Preeclampsia during birth
Preeclampsia: Signs, causes, risk factors, and treatment
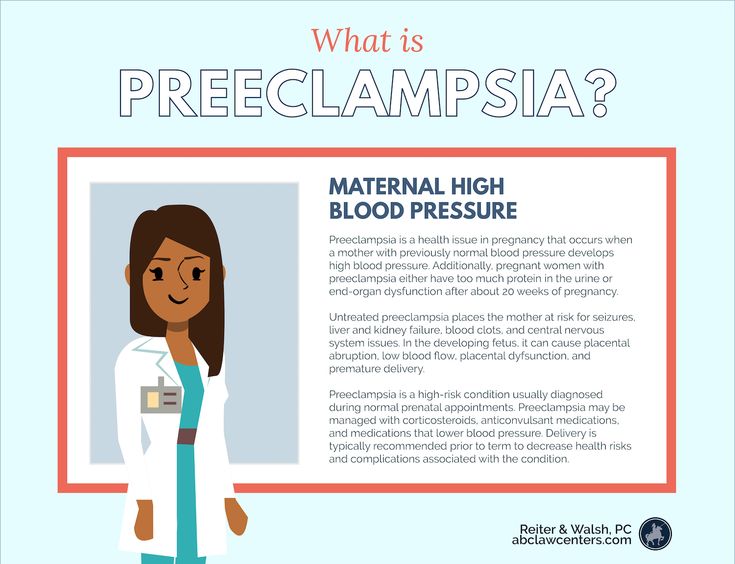
Preeclampsia is a very serious blood pressure disorder that happens after 20 weeks of pregnancy, during labor, or postpartum. It's caused by abnormal blood flow within the placenta. The most common symptom is unusual swelling. Your healthcare provider will check your blood pressure at each prenatal visit and, if it's high, test for protein in your urine. If you have preeclampsia, you'll probably be given medication. If your symptoms become severe or your baby isn't doing well, you'll be admitted to the hospital for delivery.
What is preeclampsia?
Preeclampsia is a serious high blood pressure disorder that happens during pregnancy or soon after childbirth. It's a potentially life-threatening condition that affects about 5 percent of pregnancies in the United States. With proper care, most pregnant women with preeclampsia have healthy babies and stay healthy themselves.
Preeclampsia may not cause any noticeable symptoms but can still be very dangerous for you and your baby, even if you feel fine. Your healthcare provider will screen you for the condition at every prenatal visit by taking your blood pressure, and, if it's high, testing your urine for protein.
Preeclampsia most commonly develops during the last trimester. (Ninety percent of cases occur at 34 weeks or later), but it can happen at any time after 20 weeks, during labor, or even up to six weeks after delivery. When it develops before 34 weeks it's called early-onset preeclampsia.
What causes preeclampsia?
Experts believe that preeclampsia is caused by abnormal blood flow within the placenta. In many women, the roots of their preeclampsia stretch back to the early days of their pregnancy.
Preeclampsia is a disease of abnormal blood vessels. The placenta learns to grow from signals from maternal circulation. If a mom's blood vessels have damage – from long-term diabetes or chronic hypertension, for example – they will "teach" this damage to the growing placenta, increasing the risk of preeclampsia.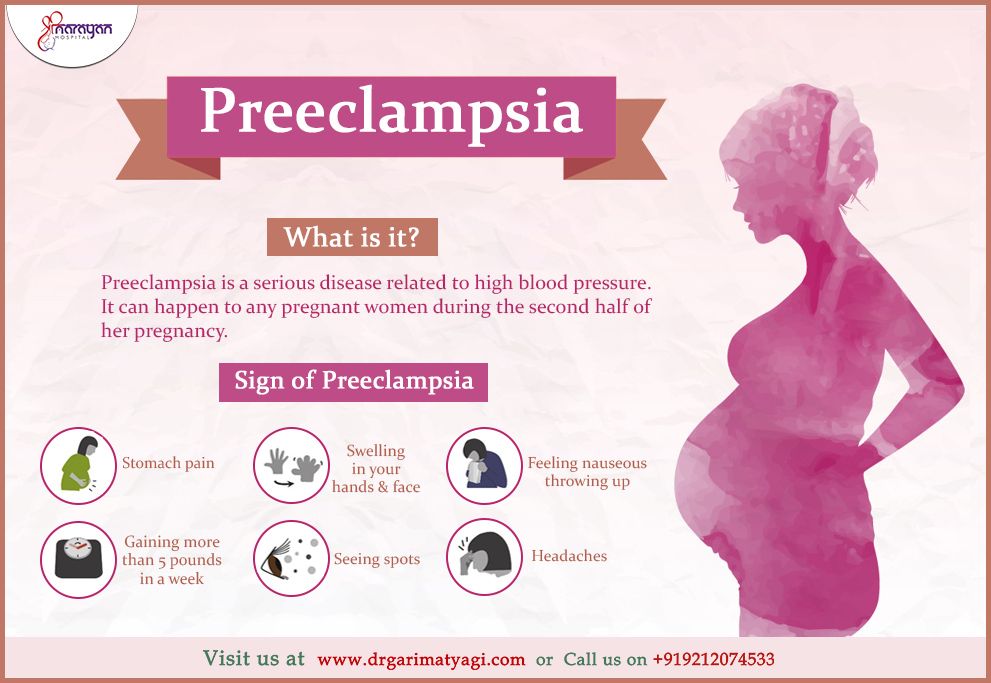
There's also evidence that changes in blood flow within the placenta trigger the release of high levels of certain placental proteins into your bloodstream. This can set off a complex chain of reactions that includes:
- Constricted blood vessels, leading to high blood pressure
- Damage to the vessel walls, leading to swelling and protein in your urine
- Kidney and liver damage, leading to pain and reduced urine output
- Dramatic drop in platelets, leading to a difficulty clotting normally and a potential increase in your blood loss during delivery
- Swelling around your brain, leading to headaches and/or seizures
- Reduced blood flow to your baby, leading to growth restriction or low amniotic fluid
Why this happens to some women and not others isn't fully understood, and there's probably no single explanation. Genetics, nutrition, certain underlying diseases, the way your immune system reacts to pregnancy, and other factors may all play a role.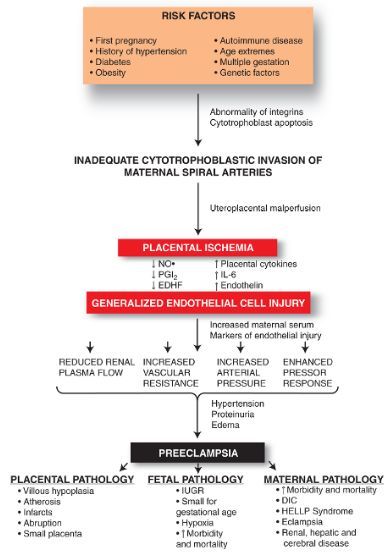
Preeclampsia symptoms
Preeclampsia doesn't always cause noticeable symptoms, especially in the early stages, and symptoms can also vary from woman to woman. Some signs of preeclampsia – such as swelling, nausea, and weight gain – may seem like normal pregnancy complaints, so it's important to be aware of any potential warning signs.
Advertisement | page continues below
Unusual swelling is the most common symptom of preeclampsia, so call your healthcare provider if you:
- Notice swelling in your face or puffiness around your eyes
- Have more than slight swelling in your hands
- Have sudden or excessive swelling of your feet or ankles
- Gain more than 4 pounds in a week (often a result of water retention)
Note: Not all women with preeclampsia have obvious swelling or dramatic weight gain, and not all women with swelling or rapid weight gain have preeclampsia.
Preeclampsia complications
Most women who get preeclampsia develop it near their due dates and do fine with proper care.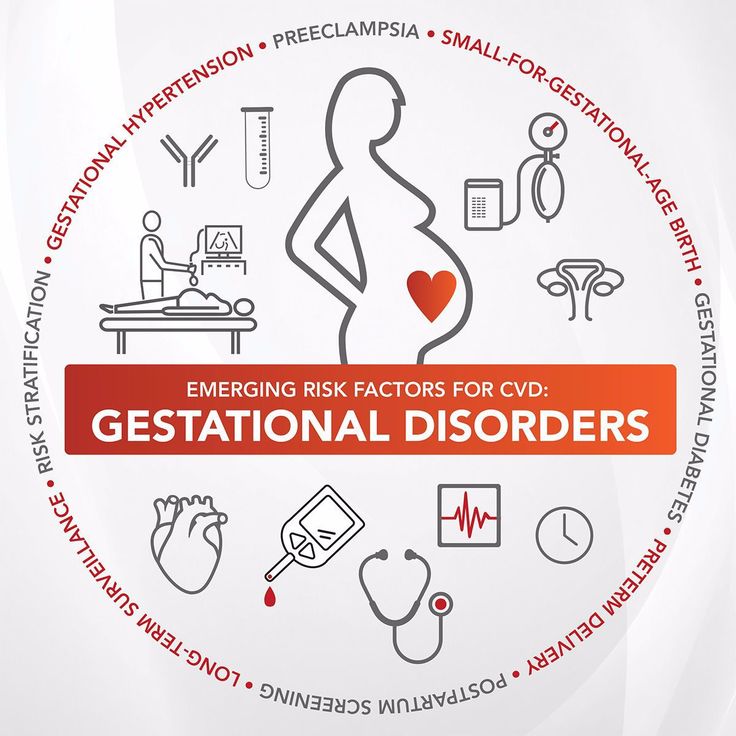 But the earlier you have it, and the more severe it is, the greater the risks for you and your baby.
But the earlier you have it, and the more severe it is, the greater the risks for you and your baby.
Here's what can happen:
- High blood pressure and preeclampsia can affect your liver, kidneys, eyes, and other body systems.
- Severe high blood pressure in pregnancy can cause a stroke.(Strokes happen at much lower blood pressures during pregnancy.)
- Abnormal blood flow in the uterus can cause complications for your baby, such as poor growth and too little amniotic fluid.
- Uncontrolled hypertension can lead to placental abruption (when the placenta separates from the uterine wall before delivery).
- You may need to deliver early if the condition is severe or getting worse. In this case your baby may suffer effects of prematurity. Fifteen percent of premature births in the United States are due to preeclampsia.
