What is a congenital malformation
Congenital anomalies
Congenital anomalies- All topics »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Resources »
- Fact sheets
- Facts in pictures
- Multimedia
- Publications
- Questions & answers
- Tools and toolkits
- Popular »
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Monkeypox
- All countries »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Regions »
- Africa
- Americas
- South-East Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- WHO in countries »
- Statistics
- Cooperation strategies
- Ukraine emergency
- All news »
- News releases
- Statements
- Campaigns
- Commentaries
- Events
- Feature stories
- Speeches
- Spotlights
- Newsletters
- Photo library
- Media distribution list
- Headlines »
- Focus on »
- Afghanistan crisis
- COVID-19 pandemic
- Northern Ethiopia crisis
- Syria crisis
- Ukraine emergency
- Monkeypox outbreak
- Greater Horn of Africa crisis
- Latest »
- Disease Outbreak News
- Travel advice
- Situation reports
- Weekly Epidemiological Record
- WHO in emergencies »
- Surveillance
- Research
- Funding
- Partners
- Operations
- Independent Oversight and Advisory Committee
- Data at WHO »
- Global Health Estimates
- Health SDGs
- Mortality Database
- Data collections
- Dashboards »
- COVID-19 Dashboard
- Triple Billion Dashboard
- Health Inequality Monitor
- Highlights »
- Global Health Observatory
- SCORE
- Insights and visualizations
- Data collection tools
- Reports »
- World Health Statistics 2022
- COVID excess deaths
- DDI IN FOCUS: 2022
- About WHO »
- People
- Teams
- Structure
- Partnerships and collaboration
- Collaborating centres
- Networks, committees and advisory groups
- Transformation
- Our Work »
- General Programme of Work
- WHO Academy
- Activities
- Initiatives
- Funding »
- Investment case
- WHO Foundation
- Accountability »
- Audit
- Budget
- Financial statements
- Programme Budget Portal
- Results Report
- Governance »
- World Health Assembly
- Executive Board
- Election of Director-General
- Governing Bodies website
- Home/
- Health topics/
- Congenital anomalies
UNICEF/Noorani
Newborn baby in Timor-Leste
© Credits
Fact sheets
Questions and answers
Guidelines
Databases and tools
Resolutions and decisions
Technical work
- Newborn Health Unit
- Maternal, Newborn, Child and Adolescent Health and Ageing
- Nutrition and Food Safety
- Sensory Functions, Disability and Rehabilitation
- Sexual and Reproductive Health
Our work
News
All →Publications
All →A wide range of causes of congenital anomalies means that a portfolio of prevention approaches is needed including prevention of sexually transmitted infections,. ..
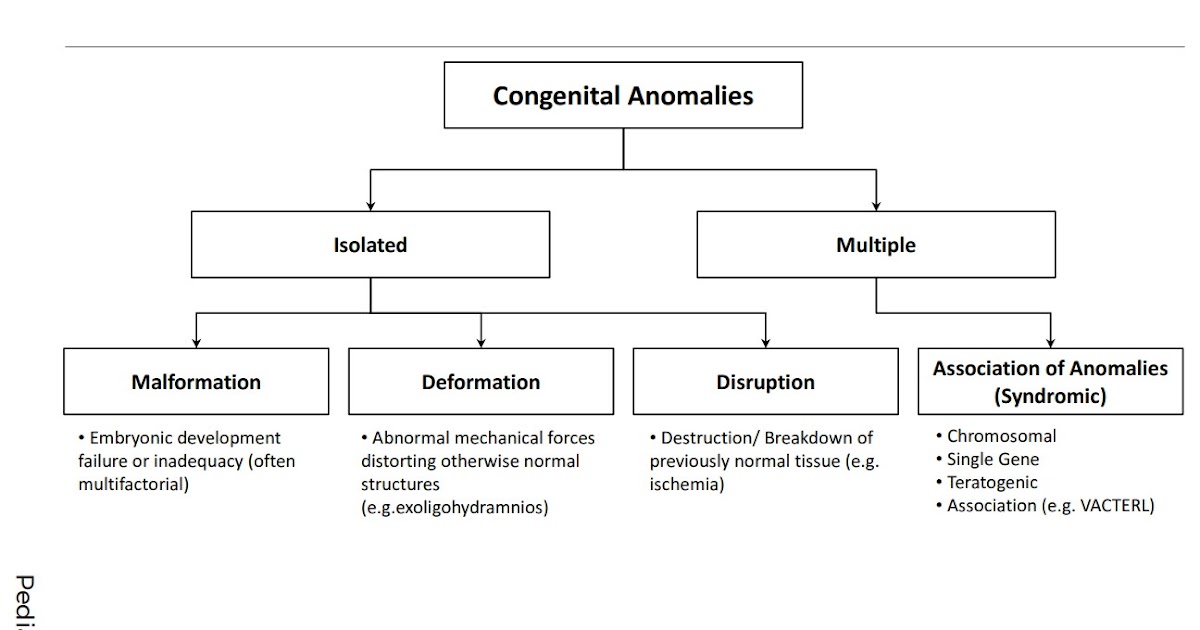
Congenital anomalies, also known as birth defects, are structural or functional abnormalities, including metabolic disorders, that are present from birth....
Survive and thrive: transforming care for every small and sick newborn maps out a pathway towards 2030. It is built upon epidemiology, historical trends,...
