Different types of child rashes
Skin rashes in children | NHS inform
Childhood rashes are common and aren't usually a cause for concern. Most rashes are harmless and disappear without the need for treatment.
However, see your GP if your child has a rash and seems unwell, or if you're worried. They'll be able to investigate the cause and recommend any necessary treatment.
This page may give you a better idea about what could be causing the rash, but don't use this to self-diagnose your child's condition – always see a GP for a proper diagnosis.
The most common causes of rashes in children are:
- cellulitis
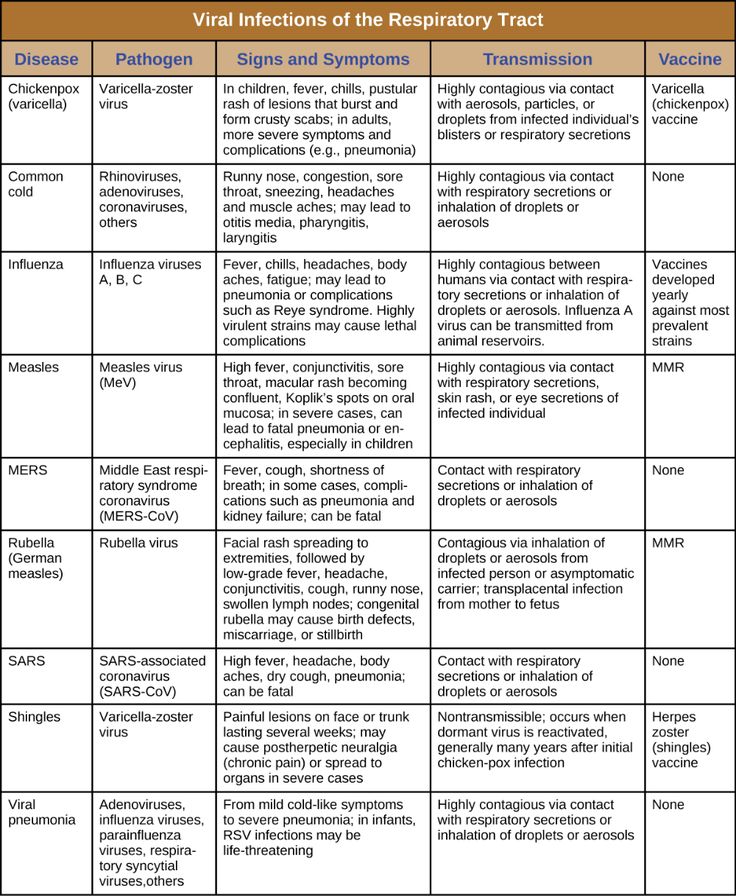
- chickenpox
- eczema
- erythema multiforme
- hand, foot and mouth disease
- impetigo
- keratosis pilaris ("chicken skin")
- measles
- molluscum contagiosum
- pityriasis rosea
- prickly heat
- psoriasis
- ringworm
- scabies
- scarlet fever
- slapped cheek syndrome
- urticaria (hives)
Although meningitis has become less common over recent years, it's important to be aware of the rash and the other signs and symptoms of meningitis.
Cellulitis
Cellulitis is an infection of the deeper layers of skin and underlying tissue. The affected area will be red, painful, swollen and hot. It often affects the legs, but can occur anywhere on the body. Your child will probably also have a fever.
See your GP immediately if an area of your child's skin suddenly turns red, hot and tender. If you can't see your GP on the same day, go to a walk-in centre or minor injuries unit.
Cellulitis can usually be diagnosed by assessing the symptoms and examining the skin. It usually responds well to treatment with antibiotics.
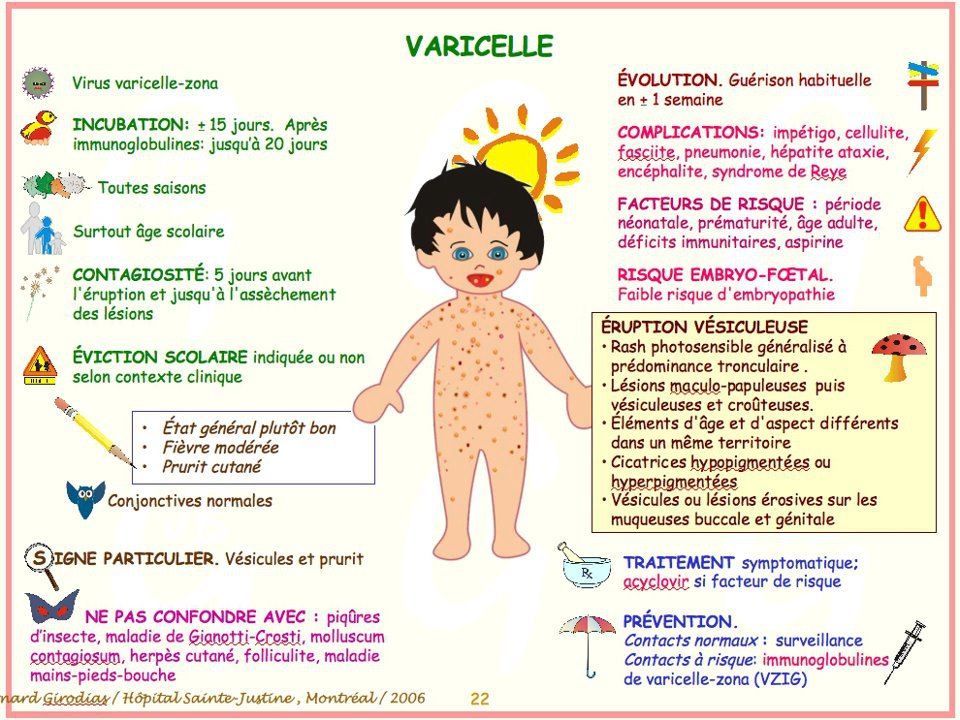
Chickenpox
Chickenpox is a viral illness that most children catch at some point. It most commonly affects children under 10 years of age.
A rash of itchy spots turns into fluid-filled blisters. They crust over to form scabs, which after a while drop off. Some children only have a few spots, whereas others have them over their entire body. The spots are most likely to appear on the face, ears and scalp, under the arms, on the chest and belly, and on the arms and legs.
There's no specific treatment for chickenpox, but you can take steps to relieve the symptoms. For example, paracetamol can help relieve fever (don't give aspirin to children under 16), and calamine lotion and cooling gels can be used to ease itching.
Read more about treating chickenpox.
Eczema
Eczema is a long-term condition that causes the skin to become itchy, red, dry and cracked. The most common type is atopic eczema, which mainly affects children but can continue into adulthood.
Atopic eczema commonly develops behind the knees or on the elbows, neck, eyes and ears. It isn't a serious condition, but if your child later becomes infected with the herpes simplex virus, it can cause the eczema to flare up into an outbreak of tiny blisters called eczema herpeticum, and will cause a fever.
About one in five children in the UK has eczema, and in eight out 10 cases it develops before the age of five, often before a child's first birthday.
