrence of the Rhesus conflict is facilitated by previous abortions: artificial (abortions) and spontaneous (miscarriages). nine0003
The entry of the baby's umbilical cord blood into the mother's bloodstream often occurs during childbirth, making the mother's body susceptible to the Rh antigen and creating a risk of Rh conflict in the next pregnancy. The likelihood of isoimmunization increases with delivery by caesarean section. Bleeding during pregnancy or childbirth due to detachment or damage to the placenta, manual separation of the placenta can provoke the development of the Rhesus conflict.
After invasive prenatal diagnostic procedures (chorionic biopsy, cordocentesis or amniocentesis), Rh-sensitization of the mother's body is also possible. In a pregnant woman with Rh (-), suffering from preeclampsia, diabetes, who had influenza and acute respiratory infections, there may be a violation of the integrity of the chorionic villi and, as a result, activation of the synthesis of anti-Rh antibodies. The cause of the Rh-conflict can be a long-term intrauterine sensitization of the Rh (-) woman, which occurred at her birth from the Rh (+) mother (2% of cases). nine0003
The cause of the Rh-conflict can be a long-term intrauterine sensitization of the Rh (-) woman, which occurred at her birth from the Rh (+) mother (2% of cases). nine0003
Mechanism of Rhesus conflict development
The Rh factor is inherited as a dominant trait, therefore, in Rh (-) mother with homozygosity (DD) Rh (+) of the father, the child is always Rh (+), which is why the risk of Rh conflict is high. In the case of heterozygosity (Dd) of the father, the chances of having a child with a positive or negative Rh are the same.
The formation of fetal hematopoiesis begins from the 8th week of intrauterine development, at this time, fetal erythrocytes in a small amount can be detected in the mother's bloodstream. At the same time, the fetal Rh antigen is foreign to the mother's Rh (-) immune system and causes sensitization (isoimmunization) of the mother's body with the production of anti-Rhesus antibodies and the risk of Rh conflict.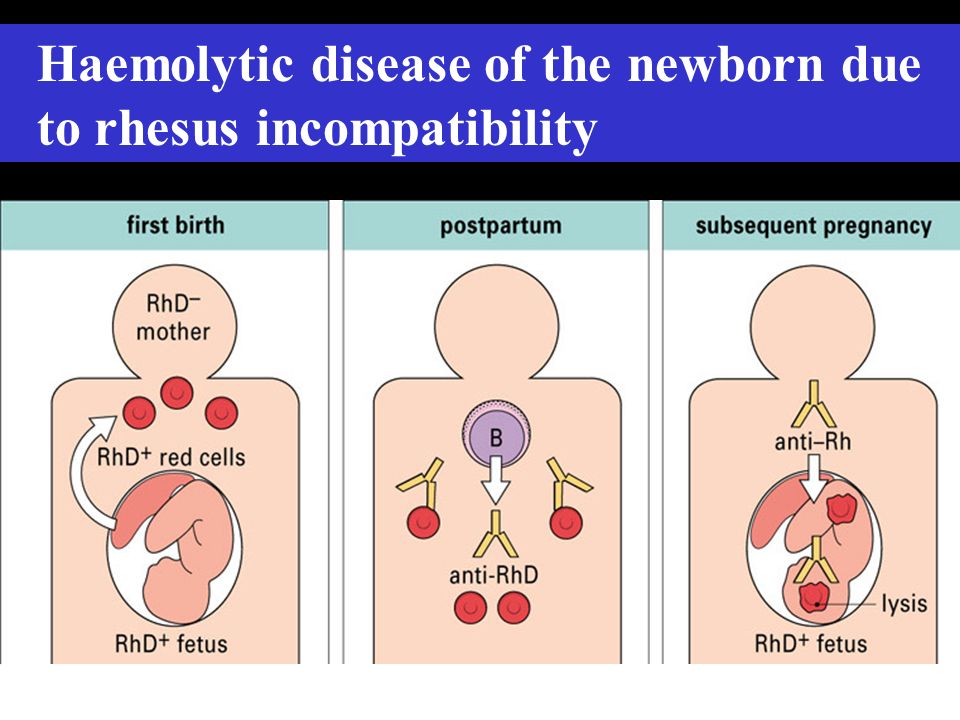 nine0003
nine0003
Rh (-) sensitization of a woman during her first pregnancy occurs in isolated cases and the chances of her bearing with an Rh conflict are quite high, since the antibodies (Ig M) formed in this case have a low concentration, poorly penetrate the placenta and do not pose a serious danger to the fetus.