Feature stories
Related health topics
Birth defects
Birth defects- All topics »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Resources »
- Fact sheets
- Facts in pictures
- Multimedia
- Publications
- Questions & answers
- Tools and toolkits
- Popular »
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Monkeypox
- All countries »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Regions »
- Africa
- Americas
- South-East Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- WHO in countries »
- Statistics
- Cooperation strategies
- Ukraine emergency
- All news »
- News releases
- Statements
- Campaigns
- Commentaries
- Events
- Feature stories
- Speeches
- Spotlights
- Newsletters
- Photo library
- Media distribution list
- Headlines »
- Focus on »
- Afghanistan crisis
- COVID-19 pandemic
- Northern Ethiopia crisis
- Syria crisis
- Ukraine emergency
- Monkeypox outbreak
- Greater Horn of Africa crisis
- Latest »
- Disease Outbreak News
- Travel advice
- Situation reports
- Weekly Epidemiological Record
- WHO in emergencies »
- Surveillance
- Research
- Funding
- Partners
- Operations
- Independent Oversight and Advisory Committee
- Data at WHO »
- Global Health Estimates
- Health SDGs
- Mortality Database
- Data collections
- Dashboards »
- COVID-19 Dashboard
- Triple Billion Dashboard
- Health Inequality Monitor
- Highlights »
- Global Health Observatory
- SCORE
- Insights and visualizations
- Data collection tools
- Reports »
- World Health Statistics 2022
- COVID excess deaths
- DDI IN FOCUS: 2022
- About WHO »
- People
- Teams
- Structure
- Partnerships and collaboration
- Collaborating centres
- Networks, committees and advisory groups
- Transformation
- Our Work »
- General Programme of Work
- WHO Academy
- Activities
- Initiatives
- Funding »
- Investment case
- WHO Foundation
- Accountability »
- Audit
- Budget
- Financial statements
- Programme Budget Portal
- Results Report
- Governance »
- World Health Assembly
- Executive Board
- Election of Director-General
- Governing Bodies website
- Home/
- Newsroom/
- Fact sheets/
- Detail/
- Birth defects
Causes and risk factors
Genetic
A minority of birth defects are caused by genetic abnormalities i.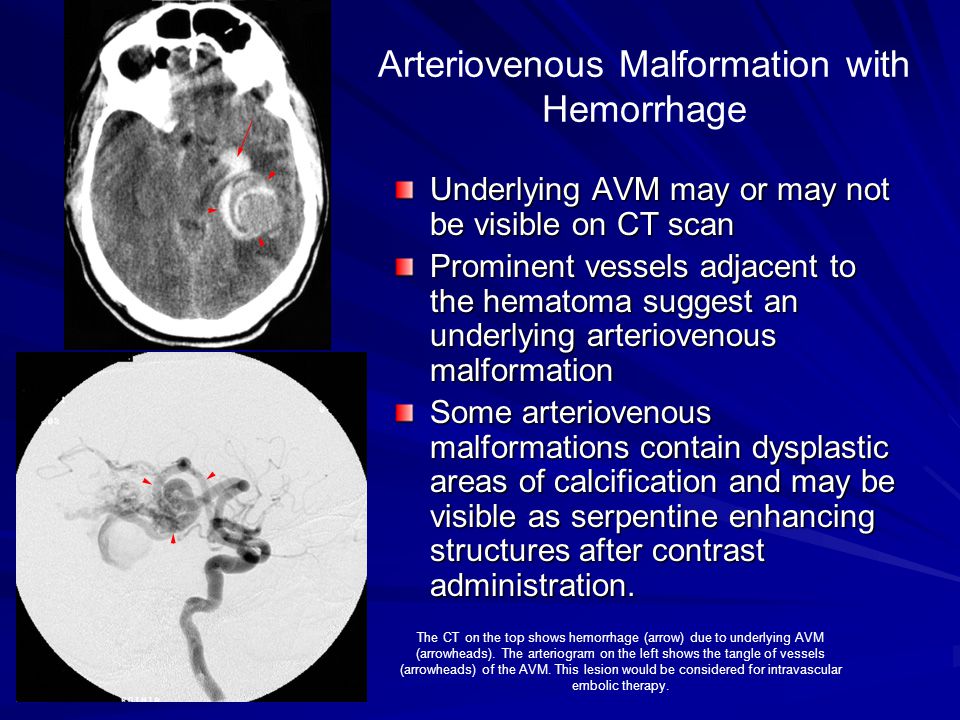 e. chromosomal abnormalities (for example Down syndrome or trisomy 21) or single gene defects (for example cystic fibrosis).
e. chromosomal abnormalities (for example Down syndrome or trisomy 21) or single gene defects (for example cystic fibrosis).
Consanguinity (when parents are related by blood) also increases the prevalence of rare genetic birth defects and nearly doubles the risk for neonatal and childhood death, intellectual disability and other anomalies.
Socioeconomic and demographic factors
Low-income may be an indirect determinant of birth defects, with a higher frequency among resource-constrained families and countries. It is estimated that about 94% of severe birth defects occur in low- and middle-income countries. An indirect determinant,\r\n this higher risk relates to a possible lack of access to sufficient nutritious foods by pregnant women, an increased exposure to agents or factors such as infection and alcohol, or poorer access to health care and screening.
