What is a molar pregnancy miscarriage
Molar pregnancy - NHS
A molar pregnancy is when there's a problem with a fertilised egg, which means a baby and a placenta do not develop the way they should after conception. A molar pregnancy will not be able to survive.
It happens by chance and is very rare. If you have a molar pregnancy, there is support available to help you.
Finding out you have a molar pregnancy
You may find out during your 1st pregnancy ultrasound scan at around 8 to 14 weeks.
Some people find out after their pregnancy ends with a miscarriage.
Finding out you have a molar pregnancy can be very difficult. A doctor or midwife can give you advice about the support that's available.
Urgent advice: Call a midwife or GP if:
You're pregnant and:
- you have any bleeding or a dark discharge from your vagina
- you're feeling or being sick often (severe morning sickness)
- you think your bump looks bigger than it should for your stage of pregnancy
- you have any other symptoms you're worried about
What happens next
If a midwife or doctor thinks you have a molar pregnancy, you'll need:
- blood tests to check your level of the pregnancy hormone hCG, which is usually higher than normal in a molar pregnancy
- an ultrasound scan
- an appointment with a specialist (gynaecologist) or at an early pregnancy assessment unit
Treatment for a molar pregnancy
A molar pregnancy will not be able to survive.
It may end on its own, with a miscarriage.
If this does not happen, it's usually treated with a procedure to remove the pregnancy.
You'll usually be given a general anaesthetic before the procedure, so you'll be asleep.
Sometimes you might be able to take medicine to end a molar pregnancy.
Follow-up care
After treatment for a molar pregnancy you'll have regular blood and urine tests to check your hCG hormone level is returning to normal.
If your hormone level does not return to normal you will need further treatment.
Sex, contraception, and trying for a baby after a molar pregnancy
You can have sex as soon as you feel ready, but it's important to use contraception while you're getting follow-up care. Talk to a GP about what type of contraception is right for you.
Having a molar pregnancy does not affect your chances of getting pregnant again. But it's important to wait until your doctor tells you it's safe before you start trying for a baby.
Causes of a molar pregnancy
A molar pregnancy happens by chance. It's not caused by either parent doing something wrong.
You may be more likely to have a molar pregnancy if:
- you're a young teenager or older than 45 when you get pregnant
- you've had a molar pregnancy before
- you have an Asian background
Types of molar pregnancy
A molar pregnancy is sometimes called a hydatidiform mole.
There are 2 types of molar pregnancy:
- a complete molar pregnancy – this is where abnormal cells grow in the womb after conception and there's no sign of a baby
- a partial molar pregnancy – this is where there may be early signs of a baby, but it cannot fully develop or survive
Where to get support
It can take time to recover after a molar pregnancy, both physically and emotionally.
The specialists looking after you can give you advice if you need support. They may be able to recommend support services in your area.
They may be able to recommend support services in your area.
You can also get more information and support from:
- Molar Pregnancy Support & Information
- Miscarriage Association
- Tommy's: Molar pregnancy – information and support
- Charing Cross Hospital Trophoblast Disease Service
Page last reviewed: 10 September 2020
Next review due: 10 September 2023
Molar pregnancy - Symptoms and causes
Overview
A molar pregnancy — also known as hydatidiform mole — is a rare complication of pregnancy characterized by the abnormal growth of trophoblasts, the cells that normally develop into the placenta.
