What is cephalic version
External cephalic version (ECV) – moving babies into position for birth
External cephalic version (ECV) – moving babies into position for birth | Pregnancy Birth and Baby beginning of content9-minute read
Listen
Key facts
- External cephalic version (ECV) is a procedure that tries to turn a breech baby into a head-down position so you can have a normal vaginal birth.
- An obstetrician will gently press on your abdomen to encourage your baby to turn.
- It is often, but not always, successful.
- ECV is done after 37 weeks, when your baby is less likely to turn by itself.
- Rarely, you may need to have an emergency caesarean after an ECV if there are complications.
What is external cephalic version?
External cephalic version (ECV) is a procedure that tries to turn your baby from a breech position to a head-down position, so you can have a normal vaginal birth.
‘Breech’ means that your baby is lying with its bottom or feet down in your uterus (womb) instead of head-down.
Why is it better for my baby to be head-down?
If your baby is in a breech position when you go into labour, a vaginal birth is more challenging. It may be more risky for your baby than if they were head-down.
There is a chance that your baby could be injured during the birth. Their head could get stuck, which is an emergency. There is a higher risk of cord prolapse, which is also an emergency.
Will my baby turn by itself?
Early in pregnancy, it’s very common for your baby to be in a breech position. Most babies will turn and settle into a head-down (cephalic) position as the pregnancy progresses.
By the end of pregnancy, about 3 in 100 babies are in a breech position.
As you get closer to your due date, the chance of your baby turning head-down by themselves gets smaller. Some breech babies turn naturally in the last month of pregnancy.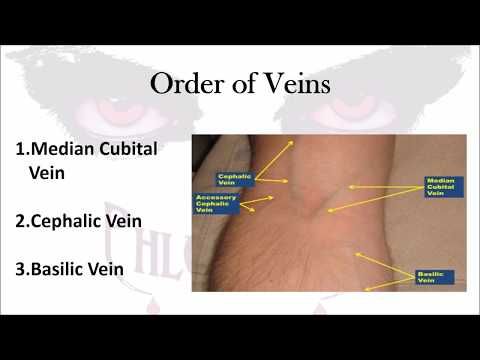 It’s more likely to happen if this is not your first baby.
It’s more likely to happen if this is not your first baby.
When should I think about having an ECV?
If your baby is still in a breech position at 36 weeks, your doctor or midwife might suggest you consider an external cephalic version (ECV).
An ECV is performed after 37 weeks of pregnancy, when your baby is unlikely to turn by themselves. If this is your first baby, you might be offered an ECV after 36 weeks.
Is an ECV suitable for all breech babies?
Most people can have an ECV if they have a healthy pregnancy. However, an ECV is not recommended if:
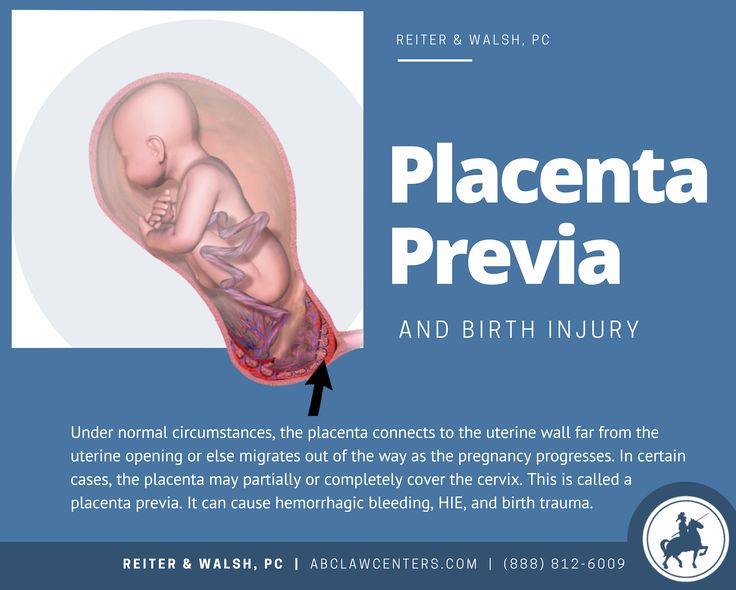
- you need a caesarean for other reasons, such as placenta praevia
- you have had vaginal bleeding in the past 7 days
- there is a problem with your baby's heart rate
- you are having twins or a multiple pregnancy
- your waters have broken
ECV might also not be recommended if:
- your baby is unwell or not growing well
- you have an unusually shaped uterus
- you have high blood pressure
- there is a lower than usual amount of amniotic fluid around your baby
- the umbilical cord is around your baby’s neck
If you have had one caesarean section in the past, you can usually still have an ECV.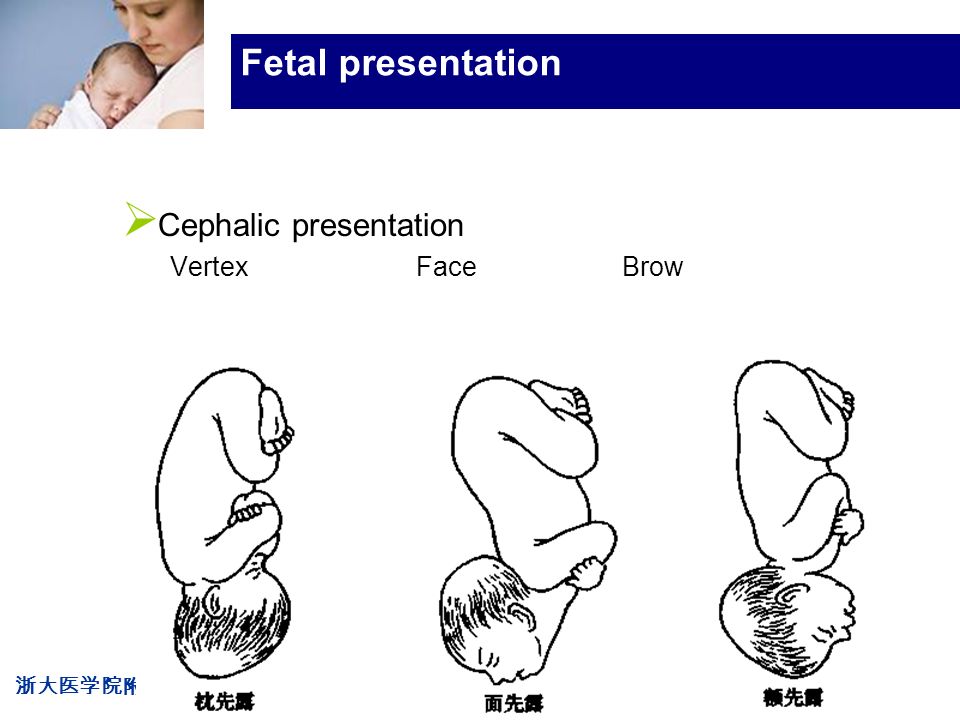 However, there are special considerations that you should discuss with your doctor.
However, there are special considerations that you should discuss with your doctor.
What can I expect during an ECV?
An ECV is performed by an obstetrician
It can take up to 3 hours from start to finish, as you and your baby will need to be monitored before and after. The turning procedure itself only takes about 10 minutes.
Before the ECV
Before the procedure, you will have an ultrasound to confirm that your baby is still breech. A midwife will connect you to a fetal monitor, also known as a CTG, to monitor your baby’s heart rate for 20 to 40 minutes.
A small needle will be inserted into a vein in your hand, to give you medicine to relax your uterus.