Maternal age is also a risk factor for abnormal intrauterine fetal development. Advanced maternal age increases the risk of chromosomal abnormalities, including Down syndrome.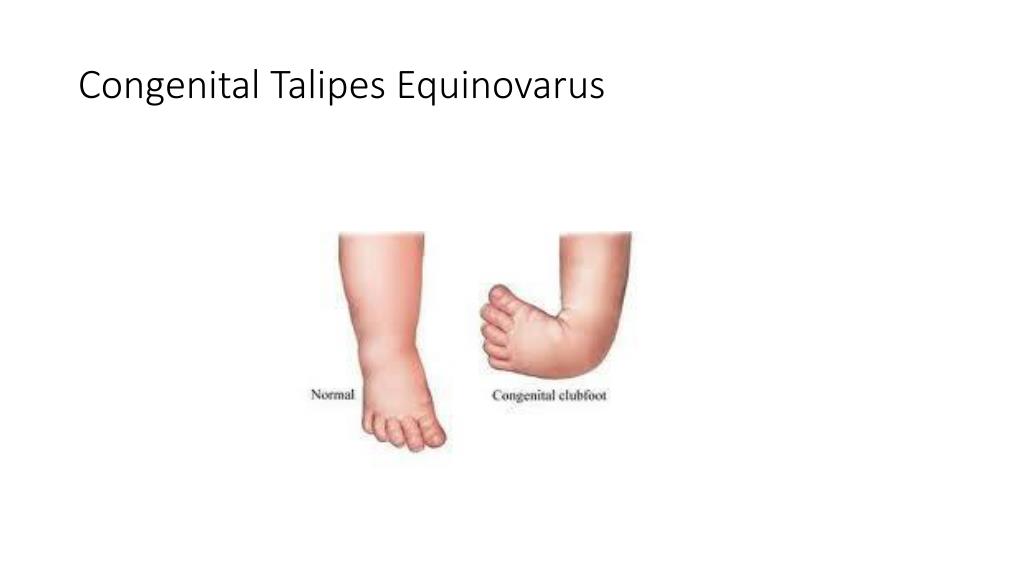
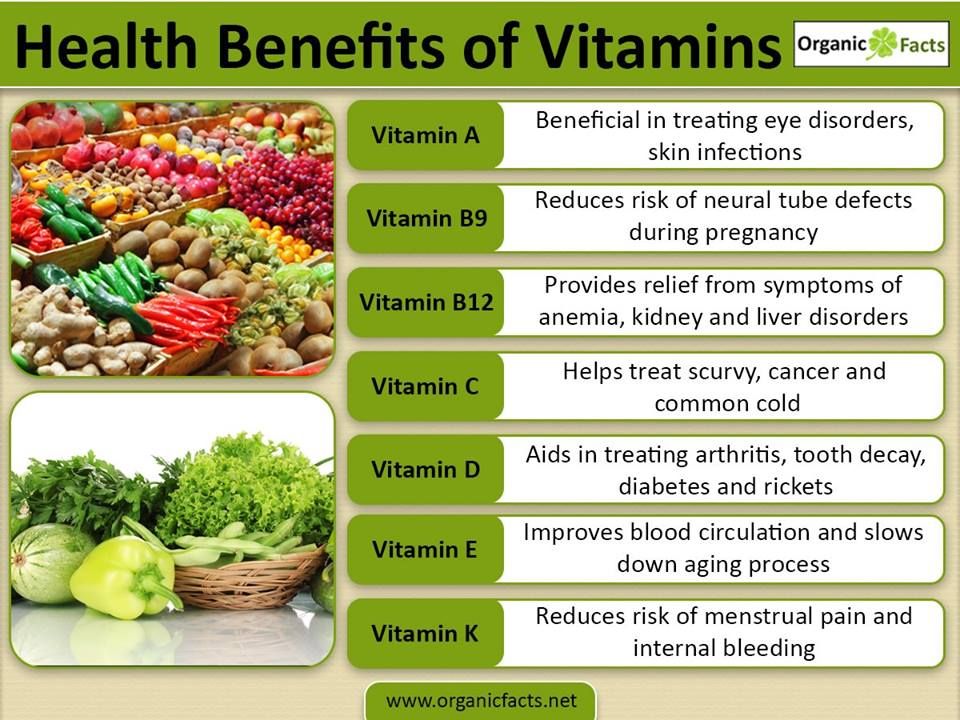
Environmental factors including infections
Others occur because of environmental factors like maternal infections (syphilis, rubella, Zika), exposure to radiation, certain pollutants, maternal nutritional deficiencies (e.g., iodine, folate deficiency), illness (maternal diabetes) or certain drugs\r\n (alcohol, phenytoin).
Unknown causes
While complex genetic and environmental interactions are proposed, most birth defects have unknown causes, including congenital heart defects, cleft lip or palate and club foot.
Prevention
Preventive public health measures work to decrease the frequency of certain birth defects through the removal of risk factors or the reinforcement of protective factors. Important interventions and efforts include:
- ensuring adolescent girls and mothers have a healthy diet including a wide variety of vegetables and fruit, and maintain a healthy weight;
- ensuring an adequate dietary intake of vitamins and minerals, particularly folic acid in adolescent girls and mothers;
- ensuring mothers avoid harmful substances, particularly alcohol and tobacco;
- avoidance of travel by pregnant women (and sometimes women of child-bearing age) to regions experiencing outbreaks of infections known to be associated with birth defects;
- reducing or eliminating environmental exposure to hazardous substances (such as heavy metals or pesticides) during pregnancy;
- controlling diabetes prior to and during pregnancy through counselling, weight management, diet and administration of insulin when required;
- ensuring that any exposure of pregnant women to medications or medical radiation (such as imaging rays) is justified and based on careful health risk–benefit analysis;
- vaccination, especially against the rubella virus, for children and women;
- increasing and strengthening education of health staff and others involved in promoting prevention of congenital anomalies; and
- screening for infections, especially rubella, varicella and syphilis, and consideration of treatment.

Screening, treatment and care
Screening
Health care before and near conception (preconception and peri-conception) includes basic reproductive health practices, as well as medical genetic screening and counselling. Screening can be conducted during the 3 periods listed:
- Preconception screening:
This can be useful to identify those at risk of specific disorders or of passing a disorder onto their children. Screening includes obtaining family histories and carrier screening and is particularly valuable in countries where consanguineous marriage\r\n is common.
- Peri-conception screening:
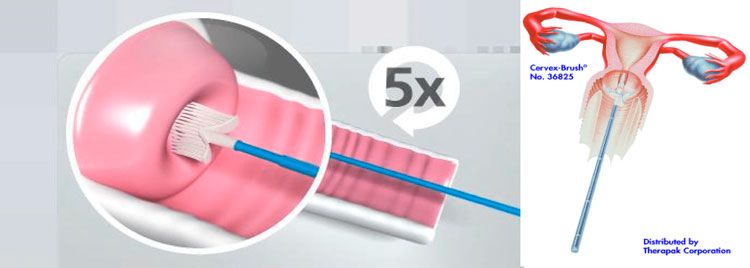
Maternal characteristics may increase risk, and screening results should be used to offer appropriate care, according to risk. This may include screening for young or advanced maternal age, as well as screening for use of alcohol, tobacco or other risks.\r\n Ultrasound can be used to screen for Down syndrome and major structural abnormalities during the first trimester, and for severe fetal anomalies during the second trimester.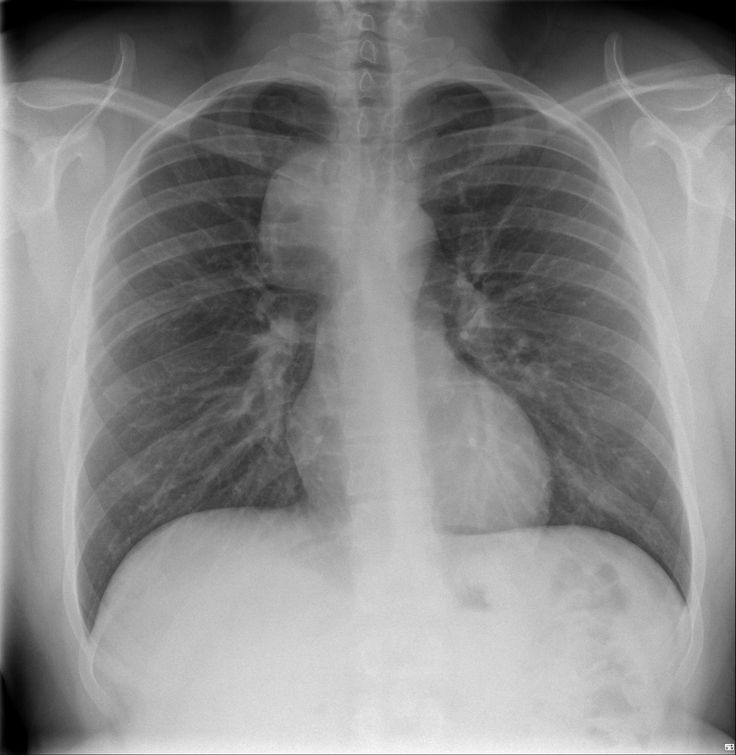 Maternal blood can be screened for placental markers to aid in prediction\r\n of risk of chromosomal abnormalities or neural tube defects, or for free fetal DNA to screen for many chromosomal abnormalities. Diagnostic tests such as chorionic villus sampling and amniocentesis can be used to diagnose chromosomal abnormalities\r\n and infections in women at high risk.
Maternal blood can be screened for placental markers to aid in prediction\r\n of risk of chromosomal abnormalities or neural tube defects, or for free fetal DNA to screen for many chromosomal abnormalities. Diagnostic tests such as chorionic villus sampling and amniocentesis can be used to diagnose chromosomal abnormalities\r\n and infections in women at high risk.
- Neonatal screening:
Screening of newborns is an important step towards detection. This helps to reduce mortality and morbidity from birth defects by facilitating earlier referral and the initiation of medial or surgical treatment.
Early screening for hearing loss provides an opportunity for early correction and allows the possibility of acquiring better language, speech and communication skills. Early screening of newborns for congenital cataract also allows early referral and\r\n surgical correction which increases the likelihood of sight.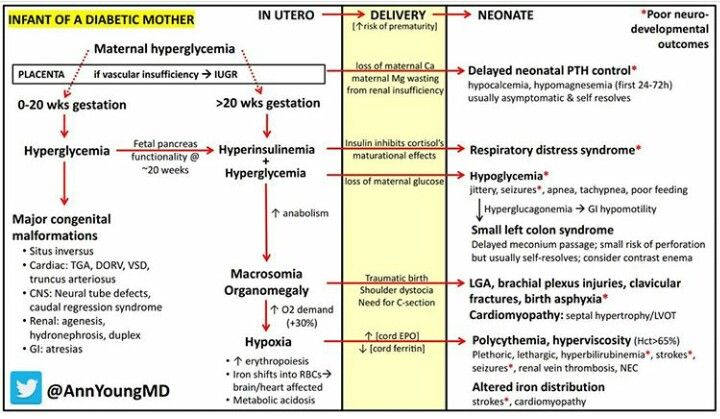
Newborns may be screened for certain metabolic, hematologic and endocrine disorders, many of which may not have immediately visible effects. The conditions screened for vary by country, depending on prevalence and cost. Newborn screening is increasingly\r\n conducted even in low- and middle-income countries.
Treatment and care
Some birth defects can be treated with medical or surgical interventions. Access to this care may vary by country and by different levels of a health system, though complex care is increasingly available in low- and middle-income settings.
Surgery with good follow up care can often mitigate the potential lethality (as in the case of congenital heart defects) or the morbidity (e.g., congenital talipes, cleft lip/palate) associated with structural birth defects. The contribution to reducing\r\n mortality and morbidity of this aspect of the treatment is often underestimated. Outcomes are improved with early detection at lower levels of the system through screening, referral and management (at specialist centres in case of some issues like\r\n cardiac defects).
Medical treatment for certain metabolic, endocrine and hematological conditions can improve quality of life. A clear example is congenital hypothyroidism, where early detection and treatment allows full physical and mental development to healthy adulthood,\r\n whereas a missed diagnosis or unavailability of a simple treatment carries a risk of serious intellectual disability.
Children with some types of birth defects may require long term support including physical therapy, speech therapy, occupational therapy and support from families and community.
WHO response
Through the resolution on birth defects of the Sixty-third World Health Assembly (2010), Member States agreed to promote primary prevention and improve the health of children with congenital anomalies by:
- developing and strengthening registration and surveillance systems;
- developing expertise and building capacity for the prevention of birth defects and care of children affected;
- raising awareness on the importance of newborn screening programmes and their role in identifying infants born with congenital birth defects;
- supporting families who have children with birth defects and associated disabilities; and
- strengthening research on major birth defects and promoting international cooperation in combatting them.
Together with partners, WHO convenes annual training programmes on the surveillance and prevention of birth defects. WHO is also working with partners to provide the required technical expertise for the surveillance of neural tube defects, for monitoring\r\n fortification of staple foods with folic acid, and for improving laboratory capacity for assessing risks for folic acid-preventable birth defects and is assisting low- and middle-income countries in improving control and elimination of rubella and\r\n congenital rubella syndrome through immunization.
WHO develops normative tools, including guidelines and a global plan of action, to strengthen medical care and rehabilitation services to support the implementation of the United Nations convention on the rights of persons with disabilities.\r\n \r\n
","datePublished":"2022-02-28T22:52:00.0000000+00:00","image":"https://cdn.who.int/media/images/default-source/imported/preterm-birth-mother-jpg.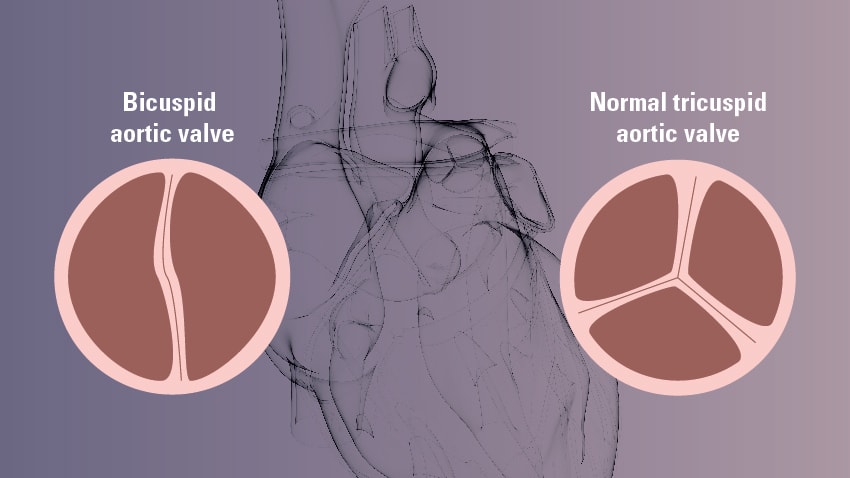 jpg?sfvrsn=c5c1adf1_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo":{"@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified":"2022-02-28T22:52:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/news-room/fact-sheets/detail/birth-defects","@context":"http://schema.org","@type":"Article"};
jpg?sfvrsn=c5c1adf1_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo":{"@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified":"2022-02-28T22:52:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/news-room/fact-sheets/detail/birth-defects","@context":"http://schema.org","@type":"Article"};
Key facts
- An estimated 240 000 newborns die worldwide within 28 days of birth every year due to birth defects. Birth defects cause a further 170 000 deaths of children between the ages of 1 month and 5 years.
- Birth defects can contribute to long-term disability, which takes a significant toll on individuals, families, health care systems and societies.
- Nine of ten children born with a serious birth defect are in low- and middle-income countries.
- As neonatal and under-5 mortality rates decline, birth defects become a larger proportion of the cause of neonatal and under-5 deaths.
- The most common severe birth defects are heart defects, neural tube defects and Down syndrome.
- Although birth defects may be the result of one or more genetic, infectious, nutritional or environmental factors, it is often difficult to identify the exact causes.
- Some birth defects can be prevented. Vaccination, adequate intake of folic acid or iodine through fortification of staple foods or supplementation, and adequate care before and during a pregnancy are examples of prevention methods.
Birth defects are also known as congenital abnormalities, congenital disorders or congenital malformations. They can be defined as structural or functional anomalies (for example, metabolic disorders) that occur during intrauterine life and can be identified prenatally, at birth, or sometimes may only be detected later in infancy, such as hearing defects. Broadly, congenital refers to the existence at or before birth.
The proportion of under-5 deaths due to birth defects increases as other causes of under-5 deaths are controlled (fig. 1).
1).
Fig 1: Changes in causes of under 5 deaths as under 5 mortality rates decline
Causes and risk factors
Genetic
A minority of birth defects are caused by genetic abnormalities i.e. chromosomal abnormalities (for example Down syndrome or trisomy 21) or single gene defects (for example cystic fibrosis).
Consanguinity (when parents are related by blood) also increases the prevalence of rare genetic birth defects and nearly doubles the risk for neonatal and childhood death, intellectual disability and other anomalies.
Socioeconomic and demographic factors
Low-income may be an indirect determinant of birth defects, with a higher frequency among resource-constrained families and countries. It is estimated that about 94% of severe birth defects occur in low- and middle-income countries. An indirect determinant, this higher risk relates to a possible lack of access to sufficient nutritious foods by pregnant women, an increased exposure to agents or factors such as infection and alcohol, or poorer access to health care and screening.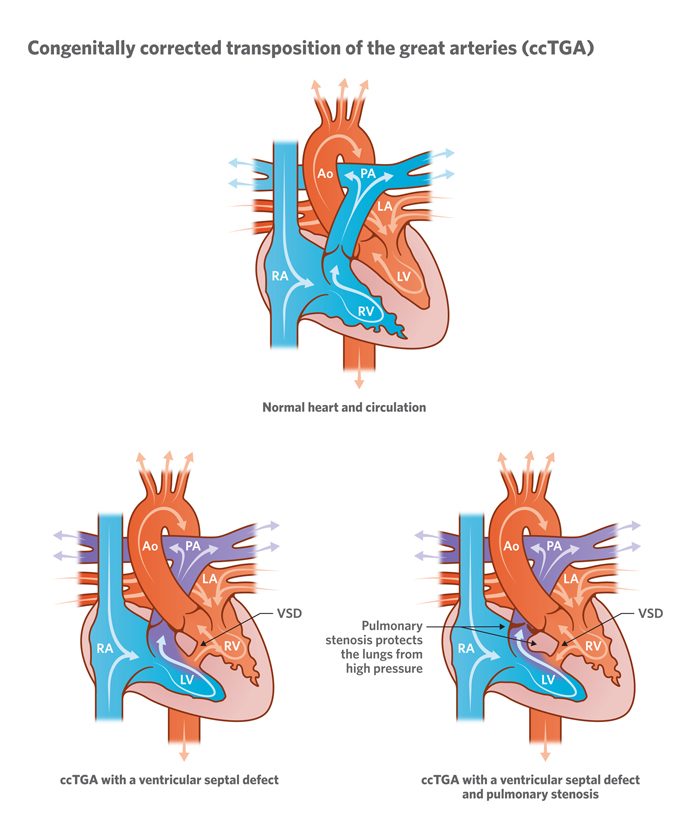
Maternal age is also a risk factor for abnormal intrauterine fetal development. Advanced maternal age increases the risk of chromosomal abnormalities, including Down syndrome.
Environmental factors including infections
Others occur because of environmental factors like maternal infections (syphilis, rubella, Zika), exposure to radiation, certain pollutants, maternal nutritional deficiencies (e.g., iodine, folate deficiency), illness (maternal diabetes) or certain drugs (alcohol, phenytoin).
Unknown causes
While complex genetic and environmental interactions are proposed, most birth defects have unknown causes, including congenital heart defects, cleft lip or palate and club foot.
Prevention
Preventive public health measures work to decrease the frequency of certain birth defects through the removal of risk factors or the reinforcement of protective factors. Important interventions and efforts include:
- ensuring adolescent girls and mothers have a healthy diet including a wide variety of vegetables and fruit, and maintain a healthy weight;
- ensuring an adequate dietary intake of vitamins and minerals, particularly folic acid in adolescent girls and mothers;
- ensuring mothers avoid harmful substances, particularly alcohol and tobacco;
- avoidance of travel by pregnant women (and sometimes women of child-bearing age) to regions experiencing outbreaks of infections known to be associated with birth defects;
- reducing or eliminating environmental exposure to hazardous substances (such as heavy metals or pesticides) during pregnancy;
- controlling diabetes prior to and during pregnancy through counselling, weight management, diet and administration of insulin when required;
- ensuring that any exposure of pregnant women to medications or medical radiation (such as imaging rays) is justified and based on careful health risk–benefit analysis;
- vaccination, especially against the rubella virus, for children and women;
- increasing and strengthening education of health staff and others involved in promoting prevention of congenital anomalies; and
- screening for infections, especially rubella, varicella and syphilis, and consideration of treatment.
Screening, treatment and care
Screening
Health care before and near conception (preconception and peri-conception) includes basic reproductive health practices, as well as medical genetic screening and counselling. Screening can be conducted during the 3 periods listed:
- Preconception screening:
This can be useful to identify those at risk of specific disorders or of passing a disorder onto their children. Screening includes obtaining family histories and carrier screening and is particularly valuable in countries where consanguineous marriage is common.
- Peri-conception screening:
Maternal characteristics may increase risk, and screening results should be used to offer appropriate care, according to risk. This may include screening for young or advanced maternal age, as well as screening for use of alcohol, tobacco or other risks. Ultrasound can be used to screen for Down syndrome and major structural abnormalities during the first trimester, and for severe fetal anomalies during the second trimester.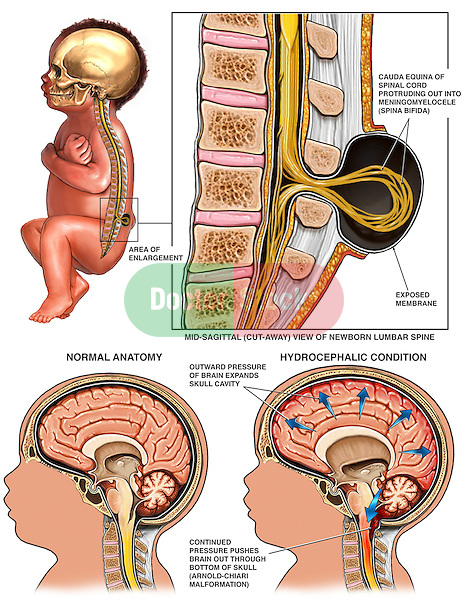 Maternal blood can be screened for placental markers to aid in prediction of risk of chromosomal abnormalities or neural tube defects, or for free fetal DNA to screen for many chromosomal abnormalities. Diagnostic tests such as chorionic villus sampling and amniocentesis can be used to diagnose chromosomal abnormalities and infections in women at high risk.
Maternal blood can be screened for placental markers to aid in prediction of risk of chromosomal abnormalities or neural tube defects, or for free fetal DNA to screen for many chromosomal abnormalities. Diagnostic tests such as chorionic villus sampling and amniocentesis can be used to diagnose chromosomal abnormalities and infections in women at high risk.
- Neonatal screening:
Screening of newborns is an important step towards detection. This helps to reduce mortality and morbidity from birth defects by facilitating earlier referral and the initiation of medial or surgical treatment.
Early screening for hearing loss provides an opportunity for early correction and allows the possibility of acquiring better language, speech and communication skills. Early screening of newborns for congenital cataract also allows early referral and surgical correction which increases the likelihood of sight.
Newborns may be screened for certain metabolic, hematologic and endocrine disorders, many of which may not have immediately visible effects. The conditions screened for vary by country, depending on prevalence and cost. Newborn screening is increasingly conducted even in low- and middle-income countries.
The conditions screened for vary by country, depending on prevalence and cost. Newborn screening is increasingly conducted even in low- and middle-income countries.
Treatment and care
Some birth defects can be treated with medical or surgical interventions. Access to this care may vary by country and by different levels of a health system, though complex care is increasingly available in low- and middle-income settings.
Surgery with good follow up care can often mitigate the potential lethality (as in the case of congenital heart defects) or the morbidity (e.g., congenital talipes, cleft lip/palate) associated with structural birth defects. The contribution to reducing mortality and morbidity of this aspect of the treatment is often underestimated. Outcomes are improved with early detection at lower levels of the system through screening, referral and management (at specialist centres in case of some issues like cardiac defects).
Medical treatment for certain metabolic, endocrine and hematological conditions can improve quality of life. A clear example is congenital hypothyroidism, where early detection and treatment allows full physical and mental development to healthy adulthood, whereas a missed diagnosis or unavailability of a simple treatment carries a risk of serious intellectual disability.
A clear example is congenital hypothyroidism, where early detection and treatment allows full physical and mental development to healthy adulthood, whereas a missed diagnosis or unavailability of a simple treatment carries a risk of serious intellectual disability.
Children with some types of birth defects may require long term support including physical therapy, speech therapy, occupational therapy and support from families and community.
WHO response
Through the resolution on birth defects of the Sixty-third World Health Assembly (2010), Member States agreed to promote primary prevention and improve the health of children with congenital anomalies by:
- developing and strengthening registration and surveillance systems;
- developing expertise and building capacity for the prevention of birth defects and care of children affected;
- raising awareness on the importance of newborn screening programmes and their role in identifying infants born with congenital birth defects;
- supporting families who have children with birth defects and associated disabilities; and
- strengthening research on major birth defects and promoting international cooperation in combatting them.
Together with partners, WHO convenes annual training programmes on the surveillance and prevention of birth defects. WHO is also working with partners to provide the required technical expertise for the surveillance of neural tube defects, for monitoring fortification of staple foods with folic acid, and for improving laboratory capacity for assessing risks for folic acid-preventable birth defects and is assisting low- and middle-income countries in improving control and elimination of rubella and congenital rubella syndrome through immunization.
WHO develops normative tools, including guidelines and a global plan of action, to strengthen medical care and rehabilitation services to support the implementation of the United Nations convention on the rights of persons with disabilities.
Congenital heart defects in children
Congenital heart disease - a disease of the heart valves, in which the organ begins to work incorrectly. As a result of a congenital change in the structure of the valvular apparatus, cardiac partitions, walls or large vessels extending from the heart, a violation of the blood flow of the heart occurs. The disease may progress. In some cases, death is possible.
As a result of a congenital change in the structure of the valvular apparatus, cardiac partitions, walls or large vessels extending from the heart, a violation of the blood flow of the heart occurs. The disease may progress. In some cases, death is possible.
Congenital heart defects occur with a frequency of 6-8 cases per thousand births, which is 30% of all malformations. They rank first in terms of mortality of newborns and children of the first year of life. After the first year of life, mortality decreases sharply, and in the period from 1 year to 15 years, no more than 5% of children die. nine0005
The earlier a congenital heart disease is detected, the greater the hope for its timely treatment.
Causes
- Rubella virus.
- Influenza viruses, as well as some others, if their effect falls on the first 3 months of pregnancy.
- Bacterial infections.
- Presence of a genetic predisposition.
Symptoms
- Blue or bluish discoloration of the skin, lips, ears.
 nine0014
nine0014 - The appearance of bluish skin when breastfeeding, the cry of the baby.
- Pale skin and cold extremities (with "pale vices").
- Murmurs in the heart.
- Signs of heart failure.
- Changes in the electrocardiogram, x-rays, echocardiography (ultrasound of the heart).
Of course, with such symptoms, concerned parents immediately go to the doctor, and heart disease is diagnosed in the first months of the child's life, or at birth during the accompanying first examinations. Small defects sometimes manifest themselves only as unusual heart murmurs when listening during regular examinations by a pediatrician. nine0005
Even with a congenital heart disease, for some time after birth, the child may look outwardly quite healthy during the first ten years of life. However, in the future, heart disease begins to manifest itself: the child lags behind in physical development, shortness of breath appears during physical exertion, pallor or even cyanosis of the skin.
To establish a true diagnosis, a comprehensive examination of the heart using modern high-tech equipment is necessary. nine0005
Surgical treatment is the most effective, and operations are often performed on newborns and children from the first year of life. Most often, the question of surgical treatment is raised even before the birth of the child, if it concerns "blue defects". Therefore, in such cases, childbirth should take place in maternity hospitals at cardiac surgical hospitals. Therapeutic treatment is necessary if the timing of the operation can be postponed to a later date. If the question is about "pale malformations", then the treatment will depend on how the defect behaves as the child grows. Most likely, all treatment will be therapeutic. nine0005
Prevention
Since the causes of congenital heart defects are still poorly understood, it is difficult to determine the necessary preventive measures that would guarantee the prevention of the development of congenital heart defects. However, parents' concern for their own health can significantly reduce the risk of congenital diseases in a child.