Read about treating atopic eczema.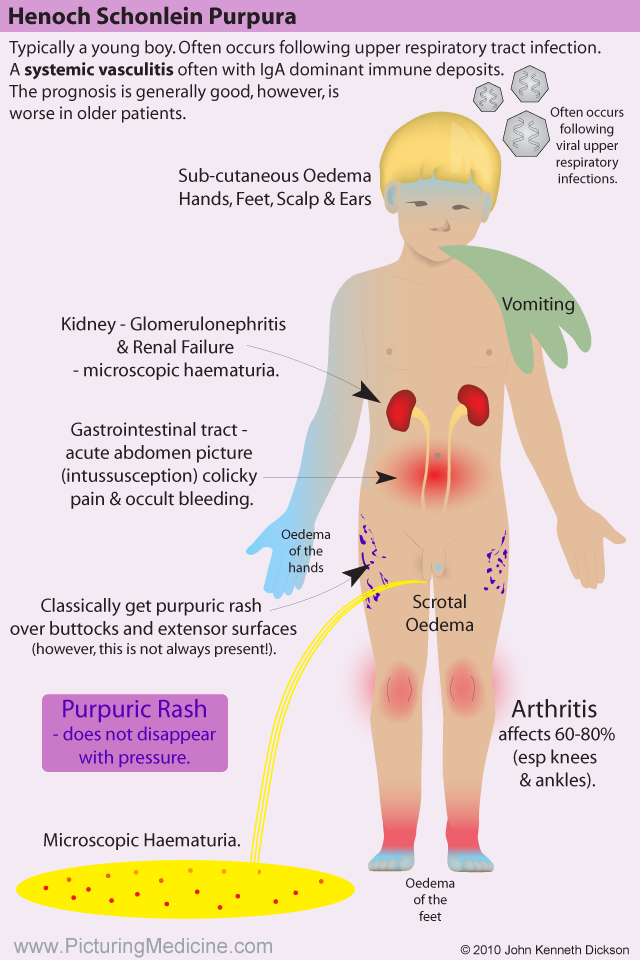
Erythema multiforme
Erythema multiforme is a skin rash (usually mild) that's caused by an allergic reaction to the herpes simplex virus.
The spots look like targets, with a dark red centre and paler ring around the outside. The hands or feet tend to be affected first, followed by the limbs, upper body and face.
Your child will probably feel unwell and may have a fever, which you should be able to treat with over-the-counter medicine. It may take from two to six weeks before they feel better. See your GP if your child has a rash and seems unwell.
In rare cases, erythema multiforme can be triggered by a reaction to certain medications, such as an antibiotic or anticonvulsant. This more severe form is called Stevens-Johnson syndrome and it can be life-threatening.
Hand, foot and mouth disease
Hand, foot and mouth disease is a common, contagious infection that causes mouth ulcers and spots and blisters on the palms of the hands and soles of the feet.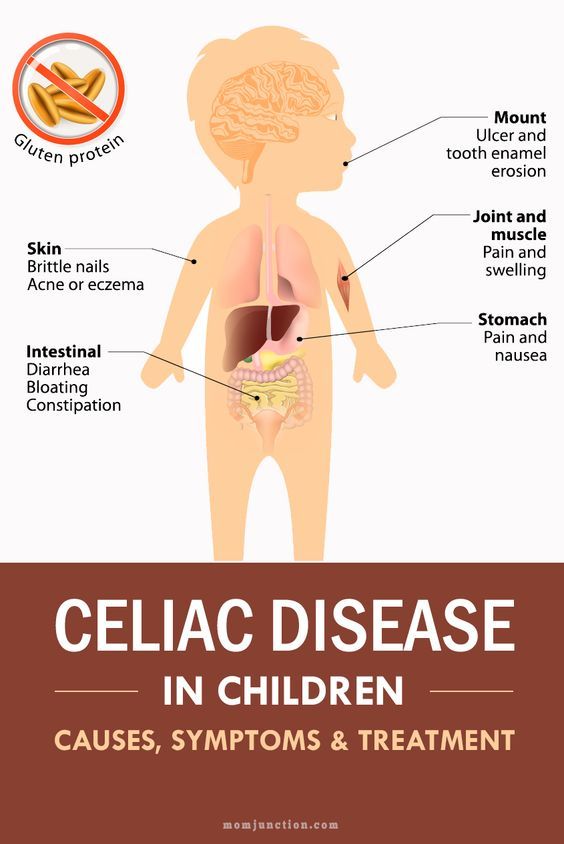
It's most common in young children (particularly those under 10), but it can also affect older children and adults.
There's no cure for hand, foot and mouth disease and it's easily spread, so you should keep your child away from school or nursery until they're better. Your child's immune system will fight the virus and it should clear up after about seven to 10 days.
Make sure your child drinks plenty of fluid, and if eating and swallowing is uncomfortable, give them soft foods, such as mashed potatoes, yoghurt and soup.
Impetigo
Impetigo is a common and highly contagious skin infection that causes sores and blisters. It isn't usually serious and often improves within a week of treatment. There are two types of impetigo called non-bullous and bullous.
Non-bullous impetigo typically affects the skin around the nose and mouth, causing sores that quickly burst to leave a yellow-brown crust.
Bullous impetigo typically affects the trunk (the area of the body between the waist and neck), and causes fluid-filled blisters that burst after a few days to leave a yellow crust.
See your GP or pharmacist if you think your child has impetigo. Antibiotics, in the form of a cream or tablets, will be prescribed. This should reduce the length of the illness to around seven to 10 days.
Keratosis pilaris ("chicken skin")
Keratosis pilaris is a common and harmless skin condition. The skin on the back of the upper arms becomes rough and bumpy, as if covered in permanent goose pimples. Sometimes, the buttocks, thighs, forearms and upper back can also be affected.
Keratosis pilaris typically begins in childhood and gets worse during puberty. Some people find it improves after this and may even disappear in adulthood.
There's no cure for keratosis pilaris, and it often gets better on its own without treatment. However, there are some measures you can take that may improve your child's rash, such as using non-soap cleansers rather than soap, and an emollient to moisturise their skin. Your GP or pharmacist will be able to recommend a suitable cream.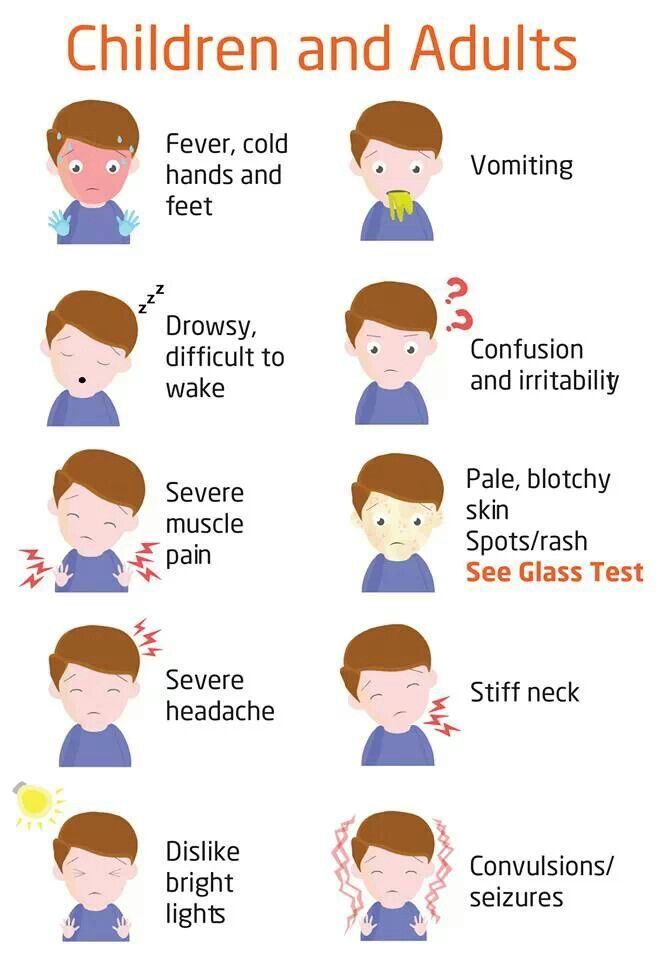
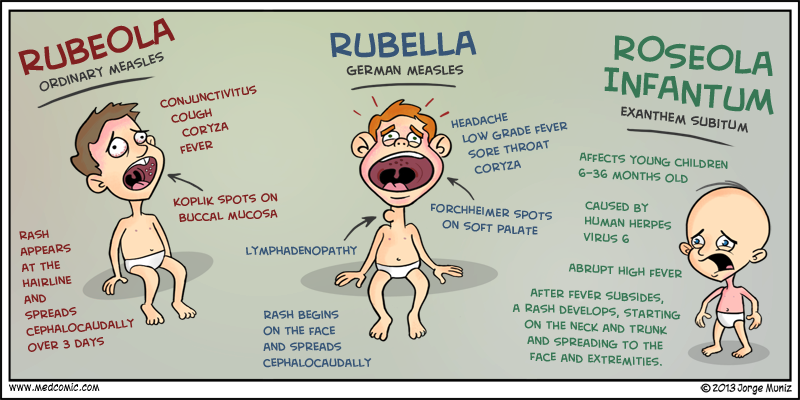
Measles
Measles is a highly infectious illness that most commonly affects young children. It's now rare in the UK because of the effectiveness of the measles, mumps and rubella (MMR) vaccine.
