Toe cramps during pregnancy
Foot Or Leg Cramps While Pregnant? Here’s What You Should Know – My FootDr
Book nowPosted on by Emma Taylor
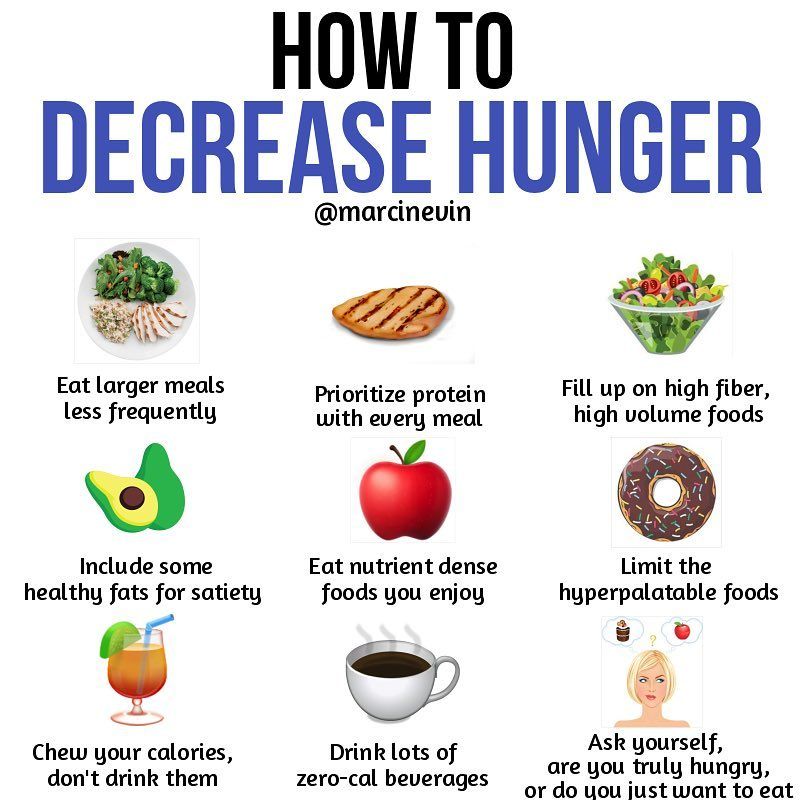
We’re all familiar with the sudden, painful and involuntary tightening of the muscles in our feet or legs known as a cramp, and in pregnancy, cramps often become even more common, affecting over 50% of women during the second and third trimesters. But what are cramps, why does pregnancy bring them on, and is there anything that can be done to help with cramps? Today, our podiatrists are talking all about foot and leg cramps in pregnancy.
What Are Cramps And What Causes Them?
A cramp is a sudden and often intense muscle contraction that occurs outside of your control. Cramps can affect entire muscle groups, individual muscles, or specific muscle fibers. Cramps feel uncomfortable, and can quickly become painful. Cramps can last from seconds to many minutes, can occur during the day or night (though they tend to be reported more frequently at night), and can affect a range of muscles from those in the the feet that cause your toes to scrunch, to those in the calves.
When it comes to the cause of cramps, it is one of those tricky topics where the exact causes haven’t been fully understood or identified in the research, and the causes seem to be very dependent on a person’s circumstances – from the medical conditions or pathologies a person may have, to their exercise habits and frequencies, to a range of other circumstances. Circumstances that are thought to lead to cramps in general include:,
- Heat-related cramps during exercise, where large losses of sweat and electrolytes are believed to lead to cramping
- Age, where approximately 37% of those aged over 60 years experience occasional night cramps
- General exercise-related cramps, where fatigue and excess strain on the feet and legs may cause them to cramp
- Having conditions such as diabetes, fibromyalgia or cirrhosis
- Venous insufficiency and peripheral vascular disease
- Cancer treatment
- Cardiovascular disease
- Neurologic deficits including peripheral neuropathy
- Osteoarthritis
Foot and leg injuries may have a similar effect to exercise-related cramps and fatigue, where changes to a person’s gait as a result of injury may result in fatigue in underused muscles, contributing to the development of cramps.
