What is an open neural tube defect
What They Are, Causes & Prevention
Overview
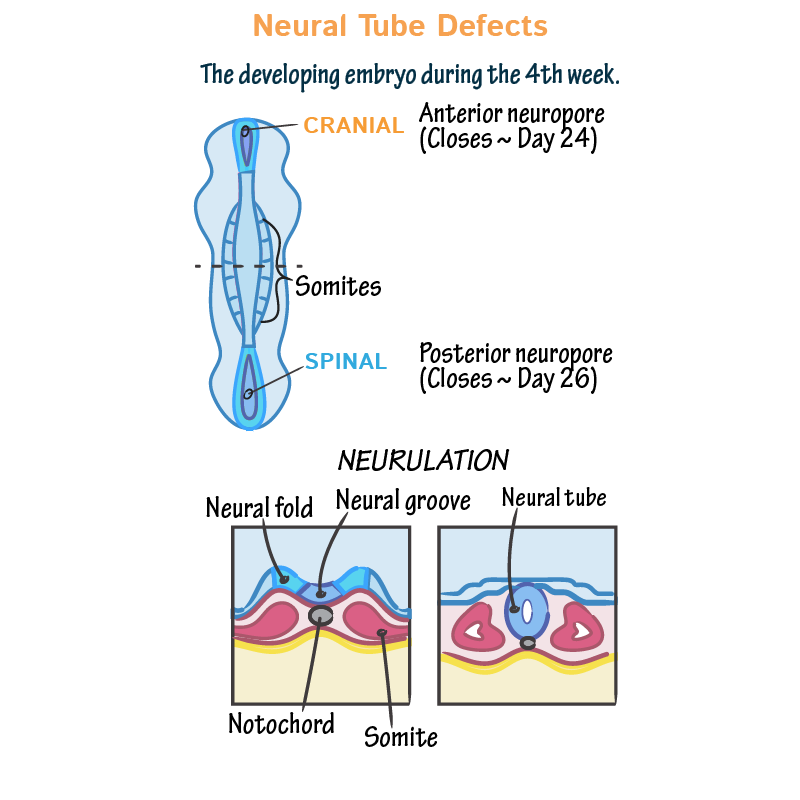
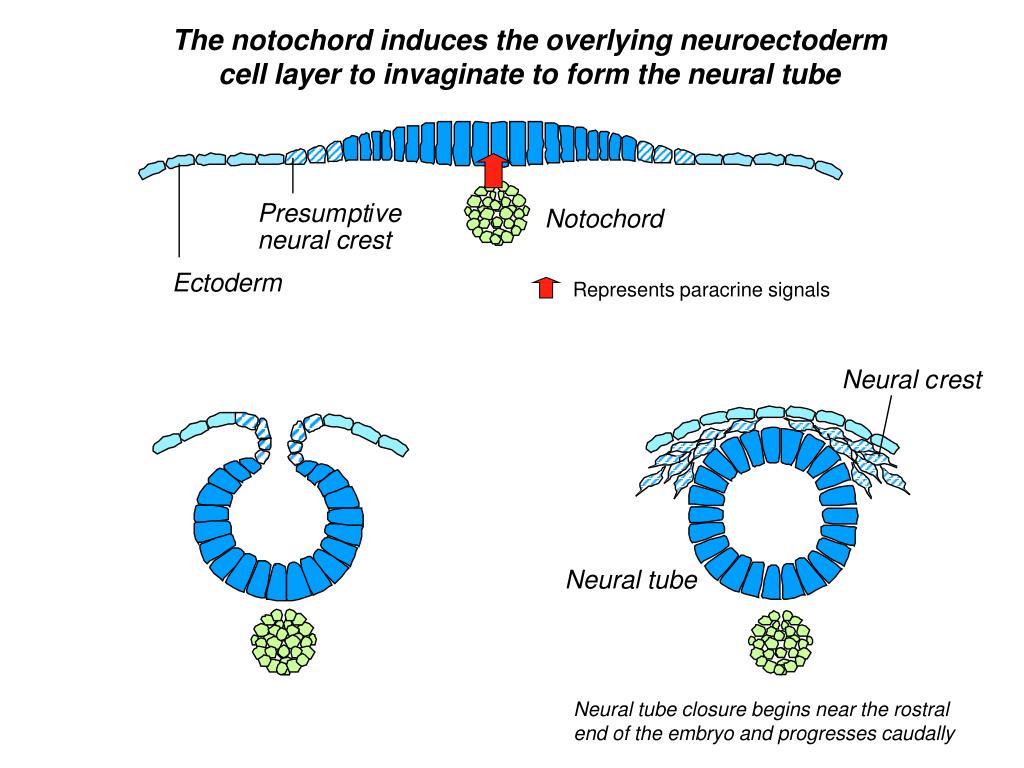
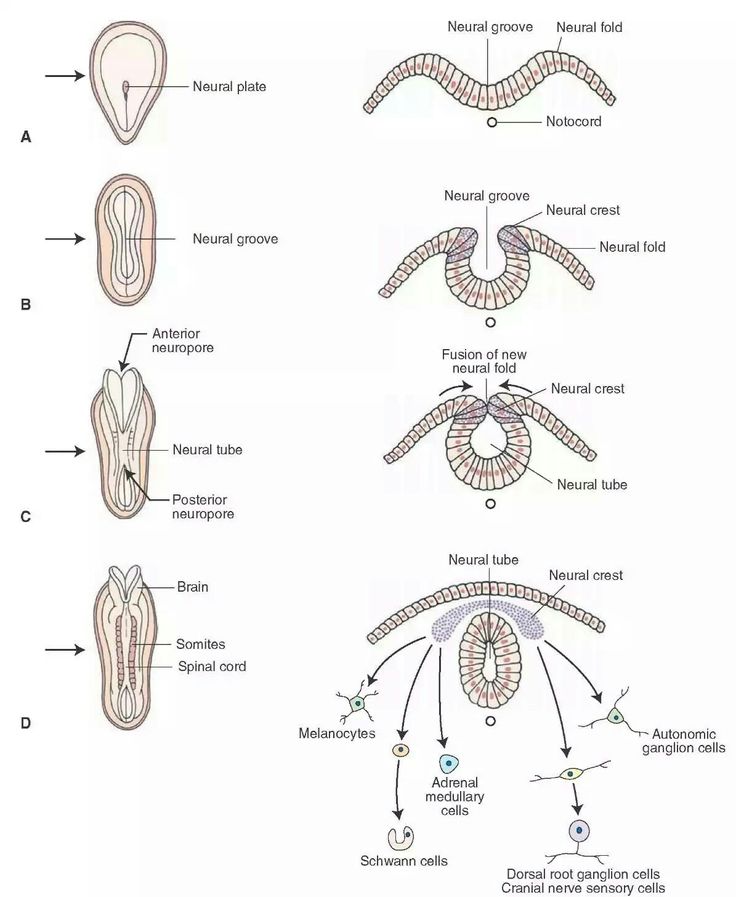
Neural tube defects (NTDs) happen to developing fetuses within the first month of pregnancy. An NTD happens when the neural tube doesn’t close completely somewhere along its length.What is a neural tube defect?
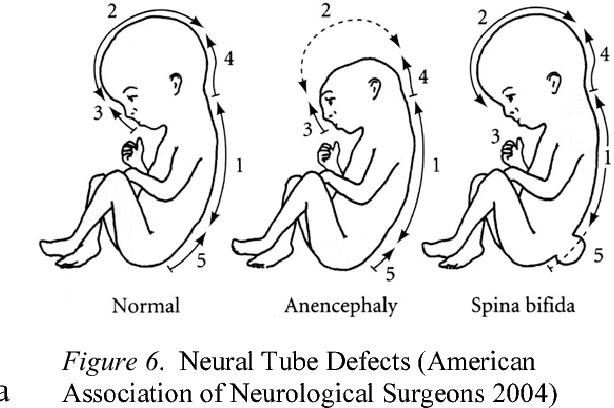
Neural tube defects (NTDs) are birth defects (congenital conditions) of the brain, spine or spinal cord. They happen to developing fetuses within the first month of pregnancy — often before you even know you’re pregnant. The two most common neural tube defects are spina bifida and anencephaly.