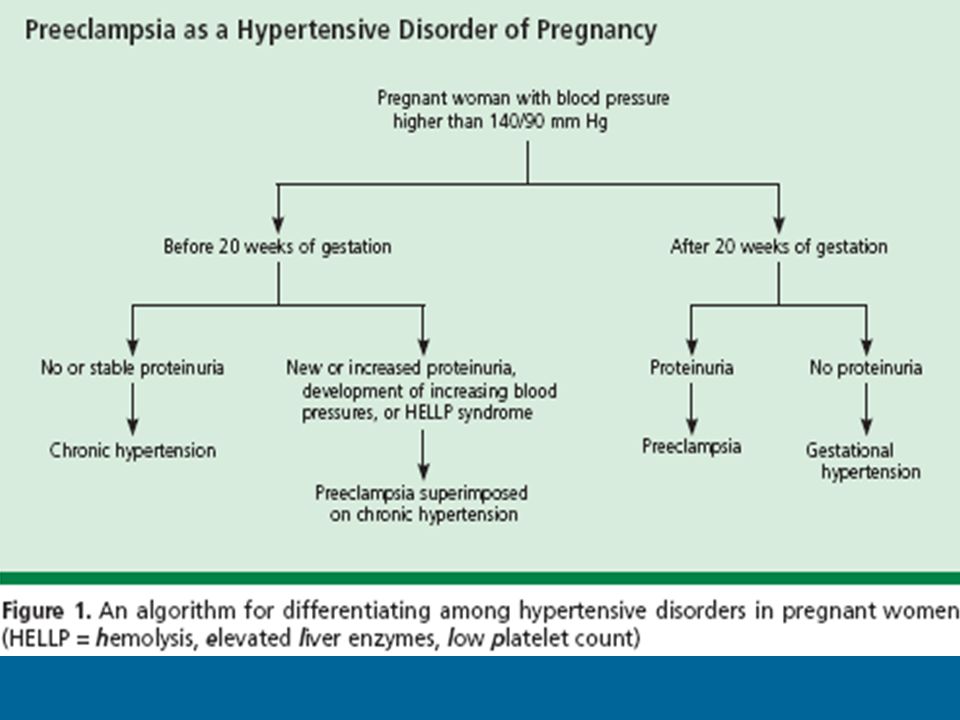
- In some cases, preeclampsia can lead to very serious complications such as eclampsia (marked by seizures) and HELLP syndrome.
 HELLP stands for Hemolysis (the destruction of red blood cells), Elevated Liver enzymes, and Low Platelet count.
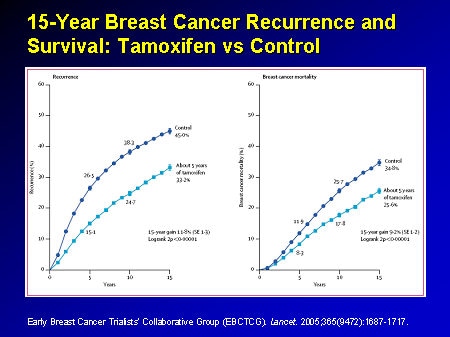
HELLP stands for Hemolysis (the destruction of red blood cells), Elevated Liver enzymes, and Low Platelet count. - Preeclampsia is linked to future heart and cardiovascular disease, especially if you've had it more than once or have had preterm preeclampsia. (Experts aren't sure if this is because people who get preeclampsia are also likely to get heart disease or if preeclampsia increases the risk of heart disease.)
If you have any of these warning signs of severe preeclampsia or HELLP syndrome:
- Severe or persistent headache
- Vision changes, including double vision, blurriness, seeing spots or flashing lights, light sensitivity, or temporary vision loss
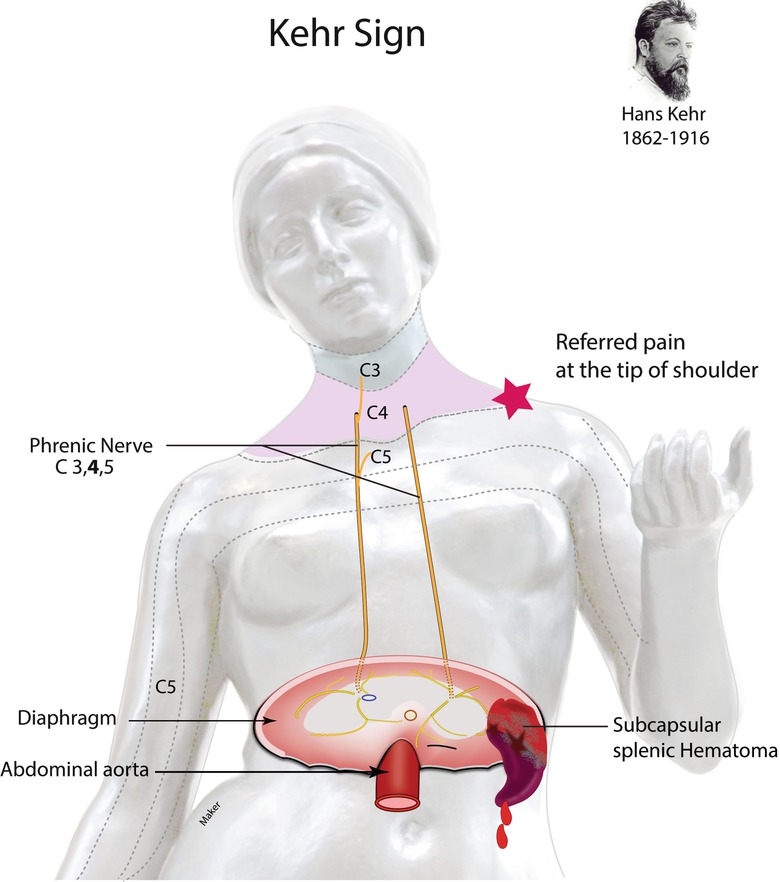
- Intense pain or tenderness in your upper abdomen or shoulder
- Chest pain
- Difficulty breathing
- New onset nausea and vomiting in the second half of pregnancy
Preeclampsia risk factors
It's more common to get preeclampsia during a first pregnancy. However, once you've had preeclampsia, you're more likely to develop it again in later pregnancies. The more severe the condition and the earlier it appears, the higher your risk.
However, once you've had preeclampsia, you're more likely to develop it again in later pregnancies. The more severe the condition and the earlier it appears, the higher your risk.
- If you had preeclampsia at the very end of your previous pregnancy, the chance of it happening again is fairly low – about 13 percent.
- If you developed severe preeclampsia before 29 weeks of pregnancy, your chance of getting it again may be 40 percent or even higher.
- If you had preeclampsia in two previous pregnancies, your risk of getting it in a third is about 30 percent.
Other risk factors for preeclampsia include:
- Having a family history (mother or sister) of preeclampsia
- Being obese (having a body mass index of 30 or more)
- Being African American
- Carrying twins or more
- Being younger than 20 or older than 35
- Having in vitro fertilization (IVF)
- Having a history of stillbirth
Certain health conditions may also make it more likely you'll develop preeclampsia.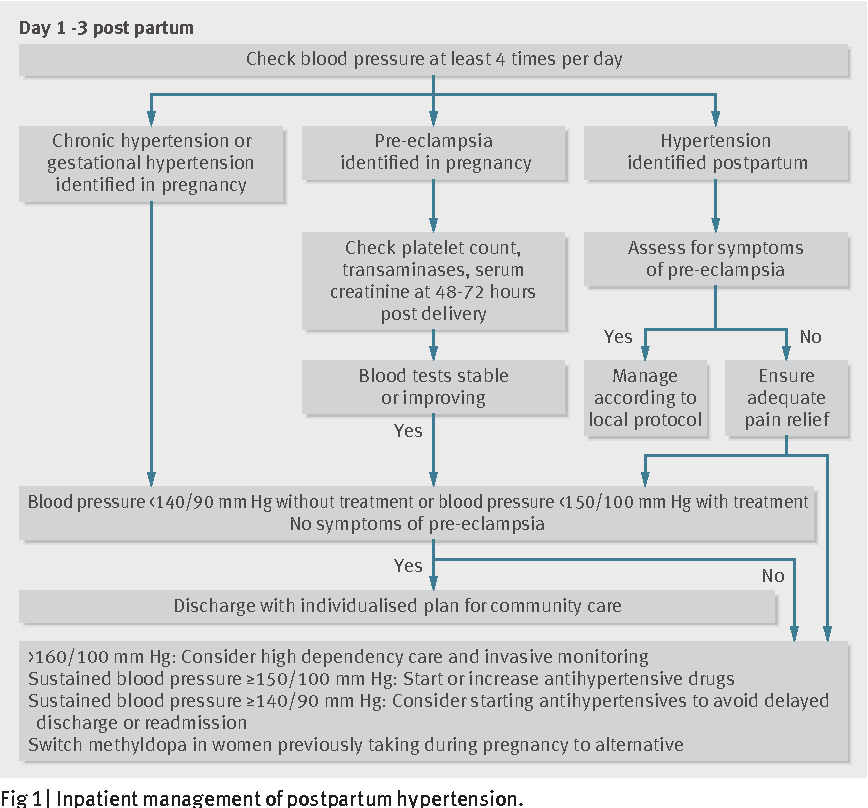 These include:
These include:
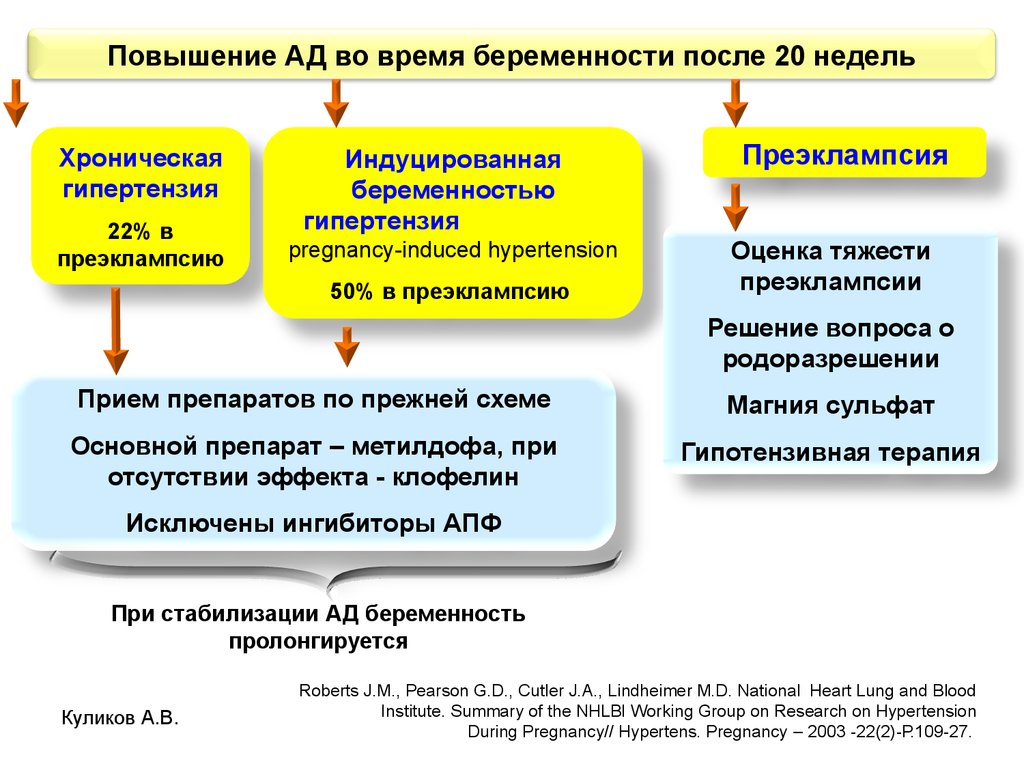
- Chronic hypertension or gestational hypertension
- Certain blood clotting disorders, such as thrombophilia or antiphospholipid syndrome
- Diabetes or kidney disease
- Autoimmune diseases, such as lupus
- Periodontal disease
If you're at risk for preeclampsia, your provider may schedule more frequent prenatal visits in your third trimester to monitor you closely. You'll likely be asked to monitor your blood pressure at home, too.