Why Do We Get More Foot And Leg Cramps When Pregnant?
In pregnancy, the increased incidence in cramps is thought to be related to the added weight, increased blood volume and potential swelling, all placing more pressure on your feet as well as compressing the blood vessels or nerves, which results in a greater likelihood of cramping. Other suggested reasons for cramps include the influx of pregnancy hormones circulating through your body, changes to your metabolism, having a vitamin deficiency, being too active or not being active enough.
Can Foot And Leg Cramps Be Prevented?
Researchers can’t confirm whether foot cramps can definitely be prevented, but there have been a number of methods suggested to help prevent foot and leg cramps, both in pregnancy and in general life.
- Given that swelling and compression are thought to be linked to foot cramps in pregnancy, keeping the feet elevated when you’re resting, or wearing compression stockings, may help prevent foot and leg cramps.

- Harvard Medical School suggests staying hydrated throughout the day, eating foods rich in magnesium (especially leafy greens) and potassium (bananas, black beans), wearing warm socks at night if you have leg cramps, and keeping your muscles strong and flexible with regular exercises.
- A 2021 study found that the combination of daily calf and hamstring stretching for six weeks may reduce the severity of night‐time lower limb muscle cramps.
- A study found that people who drank electrolyte enhanced water during and after exercise were less susceptible to muscle cramps than those who drank pure water.
What Should You Do When You Get A Cramp?
Once the cramp has started, stretching the affected muscles and other muscles in the area, using heat (like a heat pad or hot water bottle) to help promote blood flow are thought to help manage the cramp, and gently massaging the area around the cramp are thought to be helpful recommendations.
What Happens If You Also Get Foot Or Leg Pain During Pregnancy?
While cramps may have no definitive cure or treatment, foot or leg pain during pregnancy does, and is something that our experienced podiatry team can help you with. Your feet undergo a lot of changes during pregnancy – like changes in foot size, arch shape and much more, which can all lead to foot pain and discomfort. Our podiatrists can determine the cause of your foot pain and treat it while keeping your feet comfortable and supported.
Your feet undergo a lot of changes during pregnancy – like changes in foot size, arch shape and much more, which can all lead to foot pain and discomfort. Our podiatrists can determine the cause of your foot pain and treat it while keeping your feet comfortable and supported.
To book an appointment, call us on 1800 366 837 or book online by clicking the booking button at the top of the page.
References
[1] http://jsums.medsab.ac.ir/article_910.html
[2] https://www.ncbi.nlm.nih.gov/books/NBK499895/
[3] https://www.ncbi.nlm.nih.gov/books/NBK499895/
[4] https://www.aafp.org/afp/2012/0815/p350.html
[5] https://www.pregnancybirthbaby.org.au/leg-cramps-during-pregnancy
[6] https://www.health.harvard.edu/staying-healthy/take-that-muscle-cramps
[7] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8127570/
[8] https://www.sciencedaily.com/releases/2021/03/210318101536.htm
[9] https://www.health.harvard.edu/staying-healthy/take-that-muscle-cramps
Categories: BlogsCauses and How to Stop Them
A foot cramp can strike out of nowhere, waking you from a sound sleep. You may suddenly feel the muscles tighten or knot up from a few seconds to a few minutes at a time.
You may suddenly feel the muscles tighten or knot up from a few seconds to a few minutes at a time.
Up to 60 percent of adults report getting nocturnal foot cramps. Spasms may happen just once in the night or result in repeat episodes that lead to insomnia and lingering pain.
The good news is that these cramps aren’t usually a reason for concern. While they can be associated with certain medical conditions, like diabetes or hypothyroidism, stretches and lifestyle changes may help ease them or make them go away entirely.
Keep reading to learn about the potential causes of nighttime foot cramps and how to get relief.
Sitting for long periods of time or otherwise being inactive may make the muscles in your feet more apt to cramp at night.