The measles rash is red-brown blotches. It usually starts on the head or upper neck and then spreads outwards to the rest of the body. Your child may also have a fever and cold-like symptoms.
Call your GP surgery immediately if you think your child has measles. It's best to phone before visiting because the surgery may need to make arrangements to reduce the risk of spreading the infection to others.
Measles usually passes in about seven to 10 days without causing further problems. Paracetamol or ibuprofen can be used to relieve fever, aches and pains (don't give aspirin to children under 16). Also, make sure your child drinks plenty of water to avoid dehydration.
Read more about treating measles.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that causes clusters of small, firm, raised spots to develop on the skin.
It commonly affects young children aged one to five years, who tend to catch it after close physical contact with another infected child.
The condition is usually painless, although some children may experience some itchiness. It usually goes away within 18 months without the need for treatment.
Molluscum contagiosum is highly infectious. However, most adults are resistant to the virus, which means they're unlikely to catch it if they come into contact with it.
Pityriasis rosea
Pityriasis rosea is a relatively common skin condition that causes a temporary rash of raised, red scaly patches to develop on the body. Most cases occur in older children and young adults (aged between 10 and 35).
The rash can be very itchy. In most cases, it clears up without treatment in 2 to 12 weeks, although in rare cases it can last up to five months.
Emollients, steroid creams and antihistamines can be used to help relieve the itchiness. The rash doesn't usually leave scars, although the skin can sometimes be discoloured afterwards.
Prickly heat (heat rash)
Prickly heat (heat rash), also known as miliaria, is an itchy rash of small, raised red spots that causes a stinging or prickly sensation on the skin.
It occurs when the sweat ducts in the outer layer of skin (epidermis) are obstructed. You can get a heat rash anywhere on your body, but the face, neck, back, chest or thighs are most often affected.
Infants can sometimes get a prickly heat rash if they sweat more than usual – for example, when it's hot and humid or if they're overdressed. It isn't a serious condition and rarely requires any specific treatment.
Psoriasis
Psoriasis is a long-lasting (chronic) skin condition that causes red, flaky, crusty patches of skin covered with silvery scales.
The severity of psoriasis varies greatly from person to person. For some people, it's just a minor irritation, but for others it can have a major impact on their quality of life.
There's no cure for psoriasis, but there are a number of treatments that can help improve the symptoms and appearance of skin patches.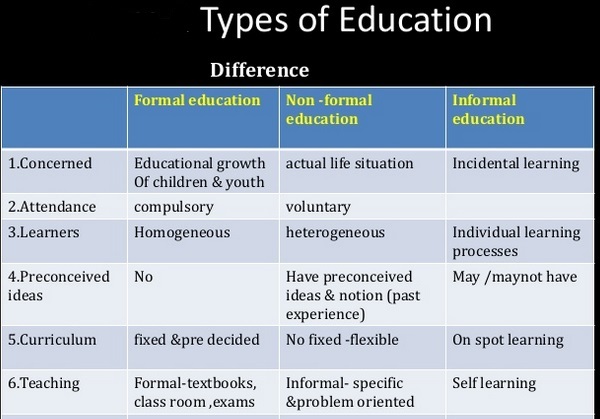 For example, topical corticosteroids are creams and ointments that can be applied to the skin.
For example, topical corticosteroids are creams and ointments that can be applied to the skin.
Ringworm
Ringworm is a highly infectious fungal skin infection that causes a ring-like red or silvery patch on the skin that can be scaly, inflamed or itchy.
Ringworm often affects the arms and legs, but it can appear almost anywhere on the body. Other similar fungal infections can affect the scalp, feet, groin and nails.
Ringworm can usually be easily treated with antifungal medicines, which are available from a pharmacy. Ringworm of the scalp can cause scaling and patches of hair loss. It's treated with antifungal tablets, often combined with antifungal shampoo.
Scabies
Scabies is a contagious skin condition that's intensely itchy. It's caused by tiny mites that burrow into the skin.
In children, scabies is usually spread through prolonged periods of skin-to-skin contact with an infected adult or child – for example, during play fighting or hugging.
The mites like warm places, such as skin folds, between the fingers, under fingernails, or around the buttock creases. They leave small red blotches, which are often found on the palms of the hands or soles of the feet. In infants, blisters are commonly found on the soles of the feet.
See your GP if you think your child has scabies. It's not usually a serious condition, but it does need to be treated. Your GP will prescribe a lotion or cream. Read more about treating scabies.
Scarlet fever
Scarlet fever is a highly contagious bacterial infection that usually affects children between two and eight years of age. It causes a distinctive pink-red rash, which feels like sandpaper to touch and may be itchy.
It often starts with a sore throat, fever and headache, with the rash developing two to five days after infection. The rash usually occurs on the chest and stomach before spreading to other areas of the body, such as the ears and neck.
Scarlet fever usually clears up after about a week, but see your GP if you think your child may have it. Antibiotics are used to treat it (liquid antibiotics, such as penicillin or amoxicillin, are often used to treat children).
Antibiotics are used to treat it (liquid antibiotics, such as penicillin or amoxicillin, are often used to treat children).
Slapped cheek syndrome
Slapped cheek syndrome – also known as fifth disease or parvovirus B19 – is a viral infection that's common in children aged six to 10.
It causes a distinctive bright red rash to develop on both cheeks. This can look alarming, but it usually clears up by itself in one to three weeks.
Unless your child is feeling unwell, they don't need to stay away from school. Once the rash appears, the infection is no longer contagious. However, it's a good idea to notify your child's school about the infection.
Urticaria (hives)
Urticaria – also known as hives, weals, welts or nettle rash – is a raised, itchy rash that can affect one part of the body or be spread across large areas. It's a common skin reaction that often affects children.
Urticaria occurs when a trigger causes high levels of histamine and other chemical messengers to be released in the skin. These substances cause the blood vessels in the skin to open up, resulting in redness or pinkness, and swelling and itchiness.
These substances cause the blood vessels in the skin to open up, resulting in redness or pinkness, and swelling and itchiness.