The ECV procedure
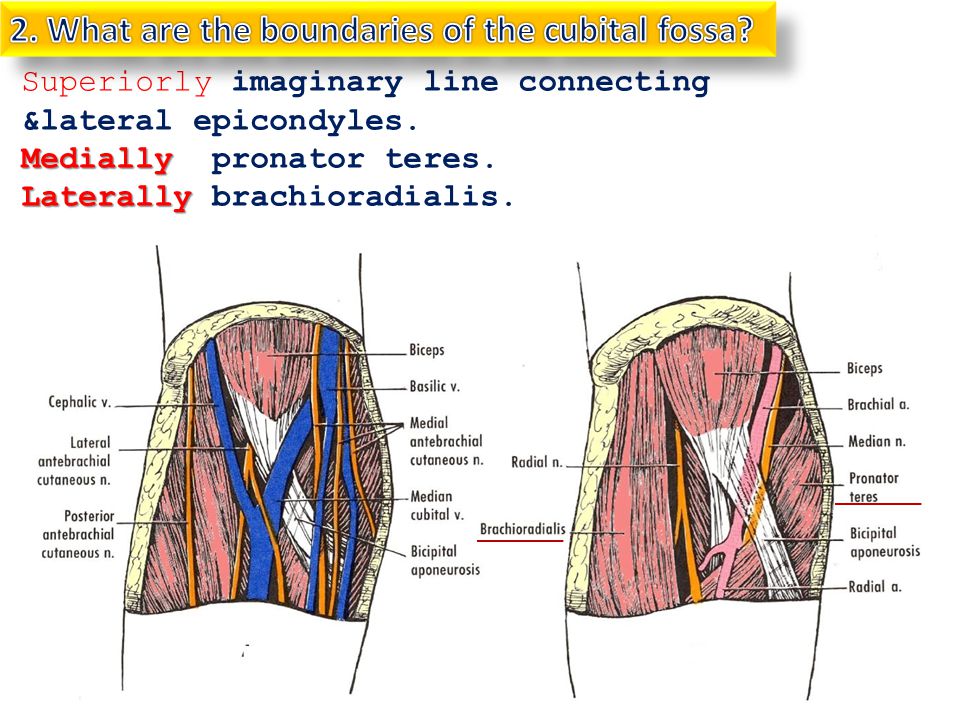
The obstetrician will try to turn your baby by pressing their hands gently on your abdomen, with one hand over the baby’s bottom and one hand behind the baby’s head. They will press in a clockwise or anti-clockwise direction to encourage your baby to roll.
Some people find this uncomfortable.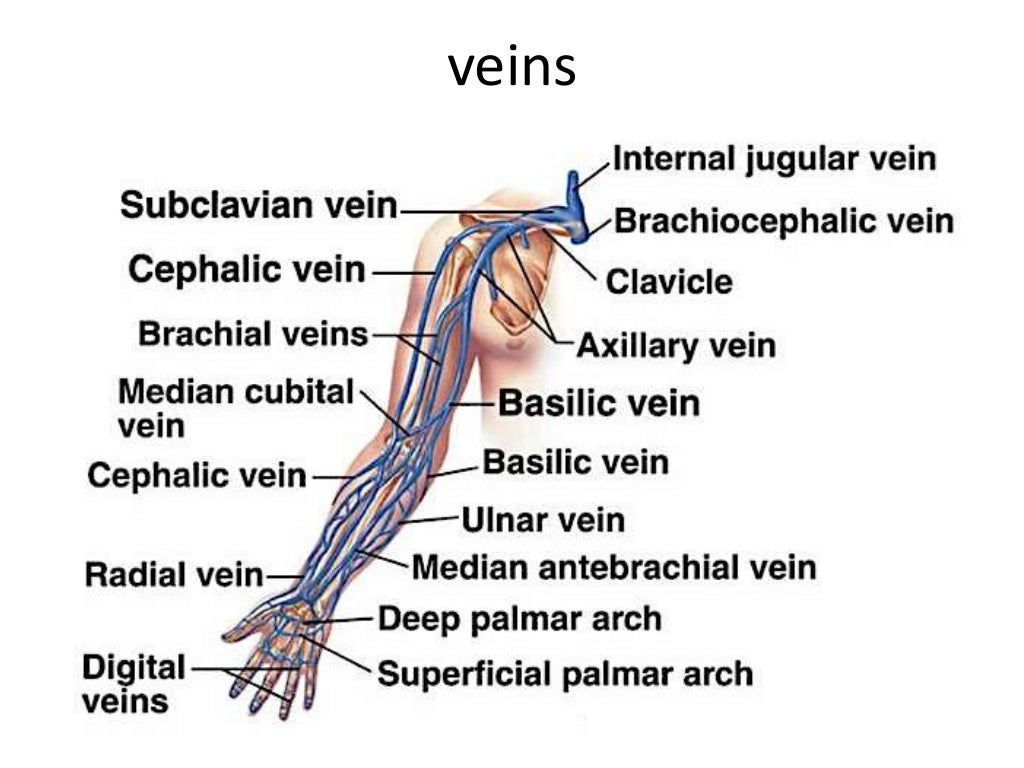 The pressure on your abdomen lasts a few minutes. If the first try is unsuccessful, the obstetrician might try again, up to 4 times.
The pressure on your abdomen lasts a few minutes. If the first try is unsuccessful, the obstetrician might try again, up to 4 times.
After the ECV
The CTG will be connected again after the procedure to check your baby’s heart rate. Your blood pressure and heart rate will also be monitored.
You might have another ultrasound to check the baby’s position.
If you needed anti-D injections during your pregnancy, you will have another injection after the ECV.
After you have had the ECV procedure, contact your docter or midwife immediately if:
- you have pain in your abdomen
- you start having contractions
- you notice bleeding or fluid leaking from your vagina
- your baby is moving less than usual
What are the risks of ECV?
ECV is a safe procedure. However, like any procedure, there is a small risk of complications. Occasionally, it can cause bleeding from the placenta or changes in your baby’s heart rate.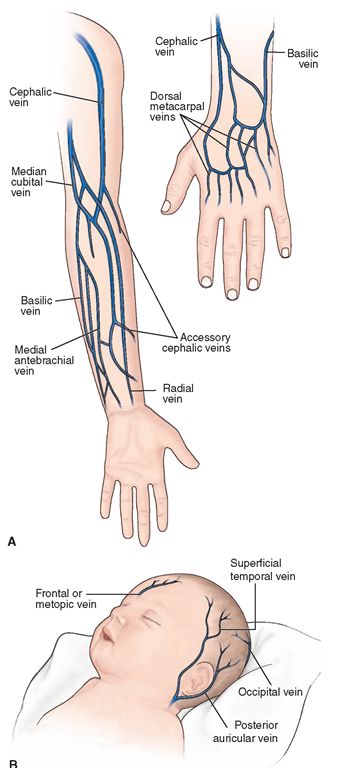 About 1 in every 200 people having an ECV may need an emergency caesarean because of complications.
About 1 in every 200 people having an ECV may need an emergency caesarean because of complications.
Occasionally, ECV can cause your waters to break.
Where should I have an ECV done?
Although complications are rare, ECV should be done in a hospital that has facilities for an emergency caesarean section, just in case it is needed.
Will ECV make my baby turn?
ECV is successful about half the time. If you’ve had a baby before, ECV is more likely to work than if this is your first baby.
If your baby does turn, there is a small chance they will turn back to the breech position. However, most babies will stay head-down.
What happens if ECV doesn’t work?
If your baby doesn’t turn, a vaginal birth may still be possible. This depends on your individual circumstances. You can also plan for a caesarean birth. Talk to your doctor or midwife about your options.
Is there anything else I can do to make my baby turn?
Some people think that you might be able to encourage your baby to turn by holding yourself in certain positions, such as kneeling with your bottom in the air and your head and shoulders flat to the ground.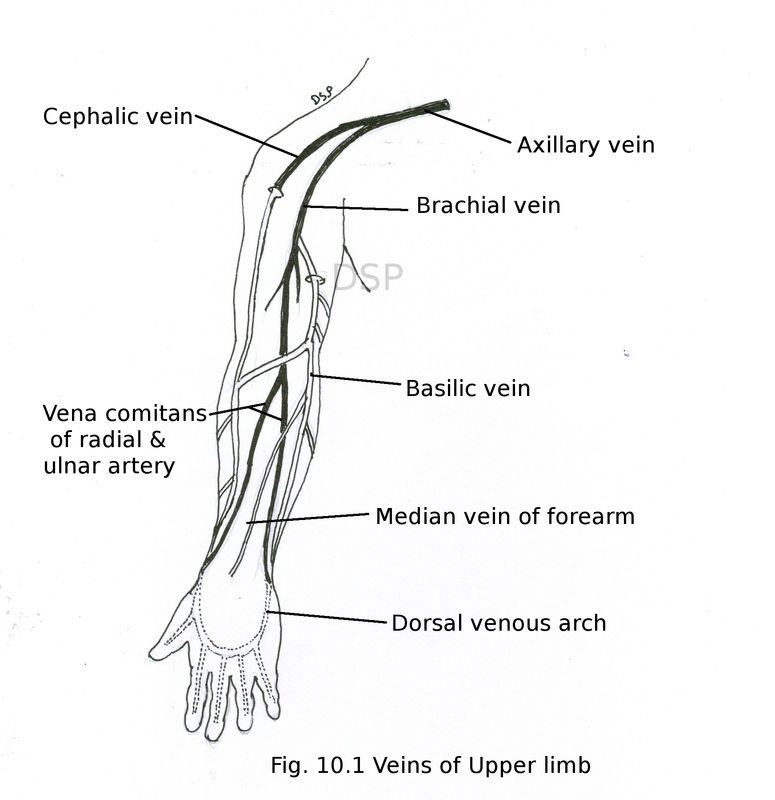 Other options you might hear about include acupuncture, a Chinese medicine treatment called moxibustion and chiropractic treatment. There is no good evidence that these work.