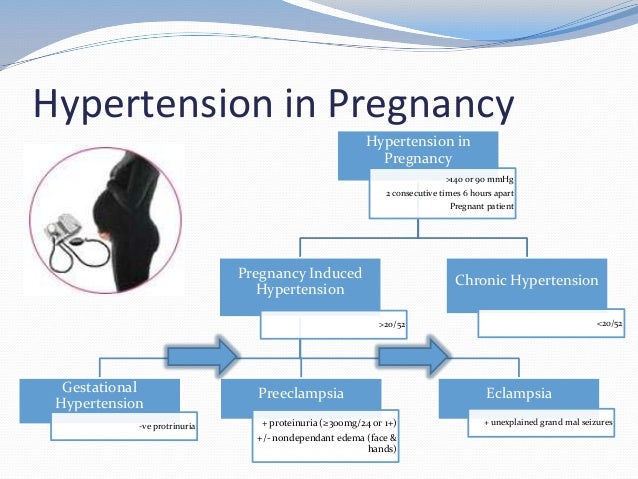
How is preeclampsia diagnosed?
Your healthcare provider will check for high blood pressure and protein in your urine and may order more tests as well, such as:
- Blood pressure checks. Your blood pressure is considered high if you have a systolic reading of 140 or greater (the upper number in the reading) or a diastolic reading of 90 or higher (the lower number). Because blood pressure changes during the day, you'll have more than one reading to confirm that it's consistently high.

- Urine tests for protein. You may have a one-time test that checks the protein-to-creatinine ratio (creatinine is a waste product that your kidneys should filter out). Or you may need to collect all your urine for 24 hours to check the total protein.
- Blood tests. If preeclampsia is a concern, your provider will order regular blood tests, including complete blood counts (CBC) and tests for liver and kidney function. These also screen for HELLP syndrome.
- Tests of baby's health. You'll likely have ultrasounds to monitor your baby's growth and amniotic fluid, and possibly a biophysical profile or nonstress test to see how your baby's doing.
Preeclampsia treatment
If you're diagnosed with preeclampsia, you and your baby will be monitored closely for the rest of your pregnancy.
Medication
If your blood pressure is extremely high, you'll be given medication immediately to lower it. If it's not extremely high, you may or may not be given medication, depending on how close you are to delivering your baby.
If it's not extremely high, you may or may not be given medication, depending on how close you are to delivering your baby.
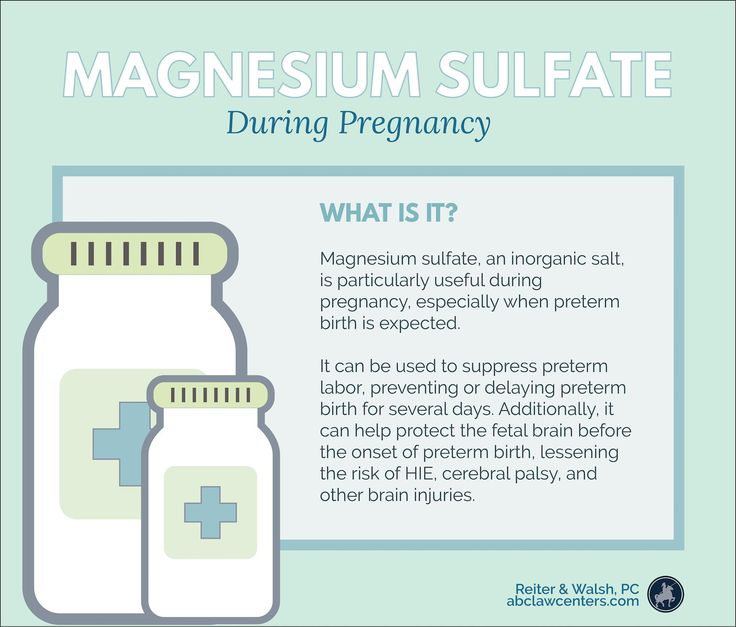
If you have preeclampsia with severe features, you'll also be given an IV medication called magnesium sulfate. This is to prevent eclampsia (seizures). Magnesium sulfate can have unpleasant side effects in some women, including nausea, flu-like symptoms, fatigue, and thirst, but it's an important part of the treatment of preeclampsia to reduce your serious risk of seizures.
Rest
Some providers may recommend restricting your activities because your blood pressure will generally be lower when you're taking it easy. But complete bedrest, in which you're confined to bed for an extended period, raises your risk of blood clots and isn't recommended.
Hospitalization
If at any time your symptoms indicate that your condition is getting severe, or that your baby isn't thriving, you'll be admitted to the hospital and will probably need to deliver early. It's not unusual for preeclampsia to become more severe during delivery, so you'll be monitored very closely throughout the birth.
It's not unusual for preeclampsia to become more severe during delivery, so you'll be monitored very closely throughout the birth.
If you're diagnosed with severe preeclampsia, you'll have to spend the rest of your pregnancy in the hospital. You may be transferred to a hospital where a high-risk pregnancy specialist can care for you.
Delivery
The only way to "treat" preeclampsia is by delivering your baby. Unless your condition or your baby's condition is so fragile that immediate delivery is needed, a c-section isn't required.
You'll probably be induced if any of the following happen:
- You're at 37 weeks or more, especially if your cervix is starting to thin out and dilate
- Your preeclampsia is getting worse
- Your baby isn't thriving
If you and your baby are doing fine, you're not yet at 37 weeks, and your preeclampsia isn't severe, you may remain in the hospital so you can be monitored. Or you may be sent home, where you may have to monitor your blood pressure.
You may be given corticosteroids to help your baby's lungs mature more quickly. (Steroids are not given to women who are diabetic and over 34 weeks, however).
After delivery
After delivery, you'll remain under close medical supervision for a few days. Most women, especially those with non-severe (or "mild") preeclampsia, see their blood pressure start to go down in a day or so.
In many cases, though, blood pressure can remain elevated for longer. Or it may go down right after delivery but start to go up again by 3 to 5 days postpartum. If either is the case for you, you'll be given blood pressure medication for a few weeks to months. You'll be asked to check your blood pressure at home and to make follow-up blood pressure appointments with your provider in the days and weeks following your delivery.
If you have severe preeclampsia, you'll probably be given magnesium sulfate intravenously for at least 24 hours after delivery to prevent seizures.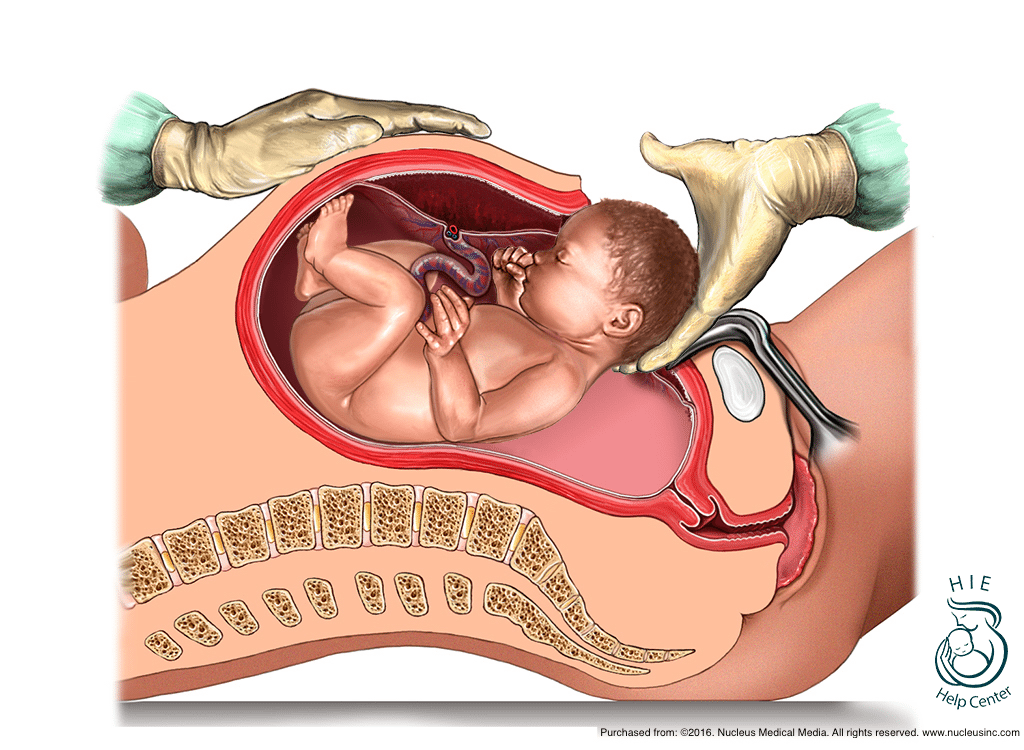 (You may also need to take blood pressure medication at home.)
(You may also need to take blood pressure medication at home.)
Postpartum preeclampsia
If you develop preeclampsia during or after labor, you'll be monitored closely. Depending on your situation, you may be given magnesium sulfate to prevent seizures and medication to reduce your blood pressure.
Sometimes cases of preeclampsia, eclampsia, and HELLP syndrome develop after delivery, usually within the first 48 hours but as late as six weeks after delivery.
You'll likely have a follow-up blood pressure check within one week of discharge from the hospital, but if you start to experience any symptoms of preeclampsia or HELLP, such as a severe headache, a pain high up in your abdomen, or changes to your vision, contact your healthcare provider right away.
How to prevent preeclampsia
To reduce your risk of developing preeclampsia, your provider may recommend that you try:
- Low-dose aspirin therapy. Currently this is considered the best prevention for preeclampsia and is recommended for anyone at risk.
 According to guidelines from the American College of Obstetricians and Gynecologists, high-risk women may start taking low-dose aspirin after 12 weeks of pregnancy. Ask your provider if this is right for you – and never take aspirin during pregnancy unless your provider advises it.
According to guidelines from the American College of Obstetricians and Gynecologists, high-risk women may start taking low-dose aspirin after 12 weeks of pregnancy. Ask your provider if this is right for you – and never take aspirin during pregnancy unless your provider advises it. - Vitamin D supplementation. Some studies point to a link between vitamin D and a lowered risk of preeclampsia, but other studies don't support this link. Your healthcare provider may check to make sure that you're not deficient in vitamin D.
