What is a uterus for
Uterus | Definition, Function, & Anatomy
uterus
See all media
- Related Topics:
- fallopian tube cervix puerperium bicornate uterus bipartite uterus
See all related content →
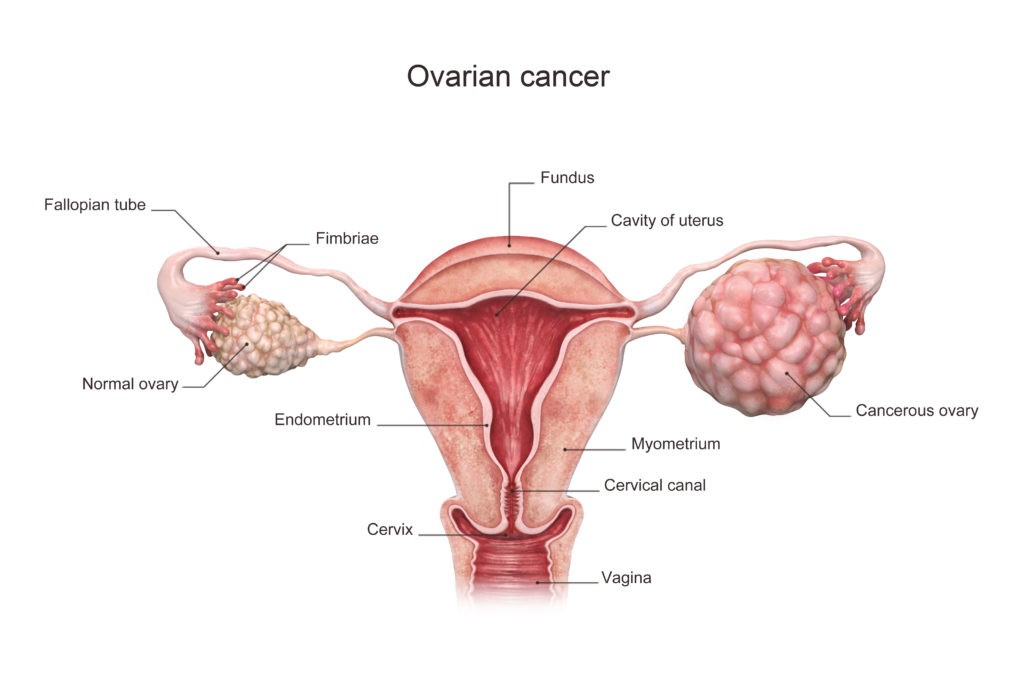
uterus, also called womb, an inverted pear-shaped muscular organ of the female reproductive system, located between the bladder and the rectum. It functions to nourish and house a fertilized egg until the fetus, or offspring, is ready to be delivered.
The uterus has four major regions: the fundus is the broad curved upper area in which the fallopian tubes connect to the uterus; the body, the main part of the uterus, starts directly below the level of the fallopian tubes and continues downward until the uterine walls and cavity begin to narrow; the isthmus is the lower, narrow neck region; and the lowest section, the cervix, extends downward from the isthmus until it opens into the vagina. The uterus is 6 to 8 cm (2.4 to 3.1 inches) long; its wall thickness is approximately 2 to 3 cm (0.8 to 1.2 inches). The width of the organ varies; it is generally about 6 cm wide at the fundus and only half this distance at the isthmus. The uterine cavity opens into the vaginal cavity, and the two make up what is commonly known as the birth canal.
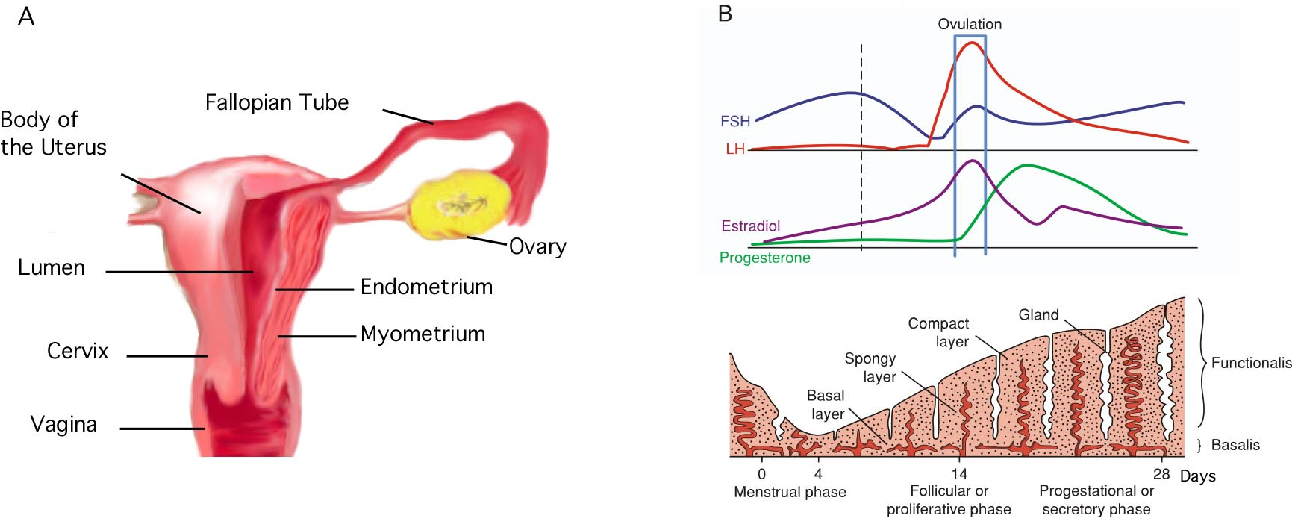
Lining the uterine cavity is a moist mucous membrane known as the endometrium. The lining changes in thickness during the menstrual cycle, being thickest during the period of egg release from the ovaries (see ovulation). If the egg is fertilized, it attaches to the thick endometrial wall of the uterus and begins developing. If the egg is unfertilized, the endometrial wall sheds its outer layer of cells; the egg and excess tissue are then passed from the body during menstrual bleeding. The endometrium also produces secretions that help keep both the egg and the sperm cells alive. The components of the endometrial fluid include water, iron, potassium, sodium, chloride, glucose (a sugar), and proteins.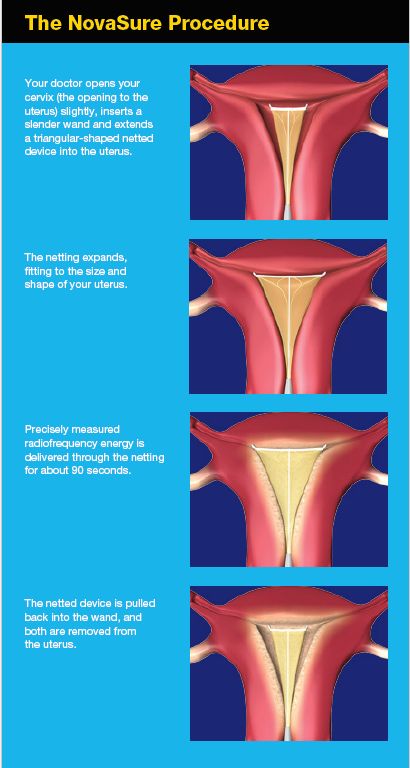 Glucose is a nutrient to the reproductive cells, while proteins aid with implantation of the fertilized egg. The other constituents provide a suitable environment for the egg and sperm cells.
Glucose is a nutrient to the reproductive cells, while proteins aid with implantation of the fertilized egg. The other constituents provide a suitable environment for the egg and sperm cells.
The uterine wall is made up of three layers of muscle tissue. The muscle fibres run longitudinally, circularly, and obliquely, entwined between connective tissue of blood vessels, elastic fibres, and collagen fibres. This strong muscle wall expands and becomes thinner as a child develops inside the uterus. After birth, the expanded uterus returns to its normal size in about six to eight weeks; its dimensions, however, are about 1 cm (0.4 inch) larger in all directions than before childbearing. The uterus is also slightly heavier and the uterine cavity remains larger.
The uterus of a female child is small until puberty, when it rapidly grows to its adult size and shape. After menopause, when the female is no longer capable of having children, the uterus becomes smaller, more fibrous, and paler. Some afflictions that may affect the uterus include infections; benign and malignant tumours; malformations, such as a double uterus; and prolapse, in which part of the uterus becomes displaced and protrudes from the vaginal opening. Uterus transplantation, in which a uterus from a healthy female is transplanted into the affected woman, has been considered a potential form of treatment in extreme cases of uterine disease or absence of the uterus; the first birth of a healthy infant to a uterus transplant recipient occurred in 2014.
Some afflictions that may affect the uterus include infections; benign and malignant tumours; malformations, such as a double uterus; and prolapse, in which part of the uterus becomes displaced and protrudes from the vaginal opening. Uterus transplantation, in which a uterus from a healthy female is transplanted into the affected woman, has been considered a potential form of treatment in extreme cases of uterine disease or absence of the uterus; the first birth of a healthy infant to a uterus transplant recipient occurred in 2014.
The Editors of Encyclopaedia Britannica This article was most recently revised and updated by Kara Rogers.
Physiology, Uterus - StatPearls - NCBI Bookshelf
Adi Gasner; Aatsha P A.
Author Information
Last Update: May 19, 2022.