Other options you might hear about include acupuncture, a Chinese medicine treatment called moxibustion and chiropractic treatment. There is no good evidence that these work.
Talk to your doctor or midwife before trying any of these treatments.
Resources and support
For more information on breech presentation at the end of your pregnancy, ECV and other options:
- Breech presentation at the end of your pregnancy
- NSW Health’s: External cephalic version (ECV) for breech presentation
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
RANZCOG (Management of breech presentation), RANZCOG (Breech Presentation at the End of your Pregnancy), Mater Mothers’ Hospital (External cephalic version), Australian Government Department of Health and Aged Care (Pregnancy care guidelines: Fetal presentation), King Edward Memorial Hospital (Abnormalities of lie/presentation), Safer Care Victoria (Breech presentation: diagnosis and management), SA Health (Breech presentation), NSW Health (External cephalic version (ECV) for breech presentation), SA Health (Perinatal practice guideline cord presentation and prolapse)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Breech pregnancy
- Breech birth
Need more information?
External Cephalic Version for Breech Presentation - Maternal, child and family health
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website
Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website
Breech pregnancy
When a baby is positioned bottom-down late in pregnancy, this is called the breech position.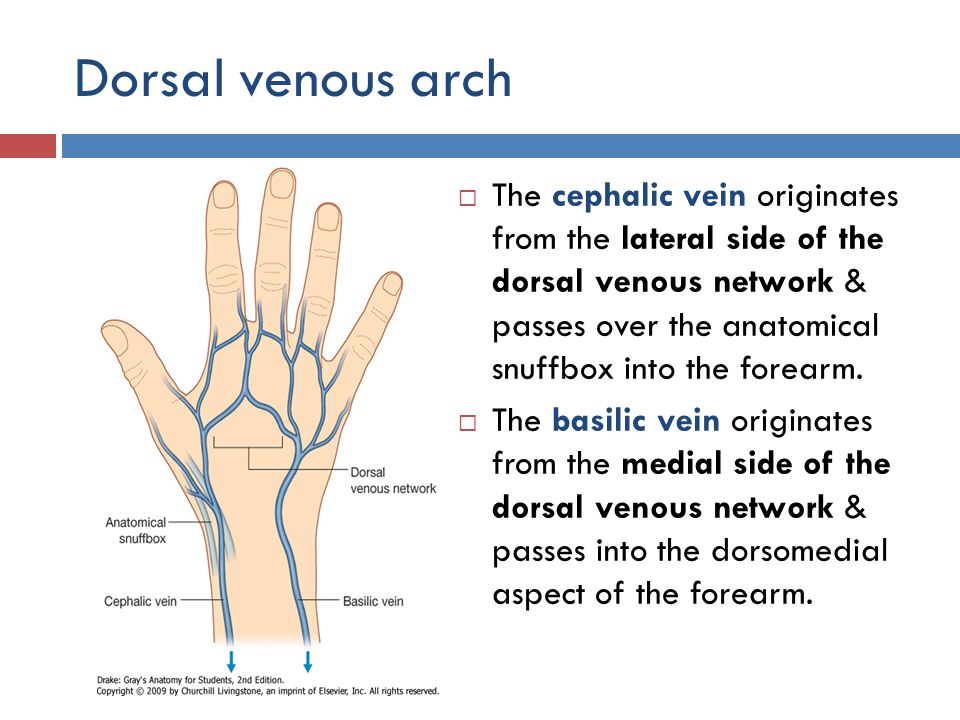 Find out about 3 main types and safe birthing options.
Find out about 3 main types and safe birthing options.
Read more on Pregnancy, Birth & Baby website
Malpresentation
Malpresentation is when your baby is in an unusual position as the birth approaches. Sometimes it’s possible to move the baby, but a caesarean maybe safer.
Read more on Pregnancy, Birth & Baby website
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 35
You'll probably be having lots of Braxton Hicks contractions by now.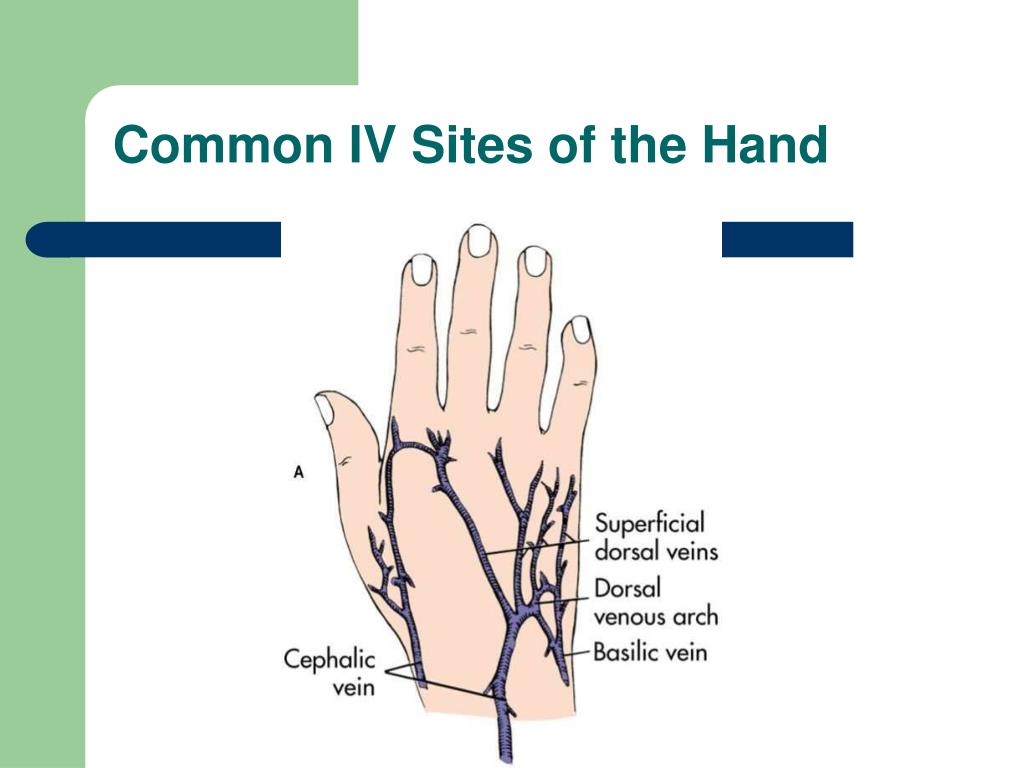 It's your body's way of preparing for the birth. They should stop if you move position.
It's your body's way of preparing for the birth. They should stop if you move position.
Read more on Pregnancy, Birth & Baby website
Anatomy of pregnancy and birth - pelvis
The pelvis helps carry your growing baby and is especially tailored for vaginal births. Learn more about the structure and function of the female pelvis.
Read more on Pregnancy, Birth & Baby website
Placental abruption - Better Health Channel
Placental abruption means the placenta has detached from the wall of the uterus, starving the baby of oxygen and nutrients.
Read more on Better Health Channel website
Rhesus D negative in pregnancy
Rhesus disease is an incompatibility between your and your baby’s blood types.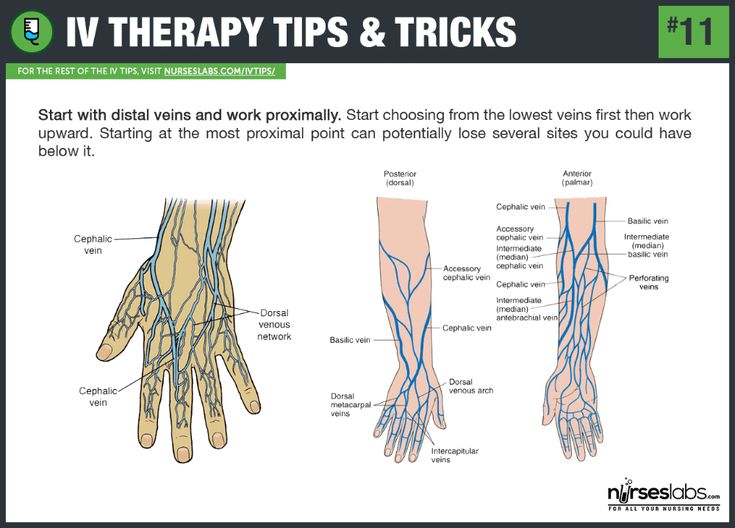 Find out what it could mean for your baby and how it is treated.
Find out what it could mean for your baby and how it is treated.
Read more on Pregnancy, Birth & Baby website
Glossary of pregnancy and labour
Glossary of common terms and abbreviations used in pregnancy and labour.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.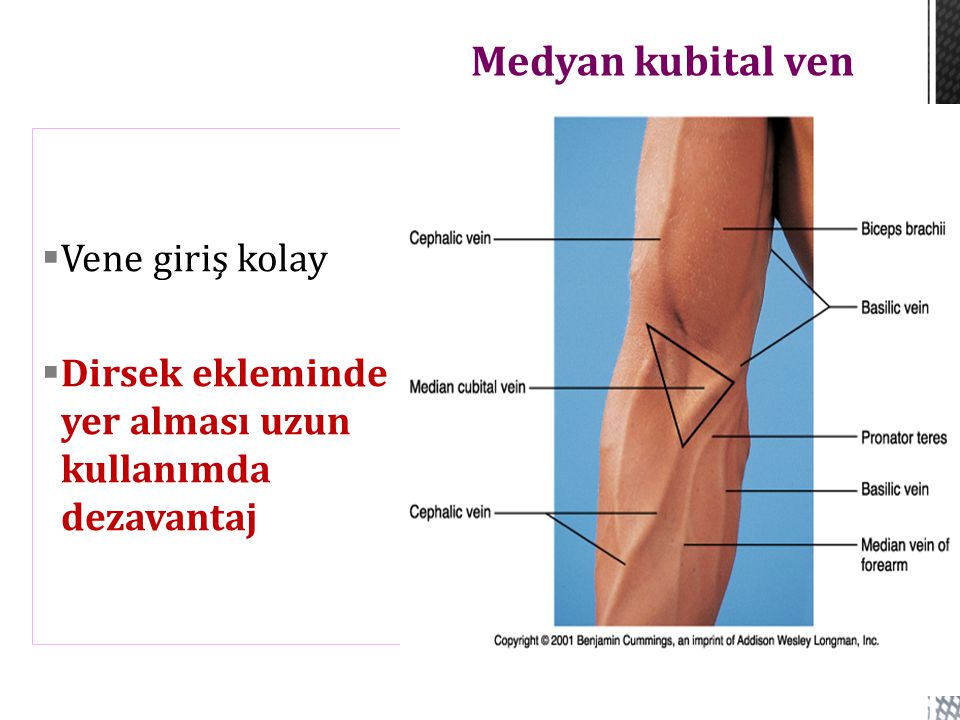
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care.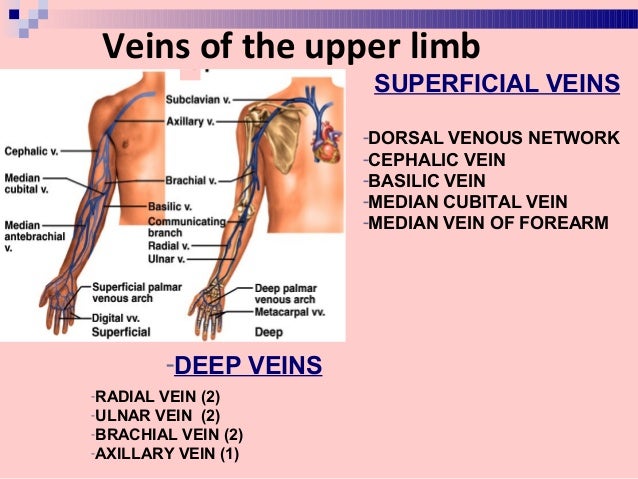 If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
External Cephalic Version - StatPearls
Meaghan M. Shanahan; Caron J. Gray.
Shanahan; Caron J. Gray.
Author Information and Affiliations
Last Update: July 4, 2022.
Continuing Education Activity
About 25 percent of fetuses will be in breech presentation at 28 weeks, though this decreases to roughly 3 to 4 percent at term. Most infants who are in breech presentation at the time of delivery will require a cesarean delivery. However, an alternative to immediately proceeding with cesarean section is a trial of external cephalic version. This procedure successfully brings the fetus into the vertex position, the ideal position for a vaginal birth, about 58 percent of the time. External cephalic version is performed strategically placing the hands on the gravid abdomen and applying pressure to encourage the fetus to move into the vertex position. This can be attempted for fetuses in the breech, transverse, or oblique positions and has the potential to decrease cesarean delivery rates. This activity reviews the indications, contraindications, and technique involved in performing external cephalic version and highlights the role of the interprofessional team in the care of patients undergoing this procedure.
Objectives:
Describe the types of breech presentation.
Outline the indications for external cephalic version.
Review the contraindications to external cephalic version.
Summarize a structured interprofessional team approach to provide effective care and appropriate surveillance of patients undergoing external cephalic version.
Access free multiple choice questions on this topic.
Introduction
About 25% of fetuses will be in breech presentation at 28 weeks, and this decreases to about 3% to 4% of term pregnancies. Most of these patients will be delivered by cesarean delivery. It is held that the overall cesarean delivery rate is higher than it should be, and efforts to prevent the first cesarean section often present obstetricians with the task of decreasing the number of cesarean deliveries they perform. One alternative to cesarean delivery is an external cephalic version (ECV). Simply, it is a procedure to change the presentation of the fetus from breech, tranverse, or oblique to vertex by applying pressure externally to the fetus through the gravid abdomen. [1]The overall success rate for the procedure is about 58% and can lead to decreased cesarean delivery rates.[2]
Simply, it is a procedure to change the presentation of the fetus from breech, tranverse, or oblique to vertex by applying pressure externally to the fetus through the gravid abdomen. [1]The overall success rate for the procedure is about 58% and can lead to decreased cesarean delivery rates.[2]
Anatomy and Physiology
ECV can be attempted with malpresentation of the fetus such as breech, transverse and oblique presentations. Complete breech occurs when the fetus has the buttocks as the presenting part and the knees are flexed with the feet near the buttocks. Frank breech occurs when the buttocks are the presenting part, and the legs are extending with the feet near the fetal head. Incomplete breech involves one bent leg and one extended leg. Transverse presentations occur when the long axis of the fetus is at a right angle to the mother with the fetal head to one side of the maternal abdomen and the back noted to be either be up or down in relation to the rest of the fetal body.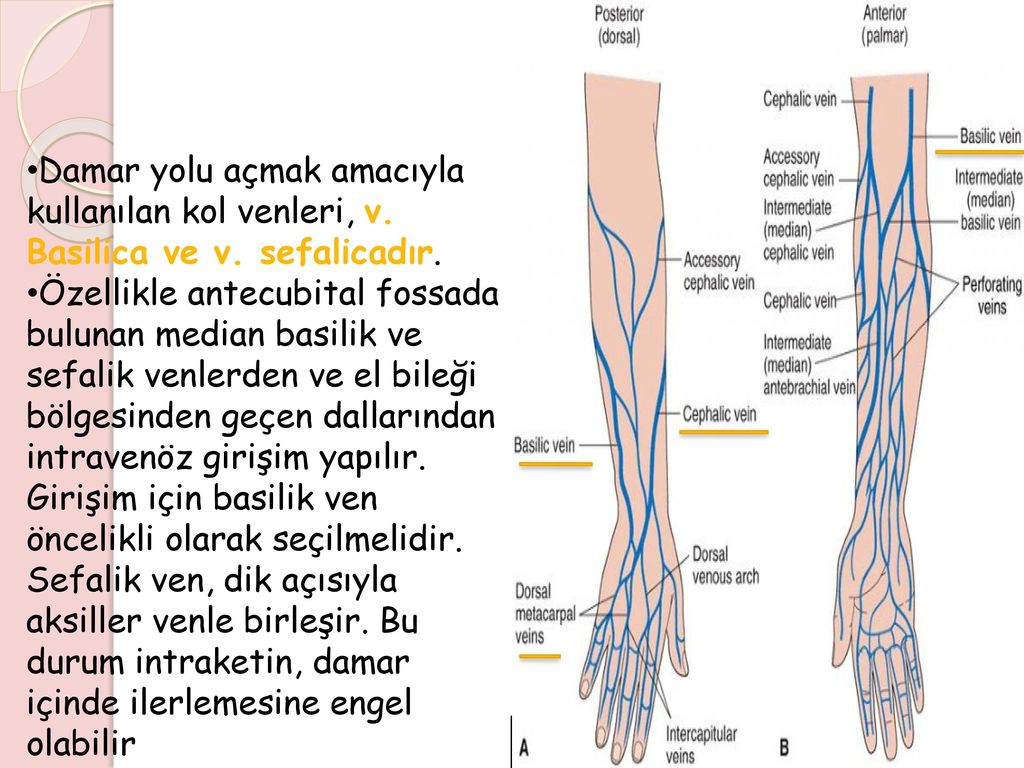 Oblique presentation is when the long axis of the fetus is at a 45-degree angle to the mother, with the fetal head usually in the right or left lower quadrants.
Oblique presentation is when the long axis of the fetus is at a 45-degree angle to the mother, with the fetal head usually in the right or left lower quadrants.
Indications
Indications for ECV include a fetus with greater than 36 weeks of gestation with malpresentation, reassuring fetal status, and no contraindications to vaginal delivery. Most practitioners will proceed with ECV at 37 weeks to decrease the risk of preterm delivery. Factors that may increase success include multiparity, transverse or oblique presentation, complete breech, adequate amniotic fluid, and unengaged presenting part. Factors that are associated with decreased success include nulliparity, advanced dilation, estimated fetal weight of less than 2,500 grams, anterior, lateral or cornual placenta, decreased amniotic fluid or ruptured membranes, maternal obesity, frank breech, fetal spine in the posterior position, and low station with an engaged presenting part.[3]
One alternative to ECV is expectant management with possible spontaneous version, although most fetuses that will spontaneously change presentations to vertex will do so before 36 weeks gestation and are noted more often in multiparous than nulliparous women. Other alternatives are expectant management with a vaginal or cesarean delivery of the breech fetus.
Other alternatives are expectant management with a vaginal or cesarean delivery of the breech fetus.
Contraindications
Any contraindication to vaginal delivery would also be a contraindication to ECV. These include but are not limited to placenta previa, vasa previa, active genital herpes outbreak, and prior classical cesarean delivery. Prior low transverse cesarean delivery is not a contraindication to external cephalic version, although not much data is available on uterine rupture rates.[4]
Antepartum ECV is contraindicated in multiple gestations, although it can be utilized for delivery of the second twin.[5]
Consideration should be used in patients with severe oligohydramnios, nonreassuring fetal monitoring, hyperextended fetal head, significant fetal or uterine anomaly, fetal growth restriction, and maternal hypertension due to these situations being associated with a low likelihood of success of ECV and possible increased risk to the fetus from the procedure.
If a woman presents in labor with malpresentation, ECV could be a reasonable option if she is in early labor, the presenting part is unengaged, there is a normal amniotic fluid index, and no contraindications to vaginal delivery or ECV.
Equipment
Not much equipment is necessary for this procedure as it is performed with the physician's own hands. Fetal monitoring and ultrasonography are necessary components for safety and reassurance.
Personnel
An obstetrician experienced in external cephalic version is needed to perform an ECV. The procedure can be performed by one or two people. Not necessary in the room, but those that should be aware of the ECV procedure would be those needed in case of emergency cesarean delivery, such as nursing, operating room, and anesthesia staff.
Preparation
In preparation for ECV, the fetal presentation must be determined by ultrasound and fetal well-being must be assessed, usually by a nonstress test. Contraindications are reviewed with the patient to confirm that they have none. Risks, benefits, and alternatives are reviewed with the patient, and informed consent is obtained. Rh status should be known before the procedure and anti-D immune globulin administered after the procedure if indicated.
Risks, benefits, and alternatives are reviewed with the patient, and informed consent is obtained. Rh status should be known before the procedure and anti-D immune globulin administered after the procedure if indicated.
Technique
Some practitioners choose to administer a tocolytic, usually terbutaline 0.25 mg subcutaneously, 15 to 30 minutes before the procedure, if are no contraindications. Data does not support either calcium channel blockers or nitroglycerin for tocolysis in this situation.[6] Some practitioners choose to use regional anesthesia in the form of either a spinal or epidural, but data is insufficient to recommend this for all external cephalic version attempts, although it may add to success if tocolysis alone is not successful.[7]
The patient is lying supine, with a sideways tilt with a wedge to keep pressure off the aorta and vena cava. If the fetal presentation is breech, then the breech is lifted out of the pelvis with one hand, and the other hand is used to apply pressure to the back of the fetal head to attempt a forward roll. If a forward roll is unsuccessful, then a backward roll can be attempted. If the fetus is in either a transverse or oblique presentation, similar manipulation of the fetus is used to attempt to move the fetal head to the pelvis, noting a shorter distance to move than if the fetus is in a breech presentation.[8]
If a forward roll is unsuccessful, then a backward roll can be attempted. If the fetus is in either a transverse or oblique presentation, similar manipulation of the fetus is used to attempt to move the fetal head to the pelvis, noting a shorter distance to move than if the fetus is in a breech presentation.[8]
Intermittent use of ultrasonography during the procedure can be used to document fetal heartbeat and current presentation. The procedure should be abandoned if there is significant fetal bradycardia, discomfort to the patient, or if the procedure is not completed easily. Afterward, the patient should be monitored for at least 30 minutes, with fetal heart rate tracing and anti-D immune globulin given if indicated. Immediate induction is not recommended to minimize reversion, although this could be considered after 39 weeks of gestation. If ECV is unsuccessful, additional attempts can be made at the same admission or in one or more days following the initial procedure.
Complications
The most common complications associated with ECV are fetal heart rate abnormalities, occurring at a rate of 4.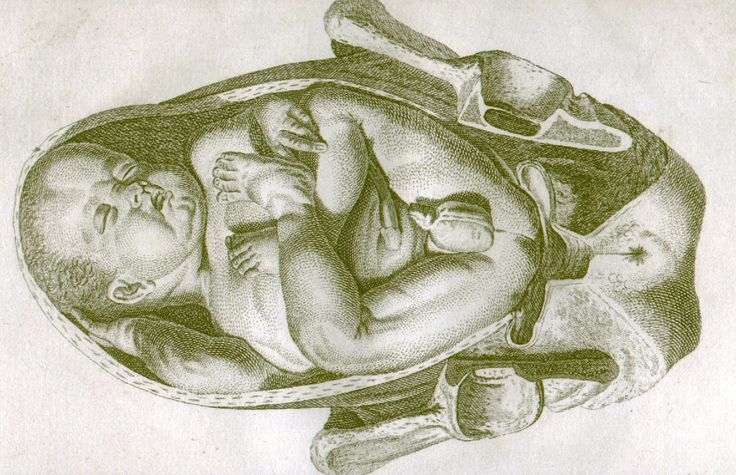 7%, but these usually are transient and improve upon completion or abandonment of the procedure. More severe complications of ECV occur at a rate of less than 1% and include emergency cesarean section, premature rupture of membranes, cord prolapse, vaginal bleeding, placental abruption, fetomaternal hemorrhage, and stillbirth. Although complications are rare, ECV should be attempted in locations where an emergency cesarean section can be performed. For this reason, some practitioners chose to perform ECV in the operating room, although this is not necessary.[9]
7%, but these usually are transient and improve upon completion or abandonment of the procedure. More severe complications of ECV occur at a rate of less than 1% and include emergency cesarean section, premature rupture of membranes, cord prolapse, vaginal bleeding, placental abruption, fetomaternal hemorrhage, and stillbirth. Although complications are rare, ECV should be attempted in locations where an emergency cesarean section can be performed. For this reason, some practitioners chose to perform ECV in the operating room, although this is not necessary.[9]
Clinical Significance
Patients should be counseled on and offered ECV when appropriate. Some data show that only 20% to 30% of eligible candidates are offered ECV.[10]
Women who have a successful ECV have a lower cesarean delivery rate than women who do not, although they are still at a higher risk of cesarean delivery than women with cephalic presenting fetuses and no ECV. ECV is cost effective if the probability of a successful ECV is greater than 32%.
Enhancing Healthcare Team Outcomes
ECV is best performed by an interprofessional team. The actual procedure is performed by an experienced obstetrician aided by a labor and delivery nurse. This is not a benign procedure and it is recommended that the operating room be informed of the ECV procedure, in case of emergency cesarean delivery, such as nursing, operating room, and anesthesia staff. Fetal monitoring is necessary and steps to ensure safety must be paramount.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Levin G, Rottenstreich A. Re: External cephalic version at term: a cohort study of 18 years' experience: External cephalic version at term: a need for modifiable predictor. BJOG. 2019 Apr;126(5):675. [PubMed: 30575279]
- 2.
Nalam RL, Chinnachamy P, Emmanuel P. External Cephalic Version: A Dying Art Worth Reviving.
 J Obstet Gynaecol India. 2018 Dec;68(6):493-497. [PMC free article: PMC6207544] [PubMed: 30416278]
J Obstet Gynaecol India. 2018 Dec;68(6):493-497. [PMC free article: PMC6207544] [PubMed: 30416278]- 3.