- Calcium supplements. For women who were deficient in calcium before pregnancy, a calcium supplement might be preventative for preeclampsia. But some experts say that women in developed countries are unlikely to have a calcium deficiency severe enough to benefit from this.
You'll also want to:
- Get good prenatal care. Schedule and keep all your appointments. At each visit, your healthcare provider will check your blood pressure.

- Know the warning signs. Understanding the symptoms of preeclampsia means you can alert your provider and start treatment as soon as possible.
If you're not pregnant yet, you can reduce your risk of preeclampsia by:
- Maintaining a healthy weight
- Keeping your blood pressure in check
- Working with your doctor to manage any chronic conditions that raise your risk, such as diabetes or lupus
- Going to the dentist regularly. There's some evidence that periodontal disease may be linked to an increased risk for preeclampsia.
Find out more about preeclampsia
Call the Preeclampsia Foundation at (800) 665-9341 or visit preeclampsia.org.
Visit the Society for Maternal-Fetal Medicine's website for more information and to find an MFM specialist near you.
Learn more:
- Pregnancy symptoms you should never ignore
- Prenatal tests: An overview
- The ultimate pregnancy to-do list: Third trimester
Preeclampsia | March of Dimes
Preeclampsia is a kind of high blood pressure some women get after the 20th week of pregnancy or after giving birth.
Most pregnant women with preeclampsia have healthy babies. But if not treated, it can cause serious problems, like preterm birth and even death.
If you’re at risk for preeclampsia, your provider may want you take low-dose aspirin to help prevent it.
If you have blurred vision, swelling in your hands and face or severe headaches or belly pain, call your provider right away.
You can have preeclampsia and not know it, so go to all of your prenatal care visits, even if you’re feeling fine.
Download our English and Spanish health action sheets on low-dose aspirin.
What is preeclampsia?
Preeclampsia is a serious condition that can happen after the 20th week of pregnancy or after giving birth (called postpartum preeclampsia). In addition to causing high blood pressure, it can cause organs, like the kidneys and liver, to not work normally. Blood pressure is the force of blood that pushes against the walls of your arteries.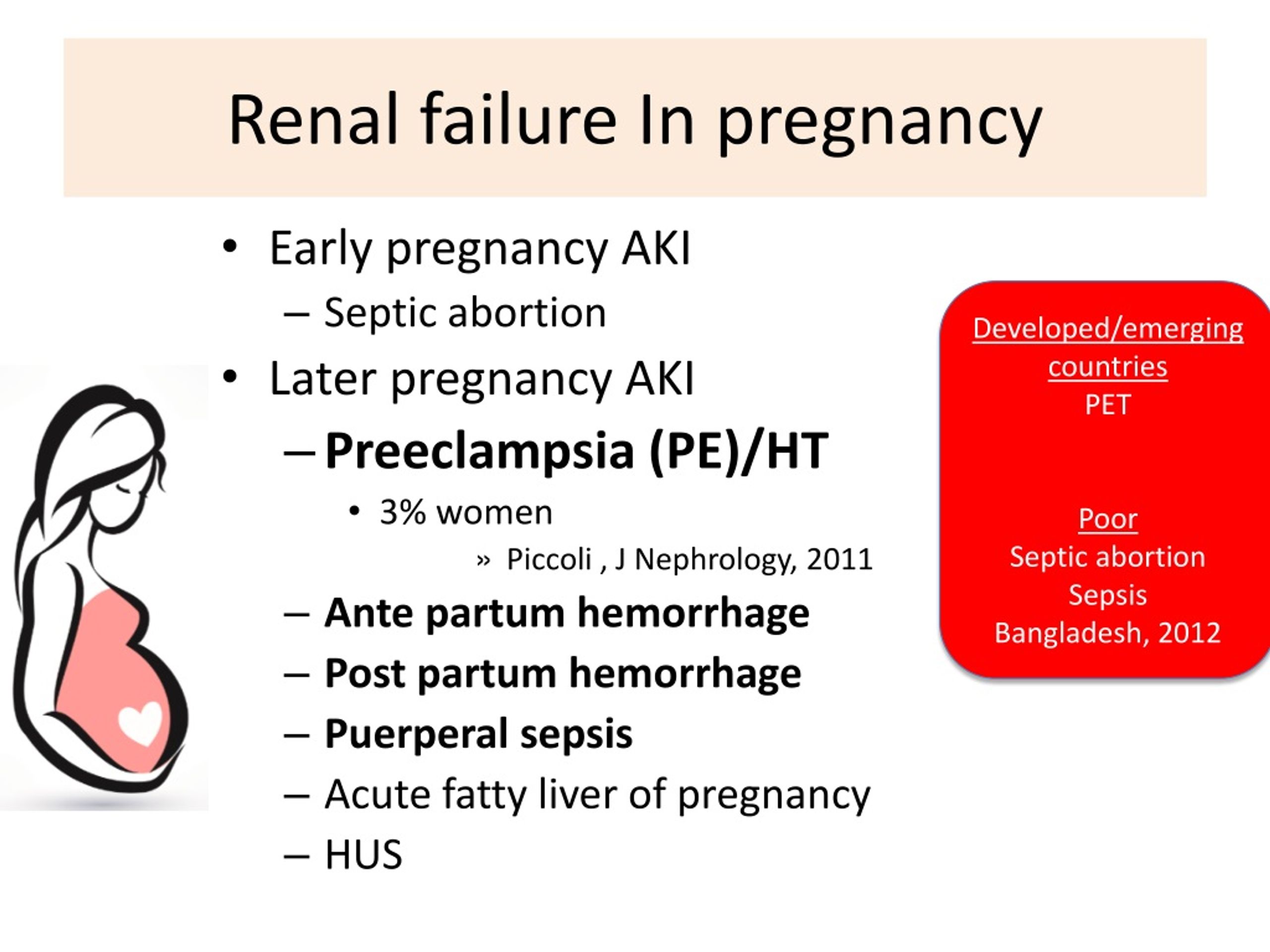 High blood pressure (also called hypertension) is when the force of blood against the walls of the blood vessels is too high. Arteries are blood vessels that carry blood away from your heart to other parts of the body. Having high blood pressure can stress your heart and cause problems during pregnancy.
High blood pressure (also called hypertension) is when the force of blood against the walls of the blood vessels is too high. Arteries are blood vessels that carry blood away from your heart to other parts of the body. Having high blood pressure can stress your heart and cause problems during pregnancy.
Preeclampsia is a serious health problem for women around the world. Between 10 to 15 percent of maternal deaths worldwide are caused by preeclampsia and associated complications, such as eclampsia. In the United States, it affects between 5 to 8 percent of pregnancies, and in most cases leads to preterm birth. Preterm birth is birth that happens too early, before 37 weeks of pregnancy.
Most women with preeclampsia have healthy babies. But if not treated, it can cause severe health problems for you and your baby.
Can taking low-dose aspirin help reduce your risk for preeclampsia and preterm birth?
For some women, yes. If your provider thinks you’re at risk for preeclampsia, low-dose aspirin may be recommended to help prevent it. Low-dose aspirin also is called baby aspirin or 81 mg (milligrams) aspirin. Talk to your provider to see if treatment with low-dose aspirin is right for you.
Low-dose aspirin also is called baby aspirin or 81 mg (milligrams) aspirin. Talk to your provider to see if treatment with low-dose aspirin is right for you.
You can buy low-dose aspirin over-the-counter, or your provider can give you a prescription for it. If your provider wants you to take low-dose aspirin to help prevent preeclampsia, take it exactly as it’s recommended. Don’t take more or take it more often than your provider says.
If you’re at high risk for preeclampsia, your provider may want you to start taking low-dose aspirin after 12 weeks of pregnancy. If you have diabetes or high blood pressure, your provider may ask you to take low-dose aspirin.
According to the American College of Obstetricians and Gynecologists (also called ACOG), daily low-dose aspirin use in pregnancy has a low risk of serious complications and its use is considered safe.
Are you at risk for preeclampsia?
We don’t know for sure what causes preeclampsia, but there are some things that may make you more likely than other women to have it. These are called risk factors. If you have even one risk factor for preeclampsia, tell your provider.
These are called risk factors. If you have even one risk factor for preeclampsia, tell your provider.
You’re at high risk for preeclampsia If:
- You’ve had preeclampsia in a previous pregnancy. The earlier in pregnancy you had preeclampsia, the higher your risk is to have it again. You’re also at higher risk if you had preeclampsia along with other pregnancy complications.
- You’re pregnant with multiples (twins, triplets or more).
- You have high blood pressure, diabetes, kidney disease or an autoimmune disease like lupus or antiphospholipid syndrome. Diabetes is when your body has too much sugar in the blood. This can damage organs, like blood vessels, nerves, eyes and kidneys. An autoimmune disease is a health condition that happens when antibodies (cells in the body that fight off infections) attack healthy tissue by mistake.
Other risk factors for preeclampsia:
- You’ve never had a baby before, or it’s been more than 10 years since you had a baby.

- You’re a person who has obesity. Obese means being very overweight with a body mass index (also called BMI) of 30 or higher. To find out your BMI, go to www.cdc.gov/bmi.
- You have a family history of preeclampsia. This means that other people in your family, like your sister or mother, have had it.
- You had complications in a previous pregnancy, like having a baby with low birthweight. Low birthweight is when your baby is born weighing less than 5 pounds, 8 ounces.
- You had fertility treatment called in vitro fertilization (also called IVF) to help you get pregnant.
- You’re older than 35.
Some groups, such as African-American women and those who are affected by lower income, are also at higher risk of complications like preeclampsia. Historically, in the United States, these groups have had a harder time getting good quality health care and access to treatments that prevent illness. This has led to serious health disparities and unequal health outcomes. Talk to your provider about your risk factors and about what you can do to stay healthy and reduce your chances of having a preterm birth. If your provider thinks you’re at risk of having preeclampsia, ask if treatment with low-dose aspirin is right for you.
Talk to your provider about your risk factors and about what you can do to stay healthy and reduce your chances of having a preterm birth. If your provider thinks you’re at risk of having preeclampsia, ask if treatment with low-dose aspirin is right for you.
What are the signs and symptoms of preeclampsia?
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy.
Signs and symptoms of preeclampsia include:
- High blood pressure with or without protein in the urine. Your provider will check these during your prenatal visit.
- Changes in vision, like blurriness, flashing lights, seeing spots or being sensitive to light
- Headache that doesn’t go away
- Nausea (feeling sick to your stomach), vomiting or dizziness
- Pain in the upper right belly area or in the shoulder
- Sudden weight gain (2 to 5 pounds in a week)
- Swelling in the legs, hands or face
- Trouble breathing
Many of these signs and symptoms are common discomforts of pregnancy. If you have even one sign or symptom, call your provider right away. Sometimes you don't realize you have preeclampsia. Go to all your prenatal visits, even if you feel fine. That’s the best way to detect preeclampsia.
If you have even one sign or symptom, call your provider right away. Sometimes you don't realize you have preeclampsia. Go to all your prenatal visits, even if you feel fine. That’s the best way to detect preeclampsia.