Sitting with poor posture may also inhibit blood flow to your feet or lead to nerve compression — two risk factors for developing cramps.
Your sleep position may also be a factor in circulation and nerve issues. Consider the following:
- Try examining how you sleep to see if it might be contributing to nighttime cramping.

- Sleeping with your feet pointing downwards may contribute to poor circulation.
- Try sleeping on your back or side with a pillow underneath your knees.
Working the muscles in your feet too hard may make them vulnerable to cramping.
The muscle fibers in your feet continually contract and expand to allow movement. If you do too much of an activity too soon, or work your feet too strenuously, you may experience fatigue in your muscles.
Fatigue depletes your body of oxygen and allows waste products to build up throughout the day. This buildup can cause cramping and spasms at night.
Wearing poorly fitted shoes or shoes without enough support throughout the day may tax foot muscles as well. Standing or working on concrete floors or other hard surfaces can have a similar effect.
The foot muscles work extra hard to support the weight of your body. Improper footwear may also impair the foot’s circulation, cutting off blood and oxygen, and producing painful spasms even when you’re off your feet.
Another possible cause of foot cramps at night is dehydration. You may not be drinking enough water during the day, or a bout of diarrhea or other illness may be dehydrating you.
Even exercising in hot weather can dehydrate you quickly, draining your body of precious fluids, salts, and minerals, such as potassium, magnesium, and calcium.
When your body gets low in fluids and electrolytes, your muscles become more vulnerable to spasms and cramps. You continue sweating and losing fluids while you sleep. This is why your foot cramps may arise at night.
Deficiencies in vitamins B-12, thiamin, folate, and other B vitamins may lead to nerve damage.
Magnesium and potassium deficiencies may lead to leg and foot cramps.
If you suspect you may have a nutritional deficiency, talk with a doctor or medical professional. A simple blood test can reveal your levels and indicate to your doctor if you need any supplementation or other treatment for underlying conditions.
Note that taking too many supplements may actually cause more harm than good, so see a doctor and get tested before adding supplements to your diet.
Drinking too much alcohol may lead to nerve damage and a condition known as alcoholic neuropathy. Symptoms include anything from muscle cramping and weakness to numbness and tingling in the arms or legs.
Heavy alcohol use may also contribute to dehydration and nutritional deficiencies in important B vitamins.
Just as with other nutritional deficiencies, lacking these vitamins may impair nerve function, which may worsen symptoms like muscle spasms.
People who are pregnant are more susceptible to leg and foot cramping at night, particularly in the second and third trimesters.
Researchers don’t know exactly why. Possible reasons may include:
- extra weight on the feet as baby grows
- dehydration
- nutritional deficiencies, particularly in magnesium
Medical conditions associated with nighttime foot cramping include:
- structural issues, such as spinal stenosis and peripheral arterial disease
- metabolic issues, such as kidney disease, anemia, hypothyroidism, hyperthyroidism, and type 1 or type 2 diabetes
- other conditions, such as nerve damage, osteoarthritis, and Parkinson’s disease
Certain medications may also make you more susceptible to cramping. These include:
These include:
- blood pressure medications
- statins
- diuretics
- birth control pills
If you’re on dialysis, this can also make you more prone to cramping.
There are no specific treatments doctors recommend to treat overnight foot cramping. Instead, it’s best to treat its underlying cause.
If you exercise regularly, keep it up! Regular movement may help prevent leg and foot cramps in the day and night.
New to exercise? Speak with a doctor or medical professional for recommendations on a plan that may work for you. Try brisk walks around your neighborhood (wearing supportive shoes) or other low-impact activities to start.
Anecdotal evidence from a 2012 study suggests that a few minutes on an exercise bike or treadmill before bed may help with nocturnal leg and foot cramps.
Stretch and soothe your muscles
Be sure to stretch each day to keep foot muscles loose, especially before and after you get in a sweat session.
What if you’re having a cramp at night? Stretch your foot gently, but forcefully to relieve the cramp by flexing your foot and pressing down on your big toe.
