Small white bumps that itch
Hives | Causes, Symptoms and Treatment
Hives are itchy red or white bumps on the skin. This itchy rash is also known as urticaria, or as nettle rash. In some cases this itchy rash is triggered by a physical stimulus. If this is the case, the condition is called inducible urticaria or physical urticaria. Examples of physical factors which can trigger hives include pressure, friction, sweating, cold, heat, sunlight and water. Treatments include avoiding the trigger (where possible), and antihistamines. Urticaria can be called acute (short-lived episode) or chronic (persisting).
What are hives?
Dr Sarah Jarvis MBEWhen you have hives (urticaria), you have an itchy rash caused by tiny amounts of fluid that leak from blood vessels just under the skin surface.
A trigger causes cells in the skin to release chemicals such as histamine. The chemicals cause fluid to leak from tiny blood vessels under the skin surface. The fluid pools to form weals. The chemicals also cause the blood vessels to open wide (dilate) which causes the flare around the weals. It is not known what the trigger is in about half of cases.
Some known triggers include:
- A physical stimulus. Where this is the case the condition is called inducible urticaria. In this type of hives, a rash appears when the skin is physically stimulated (for example, by heat, cold or pressure).
- Allergies - for example:
- Food allergies such as allergies to nuts, strawberries, citrus fruit, egg, food additives, spices, chocolate, or shellfish. Sometimes you can develop an allergy to a food even if you have eaten it without any problem many times before.
- Allergies to insect bites and stings.
- Allergies to medicines such as penicillin, aspirin, anti-inflammatory painkillers, etc.
- A viral infection such as a cold or flu can trigger an urticarial rash in some people. (You react to the virus.) A mild viral infection which causes few other symptoms is probably a common trigger of an urticarial rash that develops without an apparent cause.
- Skin contact with some substances causes a local area of contact hives in some people. For example, chemicals, latex, cosmetics, plants, ointments, nettle stings, etc.
Pine tree contact:
Contact urticaria
What can urticaria look like?
The inducible type of hives is triggered by a physical stimulus and can be either acute or chronic. Physical causes can result in repeated episodes of acute hives, or a persisting long-term condition.
Hives can be classed as follows:
- Acute - if it develops suddenly and lasts less than six weeks. Most cases last 24-48 hours. In some cases the rash only lasts a few hours. About 1 in 6 people will have at least one bout of hives in their lives. It can affect anyone at any age. Some people have recurring bouts of acute hives.
- Chronic - if it persists longer than six weeks. This is uncommon.
Hives can be triggered by a number of different physical causes. The reason why a rash appears in affected people is not clear. The physical stimulus somehow causes a release of histamine and other chemicals, which causes the rash.
The physical stimulus somehow causes a release of histamine and other chemicals, which causes the rash.
The main types of inducible urticaria include the following:
Dermatographism
Urticaria dermatographia
R1carver, CC BY-SA 3.0, via Wikimedia CommonsDermatographism (also known as dermographism and dermatographia) means skin writing. People with this condition develop the rash on areas of skin that have been firmly stroked. (Because of this, you could 'write' on someone's skin by applying firm pressure with a finger or other object. The rash follows the line of the writing on the skin.) The affected area of skin is usually very itchy but in some mild cases it does not itch much. Although any part of the skin can be affected, the palms, soles of the feet, genital skin and scalp are less commonly affected. Dermatographism is more prone to occur when you are hot. For example, it may develop more easily when you rub yourself firmly with a towel after a hot shower. The rash tends to last less than an hour. In many cases the pressure needed to be applied to cause the rash is quite firm. However, some people develop dermatographism with just light pressure.
The rash tends to last less than an hour. In many cases the pressure needed to be applied to cause the rash is quite firm. However, some people develop dermatographism with just light pressure.
Up to 1 in 20 people will develop dermatographism at some stage of life. It most commonly first develops in early adult life. In most cases, the condition tends to improve gradually over a few years and it goes or becomes less severe. However, in some cases the condition remains troublesome for many years.
Cholinergic hives
Cholinergic hives are quite common. The condition is caused by sweating and is sometimes called heat bumps. The hives rash is quite distinct as the weals are very small (2-3 mm) with a red flare around each one. The rash appears within a few minutes of sweating and tends to be worst on the chest, back and arms. The rash lasts from 30 minutes to an hour or more before fading away. Some people become slightly wheezy and short of breath for the duration of the rash.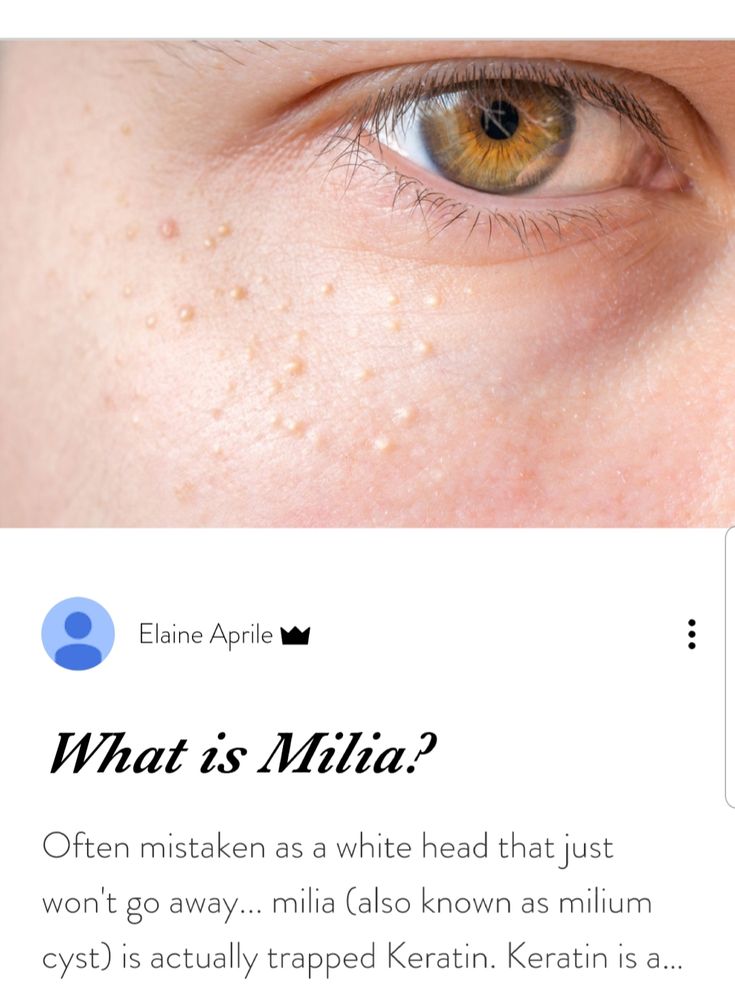
The sweating that triggers the rash may be due to exercise, heat, high temperature (fever), emotion or eating spicy food. It can be a real nuisance when trying to exercise. In severe cases, hundreds of tiny weals develop when you run or do other types of exercise. Sometimes the tiny weals join together to form larger ones. Cholinergic hives most commonly first develop in early adult life. In many cases the condition tends to improve after a few years and it goes or becomes less severe. However, in some cases the condition remains troublesome for many years.
Cold hives
Cold hives are quite an uncommon condition. An urticarial rash develops after being exposed to cold, including rain, cold winds and cold water. It may be the cold that triggers the rash, or the re-warming of the skin after coming in from the cold. The rash affects the chilled parts of the skin. If a large area of skin has been chilled, the rash can be very extensive. For example, swimming in cold water may cause a widespread and severe rash over most of the body that can make you dizzy and faint.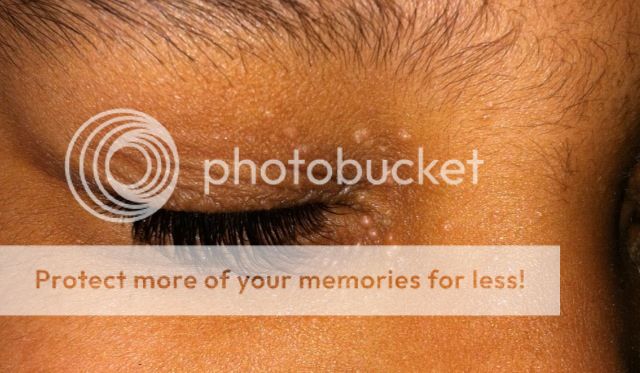 (For this reason, if you are known to develop cold hives, you should never go swimming alone.)
(For this reason, if you are known to develop cold hives, you should never go swimming alone.)
Delayed pressure hives
Delayed pressure hives are uncommon. The condition can develop alone but it commonly affects people who also have chronic hives. In this type of hives the rash develops 4-6 hours after the affected area of skin has had deep prolonged pressure applied. For example, after wearing a tight seatbelt, or wearing a tight watch strap, or after gripping a tool such as a screwdriver for a reasonable period of time. The rash can be painful and tends to last several hours, or even a day or so.
Solar hives
This is a rare condition in which an urticarial rash develops on skin exposed to sunlight.
Water contact (aquagenic) hives
In this rare condition, an urticarial rash develops on skin exposed to water of any temperature.
Vibratory hives
In this rare condition, the rash comes up after using vibrating tools.
What are the symptoms?
An itchy rash is the main symptom of hives (urticaria). The rash can affect any area of skin. Small raised areas called weals develop on the skin. The weals look like mild blisters and are itchy. Each weal is white or red and is usually surrounded by a small red area of skin which is called a flare. The weals are commonly 1-2 cm across but can vary in size. There may be just a few but sometimes many develop over various parts of the body. Sometimes weals that are next to each other join together to form larger ones. The weals can be any shape but are often round.
The rash can affect any area of skin. Small raised areas called weals develop on the skin. The weals look like mild blisters and are itchy. Each weal is white or red and is usually surrounded by a small red area of skin which is called a flare. The weals are commonly 1-2 cm across but can vary in size. There may be just a few but sometimes many develop over various parts of the body. Sometimes weals that are next to each other join together to form larger ones. The weals can be any shape but are often round.
As a weal fades, the surrounding flare remains for a while. This makes the affected area of skin look blotchy and red. The blotches then fade gradually and the skin returns to normal. Each weal usually lasts less than 24 hours. However, as some fade away, others may appear. It can then seem as if the rash is moving around the body. The rash may clear completely only to return a few hours or days later.
- Most people with acute hives do not feel ill; however, the appearance of the rash and the itch can be troublesome.

- In some cases a condition called angio-oedema develops at the same time as hives. In this condition some fluid also leaks into deeper tissues under the skin, which causes the tissues to swell. See separate leaflet called Angio-oedema for more details:
- The swelling of angio-oedema can occur anywhere in the body but most commonly affects the eyelids, lips and genitals.
- Sometimes the tongue and throat are affected and become swollen. The swelling sometimes becomes bad enough to cause difficulty breathing.
- Symptoms of angio-oedema tend to last longer than urticarial weals. It may take up to three days for the swollen areas to subside and go.
- A variation called vasculitic hives occurs in a small number of cases. In this condition the weals last more than 24 hours, they are often painful, may become dark red and may leave a red mark on the skin when the weal goes. Technically, this type of rash is not urticaria.
Are any tests needed?
Usually no tests are needed. The rash is very typical and is easily recognised as hives by doctors. In many cases you will know what caused the rash from the events leading up to it. For example if you have just been put on a new medicine, or if your skin came into contact with a nettle, or if you were stung by a bee.
The rash is very typical and is easily recognised as hives by doctors. In many cases you will know what caused the rash from the events leading up to it. For example if you have just been put on a new medicine, or if your skin came into contact with a nettle, or if you were stung by a bee.
A symptom diary
A symptom diary may be helpful in working out if there is a specific trigger or cause. If your diary shows you only develop the rash on days when you eat a certain food, for example, it may be obvious what the cause is. A diary might also show if the rash relates to stress, exercise or sunlight. It may help rule out certain causes.
Skin-prick allergy tests
In some cases if it appears to be related to an allergy, tests such as skin-prick allergy tests may be helpful. Tiny quantities of substances which might cause an allergy are placed on your skin in a special order. If the skin reacts, you may be allergic to that substance.
Blood tests
In other cases, blood tests for allergy may be useful. In some people, blood tests may help to point to a cause. These may be general blood tests, or blood tests to look for specific proteins produced by your immune system, called autoantibodies. Where these are found, it is likely that it is your own immune system over-reacting which is causing the rash.
In some people, blood tests may help to point to a cause. These may be general blood tests, or blood tests to look for specific proteins produced by your immune system, called autoantibodies. Where these are found, it is likely that it is your own immune system over-reacting which is causing the rash.
Exclusion tests
In some people, 'exclusion' or 'challenge' tests may be needed. For example, testing to see if cold or pressure always causes the rash, or excluding certain foods from the diet to see if that stops the rash from coming back.
Biopsy
Occasionally, if urticarial vasculitis is suspected, a sample of the skin may be taken (a skin biopsy) for further analysis.
Hives treatment
Often no treatment is necessary, as the rash commonly goes within 24-48 hours. A cool bath or shower may ease the itch. Calamine lotion or menthol 1% in aqueous cream can help with itching, although if it is left on for too long the itch may come back. These can be bought without a prescription.
Once you know what causes the rash, it may be possible to avoid situations that trigger it. For example, dermatographism can often be prevented by avoiding firm pressure against the skin as much as possible. In mild cases, no additional treatment may be needed.
Various other factors may make symptoms worse (but are not the main trigger). The following are tips that some people have found helpful; however, there is little proof that they work in everybody:
- Try avoiding tight clothes if weals occur at sites of local pressure. For example, under belts, under tight-fitting shoes, etc.
- Try keeping cool, as hives may tend to flare up in warmer conditions. In particular, keep the bedroom cool at night.
- For some people alcohol, hot baths, strong sunlight, and emotion make symptoms worse. If you think any of these are making symptoms worse then it may be helpful to try to avoid them.
- See a doctor if you think a medicine is making symptoms worse, as a change in medication may be an option.
 Some medicines that may be triggers include aspirin, anti-inflammatory painkillers, and angiotensin-converting enzyme (ACE) inhibitors.
Some medicines that may be triggers include aspirin, anti-inflammatory painkillers, and angiotensin-converting enzyme (ACE) inhibitors.
Antihistamines
Many types of hives are helped by taking antihistamine medicines. (However, these medicines may not help some cases of delayed pressure hives.) Antihistamines block the action of histamine which is involved in causing hives. The most commonly used antihistamines for hives are cetirizine, fexofenadine and loratadine. These do not usually cause drowsiness. Your doctor may advise doses which are higher than the usual recommended dose in order to control the rash. If the itch is making it difficult to sleep, sometimes an antihistamine which makes you sleepy can also be taken at night. Examples of antihistamines used in this way include chlorphenamine or hydroxyzine.
Antihistamines can be bought over the counter, without a prescription. However, if you need to take them for more than a few days, or on a regular basis, it is best to see your doctor for further advice. Do not take more than the recommended dose without discussing it with your doctor. Antihistamines are not usually advised in pregnancy.
Do not take more than the recommended dose without discussing it with your doctor. Antihistamines are not usually advised in pregnancy.
Some people take antihistamines now and then when a rash flares up. If you take an antihistamine as soon as the rash appears, the rash tends to fade more quickly than it would do normally. If the rash recurs frequently then your doctor may advise a regular dose of an antihistamine to prevent the rash from occurring. If you have cholinergic urticaria and know that you get a rash on exercise, a dose of an antihistamine just before you do exercise may help to prevent or limit a flare-up of the rash.
Steroid tablets
Unlike most other types of hives, those caused by a physical stimulus are not usually helped by steroids. Occasionally for severe flare-ups of hives, a course of prednisolone tablets taken for a week may be helpful.
Other treatments
If you have a severe episode of hives then you may be referred to a specialist.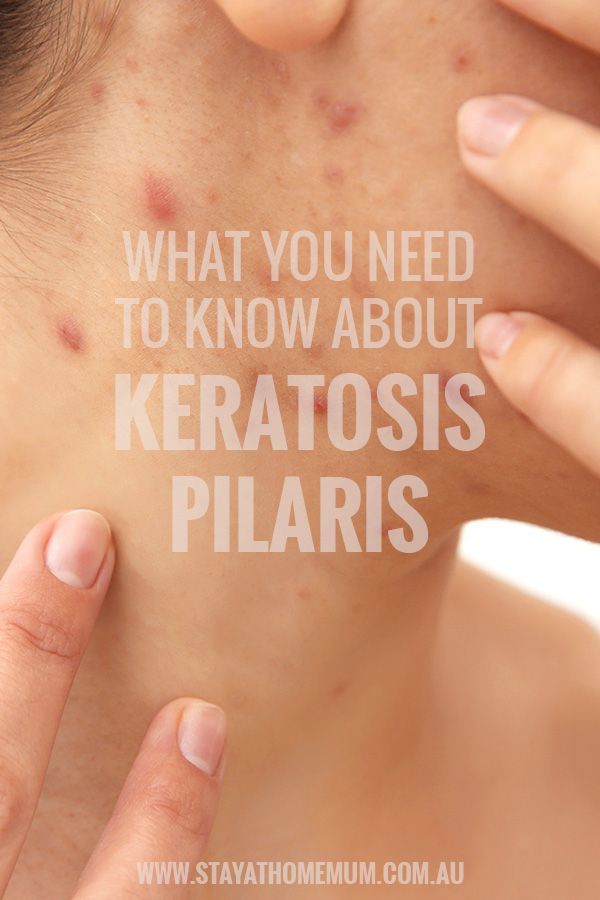 Skin specialists (called dermatologists) or allergy specialists (called immunologists) may be able to help. In particular, if angio-oedema or anaphylaxis occurred at the same time, you would be referred or admitted to hospital. This is to reverse the reaction quickly. It is also to confirm the diagnosis and, where possible, to identify a cause. For example, if a nut allergy is suspected to have caused a severe episode then this can confirmed by tests. You may then be given advice on how to avoid the cause and on what to do if it should occur again.
Skin specialists (called dermatologists) or allergy specialists (called immunologists) may be able to help. In particular, if angio-oedema or anaphylaxis occurred at the same time, you would be referred or admitted to hospital. This is to reverse the reaction quickly. It is also to confirm the diagnosis and, where possible, to identify a cause. For example, if a nut allergy is suspected to have caused a severe episode then this can confirmed by tests. You may then be given advice on how to avoid the cause and on what to do if it should occur again.
Occasionally other treatments may be used, such as a tablet called montelukast, which is usually used for asthma. This may be particularly useful in delayed pressure urticaria, where antihistamines often do not help. Omalizumab is a newer medication which acts against autoantibodies produced by the body's own immune system. It has to be given by injection once a month. This has been shown to be effective for some types of inducible urticaria in some studies. In the UK the National Institute for Health and Care Excellence (NICE) so far has not recommended its use for this particular type of hives.
In the UK the National Institute for Health and Care Excellence (NICE) so far has not recommended its use for this particular type of hives.
Treatment with ultraviolet light (phototherapy) can cause an improvement in symptoms but, unfortunately, this may only last for a few months.
Are hives serious?
Usually not. The rash is itchy but normally fades within a day or so and causes no harm. Most people with hives (acute urticaria) do not feel too unwell unless they have a cold or flu that is triggering the rash. The cause of the rash is not known in more than half of cases and it is commonly a one-off event.
However, hives may be more serious in the following situations:
- Food allergy. If a food allergy is the cause then the rash is likely to return each time you eat the particular food. This is more often a nuisance than serious.
- Severe allergies. People who have a severe allergic reaction to peanuts, insect stings, etc, often have an urticarial rash as one of the symptoms.
 This is in addition to other symptoms such as severe angio-oedema, breathing difficulties, collapse, etc. A severe allergic reaction is called anaphylaxis. Note: most people with acute urticaria feel well and do not have anaphylaxis.
This is in addition to other symptoms such as severe angio-oedema, breathing difficulties, collapse, etc. A severe allergic reaction is called anaphylaxis. Note: most people with acute urticaria feel well and do not have anaphylaxis.
What is the outlook?
Inducible urticaria most commonly occurs in healthy young adults. You can have two or more different types of hives at the same time. As a rule, hives triggered by physical stimuli tend to improve and become less troublesome with time (often going, or being much less troublesome, after 2-5 years).
Acute hives usually last less than six weeks. Most cases last 24-48 hours and in some cases the rash only lasts a few hours.
Persistent hives tend to come and go. You may have times when the rash appears on most days, and then times when the rash may go away for a while. The severity of the rash and itch varies from person to person. Some things such as heat, cold, menstrual periods, stress, or emotion may make the rash flare up worse than usual.
- Symptoms may go away completely after a few months; however, the condition lasts several years in some cases.
- In about half of cases, symptoms go within 3-5 years after the condition first starts.
- In about 1 in 5 cases the symptoms persist on and off for more than 10 years.
Pictures, Types, Causes, and Treatment
Raised skin bumps are mostly harmless. They may present in various ways, from skin tags to keloids. Conditions like acne and chickenpox can also cause them. Seek medical help if your bumps resemble those caused by MRSA or skin cancer.
Raised skin bumps are very common, and in most cases, they’re harmless. They can result from a number of conditions, including:
- infections
- allergic reactions
- skin disorders
- skin cancer
Skin bumps can vary in appearance and number depending on the cause. They may be the same color as your skin or a different color. They may be itchy, large, or small. Some can be hard, while others can feel soft and movable.
Some can be hard, while others can feel soft and movable.
Most skin bumps do not need treatment. However, you should speak with a doctor if your bumps are causing discomfort. You should also call a doctor if you’re concerned about any changes in your bumps or in the overall condition of your skin.
Many conditions can cause raised bumps to appear on the skin. Here’s a list of 25 possible causes.
Warning: Graphic images ahead.
Acne
- commonly located on the face, neck, shoulders, chest, and upper back
- breakouts on the skin composed of blackheads, whiteheads, pimples, or deep, painful cysts and nodules
- may leave scars or darken the skin if untreated
Read the full article on acne.
Cold sore
- red, painful, fluid-filled blister that appears near the mouth and lips
- affected area will often tingle or burn before the sore is visible
- may be accompanied by mild, flu-like symptoms, such as low fever, body aches, and swollen lymph nodes
Read the full article on cold sores.
Corns and calluses
- small, round circles of thickened skin with a painful, horn-like central area of hardened tissue
- commonly found on the tops and sides of the toes and on the soles of the feet
- caused by friction and pressure
Read the full article on corns and calluses.
Skin tags
- skin growths that can become up to half an inch long
- same color as your skin or slightly darker
- most likely caused by friction
- commonly found near the neck, armpits, breasts, groin, stomach, or eyelids
Read the full article on skin tags.
Nodule
- small to medium growth that may be filled with tissue, fluid, or both
- usually wider than a pimple and may look like a firm, smooth elevation under the skin
- usually harmless, but may cause discomfort if it presses on other structures
- nodules may also be located deep inside the body where you cannot see or feel them
Read the full article on nodules.
Impetigo
- common in babies and children
- irritating rash and fluid-filled blisters that pop easily and form a honey-colored crust
- rash is often located in the area around the mouth, chin, and nose
Read the full article on impetigo.
Molluscum contagiosum
- bumps that may appear in a patch of up to 20
- small, shiny, and smooth
- flesh-colored, white, or pink
- firm and dome-shaped with a dent or dimple in the middle
Read the full article on molluscum contagiosum.
Lipoma
- soft to the touch and moves easily if prodded with your finger
- small, just under the skin, and pale or colorless
- commonly located in the neck, back, or shoulders
- only painful if it presses on a nerve
Read the full article on lipoma.
Cyst
- slow-growing bump under the skin that has a smooth surface
- can be large or small and is usually painless
- typically not a problem unless it’s infected, very large, or growing in a sensitive area
- some grow deep inside your body where you can’t see or feel them
Read the full article on cysts.
Wart
- caused by many different types of a virus called human papillomavirus (HPV)
- may be found on the skin or mucous membranes
- may occur as one wart or in groups
- contagious and may be passed to others
Read the full article on warts.
Actinic keratosis
- typically less than 2 centimeters (cm), or about the size of a pencil eraser
- thick, scaly, or crusty skin patch
- appears on parts of the body that receive a lot of sun exposure (hands, arms, face, scalp, and neck)
- usually pink in color but can have a brown, tan, or gray base
Read the full article on actinic keratosis.
Basal cell carcinoma
- raised, firm, and pale areas that may resemble a scar
- dome-like, pink or red, shiny, and pearly areas that may have a sunk-in center, like a crater
- visible blood vessels on the growth
- easy bleeding or oozing wound that doesn’t seem to heal, or heals and then reappears
Read the full article on basal cell carcinoma.
Squamous cell carcinoma
- often occurs in areas exposed to ultraviolet (UV) radiation, such as the face, ears, and back of the hands
- scaly, reddish patch of skin that progresses to a raised bump and continues to grow
- growth that bleeds easily and doesn’t heal, or heals and then reappears
Read the full article on squamous cell carcinoma.
Melanoma
- the most serious form of skin cancer, more common in people with lighter skin tones
- mole anywhere on the body that has irregularly shaped edges, asymmetrical shape, and multiple colors
- mole that has changed color or gotten bigger over time
- usually larger than a pencil eraser
Read the full article on melanoma.
Boils
- bacterial or fungal infection of a hair follicle or oil gland
- can appear anywhere on the body but are most common on the face, neck, armpit, and buttock
- red, painful, raised bump with a yellow or white center
- may rupture and weep fluid
Read the full article on boils.
Bullae
- clear, watery, fluid-filled blister that is greater than 1 cm in size
- can be caused by friction, contact dermatitis, and other skin disorders
- if clear liquid turns milky, there might be an infection
Read the full article on bullae.
Contact dermatitis
- appears hours to days after contact with an allergen
- rash has visible borders and appears where your skin touched the irritating substance
- skin is itchy, red, scaly, or raw
- blisters that weep, ooze, or become crusty
Read the full article on contact dermatitis.
Cherry angioma
- common skin growth that can be found anywhere on the body but is most likely to be seen on the torso, arms, legs, and shoulders
- more common in people over age 30
- small, bright red circular or oval spots that may be raised or smooth and bleed if rubbed or scratched
- generally harmless but may require removal if they’re in problem areas
Read the full article on cherry angioma.
Keloids
- symptoms occur at the site of a previous injury
- lumpy or rigid area of skin that may be painful or itchy
- area is flesh-colored, pink, or red
Read the full article on keloids.
Keratosis pilaris
- common skin condition that’s most often seen on the arms and legs but might also occur on the face, buttocks, and torso
- often clears up on its own by age 30
- patches of skin that appear bumpy, slightly red, and feel rough
- may get worse in dry weather
Read the full article on keratosis pilaris.
Seborrheic keratoses
- common, harmless skin growth that is usually seen in older adults
- can be located anywhere on the body except for the palms of the hands and soles of the feet
- round, oval, dark-colored growth with a “stuck-on” appearance
- raised and bumpy with a waxy feel
Read the full article on seborrheic keratoses.
Chickenpox
- clusters of itchy, red, fluid-filled blisters in various stages of healing all over the body
- accompanied by fever, body aches, sore throat, and loss of appetite
- remains contagious until all blisters have crusted over
Read the full article on chickenpox.
MRSA (staph) infection
This condition is considered a medical emergency. Urgent care may be required.
- an infection caused by a type of Staphylococcus, or staph, bacteria that is resistant to many different antibiotics
- causes an infection when it enters through a cut or scrape on the skin
- skin infection that often looks like a spider bite, with a painful, raised, red pimple that may drain pus
- needs to be treated with powerful antibiotics and can lead to more dangerous conditions like cellulitis or blood infection
Read the full article on MRSA (staph) infection.
Scabies
- symptoms may take 4 to 6 weeks to appear
- extremely itchy rash that may be pimply, made up of tiny blisters, or scaly
- raised white or flesh-colored lines
Read the full article on scabies.
Strawberry nevus
- red or purplish raised mark, commonly located on the face, scalp, back, or chest
- appears at birth or in very young children
- gradually gets smaller or disappears as the child ages
Read the full article on strawberry nevus.
The most common causes of raised skin bumps are harmless and do not require medical treatment unless you have discomfort. Here are some of the possible reasons for raised skin bumps:
- Acne is the most common skin condition in the United States, according to the American Academy of Dermatology. It causes skin bumps that can range from very small and painless to large and painful. The bumps are usually accompanied by redness and swelling.
- Boils are infected hair follicles that look like red, raised bumps on the skin. They can be painful, but they eventually go away once they burst and release fluid.
- Bullae are raised, fluid-filled bumps that can result from friction, or conditions like contact dermatitis and chickenpox.
- Cherry angiomas are common skin growths that can form on most areas of the body. They develop when blood vessels clump together and create a raised, bright-red bump under or on the skin.

- Cold sores are red, fluid-filled bumps that form around the mouth or other areas of the face and can burst. They’re caused by a common virus called herpes simplex.
- Contact dermatitis is an allergic skin reaction that produces an itchy, red skin rash. The rash may consist of raised, red bumps that ooze, drain, or crust.
- Corns or calluses are rough, thickened areas of skin. They’re most often found on the feet and hands.
- Cysts are growths that contain fluid, air, or other substances. They develop under the skin in any part of the body. They feel like a small ball and can usually be moved around slightly.
- Keloids are smooth, raised growths that form around scars. They’re most commonly found on the chest, shoulders, and cheeks.
- Keratosis pilaris is a skin condition marked by an overgrowth of a protein called keratin. It causes small bumps around hair follicles on the body.

- Lipomas are collections of fatty tissue under the skin and are often painless. They usually form on the neck, back, or shoulders.
- Molluscum contagiosum are small, flesh-colored bumps with a dimple in the center that often form in all parts of the body. They can arise from skin-to-skin contact with someone affected with them.
- Nodules result from growth of abnormal tissue, and can appear on the skin in common areas like the armpits, groin, and head and neck region.
- Seborrheic keratoses are round, rough spots on the surface of the skin. They can affect many areas of the body, including the chest, shoulders, and back. They may be skin-colored, brown, or black.
- Skin tags are small, fleshy flaps of skin. They usually grow on the neck or in the armpits. They may be the same color as the skin or slightly darker.
- Strawberry nevus is a red birthmark also known as a hemangioma.
 They are most common in young children and usually disappear by age 10.
They are most common in young children and usually disappear by age 10. - Warts are raised, rough bumps caused by the human papillomavirus (HPV). They typically develop on the hands and feet. They may be skin-colored, pink, or slightly brown.
Less commonly, raised skin bumps are caused by more serious conditions that require treatment. Certain bacterial and viral infections cause bumps and will only get worse if they go undiagnosed and untreated. These serious conditions include:
- chickenpox, a common childhood virus characterized by red, itchy bumps that form all over the body
- impetigo, a bacterial skin infection common in young children that is highly contagious and results in reddish blisters that ooze and develop a honey-colored crust
- MRSA (staph) infection, an illness triggered by a staph bacteria that commonly lives on the skin, causing a swollen, painful bump with a white center
- scabies, a skin infestation caused by a tiny mite called Sarcoptes scabiei, producing an itchy, pimple-like rash
Other types of raised skin bumps can be caused by skin cancer. There are several types of skin cancer, all requiring medical management and treatment:
There are several types of skin cancer, all requiring medical management and treatment:
- Actinic keratosis is a precancerous skin condition characterized by scaly, crusty spots on areas of sun-exposed skin, such as hands, arms, or face. These spots are typically brown, gray, or pink. The affected area may itch or burn.
- Basal cell carcinoma is a form of cancer that affects the top layer of skin. It produces painful bumps that bleed in the early stages. The associated bumps appear on sun-exposed skin and may be discolored, shiny, or scar-like.
- Squamous cell carcinoma is a type of skin cancer that begins in the squamous cells. These cells make up the outermost layer of skin. The condition causes scaly, red patches and raised sores to develop on the skin. These abnormal growths often form in areas exposed to ultraviolet radiation.
- Melanoma is the least common but most serious form of skin cancer.
 It begins as an atypical mole. Cancerous moles are often asymmetrical, multi-colored, and large, with irregular borders. They can appear anywhere on the body.
It begins as an atypical mole. Cancerous moles are often asymmetrical, multi-colored, and large, with irregular borders. They can appear anywhere on the body.
Most skin bumps are harmless and aren’t cause for concern. However, you should see your doctor if:
- skin bumps change or worsen in appearance, or last for a long time
- you are in pain or they cause discomfort
- you don’t know the cause of the bumps
- you suspect you have an infection or skin cancer
Your doctor will perform a physical examination and inspect the skin bumps. Expect to answer questions about your bumps, medical history, and lifestyle habits.
Your doctor may also perform a skin biopsy to test if the skin bump is cancerous. This procedure involves taking a small sample of skin tissue from the affected area for analysis. Depending on the results, your doctor may refer you to a dermatologist or other specialist for further evaluation.
The Healthline FindCare tool can provide options in your area if you don’t already have a doctor.
Removal
Treatment for raised skin bumps depends on the underlying cause. Most of the common causes of skin bumps are harmless, so you probably won’t need treatment. However, if your skin bumps are bothering you, you might be able to have them removed for cosmetic reasons.
For example, a dermatologist can remove skin tags or warts by freezing them off. A dermatologist can also surgically remove certain skin bumps, including cysts and lipomas. Other bumps that are itchy or irritated may be treated with topical ointments and creams.
If your doctor finds that your skin bumps are cancerous or precancerous, they will most likely remove the bumps completely. You will also need to attend regular follow-up appointments so your doctor can check the area and make sure the cancer doesn’t come back.
Medication
In cases where additional medical treatment is required, your doctor will prescribe medications that can help eliminate your skin bumps and the underlying cause.
For a bacterial infection, such as MRSA, you may need antibiotics. For a viral infection, such as chickenpox, your doctor may recommend over-the-counter medications and home treatments. Some viral infections, such as herpes, can’t be cured. However, your doctor can give you medications to ease symptoms.
For most skin bumps, the long-term outlook is excellent. The majority of bumps are caused by harmless, temporary conditions that don’t require treatment. If skin bumps are caused by an infection or long-term condition, timely medical treatment should either clear it up or effectively ease the symptoms. The outlook is also good when skin cancer is caught early. However, frequent follow-ups will be necessary to ensure the cancer doesn’t return or grow. The outlook for more advanced forms of skin cancer varies with each situation.
Where does the rash on the body come from and what to do about it
July 2, 2020 Likbez Health
Sometimes just waiting is enough.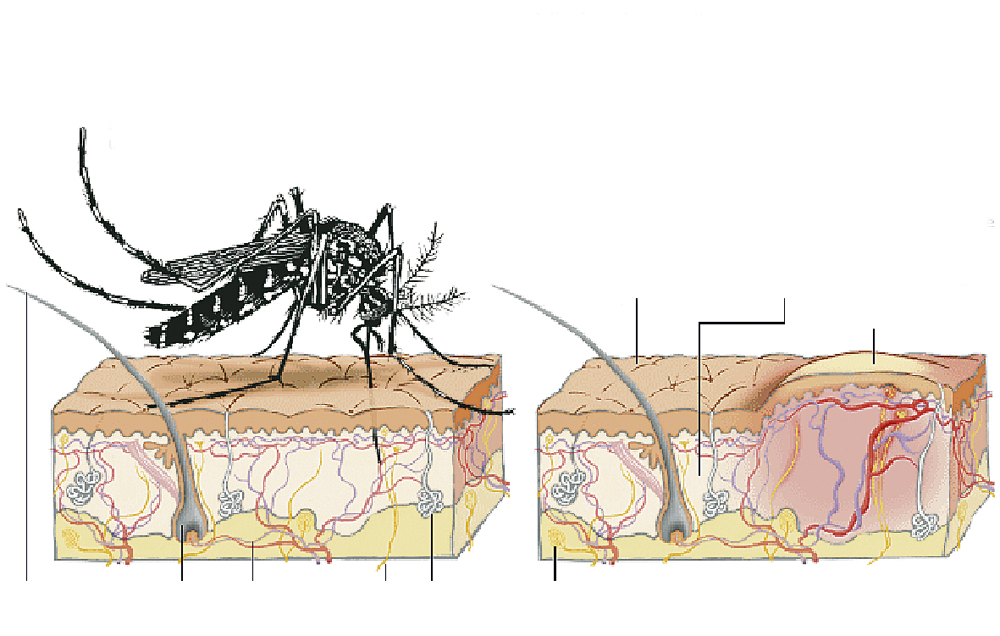
Body rash is common. Most often, it does not harm health: small red spots, pimples, bubbles spoil the appearance, itch, but quickly disappear by themselves.
However, sometimes rashes can be symptoms of serious and even life-threatening disorders.
When to see a doctor urgently
See your GP, dermatologist, nearest emergency room as soon as possible, or call an ambulance if:
- The rash has spread all over your body.
- Rash accompanied by fever. A temperature above 38.3 °C indicates an acute inflammatory process.
- The rash on the body appeared suddenly and is getting thicker. This may be a sign of a powerful allergic reaction that risks developing into Quincke's edema or even anaphylactic shock. Be especially careful if the rash appears on the face and neck. If you notice that it is becoming difficult to breathe, immediately dial 103 or 112.
- The rash is blistering. That is, in place of numerous red spots, bubbles filled with liquid begin to appear.

- The rash is painful to touch.
- The rash on the body is very itchy and you easily scratch it until it bleeds. In this case, there is a risk of introducing an infection into the wounds and getting blood poisoning.
If there are no threatening symptoms, exhale. Most likely, nothing bad is happening to you.
Now reading 🔥
- What to do if the temperature persists at 37 °C
What are the causes of a rash on the body
It is often difficult to immediately determine where the rashes come from. Here are some of the more common options.
Insect bites
Open image
Close
A mosquito bite or, say, a bee bite is easy to identify: in its place there is a rounded dense swelling that itches or hurts. You can’t confuse such damage to the skin with a rash. But there are insects whose bites look like rashes. These are, for example, fleas - bed or sandy. nine0003
If you find itchy red dots on your skin in the morning or after the beach, you may have been bitten.
Photoallergy
Open image
Close
It is also an allergic reaction to ultraviolet light (“sun poisoning”). The rash can be different:
- small itchy redness;
- flesh-coloured pimples that feel like sandpaper;
- blisters;
- patches of a distinct red color tending to merge into a single whole. nine0016
Most often, an allergy to the sun occurs due to the fact that during tanning, some harmful substance was present on the skin - cream, lotion, medicine, plant juice - and ultraviolet turned it into an allergen. Alternatively, you may be taking medication that has made your skin sensitive to the sun.
Contact dermatitis
View image
Close
Occurs when some toxic substance (allergen) comes into contact with the skin and the epidermis reacts with irritation and rashes in response. Allergens are often:
- Sap or pollen from certain plants, such as poison ivy or nettle.
 A skin reaction to nettle pollen is so common that the characteristic skin rash is called hives.
A skin reaction to nettle pollen is so common that the characteristic skin rash is called hives. - Latex.
- Certain metals that may be found in jewelry, hair clips, key rings. Most often, allergies occur on nickel, cobalt, chromium, copper.
- Various cosmetic products, from creams to eau de toilette.
- Dyes in cheap clothes. nine0016
Drug Allergy
View Image
Close
Rashes and itching can be side effects of certain medications, such as antibiotics. If you have recently started taking a new medicine, check the package leaflet. At the same time, check if there is any mention that the drug has a photosensitizing (that is, increasing sensitivity to sunlight) effect.
Hay fever
View image
Close
He is also allergic to pollen. This variant can be suspected if the rash appeared against the background of other signs of an allergic reaction:
- runny nose;
- watery eyes;
- compulsive coughing or sneezing.

Food allergy
View picture
Close
May manifest itself as hives that appear on different parts of the body, and scarlet rashes on the cheeks (this symptom is more typical for young children). nine0003
The most common food allergens are:
- eggs;
- milk;
- peanuts and tree nuts;
- fish and crustaceans;
- wheat;
- soy.
Skin infections
Rash may appear due to bacteria, fungi, viruses attacking the epidermis.
For example, with ringworm, round, itchy patches with a bright border appear. This fungal infection, contrary to stereotypes, can attack not only the scalp, but also any other part of the skin. nine0003
Open image
Close
An example of a viral infection is molluscum contagiosum. This disease makes itself felt by raised reddish-brown and, importantly, hard bumps with a diameter of 1-5 mm, which can appear on any part of the body. Despite the name, no shellfish lives under the skin. This is the skin's reaction to the virus.
This is the skin's reaction to the virus.
View image
Close
What to do if you have a rash on your body
The symptoms that require you to see a doctor as soon as possible are described above. If you do not have them, you can try to cope with the rash at home. nine0003
- Keep your skin clean. In the morning, evening, and as it gets dirty, gently wash it with warm water and a mild, unscented soap. Until the rash goes away, stop using hard washcloths and brushes.
- Wear soft, breathable clothing. Irritated skin needs to breathe.
- Monitor the humidity in the room where you are. The optimal value is 40–60%.
- Avoid foods that are potential allergens.
- If you develop a rash after you start using a new product, stop using it for a while. And monitor your condition. nine0016
- Moisturize your skin. This will reduce itching and help the epidermis recover faster. It is best to apply moisturizers immediately after a shower or bath.
 Use only hypoallergenic creams, lotions or gels.
Use only hypoallergenic creams, lotions or gels.
If itching is so severe that you cannot forget it, consult a dermatologist or a general practitioner. Your doctor will recommend antihistamines or over-the-counter ointments to help reduce discomfort.
You should also consult a doctor if the rash does not improve after a day or two or seems unusual, inexplicable, or worrisome. The doctor will make an accurate diagnosis and prescribe the most effective treatment. nine0003
Read also 🧐
- What is eczema, what it is and how to treat it
- Where do back pimples come from and how to get rid of them
- What is scarlet fever, how to recognize and treat it?0016
Causes and treatment of itching in pimples
Most instructions on how to get rid of pimples start with the simple rule of keeping your hands away from your face
160521
Share with friends
- Vkontakte
- Odnoklassniki
It seems like a simple rule, but, unfortunately, it is not easy to control this habit. Especially if the skin is irritated and the pimples itch. nine0003
Especially if the skin is irritated and the pimples itch. nine0003
Let's talk about why this happens and how to protect the face from the appearance of new inflamed acne.
Normal reaction
to irritation
Redness and swelling of the skin at the site of a pimple is the result of the immune system fighting bacteria that actively multiply in the sebaceous hair follicle in acne. The body tries to get rid of them by increasing blood flow to clogged pores. The purpose of this reaction is to deliver leukocytes to the damaged area as soon as possible and suppress the activity of pathogenic bacteria. This is how red pimples form, which itch and cause a slight tingling sensation. nine0003
If acne does not cause constant discomfort, but only periodically reminds of itself with a slight itch, this is a normal reaction to the inflammatory process.
The correct tactic in such cases is not to injure the skin, especially with sharp nails, and try not to touch the face, since even slight pressure on the skin can provoke an increase and spread of the inflammatory process. The best thing to do is to let the skin deal with the problem on its own. Then there is a high probability that acne will pass without a trace, leaving no dark spots and scars. nine0003
The best thing to do is to let the skin deal with the problem on its own. Then there is a high probability that acne will pass without a trace, leaving no dark spots and scars. nine0003
Signs that you should definitely see a doctor
- rash shortly after eating certain foods or medicines;
- fever and general malaise simultaneously with the appearance of numerous small pimples that itch;
- severe reddening of the skin, burning sensation and blistering; nine0015 rapid spread of the rash over a large area of the skin.
Redness and itching are symptoms that are not unique to the inflammatory elements of acne. They can be signs of a severe allergic reaction and some skin conditions (such as dermatitis or eczema).
If the redness does not look like the usual pimples on the face or body, the skin itches and this causes severe discomfort, you need to see a doctor - it's not worth the risk of trying to relieve irritation at home. nine0003
nine0003
How to prevent
pimples that itch?
Do not panic
If a new itchy pimple appears on your face, do not try to get rid of it immediately. Sharp actions only injure the skin. In most cases, it is enough to take a deep breath and wait a couple of minutes for the itching to go away along with the annoying desire to scratch your face.
Do not save on vitamins
Complex vitamins with a high content of zinc, copper, iron stimulate the renewal of skin cells and inhibit the formation of comedones. Vitamins A and E in capsules will help speed up the recovery of injured skin (the beneficial properties of vitamin E are enhanced with the simultaneous intake of selenium)
Avoid tanning
Ultraviolet rays damage the layer of the epidermis where new skin cells grow and mature. The renewal processes slow down, the skin itches, the exfoliating scales of the stratum corneum clog the ducts of the sebaceous hair follicles.
To avoid this, make it a rule to use cosmetics with SPF and moisturize your skin daily.
What to do if pimples have already appeared?
First of all, don't get upset and stay calm. In a state of stress, we touch our face more often, small pimples itch, and irritation only intensifies. nine0003
Complex therapy, including topical application of antibacterial drugs, for example, Zerkalin® lotion solution (1% solution of the antibiotic clindamycin), will help to solve the problem.
Zerkalin® has an antibacterial effect - inhibits the activity of pathogenic microorganisms in the sebaceous hair follicle. The lotion solution eliminates the causes of inflammation that causes redness and itching of acne.
The alcohol base of Zerkalin® facilitates the deep penetration of the active substance into the skin and additionally "dries out" the inflammatory elements of acne. nine0003
To achieve the best result, it is important to act according to the plan: apply the drug 2 times a day (morning and evening) for 6-8 weeks. The lotion solution is applied to dry, clean skin.