How can preeclampsia affect you and your baby?
Without treatment, preeclampsia can cause serious health problems for you and your baby, even death. You may have preeclampsia and not know it, so be sure to go to all your prenatal care checkups, even if you’re feeling fine. If you have any sign or symptom of preeclampsia, tell your provider.
Health problems for women who have preeclampsia include:
- Kidney, liver and brain damage
- Problems with how your blood clots. A blood clot is a mass or clump of blood that forms when blood changes from a liquid to a solid. Your body normally makes blood clots to stop bleeding after a scrape or cut. Problems with blood clots can cause serious bleeding problems.
- Eclampsia. This is a rare and life-threatening condition. It’s when a pregnant woman has seizures or a coma after preeclampsia. A coma is when you’re unconscious for a long period of time and can't respond to voices, sounds or activity.
- Stroke. This is when the blood supply to the brain is interrupted or reduced. Stroke can happen when a blood clot blocks a blood vessel that brings blood to the brain, or when a blood vessel in the brain bursts open.
Pregnancy complications from preeclampsia include:
- Preterm birth. Even with treatment, you may need to give birth early to help prevent serious health problems for you and your baby.
- Placental abruption. This is when the placenta separates from the wall of the uterus (womb) before birth. It can separate partially or completely. If you have placental abruption, your baby may not get enough oxygen and nutrients.
 Vaginal bleeding is the most common symptom of placental abruption after 20 weeks of pregnancy. If you have vaginal bleeding during pregnancy, tell your health care provider right away.
Vaginal bleeding is the most common symptom of placental abruption after 20 weeks of pregnancy. If you have vaginal bleeding during pregnancy, tell your health care provider right away. - Intrauterine growth restriction (also called IUGR). This is when a baby has poor growth in the womb. It can happen when mom has high blood pressure that narrows the blood vessels in the uterus and placenta. The placenta grows in the uterus and supplies your baby with food and oxygen through the umbilical cord. If your baby doesn’t get enough oxygen and nutrients in the womb, he may have IUGR.
- Low birthweight
Having preeclampsia increases your risk for postpartum hemorrhage (also called PPH). PPH is heavy bleeding after giving birth. It’s a rare condition, but if not treated, it can lead to shock and death. Shock is when your body’s organs don’t get enough blood flow.
Having preeclampsia increases your risk for heart disease, diabetes and kidney disease later in life.
How is preeclampsia diagnosed?
To diagnose preeclampsia, your provider measures your blood pressure and tests your urine for protein at every prenatal visit. Additional lab work evaluating your blood count, clotting factors, liver and kidney function are also assessed.
Your provider may check your baby’s health with:
- Ultrasound. This is a prenatal test that uses sound waves and a computer screen to make a picture of your baby in the womb. Ultrasound checks that your baby is growing at a normal rate. It also lets your provider look at the placenta and the amount of fluid around your baby to make sure your pregnancy is healthy.
- Nonstress test. This test checks your baby’s heart rate.
- Biophysical profile. This test combines the nonstress test with an ultrasound.
- Doppler analysis. This is a sonographic test to evaluate the blood flow through the baby’s umbilical cord -- it can provide information as to how blood flow -- which carries oxygen - is getting to your baby
Treatment depends on how severe your preeclampsia is and how far along you are in your pregnancy.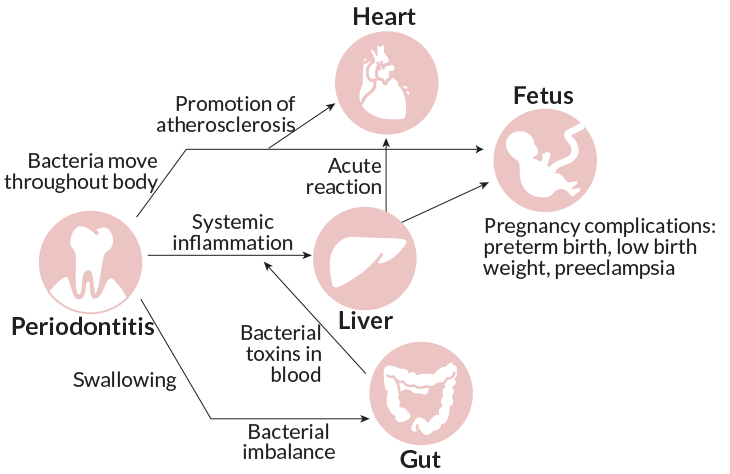 Even if you have mild preeclampsia, you need treatment to make sure it doesn’t get worse.
Even if you have mild preeclampsia, you need treatment to make sure it doesn’t get worse.
How is mild preeclampsia treated?
Most women with mild preeclampsia are delivered by 37 weeks of pregnancy . If you have mild preeclampsia before 37 weeks:
- Your provider checks your blood pressure and urine regularly. It’s possible that you may need to stay in the hospital to be monitored closely. If you’re not in the hospital, your provider may want you to have checkups once or twice a week. You may also need to take your blood pressure at home.
- Your provider may ask you to do kick counts to track how often your baby moves. There are two ways to do kick counts: Every day, time how long it takes for your baby to move ten times. If it takes longer than 2 hours, tell your provider. Or three times a week, track the number of times your baby moves in 1 hour. If the number changes, tell your provider.
- If you’re at least 37 weeks pregnant and your condition is stable, your provider may recommend that you have your baby early.
 This may be safer for you and your baby than staying pregnant. Your provider may give you medicine or break your water (amniotic sac) to make labor start. This is called inducing labor.
This may be safer for you and your baby than staying pregnant. Your provider may give you medicine or break your water (amniotic sac) to make labor start. This is called inducing labor.
How is severe preeclampsia treated?
If you have severe preeclampsia, you most likely stay in the hospital so your provider can closely monitor you and your baby. Your provider may treat you with medicines called antenatal corticosteroids (also called ACS). These medicines help speed up your baby’s lung development. You also may get medicine to control your blood pressure and medicine to prevent seizures (called magnesium sulfate).
If your condition gets worse, it may be safer for you and your baby to give birth early. Most babies of moms with severe preeclampsia before 34 weeks of pregnancy do better in the hospital than by staying in the womb. If you’re at least 34 weeks pregnant, your provider may recommend that you have your baby as soon as your condition is stable.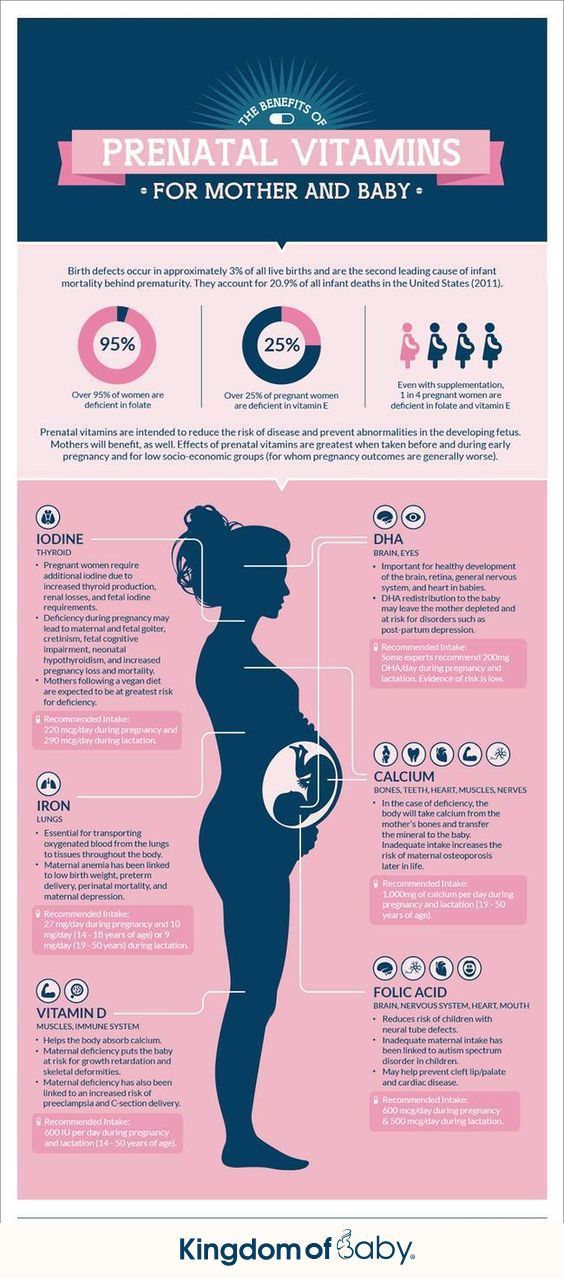 Your provider may induce your labor, or you may have a c-section. If you’re not yet 34 weeks pregnant but you and your baby are stable, you may be able to wait to have your baby.
Your provider may induce your labor, or you may have a c-section. If you’re not yet 34 weeks pregnant but you and your baby are stable, you may be able to wait to have your baby.
If you have severe preeclampsia and HELLP syndrome, you almost always need to give birth early. HELLP syndrome is a rare but life-threatening liver disorder. About 2 in 10 women (20 percent) with severe preeclampsia develop HELLP syndrome. You may need medicine to control your blood pressure and prevent seizures. Some women may need blood transfusions. A blood transfusion means you have new blood put into your body.
If you have preeclampsia, can you have a vaginal birth?
Yes. If you have preeclampsia, a vaginal birth may be better than a cesarean birth (also called c-section). A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus. With vaginal birth, there's no stress from surgery. For most women with preeclampsia, it’s safe to have an epidural to manage labor pain as long as your blood clots normally. An epidural is pain medicine you get through a tube in your lower back that helps numb your lower body during labor. It's the most common kind of pain relief during labor.
An epidural is pain medicine you get through a tube in your lower back that helps numb your lower body during labor. It's the most common kind of pain relief during labor.
What is postpartum preeclampsia?
Postpartum preeclampsia is a rare condition. It’s when you have preeclampsia after you’ve given birth. It most often happens within 48 hours (2 days) of having a baby, but it can develop up to 6 weeks after a baby’s birth. It’s just as dangerous as preeclampsia during pregnancy and needs immediate treatment. If not treated, it can cause life-threatening problems, including death.
Signs and symptoms of postpartum preeclampsia are like those of preeclampsia. It can be hard for you to know if you have signs and symptoms after pregnancy because you’re focused on caring for your baby. If you do have signs or symptoms, tell your provider right away.
We don’t know exactly what causes postpartum preeclampsia, but these may be possible risk factors:
- You had gestational hypertension or preeclampsia during pregnancy.
 Gestational hypertension is high blood pressure that starts after 20 weeks of pregnancy and goes away after you give birth.
Gestational hypertension is high blood pressure that starts after 20 weeks of pregnancy and goes away after you give birth. - You’re obese.
- You had a c-section.