The likelihood of isoimmunization during delivery is greater, which can lead to Rh conflict in subsequent pregnancies. This is due to the formation of a population of long-lived immune memory cells, and in the next pregnancy, upon repeated contact with even a small amount of Rh antigen (no more than 0.1 ml), a large number of specific antibodies (Ig G) are released. nine0003
Due to the small size of IgG, they are able to penetrate the bloodstream of the fetus through the hematoplacental barrier, cause intravascular hemolysis of Rh (+) erythrocytes of the child and inhibition of the hematopoiesis process. As a result of the Rhesus conflict, a severe, life-threatening condition for the unborn child develops - hemolytic disease of the fetus, characterized by anemia, hypoxia and acidosis.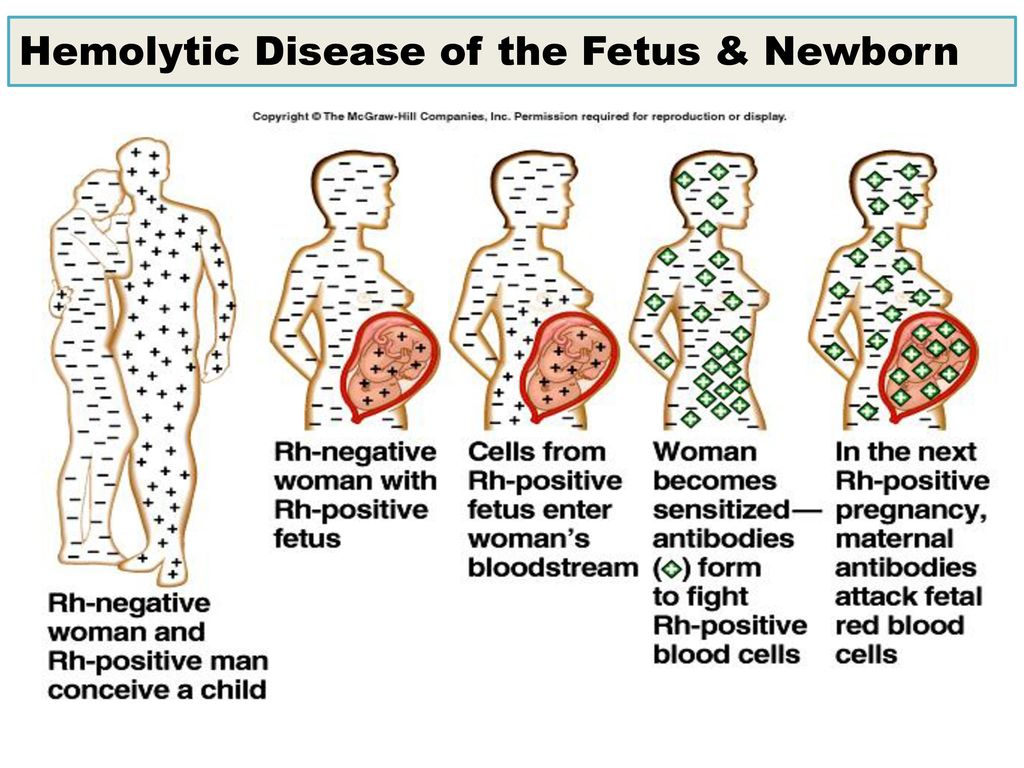 It is accompanied by damage and an excessive increase in organs: the liver, spleen, brain, heart and kidneys; toxic damage to the central nervous system of the child - "bilirubin encephalopathy". Without timely preventive measures taken, the Rh conflict can lead to intrauterine fetal death, spontaneous miscarriage, stillbirth, or the birth of a child with various forms of hemolytic disease. nine0003
It is accompanied by damage and an excessive increase in organs: the liver, spleen, brain, heart and kidneys; toxic damage to the central nervous system of the child - "bilirubin encephalopathy". Without timely preventive measures taken, the Rh conflict can lead to intrauterine fetal death, spontaneous miscarriage, stillbirth, or the birth of a child with various forms of hemolytic disease. nine0003
Rh symptoms
Rhesus conflict does not cause specific clinical manifestations in a pregnant woman, but is detected by the presence of antibodies to the Rh factor in her blood. Sometimes the Rhesus conflict can be accompanied by functional disorders similar to preeclampsia.