There are many possible triggers of urticaria, including allergens, such as food or latex, irritants, such as nettles, medicines, and physical factors, such as heat or exercise. Sometimes, a cause can't be identified.
The rash is usually short-lived and mild, and can often be controlled with antihistamines.
12 Common Summertime Skin Rashes in Children
Sunny days and starlit evenings spent playing, splashing, and exploring can leave kids with more than warm summertime memories. Balmy weather also can lead to itchy, irritated skin.
Check out the list from the American Academy of Pediatrics (AAP) to see how you can help prevent, identify, and soothe these common summertime skin rashes.
1. Heat Rash
Heat rash (also known as prickly heat or miliaria) is seen most often in babies and young children when sweat gland pores become blocked and perspiration can't escape.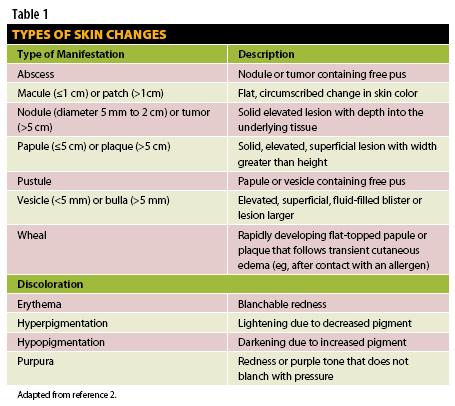 The rash looks like patches of small pink or red bumps or blisters under clothing or spots where skin tends to fold—on the neck, elbows, armpits, or thighs—although heat rash can occur on other covered areas.
The rash looks like patches of small pink or red bumps or blisters under clothing or spots where skin tends to fold—on the neck, elbows, armpits, or thighs—although heat rash can occur on other covered areas.
What parents can do:
Keep kids cool. Dress your child in clothing that keeps the skin cool and dry. If possible, use fans and air conditioning to avoid overheating.
Pay attention to hot spots. Wash areas of the skin that stay wet with sweat, urine, or drool with cool water. Pat them dry.
Keep skin bare. Leave areas open to air without clothing. Do not apply skin ointments.
2. Poison Ivy & Other Plant Rashes
Many children get a burning, intensely itchy rash where their skin touches plants—such as poison ivy, poison oak, sumac—containing a sticky oil called urushiol. An allergic skin reaction causes redness, swelling and blisters. Other plants—such as wild parsnip, giant hogweed, and citrus—contain chemicals that make skin hypersensitive to sunlight and cause a phytophotodermatitis rash.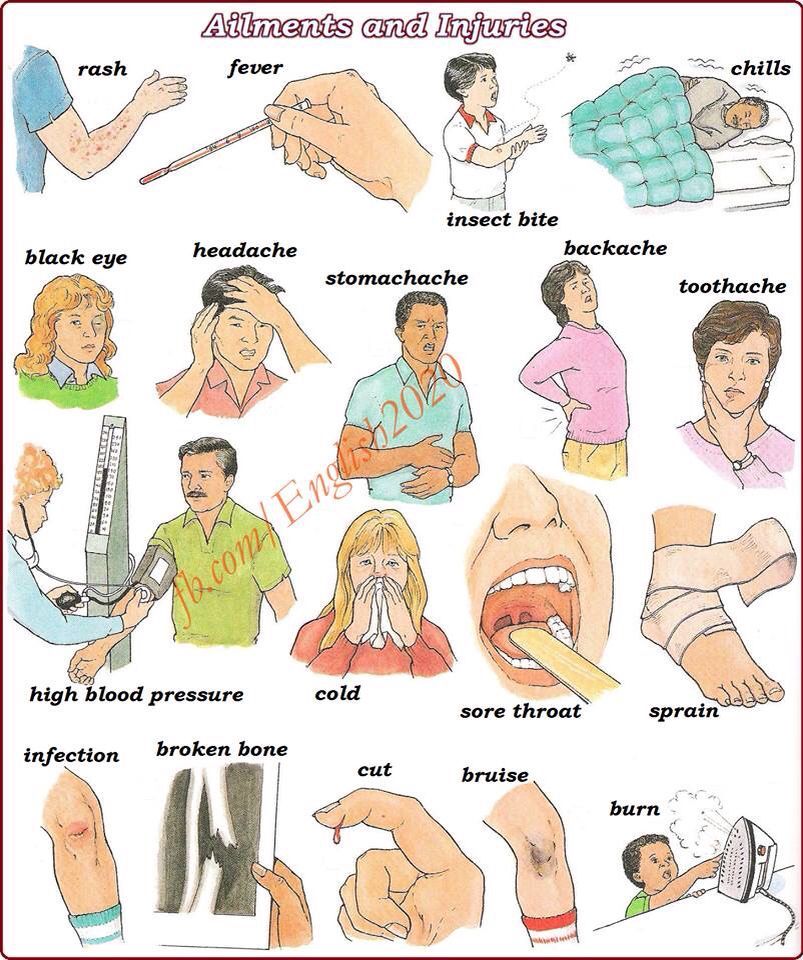
What parents can do:
Prevent exposure. Teach your child what these plants look like and how to avoid them. Both poison ivy and poison oak have shiny green leaves that grow three to a stem, so you might share the rhyme: "Leaves of three, let them be." The sumac shrub has stems that contain 7-13 leaves arranged in pairs, while wild parsnip and giant hogweed have clusters of small, flat-topped yellow and white flowers. If you have younger children, inspect the parks they play in and have rash-causing plants removed.
Wash and trim. If your child comes into contact with these plants, wash all of his or her clothes and shoes in soap and water. Also, wash the area of the skin that was exposed with soap and water for at least 10 minutes after the plant or the oil is touched. To discourage scratching and further damage to the skin, keep your child's fingernails trimmed. This will also prevent the rash from spreading if there is still a small amount of oil under the fingernails.
Soothing salves. If the rash is mild, apply calamine lotion to cut down on the itching. Avoid ointments containing anesthetics or antihistamines—they can cause allergic reactions themselves. Another good option to reduce skin inflammation is 1% hydrocortisone cream.
Talk with your pediatrician. While mild cases can be treated at home, talk with your pediatrician if your child is especially uncomfortable, the rash is severe and/or isn't going away, if the rash is on your child's face or groin area, or if you notice signs of infection (i.e., fever, redness, swelling beyond the poison ivy or oak lesions).
3. Eczema
Eczema (also called atopic dermatitis or AD) is a chronic condition common in children that causes patches of dry, scaly red skin and tends to flare up during colder months when there's less moisture in the air. But dryness caused by air conditioning and pressurized planes during summer travel can cause problems, too. Overheating, sweating and chlorine in swimming pools also can trigger eczema.
Overheating, sweating and chlorine in swimming pools also can trigger eczema.
What parents can do:
Moisturize. Apply fragrance-free creams or ointments at least once a day or more often if needed. After a bath or swimming, gently pat your child's skin with a towel and then apply moisturizer to his or her damp skin.
Dress wisely. Choose clothing made of soft, breathable fabrics like cotton when possible. Wash clothes in a detergent free of irritants such as perfumes and dyes.
Don't scratch. Keep your child's fingernails short and smooth, and remind him or her not to scratch. Scratching can make the rash worse and lead to infection.
Talk with your pediatrician. Ask your child's pediatrician if allergies, sometimes triggered by trees and plants that bloom during summer, could be a cause of the eczema. Your child's pediatrician may recommend medicines to help your child feel better and to keep the symptoms of eczema under control.