Introduction
The uterus is a female reproductive organ that is responsible for many functions in the processes of implantation, gestation, menstruation, and labor.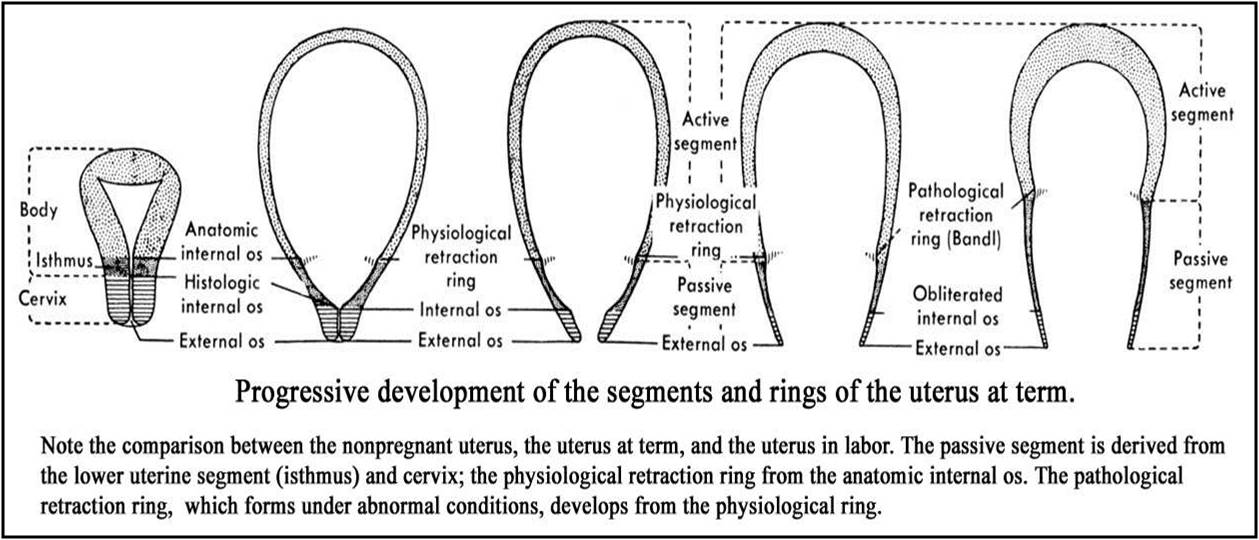
Anatomic Overview
The uterus is a thick-walled muscular structure that lies in the midline of the abdominal pelvic cavity. It contains three layers: the endometrium (innermost layer), myometrium, and the perimetrium (outermost layer). The endometrium’s thickness and structure vary based on hormonal stimulation
The uterus has four parts: the fundus, corpus, isthmus, and cervix. The corpus is the largest segment and connects to the cervix via the isthmus. The cervix connects the uterine body to the vaginal lumen. The uterus sits posterior to the bladder and anterior to the rectum.[1][2]
Uterus Support Structure
The round ligament connects the uterus to the abdominal wall and includes the artery of Sampson. The broad ligament connects the lateral portion of the uterus with the fallopian tube and ovary. The uterine artery, cardinal arteries, and ureter travel within the broad ligament. The ovarian ligament connects the ovary to the lateral surface of the uterus.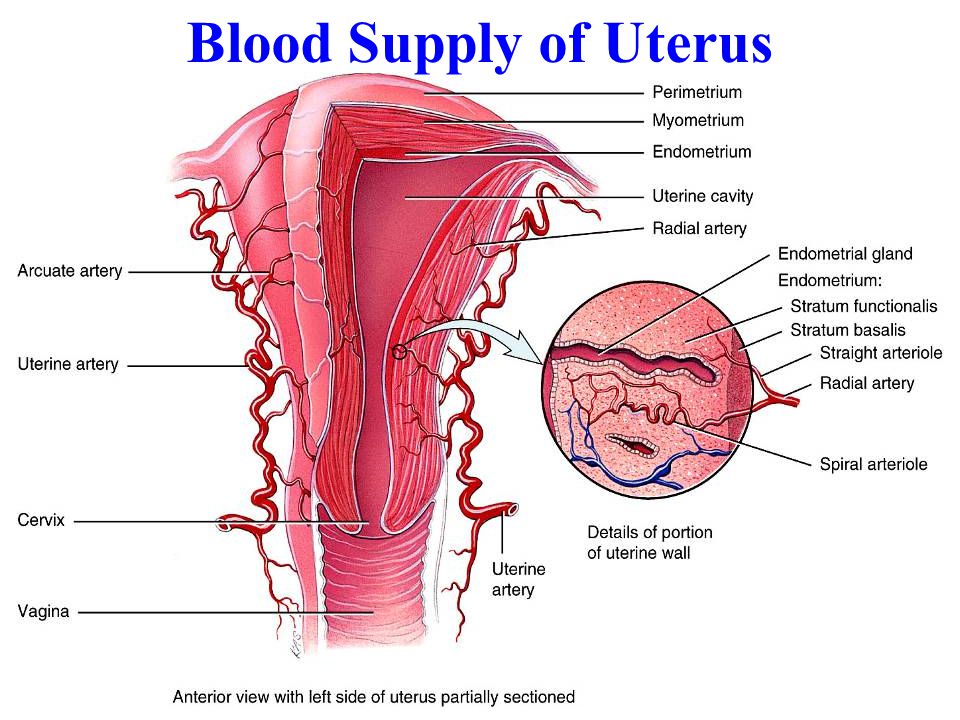 The infundibulopelvic (IP) ligament connects the ovary to the abdominal wall. Within the IP ligament are the ovarian artery and vein.
The infundibulopelvic (IP) ligament connects the ovary to the abdominal wall. Within the IP ligament are the ovarian artery and vein.
Uterine Vasculature
The uterine artery is the main blood supply to the uterus, with some collateral supply from the ovarian artery.
Uterine Innervation
The uterus is innervated sympathetically and parasympathetically through the hypogastric nerve and pelvic splanchnic nerves, respectively.[3][4][5]
Development
At 5 to 6 weeks gestation, the paramesonephric (Mullerian) ducts arise as coelomic epithelial invaginations that appear on the lateral surface of the paired urogenital ridges, the development of these ducts is due to the absence of anti-Mullerian hormone.[6][7] At eight weeks gestation, the paramesonephric ducts fuse vertically. The fused cranial and horizontal ends will give rise to what will ultimately become the fallopian tubes, while the caudal component will fuse to form the uterus, cervix, and upper third of the vagina.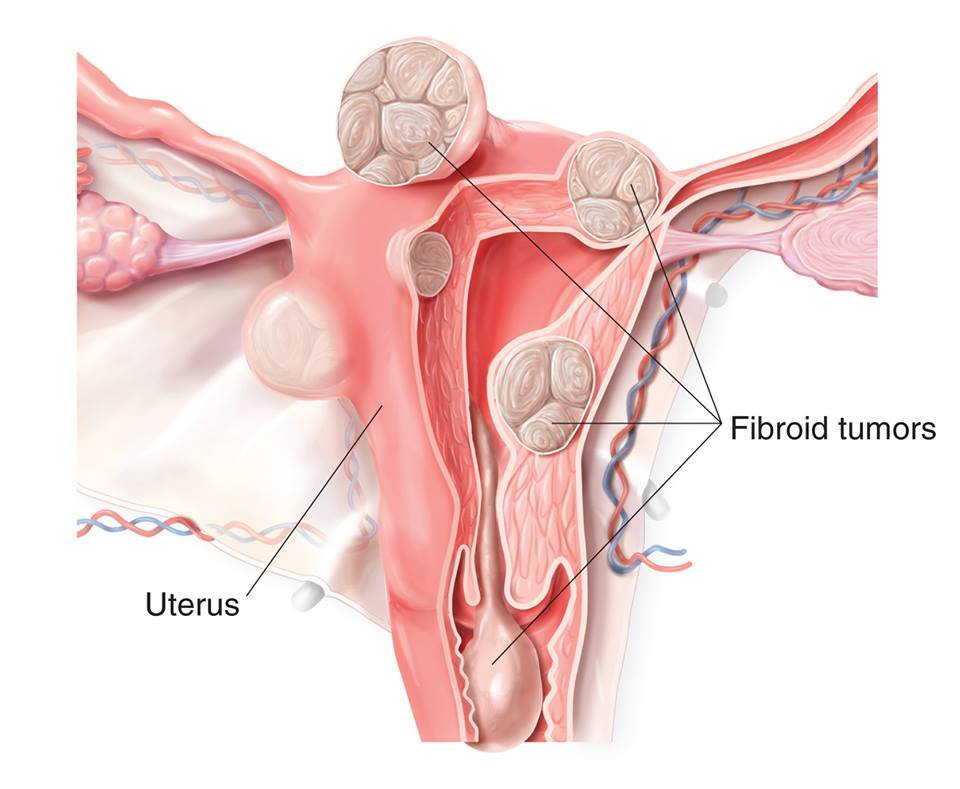 The uterine corpus remains underdeveloped at birth and reaches functional and anatomical maturity at the time of menarche.[8][9][10]
The uterine corpus remains underdeveloped at birth and reaches functional and anatomical maturity at the time of menarche.[8][9][10]
Function
The uterus carries out many functions:
Implantation site of the blastocyst
Provides protection and support for the fetus to grow
Site of menstruation
Mechanism
Reproductive Cycle
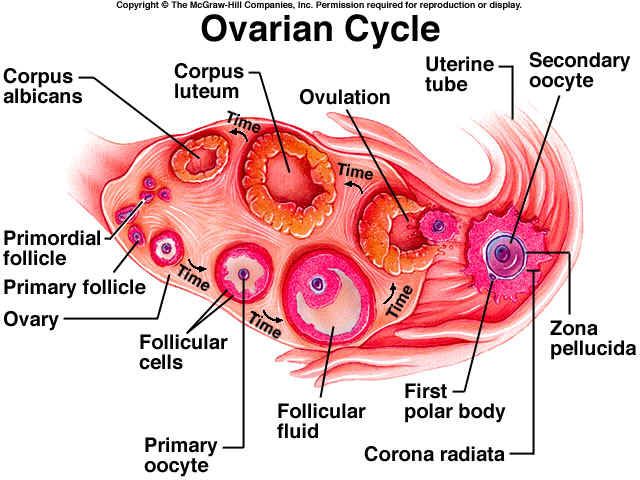
In the female reproductive cycle, there are two concurrent cycles, the ovarian cycle, and the uterine (menstrual) cycle. The ovarian cycle consists of a series of events that occur during and following oocyte maturation. The uterine cycle consists of a series of changes within the endometrium in preparation for the arrival of a fertilized ovum that will develop within the endometrium until birth.
The reproductive cycle can subdivide into the menstrual phase, preovulatory phase, ovulation, and postovulatory phase. The function of the uterus in each of these phases follows:
In the menstrual phase, a decline in estrogen and progesterone levels stimulates the release of prostaglandins, which results in vasoconstriction of arterioles within the uterus.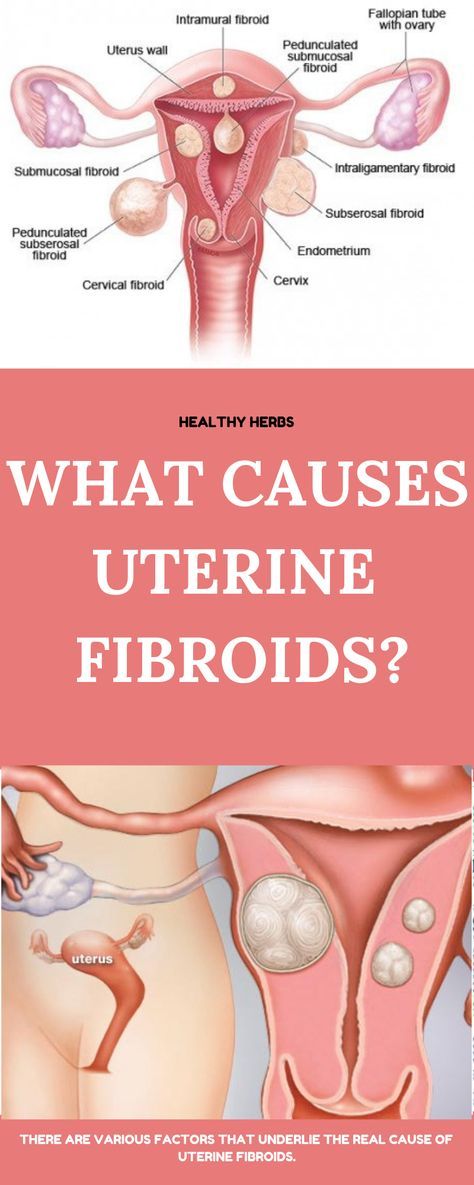 The vasoconstriction eventually leads to hypoperfusion of these cells, which results in cell death. This process initiates the sloughing off of blood, fluid, and epithelial cells from the endometrial walls into the cervix and out through the vagina.
