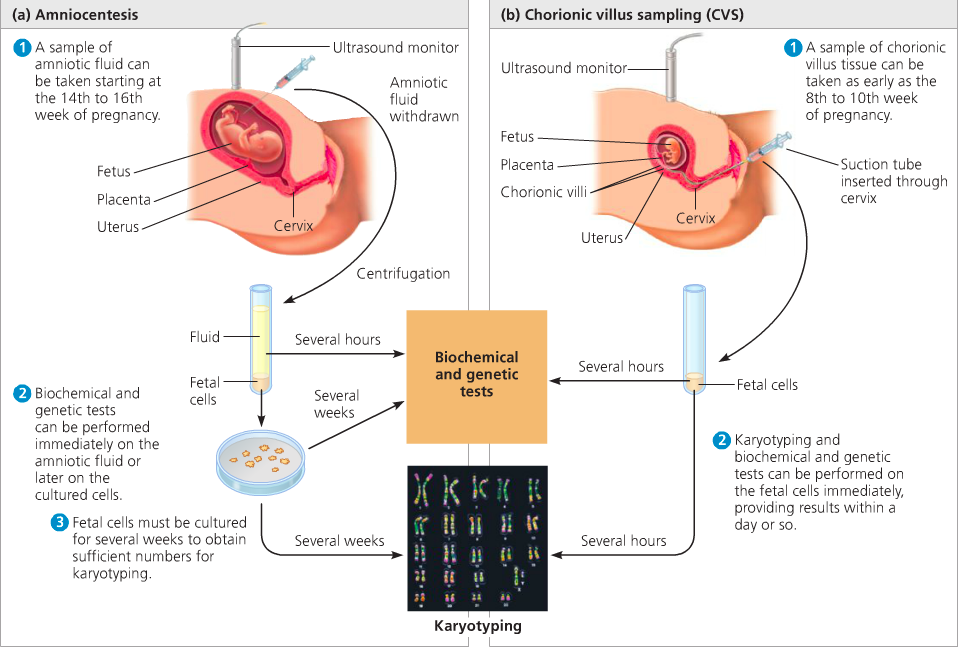
Cvs amniotic fluid test
Chorionic Villus Sampling (CVS) | Johns Hopkins Medicine
What is chorionic villus sampling?
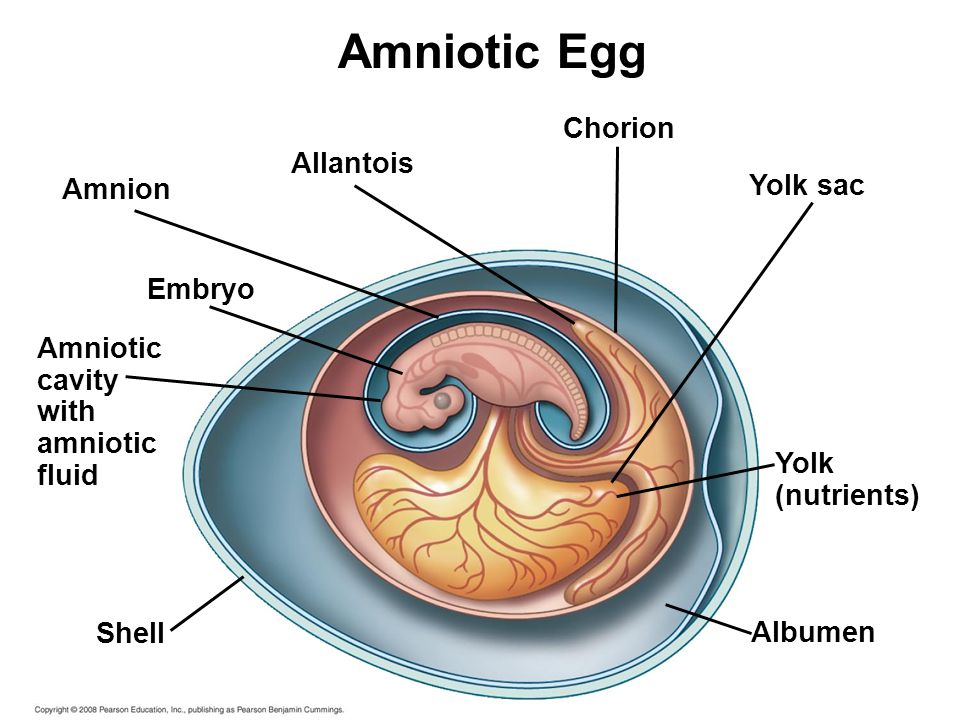
Chorionic villus sampling (CVS), or chorionic villus biopsy, is a prenatal test that involves taking a sample of tissue from the placenta to test for chromosomal abnormalities and certain other genetic problems. The placenta is a structure in the uterus that provides blood and nutrients from the mother to the fetus,
The chorionic villi are tiny projections of placental tissue that look like fingers and contain the same genetic material as the fetus. Testing may be available for other genetic defects and disorders depending on the family history and availability of lab testing at the time of the procedure.