Complications from postpartum preeclampsia include these life-threatening conditions:
- HELLP syndrome
- Postpartum eclampsia (seizures). This can cause permanent damage to our brain, liver and kidneys. It also can cause coma.
- Pulmonary edema. This is when fluid fills the lungs.
- Stroke
- Thromboembolism. This is when a blood clot travels from another part of the body and blocks a blood vessel.
Your provider uses blood and urine tests to diagnose postpartum preeclampsia. Treatment can include magnesium sulfate to prevent seizures and medicine to help lower your blood pressure. Medicine to prevent seizures also is called anticonvulsive medicine. If you’re breastfeeding, talk to your provider to make sure these medicines are safe for your baby.
Reviewed January 2023
Preeclampsia and pregnancy | Ida-Tallinna Keskaigla
Preeclampsia and pregnancy
The purpose of this information leaflet is to provide the patient with information about the nature, occurrence, risk factors, symptoms and treatment of preeclampsia.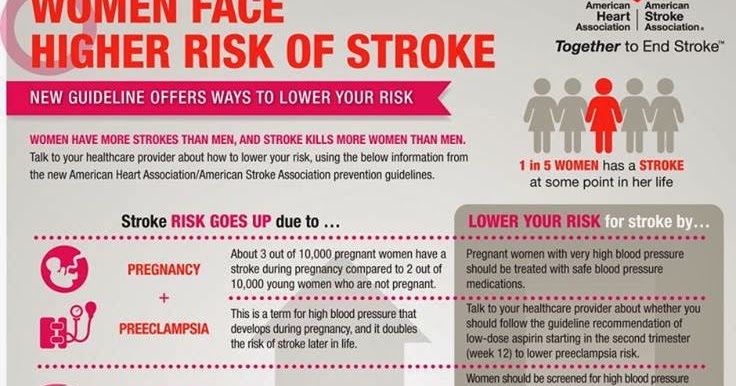
What is preeclampsia?
Pre-eclampsia is a disease that occurs during pregnancy and is characterized by high blood pressure and protein in the urine. Preeclampsia is one of the most common complications of pregnancy. Epilepsy-like seizures occur in severe preeclampsia and are life-threatening. nine0005
What symptoms may indicate the development of preeclampsia?
High blood pressure - blood pressure values are 140/90 mmHg. Art. or higher. If systolic (upper) or diastolic (lower) blood pressure rises by 30 mm Hg. Art. or more, then such an increase cannot be ignored.
Protein in urine - 300 mg in urine collected over 24 hours, or +1 value on a rapid test.
Swelling of the arms, legs or face , especially under the eyes or if the skin is pitted when pressed. Edema can occur in all pregnant women and is generally harmless, but rapidly developing edema should be taken into account.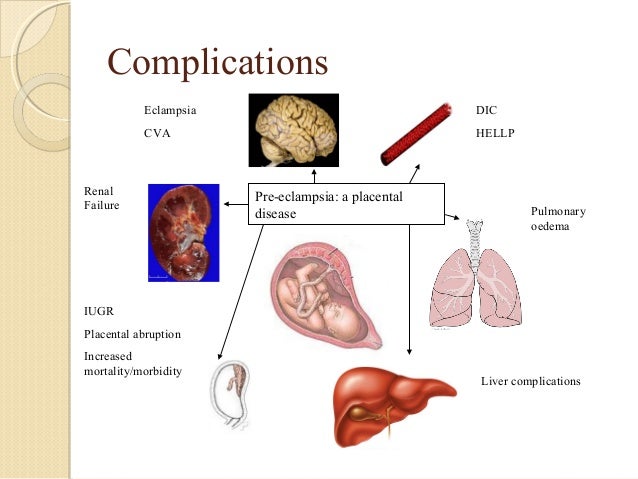
Headache that does not improve after taking pain medication.
Visual disturbances - double vision or blurred vision, dots or flashes before the eyes, auras.
Nausea or pain in the upper abdomen - These symptoms are often mistaken for indigestion or gallbladder pain. Nausea in the second half of pregnancy is not normal.
Sudden weight gain - 2 kg or more per week.
As a rule, there is a mild course of the disease that occurs at the end of pregnancy and has a good prognosis. Sometimes, preeclampsia can worsen quickly and be dangerous to both mother and fetus. In such cases, rapid diagnosis and careful monitoring of the mother and child are of paramount importance. nine0005
Unfortunately, most women develop symptoms in the final stages of the disease. If you experience any of the above symptoms, you should contact your midwife, gynecologist, or the Women's Clinic emergency department.
Is preeclampsia called toxemia of pregnancy?
Previously, pre-eclampsia was really called toxicosis, or toxemia, since it was believed that the cause of the disease was toxins, that is, poisons in the blood of a pregnant woman.
What is the difference between preeclampsia and gestational hypertension?
Pregnancy hypertension is an increase in blood pressure above normal after the 20th week of pregnancy. With hypertension of pregnant women, protein in the urine is not observed.
What is HELLP syndrome?
HELLP syndrome is one of the most severe forms of preeclampsia. HELLP syndrome is rare and sometimes develops before symptoms of preeclampsia appear. Sometimes the syndrome is difficult to diagnose, as the symptoms resemble gallbladder colic or a cold. nine0005
When does preeclampsia occur?
Preeclampsia usually occurs after the 20th week of pregnancy. As a rule, preeclampsia goes away after delivery, but complications can occur up to six weeks after delivery, during which careful monitoring of the condition is necessary.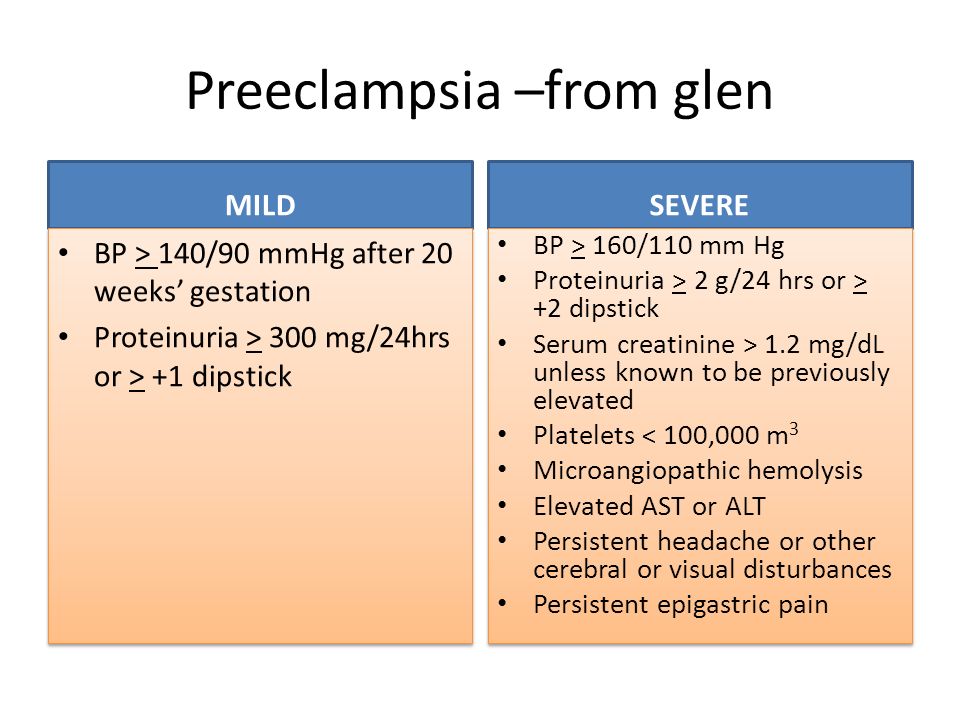 If by the sixth week after birth, blood pressure does not return to normal, then you need to contact a cardiologist, who will begin treatment against hypertension.
If by the sixth week after birth, blood pressure does not return to normal, then you need to contact a cardiologist, who will begin treatment against hypertension.
What is the cause of preeclampsia? nine0004
The causes of the disease are still not clear, there are only unproven hypotheses.
How does the disease affect pregnant women and pregnancy?
Most preeclamptic pregnancies have a favorable outcome and a healthy baby is born. However, the disease is very serious and is one of the most common causes of death of the child and mother. Preeclampsia affects a woman's kidneys, liver, and other vital organs, and if left untreated, it can cause seizures (eclampsia), cerebral hemorrhage, multiple organ failure, and death. nine0005
How does the disease affect the fetus?
In preeclampsia, the fetus does not receive enough oxygen and nutrients to grow, and intrauterine growth retardation may occur. In addition, the placenta may separate from the uterine wall before the baby is born. Since the only treatment for preeclampsia is childbirth, sometimes a pregnancy has to be terminated prematurely. Until the 34th week of pregnancy, the lungs of the fetus have not yet matured, and steroid hormones are injected intramuscularly into the pregnant woman to prepare his lungs. In addition to the immaturity of the lungs, the health of a premature baby is threatened by many other diseases. nine0005
Since the only treatment for preeclampsia is childbirth, sometimes a pregnancy has to be terminated prematurely. Until the 34th week of pregnancy, the lungs of the fetus have not yet matured, and steroid hormones are injected intramuscularly into the pregnant woman to prepare his lungs. In addition to the immaturity of the lungs, the health of a premature baby is threatened by many other diseases. nine0005
Who is at risk of developing preeclampsia?
Preeclampsia occurs in approximately 8% of pregnant women, many of whom have no known risk factors.
What are the risk factors for preeclampsia?
Patient-related risk factors
- First pregnancy
- Pre-eclampsia during a previous pregnancy
- Age over 40 or under 18
- High blood pressure before pregnancy
- Diabetes before or during pregnancy
- Multiple pregnancy
- Overweight (BMI> 30)
- Systemic lupus erythematosus or other autoimmune disease
- Polycystic ovary syndrome
- Long interval between two pregnancies
Risk factors associated with the patient's family
- Pre-eclampsia in the mother's or father's family
- Parental high blood pressure or heart disease
- Diabetes mellitus
What is the prevention and treatment of preeclampsia
The first trimester screening or Oscar test also calculates the risk of preeclampsia in addition to the most common chromosomal disorders. In case of high risk, pregnant women are advised to take aspirin (acetylsalicylic acid) at a dose of 150 mg in the evenings until the 36th week of pregnancy. This helps reduce the chance of preeclampsia by the 34th week of pregnancy by up to 80%. nine0005
In case of high risk, pregnant women are advised to take aspirin (acetylsalicylic acid) at a dose of 150 mg in the evenings until the 36th week of pregnancy. This helps reduce the chance of preeclampsia by the 34th week of pregnancy by up to 80%. nine0005
Childbirth is the only treatment for preeclampsia. Sometimes a child can be born naturally, but sometimes, if the disease is very acute, an emergency caesarean section is necessary. The best time to have a baby is after the 37th week of pregnancy. Bed rest, medications, and, if necessary, hospitalization can sometimes help bring the condition under control and prolong the pregnancy. Often, a doctor will refer a woman with preeclampsia to the hospital for observation, as the condition of the fetus and pregnant woman may suddenly worsen. nine0005
Does bed rest help?