The vasoconstriction eventually leads to hypoperfusion of these cells, which results in cell death. This process initiates the sloughing off of blood, fluid, and epithelial cells from the endometrial walls into the cervix and out through the vagina.
In the preovulatory phase, estrogen is released into the blood, which repairs the endometrium. The endometrium undergoes other changes and doubles in thickness.
During ovulation, the follicle ruptures and releases an oocyte that enters the uterine tube.
In the postovulatory phase, progesterone and estrogen stimulate further growth of endometrial glands and thickening of the endometrium in preparation for the implantation of a fertilized ovum. If fertilization does not occur, progesterone end estrogen levels decline, and the menstruation stage occurs.
If the egg becomes fertilized, the zygote is propelled down the fallopian tubes into the uterus. The zygote cells divide rapidly during this descent. The cells of the zygote continue to divide until it becomes a blastocyst.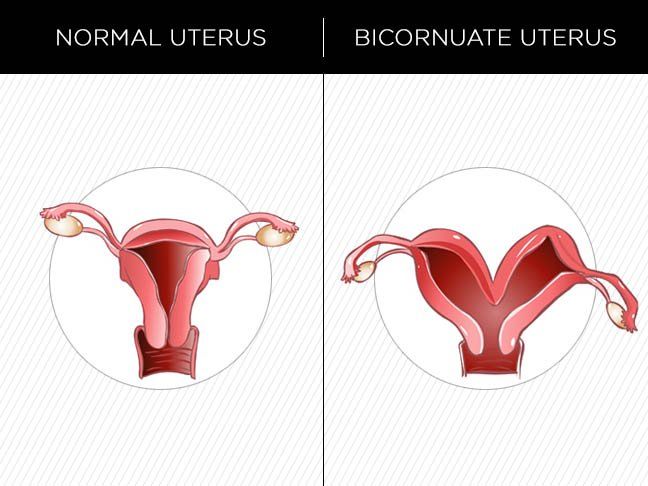 This blastocyst implants by invading the wall of the endometrium.[11]
This blastocyst implants by invading the wall of the endometrium.[11]
Pregnancy
When the blastocyst successfully implants into the endometrial lining, it develops over many weeks into an embryo and then a fetus. During the development of an embryo into a fetus, changes occur within the endometrium that leads to placental formation. The placenta provides a crossing point between the developing fetus and maternal circulation. In pregnancy, the uterus hypertrophies to accommodate the growing fetus. It typically reaches the height of the umbilicus at 20 weeks and the xiphoid process at 38 weeks.
Labor
The uterus undergoes many changes during labor due to the release of various hormones. Nearing the seventh month of pregnancy, progesterone levels begin to decline while estrogen levels steadily rise. The increasing ratio of estrogen to progesterone causes the myometrium to become more sensitive to stimuli that promote contractions. Additionally, fetal cortisol rises in the eighth month of pregnancy, which further reduces progesterone’s effects.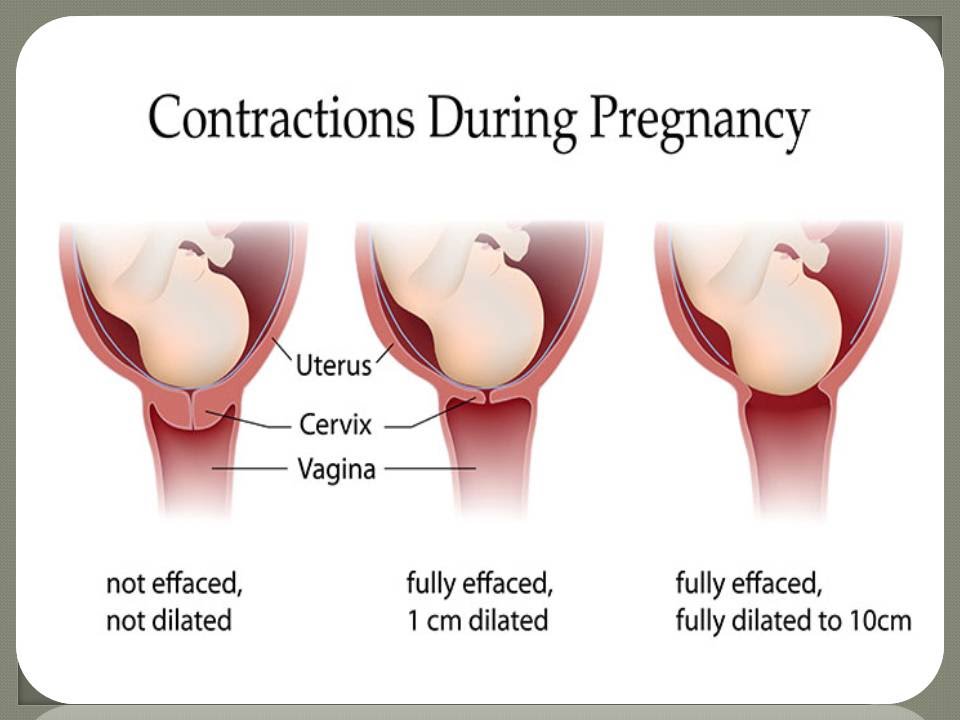 [12][13]
[12][13]
As true labor approaches, oxytocin and prostaglandins both play a role in further stimulating myometrial contractions and increasing contractile strength. The fetus causes the myometrium and cervix to stretch, which also stimulates uterine contractions.[14]
During true labor, the release of oxytocin and prostaglandins stimulate a positive feedback loop which continues to increase uterine contractile strength. These uterine contractions dilate and efface the cervix. Again a positive feedback loop begins where the effacement and dilation of the cervix further promote uterine contractions. Contractions become more frequent and longer in duration as labor progresses. The next stage of labor begins when the fetal head enters the birth canal and completes when the infant is born. The myometrium continues to contract after birth, causing the placenta to shear from the back of the uterine wall for delivery through the birth canal.[15]
Pathophysiology
Within uterine development, Mullerian duct abnormalities can be present.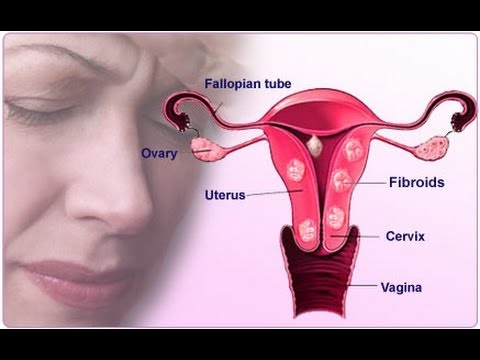 These can include incomplete fusion of the Mullerian ducts during embryogenesis, leading to abnormal uterine development. There are also a host of acquired uterine conditions that can occur in any of the three uterine layers but most commonly target the endometrium and myometrium. In acquired or congenital uterine abnormalities, patients can either appear symptomatic or have associated complications such as infertility, recurrent miscarriages, and prematurity. Appropriate application of the function and common pathologies of the uterus can directly impact the mortality and morbidity of women everywhere, especially as it relates to pregnancy-related changes. A discussion of the most common pathologies in each of these categories will appear below.
These can include incomplete fusion of the Mullerian ducts during embryogenesis, leading to abnormal uterine development. There are also a host of acquired uterine conditions that can occur in any of the three uterine layers but most commonly target the endometrium and myometrium. In acquired or congenital uterine abnormalities, patients can either appear symptomatic or have associated complications such as infertility, recurrent miscarriages, and prematurity. Appropriate application of the function and common pathologies of the uterus can directly impact the mortality and morbidity of women everywhere, especially as it relates to pregnancy-related changes. A discussion of the most common pathologies in each of these categories will appear below.