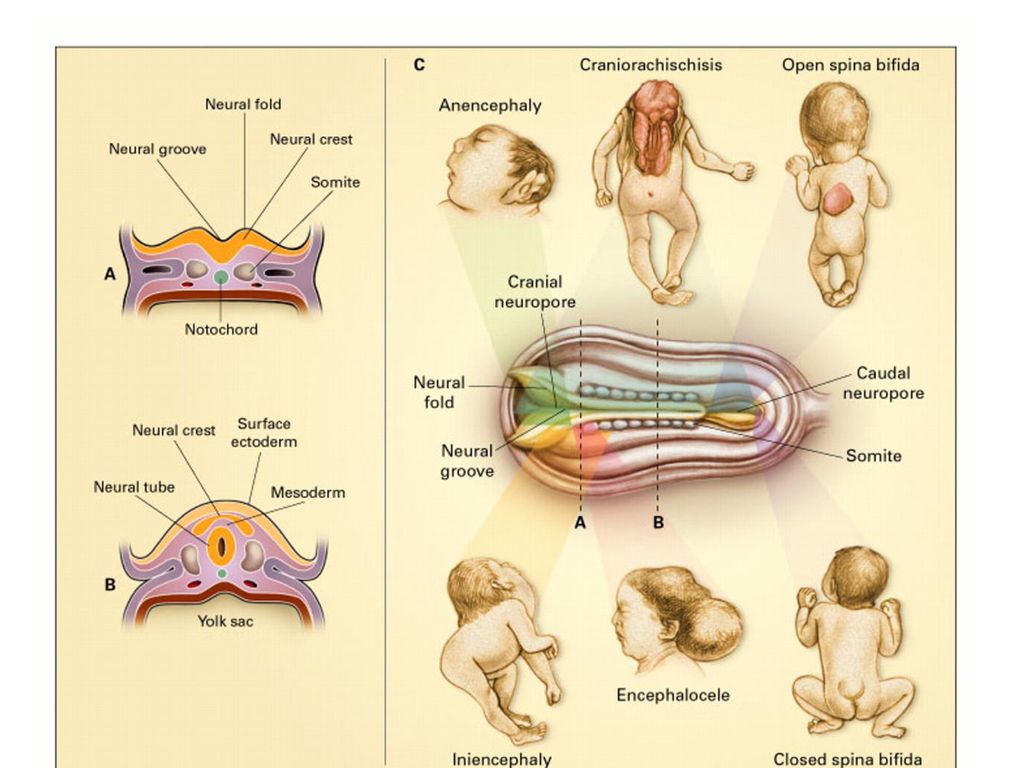
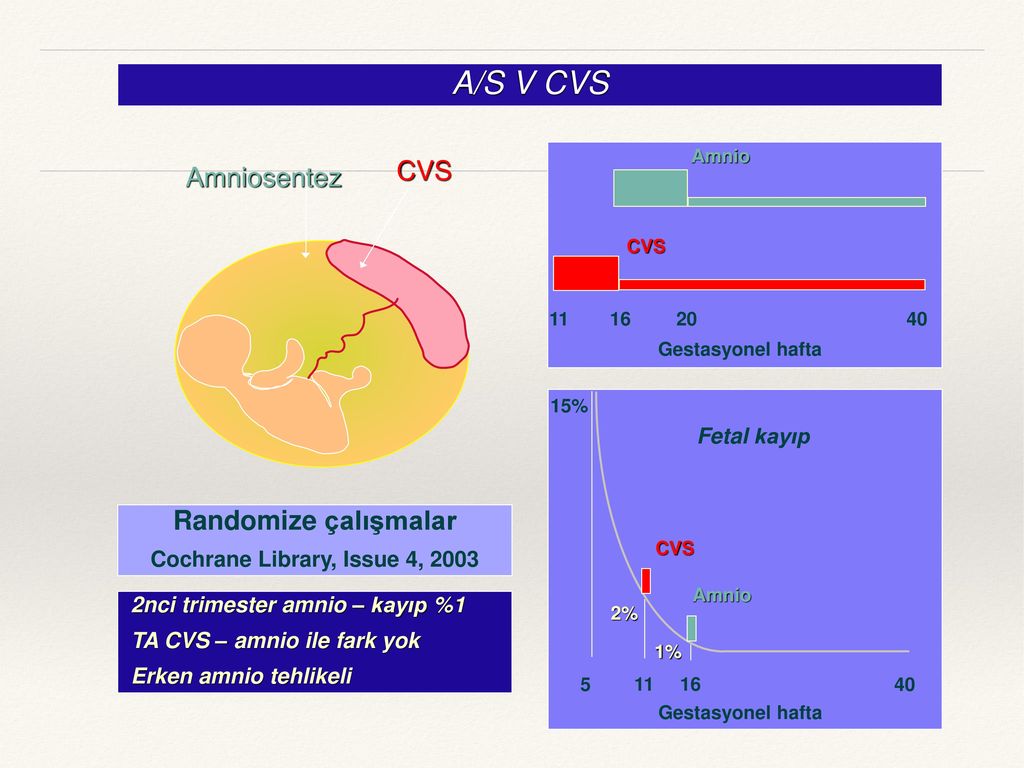
CVS is usually done between the 10th and 12th weeks of pregnancy. Unlike amniocentesis (another type of prenatal test), CVS does not provide information on neural tube defects, such as spina bifida. For this reason, women who undergo CVS also need a follow-up blood test between 16 to 18 weeks of their pregnancy to screen for neural tube defects.
There are two types of CVS procedures:
-
Transcervical. In this procedure, a catheter is inserted through the cervix into the placenta to obtain the tissue sample
-
Transabdominal. In this procedure, a needle is inserted through the abdomen and uterus into the placenta to obtain the tissue sample
Another related procedure that may be used to diagnose genetic and chromosomal defects is amniocentesis.
Anatomy of the fetus in utero
Click image to enlarge.
-
Amniotic sac. This is a thin-walled sac that surrounds the fetus during pregnancy. The sac is filled with amniotic fluid (liquid made by the fetus) and the amnion (the membrane that covers the fetal side of the placenta), which protects the fetus from injury and helps to regulate the temperature of the fetus.
-
Anus. This is the opening at the end of the anal canal.

-
Cervix. This is the lower part of the uterus that projects into the vagina. Made up of mostly fibrous tissue and muscle, the cervix is circular in shape.
-
Fetus. An unborn baby from the eighth week after fertilization until birth is called a fetus.
-
Placenta. This is an organ, shaped like a flat cake that only grows during pregnancy and provides a metabolic interchange between the fetus and mother. (The fetus takes in oxygen, food, and other substances and eliminates carbon dioxide and other wastes.)
-
Umbilical cord. This is a rope-like cord connecting the fetus to the placenta. The umbilical cord contains 2 arteries and a vein, which carry oxygen and nutrients to the fetus and waste products away from the fetus.
-
Uterine wall. This is the wall of the uterus.

-
Uterus (also called the womb). The uterus is a hollow, pear-shaped organ located in a woman's lower abdomen, between the bladder and the rectum. It sheds its lining each month during menstruation and in which a fertilized egg (ovum) becomes implanted and the fetus develops.
-
Vagina. This is part of the female genitals sits behind the bladder and in front of the rectum. It forms a canal extending from the uterus to the vulva.
Reasons for the procedure
Chorionic villus sampling may be used for genetic and chromosome testing in the first trimester of pregnancy . Here are some reasons that a woman might elect to undergo CVS:
-
Previously affected child or a family history of a genetic disease, chromosomal abnormalities, or metabolic disorder
-
Maternal age over 35 years by the pregnancy due date
-
Risk of a sex-linked genetic disease
-
Previous ultrasound with questionable or abnormal findings
-
Abnormal cell-free DNA test
There may be other reasons for your doctor to recommend a chorionic villus sampling.
Risks of the procedure
As with any invasive procedure, complications may occur. Some possible complications may include, but are not limited to, the following:
-
Cramping, bleeding, or leaking of amniotic fluid (water breaking)
-
Infection
-
Miscarriage
-
Preterm labor
-
Limb defects in infants, especially in CVS procedures done before 9 weeks (rare)
People who are allergic to or sensitive to medications or latex should notify their doctor.
Women with twins or other multiples will need sampling from each placenta in order to study each baby.
There may be other risks depending upon your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
Certain factors or conditions may interfere with CVS. These factors include, but are not limited to, the following:
-
Pregnancy earlier than seven weeks or later than 13 weeks
-
Position of the baby, placenta, amount of amniotic fluid, or mother's anatomy
-
Vaginal or cervical infection
-
Samples that are inadequate for testing, or that may contain maternal tissue
Before the procedure
-
The doctor will explain the procedure to you and offer you the opportunity to ask any questions that you might have about the procedure.

-
You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if something is not clear.
-
Generally, there is no special restriction on diet or activity prior to chorionic villus sampling.
-
Tell your doctor if you are sensitive to or are allergic to any medications, latex, iodine, tape, and anesthetic agents (local and general).
-
Tell your doctor of all medications (prescribed and over-the-counter) and herbal supplements that you are taking.
-
Tell your doctor if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medications, aspirin, or any other medications that may affect blood clotting. It may be necessary for you to stop these medications prior to the procedure.
-
Tell your doctor if you are Rh negative.
 During the CVS procedure, blood cells from the mother and fetus can mix. This may lead to Rh sensitization and breaking down of fetal red blood cells. In most cases, prenatal blood tests will have determined whether you are Rh negative. You may be asked to provide these lab results before the procedure.
During the CVS procedure, blood cells from the mother and fetus can mix. This may lead to Rh sensitization and breaking down of fetal red blood cells. In most cases, prenatal blood tests will have determined whether you are Rh negative. You may be asked to provide these lab results before the procedure. -
You may or may not be asked to have a full bladder right before the procedure. Depending on the position of the uterus and placenta, a full or empty bladder may help move the uterus into a better position for the procedure.
-
Based upon your medical condition, your doctor may request other specific preparation.
During the procedure
Click image to enlarge.
A CVS procedure may be done on an outpatient basis, or as part of your stay in a hospital. Procedures may vary depending on your condition and your doctor’s practices.
Generally, a CVS procedure follows this process:
-
You will be asked to undress completely, or from the waist down, and put on a hospital gown.
-
You will be asked to lie down on an exam table and place your hands behind your head.
-
Your vital signs (blood pressure, heart rate, and breathing rate) will be checked.
-
An ultrasound will be performed to check the fetal heart rate, and the position of the placenta, fetus, and umbilical cord.
-
Based on the location of the placenta, the CVS procedure will be performed through your cervix (transcervical) or through your abdominal wall (transabdominal).
For a transcervical CVS procedure:
-
The doctor will insert an instrument called a speculum into your vagina so that he or she can see your cervix.
-
Your vagina and cervix will be cleansed with an antiseptic solution.
-
Using ultrasound guidance, a thin tube will be guided through the cervix to the chorionic villi.
-
Cells will be gently suctioned through the tube into a syringe.
 You may feel a twinge or slight cramping. More than one sample may be needed to obtain enough tissue for testing.
You may feel a twinge or slight cramping. More than one sample may be needed to obtain enough tissue for testing. -
The tube will then be removed.
For a transabdominal CVS procedure:
-
For an abdominal CVS, your abdomen will be cleansed with an antiseptic. You will be instructed not to touch the sterile area on your abdomen during the procedure.
-
The doctor may inject a local anesthetic to numb the skin. If a local anesthetic is used, you will feel a needle stick when the anesthetic is injected. This may cause a brief stinging sensation.
-
Ultrasound will be used to help guide a long, thin, hollow needle through your abdomen and into the uterus and placenta. This may be slightly painful, and you may feel a cramp as the needle enters the uterus.
-
Cells will be gently suctioned into a syringe. More than one sample may be needed to obtain enough tissue for testing.
-
The needle will then be removed. An adhesive bandage will be placed over the abdominal needle insertion site.
Procedure completion, both methods:
-
The fetus’ heart rate and your vital signs will be reassessed.
-
If you are Rh negative, you may be given Rho(D) immune globulin. This is a specially developed blood product that can prevent an Rh negative mother's antibodies from reacting to Rh positive fetal cells.
-
The chorionic villus tissue will be sent to the lab.
After the procedure
You and your fetus will be monitored for a while after the procedure. Your vital signs and the fetal heart rate will be checked periodically for an hour or longer.
The CVS tissue will be sent to a specialty genetics lab for analysis. Counseling with a genetics specialist may be recommended depending on the test results.
You may experience some slight cramping and light spotting for a few hours after CVS.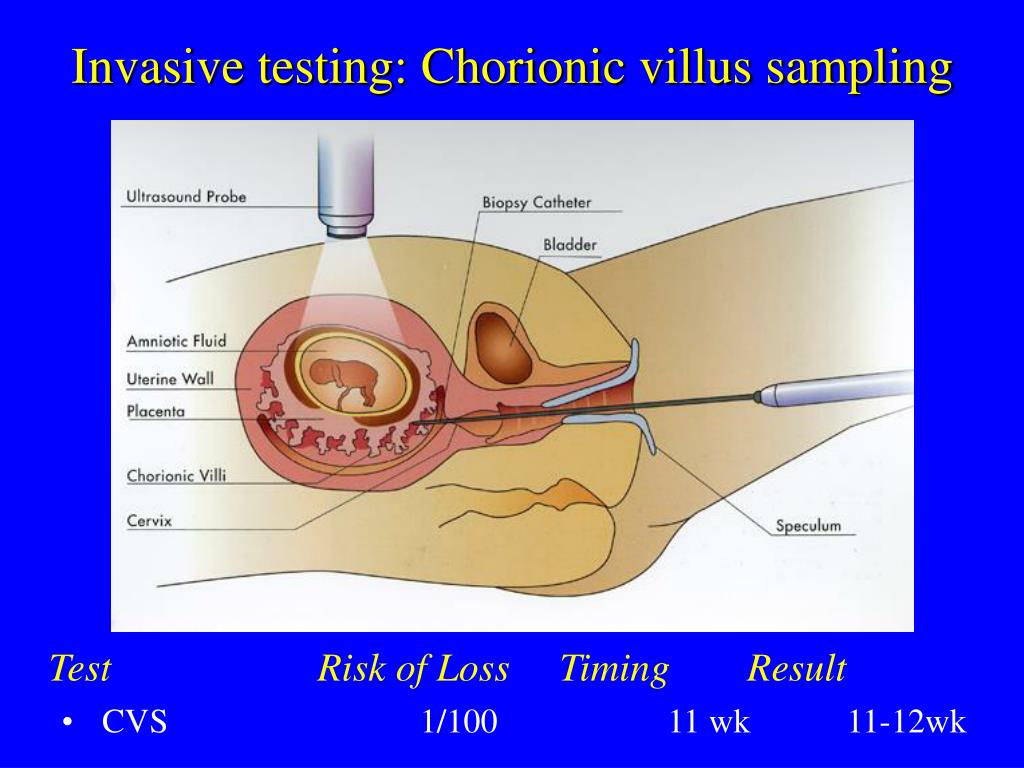
You should rest at home and avoid strenuous activities for at least 24 hours. You should not douche or have sexual intercourse for 2 weeks, or until directed by your doctor.
Tell your doctor to report any of the following:
If a transabdominal procedure was performed, check the bandaged needle site on your abdomen for any bleeding or drainage of fluid.
Your doctor may give you additional or alternate instructions after the procedure, depending on your particular situation.
Chorionic villus sampling - NHS
Chorionic villus sampling (CVS) is a test you may be offered during pregnancy to check if your baby has a genetic or chromosomal condition, such as Down's syndrome, Edwards' syndrome or Patau's syndrome.
It involves removing and testing a small sample of cells from the placenta, the organ linking the mother's blood supply with the unborn baby's.
When CVS is offered
CVS is not routinely offered in pregnancy.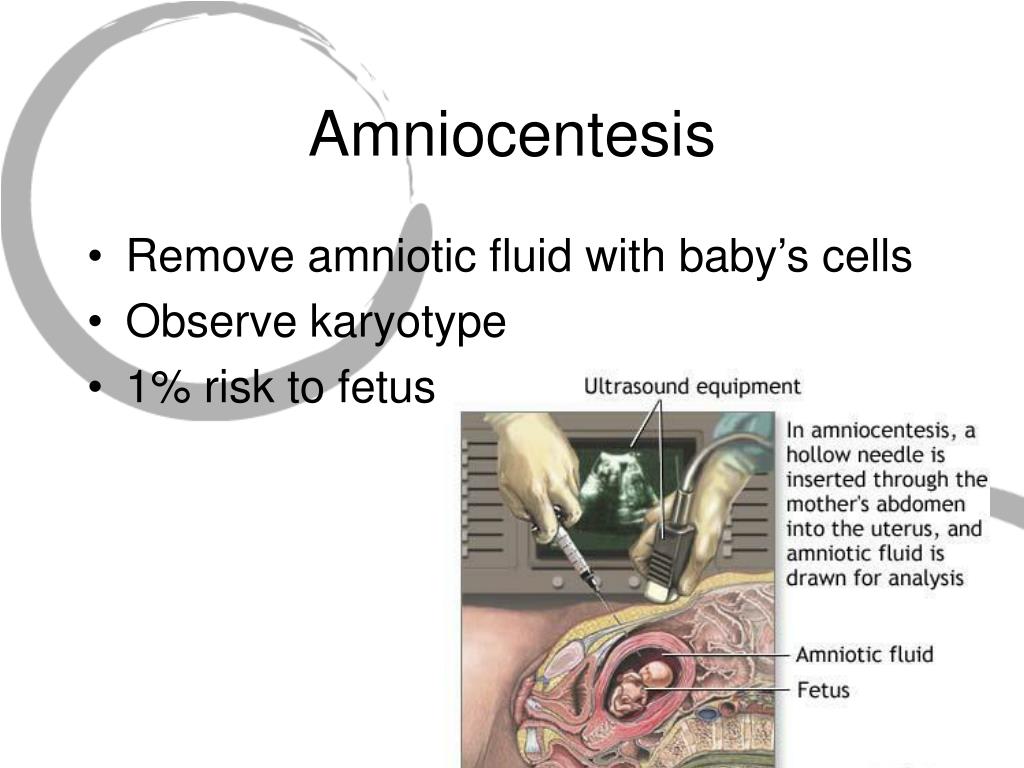
It's only offered if there's a high chance your baby could have a genetic or chromosomal condition.
This could be because:
- an antenatal screening test has suggested your baby may be born with a condition, such as Down's syndrome, Edwards' syndrome or Patau's syndrome
- you had a previous pregnancy affected by a genetic condition
- you have a family history of a genetic condition, such as sickle cell disease, thalassaemia, cystic fibrosis or muscular dystrophy
It's important to remember that you do not have to have CVS if it's offered. It's up to you to decide whether you want it.
A midwife or doctor will speak to you about what the test involves, and let you know what the possible benefits are, to help you make a decision.
Find out more about why CVS is offered and deciding whether to have it
How CVS is performed
CVS is usually carried out between the 11th and 14th weeks of pregnancy, although it's sometimes performed later than this if necessary.
During the test, a small sample of cells is removed from the placenta using 1 of 2 methods:
- transabdominal CVS – a needle is inserted through your tummy (this is the most common method used)
- transcervical CVS – a tube or small forceps (smooth metal instruments that look like tongs) are inserted through the cervix (the neck of the womb)
The test itself takes about 10 minutes, although the whole consultation may take about 30 minutes.
The CVS procedure is usually described as being uncomfortable rather than painful, although you may experience some cramps that are similar to period pains for a few hours afterwards.
Find out more about what happens during CVS
Getting your results
The first results of the test should be available in about 3 days.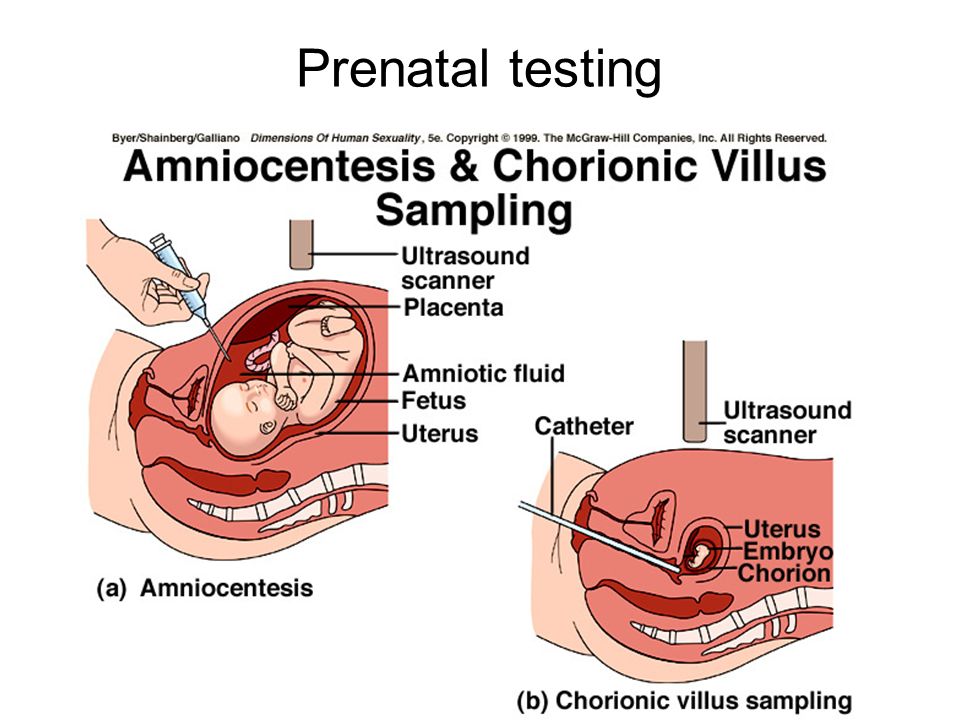 This is known as the rapid CVS result.
This is known as the rapid CVS result.
A more detailed set of CVS results will be available after 2 weeks.
If the rapid CVS result and a previous ultrasound scan both indicate your baby has a condition, your doctor will discuss your options with you straightaway.
If your previous ultrasound did not find anything unexpected, it’s recommended you wait until the more detailed set of CVS results before making a decision about ending your pregnancy.
If the results of these tests suggest it is highly likely your baby has a genetic condition, a specialist doctor (obstetrician) or midwife will explain what the screening results mean and talk to you about your options.
There's no cure for most of the conditions found by CVS, so you'll need to consider your options carefully.
You may decide to continue with your pregnancy while gathering information about the condition so you're fully prepared.
Find out more about having a baby that might be born with a genetic condition
Or you may consider ending your pregnancy (having a termination).
Find out more about the results of CVS
Miscarriage and infections.
Before you decide to have CVS, the possible complications will be discussed with you.
CVS can cause miscarriage, the loss of the pregnancy in the first 23 weeks. The chance of miscarrying after CVS is thought to be less than 1 in 200 for most pregnancies, and at around 1 in 100 for multiple pregnancies (such as twins).
You might also get an infection, or need to have CVS again because it was not successful the first time.
Read more about the complications of CVS
What are the alternatives?
An alternative to CVS is a test called amniocentesis.
This is where a small sample of amniotic fluid, the fluid that surrounds the baby in the womb, is removed for testing.
It's usually carried out between the 15th and 18th week of pregnancy, although it can be performed later than this if necessary.
This test can also cause a miscarriage, but your pregnancy will be at a more advanced stage before you can get the results, so you'll have less time to consider your options.
If you're offered tests to look for a genetic or chromosomal condition in your baby, a specialist involved in carrying out the test will be able to discuss the different options with you and help you make a decision.
Page last reviewed: 03 January 2023
Next review due: 03 January 2026
Amniocentesis / CVS (Chorionic Villus Biopsy | www.drmustafakir.com
Definitive diagnosis of chromosomal abnormalities can only be made by examining the infant's cells.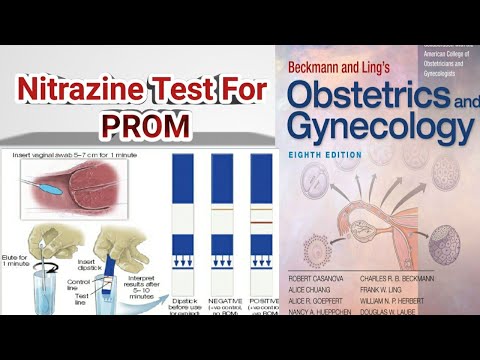 Methods used - placental biopsy - CVS (Chorionic Villus Biopsy) after 10 weeks or amniocentesis after 16 week
Methods used - placental biopsy - CVS (Chorionic Villus Biopsy) after 10 weeks or amniocentesis after 16 week
What is CVS
The placenta is in the same chromosomal structure as the baby For this reason, chromosomal analysis from the placenta also represents the baby Cvs can be performed after the 10th week With amniocentesis possible results 4-6 weeks earlier and if necessary, early termination of pregnancy Especially in the investigation of known genetic diseases, patients who test positive for "double test", ultrasound at 11-14 weeks
This can be done especially in the study of known genetic diseases, in which patients have a positive result on the "double test", as well as in the case of an abnormal structural substance that is noticeable in the ultrasound examination for 11-14 weeks. In this procedure, tissues are taken with a thicker needle than in amniocentesis.