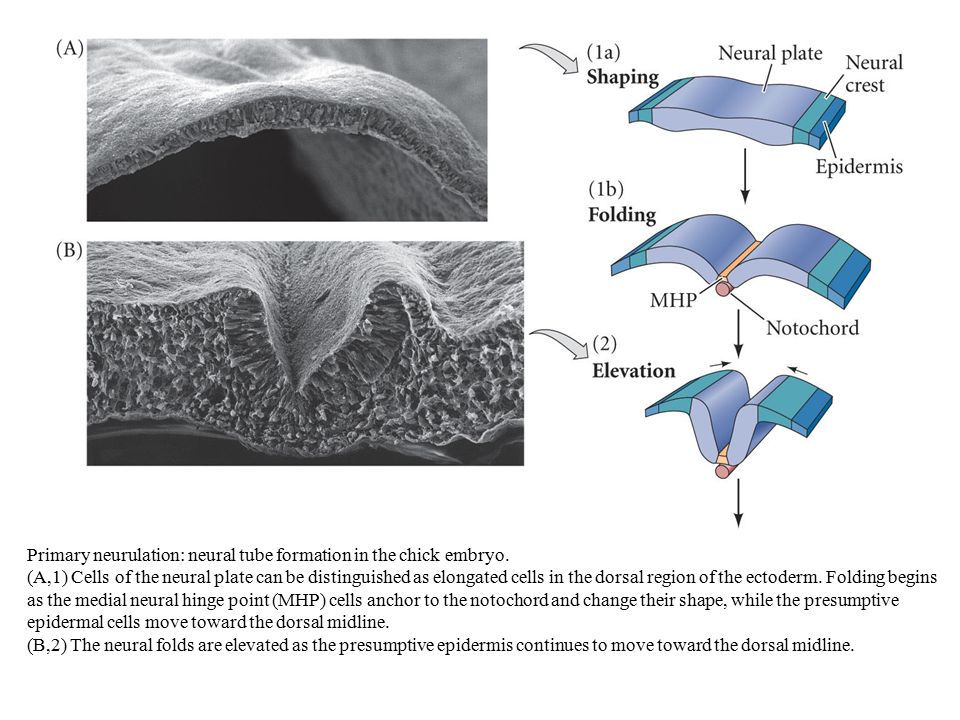
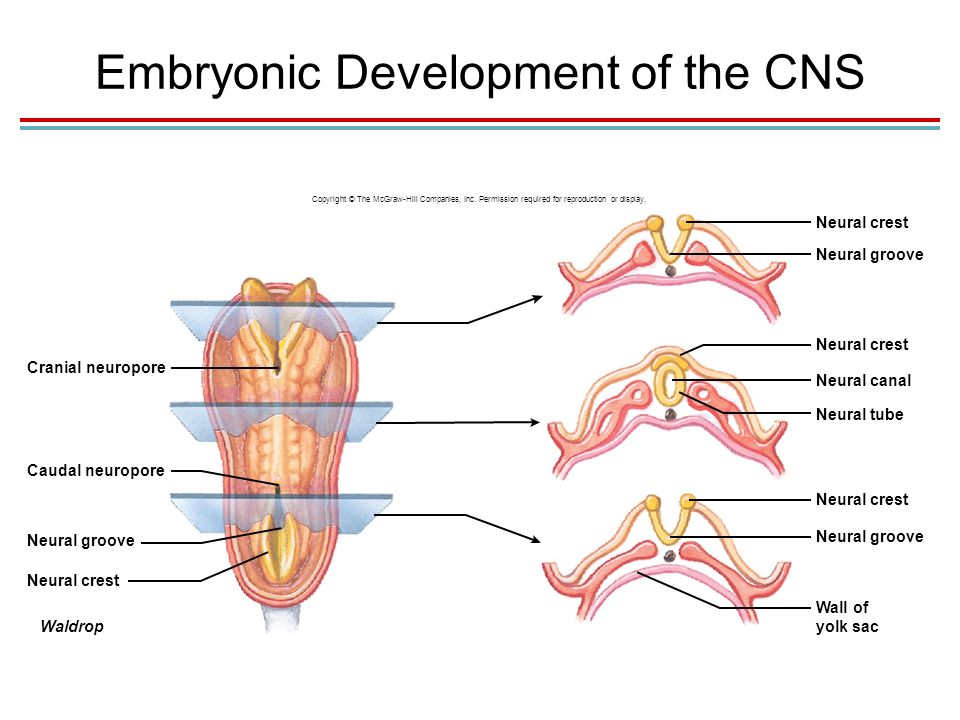
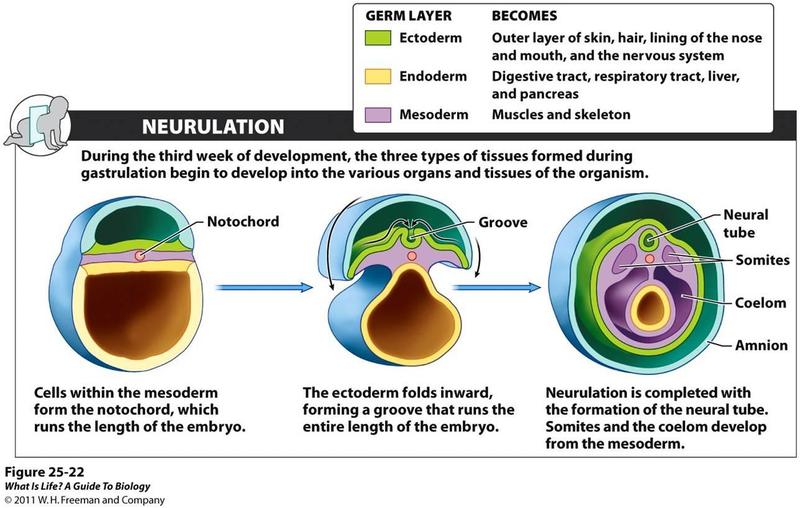
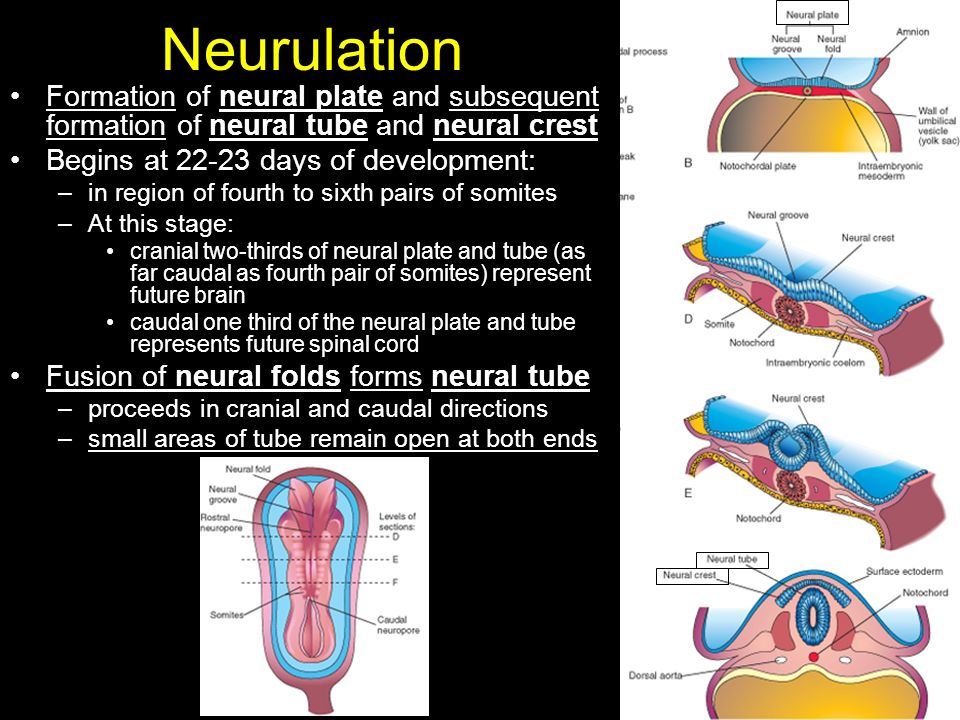
Normally, during your first month of pregnancy, the two sides of the fetus's spine (backbone) join together to cover and protect the spinal cord, spinal nerves and meninges (the tissues covering the spinal cord). At this point, the developing brain and spine are called the neural tube.
As development progresses, the top of the neural tube becomes the brain, and the rest of the tube becomes the spinal cord. An NTD happens when this tube doesn’t close completely somewhere along its length.
What are the types of neural tube defects (NTDs)?
There are several types of neural tube defects, including:
- Spina bifida.
- Anencephaly.
- Encephalocele.
- Iniencephaly.
Spina bifida
Spina bifida is the most common type of neural tube defect (NTD). It happens when the neural tube doesn’t close completely somewhere along the spine during fetal development.
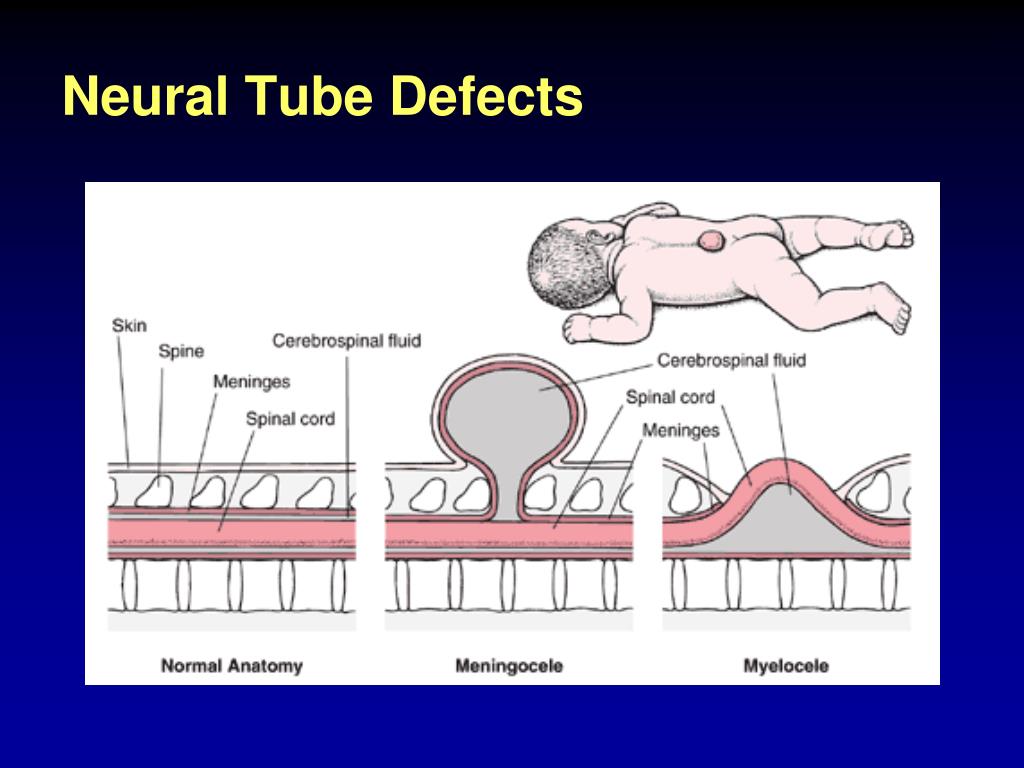
There are a few different types of spina bifida, including:
- Myelomeningocele (open spina bifida): This NTD is characterized by incomplete neural tube closure and a fluid-filled sac that protrudes (sticks out) from your baby’s back. The sac contains part of their spinal cord, meninges, nerves and cerebrospinal fluid (CSF). Myelomeningocele is the most severe and the most common form of spina bifida.
- Meningocele: This NTD is characterized by a sac of fluid that protrudes through an opening in your baby’s back, but their spinal cord is not involved or damaged.
- Spina bifida occulta: This NTD is characterized by a small gap in your baby’s spine, but there isn’t an opening or sac on their back. Their nerves and spinal cord aren’t damaged, and the condition usually doesn’t cause any disability. This is the mildest form of spina bifida.
Anencephaly
Anencephaly happens when the fetus's neural tube doesn’t close at the top during fetal development. This causes the skull, scalp and brain not to develop properly, and portions of the brain and skull are missing. The brain tissue that does form is usually exposed because there isn’t enough skin and bone to cover it. Infants with anencephaly are either stillborn or die soon after birth.