Clinical Significance
Congenital Defects
The septate uterus is the most common structural uterine anomaly.[16] It occurs when the partition between the two fused Mullerian ducts fails to resorb. This remnant results in a fibromuscular septum that can be partial or complete, which would divide the uterine cavity and cervix into two separate components.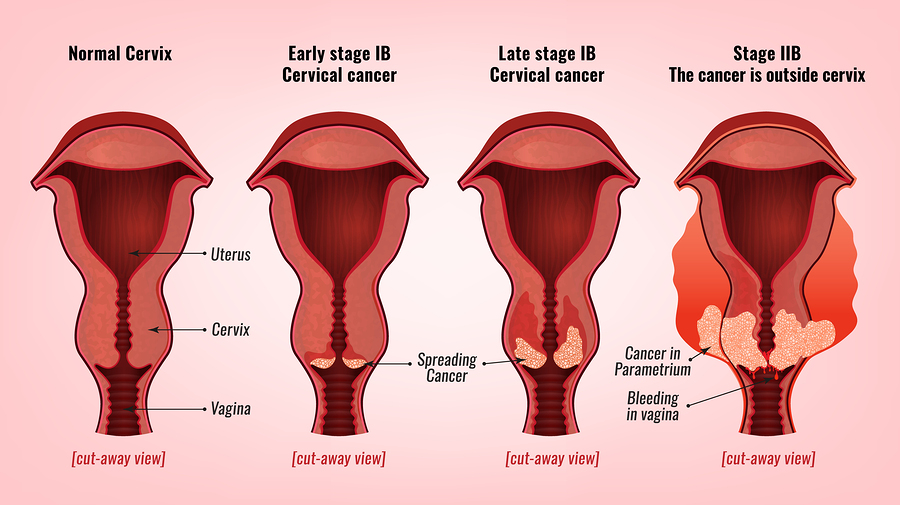 [17] Uterus didelphys occurs when there is a complete failure of fusion of the paired Mullerian ducts. As such, the uterus presents as a paired organ with two endometrial cavities, each with a cervix.[18] Additionally, a bicornuate uterus is a structural anomaly that can occur. In this condition, there is an incomplete fusion of the paramesonephric ducts, which produces a bicornuate uterus. Similar to uterus didelphys, there are two separate endometrial cavities; however, there is one cervix.[18]
[17] Uterus didelphys occurs when there is a complete failure of fusion of the paired Mullerian ducts. As such, the uterus presents as a paired organ with two endometrial cavities, each with a cervix.[18] Additionally, a bicornuate uterus is a structural anomaly that can occur. In this condition, there is an incomplete fusion of the paramesonephric ducts, which produces a bicornuate uterus. Similar to uterus didelphys, there are two separate endometrial cavities; however, there is one cervix.[18]
Acquired Conditions
One of the most common diseases of the uterus is uterine fibroids, also known as leiomyomata. This disorder characteristically presents with benign, smooth muscle tumors found in the myometrial layer [18]. Another condition that affects the myometrium is adenomyosis. In this disease, endometrial tissue embeds into the myometrium, which can result in abnormal uterine bleeding and secondary dysmenorrhea.[19]
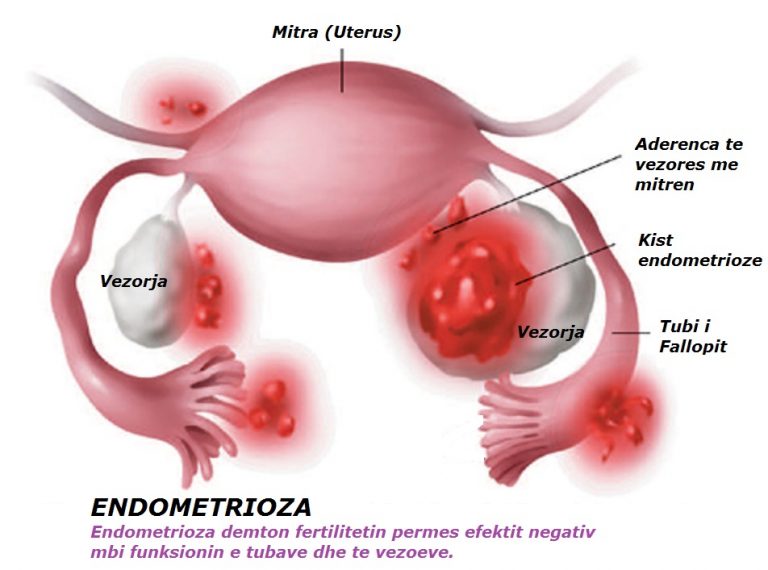
A common pathology affecting the endometrium is endometriosis.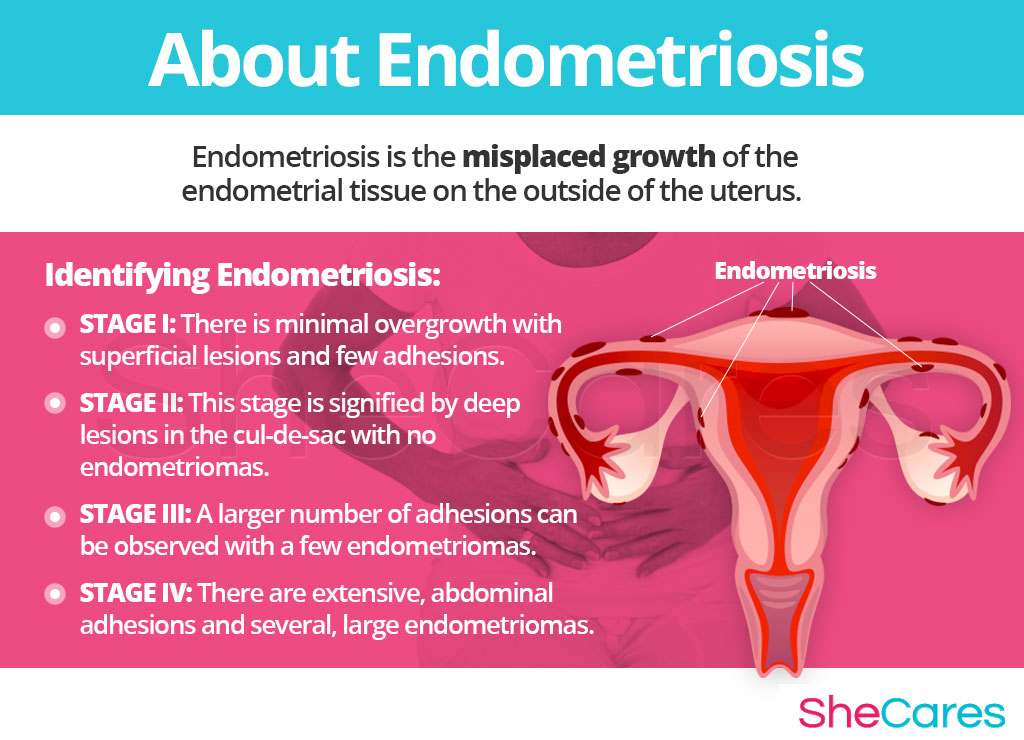 This condition is an estrogen-dependent disorder characterized by glandular tissue and stroma outside the uterine cavity.[20] It can often be accompanied by dyspareunia, bleeding, dysmenorrhea, and infertility.[21] Endometrial polyps are another common pathology that causes benign, local overgrowths of endometrial tissue.[21] Endometritis, an inflammatory disorder of the endometrium, is due to a bacterial infection either from external bacteria such as Chlamydia trachomatis or from the normal bacterial flora found in the vagina.[22] Another condition that can affect the endometrium is endometrial hyperplasia, which is caused by excessive growth of endometrial glands due to increased unopposed exposure to estrogen and can be a predisposing factor for endometrial carcinoma.[23]
This condition is an estrogen-dependent disorder characterized by glandular tissue and stroma outside the uterine cavity.[20] It can often be accompanied by dyspareunia, bleeding, dysmenorrhea, and infertility.[21] Endometrial polyps are another common pathology that causes benign, local overgrowths of endometrial tissue.[21] Endometritis, an inflammatory disorder of the endometrium, is due to a bacterial infection either from external bacteria such as Chlamydia trachomatis or from the normal bacterial flora found in the vagina.[22] Another condition that can affect the endometrium is endometrial hyperplasia, which is caused by excessive growth of endometrial glands due to increased unopposed exposure to estrogen and can be a predisposing factor for endometrial carcinoma.[23]
Endometrial carcinoma is a common gynecological malignancy and the most common type of uterine cancer. Its characteristics include malignant cells arising in the endometrial layer. It classifies into two major types: Type I and Type II and can present with abnormal uterine bleeding, including post-menopausal bleeding.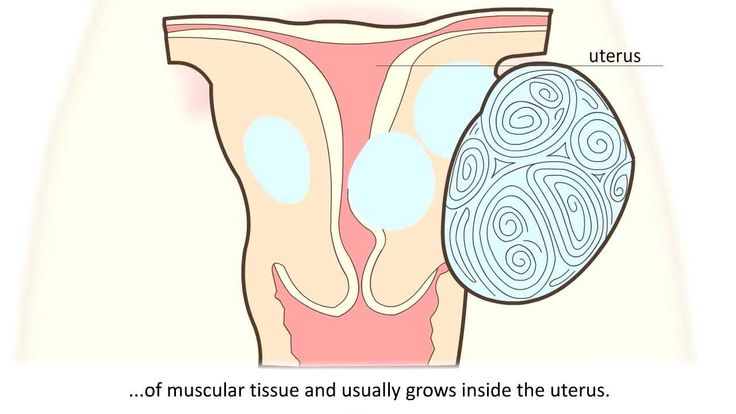 [24][25]
[24][25]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Roach MK, Andreotti RF. The Normal Female Pelvis. Clin Obstet Gynecol. 2017 Mar;60(1):3-10. [PubMed: 28005593]
- 2.
Cooke PS, Spencer TE, Bartol FF, Hayashi K. Uterine glands: development, function and experimental model systems. Mol Hum Reprod. 2013 Sep;19(9):547-58. [PMC free article: PMC3749806] [PubMed: 23619340]
- 3.
Kido A, Togashi K. Uterine anatomy and function on cine magnetic resonance imaging. Reprod Med Biol. 2016 Oct;15(4):191-199. [PMC free article: PMC5715863] [PubMed: 29259437]
- 4.
Ameer MA, Fagan SE, Sosa-Stanley JN, Peterson DC. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Feb 23, 2022. Anatomy, Abdomen and Pelvis, Uterus. [PubMed: 29262069]
- 5.
Rosner J, Samardzic T, Sarao MS.
 StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Oct 9, 2021. Physiology, Female Reproduction. [PubMed: 30725817]
StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Oct 9, 2021. Physiology, Female Reproduction. [PubMed: 30725817]- 6.
Moncada-Madrazo M, Rodríguez Valero C. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 31, 2021. Embryology, Uterus. [PubMed: 31613528]
- 7.
Cunha GR, Kurita T, Cao M, Shen J, Cooke PS, Robboy SJ, Baskin LS. Tissue interactions and estrogenic response during human female fetal reproductive tract development. Differentiation. 2018 May - Jun;101:39-45. [PMC free article: PMC5993605] [PubMed: 29684808]
- 8.
Sulak O, Cosar F, Malas MA, Cankara N, Cetin E, Tagil SM. Anatomical development of the fetal uterus. Early Hum Dev. 2007 Jun;83(6):395-401. [PubMed: 17045762]
- 9.
Ye L, Mayberry R, Lo CY, Britt KL, Stanley EG, Elefanty AG, Gargett CE. Generation of human female reproductive tract epithelium from human embryonic stem cells. PLoS One. 2011;6(6):e21136.
 [PMC free article: PMC3115988] [PubMed: 21698266]
[PMC free article: PMC3115988] [PubMed: 21698266]- 10.
Cunha GR, Robboy SJ, Kurita T, Isaacson D, Shen J, Cao M, Baskin LS. Development of the human female reproductive tract. Differentiation. 2018 Sep - Oct;103:46-65. [PMC free article: PMC6234064] [PubMed: 30236463]
- 11.
Kapila V, Chaudhry K. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 26, 2021. Physiology, Placenta. [PubMed: 30855916]
- 12.
Chwalisz K, Garfield RE. Regulation of the uterus and cervix during pregnancy and labor. Role of progesterone and nitric oxide. Ann N Y Acad Sci. 1997 Sep 26;828:238-53. [PubMed: 9329845]
- 13.
Olson DM, Mijovic JE, Sadowsky DW. Control of human parturition. Semin Perinatol. 1995 Feb;19(1):52-63. [PubMed: 7754411]
- 14.
Hutchison J, Mahdy H, Hutchison J. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Feb 26, 2022. Stages of Labor. [PubMed: 31335010]
- 15.
Gross MM. [The five stages of labour]. Z Geburtshilfe Neonatol. 2002 Nov-Dec;206(6):236-41. [PubMed: 12476398]
- 16.
Raga F, Bauset C, Remohi J, Bonilla-Musoles F, Simón C, Pellicer A. Reproductive impact of congenital Müllerian anomalies. Hum Reprod. 1997 Oct;12(10):2277-81. [PubMed: 9402295]
- 17.
Taylor E, Gomel V. The uterus and fertility. Fertil Steril. 2008 Jan;89(1):1-16. [PubMed: 18155200]
- 18.
Patton PE. Anatomic uterine defects. Clin Obstet Gynecol. 1994 Sep;37(3):705-21. [PubMed: 7955655]
- 19.
Pavlik RM. Adenomyosis--an ignored uterine disease. Nurse Pract. 1995 Apr;20(4):32-4, 39-40, 43. [PubMed: 7596529]
- 20.
Lim HJ, Wang H. Uterine disorders and pregnancy complications: insights from mouse models. J Clin Invest. 2010 Apr;120(4):1004-15. [PMC free article: PMC2846054] [PubMed: 20364098]
- 21.
Cakmak H, Taylor HS. Implantation failure: molecular mechanisms and clinical treatment.
 Hum Reprod Update. 2011 Mar-Apr;17(2):242-53. [PMC free article: PMC3039220] [PubMed: 20729534]
Hum Reprod Update. 2011 Mar-Apr;17(2):242-53. [PMC free article: PMC3039220] [PubMed: 20729534]- 22.
Kitaya K, Takeuchi T, Mizuta S, Matsubayashi H, Ishikawa T. Endometritis: new time, new concepts. Fertil Steril. 2018 Aug;110(3):344-350. [PubMed: 29960704]
- 23.
Reed SD, Newton KM, Clinton WL, Epplein M, Garcia R, Allison K, Voigt LF, Weiss NS. Incidence of endometrial hyperplasia. Am J Obstet Gynecol. 2009 Jun;200(6):678.e1-6. [PMC free article: PMC2692753] [PubMed: 19393600]
- 24.
Sorosky JI. Endometrial cancer. Obstet Gynecol. 2012 Aug;120(2 Pt 1):383-97. [PubMed: 22825101]
- 25.
Di Cristofano A, Ellenson LH. Endometrial carcinoma. Annu Rev Pathol. 2007;2:57-85. [PubMed: 18039093]
How is the female body? - Family clinic Arnika, Krasnoyarsk
Services
Virtual tour. Clinic "ARNIKA"
Did you know that the uterus can increase 20 times during pregnancy? This is a unique organ located in the pelvis and connected to the fallopian tubes.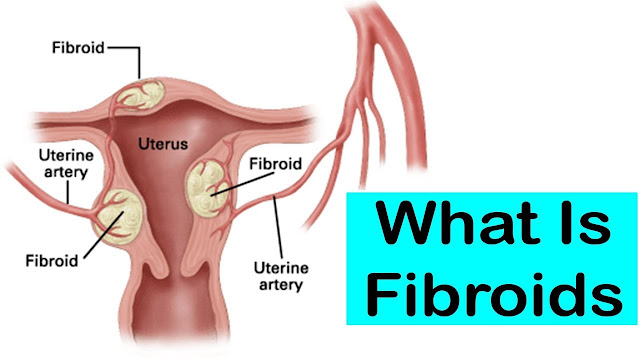 If the fallopian tubes are blocked, infertility or an ectopic pregnancy may develop. The cervix connects the uterus and vagina, and the ovaries produce eggs.
If the fallopian tubes are blocked, infertility or an ectopic pregnancy may develop. The cervix connects the uterus and vagina, and the ovaries produce eggs.
Uterus
The most important function of the uterus is to carry the fetus (unborn child) during pregnancy. The uterus is a truly unique organ: during pregnancy, it increases about 20 times. You can calculate it yourself: in a non-pregnant woman, the uterus weighs about 50-60 g, and by the end of pregnancy, its weight reaches 1 kg. After childbirth, the uterus contracts, decreasing to its normal size.
The uterus is located in the small pelvis, behind the pubis. In front of the uterus is the bladder, and behind the uterus is the intestines. During the examination on the gynecological chair, the gynecologist cannot see the uterus, but he can feel it and determine the size.
The uterus looks like a pouch turned upside down. The walls of the uterus are very thick and are made up of muscles.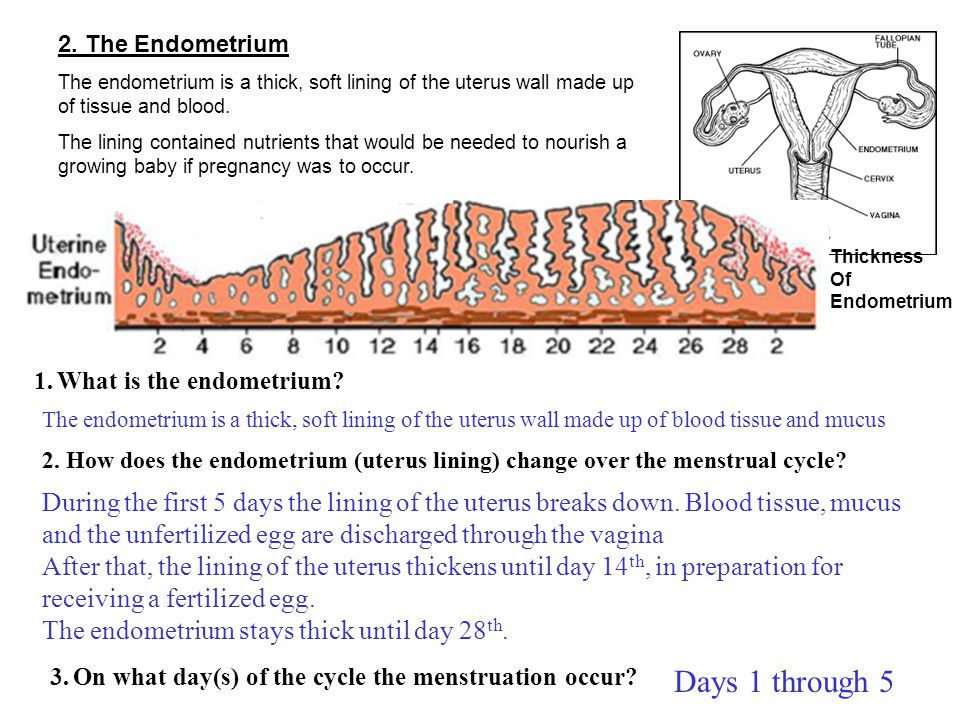 Thanks to these muscles, the birth of a child is possible. During childbirth, the muscles of the uterus begin to contract intensely, pushing the baby out.
Thanks to these muscles, the birth of a child is possible. During childbirth, the muscles of the uterus begin to contract intensely, pushing the baby out.
There is a small cavity inside the uterus. In the uterine cavity is the endometrium - the inner layer of the uterus. Every month, the endometrium is shed from the uterine cavity, coming out through the vagina. This is menstruation, or menstruation.
Cervix
The cervix is the continuation of the uterus, its lower part, which also consists of muscles and separates the uterus from the vagina.
There is a channel in the center of the cervix called the cervical canal. Through this channel, the endometrium is excreted during menstruation, and through it the spermatozoa enter the uterus, and then meet with the egg. The cervical canal is very narrow, but during childbirth it expands to allow the baby to leave the uterus.
The gynecologist can see the lower part of the cervix, as well as the external opening of the cervical canal during examination on the gynecological chair.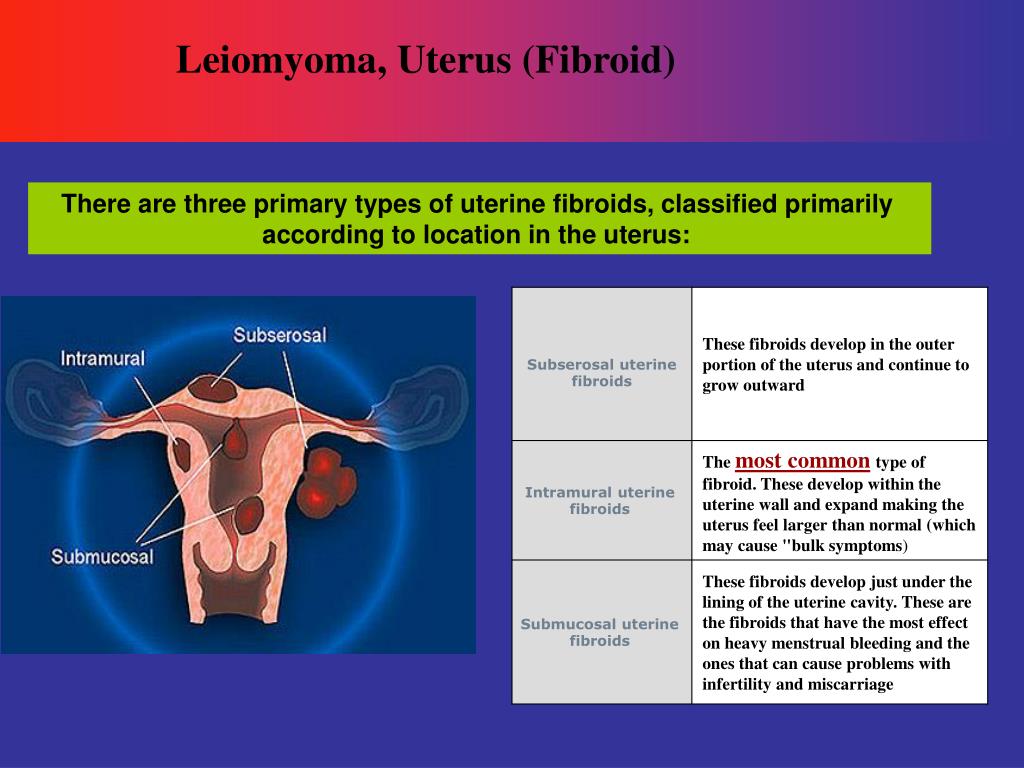 In order to have a good look at the cervix, the gynecologist uses a speculum.
In order to have a good look at the cervix, the gynecologist uses a speculum.
The cervix is subject to various diseases: erosion and pseudo-erosion of the cervix (ectopia), cervical dysplasia, cervical cancer, inflammation of the cervix (cervicitis), etc. In order to identify these diseases in time, every woman should regularly visit a gynecologist and take a smear for cytology at least once every 2 years.
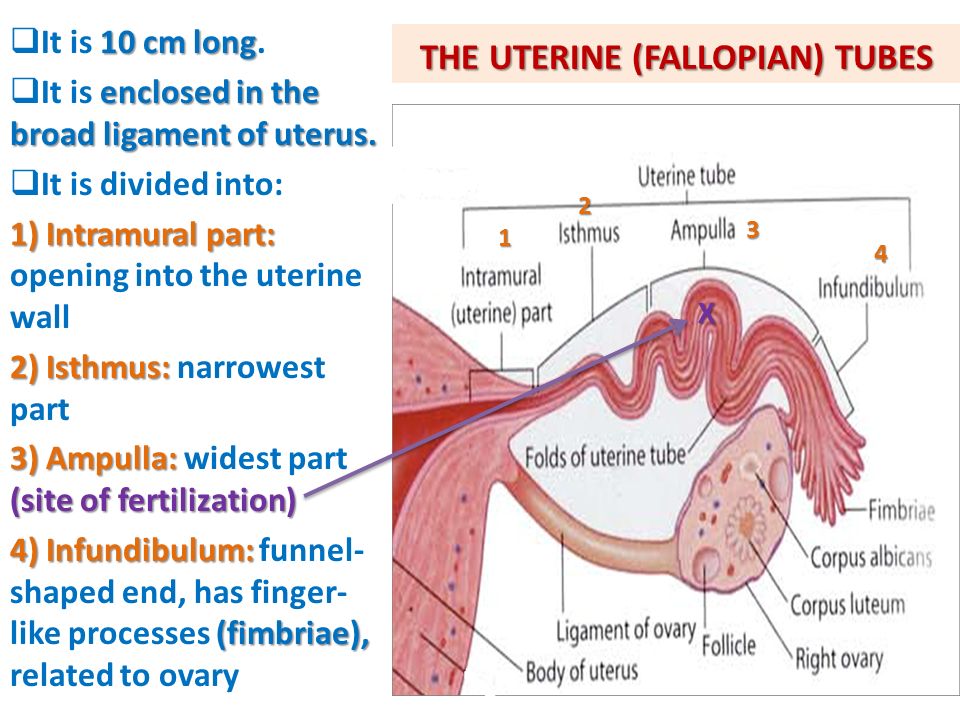
Fallopian tubes
Every woman has 2 fallopian tubes: to the left and to the right of the uterus. Fallopian tubes are also called fallopian tubes, after the scientist Fallopius, who first described them. The fallopian tubes connect to the uterine cavity on the sides, at the top of the uterus.