Walking around and jiggling your leg may also help with both foot and leg cramps. Taking a warm bath or shower, or using ice may ease any lingering pain. Deep tissue massage may help in the long term.
Examine your shoes
Wear supportive shoes that are comfortable, especially if you walk a lot on hard surfaces.
The part of your shoes that help nest your heel in place is called a heel counter. Shoes with a firm heel counter may be better in terms of providing support throughout the day. Well-fitted, well-supporting shoes may also help you avoid nocturnal foot cramps.
If you’re having trouble or don’t find any comfortable shoes, your doctor may refer you to a podiatrist for custom inserts.
Drink more water
Experts recommend that men drink 15.5 cups and women drink 11.5 cups of fluids like water each day. Keeping your muscles hydrated can help prevent cramping.
Keeping your muscles hydrated can help prevent cramping.
A good rule of thumb is that your urine should be light yellow to clear. If it’s darker than that, consider drinking another glass of water.
People who are pregnant or breastfeeding may need additional fluid each day to meet their hydration needs. Speak with a doctor if you have concerns about hydrating your body.
Eat well and supplement
Eat a well-balanced diet that includes plenty of calcium, potassium, and magnesium. If you have a diagnosed deficiency, address it with your doctor’s supervision.
There are multiple studies that support magnesium supplementation as a means to help with cramping. Ask your doctor about dosage and brand suggestions. Supplements are available in your local grocery store, health food store, or online.
Foods rich in magnesium include:
- whole grains
- beans
- nuts
- seeds
- unsweetened dried fruits
Bananas and leafy greens may also help balance electrolytes.
Lower your alcohol intake
Limit alcoholic beverages, like beer, wine, and mixed drinks. These beverages can dehydrate you.
In the case of alcohol-related nerve damage, seek help if you’re having a hard time quitting drinking. Consider reaching out to your doctor, a friend, or a local support program.
Conditions like alcoholic neuropathy can lead to permanent and progressive nerve damage. Early treatment is key in preventing this.
Practice self-care
You may be able to prevent nocturnal foot cramping with some simple self-care practices:
- Untuck the covers from the foot of your bed before you go to sleep so that your feet aren’t confined.
- Take a warm bath before bedtime to relax your muscles.
- Practice some light stretching throughout the day so that your muscles aren’t tight before bed.
Essential oils
You may also want to try massaging some topical essential oils onto your feet before bed. Oils such as geranium, chamomile, coriander, and ylang-ylang oils have anti-spasmodic properties.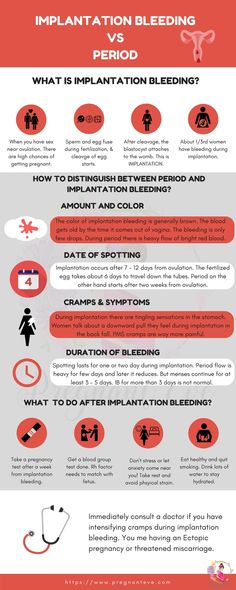
Aromatherapy with lavender or mint scents may also provide a calming sleep environment, which could decrease cramping.
During pregnancy
Let your doctor know if you’re experiencing nighttime foot cramping (or any severe muscle cramping) during pregnancy. While many of the same self-care measures may help you, your doctor can provide additional guidance.
Stretch your foot when a cramp strikes and elevate your legs to keep cramps at bay. Staying active, getting a massage, and taking a warm (not hot) shower or bath may also help.
Remember to take your prenatal vitamins each day to prevent nutritional deficiencies. Your doctor may recommend a magnesium supplement if the cramping is keeping you from sleeping.
You may find that the cramps go away on their own after you deliver your baby.
Foot cramps tend to go away on their own with home treatment, such as stretching or lifestyle changes, like drinking more water.
Talk with a doctor or medical professional if your cramps are causing severe discomfort, or if you notice any swelling, redness, or other changes to the foot or surrounding structures.
You may also want to make an appointment if the cramps are happening frequently and don’t improve with changes to your routine.
Interventions for leg cramps during pregnancy
What is the problem?