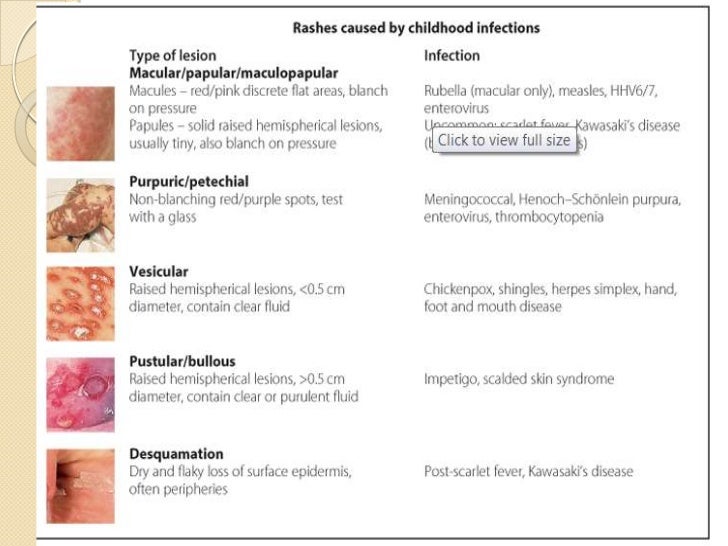
4. Insect Bites & Stings
Insects such as bees, wasps, mosquitos, fire ants, and ticks can cause itching and minor discomfort where they prick the skin. For some children, insect bites and stings can cause a severe allergic reaction called anaphylaxis—which includes a rash or hives and life-threatening symptoms such as airway swelling. (For children with a known allergy to insect bites and stings, it is important to have anaphylaxis emergency care plan in place). Other times, diseases spread by insects such as Lyme Disease, Rocky Mountain Spotted Fever, and Zika Virus can cause rashes and other health problems.
What parents can do:
Avoidance. When spending time outdoors, avoid scented soaps and shampoos and brightly colored clothing—they can attract insects. If possible, steer clear of areas where insects nest and gather (i.e., stagnant pools of water, uncovered food, and blooming flowers).
Use insect repellent. Products with DEET can be used on the skin, but look for family-friendly products that contain concentrations of no more than 30% DEET. Wash the insect repellent off with soap and water when your child returns indoors.
Cover up. When in wooded areas or in or near tall grass, stay on cleared trails as much as possible. Have your child wear a long-sleeved shirt, pants, and hat. Avoid wearing sandals in an area where ticks may live.
Look closely. Wear light-colored clothing to make it easier to spot ticks. After coming indoors, check for ticks on your child's skin—they often hide behind the ears or along the hairline.
Remove stingers and ticks. To remove a visible stinger from skin, gently scrape it off horizontally with a credit card or your fingernail. If you find a tick, gently grasp it with fine-tipped tweezers as close to the skin as possible.
 Without squeezing the tick's body, slowly pull it away from the skin. See How To Remove A Tick for more information.
Without squeezing the tick's body, slowly pull it away from the skin. See How To Remove A Tick for more information. Clean the skin. After the stinger or tick is out, clean the bitten area with rubbing alcohol or other first aid ointment.
Treat swelling. Apply a cold compress or an ice pack to any swelling for at least 10 minutes.
Help relieve the itch. Applying ice, along with calamine lotion or 1% hydrocortisone cream, can also help relieve itching.
5. Impetigo
Impetigo is a bacterial skin infection that's more common during hot, humid weather. It causes a rash that may have fluid-filled blisters or an oozing rash covered by crusted yellow scabs. Impetigo is more likely to develop where there is a break in the skin, like around insect bites.
What parents can do:
Clean and cover. Clean the infected area with soap and water.
 Cover the infected area loosely to help prevent contact that would spread the infection to others or to other parts of the body. Wash your own hands well after treating your child's sores.
Cover the infected area loosely to help prevent contact that would spread the infection to others or to other parts of the body. Wash your own hands well after treating your child's sores. Avoid scratching. Trim your child's fingernails and discourage scratching. A child can spread the infection to other parts of his or her body by scratching. You can cover the rash loosely with a bandage to discourage your child from touching the rash, but make sure air can flow through so the skin can heal.
Talk with your pediatrician. While mild cases may respond to over-the-counter antibiotics such as bacitracin or bacitracin-polymyxin, impetigo is usually treated with prescription antibiotics—either a skin cream or oral medication. Your pediatrician may order a skin culture (test of your child's skin) to determine which bacteria are causing the rash.
6. Swimmer's Itch
Swimmer's itch (also called clam digger's itch or cercarial dermatitis) may appear after playing in lakes, oceans, and other bodies of water.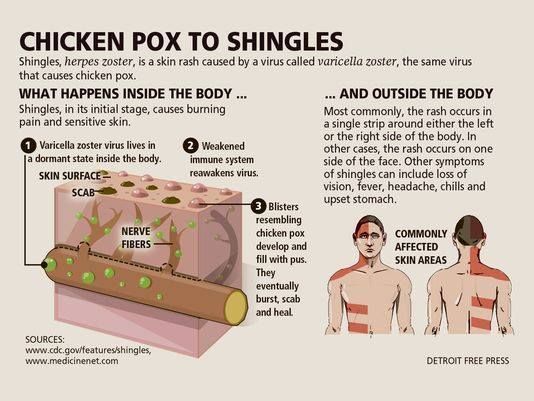 The rash is caused by microscopic parasites found in shallow, warmer water near the shoreline where children tend to stay. The parasites burrow into skin, and cause tiny reddish, raised spots on skin not covered by the swimsuit to appear. Welts and blisters may also form.
The rash is caused by microscopic parasites found in shallow, warmer water near the shoreline where children tend to stay. The parasites burrow into skin, and cause tiny reddish, raised spots on skin not covered by the swimsuit to appear. Welts and blisters may also form.
What parents can do:
Be aware. Don't swim near or wade in marshy areas where snails are commonly found. Try not to attract birds (by feeding them, for example) where your family swims. Birds may eat the snails and spread the parasites in the water.
Shower or towel dry. Shower or briskly rub the skin with a towel immediately after getting out of the water. The parasites start to burrow when the water on skin begins evaporating. If your skin child's skin stings with rubbing—and the rash appears under the swimsuit—he or she may instead have Seabather's Eruption from stinging larvae of sea critters such as jellyfish or sea anemone. Stop rubbing and shower instead.

Don't scratch. Trim your child's fingernails and discourage scratching. Home treatments such cool compresses on the affected areas, Epsom salt or oatmeal baths, or baking soda paste may help to relieve the discomfort. If itching is severe, talk with your child's pediatrician. He or she may suggest prescription-strength lotions or creams to reduce your child's symptoms.
7. Cutaneous Larva Migrans (Sandworms)
Sandworms may be present in sand contaminated with feces from pets or stray animals. When a child stands or sits in contaminated sand on a beach or in a sandbox, the worms may burrow under the skin, usually around the feet or buttocks. Lines of itchy, reddish rash known as a creeping eruption appear as the worms move under the skin, up to a few centimeters a day. The condition is more common subtropical and tropical areas such as the Caribbean, as well as parts of the southwestern United States.
What parents can do:
Keep shoes on.
 Don't let your child play on beaches where people walk their dogs. If your family goes on an outing to a designated pet-friendly beach, make sure your child keeps shoes on and doesn't sit in the sand without a blanket or towel.
Don't let your child play on beaches where people walk their dogs. If your family goes on an outing to a designated pet-friendly beach, make sure your child keeps shoes on and doesn't sit in the sand without a blanket or towel.Talk with your pediatrician. Your pediatrician can prescribe anti-parasitic medications such as albendazole or ivermectin to treat the rash. Without treatment, the larvae usually will die off in 5 to 6 weeks. Your pediatrician may suggest a cream to help relieve itching.
8. Folliculitis (Hot Tub Rash)
Folliculitis (hot tub rash) is an itchy, pimply rash that occurs when bacteria in unclean pools and hot tubs gets into hair follicles on the skin. The area where hairs grow from the skin becomes infected and inflamed, sometimes forming small, pus-filled blisters. A similar rash may come from wearing a damp swimsuit that wasn't washed and dried well after previous use. Hot rub rash typically starts 12-48 hours after being in a hot tub.
What parents can do:
Avoid dirty pools. If you're unsure whether the acid and chlorine levels are properly controlled in a heated pool, don't allow your child to go in.
Don't allow young children in spas or hot tubs. In addition to the risk for drowning and overheating, young children are also at higher risk of bacterial skin infection because they tend to spend more time in the water than teens or adults.
Talk with your pediatrician. Hot tub rash usually clears up without medical treatment. In the meantime, warm compresses and an over-the-counter anti-itch cream recommended by your pediatrician can help your child be more comfortable. If your child's rash lasts more than a few days, talk with your pediatrician.
9. Molluscum Virus
Molluscum contagiosum is a viral infection that causes pearly bumps on the skin on a child's chest, back, arms or legs. The dome-shaped bumps, also known as "water warts," may have a dimple in the center.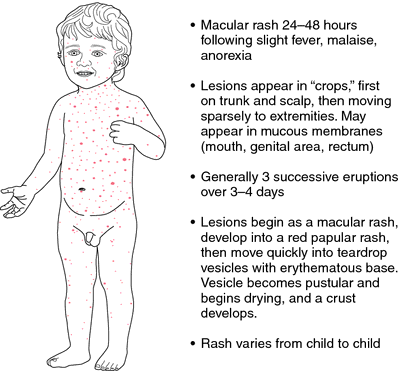 The poxvirus that causes the bumps is more common in hot, humid climates. Some studies suggest the infection may spread in contaminated swimming pools.
The poxvirus that causes the bumps is more common in hot, humid climates. Some studies suggest the infection may spread in contaminated swimming pools.
What parents can do:
Wait it out. In most cases, molluscum contagiosum does not need treatment. The bumps usually will go away in 6 to 12 months.
Stop the spread. A child with molluscum contagiosum should not share towels, bedding, or clothing with others to avoid spreading the virus. The bumps are contagious as long as they are present.
Avoid scratching. Scratching the bumps can spread the virus and cause a second, bacterial infection where the skin is open.
10. Juvenile Plantar Dermatosis (Sweaty Sock Syndrome)
A smooth, reddened rash on your child's feet, sometimes with peeling, cracking skin or scaly skin, could be from a condition called Juvenile Plantar Dermatosis (Sweaty Sock Syndrome). It happens when feet get wet and then dry quickly, again and again—like when shoes are taken on and off coming in and out of the house during summer.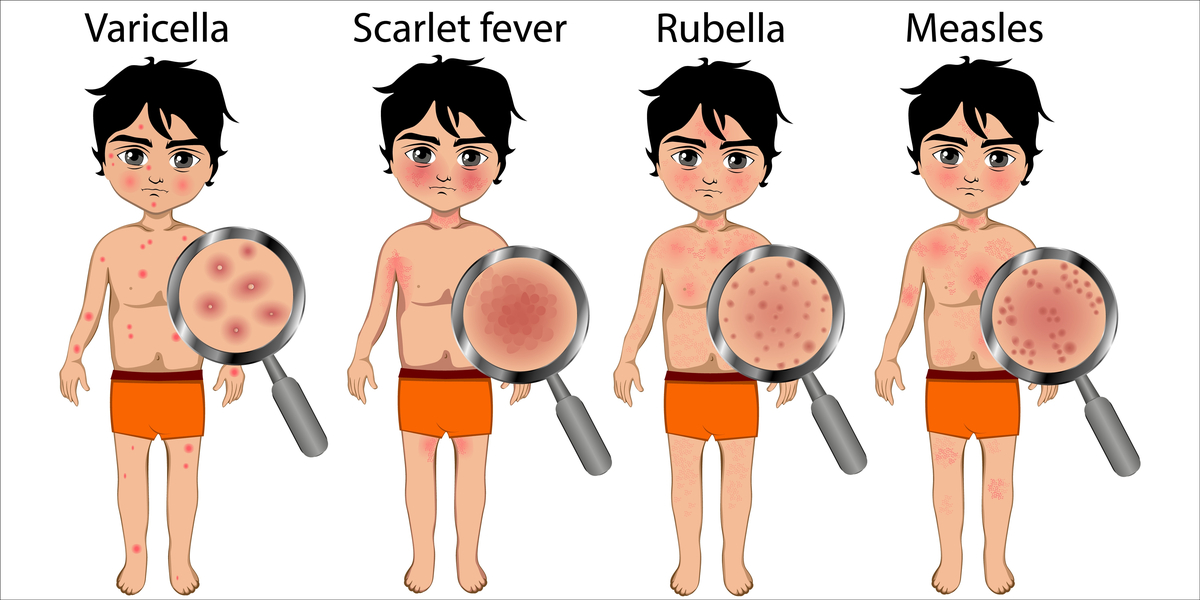
What parents can do:
Breathable footwear. Reduce how often the feet go from wet to dry quickly by having your child wear open or more breathable footwear made of materials like mesh or cotton (i.e., water shoes) and/or thicker more absorbent socks.
Apply ointment. Applying moisturizing ointment or an over-the-counter steroid cream to the affected areas of your child's foot immediately after taking shoes off or getting out of water can help. If the condition does not improve, or if you notice any sign of infection where your child's skin is cracking, talk to your pediatrician.
11. Tinea (Ringworm)
Despite having "worm" in its misleading name, tinea (ringworm) is an infection caused by a fungus that thrives in warm, damp conditions. It is similar to athlete's foot and jock itch and can appear on a child's scalp or other parts of the body. It's called ringworm because the rash from the infection tends to form round or oval spots that become smooth in the center as they grow while the border remains red and scaly.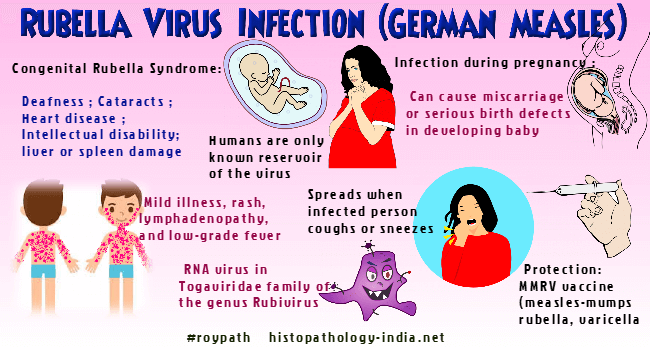 The fungus can spread quickly among student athletes, especially during sweaty, summertime practices and games, when they share sports equipment and locker rooms.
The fungus can spread quickly among student athletes, especially during sweaty, summertime practices and games, when they share sports equipment and locker rooms.
What parents can do:
Stop the spread. Check and treat any pets that may have the fungus—look for scaling, itchy, hairless areas on their fur. Family members, playmates, or schoolmates who show symptoms also should be treated. Do not allow your child to share combs, brushes, hair clips, barrettes, or hats. Make sure mats used in sports like wrestling and gymnastics are properly disinfected after use.
Talk with your pediatrician. A single ringworm patch on the body can be treated with an over-the-counter cream recommended by your pediatrician. If there are any patches on the scalp or more than one on the body, or if the rash is getting worse while being treated, your pediatrician may prescribe a stronger medication and special shampoo.
12.
 Hand, Foot & Mouth Disease
Hand, Foot & Mouth DiseaseMany parents assume virus season winds down after winter. But some viral illnesses, such as hand, foot, and mouth disease, are more common during summer and early fall. Outbreaks are most common in younger children and can spread in child care centers, preschools, and summer camps. Caused by Enterovirus coxsackie, the illness starts with a fever, sore throat, and runny nose—much like the common cold—but then a rash with tiny blisters may appear on any or all the following places on the body:
In the mouth (inner cheeks, gums, sides of the tongue or back of the mouth)
Fingers or palms of hands
Soles of feet
Buttocks
Symptoms are the worst in the first few days, but they are usually gone within a week. Peeling skin on the fingers, toes, and nails may begin after a week or two, but it is harmless. Parents of children with a history of atopic dermatitis or eczema should be aware that their children may be prone to a more severe outbreak.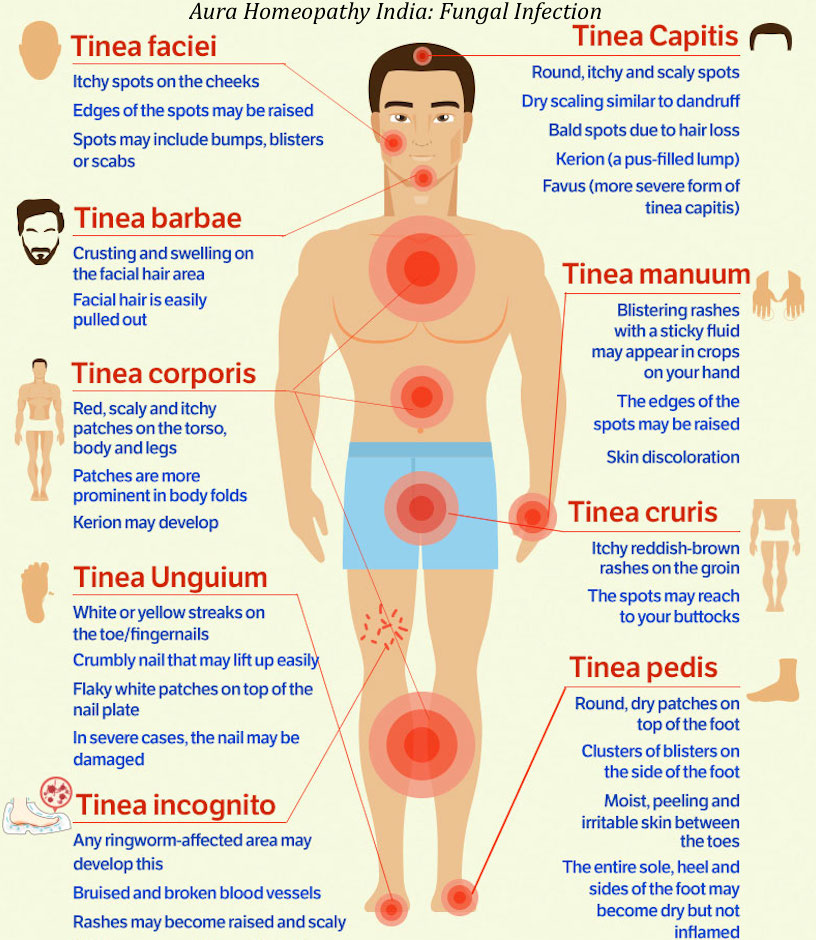
What parents can do:
Monitor symptoms. Be sure to call your pediatrician if your child's fever lasts more than 3 days or if he or she is not drinking fluids. If symptoms are severe, your pediatrician may collect samples from your child's throat for lab testing.
Ease the pain. For fever and pain, the pediatrician may also recommend acetaminophen or ibuprofen. Liquid mouth-soothing remedies may be useful to alleviate mouth ulcer pain. Do not use regular mouthwashes, because they sting.
Avoid dehydration: Children with hand, foot, and mouth disease need to drink plenty of fluids. Call your pediatrician or go to the ER if you suspect your child is dehydrated. See Signs of Dehydration in Infants & Children for more information.
Inform others. Tell child care providers and playmates' parents to watch for symptoms of the illness.
 Children with hand, foot, and mouth disease may spread the virus through the respiratory tract (nose, mouth and lungs) for 1-3 weeks, and in the stool for weeks to months after the infection starts. Once a child's fever has gone away and he or she is feeling better, there is no need to keep him or her home unless there are still open and oozing blisters. See When to Keep Your Child Home from Child Care for more information.
Children with hand, foot, and mouth disease may spread the virus through the respiratory tract (nose, mouth and lungs) for 1-3 weeks, and in the stool for weeks to months after the infection starts. Once a child's fever has gone away and he or she is feeling better, there is no need to keep him or her home unless there are still open and oozing blisters. See When to Keep Your Child Home from Child Care for more information.
Remember…
Protecting your child's skin is a year-round concern, but it's especially important in the summer months when so much skin is exposed and vulnerable. Fortunately, many summertime rashes clear up quickly on their own. Be sure to talk with your pediatrician about any rash that you're unsure about—especially if you don't know what caused it, if it is making your child feel miserable or doesn't clear up quickly, or if it shows signs of infection or is accompanied by any shortness of breath.
Additional Information:
- Summer Safety Tips: Staying Safe Outdoors
- Antibiotic Prescriptions for Children: 10 Common Questions Answered
- American Academy of Dermatology
- American College of Allergy, Asthma & Immunology
- Society for Pediatric Dermatology
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician.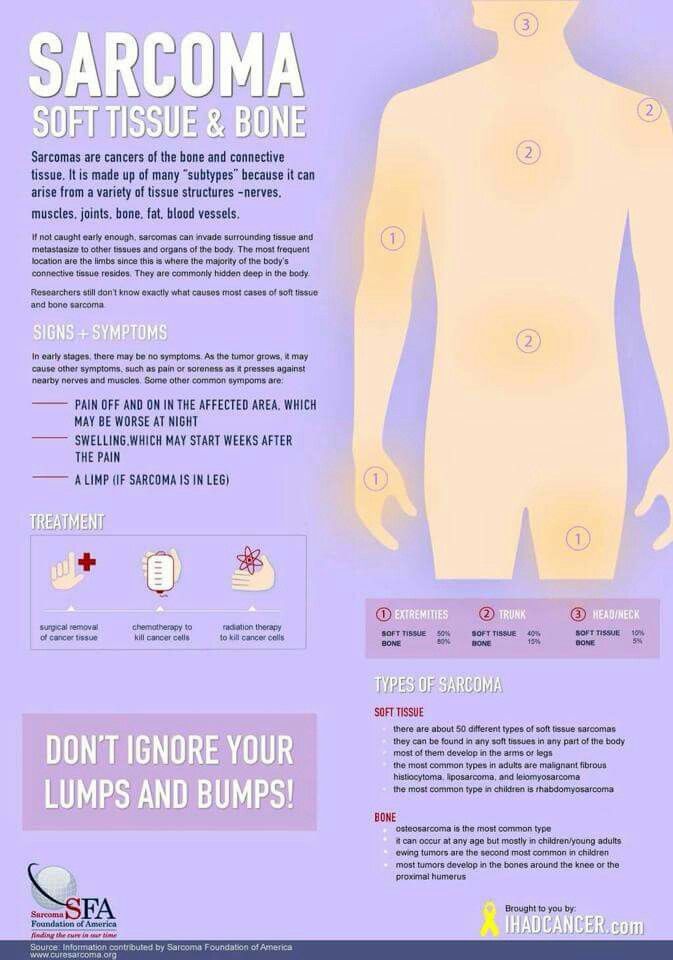 There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Have you noticed a rash on your child's skin? Contact your pediatrician to find out the reason. Redness itself is not a disease, but can signal internal disorders in the body.
In the article we will talk about the causes, types and methods of treating rash in children.
What causes a rash?
Rashes on the skin of a child do not appear just like that. In any case, this is the body's immune response to the influence of external or internal factors. nine0003
Different types of rashes are similar in appearance, especially for parents who are faced with a problem for the first time. But if some spots are completely harmless, then others can threaten health. That is why it is important to understand their origin.
The main causes of the rash:
- Reaction to stimuli.
 If the child is dressed too warmly, the rash may be due to overheating and excessive sweating. Most often, prickly heat occurs on the back, neck, chest and abdomen. The same goes for the diaper. If you do not arrange air baths and do not change it to a new one in time, the skin in the inguinal region and on the buttocks will disappear. nine0020 Prickly heat does not require special treatment, it is only important to eliminate the irritating factor.
If the child is dressed too warmly, the rash may be due to overheating and excessive sweating. Most often, prickly heat occurs on the back, neck, chest and abdomen. The same goes for the diaper. If you do not arrange air baths and do not change it to a new one in time, the skin in the inguinal region and on the buttocks will disappear. nine0020 Prickly heat does not require special treatment, it is only important to eliminate the irritating factor. - Physiological. In the first months of life, breastfed babies are often diagnosed with infantile acne. With milk, maternal hormones enter the body, which activate the sebaceous glands. As a result, small comedones and pimples appear on the face. Over time, they disappear.
- Viral and bacterial infections. Measles, chicken pox, rubella, herpes simplex virus, roseola, scarlet fever, meningococcal infection, fungus and streptoderma. These diseases are characterized by specific rashes on the arms, legs and other parts of the body.
 Many are accompanied by itching and a steady increase in body temperature for 3-5 days. nine0021
Many are accompanied by itching and a steady increase in body temperature for 3-5 days. nine0021 - Allergy. Urticaria and various types of atopic dermatitis: eczema, diathesis, neurodermatitis. Spots without suppuration may cover the head, face, shoulders, armpits, back and groin.
- Comorbidities. Rash may indicate gastrointestinal, vascular, or kidney problems.
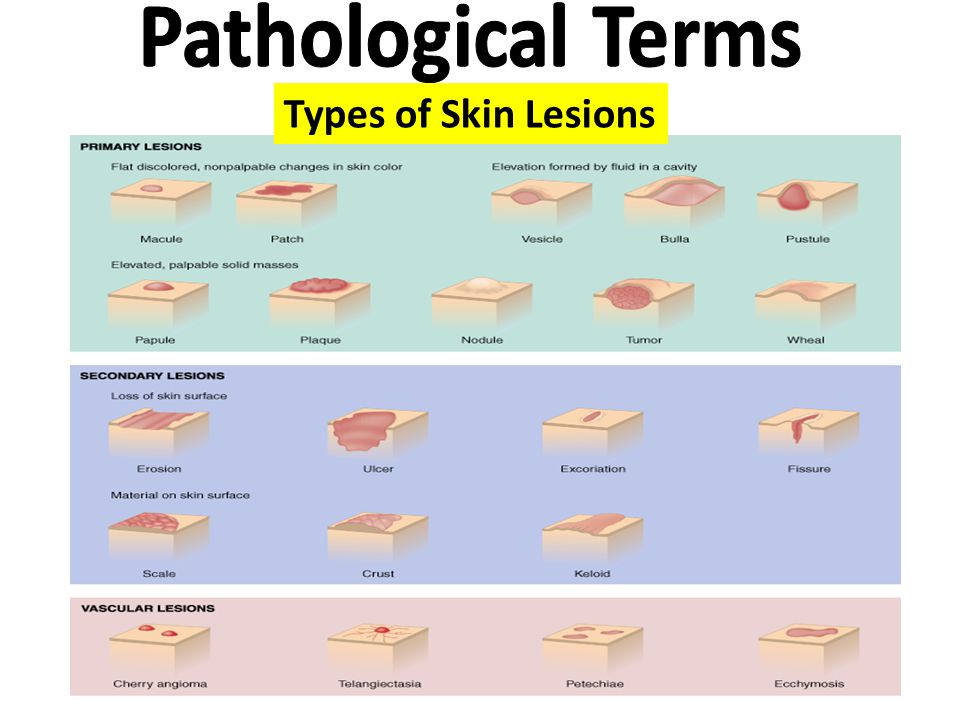
Eruptions in children
Depending on the appearance, localization and size, the following types are distinguished:
- Tubercles. nine0017 Vesicles.
- Blisters.
- Purples.
- Pustules.
- Stains.
- Erythema.
Why are rashes dangerous?
With any kind of redness, it is important to consult a doctor to determine the cause. The most dangerous rash of viral and bacterial origin, especially if there are other symptoms:
- cough;
- sore throat;
- enlarged tonsils and lymph nodes;
- tearing; nine0021
- temperature increase.

Without timely treatment, complications are possible. For example, measles can lead to pneumonia, meningitis, and hearing loss.
With skin allergic reactions, it is important to determine the source of the problem. A neglected allergy can cause swelling and suffocation.
What should parents do?
If you find bumps, vesicles or redness on the child's body, proceed in sequence:
- examine the entire skin; nine0021
- estimate the area and number of lesions;
- check throat, tonsils and take temperature;
- remember what the child ate, did or touched before the redness appeared.
Is the baby already talking? Then try to figure out what's bothering him. Ask about the sensations (spots hurt, itch) and general well-being.
If you have a high temperature, call your doctor at home. It could be a contagious infectious disease that definitely shouldn't be spread. But even if the child looks healthy and vigorous, do not postpone a visit to a specialist - make an appointment at a medical institution. nine0003
nine0003
It is strictly forbidden to self-medicate, comb or squeeze out neoplasms.
Diagnostics
Diagnostic measures help to choose the right therapy. First, the pediatrician prescribes to small patients:
- analysis of blood, urine and feces;
- skin scrapings;
- collection of exudate samples, in the presence of watery formations.
Based on the results, the doctor makes a preliminary conclusion and sends the parents with the child for examination to narrow specialists: an allergist, dermatologist, endocrinologist or gastroenterologist. nine0003
Treatment
Treatment of rashes is carried out in a complex way to eliminate both the symptoms and the cause. A young patient is prescribed anti-allergic, anti-inflammatory or hormonal drugs in the form of tablets, ointments or suspensions.
Along with this, parents are advised to reconsider nutrition and living conditions:
- exclude potentially allergenic products;
- use gentle detergents for the body, dishes and laundry; nine0017 wear loose clothing made from natural fabrics;
- dress the child according to the weather, do not wrap too tightly to avoid overheating;
- change the diaper in a timely manner, arrange air baths and lubricate the groin area with a special cream.
Conclusion
Rashes in a child are a common problem that can bother from birth. Innocent at first glance spots are sometimes a sign of a serious illness. Consult a doctor to determine the cause in time and start treatment. nine0003
GET PRICES
Rash in a child on the body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and medicines! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.