Therefore, the skin and subcutaneous tissues are anesthetized first. But since it is impossible to anesthetize the uterus, there may be a slight burning sensation.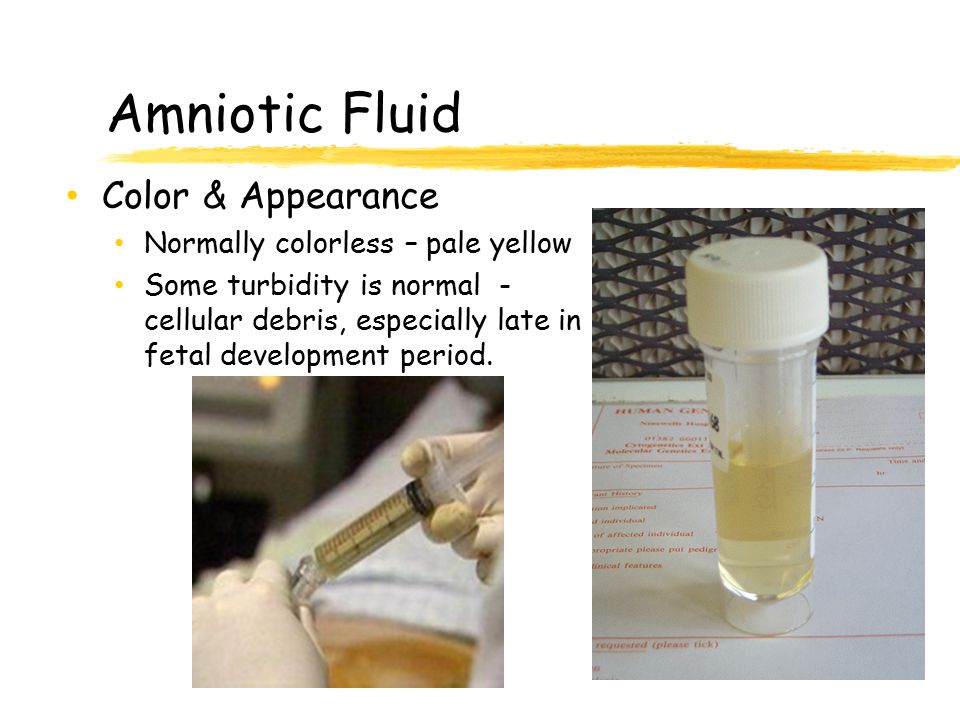 The risk of miscarriage is approximately 1%. nine0003
The risk of miscarriage is approximately 1%. nine0003
What is amniocentesis?
This is an amniotic fluid test in which a puncture is made in the fetal membrane and a sample of the amniotic fluid is taken. It contains fetal cells that are suitable for testing for the presence or absence of genetic diseases. The ideal time for this is after the 16th week of pregnancy. An early procedure can cause orthopedic problems in children. Approximately 15-20 ml of liquid is taken. There are cells in the amniotic fluid that spill out of the baby. These cells are separated from the fluid, and the structure and number of the child's chromosomes are determined in a genetic laboratory. This process takes about 2-3 weeks. Amniocentesis is also done in the diagnosis of some infections that affect the baby, in case of an increase in the amount of fluid (to decrease). nine0003
Is amniocentesis difficult? Can a child get hurt?
Amniocentesis is performed under ultrasound guidance with a fine needle. Usually a sample is taken at one time. It is not harmful to the child, because it is carried out under the supervision of an ultrasound.
Usually a sample is taken at one time. It is not harmful to the child, because it is carried out under the supervision of an ultrasound.
Can there be amniotic fluid leakage after amniocentesis?
In amniocentesis, approximately 10% of the fluid around the baby is taken and restored within a few hours. Therefore, there is always a sufficient amount of amniotic fluid around the baby. nine0003
Can light bleeding or leakage be a symptom of a miscarriage after a procedure?
1% of patients may have slight bleeding and leakage. It basically does not result in miscarriage.
When should I call my doctor?
Bleeding, severe pain, fever, leaks
Is proper bed rest required after amniocentesis?
Enough to rest at home that day. From the next day you can return to your daily life. nine0003
If amniocentesis is the definitive diagnostic tool, why is it not recommended for everyone?
Amniocentesis carries a 2-4% risk. Our main goal in detecting children with chromosomal disorders is to minimize the loss of a healthy child as a result of this procedure.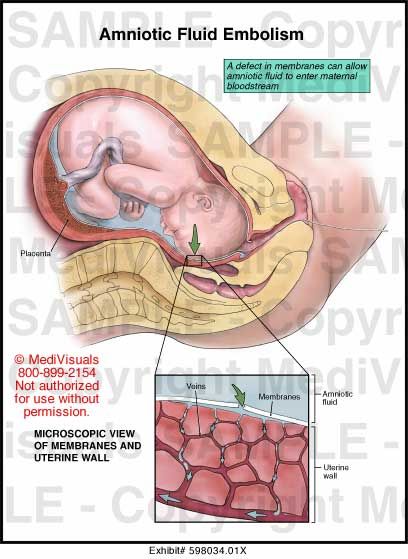 If we do an amniocentesis on every pregnant woman, we can miscarry 4-5 healthy pregnancies to capture a down syndrome pregnancy.
If we do an amniocentesis on every pregnant woman, we can miscarry 4-5 healthy pregnancies to capture a down syndrome pregnancy.
Who is recommended for amniocentesis?
Amniocentesis is recommended for high-risk pregnancies. Scanning methods are used to determine the risk.
Age: Numerical chromosomal abnormalities increase with age. The age of the mother may be an indication for amniocentesis. In particular, screening tests should be performed instead of direct amniocentesis in pregnant women, especially those under 40 years of age, and amniocentesis should be used in those who are at positive risk. For pregnant women over 40 years of age, screening tests or direct amniocentesis should be discussed and a decision made. nine0003
High-risk screening test
Suspected chromosomal/genetic disorder on ultrasound
Positive maternal DNA test
What is prenatal diagnosis (womb diagnosis)? | Prof. Dr. Selahattin KUMRU
Prenatal diagnosis, as a general concept, can be considered as identifying the problems of a baby still in the womb. The diagnosis of abnormalities or diseases of the fetus, as a promising field, has become of great interest, especially due to recent advances in engineering science and medicine. The advantages of detecting fetal abnormalities are the possibility of timely assistance if the disease is curable in utero, and if the treatment requires emergency postpartum intervention, this gives a chance to prepare all the necessary conditions for this in advance, and finally, in situations of incurable diseases, such a diagnosis allows us to discuss issue of termination of pregnancy. nine0003
The diagnosis of abnormalities or diseases of the fetus, as a promising field, has become of great interest, especially due to recent advances in engineering science and medicine. The advantages of detecting fetal abnormalities are the possibility of timely assistance if the disease is curable in utero, and if the treatment requires emergency postpartum intervention, this gives a chance to prepare all the necessary conditions for this in advance, and finally, in situations of incurable diseases, such a diagnosis allows us to discuss issue of termination of pregnancy. nine0003
How is prenatal diagnosis performed?
Today there are many ways to carry out prenatal diagnosis. Some of them are performed by methods that do not carry any discomfort and risk for the mother (non-invasive prenatal diagnosis), while others are diagnostic methods that may pose a danger to the mother and fetus (invasive prenatal diagnosis). This article will briefly describe the invasive methods that we use in diagnosing a fetus in the womb. nine0003
nine0003
Procedures performed by intervention in the mother's body for prenatal diagnosis can be called invasive diagnostic procedures. Their method is to get to the uterus, where the baby is, and take samples of the material from the fetus itself, the placenta, or amniotic fluid (amniotic fluid). Methods used today include amniocentesis (puncture of the amniotic membrane to obtain amniotic fluid for analysis), chorionic villus sampling (chorionic villus biopsy: CVS), fetal blood sampling (cordocentesis) and, in very rare cases, tissue biopsy. nine0003
What is amniocentesis?
Amniocentesis is the removal of amniotic fluid, which allows him to move and grow comfortably, as well as help the development of his lungs, and allow him to move without being under pressure from the umbilical cord. Virtually all of this amniotic fluid is made up of urine produced by the baby's kidneys after the first three months of pregnancy. Today, this amniocentesis procedure is performed accompanied by an ultrasound (video 1).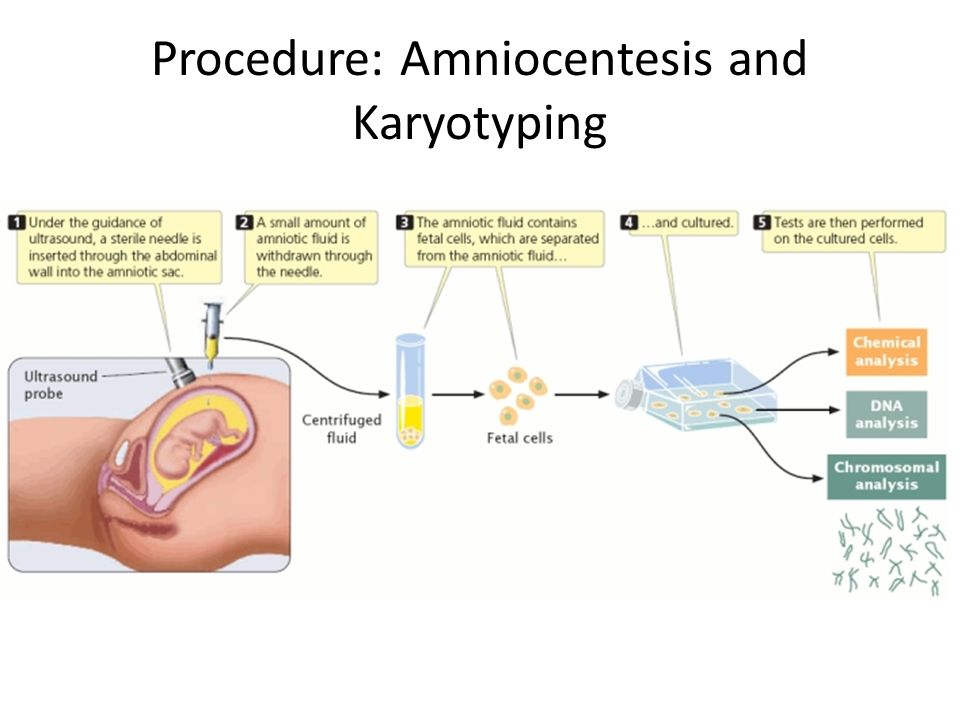
Video-1: Amniocentesis procedure (from our clinic's own practice). nine0003
What fetal disorders can be diagnosed by amniocentesis?
Because amniotic fluid is mostly fetal urine, many cells from the urinary tract get into this fluid. In addition, as the baby passes amniotic fluid through his lungs, cells from his skin and respiratory tract are also found in the amniotic fluid. Therefore, all tests carried out using the material of these cells can be carried out thanks to amniocentesis. nine0003
Around the world, amniocentesis is mainly performed to diagnose chromosomal problems and genetic disorders of the fetus. After sampling of the amniotic fluid, accompanied by ultrasound, the material is sent under sterile conditions to the genetic laboratory, where, after a series of careful studies, the results are obtained. Chromosomal disorders such as Down syndrome, Turner syndrome, trisomy 13 and trisomy 18, as well as many other genetically inherited monogenic diseases, can be detected by determining the number of chromosomes in a fetus by analyzing amniotic fluid obtained during amniocentesis (cytogenetic study).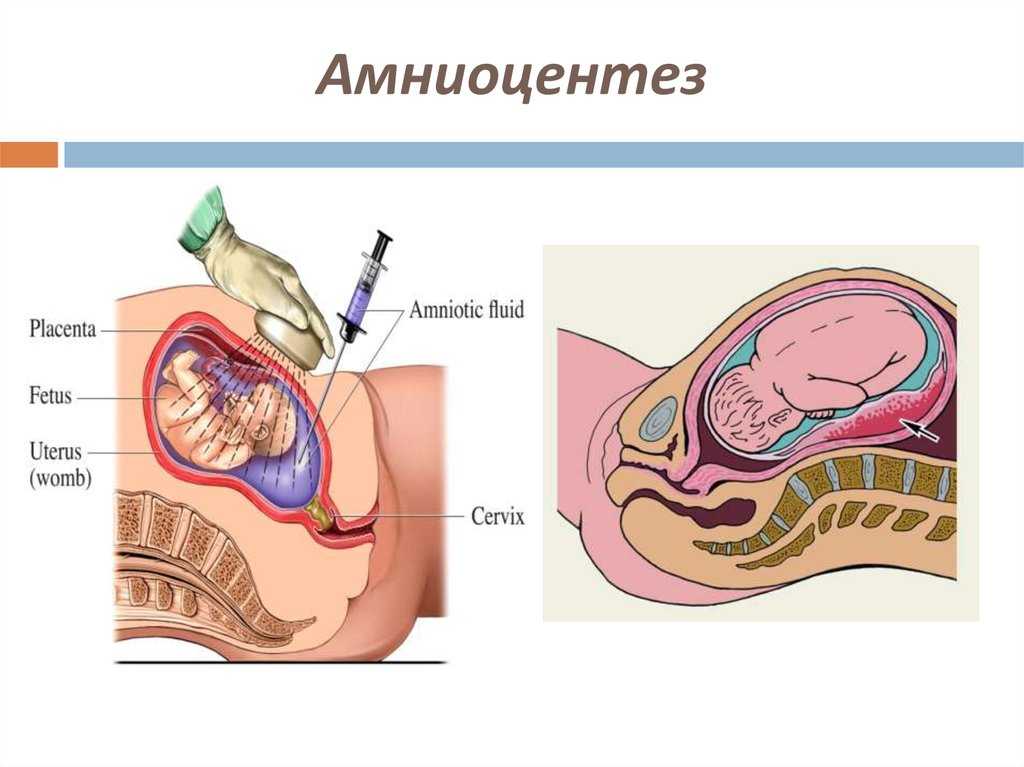 In addition, with the help of more detailed chromosomal studies, it is possible to identify more serious anomalies. Based on the amniotic fluid obtained by amniocentesis, it is possible to conduct a complete sequencing of the exome (a detailed analysis of the genetic material) of the fetus, as well as to conduct a study of the clinical exome, taking into account the results of ultrasound and the baby's medical history. It is also possible to determine from the amniotic fluid whether the child has any infectious diseases (toxoplasma, rubella, cytomegalovirus, syphilis, etc.). For this purpose, it is possible to examine both immunoglobulins in the amniotic fluid and the genetic material (DNA, RNA) of the diagnosed infection. Although amniocentesis is not common in our country, it can also be used to establish the fact of lung development in babies who, for whatever reason, should be born prematurely. nine0003
In addition, with the help of more detailed chromosomal studies, it is possible to identify more serious anomalies. Based on the amniotic fluid obtained by amniocentesis, it is possible to conduct a complete sequencing of the exome (a detailed analysis of the genetic material) of the fetus, as well as to conduct a study of the clinical exome, taking into account the results of ultrasound and the baby's medical history. It is also possible to determine from the amniotic fluid whether the child has any infectious diseases (toxoplasma, rubella, cytomegalovirus, syphilis, etc.). For this purpose, it is possible to examine both immunoglobulins in the amniotic fluid and the genetic material (DNA, RNA) of the diagnosed infection. Although amniocentesis is not common in our country, it can also be used to establish the fact of lung development in babies who, for whatever reason, should be born prematurely. nine0003
How risky is amniocentesis?
The amniocentesis procedure is very low risk if performed correctly and in experienced hands.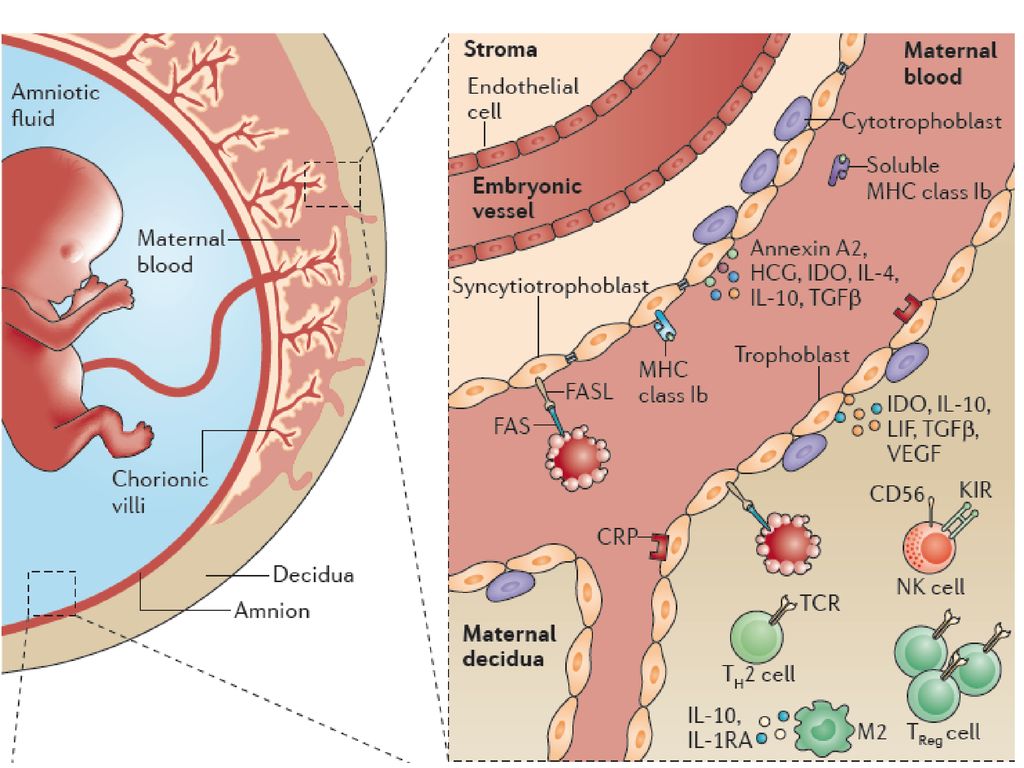 The chance of miscarriage due to amniocentesis is about one in two hundred (1/200). Considering that some babies undergoing this procedure have serious abnormalities that are practically incompatible with life from the very beginning, the threat of miscarriage due to amniocentesis in the case of healthy babies will be even less.
The chance of miscarriage due to amniocentesis is about one in two hundred (1/200). Considering that some babies undergoing this procedure have serious abnormalities that are practically incompatible with life from the very beginning, the threat of miscarriage due to amniocentesis in the case of healthy babies will be even less.
Chorionic villus sampling (chorionic villus biopsy)
Chorionic villus sampling (chorionic villus biopsy) is the process of taking samples from the fetal placenta accompanied by ultrasound. Since the fetus and placenta come from the same fertilized egg, it is assumed that the genetic structure of the placenta should match the genetic structure of the fetus. Because after the egg is fertilized, and the resulting zygote begins to divide, one part of these dividing cells forms the fetus, and the other part forms the placenta. That is why it is expected that their genetic composition will be the same. However, it is reported that very rarely (in less than one percent of cases) the genetic structure of the placenta does not always match that of the fetus. nine0003
nine0003
Why is it necessary to take a sample of chorionic villi (chorionic villus sampling)?
Chorionic villus sampling (chorionic villus biopsy) is used for prenatal genetic diagnosis in the same way as amniocentesis. Thanks to CVS, it is possible to recognize anomalies of the chromosomal number, as well as, having studied molecular genetics, monogenic diseases of the fetus.
When and how is a chorionic villus sample taken (chorionic villus biopsy)?
Compared to amniocentesis, CVS is done earlier in the pregnancy. Globally, the CVS procedure is usually performed between 11 and 14 weeks of pregnancy. The choice of exactly 11 weeks as the start is determined by concerns about an increase in the likelihood of anomalies in infants with CVS performed earlier. Given that amniocentesis is performed after the 16th week, CVS allows the recognition of fetal chromosomal disorders earlier than amniocentesis, which makes it possible to plan pregnancy in accordance with this result.