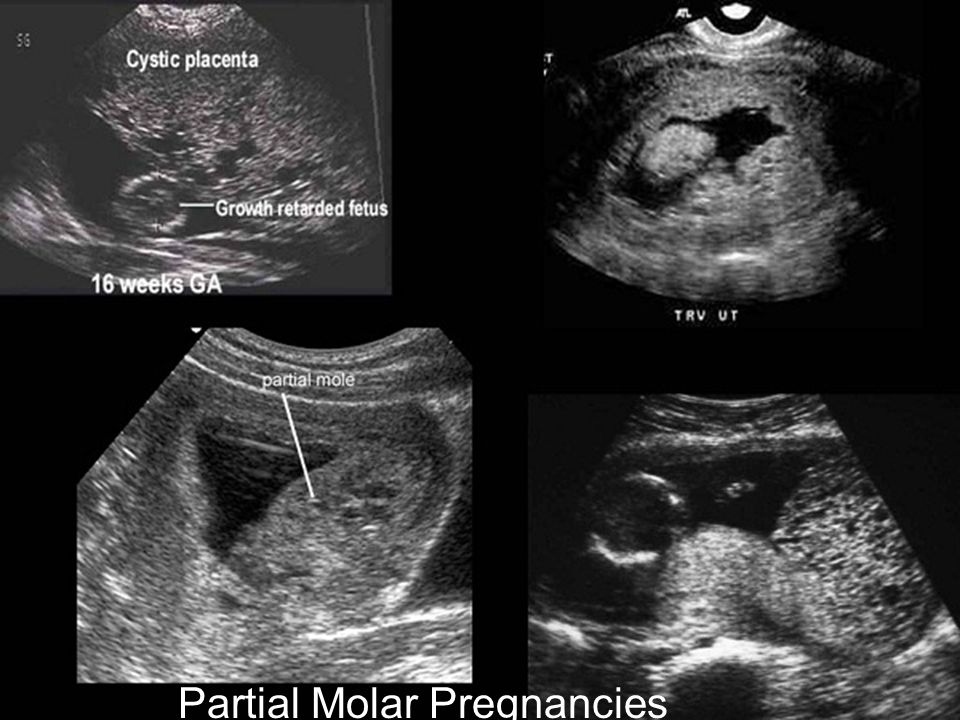
There are two types of molar pregnancy, complete molar pregnancy and partial molar pregnancy. In a complete molar pregnancy, the placental tissue is abnormal and swollen and appears to form fluid-filled cysts. There's also no formation of fetal tissue. In a partial molar pregnancy, there may be normal placental tissue along with abnormally forming placental tissue. There may also be formation of a fetus, but the fetus is not able to survive, and is usually miscarried early in the pregnancy.
There may also be formation of a fetus, but the fetus is not able to survive, and is usually miscarried early in the pregnancy.
A molar pregnancy can have serious complications — including a rare form of cancer — and requires early treatment.
Products & Services
- Book: Your Guide to Miscarriage and Pregnancy Loss
Symptoms
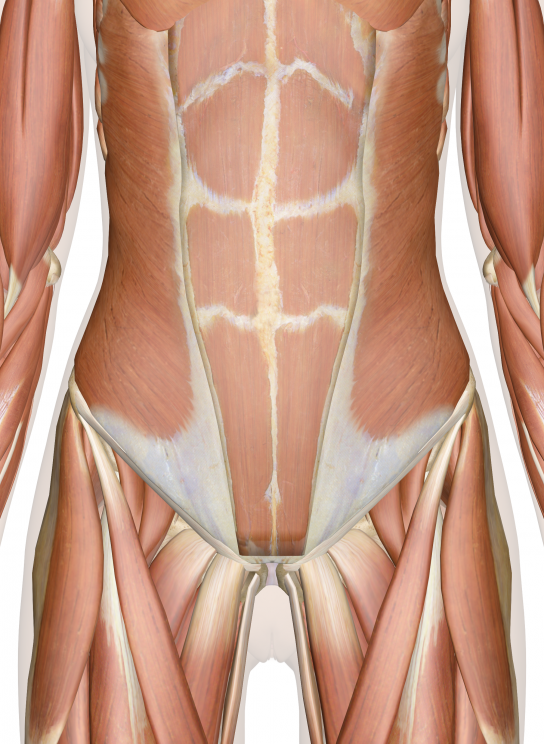
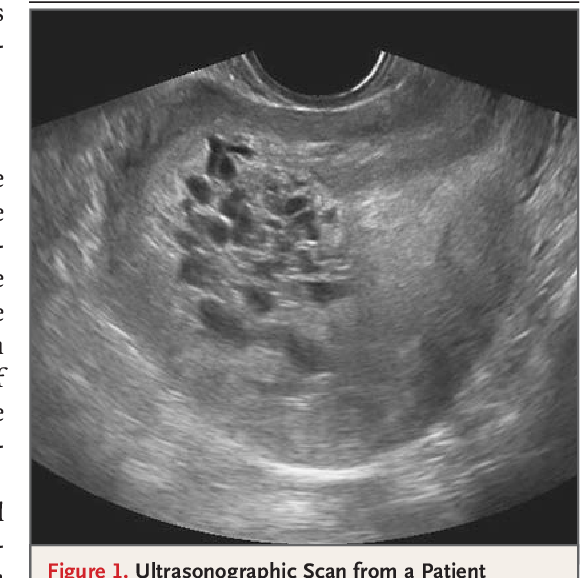
Molar pregnancy
Molar pregnancy
During a molar pregnancy, the placental tissue develops abnormally, and can appear as a mass of cysts. The embryo either doesn't form or is malformed and can't survive.