Leg cramps manifest themselves as sudden, intense involuntary contractions of the leg muscles. This is a common problem during pregnancy, especially in the third trimester. They are painful and can interfere with daily activities, disrupt sleep, and reduce quality of life. Various types of interventions are used to treat leg cramps during pregnancy, including medications, electrolytes (magnesium, calcium, sodium) and vitamins, as well as non-drug therapies such as muscle stretching. nine0005
Why is this important?
The aim of this review was to find out which treatment for leg cramps during pregnancy is effective and safe.
What evidence did we find?
In September 2019, we searched for evidence and identified eight randomized controlled trials in 576 women 14 to 36 weeks pregnant comparing magnesium, calcium, calcium with vitamin D or B vitamins versus placebo or no treatment, and compared vitamin C with calcium. All drugs were given as tablets to chew or swallow. nine0005
All drugs were given as tablets to chew or swallow. nine0005
Magnesium supplements may reduce the incidence of leg cramps in women compared with placebo or no treatment, although studies have not been consistent. Different studies have assessed the effect of magnesium supplementation differently. Some studies have shown magnesium to help reduce the incidence of leg cramps, while others have shown little or no effect. Data on the effect of magnesium on pain reduction was also inconclusive, with only one study showing a reduction in pain intensity, while others showed no difference. Differences in the occurrence of side effects such as nausea and diarrhea were negligible or non-existent. nine0005
Calcium did not always reduce the incidence of leg cramps in women after treatment compared to those who did not receive any treatment. It also found that the evidence was of very low quality, so we cannot be sure of the results.
More women who received B-vitamin supplements made a full recovery compared to those who received no treatment; however, these results were based on a small sample size and the study had design limitations. nine0005
nine0005
Frequency of leg cramps did not differ between women receiving calcium and women receiving vitamin C. with placebo.
What does this mean?
The quality of the evidence was low to very low. This was mainly due to small study sample sizes and study design weaknesses. Four studies were well-conducted and presented their reports. The remaining four had flaws in their design: in several studies, women were not best assigned to different treatment groups, and in two studies, women knew whether they were receiving treatment or not. Adverse effects, such as the effect of treatment on complications of pregnancy, childbirth and child, were not reported. Several studies have focused primarily on serum calcium and magnesium levels. The frequency and intensity of seizures and duration of pain were not uniformly reported, and there was often no information on whether they were assessed during treatment, at the end of treatment, or after treatment was discontinued. nine0005
nine0005
It is not clear from the evidence reviewed whether any oral interventions (magnesium, calcium, calcium with vitamin D, B vitamins, vitamin D, or vitamin C) are an effective and safe treatment for leg cramps during pregnancy. Supplements can have different effects depending on how women usually take them. None of the trials looked at forms of treatment such as muscle stretching, massage, relaxation, or heat therapy.
Translation notes:
Translation: Luzan Maria Alexandrovna. Editing: Yudina Ekaterina Viktorovna. Russian translation project coordination: Cochrane Russia - Cochrane Russia, Cochrane Geographic Group Associated to Cochrane Nordic. For questions related to this transfer, please contact us at: [email protected]
Reduces legs during pregnancy: what to do?
Pregnancy is a time of waiting and doubts. Probably, women never have so many questions. Why does it bring her legs together so often? What to do if you wake up with cramps at night? How to deal with this scourge and avoid bouts of pain in the legs? We are looking for answers to these and other questions. nine0005
nine0005
What are seizures?
Legs cramps not only during pregnancy, from time to time every person faces unpleasant painful cramps. A cramp is a sudden, uncontrollable muscle contraction that a person cannot relax. This condition can be caused by neurological disorders (for example, seizures are characteristic of epilepsy), a number of diseases (such as diabetes mellitus, osteochondrosis, and others), and can also be associated with physiological conditions. After all, convulsions occur, for example, after a strong overload, dehydration, hypothermia, etc. Sometimes cramps cause severe sharp pain. Sometimes it seems that the legs are pulling. During pregnancy, this condition, unfortunately, is noted quite regularly. nine0005
Why do pregnant women cramp their legs?
The mechanism of muscle contraction is quite complex, it involves different ions (charged particles): potassium, calcium, sodium and magnesium. If we are talking about a cramp, that is, a condition when we cannot relax a muscle, then magnesium ions play a leading role here.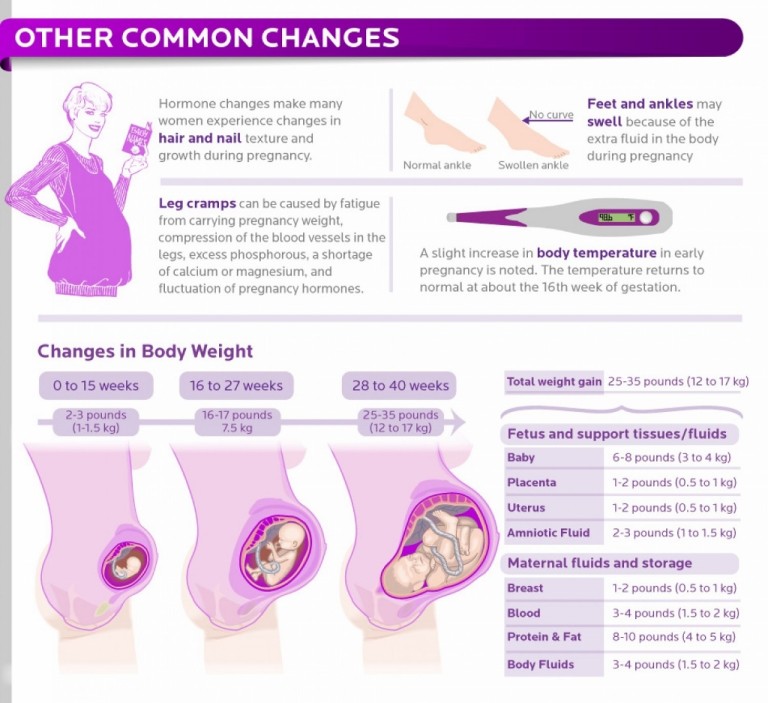 It is their lack that leads to the fact that women cramp their calves during pregnancy at night.
It is their lack that leads to the fact that women cramp their calves during pregnancy at night.
The lack of minerals in the body of the expectant mother is simply explained: such consequences are the restructuring of metabolism and functioning in the "double load" mode. In particular, the expectant mother needs one and a half times more magnesium than usual. nine0005
In addition to helping muscles relax, magnesium is also involved in a number of important physiological processes. In particular, magnesium is needed to regulate the processes of formation and expenditure of energy, it is involved in several hundred enzymatic reactions, and if there is little magnesium, then disturbances can occur in the work of almost any body system. Therefore, if magnesium preparations are prescribed during pregnancy, this recommendation should not be ignored. nine0005
Why do pregnant women cramp their legs at night?
The answer to this question is very simple. The fact is that during the day the body of the expectant mother bears an increased load. And the longer the gestation period, the greater this load. Violation of blood circulation, increased stress on the muscles - all this can cause night cramps.
And the longer the gestation period, the greater this load. Violation of blood circulation, increased stress on the muscles - all this can cause night cramps.
What should I do if my legs cramp during pregnancy?
To begin with, tell the doctor you are seeing about this. The magnesium preparations already mentioned, which he most likely recommends to you, can help solve the problem. nine0005
However, the reason that the expectant mother cramps her legs during pregnancy may be not only a metabolic disorder. Often muscle spasms begin as a result of varicose veins - the "faithful" companion of pregnancy. The veins of a woman carrying a baby are subject to increased stress. In addition, hormonal changes in the body seriously affect the state of blood vessels. All this contributes to the development of varicose veins. And a violation of the blood supply to the muscles of the legs, in turn, leads to convulsions.
If the expectant mother is faced with varicose veins, then the best prevention of its progression is to wear compression stockings selected by the doctor in accordance with the gestational age.