Encephalocele
Encephalocele happens when the neural tube doesn’t close near the brain, and there’s an opening in the skull. The fetus's brain and the membranes that cover it can protrude through the skull, forming a sac-like bulge. In some cases, there’s only a small opening in the nasal cavity or forehead area that’s not noticeable.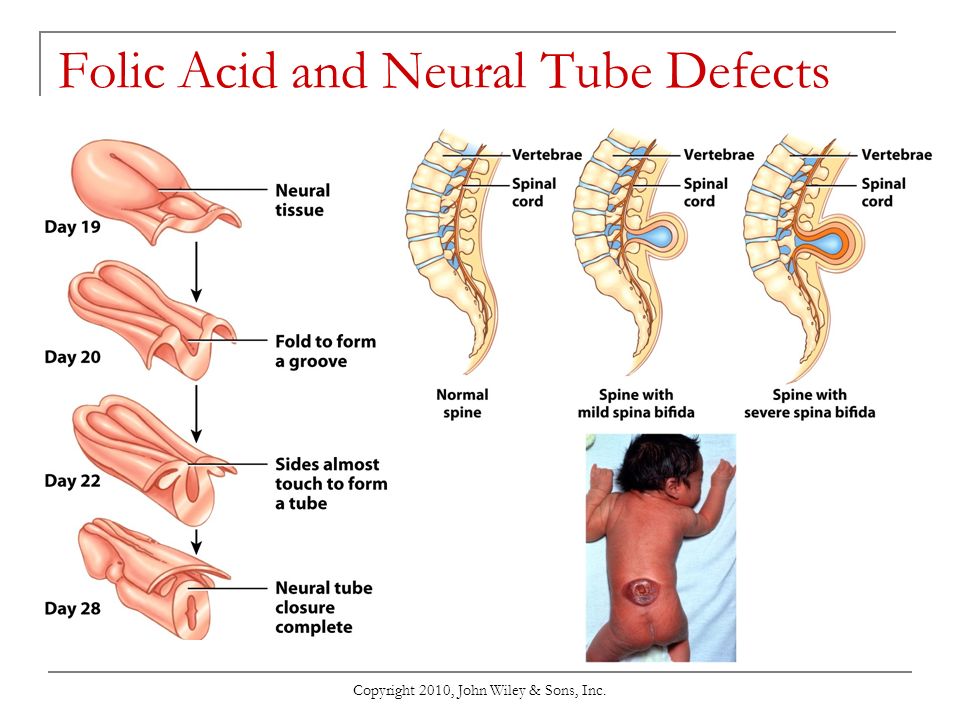
Iniencephaly
Iniencephaly happens when the spine is severely malformed (misshapen). It often causes a lack of a neck, and your baby’s head is bent severely backward. The skin of your baby’s face is connected to their chest, and their scalp is connected to their back. Babies with iniencephaly are usually stillborn.
Who do neural tube defects affect?
Neural tube defects (NTDs) are birth defects (congenital conditions), so they develop in fetuses. NTDs develop within the first month of pregnancy.
How common are neural tube defects?
Neural tube defects (NTDs) occur in about 3,000 pregnancies each year in the United States. To put that into perspective, there were approximately 3,605,000 births in the U.S. in 2020.
The two most common NTDs are spina bifida and anencephaly. Spina bifida affects about 1,500 babies a year in the U.S., with myelomeningocele being the most common form. Anencephaly affects about 1,000 babies each year in the U.S.
Encephalocele and iniencephaly are both rare NTDs.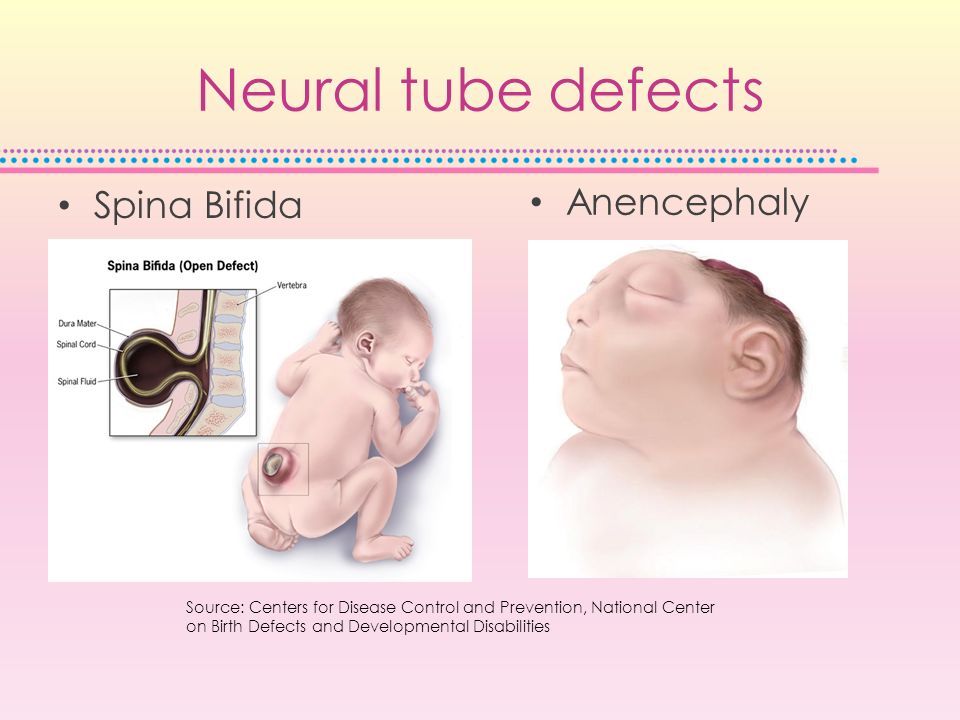
Symptoms and Causes
What causes neural tube defects (NTDs)?
Healthcare providers and scientists don’t yet know the exact cause of neural tube defects (NTDs), but they believe it’s a complex combination of genetic, nutritional and environmental factors.
In particular, low levels of folic acid in a person’s body before and during early pregnancy appear to play a part in this type of congenital condition. Folic acid (or folate) is important for the fetal development of the brain and spinal cord.
What are the symptoms of neural tube defects (NTDs)?
Each type of neural tube defect (NTD) has different symptoms.
Some babies with NTDs have no symptoms, while others experience serious disabilities. Babies with iniencephaly and anencephaly are typically stillborn or die shortly after birth due to complications from the defect.
General symptoms of NTDs can include:
- Physical problems, such as paralysis and urinary and bowel control issues.
- Blindness.
- Deafness.
- Intellectual disability.
- Lack of consciousness and, in some cases, death.
If your healthcare provider suspects that the fetus you're carrying has a neural tube defect, your medical team will be able to provide more information about what to expect. NTDs affect each baby differently.
What are the signs of neural tube defects (NTDs) during pregnancy?
If you’re pregnant with a fetus that has a neural tube defect (NTD), you won’t experience any symptoms directly related to it.
When you undergo a fetal ultrasound, your healthcare provider will look for certain signs of the fetus's health and development depending on its fetal age, including looking for signs of NTDs in the spine and head. Healthcare providers can usually diagnose NTDs with an ultrasound.
Diagnosis and Tests
How are neural tube defects (NTDs) diagnosed?
Healthcare providers typically diagnose neural tube defects (NTDs) during pregnancy through prenatal tests, such as ultrasound.+6.+Deficiencies/disease,+treatment.jpg)
What tests will be done to diagnose neural tube defects (NTDs)?
Healthcare providers use the following tests to help diagnose neural tube defects (NTDs) before birth:
- Blood test: Your healthcare provider will order a screening test that measures the amount of alpha-fetoprotein (AFP) in your blood during the 16th to 18th week of pregnancy. The amount is higher than normal in about 75% to 80% of pregnant people who are carrying a fetus with an NTD. If your level is elevated, your healthcare provider will order other tests, such as an ultrasound, to better evaluate the growing fetus.
- Fetal (prenatal) ultrasound: An ultrasound during pregnancy is the most accurate method to diagnose several NTDs. Healthcare providers typically recommend ultrasounds during the first trimester (11 to 14 weeks of pregnancy) and second trimester (18 to 22 weeks of pregnancy).
- Amniocentesis: Healthcare providers use this test to check for NTDs and other birth defects.
 During amniocentesis, they use a needle to remove a sample of fluid from the amniotic sac that surrounds te fetus. You can get this test at 15 to 20 weeks of pregnancy. This test carries certain risks. Be sure to talk to your healthcare provider about the process.
During amniocentesis, they use a needle to remove a sample of fluid from the amniotic sac that surrounds te fetus. You can get this test at 15 to 20 weeks of pregnancy. This test carries certain risks. Be sure to talk to your healthcare provider about the process.
Healthcare providers also use imaging tests, such as an MRI (magnetic resonance imaging) or CT (computed tomography) scan, to diagnose some NTDs after birth.
Management and Treatment
How are neural tube defects (NTDs) treated?
There are several treatment options for spina bifida and encephalocele depending on the severity of the condition.
There isn’t a treatment for anencephaly or iniencephaly. Infants with these conditions are typically stillborn or die shortly after birth.
Treatment for spina bifida and encephalocele
Treatment for both spina bifida and encephalocele depends on the severity of the condition and if your baby has other complications. Surgery is a common option for both conditions.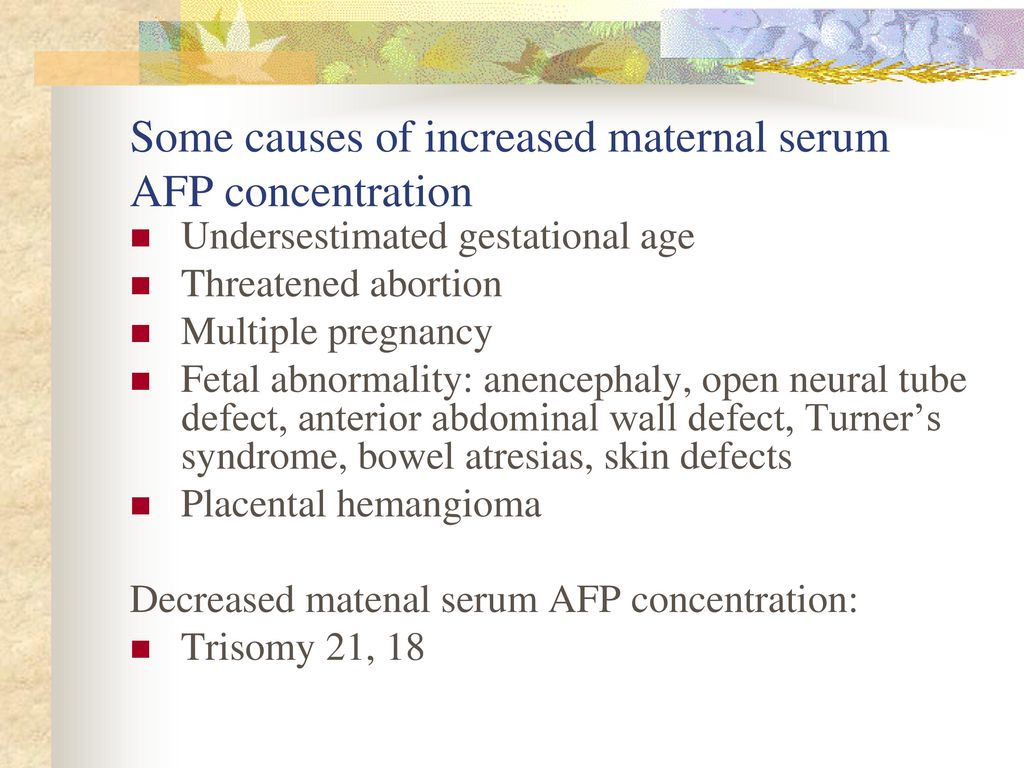
Healthcare providers typically treat encephalocele with surgery to place the protruding part of your baby’s brain and the membranes covering it back into their skull. They then close the opening in your baby’s skull.
Treatment for myelomeningocele, the most common form of spina bifida, typically involves surgery to repair the opening in your baby’s spine. Healthcare providers can perform surgery before birth (fetal surgery) or shortly after birth (postnatal surgery).
Long-term treatment for both conditions depends on your child’s condition. They may need multiple surgeries over time and other treatments related to complications, such as a shunt to treat hydrocephalus (excess fluid surrounding their brain).
Prevention
What are the risk factors for developing a neural tube defect (NTD)?
Any person can have a baby with a neural tube defect (NTD). But certain factors make you more likely to have a baby with an NTD, including:
- Folate (folic acid) deficiency: Folate, the natural form of vitamin B-9, is important for healthy fetal development.
 A folate deficiency before and during pregnancy increases the risk of having a baby with spina bifida and other NTDs. If you’re pregnant or thinking of becoming pregnant, it’s important to take prenatal vitamins to ensure you’re getting enough folate (folic acid) and other nutrients to support a healthy pregnancy. The Centers for Disease Control and Prevention (CDC) recommends all people who can become pregnant take 400 micrograms (mcg) of folic acid every day, in addition to eating food with folate, to help prevent NTDs.
A folate deficiency before and during pregnancy increases the risk of having a baby with spina bifida and other NTDs. If you’re pregnant or thinking of becoming pregnant, it’s important to take prenatal vitamins to ensure you’re getting enough folate (folic acid) and other nutrients to support a healthy pregnancy. The Centers for Disease Control and Prevention (CDC) recommends all people who can become pregnant take 400 micrograms (mcg) of folic acid every day, in addition to eating food with folate, to help prevent NTDs. - Family history of neural tube defects: People who’ve had one baby with an NTD have a 2% to 3% increased risk of having a second baby with an NTD. To learn more about your risk of having a baby with an NTD, consider seeing a genetic counselor.
- Certain antiseizure medications: These medications are linked to neural tube defects when taken during pregnancy. If you take medicine to prevent seizures, talk to your healthcare provider before you get pregnant about how the medicine may affect your pregnancy.
- Diabetes: People with poorly managed diabetes who are pregnant have a higher risk of having a baby with an NTD.
- Obesity: People who have obesity before pregnancy have an increased risk of having a baby with an NTD.
- Increased body temperature in early pregnancy: Increases in core body temperature (hyperthermia) in the early weeks of pregnancy due to a prolonged fever or use of a sauna or hot tub have been associated with a slightly increased risk of NTDs.
- Opioid use in early pregnancy: Opioids are a class of very powerful and highly addictive drugs that reduce pain. People who are pregnant and who’ve taken opioids in the first two months of pregnancy have an increased chance of having a baby with an NTD, in addition to other complications. If you’re pregnant and taking any drugs or medications that may be an opioid, tell your healthcare provider right away.
Outlook / Prognosis
Can a baby live with a neural tube defect?
Yes, your baby can live with certain neural tube defects, including spina bifida and encephalocele.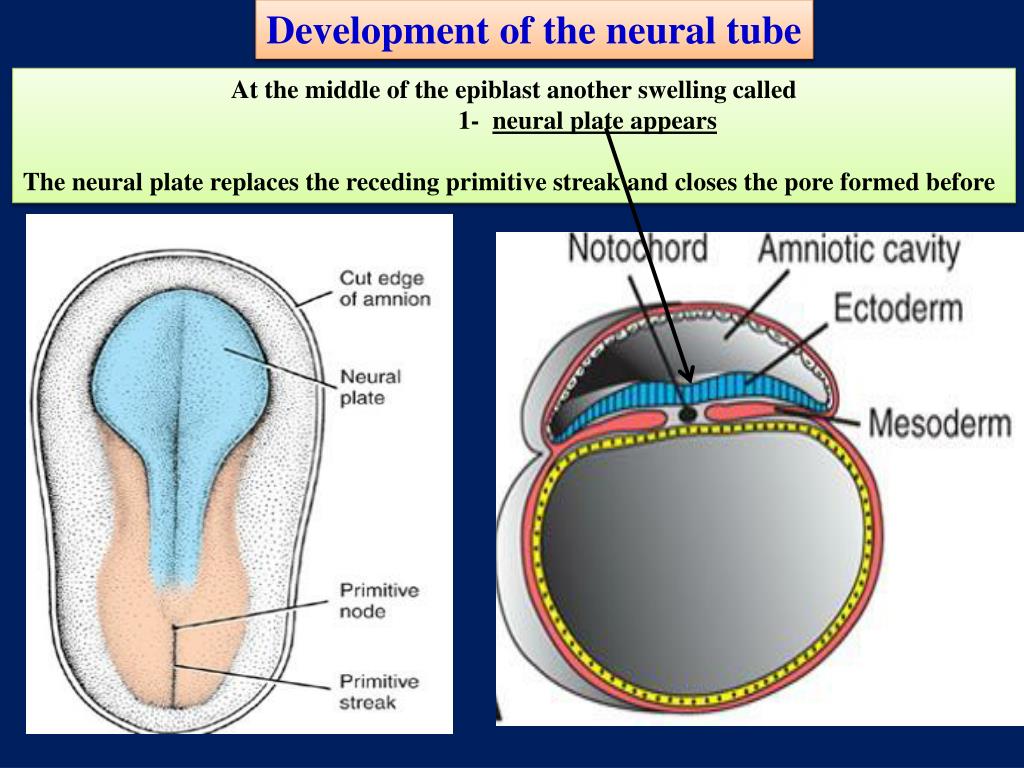
Babies with anencephaly and iniencephaly are typically stillborn or die shortly after birth, however.
What is the prognosis (outlook) for neural tube defects (NTDs)?
For babies with spina bifida, especially myelomeningocele, or encephalocele, there’s a high likelihood of nerve damage, which can cause paralysis and other issues. The nerve damage and loss of function that are present at birth are usually permanent. But there are a number of treatments that can sometimes prevent further damage and help with complications.
Some babies with spina bifida have no or minimal complications.
Living With
How do I take care of my baby with a neural tube defect?
It’s important to remember that no two people with a neural tube defect (NTD), especially spina bifida and encephalocele, are affected in the same way. It’s impossible to predict how your baby will be affected. The best way you can prepare is to talk to healthcare providers who specialize in researching and treating your baby’s condition.
As they grow, your child may benefit from a team of healthcare providers who can care for their needs. It’s important to advocate for your child and to arrange the best medical care possible.
When should I see my healthcare provider about neural tube defects (NTDs)?
If your child was born with a neural tube defect (NTD), they’ll likely need to see their healthcare provider — or team of healthcare providers — regularly throughout their life.
If you take antiseizure medication or opioids, it’s important to talk to your healthcare provider before becoming pregnant about how these medications could affect your pregnancy and the likelihood of having a child with an NTD.
A note from Cleveland Clinic
Learning that the fetus you're carrying has a neural tube defect (NTD) is scary and overwhelming. But know that you’re not alone — many resources are available to help you and your family. It’s important that you speak with a healthcare provider who’s very familiar with neural tube defects so you can learn more about how your baby will be affected and how to prepare.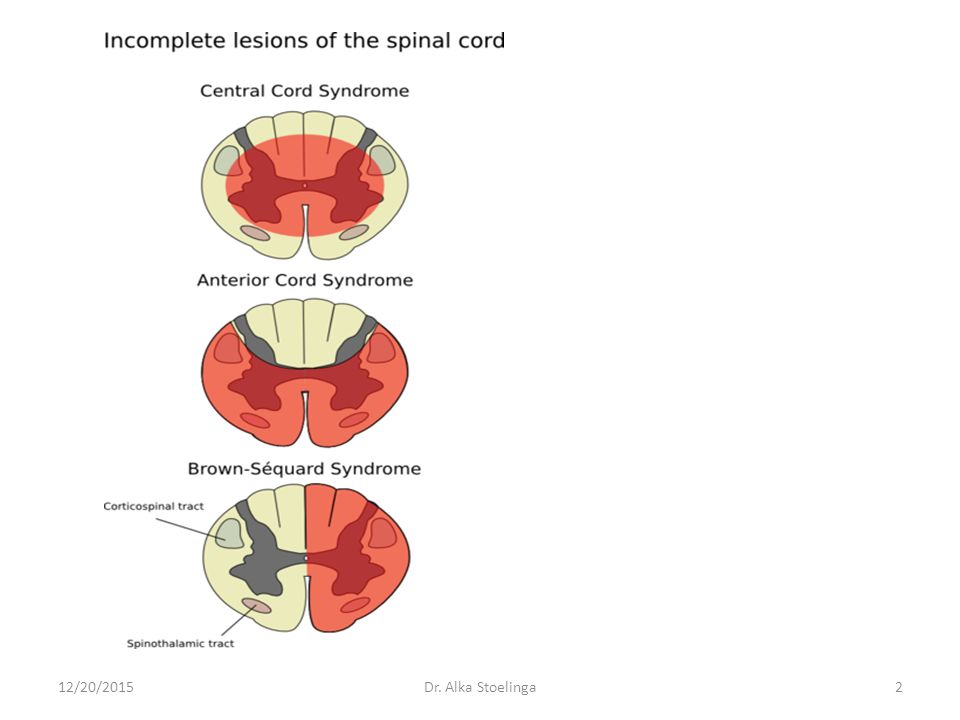
What They Are, Causes & Prevention
Overview
Neural tube defects (NTDs) happen to developing fetuses within the first month of pregnancy. An NTD happens when the neural tube doesn’t close completely somewhere along its length.What is a neural tube defect?
Neural tube defects (NTDs) are birth defects (congenital conditions) of the brain, spine or spinal cord. They happen to developing fetuses within the first month of pregnancy — often before you even know you’re pregnant. The two most common neural tube defects are spina bifida and anencephaly.
Normally, during your first month of pregnancy, the two sides of the fetus's spine (backbone) join together to cover and protect the spinal cord, spinal nerves and meninges (the tissues covering the spinal cord). At this point, the developing brain and spine are called the neural tube.
As development progresses, the top of the neural tube becomes the brain, and the rest of the tube becomes the spinal cord.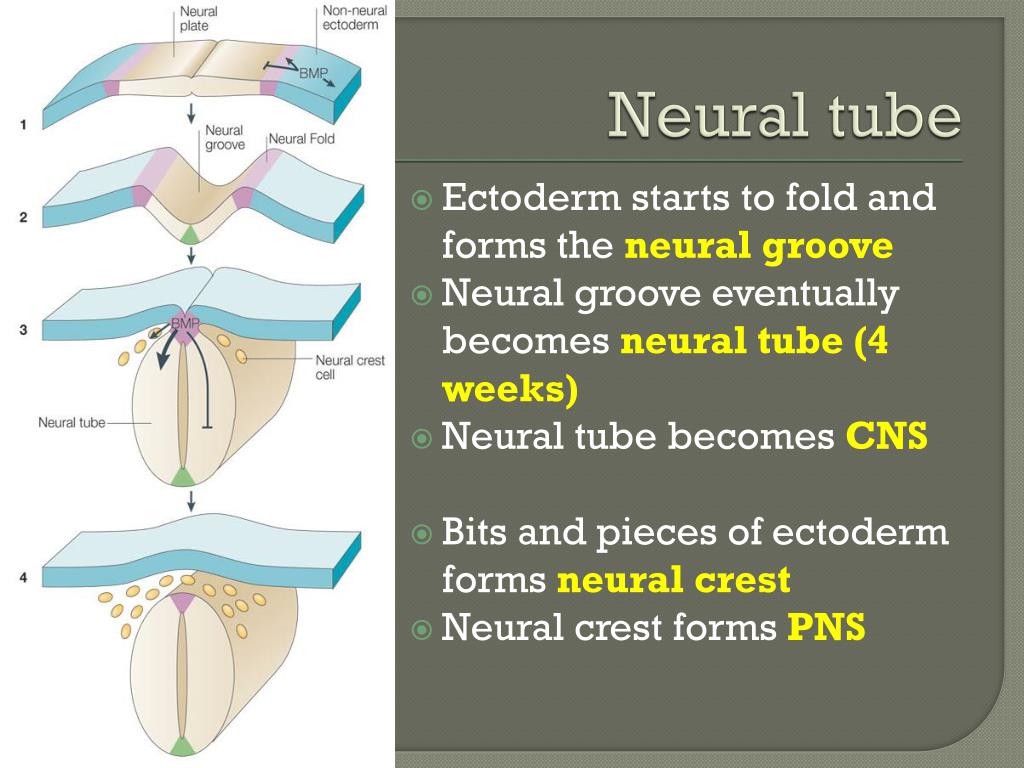 An NTD happens when this tube doesn’t close completely somewhere along its length.
An NTD happens when this tube doesn’t close completely somewhere along its length.
What are the types of neural tube defects (NTDs)?
There are several types of neural tube defects, including:
- Spina bifida.
- Anencephaly.
- Encephalocele.
- Iniencephaly.
Spina bifida
Spina bifida is the most common type of neural tube defect (NTD). It happens when the neural tube doesn’t close completely somewhere along the spine during fetal development.
There are a few different types of spina bifida, including:
- Myelomeningocele (open spina bifida): This NTD is characterized by incomplete neural tube closure and a fluid-filled sac that protrudes (sticks out) from your baby’s back. The sac contains part of their spinal cord, meninges, nerves and cerebrospinal fluid (CSF). Myelomeningocele is the most severe and the most common form of spina bifida.
- Meningocele: This NTD is characterized by a sac of fluid that protrudes through an opening in your baby’s back, but their spinal cord is not involved or damaged.
- Spina bifida occulta: This NTD is characterized by a small gap in your baby’s spine, but there isn’t an opening or sac on their back. Their nerves and spinal cord aren’t damaged, and the condition usually doesn’t cause any disability. This is the mildest form of spina bifida.
Anencephaly
Anencephaly happens when the fetus's neural tube doesn’t close at the top during fetal development. This causes the skull, scalp and brain not to develop properly, and portions of the brain and skull are missing. The brain tissue that does form is usually exposed because there isn’t enough skin and bone to cover it. Infants with anencephaly are either stillborn or die soon after birth.
Encephalocele
Encephalocele happens when the neural tube doesn’t close near the brain, and there’s an opening in the skull. The fetus's brain and the membranes that cover it can protrude through the skull, forming a sac-like bulge. In some cases, there’s only a small opening in the nasal cavity or forehead area that’s not noticeable.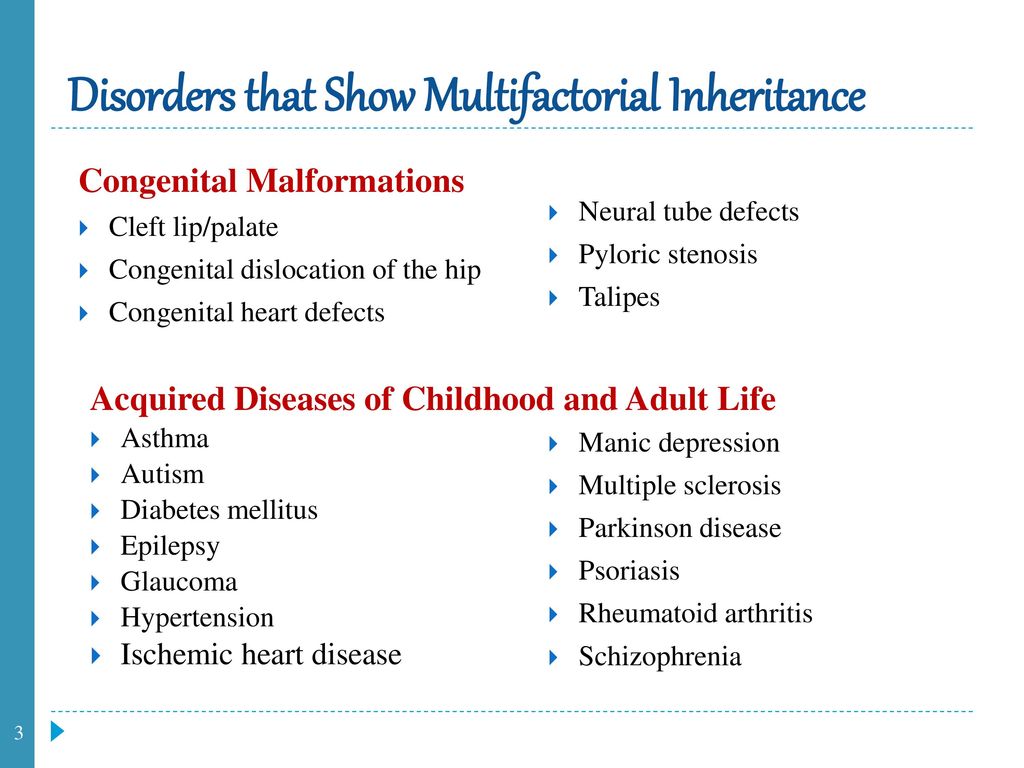
Iniencephaly
Iniencephaly happens when the spine is severely malformed (misshapen). It often causes a lack of a neck, and your baby’s head is bent severely backward. The skin of your baby’s face is connected to their chest, and their scalp is connected to their back. Babies with iniencephaly are usually stillborn.
Who do neural tube defects affect?
Neural tube defects (NTDs) are birth defects (congenital conditions), so they develop in fetuses. NTDs develop within the first month of pregnancy.
How common are neural tube defects?
Neural tube defects (NTDs) occur in about 3,000 pregnancies each year in the United States. To put that into perspective, there were approximately 3,605,000 births in the U.S. in 2020.
The two most common NTDs are spina bifida and anencephaly. Spina bifida affects about 1,500 babies a year in the U.S., with myelomeningocele being the most common form. Anencephaly affects about 1,000 babies each year in the U.S.
Encephalocele and iniencephaly are both rare NTDs.
Symptoms and Causes
What causes neural tube defects (NTDs)?
Healthcare providers and scientists don’t yet know the exact cause of neural tube defects (NTDs), but they believe it’s a complex combination of genetic, nutritional and environmental factors.
In particular, low levels of folic acid in a person’s body before and during early pregnancy appear to play a part in this type of congenital condition. Folic acid (or folate) is important for the fetal development of the brain and spinal cord.
What are the symptoms of neural tube defects (NTDs)?
Each type of neural tube defect (NTD) has different symptoms.
Some babies with NTDs have no symptoms, while others experience serious disabilities. Babies with iniencephaly and anencephaly are typically stillborn or die shortly after birth due to complications from the defect.
General symptoms of NTDs can include:
- Physical problems, such as paralysis and urinary and bowel control issues.
- Blindness.
- Deafness.
- Intellectual disability.
- Lack of consciousness and, in some cases, death.
If your healthcare provider suspects that the fetus you're carrying has a neural tube defect, your medical team will be able to provide more information about what to expect. NTDs affect each baby differently.
What are the signs of neural tube defects (NTDs) during pregnancy?
If you’re pregnant with a fetus that has a neural tube defect (NTD), you won’t experience any symptoms directly related to it.
When you undergo a fetal ultrasound, your healthcare provider will look for certain signs of the fetus's health and development depending on its fetal age, including looking for signs of NTDs in the spine and head. Healthcare providers can usually diagnose NTDs with an ultrasound.
Diagnosis and Tests
How are neural tube defects (NTDs) diagnosed?
Healthcare providers typically diagnose neural tube defects (NTDs) during pregnancy through prenatal tests, such as ultrasound.
What tests will be done to diagnose neural tube defects (NTDs)?
Healthcare providers use the following tests to help diagnose neural tube defects (NTDs) before birth:
- Blood test: Your healthcare provider will order a screening test that measures the amount of alpha-fetoprotein (AFP) in your blood during the 16th to 18th week of pregnancy. The amount is higher than normal in about 75% to 80% of pregnant people who are carrying a fetus with an NTD. If your level is elevated, your healthcare provider will order other tests, such as an ultrasound, to better evaluate the growing fetus.
- Fetal (prenatal) ultrasound: An ultrasound during pregnancy is the most accurate method to diagnose several NTDs. Healthcare providers typically recommend ultrasounds during the first trimester (11 to 14 weeks of pregnancy) and second trimester (18 to 22 weeks of pregnancy).
- Amniocentesis: Healthcare providers use this test to check for NTDs and other birth defects.
During amniocentesis, they use a needle to remove a sample of fluid from the amniotic sac that surrounds te fetus. You can get this test at 15 to 20 weeks of pregnancy. This test carries certain risks. Be sure to talk to your healthcare provider about the process.
Healthcare providers also use imaging tests, such as an MRI (magnetic resonance imaging) or CT (computed tomography) scan, to diagnose some NTDs after birth.
Management and Treatment
How are neural tube defects (NTDs) treated?
There are several treatment options for spina bifida and encephalocele depending on the severity of the condition.
There isn’t a treatment for anencephaly or iniencephaly. Infants with these conditions are typically stillborn or die shortly after birth.
Treatment for spina bifida and encephalocele
Treatment for both spina bifida and encephalocele depends on the severity of the condition and if your baby has other complications. Surgery is a common option for both conditions.
Healthcare providers typically treat encephalocele with surgery to place the protruding part of your baby’s brain and the membranes covering it back into their skull. They then close the opening in your baby’s skull.
Treatment for myelomeningocele, the most common form of spina bifida, typically involves surgery to repair the opening in your baby’s spine. Healthcare providers can perform surgery before birth (fetal surgery) or shortly after birth (postnatal surgery).
Long-term treatment for both conditions depends on your child’s condition. They may need multiple surgeries over time and other treatments related to complications, such as a shunt to treat hydrocephalus (excess fluid surrounding their brain).
Prevention
What are the risk factors for developing a neural tube defect (NTD)?
Any person can have a baby with a neural tube defect (NTD). But certain factors make you more likely to have a baby with an NTD, including:
- Folate (folic acid) deficiency: Folate, the natural form of vitamin B-9, is important for healthy fetal development.
 A folate deficiency before and during pregnancy increases the risk of having a baby with spina bifida and other NTDs. If you’re pregnant or thinking of becoming pregnant, it’s important to take prenatal vitamins to ensure you’re getting enough folate (folic acid) and other nutrients to support a healthy pregnancy. The Centers for Disease Control and Prevention (CDC) recommends all people who can become pregnant take 400 micrograms (mcg) of folic acid every day, in addition to eating food with folate, to help prevent NTDs.
A folate deficiency before and during pregnancy increases the risk of having a baby with spina bifida and other NTDs. If you’re pregnant or thinking of becoming pregnant, it’s important to take prenatal vitamins to ensure you’re getting enough folate (folic acid) and other nutrients to support a healthy pregnancy. The Centers for Disease Control and Prevention (CDC) recommends all people who can become pregnant take 400 micrograms (mcg) of folic acid every day, in addition to eating food with folate, to help prevent NTDs. - Family history of neural tube defects: People who’ve had one baby with an NTD have a 2% to 3% increased risk of having a second baby with an NTD. To learn more about your risk of having a baby with an NTD, consider seeing a genetic counselor.
- Certain antiseizure medications: These medications are linked to neural tube defects when taken during pregnancy. If you take medicine to prevent seizures, talk to your healthcare provider before you get pregnant about how the medicine may affect your pregnancy.

- Diabetes: People with poorly managed diabetes who are pregnant have a higher risk of having a baby with an NTD.
- Obesity: People who have obesity before pregnancy have an increased risk of having a baby with an NTD.
- Increased body temperature in early pregnancy: Increases in core body temperature (hyperthermia) in the early weeks of pregnancy due to a prolonged fever or use of a sauna or hot tub have been associated with a slightly increased risk of NTDs.
- Opioid use in early pregnancy: Opioids are a class of very powerful and highly addictive drugs that reduce pain. People who are pregnant and who’ve taken opioids in the first two months of pregnancy have an increased chance of having a baby with an NTD, in addition to other complications. If you’re pregnant and taking any drugs or medications that may be an opioid, tell your healthcare provider right away.
Outlook / Prognosis
Can a baby live with a neural tube defect?
Yes, your baby can live with certain neural tube defects, including spina bifida and encephalocele.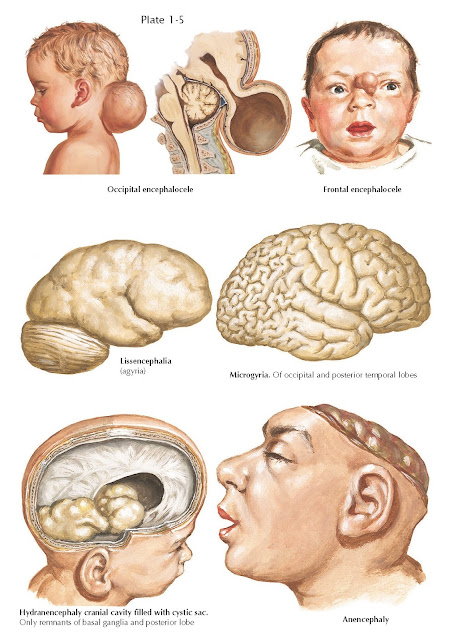
Babies with anencephaly and iniencephaly are typically stillborn or die shortly after birth, however.
What is the prognosis (outlook) for neural tube defects (NTDs)?
For babies with spina bifida, especially myelomeningocele, or encephalocele, there’s a high likelihood of nerve damage, which can cause paralysis and other issues. The nerve damage and loss of function that are present at birth are usually permanent. But there are a number of treatments that can sometimes prevent further damage and help with complications.
Some babies with spina bifida have no or minimal complications.
Living With
How do I take care of my baby with a neural tube defect?
It’s important to remember that no two people with a neural tube defect (NTD), especially spina bifida and encephalocele, are affected in the same way. It’s impossible to predict how your baby will be affected. The best way you can prepare is to talk to healthcare providers who specialize in researching and treating your baby’s condition.
As they grow, your child may benefit from a team of healthcare providers who can care for their needs. It’s important to advocate for your child and to arrange the best medical care possible.
When should I see my healthcare provider about neural tube defects (NTDs)?
If your child was born with a neural tube defect (NTD), they’ll likely need to see their healthcare provider — or team of healthcare providers — regularly throughout their life.
If you take antiseizure medication or opioids, it’s important to talk to your healthcare provider before becoming pregnant about how these medications could affect your pregnancy and the likelihood of having a child with an NTD.
A note from Cleveland Clinic
Learning that the fetus you're carrying has a neural tube defect (NTD) is scary and overwhelming. But know that you’re not alone — many resources are available to help you and your family. It’s important that you speak with a healthcare provider who’s very familiar with neural tube defects so you can learn more about how your baby will be affected and how to prepare.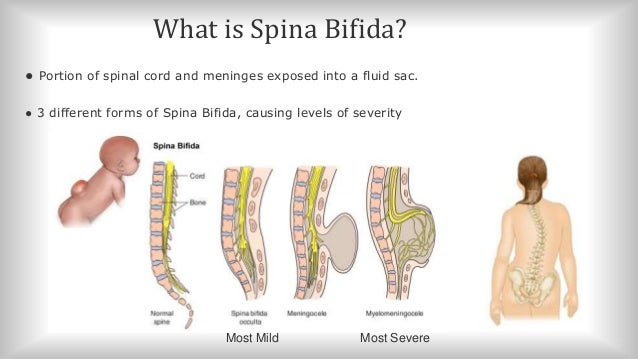
Spina bifida (spina bifida) - treatment, symptoms, causes, diagnosis
Spina bifida (spina bifida) is a complex congenital defect in the development of the spinal cord and spine. This is a type of open neural tube defect in which there is an abnormal development of the back of the spine, the spinal cord, the surrounding nerves, and/or the fluid-filled sac that surrounds the spinal cord.
Spina bifida (back bifida) is an incurable, life-long condition that affects the neuromuscular and musculoskeletal systems. nine0003
This defect varies by type and ranges from moderate to severe.
Children with this defect may need corsets as the body grows, and in severe cases, a wheelchair.
Treatment is mainly aimed at slowing down the deformity and maintaining motor activity.
The defect may occur along the entire length of the spine and may present as part of the spinal cord and surrounding tissues protruding outward rather than inward. Approximately 85 percent of defects occur in the lower back and 15 percent in the neck and thoracic region.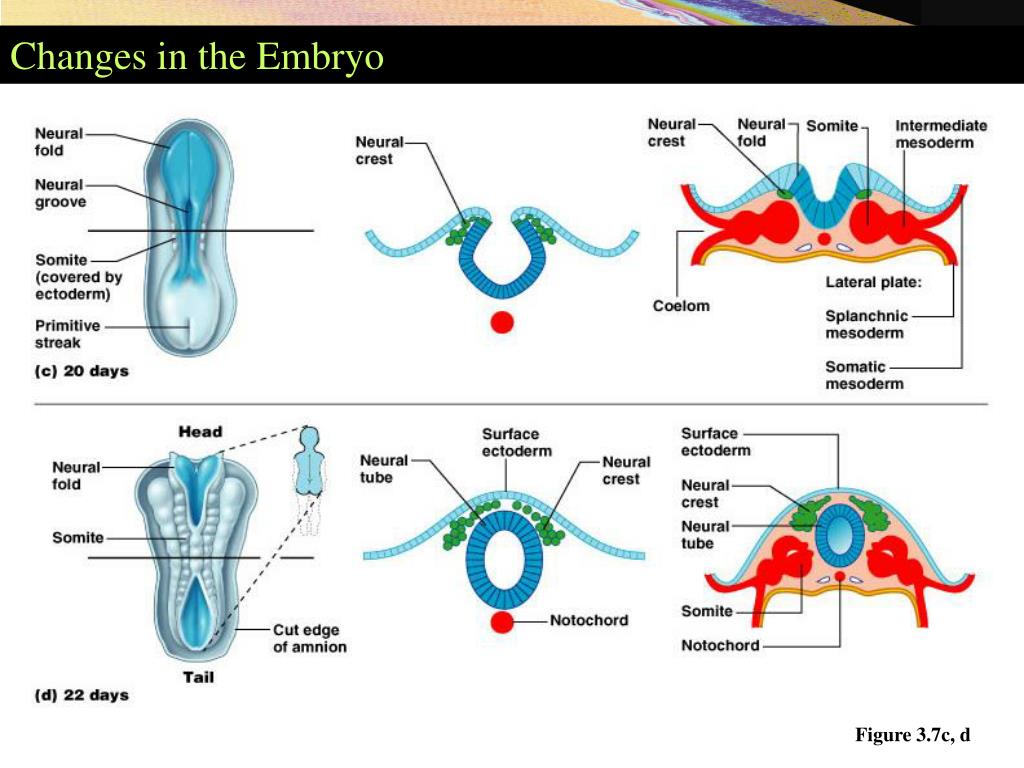 Surgically, it is possible to restore the integrity of the spinal column, but nerve damage cannot be restored, and if they are pronounced, then patients have various degrees of paresis of the lower extremities. The higher the defect on the spinal column, the more severe the nerve damage and movement disorders (paresis and paralysis). nine0003
Surgically, it is possible to restore the integrity of the spinal column, but nerve damage cannot be restored, and if they are pronounced, then patients have various degrees of paresis of the lower extremities. The higher the defect on the spinal column, the more severe the nerve damage and movement disorders (paresis and paralysis). nine0003
According to studies, this developmental anomaly occurs in 7 cases per 10,000 newborns. There are several types of spina bifida that have varying degrees of severity.
- Latent spina bifida (spina bifida occulta) - the most moderate form, in which there are no obvious signs of malformation and changes in the skin. In this form, at least one vertebra changes, but the nerves and spinal cord do not bulge. A child at birth may have a spot or depression in the area of the anomaly. And usually, the baby will not have symptoms. With this form of anomaly (as well as with others), there may be an anomaly in the development of the spinal cord, characterized by attachment of the spinal cord to the spine to the end of the lumbar region, when normally the spinal cord ends at the level of the first lumbar vertebrae and sags freely without attachment to the spine.
 nine0018
nine0018 - Meningocele is a moderate (and the most common) anomaly in which the spinal canal is not properly closed and the meninges (membranes that cover the spinal cord) bulge outside the bony structures of the spinal canal, but the spinal cord itself remains intact. The cystic mass is covered with skin. Most children with meningocele have normal limb function, but may have partial paresis or abnormalities of the bladder or bowel. With this anomaly, there is often underdevelopment of the spinal cord. Almost all patients with this anomaly require surgery to close the defect and free the spinal cord. nine0018
- Lipomeningocele is an anomaly in which fatty tissue is attached to the spinal cord and puts pressure on it. Children with this form of anomaly may not have severe nerve damage, but bladder and bowel function may be impaired. In these cases, surgical treatment is also often used.
- Myelomeningocele: the most severe common form and associated with spina bifida.
 The spinal canal is not closed, and the bulging mass consists of the meninges, pathologically altered spinal cord, and nerves. In addition, in this area the skin is also underdeveloped. In children with this form of spinal cord splitting, paresis below the defect and dysfunction of the pelvic organs are observed in whole or in part. In addition, nerve damage and other pathologies are observed. nine0018
The spinal canal is not closed, and the bulging mass consists of the meninges, pathologically altered spinal cord, and nerves. In addition, in this area the skin is also underdeveloped. In children with this form of spinal cord splitting, paresis below the defect and dysfunction of the pelvic organs are observed in whole or in part. In addition, nerve damage and other pathologies are observed. nine0018
Symptoms
The symptoms of spina bifida vary greatly, depending on the form and severity of the individual child. For example, at birth:
- In latent splitting (spina bifida occulta), there may be no obvious signs or symptoms—only a small spot, depression, or birthmark.
- With a meningocele, there will be a sac-like protrusion that will be located on the back in the spinal region. nine0018
- With myelomeningocele, there will also be a protrusion, but with altered skin, there will be a release of nerves and spinal cord.
In severe spina bifida with localization in the lumbar spine, the following symptoms may occur: paralysis of the lower extremities, dysfunction of the bladder, intestines.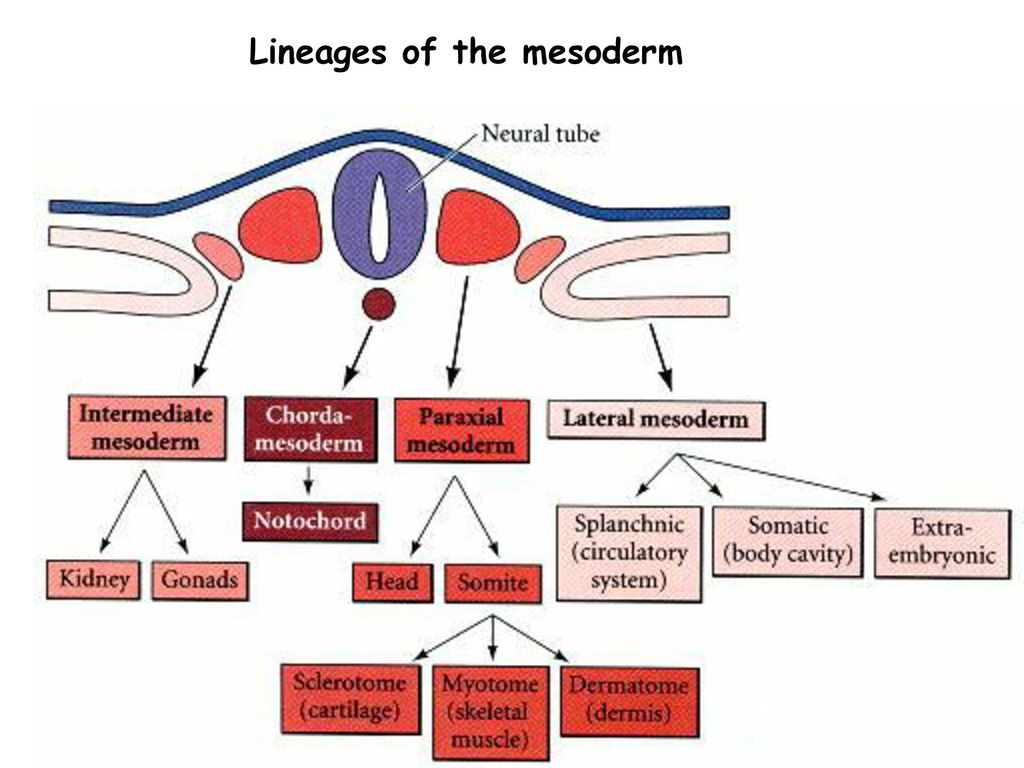 In addition, these patients usually have other developmental anomalies:
In addition, these patients usually have other developmental anomalies:
- Hydrocephalus occurs in 75 percent of myelomeningocele cases and this condition requires operative endoscopic treatment in order to restore normal CSF flow or a shunt to drain excess fluid from the brain. nine0018
- Chiari anomaly (displacement of the brain into the upper cervical vertebrae) can cause pressure on the brainstem, which can manifest as impaired speech, swallowing, and motor disorders in the limbs.
- Underdevelopment of the spinal cord Orthopedic problems including scoliosis, kyphosis, hip dysplasia (congenital dislocation), combined deformities, clubfoot, etc.
- Precocious puberty (especially in girls with spina bifida and hydrocephalus). nine0017 depression and other neurotic conditions
- obesity
- dermatological problems
- developmental anomalies of the urinary tract.
- heart disease
- vision problems
Diagnosis
Diagnosis may be performed during pregnancy to evaluate the fetus for spina bifida.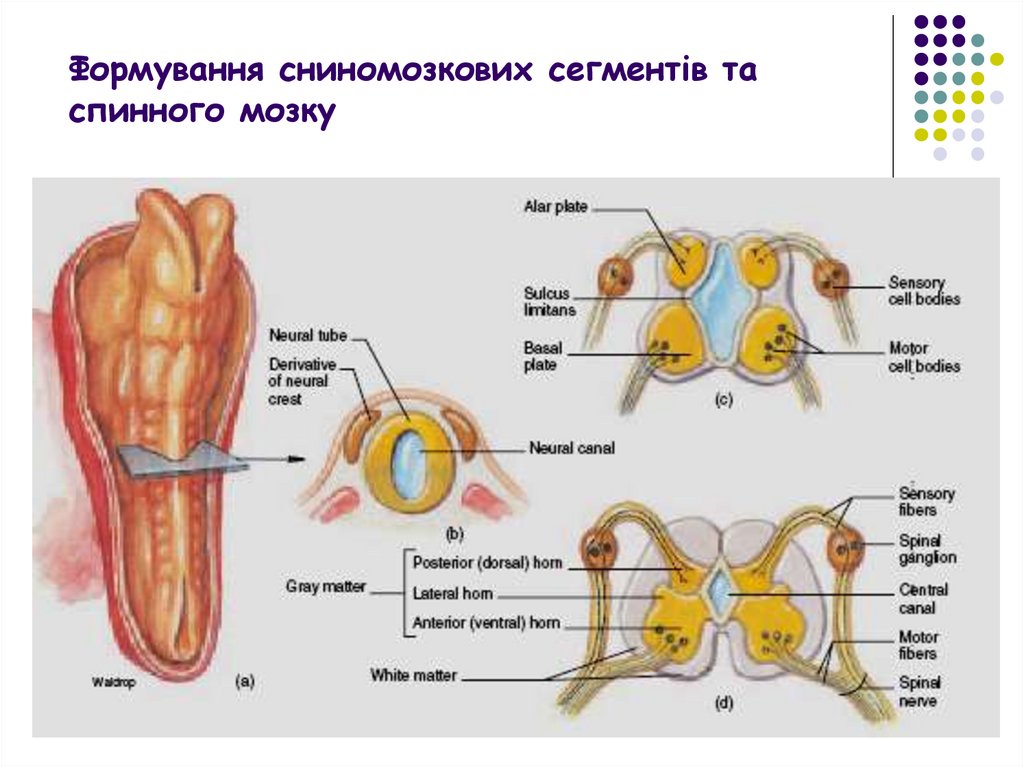 These include:
These include:
- Amniocentesis: A procedure in which a long, thin needle is inserted through the mother's abdomen into the amniotic sac to remove a small amount of amniotic fluid for examination. The fluid is analyzed to determine the presence or absence of an open neural tube defect. Although the analysis is very reliable, it does not allow diagnosing small or closed defects. nine0018
- Prenatal ultrasound: this technique, being absolutely harmless, allows you to non-invasively assess the condition and visualize the internal organs, vessels, tissues of the fetus. Sometimes it is possible to diagnose not only spina bifida, but also other anomalies.
- Blood tests: It is recommended that blood tests be performed between 15 and 20 weeks of gestation for all women who have not previously had a child with an open neural tube defect and who have no family history of the condition. A blood test for alpha-fetoprotein and other biochemical parameters can determine how high the risk of developing spinal anomalies is.
 nine0018
nine0018 - At birth, severe cases of spina bifida are evident by the presence of a fluid-filled sac bulging on the back of the newborn. Visual indicators of mild forms (spina occulta) may be a hairy patch on the skin or a depression along the spine. Unusual weakness or lack of coordination in the lower extremities also suggests spina bifida. In children and adults, this anomaly is often diagnosed during routine studies or, if necessary, to differentiate neurological symptoms using instrumental research methods (MRI, CT, radiography). nine0018
Causes
During pregnancy, the human brain and spinal column begin to form as a flat sheet of cells that folds into a tube called the neural tube. If all or part of the neural tube fails to close, then the open area is called an open neural tube defect. An open neural tube is open in 80 percent of cases, and is covered by bone or skin in 20 percent of cases. The cause of spina bifida (spina bifida and other defects) remains unknown, but is most likely the result of a combination of genetic, nutritional, and environmental factors, such as: nine0003
- maternal dietary deficiency of folic acid (vitamin B) during pregnancy (sufficient folic acid intake during pregnancy may reduce the risk of this anomaly).

- Maternal uncontrolled diabetes
- Certain medicines (antibiotics, anticonvulsants).
- A genetic factor is usually only relevant in 10 percent of cases.
- Mother's age
- What kind of births on the account (firstborns are more at risk). nine0018
- Socioeconomic status (children born in lower socioeconomic families are at higher risk).
- ethnicity
- obesity or excessive consumption of alcohol by a pregnant woman
- When exposed to pregnant hyperthermia in the early stages (sauna, jacuzzi).
Treatment
Spina bifida can be treated immediately after birth. If this defect is diagnosed prenatally, then a caesarean section is recommended in order to reduce possible damage to the spinal cord during the passage of the birth canal. Newborns with meningocele or myelomeningocele are recommended to have surgery within 24 hours of birth. With such an operation, the bone defect is closed and it is possible to preserve the function of the intact part of the spinal cord.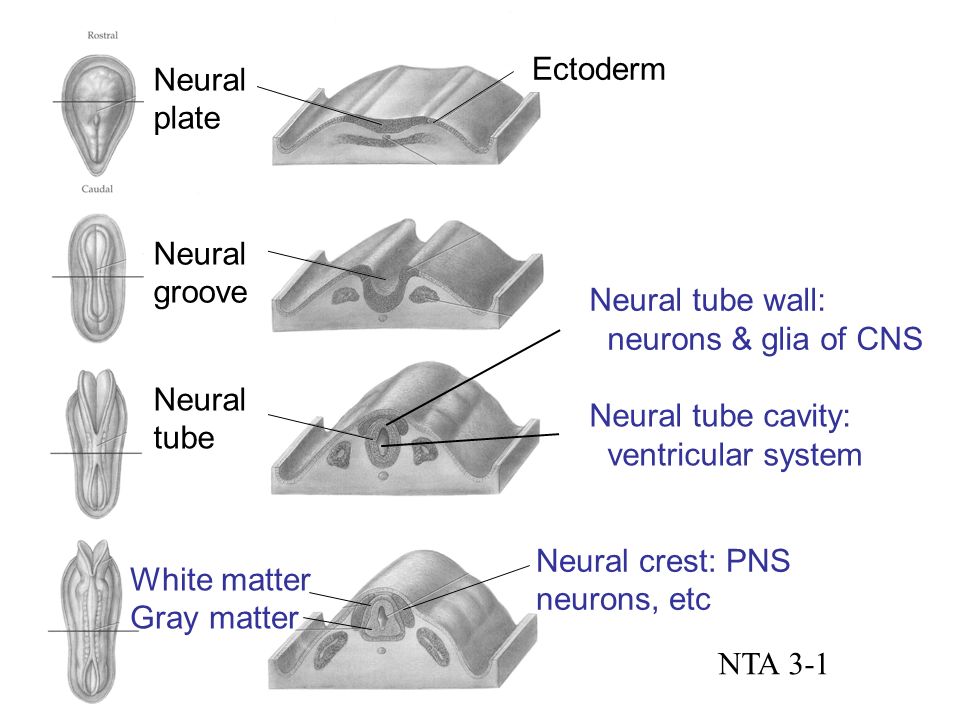 Unfortunately, surgical treatment cannot restore the function of damaged nerves as they are irreversible. nine0003
Unfortunately, surgical treatment cannot restore the function of damaged nerves as they are irreversible. nine0003
Currently, there are clinics that perform prenatal surgery to close the defect, but the techniques have not yet found wide application. The main task of treatment, both in a non-severe form and in the postoperative period, is to preserve the functions of both the musculoskeletal system and the functions of the bladder and intestines. If necessary, orthoses, therapeutic exercises, physiotherapy are used.
In cases where spina bifida is detected by chance during X-ray (MRI, CT) examination, measures must be taken to reduce the risk of spinal cord injury in the area of the spine where this defect exists. nine0003
Operative treatment in adults is used only in the presence of complications. Basically, treatment in adults is aimed only at preventing possible complications (exercise therapy, physiotherapy, wearing a corset).
Fomina Clinic - a network of multidisciplinary clinics
We have already found out that when planning a pregnancy, the lifestyle of the future mother plays an important role, namely the rejection of bad habits, proper nutrition, hygiene and sports.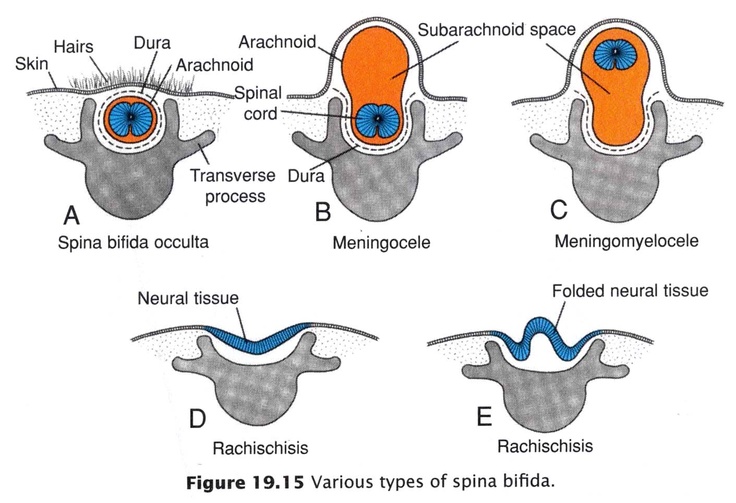 Vitamins play an important role in this, namely folic acid, which is advised to start taking 1-3 months before the expected pregnancy. It is its use that prevents possible malformations that can lead to the death of the child. nine0003
Vitamins play an important role in this, namely folic acid, which is advised to start taking 1-3 months before the expected pregnancy. It is its use that prevents possible malformations that can lead to the death of the child. nine0003
This is a B vitamin that prevents fetal neural tube defects. Moreover, it is important to understand that such an effect is possible only if folic acid begins to enter the mother's body before pregnancy and continues to be taken during pregnancy. Thus, from the first days after conception, the child begins to develop in the right conditions, because by this time folic acid has time to get into your bloodstream in sufficient quantities.
Unfortunately not. The fact is that violations of the laying of the neural tube usually occur on the 18th - 30th day after conception, when a woman may still not know about her pregnancy. nine0003
Let's start with the statistics: neural tube defects (yes, there are several!) are found in approximately 7 out of 10,000 newborns, and it is believed that in half of these cases they are caused by a lack of folic acid in the mother's diet.
The two most common neural tube defects are:
- Spina bifida damages the spinal cord: with this defect, most children survive to adulthood, but may be accompanied by central nervous system disorders throughout life, such as paralysis or inability to control urination and defecation; nine0018
- with anencephaly, all or a significant part of the brain is missing, in which case most children die shortly after birth.
Recommended foods include: Green vegetables, legumes (beans, peas, lentils), lettuce, berries, citrus fruits (fruits and juices), breakfast cereal, whole grain bread/bread.
This, of course, is not enough, because in most of these products the content of folic acid is less than 20% (or even 10%) of the recommended daily amount by doctors. The only exception is lentils, one glass of which contains 90%. Therefore, additionally every day when planning pregnancy and throughout its duration, you need to take vitamins that contain 400 mcg of folic acid.