Sometimes bed rest is enough to control mild preeclampsia. In this case, the patient often visits a doctor who measures blood pressure, does blood and urine tests, and monitors the course of the disease. The condition of the fetus is also often examined using a cardiotocogram (CTG) and ultrasound.
The condition of the fetus is also often examined using a cardiotocogram (CTG) and ultrasound.
Are drugs used to treat preeclampsia?
High blood pressure sometimes requires medication. The medications used have few side effects, the drugs prescribed do not have much effect on the fetus, but are very important in the treatment of maternal high blood pressure. nine0005
Seizures are a rare but very serious complication of preeclampsia. Magnesium sulfate is sometimes given intravenously to prevent seizures in a pregnant woman with preeclampsia both during and after childbirth. It is safe for the fetus, but the mother may experience side effects such as hot flashes, sweating, thirst, visual disturbances, mild confusion, muscle weakness, and shortness of breath. All these side effects disappear when the drug is discontinued.
Can preeclampsia recur? nine0004
Preeclampsia does not necessarily recur in the next pregnancy, but the main risk factor for preeclampsia is the presence of preeclampsia in a previous pregnancy(s). Risk factors for relapse include the severity of the previous case and the woman's overall health during pregnancy. A woman who has previously had preeclampsia should consult a gynecologist during a new pregnancy or when planning a pregnancy.
Risk factors for relapse include the severity of the previous case and the woman's overall health during pregnancy. A woman who has previously had preeclampsia should consult a gynecologist during a new pregnancy or when planning a pregnancy.
ITK1013
The information material was approved by the Health Care Quality Committee of East-Tallinn Central Hospital on 11/30/2022 (Minutes No. 18-22).
Preeclampsia during pregnancy
Pre-eclampsia in pregnancy
What is preeclampsia?
Preeclampsia is a serious blood pressure disorder that can occur after the 20th week of pregnancy or after childbirth (called postpartum preeclampsia). This is when a woman has high blood pressure and signs that some of her organs, such as her kidneys and liver, are malfunctioning. nine0005
Blood pressure is the force with which blood presses against the walls of the arteries.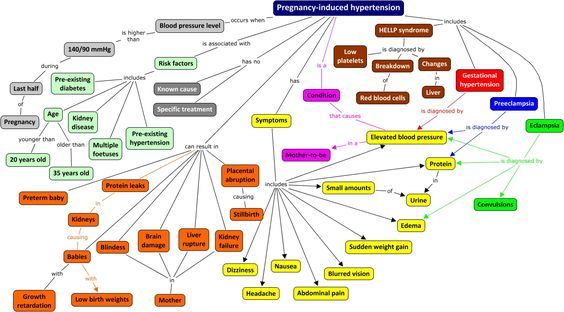 Arteries are blood vessels that carry blood from the heart to other parts of the body. High blood pressure (also called hypertension) occurs when the pressure of blood against the walls of blood vessels is too high. This can be stressful for your heart and cause problems during pregnancy.
Arteries are blood vessels that carry blood from the heart to other parts of the body. High blood pressure (also called hypertension) occurs when the pressure of blood against the walls of blood vessels is too high. This can be stressful for your heart and cause problems during pregnancy.
Pre-eclampsia is a serious health problem for pregnant women. It affects 2 to 8 percent of pregnant women worldwide. It is also the cause of 15% of preterm births. A preterm birth is a birth that occurs too early, before 37 weeks of gestation. nine0005
Diagnosis of preeclampsia during pregnancy
Most women with preeclampsia give birth to healthy babies. But if left untreated, it can cause serious health problems for you and your baby.
Causes of preeclampsia
The exact cause of preeclampsia is likely related to several factors. Experts believe it begins in the placenta, the organ that nourishes the fetus throughout pregnancy.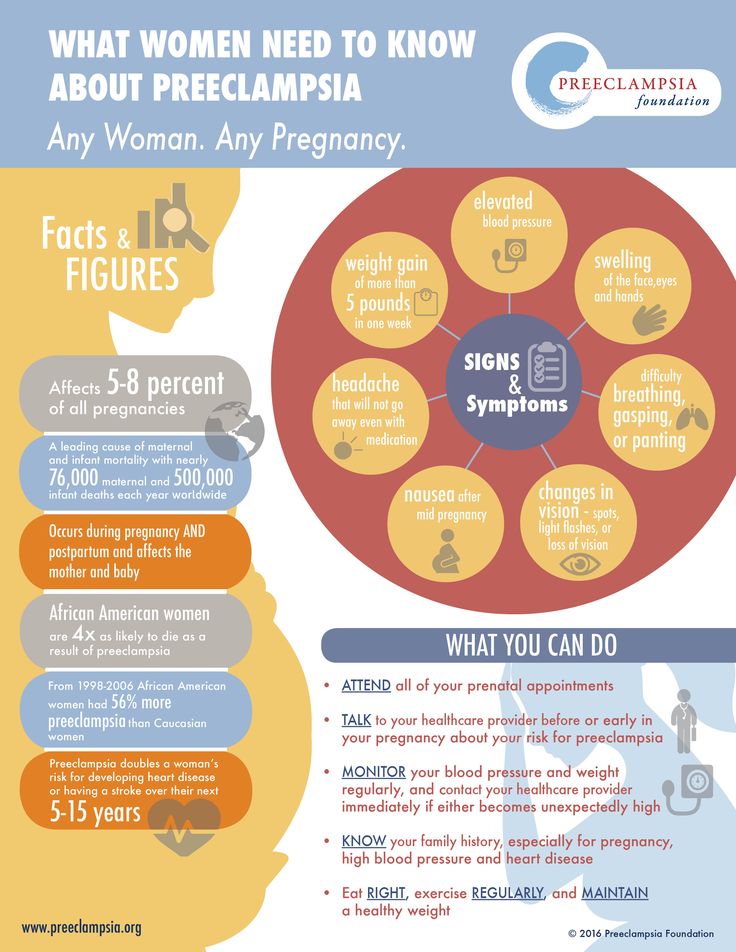 During early pregnancy, new blood vessels form and develop to supply the placenta with oxygen and nutrients. nine0005
During early pregnancy, new blood vessels form and develop to supply the placenta with oxygen and nutrients. nine0005
Make an appointment with a gynecologist ►
In women with preeclampsia, these blood vessels do not develop and function properly. Problems with blood circulation in the placenta can lead to irregular regulation of blood pressure in the mother.
Risk factors for preeclampsia
Conditions that are associated with a higher risk of preeclampsia include:
-
Preeclampsia in a previous pregnancy
-
Pregnancy with more than one child
-
Chronic high blood pressure (hypertension)
-
Type 1 or 2 before pregnancy
-
Piseases of the kidneys
- Autoimmune conditions
Use of extorpolnodal core
) that are associated with a moderate risk of preeclampsia include:-
First pregnancy with current partner
-
Obesity
-
Family history of preeclampsia
-
Mother's age 35 years and over
-
Complications in the previous pregnancy
-
more than 10 years after the previous pregnancy
7 7 -
-
Changes in vision such as blurring, flashing lights and spots, or sensitivity to light.
-
Headache, which does not pass
-
Nausea (feeling of nausea in the stomach), vomiting or dizziness
-
Pain in the upper right of the abdomen
-
sudden weight gain
07 9000 9000 or persons -
Difficulty breathing
-
Severe vomiting and nausea
-
Fetal growth restriction
Preeclampsia affects the arteries that carry blood to the placenta. If the placenta does not receive enough blood, the baby may not receive enough blood and oxygen and fewer nutrients. This can lead to growth retardation, known as fetal growth retardation. -
Preterm birth
Preeclampsia can lead to unplanned preterm birth - delivery before 37 weeks. In addition, planned preterm birth is the main treatment for preeclampsia. A premature baby is at increased risk of breathing and feeding difficulties, vision or hearing problems, developmental delays, and cerebral palsy. Treatment before preterm labor may reduce some of the risks. nine0005 -
Placental abruption
Preeclampsia increases the risk of placental abruption. In this condition, the placenta separates from the inner wall of the uterus before delivery.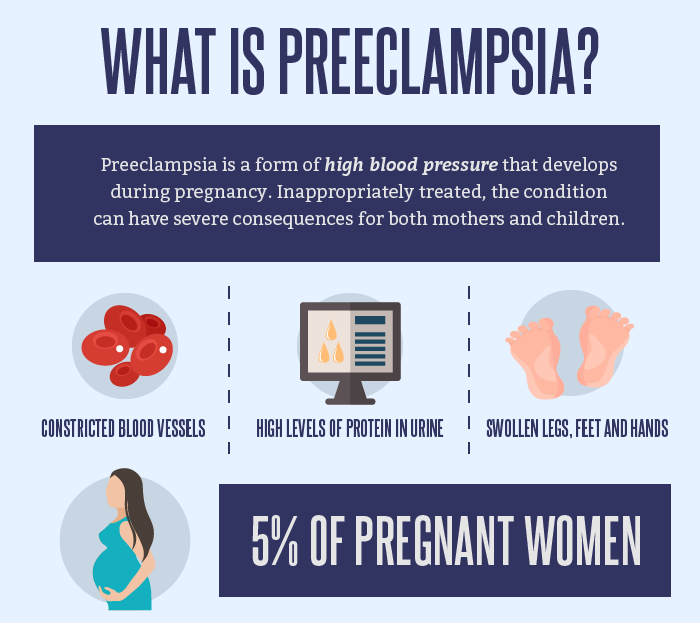 A severe detachment can cause severe bleeding, which can be life-threatening for both mother and baby.