A molar pregnancy may seem like a normal pregnancy at first, but most molar pregnancies cause specific signs and symptoms, including:
- Dark brown to bright red vaginal bleeding during the first trimester
- Severe nausea and vomiting
- Sometimes vaginal passage of grapelike cysts
- Pelvic pressure or pain
If you experience any signs or symptoms of a molar pregnancy, consult your doctor or pregnancy care provider.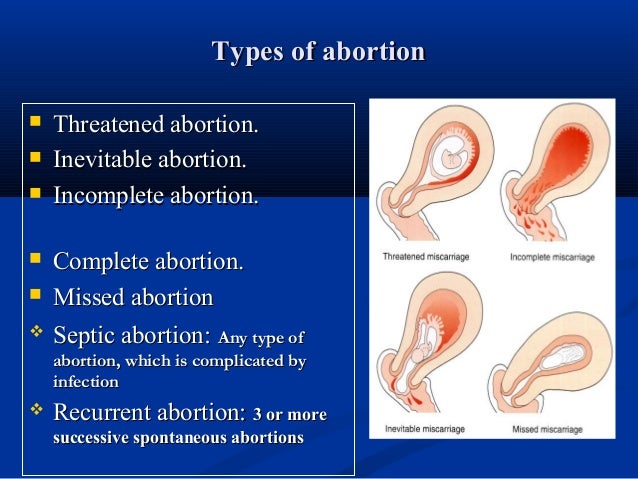 He or she may detect other signs of a molar pregnancy, such as:
He or she may detect other signs of a molar pregnancy, such as:
- Rapid uterine growth — the uterus is too large for the stage of pregnancy
- High blood pressure
- Preeclampsia — a condition that causes high blood pressure and protein in the urine after 20 weeks of pregnancy
- Ovarian cysts
- Anemia
- Overactive thyroid (hyperthyroidism)
Request an Appointment at Mayo Clinic
Causes
A molar pregnancy is caused by an abnormally fertilized egg. Human cells normally contain 23 pairs of chromosomes. One chromosome in each pair comes from the father, the other from the mother.
In a complete molar pregnancy, an empty egg is fertilized by one or two sperm, and all of the genetic material is from the father. In this situation, the chromosomes from the mother's egg are lost or inactivated and the father's chromosomes are duplicated.
In a partial or incomplete molar pregnancy, the mother's chromosomes remain but the father provides two sets of chromosomes.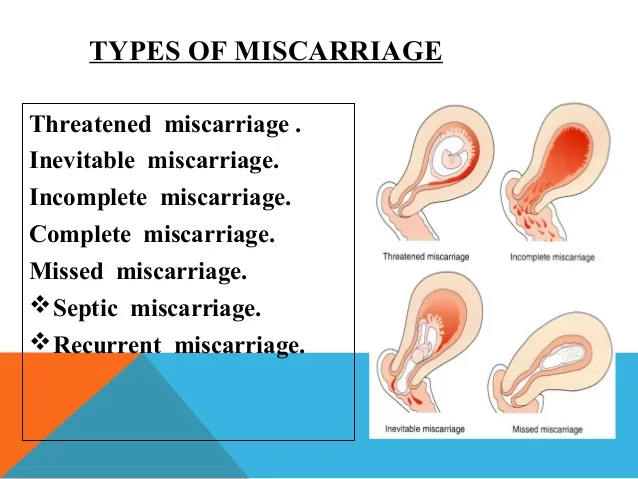 As a result, the embryo has 69 chromosomes instead of 46. This most often occurs when two sperm fertilize an egg, resulting in an extra copy of the father's genetic material.
As a result, the embryo has 69 chromosomes instead of 46. This most often occurs when two sperm fertilize an egg, resulting in an extra copy of the father's genetic material.
Risk factors
Approximately 1 in every 1,000 pregnancies is diagnosed as a molar pregnancy. Various factors are associated with molar pregnancy, including:
- Maternal age. A molar pregnancy is more likely in women older than age 35 or younger than age 20.
- Previous molar pregnancy. If you've had one molar pregnancy, you're more likely to have another. A repeat molar pregnancy happens, on average, in 1 out of every 100 women.
Complications
After a molar pregnancy has been removed, molar tissue may remain and continue to grow. This is called persistent gestational trophoblastic neoplasia (GTN). This occurs in about 15% to 20% of complete molar pregnancies, and up to 5% of partial molar pregnancies.
One sign of persistent GTN is a high level of human chorionic gonadotropin (HCG) — a pregnancy hormone — after the molar pregnancy has been removed. In some cases, an invasive hydatidiform mole penetrates deep into the middle layer of the uterine wall, which causes vaginal bleeding.
In some cases, an invasive hydatidiform mole penetrates deep into the middle layer of the uterine wall, which causes vaginal bleeding.
Persistent GTN can nearly always be successfully treated, most often with chemotherapy. Another treatment option is removal of the uterus (hysterectomy).
Rarely, a cancerous form of GTN known as choriocarcinoma develops and spreads to other organs. Choriocarcinoma is usually successfully treated with multiple cancer drugs. A complete molar pregnancy is more likely to have this complication than a partial molar pregnancy.
Prevention
If you've had a molar pregnancy, talk to your doctor or pregnancy care provider before conceiving again. He or she may recommend waiting for six months to one year before trying to become pregnant. The risk of recurrence is low, but higher than the risk for women with no previous history of molar pregnancy.
During any subsequent pregnancies, your care provider may do early ultrasounds to monitor your condition and offer reassurance of normal development. Your provider may also discuss prenatal genetic testing, which can be used to diagnose a molar pregnancy.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Molar pregnancy - what is it?
Despite the happiness that pregnancy brings to a woman's life, some rare complications can have an adverse effect. The effect is so great that even after a miscarriage, a complication can have a devastating effect on a woman's health. We will be dealing with a rare but serious pregnancy problem that affects approximately 1 in 1000 women.
Molar pregnancy
Molar pregnancy, often referred to as a Hydatidiform Mole, is a rare complication of pregnancy. Molar pregnancy is basically a type of gestational trophoblastic disease that occurs when tissues that, instead of developing normally into a fetus, form abnormal growth. The condition is characterized by an unusual growth of trophoblasts, cells that normally develop and make up the bulk of the placenta during pregnancy.
The condition is characterized by an unusual growth of trophoblasts, cells that normally develop and make up the bulk of the placenta during pregnancy.
Molar pregnancy is a terrible thing, because what grows inside is not an embryo, but a chromosomal anomaly. Pathological tissue must be removed immediately, as this can cause serious complications in some women.
Molar pregnancies
Molar pregnancy usually occurs in the first trimester. This condition affects 1 in 1000 pregnancies worldwide. According to some studies, the recurrence rate is very high in South Asia. In another study on 8,104 pregnant women, 37 were found with molar pregnancies, corresponding to 4.56 per 1,000 births.
Most of the cases identified during the study were in remote areas with low socioeconomic and educational status.
What Causes Molar Pregnancy?
Molar pregnancy is divided into two categories: partial and complete molar pregnancy.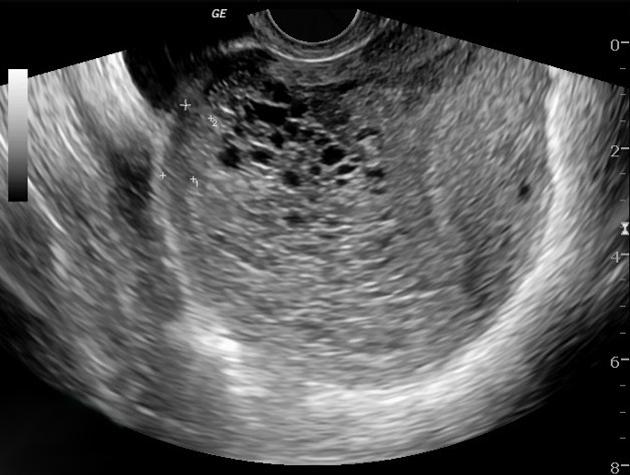 Both occur due to chromosomal abnormalities in the fertilized egg.
Both occur due to chromosomal abnormalities in the fertilized egg.
-
In a partial molar pregnancy, the embryo receives one chromosome from the mother and two from the father. This can result in the embryo having 69 chromosomes instead of the normal 46.
-
In a complete molar pregnancy, the egg has no genetic information. As a result, the fertilized egg does not develop into a fetus. However, it continues to grow as a mass or piece of anomalous tissue.
-
This pathology rarely occurs during pregnancy with twins. In such a case, one fetus will be normal and the other molar.
Signs and symptoms of molar pregnancy
A molar pregnancy usually has the same signs and symptoms as a normal pregnancy, such as morning sickness and no period..... However, it also has its own specific symptoms, which include:
- Vaginal bleeding dark brown and bright red
- Uterus that is larger than usual
- Severe nausea and vomiting
- High blood pressure
- Pressure on the pelvis with pain
- Signs of hyperthyroidism such as nervousness and fatigue or irregular heartbeat.
Many of the above signs can also indicate miscarriages. Therefore, any woman experiencing these symptoms should immediately contact a gynecologist.
Molar pregnancy risk factors
There are several risk factors associated with molar pregnancy. These include:
- Mother's age less than 20 years and over 35 years
- History of molar pregnancies
- History of miscarriage
- Anomalies of the uterus
- Lack of protein, folic acid or carotene in the diet
Molar Pregnancy Diagnosis
Since molar pregnancies mostly occur in the first trimester, they can be detected during a routine examination. Especially, it can be determined when the fetal heartbeat is not detected by 12 weeks. The doctor usually performs a gynecological examination, sends for blood tests to check the level of pregnancy hormones.
However, the diagnosis of molar pregnancy is usually based on ultrasound. An ultrasound, which uses high frequency sound waves to create images of the uterus, can reveal:
An ultrasound, which uses high frequency sound waves to create images of the uterus, can reveal:
- Missing fetus or embryo inside
- Little or no amniotic fluid
- Dense cystic placenta
- Ovarian cysts
Your doctor may also test for preeclampsia, anemia, and hyperthyroidism.
Is molar pregnancy related to cancer?
About 80% of molar pregnancies are benign. However, the tissues of the pregnancy can turn into a cancer called choriocarcinoma, which is a type of gestational trophoblastic disease. This can happen when, after removal of a molar pregnancy, the tissue remains growing.
More than half of choriocarcinoma cases are associated with molar pregnancies. Choriocarcinoma can also occur after an early miscarriage or after an ectopic pregnancy. However, women who develop cancer after a failed pregnancy can be successfully treated.
How is molar pregnancy treated?
If you have a molar pregnancy, be sure it will not lead to a successful delivery. Without delay, the abnormal tissue must be removed in order to prevent serious complications. The main treatment methods are:
Without delay, the abnormal tissue must be removed in order to prevent serious complications. The main treatment methods are:
- Dilatation and curettage is usually an outpatient procedure and you can be discharged from the hospital on the same day. First, you are given a local anesthetic, then the doctor inserts a device called a Speculum into your vagina and dilates your cervix. After that, the inner tissue is removed through vacuum suction.
- Hysterectomy - Some women with molar pregnancies may choose to remove the entire uterus, also known as a hysterectomy. After this operation, these women will not be able to get pregnant again. Therefore, it is important to consult a doctor before this operation, especially if you want children in the future.
There is a small chance that after gestational trophoblastic disease, a molar pregnancy will turn into cancer. But if detected, it can be successfully treated with chemotherapy.
Can a woman with a molar pregnancy become pregnant in the future?
Even if a molar pregnancy turns into a trophoblastic disease or choriocarcinoma, this does not prevent a woman from becoming pregnant in the future.
However, after treatment, she may have to wait up to 12 months before she can become pregnant again. This is to make sure your hCG (human chorionic gonadotropin) hormone levels are back to normal.
Elevated hCG levels (a sign of pregnancy) can be a sign of invasive moles or choriocarcinoma, so waiting 6 months or so will allow your doctor to differentiate between pregnancy and choriocarcinoma.
Molar pregnancy may also recur in the future; the chances of occurrence are 1 in 100. Therefore, if you have just recently been treated for a molar pregnancy, be carefully examined in order to rule out a recurrence.
What is a miscarriage and what to do when it occurs?
Sometimes a pregnancy just ends. We will tell you what the reason may be, and why the risk of repeated miscarriages is lower than we think.
Anastasia Nikiforova
Our author, Daria Andreeva, shared her story of missed pregnancy. One of the most painful aspects of perinatal loss for her was a collision with post-Soviet gynecology: “The doctor returned, examined me, felt something, said that everything was very bad and hospitalization was needed. What exactly was bad, she could not explain. But she said that I would have sepsis and die. I said that I know the signs of sepsis, and right now I definitely don’t have any sepsis and it’s close. And if it starts, I will have time to call an ambulance.
One of the most painful aspects of perinatal loss for her was a collision with post-Soviet gynecology: “The doctor returned, examined me, felt something, said that everything was very bad and hospitalization was needed. What exactly was bad, she could not explain. But she said that I would have sepsis and die. I said that I know the signs of sepsis, and right now I definitely don’t have any sepsis and it’s close. And if it starts, I will have time to call an ambulance.
Then she said that I must have a pathology, and if you don’t find out now what caused this pregnancy to stop, then it will always be like this.
I told her that this is not so, and that, according to statistics, up to 20% of pregnancies freeze, and, as a rule, this happens due to a genetic defect in the fetus, and according to the protocols, it is supposed to look for pathology after several frozen in a row, and not one ( I was very lucky that this was my second pregnancy, and I managed to read several books and figure out what's what). It was an absolutely stupid and pointless conversation, it ended with me signing a waiver of hospitalization and going home to cry.”
It was an absolutely stupid and pointless conversation, it ended with me signing a waiver of hospitalization and going home to cry.”
We decided to find out if “cleansing” is really a prerequisite for miscarriage therapy, and how it is treated in the framework of evidence-based medicine.
What is a miscarriage?
A miscarriage (or perinatal loss) is a spontaneous termination of pregnancy that results in the loss of a fetus before 20 weeks of gestation. This usually happens during the first trimester. Miscarriages can occur for a variety of medical reasons, many of which cannot be controlled at all costs. But knowing the risk factors, signs, and causes can help you understand what happened and get the support or treatment you need.
What are the signs of a miscarriage?
The symptoms of a miscarriage vary depending on the duration. In some cases, this happens so quickly that the woman may not even know she was pregnant.
Here are some of the signs of a miscarriage:
- severe spotting;
- vaginal bleeding;
- discharge of tissue or fluid from the vagina;
- severe abdominal pain or cramps, as at the onset of menstruation;
- back pain, mild to severe.
If you experience any of these symptoms while pregnant, contact your doctor immediately. They do not necessarily mean the beginning of a spontaneous interruption, but it is better to be safe and get examined by a gynecologist.
Other less common symptoms:
- diarrhea;
- nausea;
- inexplicable weakness;
- disappearance of pregnancy symptoms such as breast tenderness or morning sickness.
Why do miscarriages happen?
Although some factors may increase the risk of miscarriage, it usually occurs regardless of the woman's actions. Most spontaneous abortions in the first trimester of pregnancy occur due to a violation of the normal development of the fetus. Here's what could be the reasons for this:
Most spontaneous abortions in the first trimester of pregnancy occur due to a violation of the normal development of the fetus. Here's what could be the reasons for this:
Genetic or chromosomal problems
At fertilization, two genetic sets "meet" - from the mother's egg and the father's sperm, 23 chromosomes each. The zygote begins to divide again and again, gradually forming an embryo. Each of us is supposed to have 46 complete chromosomes. If something goes wrong during cell division, the chromosome may be missing or repeated. About 50% of all first trimester miscarriages are due to chromosomal abnormalities. The risk of this increases somewhat after age 35.
Examples of these chromosomal abnormalities:
- Intrauterine fetal death (or “missed pregnancy”): An embryo forms but stops developing before signs of miscarriage appear.
- Anembryonic pregnancy: the egg is implanted in the uterus, but the embryo does not develop in it (another name for this is "empty ovum syndrome").
- Molar pregnancy: both sets of chromosomes are from the father and no fetal development occurs. There is also a partial molar pregnancy, when, with a double set from the father, there are still chromosomes from the mother, but they are unsuitable for development.
Sometimes there are random cell division errors or egg/sperm damage. Problems with the placenta can also lead to miscarriage.
Infections
Infections can be dangerous for a developing baby and lead to miscarriage. Here are some of them:
- Listeria
- Parvovirus (B19)
- Toxoplasma
- Rubella virus
- Herpes simplex virus
- Cytomegalovirus
Blood clotting disorders
These are conditions that cause our bodies to form more blood clots than usual (such as lupus anticoagulant and antiphospholipid syndrome).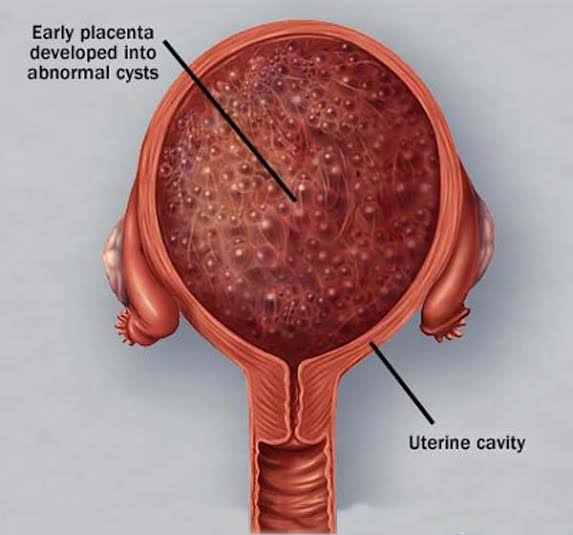 If pregnancy occurs against the background of these conditions, blood clots may form in the placenta, which disrupts metabolic processes and oxygen supply.
If pregnancy occurs against the background of these conditions, blood clots may form in the placenta, which disrupts metabolic processes and oxygen supply.
Maternal health, habits and lifestyle
Various health conditions and habits can also interfere with the development of the fetus. However, it is important to remember: exercise and sex life do not lead to miscarriages! As well as work - unless, of course, the woman is exposed to harmful chemicals or radiation.
- Poor nutrition or malnutrition
- Drug and alcohol use
- Advanced maternal age
- Thyroid disease without drug compensation
- Hormone problems
- Uncontrolled diabetes
- injury
- Obesity
- Problems with cervix
- Anomalous form of the uterus
- Very high blood pressure
- Food poisoning
- Take some drugs (therefore it is very important to clarify the doctor, is the drug is safe during pregnancy)
Is it possible to carry a pregnancy normally after a miscarriage?