Rhesus conflict is manifested by the development of hemolytic disease of the fetus, which, at an early onset, can lead to intrauterine death from the 20th to the 30th week of pregnancy, miscarriage, stillbirth, premature birth, as well as the birth of a full-term baby with an anemic, icteric or edematous form of this disease.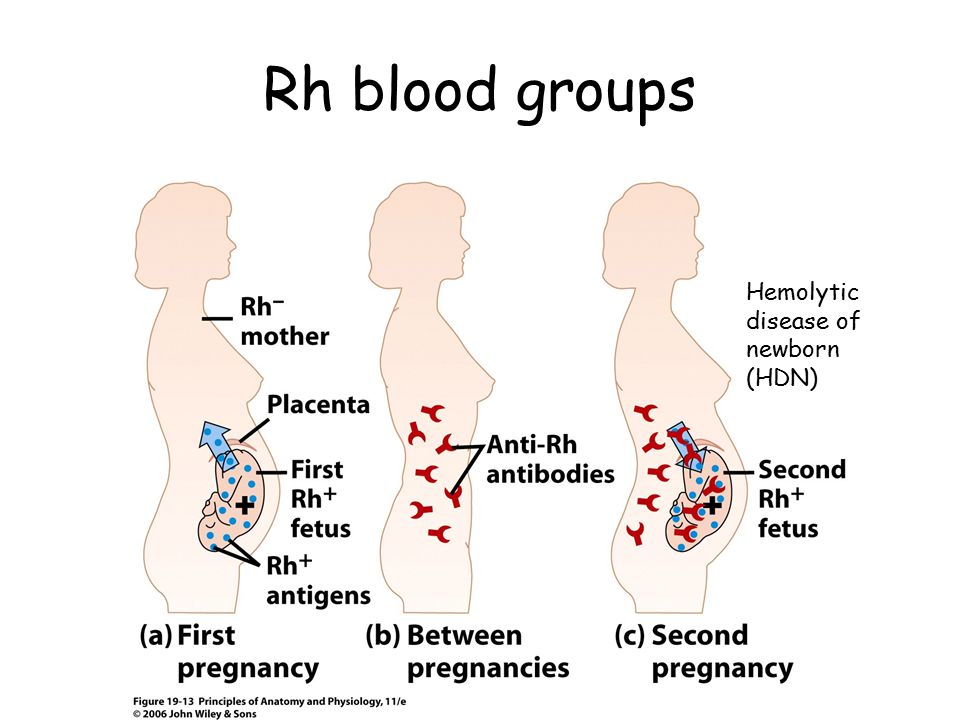 Common manifestations of Rh-conflict in the fetus are: anemia, the appearance of immature erythrocytes in the blood (reticulocytosis, erythroblastosis), hypoxic damage to important organs, hepato- and spelenomegaly. nine0003
Common manifestations of Rh-conflict in the fetus are: anemia, the appearance of immature erythrocytes in the blood (reticulocytosis, erythroblastosis), hypoxic damage to important organs, hepato- and spelenomegaly. nine0003
The severity of the manifestations of the Rh conflict can be determined by the amount of anti-Rh antibodies in the mother's blood and the degree of maturity of the child. An edematous form of hemolytic disease of the fetus can be extremely difficult with an Rhesus conflict - with an increase in the size of the organs; pronounced anemia, hypoalbuminemia; the appearance of edema, ascites; thickening of the placenta and an increase in the volume of amniotic fluid. With Rhesus conflict, fetal dropsy, edematous syndrome of the newborn, an increase in the weight of the child by almost 2 times can develop, which can lead to death. nine0003