A severe detachment can cause severe bleeding, which can be life-threatening for both mother and baby. -
HELLP syndrome
HELLP stands for hemolysis (destruction of red blood cells), elevated liver enzymes and low platelets. This severe form of preeclampsia affects multiple organ systems. HELLP syndrome is life threatening for mother and baby and can cause lifelong health problems for the mother. Signs and symptoms include nausea and vomiting, headache, pain in the upper right side of the abdomen, and general malaise or feeling unwell. Sometimes it develops suddenly, even before high blood pressure is detected. It can also develop without any symptoms. nine0005 -
Eclampsia
Eclampsia is the onset of seizures or coma with signs or symptoms of preeclampsia. It is very difficult to predict whether a patient with preeclampsia will develop eclampsia.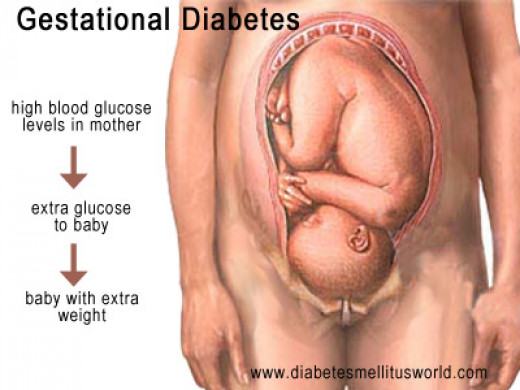 Eclampsia can occur without any previously observed signs or symptoms of preeclampsia. Signs and symptoms that may occur before seizures include severe headaches, vision problems, confusion, or altered behavior. But often there are no symptoms or warning signs. Eclampsia can occur before, during, or after childbirth. nine0005
Eclampsia can occur without any previously observed signs or symptoms of preeclampsia. Signs and symptoms that may occur before seizures include severe headaches, vision problems, confusion, or altered behavior. But often there are no symptoms or warning signs. Eclampsia can occur before, during, or after childbirth. nine0005 -
Other organ damage
Preeclampsia can cause damage to the kidneys, liver, lungs, heart, or eyes, as well as stroke or other brain damage. The extent of damage to other organs depends on how severe the preeclampsia is. -
Cardiovascular disease
Having preeclampsia can increase your risk of future heart and blood vessel disease (cardiovascular disease). The risk is even higher if you have had preeclampsia more than once or have had a preterm birth. nine0005 -
Bed rest at home or in the hospital; rest mainly on left side
-
Careful monitoring of fetal heart rate and frequent ultrasounds
-
Blood pressure medicines
-
Blood and urine tests
-
Medicine to help prevent seizures, lower blood pressure, and prevent other problems.
-
Steroid injections to speed up your child's lung development
-
There is too much protein in the urine
-
None of blood platelets
-
High level of chemicals associated with the kidneys
-
High level of chemicals associated with the liver, in the blood
01010101010101010101010101010IS -
New headache that doesn't get better with medication
-
Blood tests to check platelets and look for chemicals in the kidneys or liver.
-
Urinalysis to measure proteins
-
Ultrasounds, non-stress tests or biophysical profiles to see how your baby is growing
-
Lose weight, if you have overweight
-
, stop smoking
-
Regularly play sports
-
Control blood pressure or blood sugar
-
You had gestational hypertension or preeclampsia during pregnancy. Gestational hypertension is high blood pressure that starts after 20 weeks of pregnancy and resolves after childbirth
-
Obesity
-
You had a Caesarean section
-
Hellp-syndrome
-
postcard ecrama).

Symptoms of pre-eclampsia during pregnancy
What are the signs and symptoms of preeclampsia?
Signs of illness are things that someone else might notice about you, such as having a rash or coughing. Symptoms are things you feel yourself that others don't see, such as a sore throat or dizziness. nine0005
Symptoms are things you feel yourself that others don't see, such as a sore throat or dizziness. nine0005
Signs and symptoms of pre-eclampsia include:
Many of these signs and symptoms are a common discomfort during pregnancy. If you have even one sign or symptom, call your doctor right away.
How can preeclampsia affect you and your baby?
Without treatment, preeclampsia can cause serious health problems for you and your baby, including death. You can have preeclampsia even if you don't know it, so be sure to attend all prenatal checkups, even if you feel well. Tell your doctor if you have any signs or symptoms of preeclampsia. nine0005
Tell your doctor if you have any signs or symptoms of preeclampsia. nine0005
Treatment of preeclampsia
Treatment of preeclampsia
The only cure for preeclampsia and eclampsia is to give birth.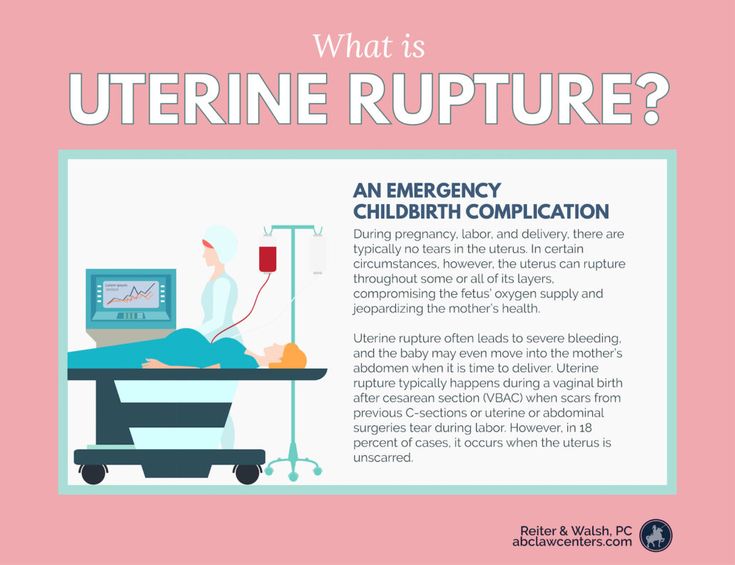 Your doctor will discuss with you when to give birth, depending on how your baby has developed, how well your baby is doing in your womb, and the severity of your preeclampsia.
Your doctor will discuss with you when to give birth, depending on how your baby has developed, how well your baby is doing in your womb, and the severity of your preeclampsia.
If your baby is growing well, usually by 37 weeks or later, your doctor may order induction of labor or a caesarean section. This will prevent preeclampsia from worsening.
If your baby is not yet due, you and your doctor can treat mild preeclampsia until your baby is mature enough to deliver safely. The closer your due date is, the better for your baby.
If you have mild preeclampsia, also known as preeclampsia without severe symptoms, your doctor may prescribe:
Your doctor may also recommend that you stay in the hospital so they can monitor you closely.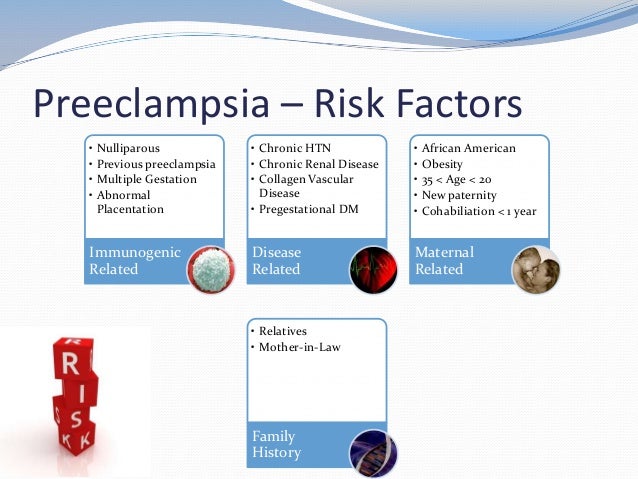 At the hospital you can get:
At the hospital you can get:
Other treatments include:
If you have severe preeclampsia, your doctor may need to deliver you immediately, even if you are not close to your due date. Thereafter, symptoms of preeclampsia should resolve within 1 to 6 weeks, but may persist for longer.
Diagnosis of preeclampsia in pregnant women
Diagnosis of preeclampsia
You have preeclampsia if you have high blood pressure and at least one of the following:
Fluid in the lungs
Your doctor may order tests to confirm your diagnosis, including:
Pre-eclampsia prevention
lifestyle that will help keep you healthy. You may need:
Your doctor can also assemble a small doctor. dose (81 milligrams) of aspirin every day. But do not take any medications, vitamins, or nutritional supplements without first talking to them.
Can low-dose aspirin help reduce the risk of preeclampsia and preterm birth? nine0179
For some women, yes. If your healthcare provider thinks you are at risk for preeclampsia, they may ask you to take low doses of aspirin to help prevent it. Low-dose aspirin is also called baby aspirin or 81 mg (milligram) aspirin.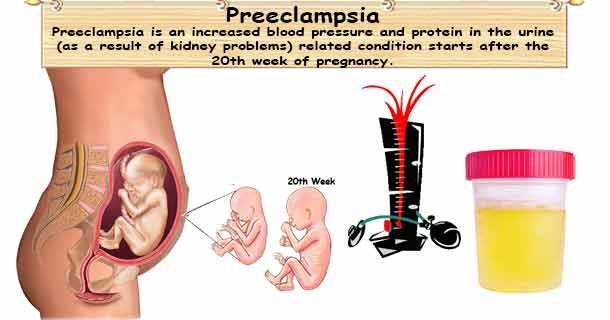 Talk to your doctor to see if low-dose aspirin treatment is right for you.
Talk to your doctor to see if low-dose aspirin treatment is right for you.
If your doctor wants you to take low-dose aspirin to prevent preeclampsia, take it exactly as he tells you to. Do not take more or more often than your doctor tells you to. nine0005
If you have preeclampsia, can you give birth naturally?
Yes. If you have preeclampsia, a vaginal delivery may be better than a caesarean section (also called a caesarean section). A caesarean section is an operation in which your baby is delivered through an incision the doctor makes in the abdomen and uterus. With vaginal delivery, there is no stress from the operation. For most women with preeclampsia, epidural anesthesia is safe to relieve the pain of childbirth. An epidural is a pain medication given through a tube in the lower back to help relieve pain in the lower body during childbirth. This is the most common type of pain relief during childbirth. nine0005
Prevention of pre-eclampsia
What is postpartum preeclampsia?
Postpartum preeclampsia is a rare condition.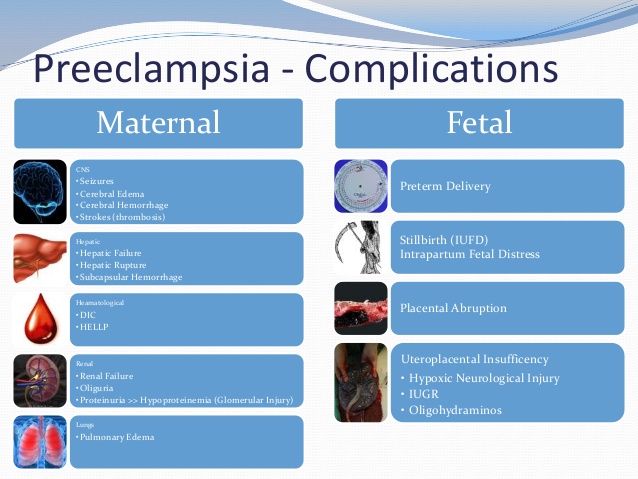 This is when you have preeclampsia after giving birth. It most often occurs within 48 hours (2 days) after the baby is born, but can develop up to 6 weeks after the baby is born. It is as dangerous as preeclampsia during pregnancy and requires immediate treatment. If left untreated, it can cause life-threatening problems, including death. nine0005
This is when you have preeclampsia after giving birth. It most often occurs within 48 hours (2 days) after the baby is born, but can develop up to 6 weeks after the baby is born. It is as dangerous as preeclampsia during pregnancy and requires immediate treatment. If left untreated, it can cause life-threatening problems, including death. nine0005
The signs and symptoms of postpartum preeclampsia are the same as those of preeclampsia. It may be difficult for you to know if you have signs and symptoms after pregnancy because you are focused on caring for your baby. If you have signs or symptoms, tell your doctor right away.
We don't know exactly what causes postpartum preeclampsia, but these could be possible risk factors:
The complications of postpartum pre-eeclampsia include the following life-threatening conditions: