Early delivery survival rates
Premature Babies’ Survival Rate is Climbing, Study Says
| Ruthann Richter
Research and Innovation.
A comprehensive new study of premature babies in the United States is helping to redefine what it means for a premature infant to survive.
The study looked at 10,877 babies born between 2013 and 2018 and found a significant improvement in survival of those born between 22 and 28 weeks, compared to the past. Some 78% were rescued, compared to 76% of those born between 2008 and 2012. Two percent may not sound like much but it translates into many hundreds of infants saved each year.
This study showed that even those delivered at 22 weeks — 18 weeks early — had a chance of living. With active treatment, about 28% of them survived; among those born at 23 weeks, 55% survived. “When I was in residency in the mid-1980s, babies born at 500 grams [about 1.1 pounds] and 25 weeks didn’t survive; it just didn’t happen. Now we see the borderline of viability dropping to 22 weeks,” said neonatologist Krisa Van Meurs, MD, a Stanford Medicine emerita professor of pediatrics and a co-author on the study. “With all of these new treatment strategies we’ve developed, we’ve seen an amazing impact.”
This analysis shows infants even at the lowest gestational ages — 22 and 23 weeks — might live if they are actively resuscitated, said Susan Hintz, MD, professor of pediatrics and a co-author on the paper. “There has been a shift toward considering a more active initial treatment in prenatal discussions with families over the past several years in light of increasing data to support this approach,” she said.
This study appeared Jan. 18 in the Journal of the American Medical Association.
Tracking babies
The researchers studied the neurosensory, developmental and functional progress of babies born at 22-26 weeks of gestation, conducting evaluations when the children were 2 years old.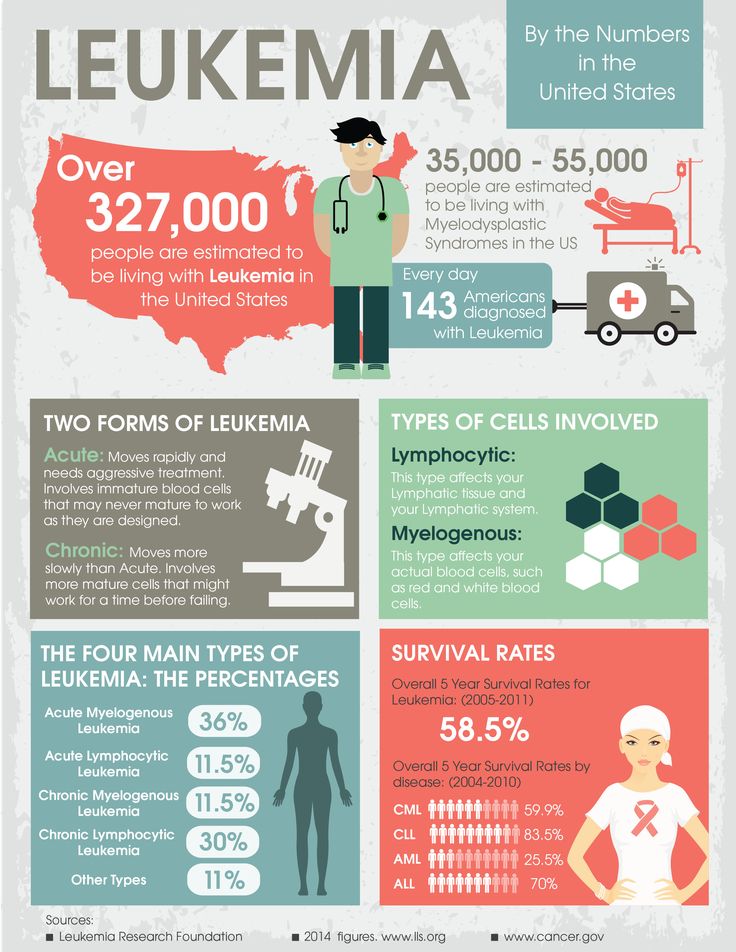 Overall, about half had mild or no signs of neurodevelopmental problems, while 29% had moderate disabilities. About 21% of the children had severe impairments, including approximately 1.5% with blindness and 2.5% with severe hearing loss. Some 15% of the children used a mobility aid such as an orthotic, brace or walker, while 8% had moderate to severe cerebral palsy. About half had been re-hospitalized after being discharged from the neonatal intensive care unit.
Overall, about half had mild or no signs of neurodevelopmental problems, while 29% had moderate disabilities. About 21% of the children had severe impairments, including approximately 1.5% with blindness and 2.5% with severe hearing loss. Some 15% of the children used a mobility aid such as an orthotic, brace or walker, while 8% had moderate to severe cerebral palsy. About half had been re-hospitalized after being discharged from the neonatal intensive care unit.
“It is encouraging that half of the children had no or minimal neurodevelopmental impairments at 2 years. But moderate to severe neurodevelopmental challenges are not uncommon in this group, particularly for those born at the lowest gestational ages,” said Hintz. “We also explored other important outcomes, like feeding challenges and equipment and medication needs, which inform complex care preparations and counseling.”
Improving outcomes
In the past 20 to 30 years, researchers have discovered myriad approaches to improve the survival and care of premature infants, Van Meurs said. That includes using surfactant, a mix of protein and fat that aids lung development, as well as steroids in pregnant mothers, which helps the baby’s lungs and other organs mature and minimizes the risk of breathing problems, bleeding in the brain and other complications, she said.
That includes using surfactant, a mix of protein and fat that aids lung development, as well as steroids in pregnant mothers, which helps the baby’s lungs and other organs mature and minimizes the risk of breathing problems, bleeding in the brain and other complications, she said.
Clinicians also have enhanced the environment in which preterm infants are treated, creating a womb-like atmosphere with low lighting, and minimal noise and disruption. They are also using CPAP devices, which help keep the airways open and are a gentler way of supporting breathing, instead of using ventilators, which can damage the lungs, Van Meurs said.
Parents are also being included in the treatment process—it’s been shown that regular parental touch and especially skin-to-skin “kangaroo care” can increase weight gain, decrease the chance of sepsis—a severe blood infection—and improve survival and neurodevelopment, she said.
Van Meurs said Stanford uses innovative neuromonitoring devices to monitor brain activity and oxygen levels in the brains of fragile newborns to minimize brain injury in the neonatal intensive care unit. “That’s the focus for the next decade—how can we protect the brain and improve outcomes for these children,” she said.
“That’s the focus for the next decade—how can we protect the brain and improve outcomes for these children,” she said.
According to Hintz, investigators in the National Institute for Child Health and Human Development Neonatal Research Network, a group of 18 academic medical centers funded by the institute, are continuing to follow some of the children born extremely preterm through 5-7 years of age. “At an early school age, we can better understand abilities and challenges over a range of more detailed neurologic and cognitive skills, behavioral and social interactions and functional outcomes,” said Hintz, who is the lead investigator for the research network’s follow-up activities.
Continuing care at home
With the increasing probability of survival for extraordinarily preterm infants, Hintz said, more emphasis needs to be placed on life beyond the hospital.
“We need to shift our focus from the NICU hospitalization to far beyond that period, investing in parents and the family, launching interventions and support strategies to improve outcomes that are important to families,” Hintz said.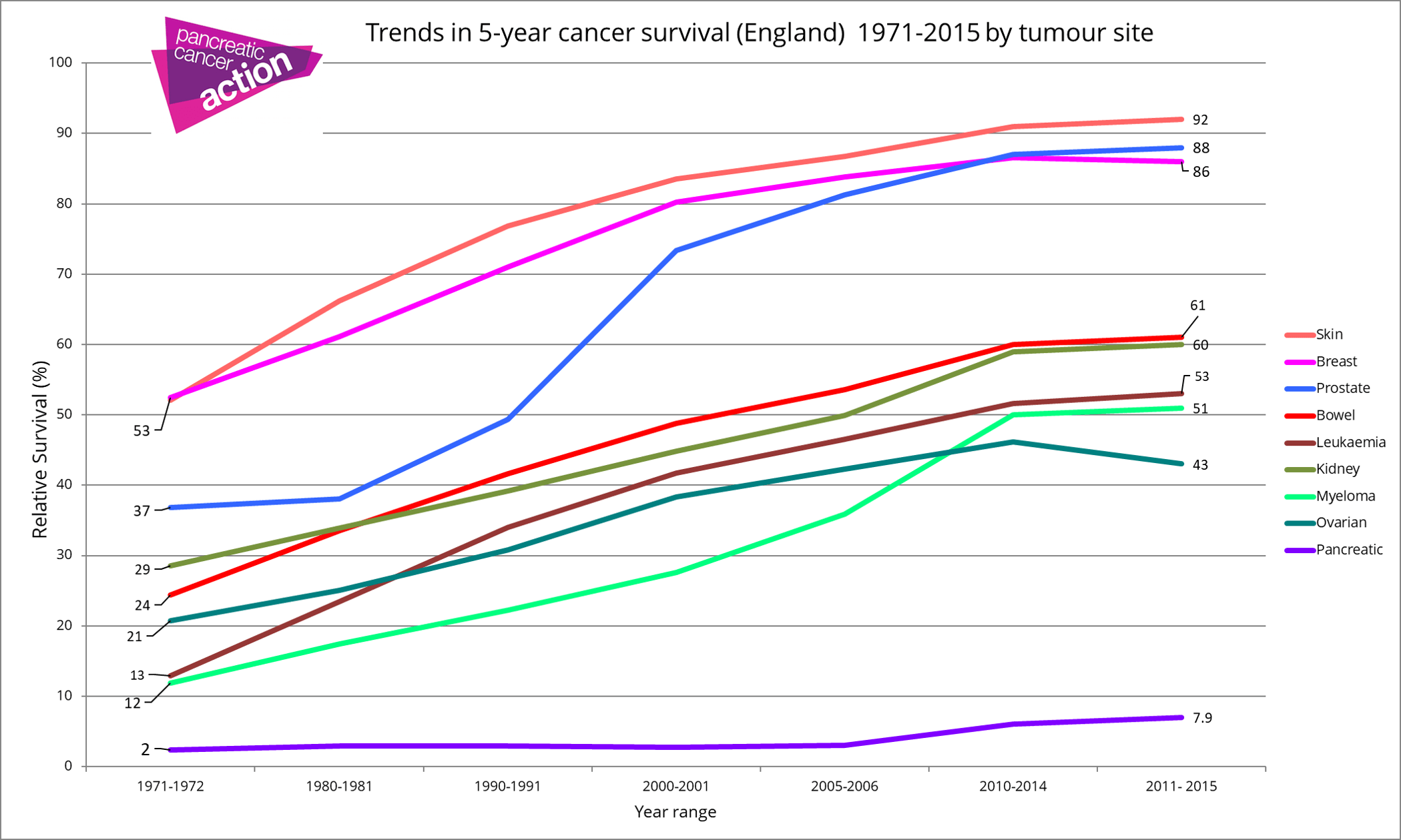 “We have made enormous strides and are doing amazing things for children in the NICU. Now it’s time for us to take a truly life-course view—listening to families, integrating the concerns and outcomes important to them in research and quality improvement efforts. This is how we will help families and children to live their best lives.”
“We have made enormous strides and are doing amazing things for children in the NICU. Now it’s time for us to take a truly life-course view—listening to families, integrating the concerns and outcomes important to them in research and quality improvement efforts. This is how we will help families and children to live their best lives.”
Authors
Tags: NICU, premature babies, research
Premature Baby Survival Rates
So, your little one couldn’t wait to join you in the big, big world and has decided to make a grand entrance! If your baby is premature, or “preterm,” they’re in good company — about 1 in 10 babies are born prematurely in the United States.
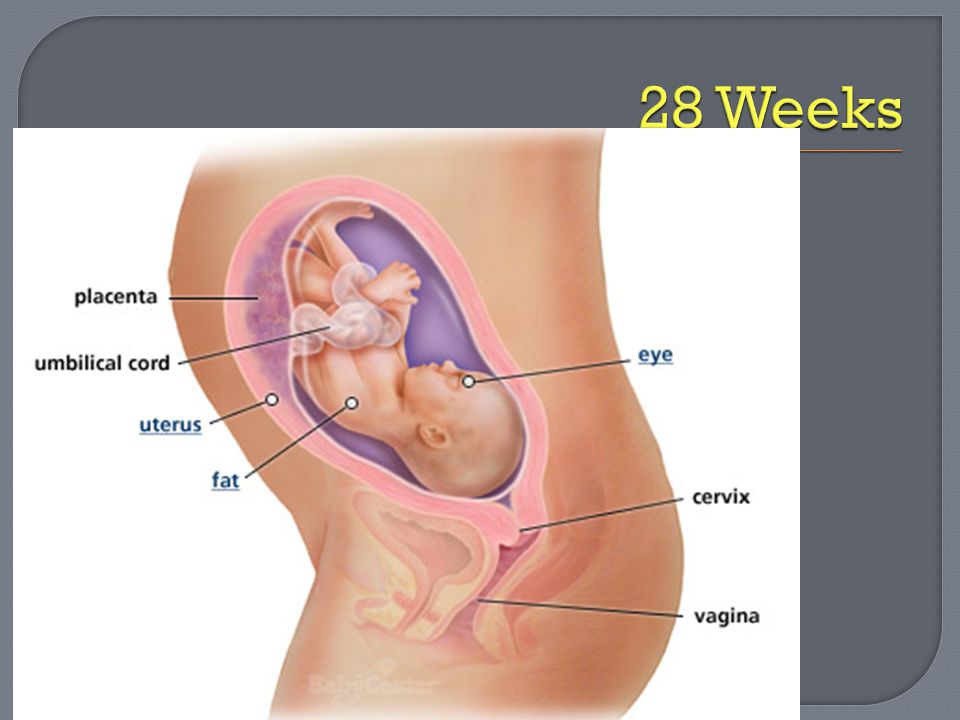
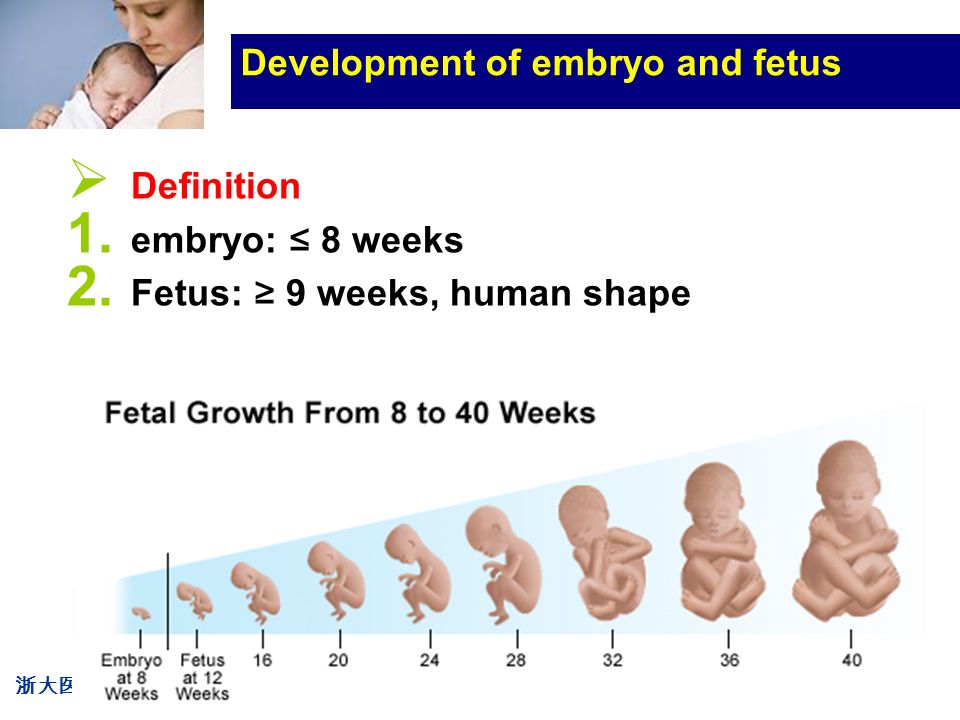
A premature birth is one that happens at least three weeks before your estimated 40-week due date — so, before the 37th week of pregnancy. That said, “premature” is a range.
Premature birth ranges are called:
- extremely preterm (before 28 weeks)
- very preterm (28 to 32 weeks)
- moderate preterm (32 to 34 weeks)
- late preterm (34 to 37 weeks)
You may also hear the term “periviable birth,” which refers to delivery between 20 and 26 weeks, according to the American College of Obstetricians and Gynecologists.
How early your baby is born makes a difference in what kind of interventions they might need. The more premature a little one is, the higher the chance of some complications. Each gestational week makes a difference in survival rate, when it comes to premature babies.
Doctor’s don’t always know why a baby is born premature, and they can’t always prevent it. What’s more, the research on preemie survival rates is extremely broad.
Outcomes vary widely based on country, maternal factors, and baby’s birth weight. But rest assured, the survival rate for babies born extremely preterm without neurodevelopmental problems has been improving since 2000.
A baby born between 20 and 26 weeks is a considered to be periviable, or born during the window when a fetus has a chance of surviving outside the womb. These babies are called “micro-preemies.”
A baby born before 24 weeks has less than a 50 percent chance at survival, say the experts at University of Utah Health.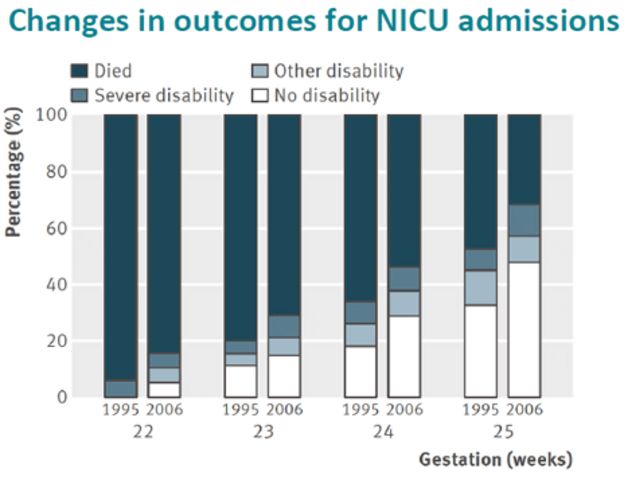
However, according to this 2016 analysis of more than 8,300 deliveries in the United States, babies born at 24 weeks had a 68 percent chance of survival. A 2016 cohort study of more than 6,000 births found a survival rate of 60 percent. (Utah Health notes a 60 to 70 percent survival rate for this gestational age.)
With an extremely premature birth, you and your baby may face some rough times (and choices) together. Fortunately, advances in medicine means even the tiniest babies can likely get bigger and stronger in neonatal intensive care units (NICU).
About 40 percent of babies born at 24 weeks will have health problems, says the Irish Neonatal Health Alliance. Some of these complications may happen right away, or others that appear later in life.
Risks for a baby born this early include complications regarding:
Skin and warmth
Your tiny one will need to go into an incubator (like a portable womb) right away to keep them warm. Babies born this early have not yet had the chance to develop brown fat — the kind just under the skin that keeps them toasty. Their skin will also be extremely thin and delicate.
Their skin will also be extremely thin and delicate.
Breathing
A baby’s lower lungs and airways are only just beginning to develop around 24 weeks. A baby born at this time will need help to breathe. This might mean little tubes going into their nose, as they grow in the incubator.
Eyesight
At about 24 weeks in the womb, a baby’s eyes are still closed. Their eyelids and eyes are not yet developed enough to open them. Your baby will need to have soft cotton or gauze taped over their eyes to protect them from the light as their sight continues to develop.
In some cases, a baby’s eyes might not grow as they should, which could lead to vision problems or even blindness.
Hearing
Amazingly, an extremely premature baby already has fully formed ears. Your baby can start to hear you at about 18 weeks gestation! However, your little one’s eardrums are still very delicate and sensitive at 24 weeks. Some babies born this early may have problems hearing or experience deafness.
Some extremely premature babies may have issues that affect the brain and nervous system as they get older. Some of these are serious. Complications include cerebral palsy, learning problems, and behavioral issues.
If your baby is born at 26 weeks, they’re still considered “extremely preterm.” But a lot can improve for a developing baby in just a couple of weeks of gestation time, increasing chances of survival.
Babies born at 26 weeks were found to have a survival rate of 89 percent in the 2016 analysis and 86 percent in the 2016 cohort study.
A big difference contributing to the jump in survival rate at 26 weeks versus 24 weeks is your baby’s lung development. By about 26 weeks of gestational age, a baby’s lower lungs have grown and developed little air sacs called alveoli.
Your baby will still be too little to breathe on their own, but their lungs will be more developed and stronger. Your little one will still need to be in an incubator for warmth with breathing tubes to help bathe them in life-giving oxygen.
About 20 percent of babies born at 26 weeks may still have some health problems as they age. These might include issues with:
- seeing
- hearing
- learning
- understanding
- behavior
- social skills
Babies born at 26 weeks may also develop heart problems.
A baby born after 28 weeks is considered “very preterm” but has a big head start compared to babies born just 2 to 4 weeks earlier. This is because their vital organs — like the heart and lungs — are much more developed.
According to the University of Utah Health, the survival rate for your baby is 80 to 90 percent at 28 weeks. Some clinical studies have even more promising data, showing survival rates of 94 percent and 98 percent at this age.
Only 10 percent of babies born at 28 weeks risk long-term complications. These can include:
- breathing problems
- infections
- digestive problems
- blood problems
- kidney problems
- brain and nervous system problems like seizures
What a difference a few womb weeks make! Babies born between 30 and 32 weeks, while still considered preterm, have at least a 99 percent chance of survival. They also have very low risk of health and development complications later on.
They also have very low risk of health and development complications later on.
If your baby is born at 34 to 36 weeks they are in a new category called “late preterm.” This is the most common kind of premature baby. It’s also the one with the least risks because your baby has more time to grow and develop inside you.
In fact — good news — a preemie baby born at 34 to 36 weeks has nearly a 100 percent chance at survival and the same chances at long-term health as a baby who was born full-term.
Still, your 34- to 36-week-old baby might be smaller and a bit more delicate than a 40-week or full-term baby. Your doctor may recommend that they stay in an incubator at the hospital for a week or two, so they can rest and get a bit bigger before going home.
If your baby is born prematurely, there are several things that affect their survival rate and how healthy they’ll be as they age. A week or two more in the womb can make a big difference for your baby.
Medical advances in caring for premature babies means better outcomes, and more peace of mind for parents. While every week in the womb will give you more assurance, know that chances for your preemie’s survival are increasing every year.
While every week in the womb will give you more assurance, know that chances for your preemie’s survival are increasing every year.
Premature birth statistics
Premature births are those that occur between 22 and 37 weeks of gestation (from 154 to less than 259 days). Preterm birth is divided according to gestational age into very early preterm birth - 22-27 weeks, early preterm birth - 28-33 weeks and preterm birth - 34-37 weeks, which is associated with the peculiarities of obstetric tactics and outcomes of preterm birth [11]. According to the results of scientific studies, about 5% of preterm births occur at a gestational age of up to 28 weeks, about 15% - at 28-31 weeks, about 20% - at 32-33 weeks, 60-70% - at 34-37 weeks [16 ]. nine0003
Over the past 50 years, despite progress in the provision of medical care, including the widespread use of beta-agonists as tocolytic agents since the 70s of the XX century, the frequency of preterm birth has not changed [1] and is 5-10%, changing from region to region, is not the same in different countries; in developed countries has increased in recent years as a result of the use of new reproductive technologies [15]. According to the literature [11], at the beginning of the 21st century, this figure in the United States was 10.1%, in England - 7.8%, in France - 7.2%, in Germany - 9-10%, in Hungary - 10%. In Norway, the rate of preterm birth varies by region from 5 to 7.8%, averaging 7%. In the United States in 1981, this figure was 9.5%, and in 2005 - 12.7% [16] and differs in different ethnic groups: in the United States and Great Britain, African American and Afro-Caribbean women had preterm births in 16- 18% of women compared to 5-9% of white women. In East Asia, Spain, rates of prematurity are low, in South Asia, including the Indian subcontinent, the rate of birth of children with low birth weight is high, due to a decrease in fetal growth, but the percentage of preterm births is not increased [16]. According to the research results of R. Goldenberg et al. (2008), in the US, about 20-25% of pregnant women smoke, of which 12-15% continue to smoke during pregnancy, nicotine is known to increase the risk of preterm birth.
According to the literature [11], at the beginning of the 21st century, this figure in the United States was 10.1%, in England - 7.8%, in France - 7.2%, in Germany - 9-10%, in Hungary - 10%. In Norway, the rate of preterm birth varies by region from 5 to 7.8%, averaging 7%. In the United States in 1981, this figure was 9.5%, and in 2005 - 12.7% [16] and differs in different ethnic groups: in the United States and Great Britain, African American and Afro-Caribbean women had preterm births in 16- 18% of women compared to 5-9% of white women. In East Asia, Spain, rates of prematurity are low, in South Asia, including the Indian subcontinent, the rate of birth of children with low birth weight is high, due to a decrease in fetal growth, but the percentage of preterm births is not increased [16]. According to the research results of R. Goldenberg et al. (2008), in the US, about 20-25% of pregnant women smoke, of which 12-15% continue to smoke during pregnancy, nicotine is known to increase the risk of preterm birth. nine0003
nine0003
According to ICD-10, “Premature birth” has an independent heading O 60 - the onset of labor (spontaneous) before 37 completed weeks of pregnancy [5]. Registration of preterm births in our country is carried out according to the annual statistical reporting form of the Ministry of Health of Russia No. 32 "Report on medical care for pregnant women, women in labor and puerperas." In the Russian Federation, until recently, the registration of preterm birth was carried out from 28 weeks of pregnancy, and in economically developed countries - from 22 weeks. In this regard, the indicators of perinatal losses were not comparable. nine0003
The following frequency of preterm births (28-37 weeks of pregnancy) was registered in the Russian Federation: 2008 - 3.6% of the total number of births, 2009 - 4.1%, 2010 - 3.8%, 2011 - 3.9%. In connection with the transition in 2012 of Russia to the birth registration criteria recommended by WHO (fetal weight 500 g or more, gestational age 22 weeks or more) [6], the proportion of preterm births at 22-37 weeks in 2012 was 4. 3% [8].
3% [8].
The etiology and pathogenesis of preterm labor are not fully understood. Premature birth at 22-27 weeks of gestation (fetal weight from 500 to 1000 g) is most often caused by isthmic-cervical insufficiency, infection of the lower pole of the fetal bladder and its premature rupture. Premature birth with a gestational age of 28-33 weeks (fetal weight 1000-1800 g) and preterm birth with a gestational age of 34-37 weeks (fetal weight 1900-2500 g and more) are due to various reasons: the woman's age (up to 20 years and over 35 years), preeclampsia, multiple pregnancy, etc. The highest percentage of abortion occurs at 34-37 weeks of gestation, while at 22-27 weeks of gestation this figure is 12 times lower. High morbidity and mortality in premature newborns is noted in the early stages - 22-33 weeks of gestation.
Preterm birth is a multifactorial process. In the 70s and 80s. of the last century, the world scientific community discussed articles on the identified social risk factors for preterm birth, among which the frequency of preterm birth was higher among residents of the northern and remote areas; among visiting women in remote areas, it was 18%, since they are not adapted to extreme conditions; in large cities, near airfields, major highways, the frequency of preterm birth is higher; in women working 42 hours a week, the frequency of preterm birth was 8. 5%, and in women working less than 42 hours a week - 4.5%; among women using several modes of transport on their way to work, premature births were observed in 22%, with a lower load - in 6.3%; in women engaged in physical labor, combining work and study, premature births occurred 2 times more often; in women younger than 20 and older than 40, the percentage of preterm births is higher, etc. [sixteen]. nine0003
5%, and in women working less than 42 hours a week - 4.5%; among women using several modes of transport on their way to work, premature births were observed in 22%, with a lower load - in 6.3%; in women engaged in physical labor, combining work and study, premature births occurred 2 times more often; in women younger than 20 and older than 40, the percentage of preterm births is higher, etc. [sixteen]. nine0003
Women with preterm labor are 2.5 times more likely to have them again in their next pregnancy. The study of all these factors makes it possible to predict the likelihood of preterm birth in women who do not have clinical signs of the disease. This is not about the early detection of the disease, but about the forecast of the degree of probability of its development. Among the risk factors, the interval between births plays an important role: successive pregnancies and childbirth deplete the mother's body, reduce its resistance, thereby contributing to an increase in morbidity.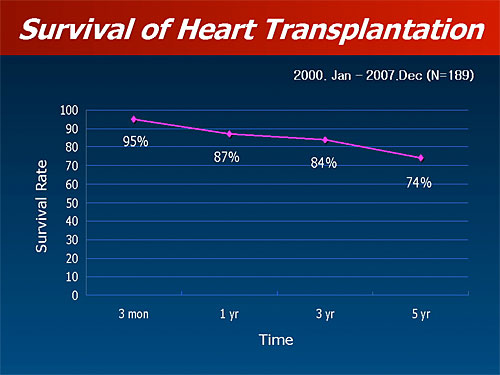 nine0003
nine0003
Significant progress in the study of preterm labor was achieved by the French scientist E. Papernik [12]. A group of researchers under his leadership managed to reduce the frequency of preterm birth by 2-2.5 times (1969-1984). Thanks to taking into account the influence of socio-demographic, professional and household factors, perinatal mortality has significantly decreased in European countries. According to E. Papernik [12], the preterm birth prevention program can be implemented only if the work is well organized, both in the medical part and in the social part. nine0003
P.G. Martynenko, V.G. Volkov [3] based on a retrospective analysis of the birth histories of 25,297 puerperas in obstetric institutions in the Tula region during 2006-2008. revealed that the main risk factors for early preterm birth (22-31 weeks) are multiple pregnancies (75.8%) and isthmic-cervical insufficiency (54.9%). The presented materials testify to the social orientation of risk factors for preterm birth. In this regard, preterm birth is not only a medical but also a social problem. nine0003
In this regard, preterm birth is not only a medical but also a social problem. nine0003
Pregnancy and preterm birth itself are associated with a significant number of complications, and maternal and fetal outcomes with increased levels of reproductive losses. It is preterm birth that determines the level of perinatal morbidity and mortality. The problem of preterm birth is of great social importance, given the high cost of nursing low birth weight children. The average cost of nursing a 500 g baby is over $150,000, and only 44% of them survive. With a child weighing 1251-1500 g, the average cost of nursing is approximately US$ 30,000 and the survival rate is 97% [11, 12]. The total cost of medical care for premature newborns is 16.9 billion dollars a year. This is 10% of all childhood costs and 35% of all newborn costs.
Ola Didrik Zaugstad, a well-known neonatologist and author of a study in the field of problems related to newborns and premature babies [17], believes that to date, not enough is known about the causes of preterm birth. At the same time, he notes the following causes of premature birth: bleeding during pregnancy, stress, pregnancy complications, hard physical work, cervical weakness, multiple pregnancies, early discharge of water, heredity. nine0003
At the same time, he notes the following causes of premature birth: bleeding during pregnancy, stress, pregnancy complications, hard physical work, cervical weakness, multiple pregnancies, early discharge of water, heredity. nine0003
When analyzing the mechanisms of development of preterm birth, four main causes of preterm birth were identified:
- infection - acute, chronic, systemic, ascending, bacterial and / or viral;
- maternal and/or fetal stress due to extragenital pathology, pregnancy complications and placental insufficiency;
- thrombophilic disorders leading to placental abruption, thrombosis in the placenta;
- overstretching of the uterus with multiple pregnancy, polyhydramnios, with malformations of the uterus, infantilism [10, 12]. nine0003
The high incidence of pregnancy complications and preterm birth itself is responsible for significant neonatal morbidity and mortality in newborns. Premature babies account for 60-70% of cases of early neonatal mortality, 50% of neurological diseases [17]. Stillbirth in preterm birth is observed 8-13 times more often than in timely. In developed countries, the mortality of children weighing 1000-1500 g at birth has decreased from 50 to 5%, the mortality of children weighing 500-1000 g - from 90 to 20% [9].
Stillbirth in preterm birth is observed 8-13 times more often than in timely. In developed countries, the mortality of children weighing 1000-1500 g at birth has decreased from 50 to 5%, the mortality of children weighing 500-1000 g - from 90 to 20% [9].
Preterm infant survival has improved significantly with the development of intensive neonatal care. Although most premature babies survive, they are at increased risk of neurological, respiratory, and gastrointestinal complications. The shorter the gestational age at the time of delivery, the higher the risk of morbidity and mortality for the child.
Finnish scientists [2] calculated that the decrease in perinatal mortality is due to 40% improvement in social living conditions, 35% - the development of the country's economy and 30% - medical organizational measures. nine0003
The infant mortality rate in Russia under the new birth criteria [6], according to Rosstat, increased from 7.4 to 8.7‰ (by 17.6%). The perinatal mortality rate increased from 7. 17 in 2011 to 10.0 per 1000 live births and stillbirths in 2012 (by 39.7%): the stillbirth rate - from 4.5 to 6.34‰ (by 40. 9%), and early neonatal mortality - from 2.7 to 3.6‰ (by 33.3%). The level of perinatal mortality in obstetric hospitals in 2012 increased by 45.1%, mainly due to accounting for children weighing 500-999 g, and amounted to 9.75 per 1000 live births and stillbirths - against the level of 6.72% in 2011 for children weighing 1000 g or more. According to L.P. Sukhanova [7], in obstetric hospitals of the 2nd level, 53.2% of preterm births and 50.3% of births in the period of 22-27 weeks are carried out.
17 in 2011 to 10.0 per 1000 live births and stillbirths in 2012 (by 39.7%): the stillbirth rate - from 4.5 to 6.34‰ (by 40. 9%), and early neonatal mortality - from 2.7 to 3.6‰ (by 33.3%). The level of perinatal mortality in obstetric hospitals in 2012 increased by 45.1%, mainly due to accounting for children weighing 500-999 g, and amounted to 9.75 per 1000 live births and stillbirths - against the level of 6.72% in 2011 for children weighing 1000 g or more. According to L.P. Sukhanova [7], in obstetric hospitals of the 2nd level, 53.2% of preterm births and 50.3% of births in the period of 22-27 weeks are carried out.
The severity of the contingent of women with early preterm birth is evidenced by the high frequency of their operative delivery and forced obstetric hysterectomy during all years. Thus, according to the average annual indicator for 5 years, the frequency of hysterectomy in the process of abortion in women with a gestational age of 22-27 weeks is 18.6 times higher than the rate in childbirth (28. 4) per 1000 interruptions in the period of 22-27 weeks against 1.53 per 1000 deliveries at 28 weeks or more. The frequency of small cesarean section (307.0 per 1000 interruptions in the period of 22-27 weeks according to the average annual rate for 2008-2012) is 1.4 times higher than the rate in the period of 28 weeks or more (219,2 per 1000 births) - with higher mortality in short gestations. The frequency of complications during small caesarean section (0.55 per 100 operations) is higher than in the period of 28 weeks or more (0.35) [7].
4) per 1000 interruptions in the period of 22-27 weeks against 1.53 per 1000 deliveries at 28 weeks or more. The frequency of small cesarean section (307.0 per 1000 interruptions in the period of 22-27 weeks according to the average annual rate for 2008-2012) is 1.4 times higher than the rate in the period of 28 weeks or more (219,2 per 1000 births) - with higher mortality in short gestations. The frequency of complications during small caesarean section (0.55 per 100 operations) is higher than in the period of 28 weeks or more (0.35) [7].
Russian researchers [13] showed an increased risk of maternal mortality associated with preterm birth. Thus, the leading causes of death of women in preterm birth were preeclampsia (26.6%), extragenital diseases (23.4%), bleeding (21.9%) and sepsis (12.4%). In the group of women who died during timely delivery, the 1st place in the structure of causes of death was occupied by bleeding (25.8%), 2nd by sepsis (22.3%), 3rd by uterine rupture (18.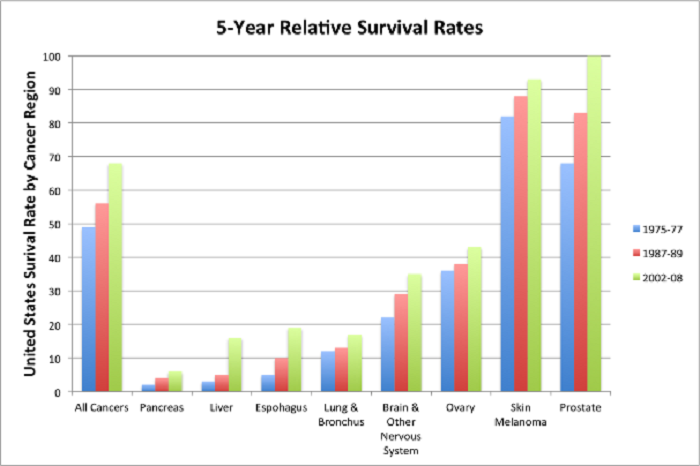 2%) , 4th - extragenital diseases (9.9%).
2%) , 4th - extragenital diseases (9.9%).
According to M.E. Matveenko [4], the primary medical documentation for 82 cases of maternal death in multiple pregnancy, which occurred spontaneously in 81 women, in 1 woman after IVF and PE, was subjected to clinical analysis. After childbirth, 93.9% died, of which 48.7% died after premature birth. nine0003
Among the mothers who died in 2008 in Russia, women in labor and childbirth accounted for 69.4%, of which 31.3% died during premature births. The study showed that preterm birth, with a frequency of 3.4% in the population, is responsible for 21.7% of maternal deaths. In this regard, the prevention of preterm birth is a reserve for reducing maternal mortality [13].
The tactics of managing and treating the threat of preterm birth takes into account the possible causes of preterm birth and is determined by: gestational age, the condition of the mother and fetus, the presence of a whole amniotic sac, the nature of the contractile activity of the uterus, the degree of changes in the cervix, the presence of bleeding and its severity [12].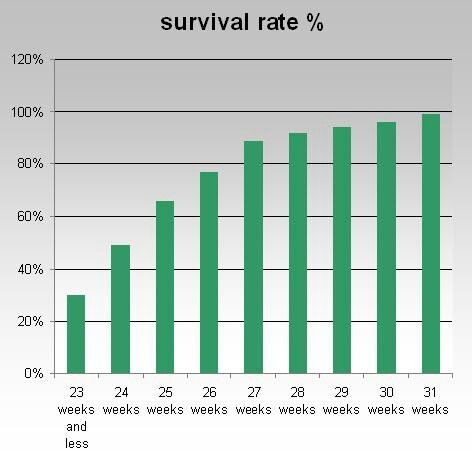 The main tasks in the management of women with the threat of preterm labor are the prolongation of pregnancy to the optimal term of labor, timely prevention and correction of emerging complications, monitoring the condition and development of the fetus, the correct choice of the method of delivery, rational management of labor and the postpartum period [1]. Therapy to prevent preterm birth, methods of delivery in them, the effectiveness or danger of interventions that do not have the necessary evidence base are set out in the Cochrane Guidelines, as well as in the clinical protocol for preterm birth [1, 14]. Knowledge of these documents will change the priorities in the national obstetric service from excessive "obstetric aggression" towards preventive basic care, based on the basic principle of perinatal obstetrics - ensuring the safety of women and children. nine0003
The main tasks in the management of women with the threat of preterm labor are the prolongation of pregnancy to the optimal term of labor, timely prevention and correction of emerging complications, monitoring the condition and development of the fetus, the correct choice of the method of delivery, rational management of labor and the postpartum period [1]. Therapy to prevent preterm birth, methods of delivery in them, the effectiveness or danger of interventions that do not have the necessary evidence base are set out in the Cochrane Guidelines, as well as in the clinical protocol for preterm birth [1, 14]. Knowledge of these documents will change the priorities in the national obstetric service from excessive "obstetric aggression" towards preventive basic care, based on the basic principle of perinatal obstetrics - ensuring the safety of women and children. nine0003
In order to understand the causes and earlier treatment of preterm birth, rather than their consequences, the issue of introducing markers of preterm birth into clinical practice is currently being urgently raised. It is known that preterm birth is accompanied by an imbalance of pro- and anti-angiogenic factors, which is, apparently, the result of the activity of certain alleles. With the progress of molecular biology, it became possible to isolate the DNA of almost any protein from biological fluids (amniotic fluid, urine, cervical mucus, vaginal discharge, serum, plasma, saliva) using polymerase chain reaction. An attempt is being made to find molecular predictors of premature development of labor, which will allow choosing a rational etiologically and pathogenetically substantiated therapy. nine0003
It is known that preterm birth is accompanied by an imbalance of pro- and anti-angiogenic factors, which is, apparently, the result of the activity of certain alleles. With the progress of molecular biology, it became possible to isolate the DNA of almost any protein from biological fluids (amniotic fluid, urine, cervical mucus, vaginal discharge, serum, plasma, saliva) using polymerase chain reaction. An attempt is being made to find molecular predictors of premature development of labor, which will allow choosing a rational etiologically and pathogenetically substantiated therapy. nine0003
Thus, preterm birth is a medical and social problem and is associated with a woman's low socioeconomic and educational status, often stress, hard physical labor. The frequency of preterm birth in the world ranges from 5 to 10%. The role of infection, premature rupture of amniotic fluid, isthmic-cervical insufficiency, multiple pregnancy, aggravated obstetric and gynecological history in the occurrence of preterm labor was studied. However, in 40-50% of cases, the cause of preterm birth cannot be established. It is known that women with preterm birth are at risk of high reproductive losses. Recently, the search for predictors of preterm birth has been of particular interest in order to identify risk groups for the development of this complication and prevent its development, which is the subject of our scientific study. nine0003
However, in 40-50% of cases, the cause of preterm birth cannot be established. It is known that women with preterm birth are at risk of high reproductive losses. Recently, the search for predictors of preterm birth has been of particular interest in order to identify risk groups for the development of this complication and prevent its development, which is the subject of our scientific study. nine0003
Prevention of preterm birth | Serov V.N., Sukhorukova O.I.
Until 2012 in Russia, the concept of “birth of a live child (newborn)” was understood as “complete isolation or removal of a fetus from the mother’s body at a gestational age of 28 weeks or more” (Order of the Ministry of Health of the USSR of 12.06.86 No. 848, Appendix 1 , item 3).
In 2012, the Ministry of Health of Russia, "according to the International Convention on the Rights of the Child, the Declaration on ensuring the survival, protection and development of children", canceled this instruction on the territory of the Russian Federation. Since January 2012, the criteria recommended by the World Health Organization have been introduced in the Russian Federation (order of the Ministry of Health of the Russian Federation No. 318 dated 04.12.2011). Fetal viability criteria: term - 22 weeks. and more, body weight - 500 g or more. Among those born at 22-23 weeks. 20% survive (every 5th newborn), at 26 weeks. - 60%, at 27-28 weeks. – about 80% of premature newborns [19, 21]. Nearly 100% survival was noted among newborns at 32 weeks. pregnancy or more. Preterm infants account for 60–70% of early neonatal mortality and 65–75% of infant mortality [3, 5, 6, 20]. The stillbirth rate in preterm births is 8–13 times higher than in timely ones [7, 11]. Children born weighing less than 1500 g are 200 times more likely to die as newborns and, if they survive, 10 times more likely to have neurological and somatic complications than children born weighing more than 2500 g [1, 8]. nine0003
Since January 2012, the criteria recommended by the World Health Organization have been introduced in the Russian Federation (order of the Ministry of Health of the Russian Federation No. 318 dated 04.12.2011). Fetal viability criteria: term - 22 weeks. and more, body weight - 500 g or more. Among those born at 22-23 weeks. 20% survive (every 5th newborn), at 26 weeks. - 60%, at 27-28 weeks. – about 80% of premature newborns [19, 21]. Nearly 100% survival was noted among newborns at 32 weeks. pregnancy or more. Preterm infants account for 60–70% of early neonatal mortality and 65–75% of infant mortality [3, 5, 6, 20]. The stillbirth rate in preterm births is 8–13 times higher than in timely ones [7, 11]. Children born weighing less than 1500 g are 200 times more likely to die as newborns and, if they survive, 10 times more likely to have neurological and somatic complications than children born weighing more than 2500 g [1, 8]. nine0003
The leading causes of preterm birth before 28 weeks are: infection, premature rupture of amniotic fluid and isthmic-cervical insufficiency with subsequent prolapse and infection of the membranes of the membranes [Shazly S. , Makhseed M., Azizieh, 2004]. According to the literature, from 30 to 40% of preterm births are due to the presence of an infectious process [Vlasova T.A., Valdman S.F., Ivanova N.V., 2008]. Urogenital infection plays a key role in the genesis of various pathological processes during pregnancy and the health of the newborn [Goldenberg R.L., Culhane J.F., Iams J.D., 2008]. The most common cause of preterm birth is the opportunistic flora of the urogenital tract. At the same time, a change in the vaginal biocenosis with a corresponding change in pH can be used as a marker for assessing the risk of preterm birth [Radzinsky V.E., Khamoshina M.B., Kalendzhyan A.S., 2010]. Premature rupture of the membranes complicates the course of preterm labor in 1995% of cases [Alanen A., 2008]. Studies have shown that the main way of changing the membranes with their subsequent rupture is infection with various microorganisms in the ascending way [Alvarez J.R., Williams S.F., Ganeshi v. L., 2007]. Early diagnosis of premature rupture of amniotic fluid largely determines further management tactics [Crowther C.
, Makhseed M., Azizieh, 2004]. According to the literature, from 30 to 40% of preterm births are due to the presence of an infectious process [Vlasova T.A., Valdman S.F., Ivanova N.V., 2008]. Urogenital infection plays a key role in the genesis of various pathological processes during pregnancy and the health of the newborn [Goldenberg R.L., Culhane J.F., Iams J.D., 2008]. The most common cause of preterm birth is the opportunistic flora of the urogenital tract. At the same time, a change in the vaginal biocenosis with a corresponding change in pH can be used as a marker for assessing the risk of preterm birth [Radzinsky V.E., Khamoshina M.B., Kalendzhyan A.S., 2010]. Premature rupture of the membranes complicates the course of preterm labor in 1995% of cases [Alanen A., 2008]. Studies have shown that the main way of changing the membranes with their subsequent rupture is infection with various microorganisms in the ascending way [Alvarez J.R., Williams S.F., Ganeshi v. L., 2007]. Early diagnosis of premature rupture of amniotic fluid largely determines further management tactics [Crowther C. A., Harding J.E., 2003]. The detection of protein-1 that binds insulin-like growth factor in the vaginal discharge is one of the reliable methods for diagnosing premature rupture of the membranes [Drife J., 2006, Krupa F.G., Faltin D., 2006]. In the existing medical examination system, unified methodological guidelines in relation to the prevention of preterm birth are not sufficiently developed and the possibilities of using modern methods for their prediction are limited, which allow early identification of risk factors and the choice of optimal tactics for managing pregnancy [Radzinsky V.E., Orazmuradova A.A., 2009].
A., Harding J.E., 2003]. The detection of protein-1 that binds insulin-like growth factor in the vaginal discharge is one of the reliable methods for diagnosing premature rupture of the membranes [Drife J., 2006, Krupa F.G., Faltin D., 2006]. In the existing medical examination system, unified methodological guidelines in relation to the prevention of preterm birth are not sufficiently developed and the possibilities of using modern methods for their prediction are limited, which allow early identification of risk factors and the choice of optimal tactics for managing pregnancy [Radzinsky V.E., Orazmuradova A.A., 2009].
The risk of developing idiopathic respiratory distress syndrome in premature babies with a gestational age of less than 28 weeks. is 60%, from 32 to 36 weeks. — 20%, more than 37 weeks. — 5% [14, 16]. Steroid therapy with glucocorticoids reduces early neonatal mortality by 40%.
Preterm birth is divided into spontaneous and induced due to the health of the pregnant woman and/or the fetus. Spontaneous preterm labor, in turn, can begin with regular labor activity with a whole amniotic sac — idiopathic (about 40–50% of cases) or with discharge of amniotic fluid in the absence of labor activity (about 50%) [12, 13, 17]. According to the clinical picture, preterm labor is divided into threatening, characterized by irregular contractions of the uterus and opening of the cervix up to 3-4 cm, and those that have begun - in this case, regular labor occurs and the cervix opens by 3-4 cm or more. Every third case of preterm birth occurs in primigravida, in which risk factors include previous abortions or spontaneous miscarriages, urinary tract infections, inflammatory diseases of the genitals [9, 15, 18, 21].
Spontaneous preterm labor, in turn, can begin with regular labor activity with a whole amniotic sac — idiopathic (about 40–50% of cases) or with discharge of amniotic fluid in the absence of labor activity (about 50%) [12, 13, 17]. According to the clinical picture, preterm labor is divided into threatening, characterized by irregular contractions of the uterus and opening of the cervix up to 3-4 cm, and those that have begun - in this case, regular labor occurs and the cervix opens by 3-4 cm or more. Every third case of preterm birth occurs in primigravida, in which risk factors include previous abortions or spontaneous miscarriages, urinary tract infections, inflammatory diseases of the genitals [9, 15, 18, 21].
The diagnosis of the onset of preterm labor is associated with certain difficulties due to the absence of specific symptoms. Predicting the onset of preterm labor is an extremely important problem in practical terms, since in about 50% of cases, the contractile activity of the uterus spontaneously stops [2, 4]. As a predictor of preterm birth, an express test for determining the phosphorylated form of protein-1 is currently quite successfully used, the diagnostic sensitivity of which is 88.9%, and the diagnostic specificity is 100% [10].
As a predictor of preterm birth, an express test for determining the phosphorylated form of protein-1 is currently quite successfully used, the diagnostic sensitivity of which is 88.9%, and the diagnostic specificity is 100% [10].
Phosphorylated IGF-binding protein-1 is synthesized by decidual cells. Amniotic fluid, fetal and pregnant serum, on the contrary, contain a large amount of non-phosphorylated PSIFR-1. As the due date approaches, the amniotic membranes begin to separate from the decidua, resulting in the release of a small amount of fPSIFR-1. A negative result indicates a low risk of preterm delivery within 7 days of the test. Negative predictive value - 9four%.
At the first stage of the study, we performed a retrospective clinical and statistical analysis of 137 preterm birth histories. These studies were carried out according to a specially developed examination methodology, which took into account passport, anamnestic, clinical data, information about education, the presence of occupational hazards, parity, the course of previous and current pregnancy and childbirth, as well as the state and outcome of childbirth for the fetus and newborn . Risk factors were identified and high-risk groups for preterm birth were formed. nine0003
Risk factors were identified and high-risk groups for preterm birth were formed. nine0003
At the second stage, which constituted the main part of the study, a dynamic prospective observation of 143 pregnant women was carried out from the moment of their registration to discharge from the hospital after delivery. This group was formed on the basis of questionnaire data, during which risk factors for preterm birth were found out.
Inclusion criteria: presence of urogenital infection, diagnosed isthmic-cervical insufficiency, placental insufficiency and anamnestic factors (history of preterm birth, multiple intrauterine interventions, history of placental abruption). nine0003
Exclusion criteria: severe extragenital pathology, multiple pregnancy.
All observed pregnant women underwent an in-depth clinical examination.
Birth outcomes for the fetus, during the early neonatal period were analyzed in 280 newborns. In the course of the work, general clinical (clinical-anamnestic, laboratory), special (ultrasound, Doppler, CTG), genetic, pathological-anatomical, immunological and statistical research methods were used. nine0003
nine0003
To fulfill the objectives of the study, including the use of highly sensitive test systems based on the determination of protein-1 that binds insulin-like growth factor in the vaginal discharge, 85 patients with a threatened miscarriage and 29 patients with diagnosed mutations in thrombophilia genes were selected from among the examined pregnant women , with the subsequent use of low molecular weight heparin, familiarized with the purpose and methods of the study, who gave written consent to their inclusion in the scientific study. nine0003
Patients of both groups included in the study were comparable in age and somatic health. In the retrospective group (RG), all analyzed patients had a complicated course of pregnancy (Table 1).
Analysis of risk factors for preterm birth in the prospective group (PG) showed a similar risk frequency distribution as in the WG. In both groups, a third of cases had a combination of risk factors (R=0.22; p=0.01). Analyzing the state of the somatic status, it is worth noting that in chronic kidney diseases, as well as in conditions of asymptomatic bacteriuria, childbirth up to 28 weeks. occurred 3 times more often (58%) than at 33–37 weeks. — 17% (p<0.01). Vaginal infection in our study occupies a key position, because in 18 cases, childbirth occurred before 28 weeks, which is almost 6 times higher than those during childbirth at 33–37 weeks. (p<0.01). Half of births at 28-33 weeks. occurred against the background of a vaginal infection - 51% (p<0.01). At birth at 28-37 weeks. placenta previa was noted in 17.86% of cases. nine0003
occurred 3 times more often (58%) than at 33–37 weeks. — 17% (p<0.01). Vaginal infection in our study occupies a key position, because in 18 cases, childbirth occurred before 28 weeks, which is almost 6 times higher than those during childbirth at 33–37 weeks. (p<0.01). Half of births at 28-33 weeks. occurred against the background of a vaginal infection - 51% (p<0.01). At birth at 28-37 weeks. placenta previa was noted in 17.86% of cases. nine0003
Anomalies of placenta previa were observed 5 times more often in preterm births before 28 weeks than in births at 33-37 weeks. (p<0.01). Premature placental abruption occurred in 23 (16.8%) cases, up to 28 weeks. - 31.6%, for a period of 28-32 weeks. 6 days - 13.1% and for a period of 33-37 weeks. — 17.7% (p<0.01) (Fig. 1).