The topic of perinatal loss is rarely discussed publicly, so it may seem to us that they occur rarely and are the result of a serious pathology. This is not so - statistically, miscarriages are very common (according to various sources, 10-20% of conceptions end with them). It is difficult to give exact numbers, because many women do not even notice the onset and loss of pregnancy in the very early stages.
This is not so - statistically, miscarriages are very common (according to various sources, 10-20% of conceptions end with them). It is difficult to give exact numbers, because many women do not even notice the onset and loss of pregnancy in the very early stages.
Do not think that a single miscarriage dooms a woman to a second abortion, it is not. The likelihood of recurring perinatal losses (at least 2 or 3) is very low, only 1% of women experience them.
Accordingly, the vast majority of mothers safely carry further pregnancies after a miscarriage. Studies also show that if the first pregnancy is successful, then the risk of loss during a second one will be lower. On the other hand, repeated spontaneous interruptions indicate an increased risk of miscarriage in the future (since they indicate the presence of relevant medical causes in the body in the mother). Within the framework of evidence-based medicine, gynecologists are recommended to start searching for the cause of miscarriage after two or three perinatal losses.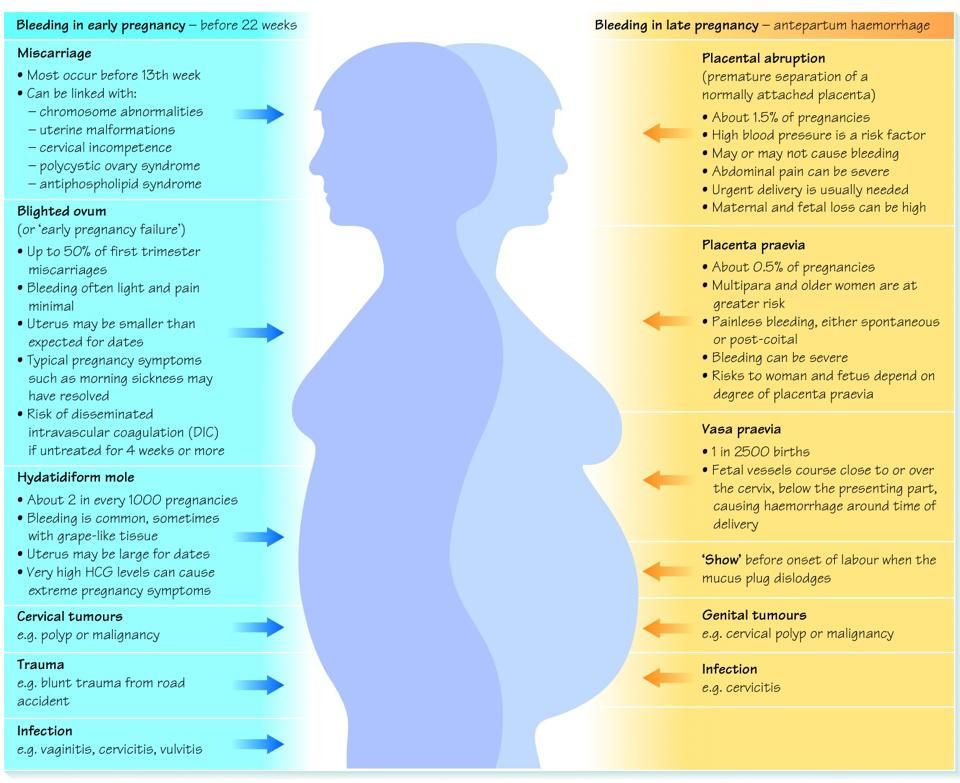
How can you tell a normal period from a miscarriage?
As we have already said, in many cases a miscarriage can occur even before a woman knows she was pregnant, and its symptoms are very similar to normal menstruation. Here are some factors that may indicate an interruption is in progress:
- Symptoms: Severe (or worsening) pain in the back or abdomen, accompanied by bleeding and large blood clots, may indicate a miscarriage.
- Timing: Termination very early in pregnancy may be mistaken for menstruation. However, this is less likely after eight weeks.
- Duration of symptoms: signs of miscarriage usually become more severe and last longer than menstruation.
If you are bleeding heavily or if you suspect a spontaneous interruption, you should see your doctor.
At what time of pregnancy is the risk of miscarriage higher?
About 80% of miscarriages occur in the first trimester of pregnancy (up to 13 weeks), then the frequency decreases sharply.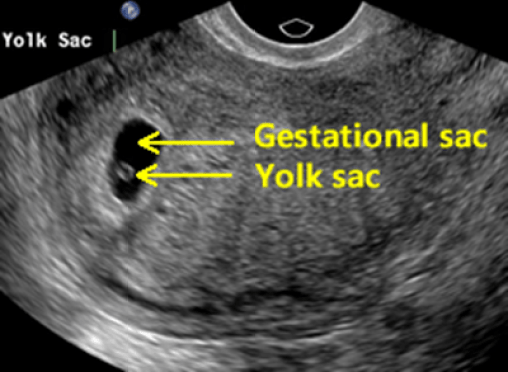
From the first to the sixth week
The first two weeks have the highest risk of miscarriage (many of which women may not be aware of, suggesting a failure in the menstrual cycle) and, decreasing slightly, persists until the sixth week.
Seventh to twelfth weeks
Once a confirmed viable pregnancy reaches six weeks, the risk of miscarriage drops to 10% and gradually decreases as the embryo grows.
Thirteenth to twentieth weeks
By week 12, the risk may be reduced to 5%. But keep in mind that this number will not drop to zero due to the likelihood of pregnancy complications
How common are miscarriages?
According to the American College of Obstetricians and Gynecologists, spontaneous abortion occurs in 10% of known pregnancies. Sometimes the cause of a miscarriage remains unknown. However, according to experts, about 50% of miscarriages are due to chromosomal problems. The risk of miscarriage definitely increases with age. At 35, it is 20%, and by forty it reaches 40%, increasing in proportion to age.
However, according to experts, about 50% of miscarriages are due to chromosomal problems. The risk of miscarriage definitely increases with age. At 35, it is 20%, and by forty it reaches 40%, increasing in proportion to age.
What is a miscarriage like?
There are many different types of miscarriages. Depending on the symptoms and stage of the pregnancy, the doctor may diagnose one of the following conditions:
- Complete miscarriage: all pregnancy tissue has left the uterine cavity.
- Incomplete miscarriage: some tissue or placental material still remains in the uterine cavity.
- Missed miscarriage: the pregnancy has stopped, but there are no obvious symptoms yet.
- Threatened miscarriage: bleeding and convulsions indicate a possible impending miscarriage.
- Inevitable miscarriage: The presence of bleeding, spasms and dilation of the cervix indicates that a miscarriage is imminent.

- Septic miscarriage: termination of pregnancy accompanied by infection in the uterine cavity.
How to reduce the risk of miscarriage?
Not all interrupts can be prevented. However, here are a few suggestions that can help reduce the risk somewhat:
- Visit your doctor and take care of yourself throughout your pregnancy.
- Avoid smoking, alcohol and drugs during pregnancy.
- Maintain a healthy weight before and during pregnancy.
- Avoid infection. Wash your hands thoroughly and keep your distance from people who are sick
- Limit your caffeine intake to 200 mg per day (one to two cups depending on the strength of the drink)
- Take prenatal vitamins to ensure you and your developing baby get enough nutrients.
- Make sure your diet is healthy, balanced and varied, with plenty of fruits and vegetables.
How do twin miscarriages happen?
Twins develop when two eggs are fertilized instead of one, or when an egg is separated into two separate embryos. Multiple pregnancies usually carry an increased risk of complications such as preterm birth, preeclampsia, or miscarriage.
Multiple pregnancies usually carry an increased risk of complications such as preterm birth, preeclampsia, or miscarriage.
When carrying twins, a type of loss called "vanished twin syndrome" can occur - in many cases one of the embryos is reabsorbed in the placenta. Sometimes it happens so early that the woman doesn't even know she was pregnant with twins.
What should I do if I have a miscarriage?
This will depend on the type of interruption - if the miscarriage was complete, no treatment is required. In cases where tissue remains in the uterine cavity, several options are possible:
- Waiting: the woman is waiting for the remaining tissue to naturally leave her body.
- Taking special medications to help complete the interruption
- Surgery (more commonly referred to as a “cleansing” in our country) during which the doctor will remove any remaining tissue.

The risk of complications from any of these treatment options is very low, so the choice should be made by the woman with a trusted gynecologist.
How to recover after a miscarriage?
Recovery will depend on how long the perinatal loss occurred. For some time, symptoms may appear - bloody discharge and discomfort in the abdomen. The menstrual cycle usually returns after 4-6 weeks, although pregnancy hormones may remain in the blood for several months. After a miscarriage, you should avoid vaginal sex and the use of sanitary tampons for two weeks.
How to deal with perinatal loss?
It's normal to experience all kinds of feelings after a miscarriage. A woman may experience sleep disturbances, low energy levels, frequent tears. After a perinatal loss, each person can grieve for as long as she (or he) needs to. Don't be afraid to ask for support when you need it.