What factors determine the success of an external cephalic version? BJOG. 2019 Mar;126(4):501. [PubMed: 30729658]
- 4.
Rosman AN, Guijt A, Vlemmix F, Rijnders M, Mol BW, Kok M. Contraindications for external cephalic version in breech position at term: a systematic review. Acta Obstet Gynecol Scand. 2013 Feb;92(2):137-42. [PubMed: 22994660]
- 5.
Bogner G, Wallner V, Fazelnia C, Strobl M, Volgger B, Fischer T, Jacobs VR. Delivery of the second twin: influence of presentation on neonatal outcome, a case controlled study. BMC Pregnancy Childbirth. 2018 May 18;18(1):176. [PMC free article: PMC5960113] [PubMed: 29776396]
- 6.
Mohamed Ismail NA, Ibrahim M, Mohd Naim N, Mahdy ZA, Jamil MA, Mohd Razi ZR. Nifedipine versus terbutaline for tocolysis in external cephalic version. Int J Gynaecol Obstet. 2008 Sep;102(3):263-6.
 [PubMed: 18554601]
[PubMed: 18554601]- 7.
Carlan SJ, Dent JM, Huckaby T, Whittington EC, Shaefer D. The effect of epidural anesthesia on safety and success of external cephalic version at term. Anesth Analg. 1994 Sep;79(3):525-8. [PubMed: 8067558]
- 8.
Nagy J, Huvar I. [External cephalic version in breech presentation of fetus]. Ceska Gynekol. 2004 Nov;69(6):444-51. [PubMed: 15633412]
- 9.
Rodgers R. External cephalic version is associated with a low complication rate. BJOG. 2019 Mar;126(4):500. [PubMed: 30461156]
- 10.
Rauf B, Nisa M, Hassan L. External cephalic version for breech presentation at term. J Coll Physicians Surg Pak. 2007 Sep;17(9):550-3. [PubMed: 17903404]
Headache and its types - GBUZ MO DCGB
Headache is one of the most common reasons patients seek medical care, mostly on an outpatient basis. During the year, a headache occurs at least once in 90% of people.
There are no pain receptors directly in the brain tissues, therefore, the factor causing pain is irritation of neighboring structures: meninges, cranial and spinal nerves, nocireceptors in the walls of extracranial vessels, muscles of the head and neck. The causes of primary headaches are still not fully understood. nine0005
Headaches are divided into primary (without an external cause) and secondary.
Primary include:
• Migraine (with aura, without aura…)
• Tension headache (chronic, episodic…)
• Trigeminal autonomic cephalalgias (Cluster headache, SUNCT syndrome…)
• Other primary headaches pain (cough headache, headache with physical exertion, headache associated with cold stimuli ...)
Secondary headaches include:
• Headaches associated with trauma or injury to the head and/or neck
• Headaches associated with lesions of the vessels of the brain and neck
• Headaches associated with non-vascular intracranial lesions
• Headaches associated with various substances or their withdrawal
• Headaches associated with infections
• Headaches and facial pains associated with pathology of the skull, neck, eyes, ears, nasal cavity, sinuses, teeth, mouth or other structures of the neck and face
• Headaches associated with mental disorders
• Painful cranial neuropathies and other facial pains.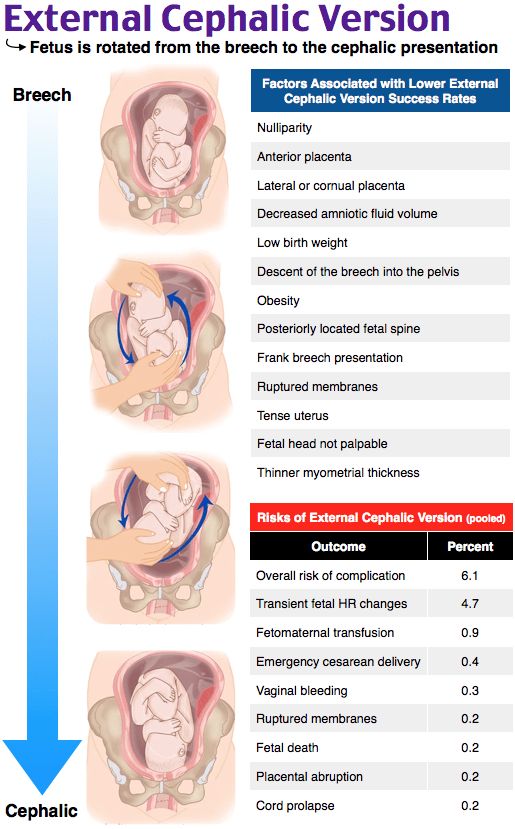
Fortunately, in only 8% of patients headaches are caused by severe organic diseases: tumor, traumatic brain injury, infection, etc. In other cases, patients suffer from primary headaches, among which tension headaches are the most common - 54% and migraine - 38%.
Secondary headache is also called symptomatic, as it is a symptom of another, sometimes formidable disease, such as meningitis, brain tumor, acute cerebrovascular accident, brain injury ...
For the timely recognition of dangerous situations that require quick decisive action
, a system of "red flags" has been developed. For ease of remembering, there are several mnemonic techniques, one of them: SNOOP .
• Systemic . Systemic symptoms. When, along with a headache, there is an increase in body temperature, weight loss, a known malignant tumor, HIV infection.
• Neurological . Neurological disorders: decreased strength, impaired sensitivity, impaired coordination, etc.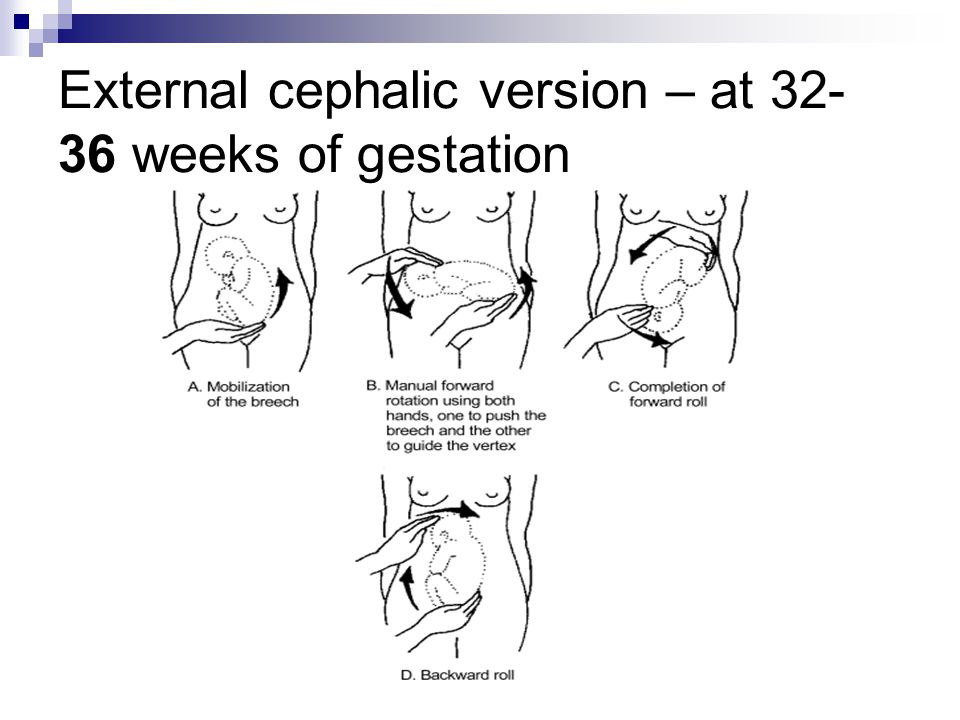
• Onset after 50 . Newly diagnosed headache after 50 years.
• Onset sudden . Sudden violent thunder-like headache.
• Pattern . Change in the nature, frequency of headache.
A timely visit to a doctor will help to suspect and identify (or exclude) a possible formidable disease. Our hospital has all the necessary diagnostic tools and qualified neurologists to help you understand the causes of headaches. nine0008
From rubric Uncategorized, NewsFrom a sick head to a healthy one
Pain from which the head simply splits in half... Do you know such a picture when it seems that you are ready to drink a whole mountain of painkillers, just to let go? Fortunately, pharmacies offer a whole arsenal of medicines. But, do not rush to grab the pills. Try first to understand why your head hurts? The head of the Regional Center for Diagnosis and Treatment of Headache of the OKDC, Candidate of Medical Sciences Elena Shestel will help to figure this out.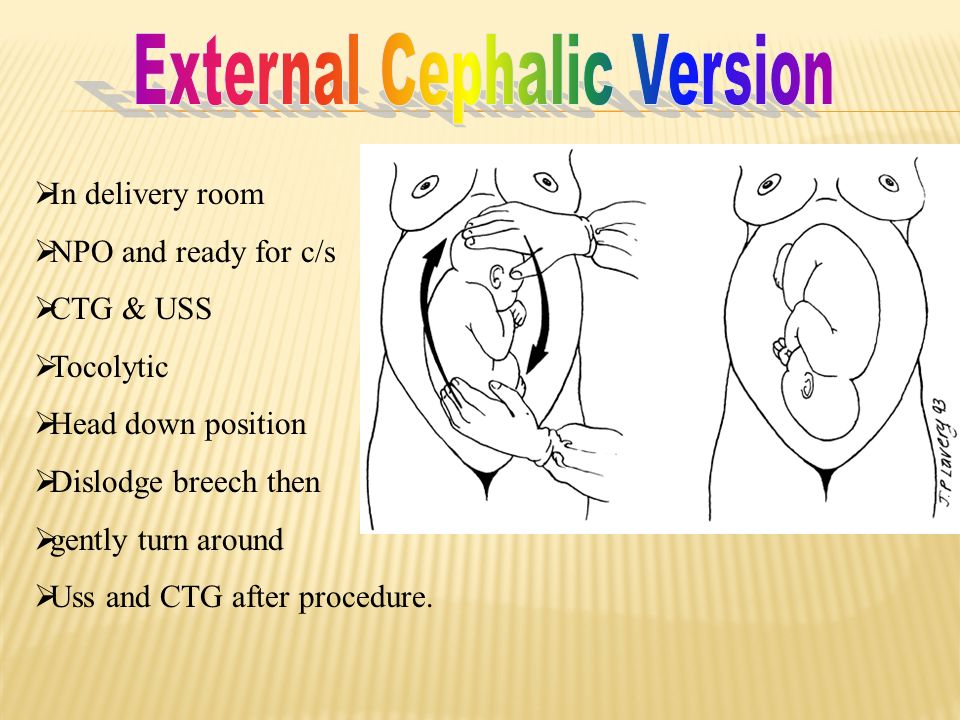 nine0008
nine0008
All "happy" heads hurt the same way...
In healthy people, headaches can be caused by stress or banal overwork. The fact is that such negative states as anger, anxiety, fear lead to prolonged tension in the muscles of the face, shoulders and neck. Nerve endings are “clamped” in tense muscles, and the nerve impulses coming from them are transmitted to receptors in the soft tissues of the head - a person feels pain. nine0017 Prolonged sitting in a half-bent position can also provoke pain, since the back and neck in this position “numb”, and this leads to vasoconstriction and a reduction in blood flow, which, in turn, causes a lack of oxygen in the tissues and the accumulation of metabolic products in them. . At the same time, dilation of the blood vessels (for example, due to excessive eye strain) leads to irritation of the nerve endings, which also causes a headache.
nine0002 According to WHO, 99% of the world's people experience a headache at least once in their lives.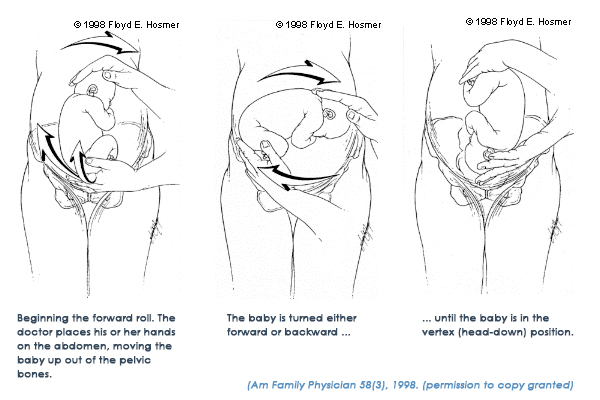 Most often, it goes away on its own: just drink hot tea, relax, take a bath, adding a few drops of essential oils to the water: lavender, lemon, peppermint... Fragrant foam and sea salt are only welcome! Or, stand under a hot shower - this will help relieve spasmodic headaches caused by spasm of the muscle on the back of the neck and head. You can do mustard foot baths - they reduce blood pressure in the brain. In addition, cold compresses help well, as they constrict blood vessels in the painful area and reduce pain pulsation. A bag with ice cubes wrapped in a towel should be applied to the forehead, temples or back of the head for about 10-15 minutes. Listen to calm, pleasant music or watch an interesting humorous program. Laughter not only tones blood vessels, but also promotes the production of endorphins, pleasure hormones, which have an analgesic effect. You can do a head massage with light stroking movements from the forehead to the back of the head
Most often, it goes away on its own: just drink hot tea, relax, take a bath, adding a few drops of essential oils to the water: lavender, lemon, peppermint... Fragrant foam and sea salt are only welcome! Or, stand under a hot shower - this will help relieve spasmodic headaches caused by spasm of the muscle on the back of the neck and head. You can do mustard foot baths - they reduce blood pressure in the brain. In addition, cold compresses help well, as they constrict blood vessels in the painful area and reduce pain pulsation. A bag with ice cubes wrapped in a towel should be applied to the forehead, temples or back of the head for about 10-15 minutes. Listen to calm, pleasant music or watch an interesting humorous program. Laughter not only tones blood vessels, but also promotes the production of endorphins, pleasure hormones, which have an analgesic effect. You can do a head massage with light stroking movements from the forehead to the back of the head But, if the pain does not go away for a long time, if it often recurs, then you need to deal with it already in the doctor's office.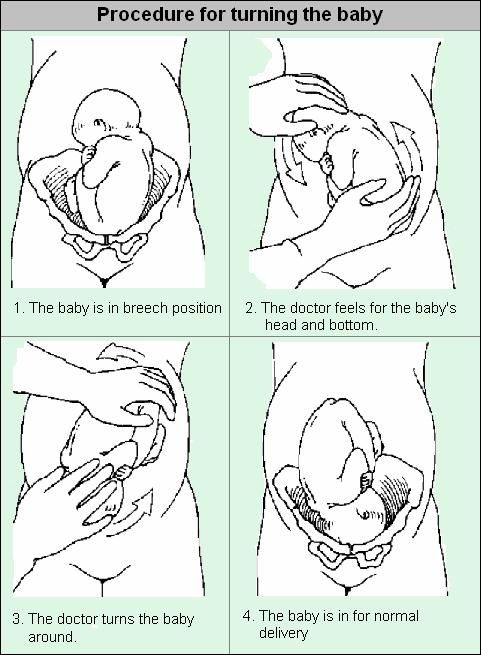
The fact is that a headache can be a manifestation of such threatening diseases as a brain tumor, heart attack or stroke, cerebral hemorrhage, meningitis, encephalitis, trauma ... In this case, we are talking about secondary headaches - in the medical classification, their number approaches three hundred. But, fortunately, this situation occurs only in 2% of cases. Most often, pains are not associated with structural disorders of the brain, they are benign in nature with a favorable prognosis. They are called primary. The most common among them are migraine, tension headache, cluster headache. nine0005
Illness of responsible people
Almost a fifth of the world's population suffers from migraines. It is noticed that the disease, as a rule, occurs in people who are ambitious, responsible and conscientious, tend to overload themselves with work. Migraines are often hereditary. It is noteworthy that the weaker sex is most susceptible to a serious, but not fatal illness.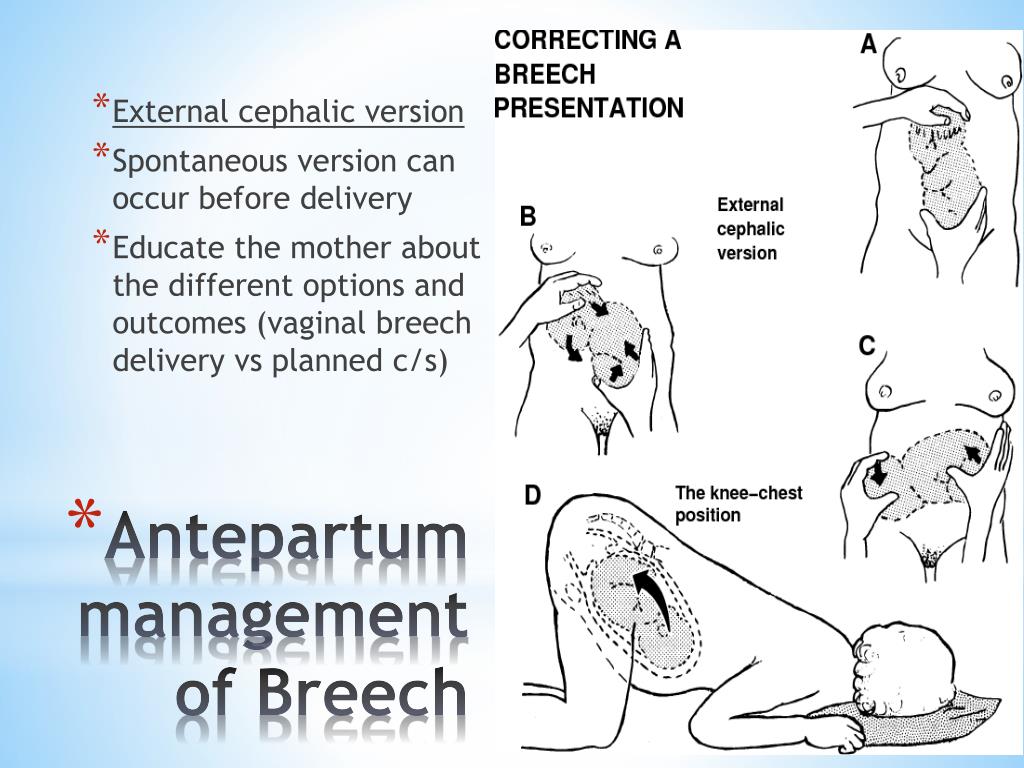 The symptom of the disease is well known: with a migraine, only half of the head hurts. Severe throbbing pain during an attack may cover the orbital, parietal, temporal or occipital region of the head. Sometimes, before an attack, a person has a special visual aura: flickering spots, fuzzy outlines of objects, darkening in the eyes. Arising several times a month, many-day attacks turn life into torment. Conventional analgesics, as a rule, are not effective - here special anti-migraine vasoconstrictor drugs are required. You need to take them at the beginning of the attack. But only a doctor should prescribe a medicine, based on the individual characteristics of the patient and concomitant diseases. nine0005
The symptom of the disease is well known: with a migraine, only half of the head hurts. Severe throbbing pain during an attack may cover the orbital, parietal, temporal or occipital region of the head. Sometimes, before an attack, a person has a special visual aura: flickering spots, fuzzy outlines of objects, darkening in the eyes. Arising several times a month, many-day attacks turn life into torment. Conventional analgesics, as a rule, are not effective - here special anti-migraine vasoconstrictor drugs are required. You need to take them at the beginning of the attack. But only a doctor should prescribe a medicine, based on the individual characteristics of the patient and concomitant diseases. nine0005
Courageous on the outside, gentle on the inside
However, one should not think that a headache is a purely female privilege. For example, cluster headache, the most excruciating of all, is unique to men. It manifests itself in characteristic pain periods with a duration of 15-180 minutes, repeated several times a day for up to 3 months. This is an extremely intense paroxysmal pain localized in the region of one eye, accompanied by lacrimation, nasal congestion and a pronounced feeling of anxiety and restlessness. The pain disappears suddenly and it happens that for several years it does not bother a person at all. There is a widespread opinion among physicians that representatives of the “strong” sex with an exceptionally masculine, but deceptive appearance suffer from cluster pains. In fact, they are soft, timid, indecisive. nine0005
This is an extremely intense paroxysmal pain localized in the region of one eye, accompanied by lacrimation, nasal congestion and a pronounced feeling of anxiety and restlessness. The pain disappears suddenly and it happens that for several years it does not bother a person at all. There is a widespread opinion among physicians that representatives of the “strong” sex with an exceptionally masculine, but deceptive appearance suffer from cluster pains. In fact, they are soft, timid, indecisive. nine0005
Tired - rest
Everyone knows the headache associated with overwork. Its cause is not only stress, but also a busy work schedule, personal problems, weather changes. This is the most common type of headache, the so-called tension headache. It manifests itself in the form of episodes lasting from several minutes to several days, usually bilateral, compressing or pressing, of moderate intensity. But often, in the absence of proper treatment, such a headache becomes chronic, is permanent and is poorly relieved by taking classic analgesics.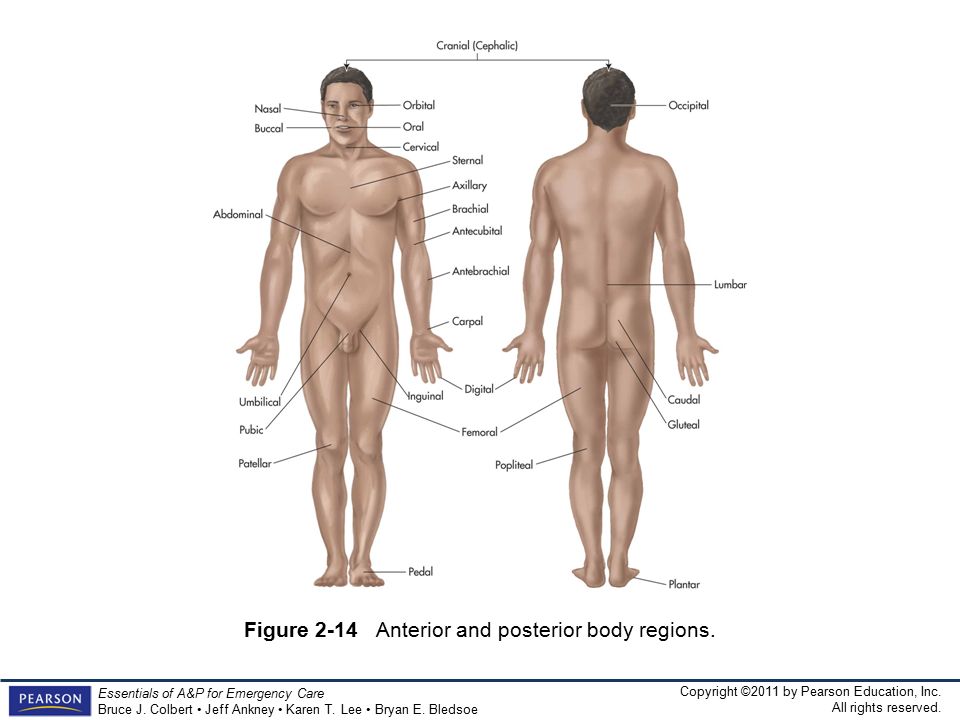 nine0005
nine0005
Do not rush to take pills
What to do if you have a headache? First and foremost, don't rush to take your medication. No matter how good, modern and expensive the drug is, any of them has side effects. This is especially true for homeopathic remedies and dietary supplements. In addition, self-administration of medications gives only a short-term result, but does not affect the mechanisms of pain syndrome. As a result, the headache returns again and again, the number of painkillers increases, which leads not only to the development of side effects of the drug itself, but also to the development of dependence on analgesics, which in itself can also provoke a headache. Competent therapy with specific drugs can only be selected by a doctor, and in such cases it is necessary to take medications under strict medical supervision. nine0005
Important
Very often, headaches are caused by certain provoking factors - triggers. They are different for everyone and can change in one person from attack to attack. Here are the most common ones:
They are different for everyone and can change in one person from attack to attack. Here are the most common ones:
- Nutrition. Basically, this is an irregular diet. In addition, some people are sensitive to certain types of foods (cheese, chocolate, coffee, citrus fruits). Alcohol, especially red wine, beer, champagne, cocktails are common headache triggers. nine0110
- Sleep. Lack of sleep or prolonged sleep are common causes of headaches. Try to get up on weekends no later than 2 hours from your usual awakening on weekdays.
- Physical activity. Hard physical work or intense workouts in the gym can trigger a headache, but at the same time, regular exercise and keeping fit are a good defense against this scourge. Dosed aerobic exercise and swimming are desirable. nine0110
- Environment: bright or flickering lights, strong (sometimes even pleasant) odors, stuffy rooms, sudden weather changes, long journeys (especially jet lag).
- Psychological factors: negative emotions or, surprisingly, relaxation after a stressful situation.
- Hormonal factors in women: a certain phase of the menstrual cycle, pregnancy, menopause, taking or interrupting hormonal contraception. nine0110
If you have made lifestyle changes and your headaches persist and you have to take more than 2 analgesics a month, you should see your doctor.
What is strictly forbidden:
Consume alcohol. It dilates the blood vessels and at first it really becomes easier, but then the condition worsens.
Drink coffee. If you have high blood pressure or are prone to atherosclerosis, even one cup of coffee can be harmful. However, for hypertensive patients, on the contrary, a couple of sips of coffee will be a salvation. For those who constantly take horse doses of this drink, an extra dose will not help, but will only make it worse.