We noted that all women of the RG had a aggravated obstetric and gynecological history. Thus, 56.93% of women had a history of preterm birth, 33.58% had artificial termination of pregnancy or diagnostic curettage, and 24. 82% had surgical interventions on the cervix in anamnesis (Table 2). nine0003
82% had surgical interventions on the cervix in anamnesis (Table 2). nine0003
In 54% of RG patients, pregnancy proceeded with the threat of termination at various times, of which 89% received inpatient care. Tocolytic therapy in the hospital was carried out mainly with magnesium sulfate preparations - 54%, β-agonists - 27%, non-steroidal anti-inflammatory drugs - 11%, their combination occurred in 7.5% of cases. Therapy with β-agonists and non-steroidal anti-inflammatory drugs for up to 28 weeks. was not assigned.
The closest relatives of the analyzed pregnant women in the study of heredity were noted in 24 cases of strokes, deep vein thrombosis and heart attacks. When studying the anamnesis of women in the retrospective group, premature detachment of the placenta was noted in 17% of cases, placental insufficiency with intrauterine growth retardation in 53% of cases. In such patients, in 63.33% of cases, very early preterm labor occurred, which is 3 times more likely than childbirth at 33–37 weeks. (R=0.21; p=0.01). nine0003
(R=0.21; p=0.01). nine0003
In 63% of cases, preterm birth before 28 weeks. began with premature rupture of amniotic fluid, at a period of 28-32 weeks. 6 days - in 74%, at birth at 33–37 weeks. — in 30% of cases (p<0.02).
The frequency of preterm birth in the period 2010-2012, according to statistical reports, ranged from 7.8 to 10.6% (Fig. 2).
All pregnant PGs were registered before 6 weeks of gestation, after ultrasound, specifying the gestational age and the place of implantation of the ovum. nine0003
During self-screening for vaginal infection, a deviation in the pH value of vaginal contents in PG was detected in 43% of pregnant women. A bacterioscopic study found that bacterial vaginosis occurs in 37 (59.68%) cases, vaginal candidiasis - in 11 (17.74%), nonspecific vaginitis - in 14 (22.58%) cases (p<0.05) (Table 3).
VPG examination for mutations in the hemostasis system was carried out in all pregnant women with a history of preterm birth - in 59% of cases, premature placental abruption - in 19%, placenta previa — in 17% of cases. In a third of pregnant women out of 102 examined, mutations in the genes of the hemostasis system were detected (Table 4). All pregnant women with confirmed genetic mutations of thrombophilia were hospitalized for additional examination and selection of therapy with low molecular weight heparins.
In a third of pregnant women out of 102 examined, mutations in the genes of the hemostasis system were detected (Table 4). All pregnant women with confirmed genetic mutations of thrombophilia were hospitalized for additional examination and selection of therapy with low molecular weight heparins.
Patients with a mutation in the MTFHR gene (C667TT) additionally received folic acid preparations during pregnancy. Homocysteine levels were assessed. Dynamic monitoring of treatment was carried out according to hemostasiogram parameters 1 time in 2 weeks. nine0003
When dealing with complaints of discomfort or pain in the lower abdomen, starting from 22 weeks. gestation, in 85 pregnant women, a highly sensitive test on strips was used to diagnose and predict the onset of preterm labor, which determines the phosphorylated form of protein-1 that binds insulin-like growth factor. In 53% of cases of threatened abortion, a positive result was obtained at the first visit, confirmed by ultrasound and manual examination, these pregnant women were hospitalized, 47% of patients continued outpatient monitoring. The assessment of the quality of therapy, the threat of termination of pregnancy in the hospital was carried out using a repeated test for the determination of fPSIFR-1 (Fig. 3). nine0003
The assessment of the quality of therapy, the threat of termination of pregnancy in the hospital was carried out using a repeated test for the determination of fPSIFR-1 (Fig. 3). nine0003
We noted that with the use of β-agonists, the frequency of repeated positive results during testing is 2 times lower than with the use of calcium channel blockers and NSAIDs (P<0.02). According to the results of our study, the most preferable for removing the threat of termination of pregnancy for up to 28 weeks. is a calcium channel blocker - nifedipine, and for a period of 28-33 weeks. - magnesium sulfate and hexaprenaline sulfate (p<0.02).
In RG very early preterm birth before 28 weeks. gestations occurred at 13.9% of cases, early at 28-32 weeks. 6 days - 61.3% and childbirth at 33–37 weeks. — in 25.8% of cases. In PG, thanks to the comprehensive prevention, preterm birth up to 28 weeks. did not happen. Childbirth at 28–32 weeks. 6 days pregnancies occurred in 2 cases.
Analysis of data by group showed that preterm birth at 33-37 weeks. in WG (4.4%) ended in caesarean section 2 times less often than in PG (11.9%) (R=0.17; p=0.01) (Table 5).
in WG (4.4%) ended in caesarean section 2 times less often than in PG (11.9%) (R=0.17; p=0.01) (Table 5).
Patients with hereditary thrombophilia had vaginal delivery at 33–37 weeks of gestation. occurred at 6.9% of cases (p<0.01), at 37–40 weeks gestation by caesarean section - in 10.3%, through the birth canal - in 79.3% of cases (p<0.01).
143 children were born in PG. Of these, for a period of 28–32 weeks. 6 days - 2.1%, 33-37 weeks. - 16.1% and at full term - 81.8% of children. 42 children were born surgically, 101 were born naturally (Fig. 4). In the retrospective group at 28–32 weeks. 6 days the leading diseases were pneumonia — 66.1%, conjugative jaundice — 37.3%, membrane respiratory distress syndrome — 59.3% (p<0.02). Comparing the results in groups, it is worth noting that the incidence of pneumonia and respiratory distress syndrome in premature babies in PG decreased by 4 times compared to RG (R=0.17; p=0.02).
In PH, the first place in the structure of morbidity was edematous syndrome — 21. 7%, conjugative jaundice — 17.4%, hemolytic disease — 17.4%, pneumonia and respiratory distress syndrome — 13.1% each (Fig. five).
7%, conjugative jaundice — 17.4%, hemolytic disease — 17.4%, pneumonia and respiratory distress syndrome — 13.1% each (Fig. five).
Comparing the results in groups, it is worth noting that the incidence of pneumonia and respiratory distress syndrome in premature babies in PG decreased by 4 times compared with RG (R=0.17; p=0.02). The number of children in PG (21.7%) in need of artificial lung ventilation decreased 3 times compared to RG (R=0.21; p=0.02). nine0003
The formation of high-risk groups for preterm birth allows you to optimize diagnostic and therapeutic tactics. Detection of a urogenital infection using a simple self-diagnosis test to determine the pH of the vaginal environment, followed by bacterioscopic examination and sanitation, can reduce the incidence of preterm birth. It is necessary to determine thrombophilia, and in particular hereditary mutations in thrombophilia genes, with the prophylactic use of low molecular weight heparins. The correct selection of tocolytic therapy using a modern highly sensitive test system that determines the phosphorylated form of protein-1 that binds insulin-like growth factor in the vaginal discharge, to assess its effectiveness, helps to reduce the incidence of preterm birth.