A small degree of pathology is observed in the anemic form of hemolytic disease; the icteric form is expressed by icteric coloration of the skin, enlargement of the liver, spleen, heart and lymph nodes, hyperbilirubinemia.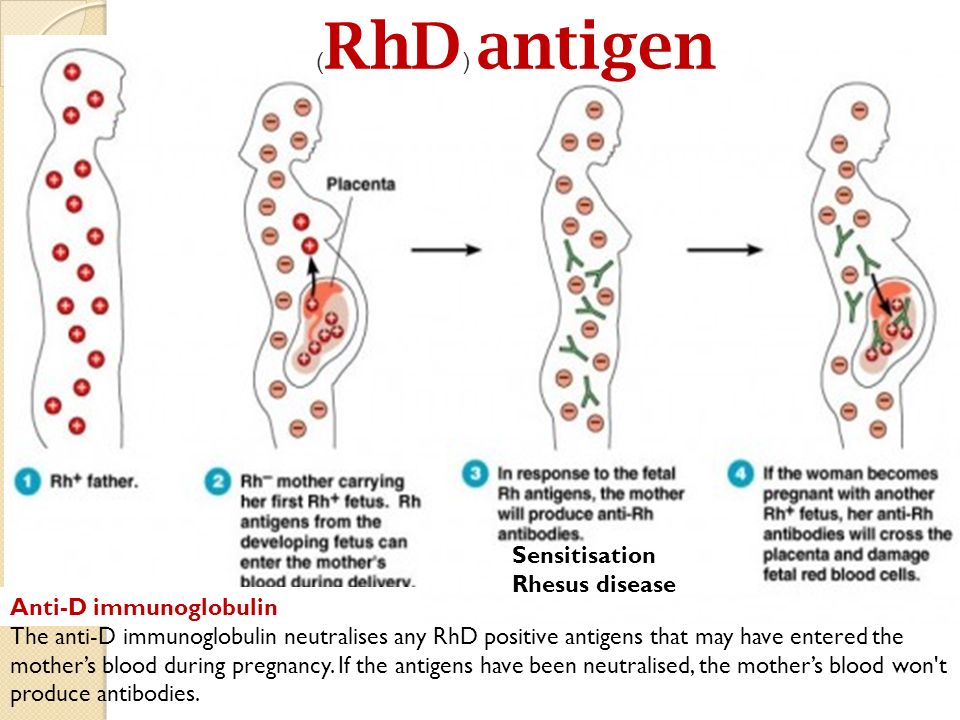 Bilirubin intoxication in Rhesus conflict causes damage to the central nervous system and is manifested by the lethargy of the child, poor appetite, frequent regurgitation, vomiting, reduced reflexes, convulsions, which can subsequently lead to a lag in his mental and mental development, hearing loss. nine0003
Bilirubin intoxication in Rhesus conflict causes damage to the central nervous system and is manifested by the lethargy of the child, poor appetite, frequent regurgitation, vomiting, reduced reflexes, convulsions, which can subsequently lead to a lag in his mental and mental development, hearing loss. nine0003
Diagnosis of Rhesus conflict
Diagnosis of Rh-conflict begins with determining the Rh-affiliation of a woman and her husband (preferably even before the onset of the first pregnancy or at its earliest possible date). If the future mother and father are both Rh negative, there is no need for further examination.
For the prediction of Rh-conflict in Rh (-) women, data on blood transfusions performed in the past without taking into account Rh-affiliation, previous pregnancies and their outcomes (the presence of spontaneous miscarriage, honeybort, intrauterine fetal death, the birth of a child with hemolytic disease) are important, which may indicate possible isoimmunization.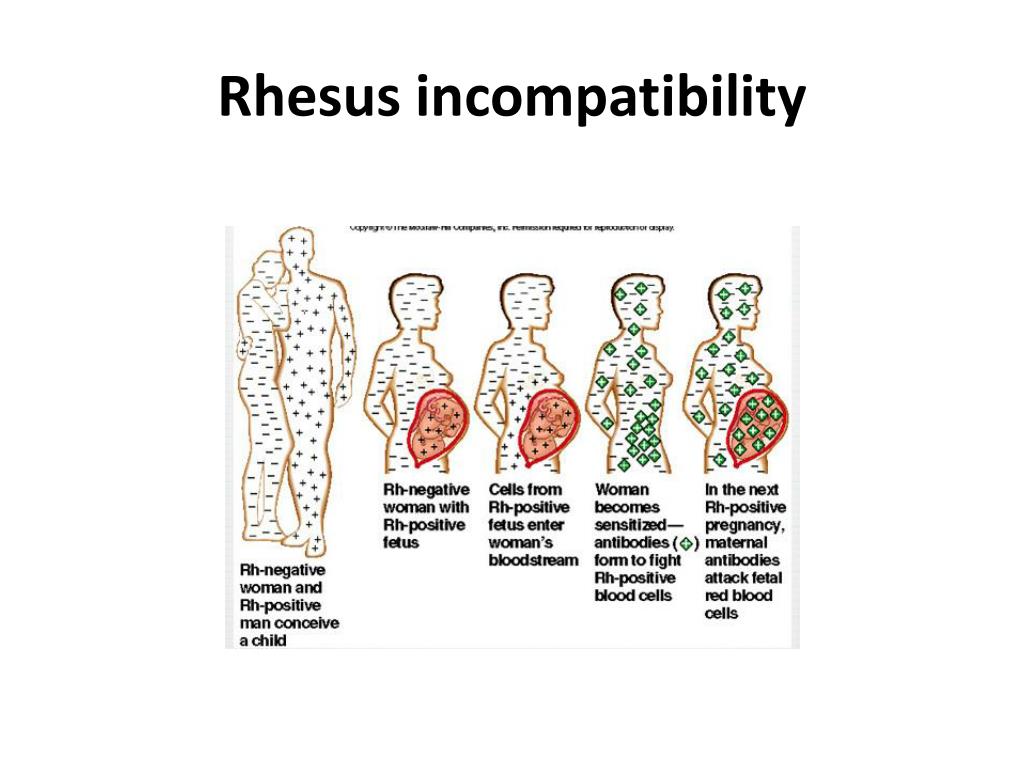 nine0003
nine0003