It is in the fallopian tubes that the meeting of the spermatozoon and the ovum most often takes place. Having united in one cell, they move towards the uterus in order to attach in its cavity and continue their development.
Inflammation of the fallopian tubes can lead to their obstruction.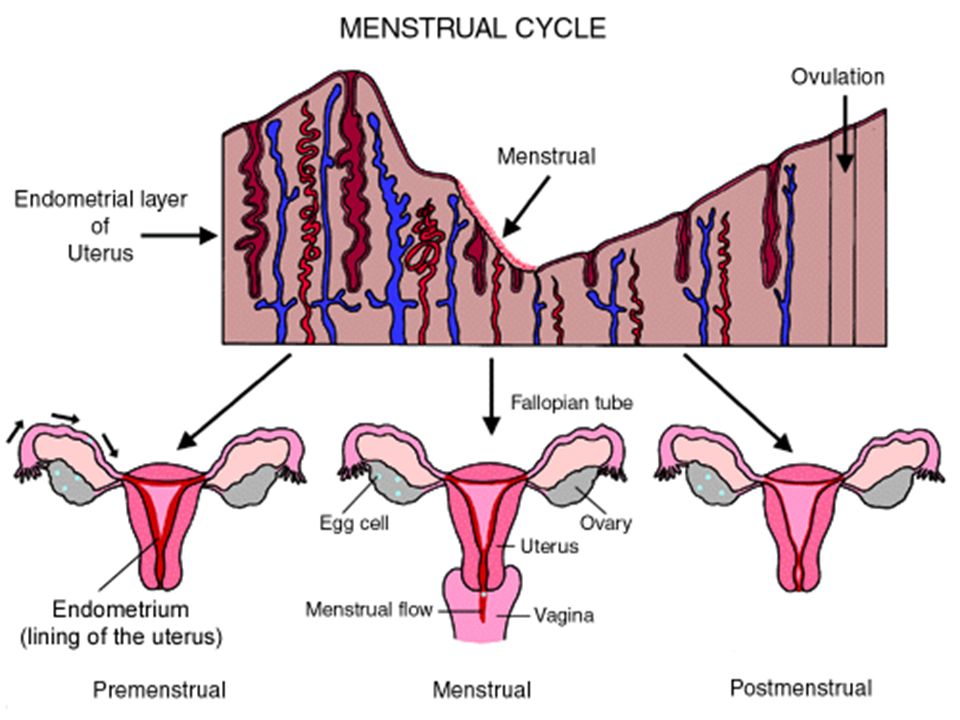 If the fallopian tubes are blocked, then the sperm and egg cannot meet, and pregnancy in this case is impossible.
If the fallopian tubes are blocked, then the sperm and egg cannot meet, and pregnancy in this case is impossible.
Fallopian tubes are normally not visible on ultrasound. During examination and palpation, the gynecologist also cannot palpate the fallopian tubes. In order to determine the condition of the fallopian tubes, hysterosalpingography is used.
Ovaries
Every woman has 2 ovaries: right and left. From the moment of puberty (from about 12-13 years old), every month an egg matures in one of the ovaries. The ovum is the "half" of the unborn child, which, when combined with the second "half" - the sperm, forms an embryo.
The egg matures inside a vesicle called a follicle. When the follicle reaches a certain size, it bursts and an egg is released from it. This moment is called ovulation. It is on the day of ovulation that a woman can become pregnant.
Another important feature of the ovaries is the ability to produce sex hormones.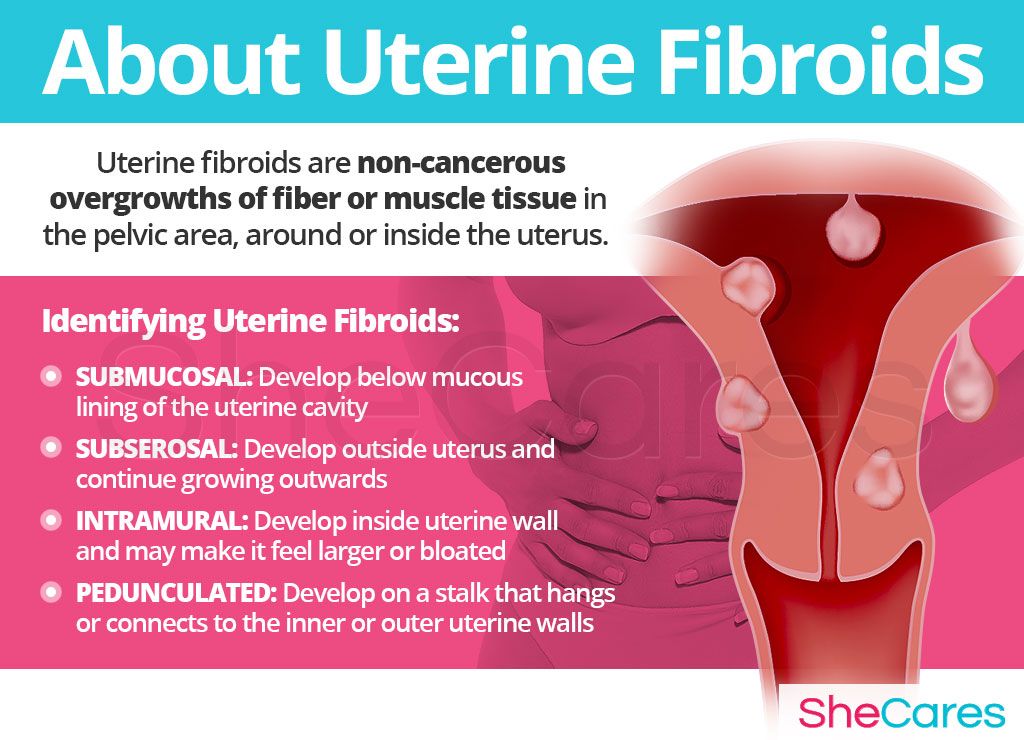 Sex hormones affect the menstrual cycle: without them, the maturation of the follicle in the ovary, ovulation, and even menstruation are impossible.
Sex hormones affect the menstrual cycle: without them, the maturation of the follicle in the ovary, ovulation, and even menstruation are impossible.
After 45-50 years, when the ovaries stop working, they no longer ovulate and no longer produce sex hormones. Menstruation also stops due to lack of hormones. This condition is called menopause, or menopause.
During a gynecological examination, the gynecologist cannot see the ovaries, but can feel them as well as the uterus. If you are still a virgin, then the gynecologist can feel the ovaries through the anus, and if you are already sexually active, then through the vagina.
Removal of the uterus. Conversation Without Taboo
Login Registration
UA EN EN
EN
- UA
- EN
- EN
Home About the hospital media center News Uterus removal. Conversation without taboo
- Alla Borisovna, let's discuss a topic that worries many women. But they are simply afraid to ask a doctor about it...
— It seems to me that many women do not ask questions not because they are afraid, but because they are sure that they are well versed in this. Let's take the most well-established myth: "They will remove my uterus - and I will immediately grow old." This is not true. The uterus is a muscular organ whose only purpose is to bear children. During pregnancy, it increases many times in size, and after childbirth it decreases. And this process can be repeated a certain number of times during life. The removal of this organ and the advent of old age are in no way connected. Agree that no one gets old from removing, for example, the phalanx of a finger. The same is with the mother.
- If we talk about the need to remove the uterus, what diseases does it occur in? Is it only oncological diseases or can there be some benign pathologies?
- And so, and so. We remove the uterus for certain malignant neoplasms - when it comes to endometrial cancer, ovarian cancer, uterine sarcoma, and cervical cancer (by the way, we can also perform organ-preserving operations for this disease, but this is a topic for a separate discussion). In fact, all major oncogynecological pathologies involve the removal of the uterus.
In addition, there are other pathologies when a hysterectomy is recommended. Despite the fact that I said that the uterus is a muscular organ, in fact it consists of two components. The first is the muscle layer itself. And the second is the endometrium, the lining of the uterus, which in menstruating women, under the influence of ovarian hormones, grows during the cycle and is rejected during menstruation. So, the pathology can concern both the endometrium and the muscle layer. In menopause, women may develop, for example, endometrial hyperplasia. Normally, it can only be in menstruating women in a certain phase of the cycle. And in menopause, it should not be, so such a problem can be a reason for removing the uterus.
Another indication for surgery is benign tumors, such as fibroids. But it is not always removed, but only in three cases - it hurts, bleeds, grows.
I emphasize: the decision to remove the uterus is made individually in each specific case and must be done jointly by the doctor and the patient. Because from the moment of the first consultation we are one team and we decide everything together. We definitely take into account a lot of indicators, up to what kind of marriage, what reproductive plans, whether the woman is going to give birth again, etc. That is, we discuss life priorities. And based on this, we understand whether it is necessary to carry out the operation or not.
— Sometimes the uterus is removed prophylactically. What diseases can be prevented in this way?
— You know, I always tell my patients that there is such a trend abroad: women who have fulfilled their reproductive function (have given birth to children), have approached the menopausal age (i. e., the ovaries and uterus have already completed their program and completed their life cycle, they are like ballast in the body), go for prophylactic laparoscopic hysterectomy. There are no incisions on the abdomen. Such an operation lasts about 30 minutes, they did it in the morning, and in the evening the patient is already at home. What is achieved by this? This is the prevention of cervical cancer, endometrial cancer, uterine sarcoma, ovarian cancer and tube cancer. In my opinion, it's worth it. That is, if there is no organ (which is no longer functioning), there is no problem. Because all these diseases, as a rule, do not occur in a working organ, but in menopausal women after 50-60 years. In my opinion, prophylactic hysterectomy is quite promising in terms of preventing cancer.
— Is a histological examination of the removed material always performed? If we are talking about preventive removal, is it necessary to perform such a study?
— Needed.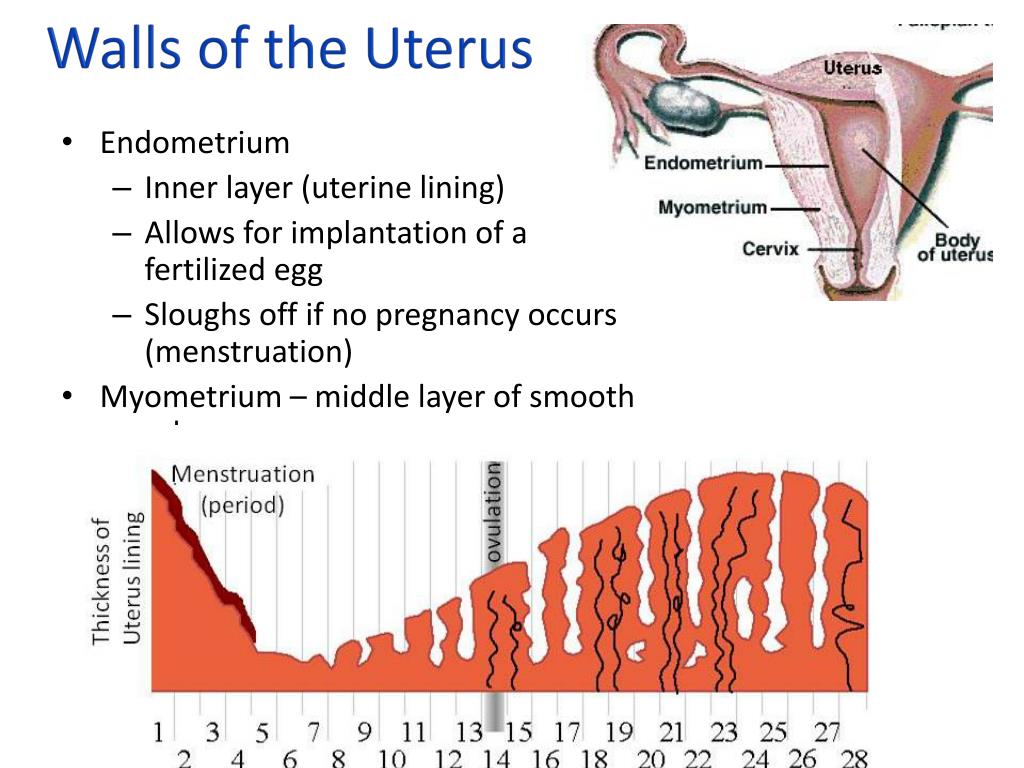 There is an unwritten rule in surgery and oncology: everything that is removed must be examined. We make sure to send the material to the lab to make sure everything is fine and to be sure that we haven't missed anything at the initial stage. Any little thing that has not been given due attention can later “shoot” and cause trouble. The person must be fully armed. He must know everything about himself.
There is an unwritten rule in surgery and oncology: everything that is removed must be examined. We make sure to send the material to the lab to make sure everything is fine and to be sure that we haven't missed anything at the initial stage. Any little thing that has not been given due attention can later “shoot” and cause trouble. The person must be fully armed. He must know everything about himself.
— Is there any special preparation required for this operation?
— No, this is a fairly standard, completely uncomplicated laparoscopic operation, which practically does not pose any danger to the body. Of course, any violation of the integrity of the skin cover, any invasive procedures can lead to some complications. But with a competent approach, they are practically reduced to zero. Therefore, no special preparation is needed.
The best prevention of complications is the qualification of the surgeon, his skills and experience. Now such operations in the open way are practically not performed, they have remained in the last century.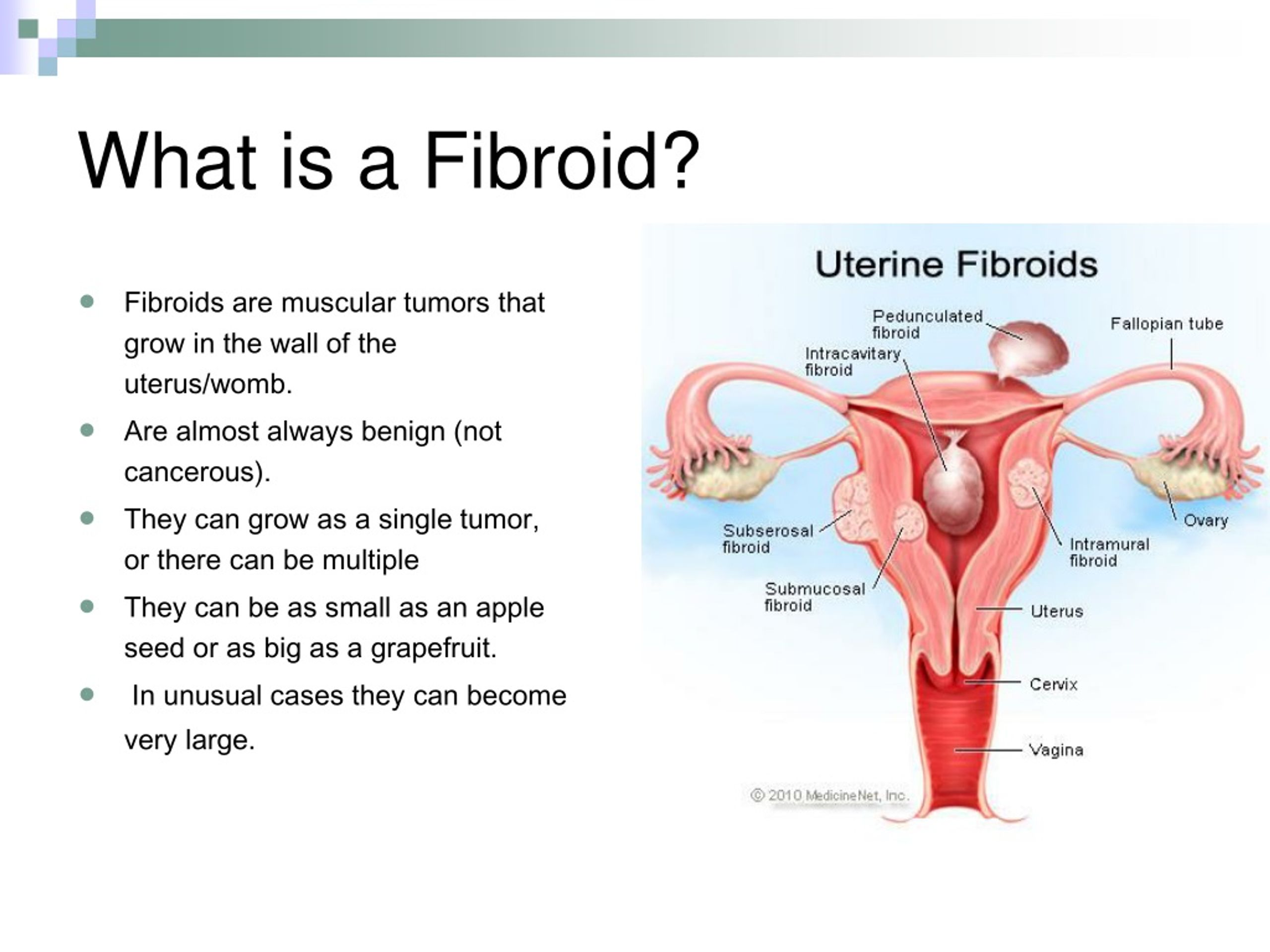 All interventions, even with fairly large benign and malignant tumors, we perform laparoscopically. And this is a worldwide trend.
All interventions, even with fairly large benign and malignant tumors, we perform laparoscopically. And this is a worldwide trend.
Patients are admitted to the hospital either the night before or early in the morning on the day of surgery and can go home the next day. Everything is very simple. This is fast track surgery, i.e. quick recovery surgery.
— And how long can the recovery after the operation last in general? What are the recommendations for patients for this period, which is absolutely impossible?
— Patients usually return to their normal lives within a week, both in terms of work and family. We ask you to refrain from sexual intercourse for about a month after the operation, so that all tissues heal well. This is the only limitation. Of course, I will not even say that we do not recommend unloading wagons with coal or sugar. But within reason, absolutely everything is permissible.
- Probably, many are convinced that after such an operation, in principle, you can put an end to your sexual life .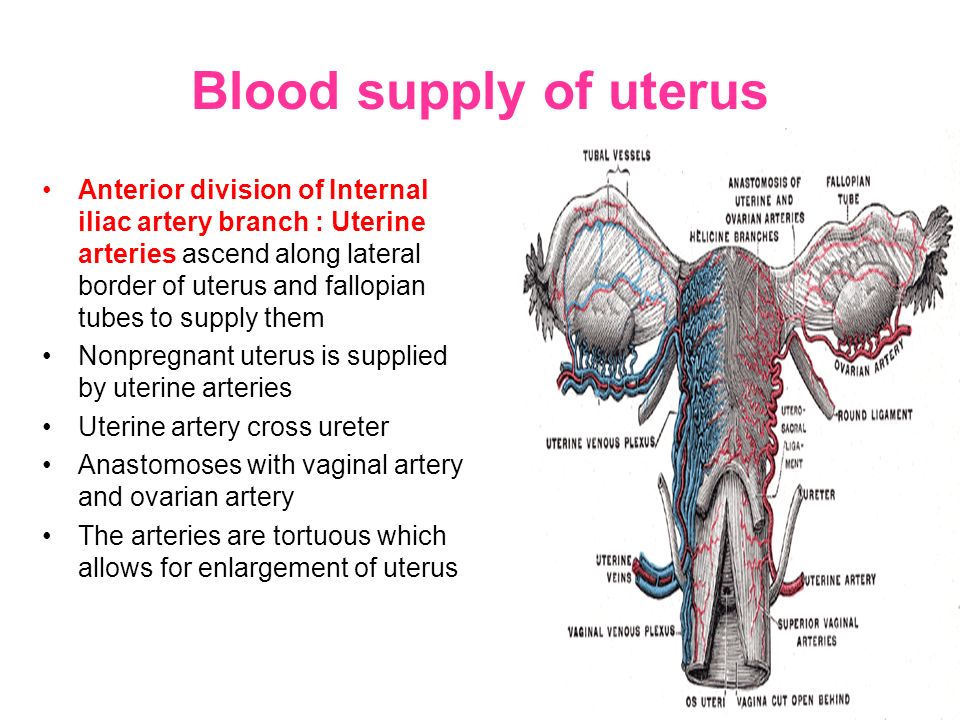 ..
..
- On the contrary! She's getting better. Judge for yourself: the threat of pregnancy is gone, the threat of bleeding is gone. And a woman can completely relax and experience only pleasure.
— Does removal of the uterus lead to menopause?
— Of course not. This is where we started the conversation. Removal of the uterus does not lead to menopause. This results in ovarian failure. That is, when the uterus is removed, and the ovaries remain, the woman does not have menopause. It continues to function exactly the same. All hormonal processes remain unchanged. The only thing missing is menstruation. And the hormonal background does not change in any way.
— And if the uterus is removed along with the ovaries, does surgical menopause occur?
— Only if the woman was in the reproductive period before the operation, that is, she had menstruation. If a woman has already been in menopause, then the removal of the uterus and ovaries, in principle, cannot have any effect.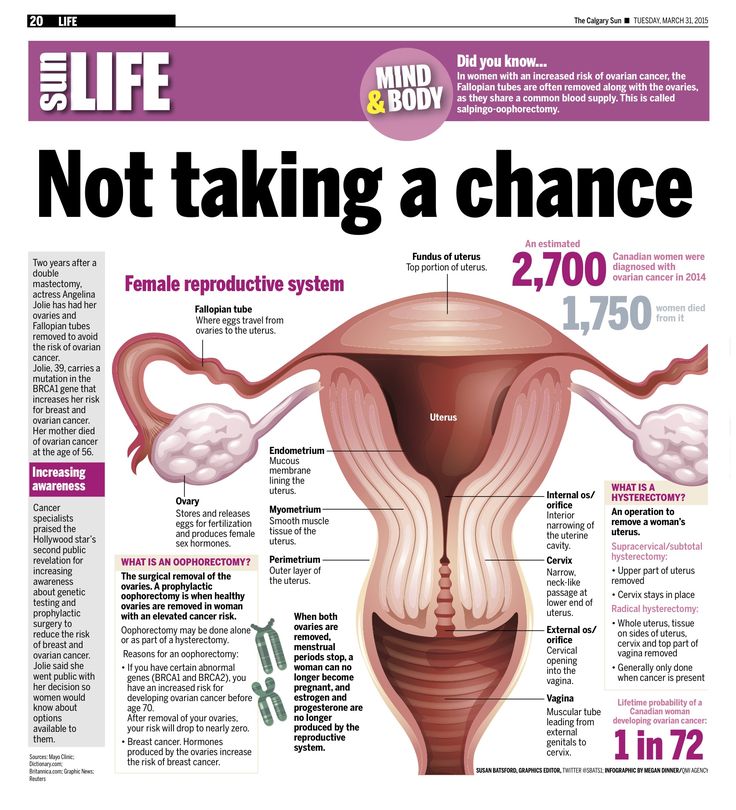
— Do women who go through natural menopause feel different than women who go through surgical menopause?
— Yes, they are slightly different. Still, a woman approaches natural menopause more smoothly. Although here, too, different situations are possible. Sometimes surgical menopause, that is, the abrupt removal of hormone-producing organs, passes quite calmly. Conversely, natural menopause can come with quite severe side effects. We have the opportunity to make adjustments to this process through hormone replacement therapy.
Patients for some reason are terribly afraid of the phrase "hormone therapy", not even understanding what it is about. See, during menstrual life and active ovarian activity, the woman was protected by her natural estrogens, which were produced by the ovaries. And when menopause came, all this disappeared. And doctors, prescribing hormone replacement therapy, help to restore the protection of the female body again. Everything that the body previously received from the ovaries, it receives from one tablet.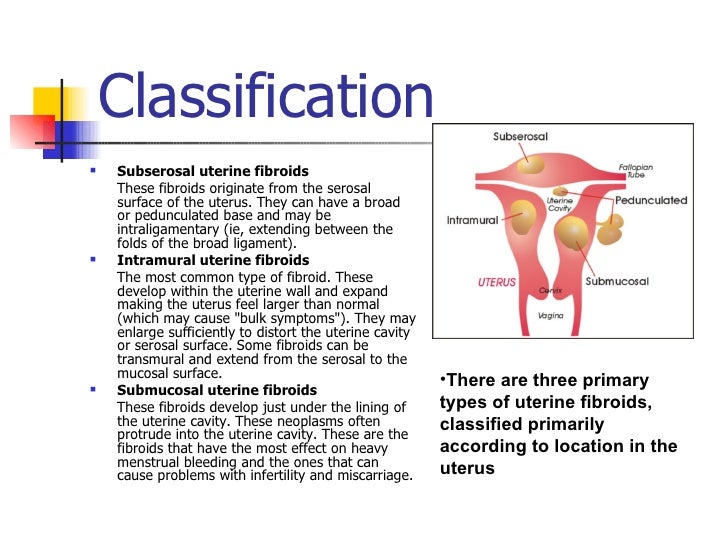 It contains a little estrogen and a little progesterone - and allows you to keep the sparkle in the eyes, excellent hair, skin turgor, good mood. It also prevents cardiovascular disease and osteoporosis. Hormone replacement therapy, as a rule, is prescribed not for a year or two, but maybe even for a decade. In fact, we know how to deal with the manifestations of menopause in any form, in whatever form it comes - surgical or natural.
It contains a little estrogen and a little progesterone - and allows you to keep the sparkle in the eyes, excellent hair, skin turgor, good mood. It also prevents cardiovascular disease and osteoporosis. Hormone replacement therapy, as a rule, is prescribed not for a year or two, but maybe even for a decade. In fact, we know how to deal with the manifestations of menopause in any form, in whatever form it comes - surgical or natural.
If earlier, at the age of 50-60, a woman already had a sunset of her life, she was already a grandmother in her natural form, she felt herself accordingly, now a woman at 50 is energetic and active, she still has almost half of her life ahead of her. She wants to walk in heels, look spectacular. And hormone replacement therapy helps a lot.
— Let's take another look at a situation where a woman, for some personal reason, does not want to let a man know about the details of the surgery...
— I don't think it's always necessary to do this.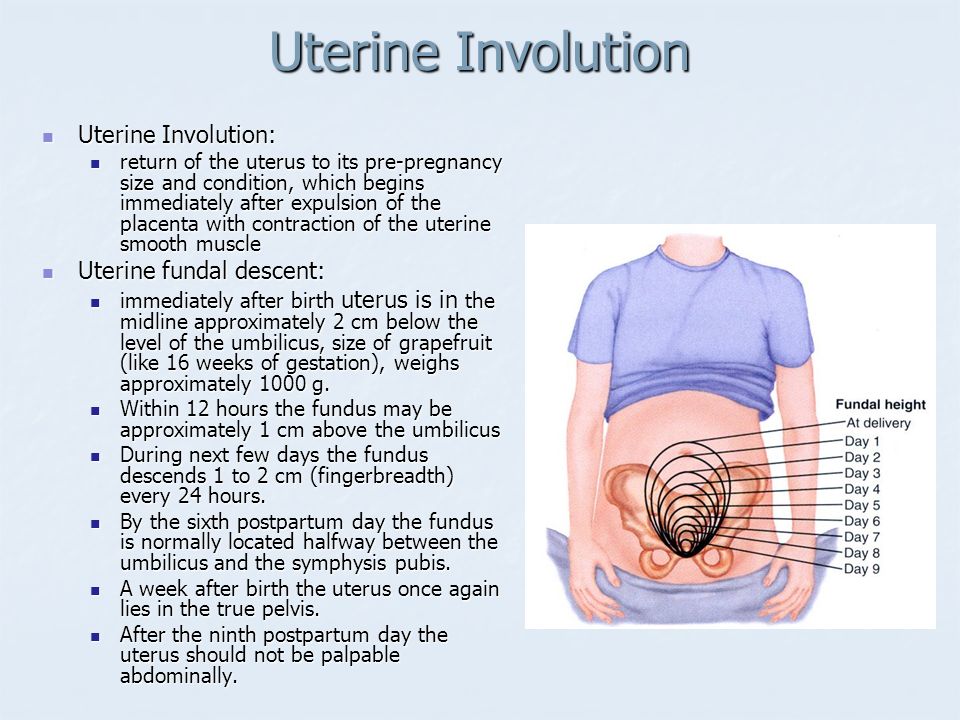 Most partners will not understand anything. Of course, exceptions are possible: a man who knows anatomy well can guess that during intercourse he rests not on the neck, but on the dome of the vagina. But this seems very unlikely to me.
Most partners will not understand anything. Of course, exceptions are possible: a man who knows anatomy well can guess that during intercourse he rests not on the neck, but on the dome of the vagina. But this seems very unlikely to me.
— Do you still need to visit a gynecologist and do a Pap test after a hysterectomy?
- If the uterus is removed along with the cervix, then a Pap test is not necessary. It is performed to detect precancerous conditions of the cervix. And if it is not there, then why take some cytology?
As for visiting a gynecologist, I will answer that it is a must. First, situations are different. We consider both malignant and benign tumors. In malignant tumors, even with high-quality operations and the most modern treatment, there is a risk of relapse. And just visits to the gynecologist allow you to find it in time in case of a relapse. If we are talking about benign processes, then there are no such strict requirements, especially if the ovaries are also removed.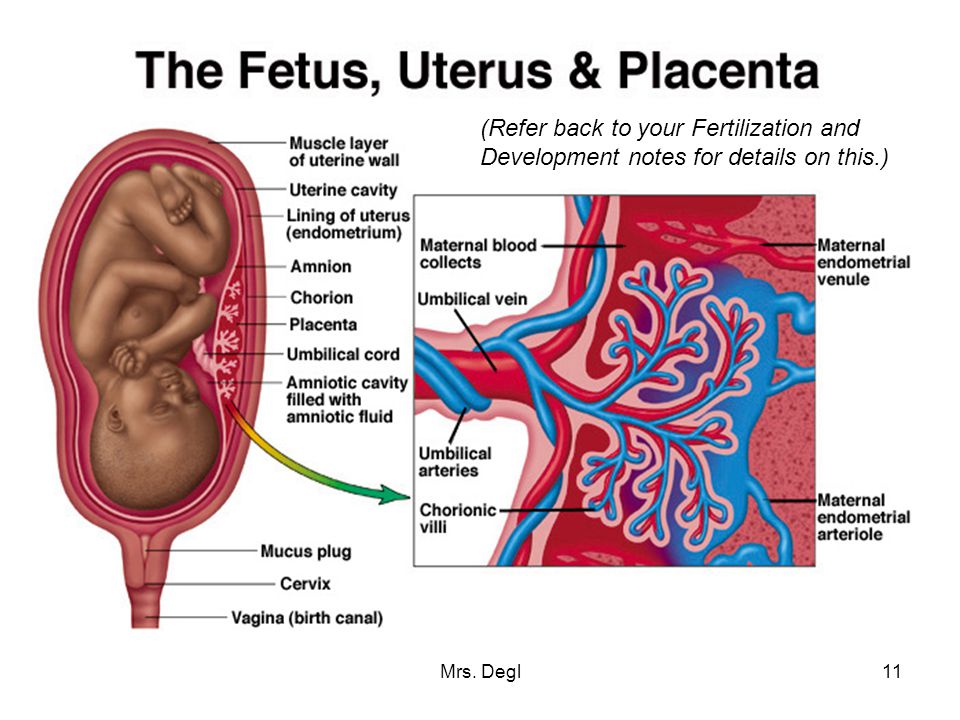 But if the ovaries remain, then, on the contrary, the woman even goes into the risk group for the development of ovarian tumors, because the ovaries are already injured by the operation, their blood supply is disrupted and the woman can, unfortunately, develop a tumor in the future. In this case, a regular annual inspection is required. If both the uterus with the cervix and both ovaries are removed, it is permissible to come for an examination every 2-3 years and do a vaginal ultrasound to make sure that everything is fine.
But if the ovaries remain, then, on the contrary, the woman even goes into the risk group for the development of ovarian tumors, because the ovaries are already injured by the operation, their blood supply is disrupted and the woman can, unfortunately, develop a tumor in the future. In this case, a regular annual inspection is required. If both the uterus with the cervix and both ovaries are removed, it is permissible to come for an examination every 2-3 years and do a vaginal ultrasound to make sure that everything is fine.
Sign up for a consultation:
0-800-500-110 — free of charge within Ukraine;
+38-044-277-8-277.
December 6 MRI in LISOD. How it works
November 21 Cancer with three cons.