Diagnosis of the Rh conflict includes the determination of the titer and class of anti-Rh antibodies in the blood, which is carried out during the first pregnancy for women who are not sensitized for Rhesus - every 2 months; sensitized - up to 32 weeks of gestation every month, from 32-35 weeks - every 2 weeks, from 35 weeks - weekly. Since there is no direct relationship between the degree of damage to the fetus and the titer of anti-Rh antibodies, this analysis does not give an accurate idea of the state of the fetus in Rhesus conflict. nine0003
To monitor the condition of the fetus, an ultrasound examination is performed (4 times in the period from 20 to 36 weeks of pregnancy and immediately before childbirth), which makes it possible to observe the dynamics of its growth and development. In order to predict the Rh conflict, ultrasound evaluates the size of the placenta, the size of the fetal abdomen (including the liver and spleen), reveals the presence of polyhydramnios, ascites, and dilated veins of the umbilical cord.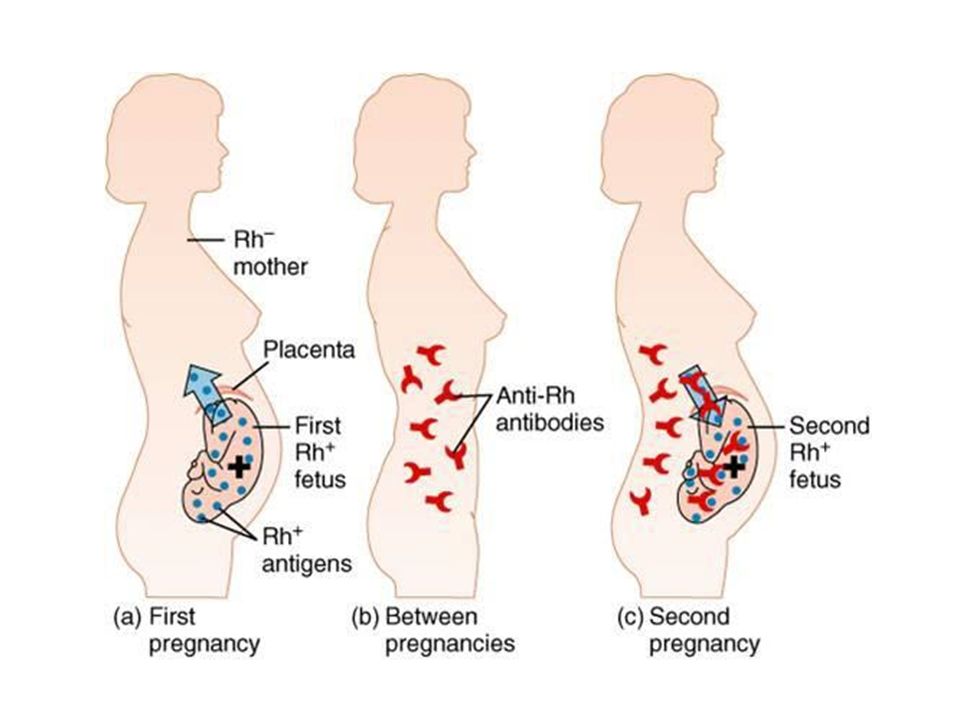
Conducting electrocardiography (ECG), fetal phonocardiography (FCG) and cardiotocography (CTG) allows the gynecologist who manages pregnancy to determine the degree of fetal hypoxia in Rh conflict. Important data are provided by prenatal diagnosis of Rhesus conflict using the methods of amniocentesis (examination of amniotic fluid) or cordocentesis (examination of umbilical cord blood) in dynamics under ultrasound control. Amniocentesis is carried out from 34 to 36 weeks of pregnancy: in the amniotic fluid, the titer of anti-Rh antibodies, the sex of the unborn child, the optical density of bilirubin, and the degree of maturity of the lungs of the fetus are determined. nine0003
Accurately determine the severity of anemia in Rhesus conflict allows cordocentesis, which helps to determine the blood type and Rh factor by the cord blood of the fetus; levels of hemoglobin, bilirubin, serum protein; hematocrit, reticulocyte count; antibodies fixed on fetal erythrocytes; blood gases.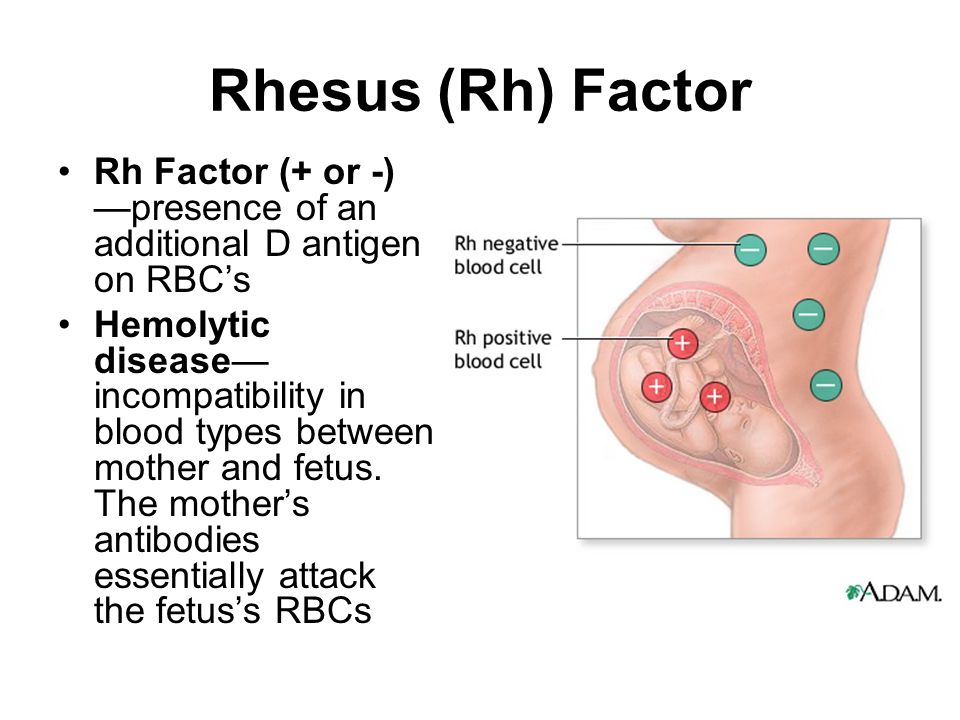
Treatment of Rh conflict
To alleviate the Rh conflict, all Rh (-) pregnant women at 10-12, 22-24 and 32-34 weeks of gestation are given courses of non-specific desensitizing therapy, including vitamins, metabolic agents, calcium and iron preparations, antihistamines, oxygen therapy. At a gestational age of more than 36 weeks, in the presence of Rh-sensitization of the mother and a satisfactory condition of the fetus, self-delivery is possible. nine0003
If a serious condition of the fetus is noted during the Rhesus conflict, a planned caesarean section is performed for a period of 37-38 weeks. If this is not possible, an intrauterine blood transfusion through the umbilical vein is performed under ultrasound control, which makes it possible to partially compensate for the effects of anemia and hypoxia and prolong the pregnancy.
With Rhesus conflict, it is possible to prescribe pregnant plasmapheresis in the second half of gestation in order to reduce the titer of antibodies to Rh (+) erythrocytes of the fetus in the mother's blood.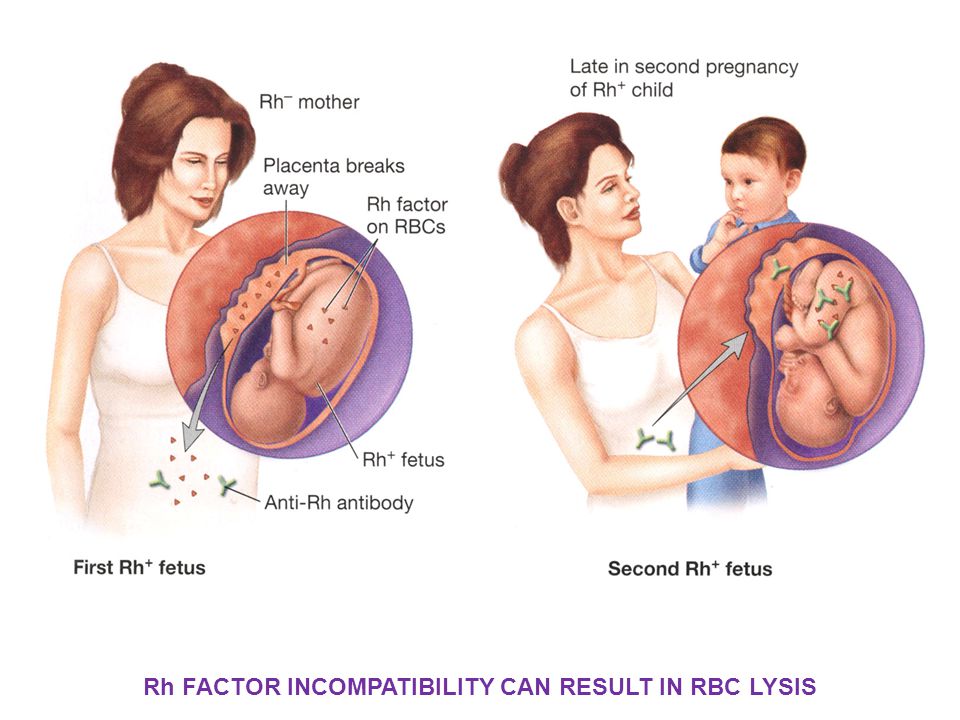 With a severe degree of hemolytic damage to the fetus, immediately after childbirth, the child undergoes a replacement transfusion of one-group Rh-negative blood or plasma or group I erythrocyte mass; begin treatment of hemolytic disease of the newborn. nine0003
With a severe degree of hemolytic damage to the fetus, immediately after childbirth, the child undergoes a replacement transfusion of one-group Rh-negative blood or plasma or group I erythrocyte mass; begin treatment of hemolytic disease of the newborn. nine0003
Within 2 weeks after birth, breastfeeding of a child with signs of hemolytic disease is not allowed, so as not to worsen the condition of the baby. If, with a Rh-conflict, the newborn does not have symptoms of this disease, then after an injection of anti-Rhesus immunoglobulin to the mother, breastfeeding is carried out without restrictions.
Prevention of Rh conflict
To avoid very serious consequences for a child with an Rh-incompatible pregnancy, the primary task in gynecology is to prevent the development of Rh-immunization and Rh-conflict. Of great importance for the prevention of Rh - conflict in Rh (-) women is taking into account Rh compatibility with a donor during blood transfusion, the obligatory preservation of the first pregnancy, and the absence of a history of abortions.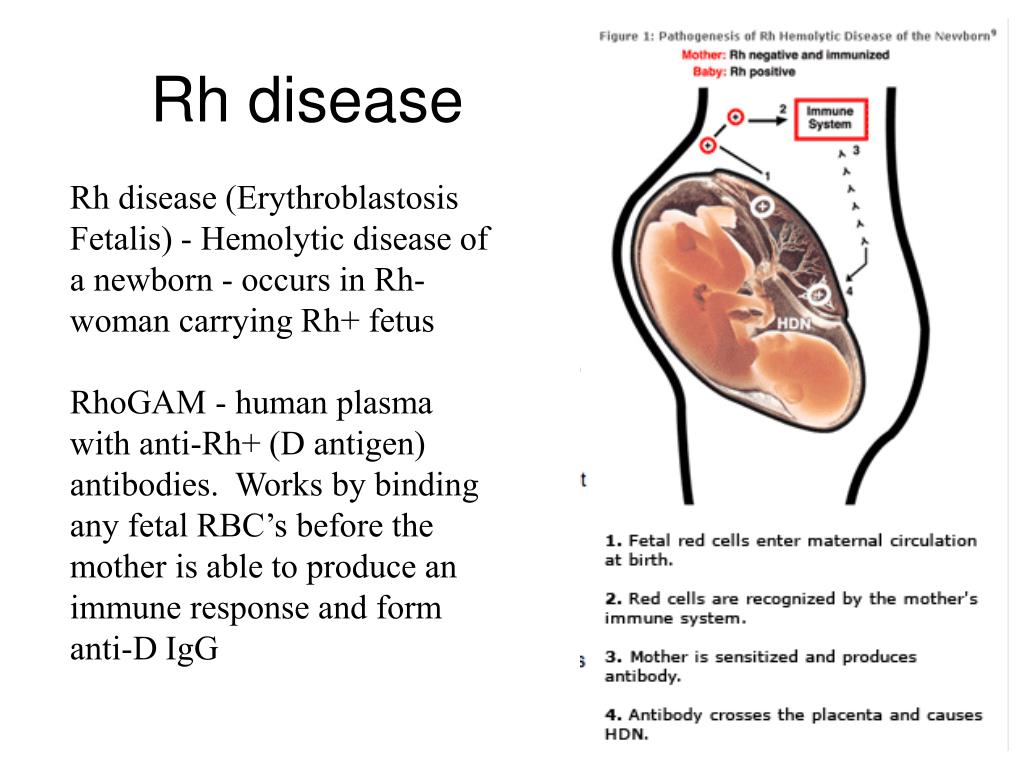 nine0003
nine0003
An important role in the prevention of Rh-conflict is played by pregnancy planning, with the examination of a woman for a blood group, Rh-factor, for the presence of anti-Rh antibodies in the blood. The risk of developing a Rh conflict and the presence of antibodies to Rh in a woman's blood is not a contraindication to pregnancy and a reason for its termination.
Specific prevention of Rh conflict is an intramuscular injection of anti-Rhesus immunoglobulin (RhoGAM) from donor blood, which is given to women with Rh (-) who are not sensitized to the Rh antigen. The drug destroys Rh (+) erythrocytes, which may have entered the woman's bloodstream, thereby preventing her isoimmunization and reducing the likelihood of Rh conflict. For the high effectiveness of the preventive action of RhoGAM, it is necessary to strictly observe the timing of the drug administration. nine0003
The introduction of anti-Rh immunoglobulin Rh (-) to women for the prevention of Rhesus conflict is carried out no later than 72 hours after transfusion of Rh (+) blood or platelet mass; artificial termination of pregnancy; spontaneous miscarriage, surgery associated with ectopic pregnancy.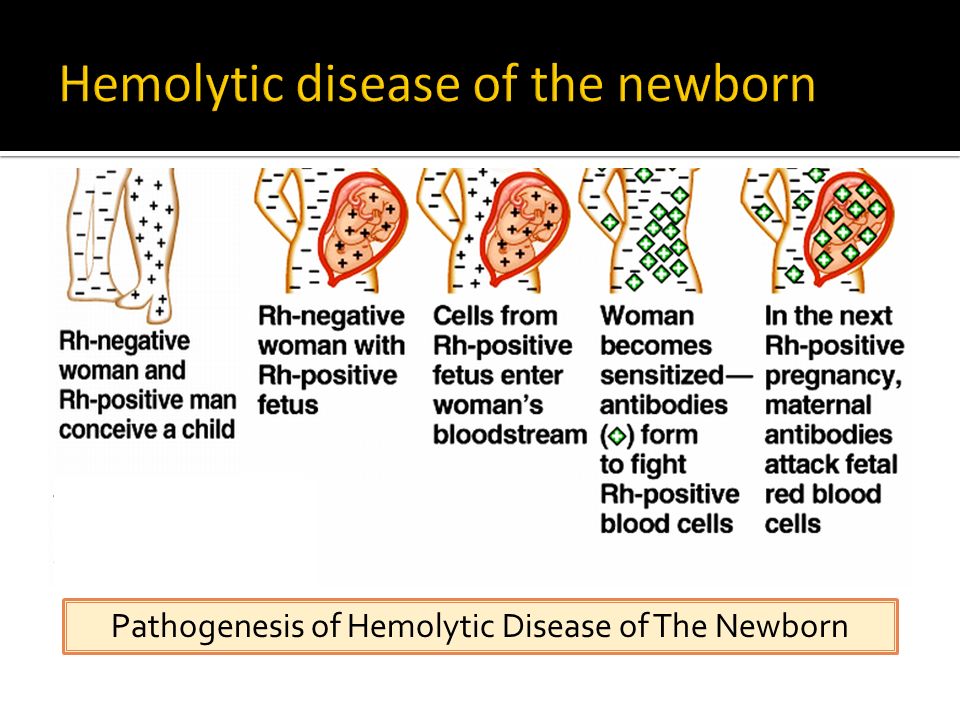 Anti-Rh immunoglobulin is prescribed to pregnant women at risk of Rhesus conflict at 28 weeks of gestation (sometimes again at 34 weeks) to prevent fetal hemolytic disease. If a pregnant woman with Rh (-) had bleeding (with placental abruption, abdominal trauma), invasive manipulations were performed with the risk of developing an Rh conflict, anti-Rhesus immunoglobulin is administered at the 7th month of gestation. nine0003
Anti-Rh immunoglobulin is prescribed to pregnant women at risk of Rhesus conflict at 28 weeks of gestation (sometimes again at 34 weeks) to prevent fetal hemolytic disease. If a pregnant woman with Rh (-) had bleeding (with placental abruption, abdominal trauma), invasive manipulations were performed with the risk of developing an Rh conflict, anti-Rhesus immunoglobulin is administered at the 7th month of gestation. nine0003
In the first 48 - 72 hours after delivery, in the case of the birth of a Rh (+) child and the absence of antibodies to Rh in the mother's blood, the injection of RhoGAM is repeated. This avoids Rh sensitization and Rh conflict in the next pregnancy. The effect of immunoglobulin lasts for several weeks, and with each subsequent pregnancy, if there is a chance of the birth of an Rh (+) child and the development of an Rh conflict, the drug must be administered again. For Rh (-) women already sensitized to the Rh antigen, RhoGAM is not effective. nine0003
You can share your medical history, what helped you in the treatment of Rhesus conflict.