However, parents' concern for their own health can significantly reduce the risk of congenital diseases in a child.
More about pediatric cardiology at YugMed clinic
By leaving your personal data, you give your voluntary consent to the processing of your personal data. Personal data refers to any information relating to you as a subject of personal data (name, date of birth, city of residence, address, contact phone number, email address, occupation, etc.). Your consent extends to the implementation by the Limited Liability Company Research and Production Association "Volgograd Center for Disease Prevention "YugMed" of any actions in relation to your personal data that may be necessary for the collection, systematization, storage, clarification (updating, changing), processing (for example, sending letters or making calls), etc. subject to current legislation. Consent to the processing of personal data is given without a time limit, but can be withdrawn by you (it is enough to inform the Limited Liability Company Scientific and Production Association "Volgograd Center for Disease Prevention" YugMed ").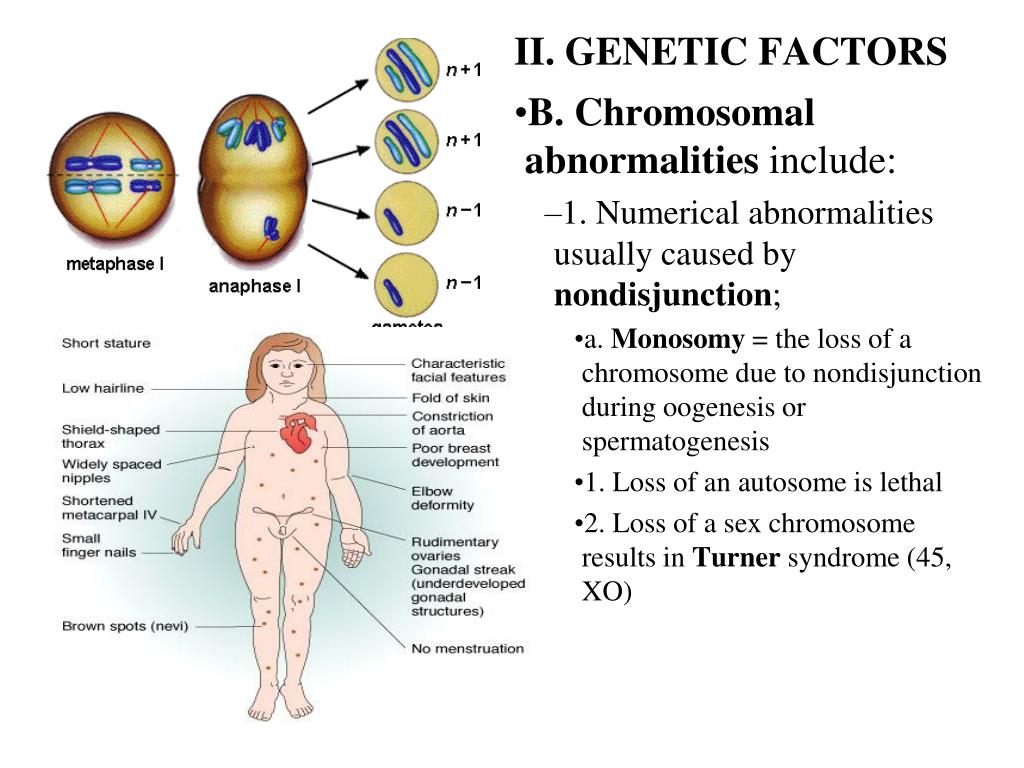 By sending your personal data to the Limited Liability Company Research and Production Association "Volgograd Center for Disease Prevention" YugMed ", you confirm that you are familiar with the rights and obligations in accordance with the Federal Law "On Personal Data". nine0005
By sending your personal data to the Limited Liability Company Research and Production Association "Volgograd Center for Disease Prevention" YugMed ", you confirm that you are familiar with the rights and obligations in accordance with the Federal Law "On Personal Data". nine0005
Congenital heart defects: types and methods of diagnosis
+7 (495) 780-07-71
Call center open 24/7
Ambulancearound the clock
Author
Polina Svetlana Aleksandrovna
Cardiologist
Creation date: 2020.03.13
Cashback 1000 rub for all services for a visit in January More All promotions
Congenital heart defects (CHD) are developmental anomalies that lead to a violation of the morphological structure of the heart, including the valvular apparatus and great vessels. nine0005
CHD occur during fetal development (usually on the 2nd-8th week) as a result of a violation of the processes of embryogenesis. These anomalies can occur both in isolation and in combination with each other.
The overall prevalence of this group of diseases is up to 5-8 cases per 1000 births. Congenital malformations can be associated with chromosomal abnormalities, however, it is often non-chromosomal congenital heart defects that are diagnosed. nine0005
The overall incidence of non-chromosomal CHD is up to 7 cases per 1000 births, of which up to 3.5% are perinatal losses, 20% are diagnosed prenatally, 5.6% of pregnancies are terminated due to a detected fetal anomaly. Complex non-chromosomal heart defects are less common, about 2 cases per 1000 births. The outcome in 8% of cases is perinatal death, 40% are diagnosed in utero, 14% cause abortion.
Any questions? nine0005
Leave the phone -
and we will call you back
Causes of CHD
The main leading causes in the formation of defects, most often, are structural and quantitative chromosomal anomalies, and mutations, i.e. primary genetic factors.
It is also necessary to pay attention to potentially teratogenic environmental factors: various intrauterine infections (rubella viruses, cytomegalovirus, coxsackie, infectious diseases in the mother in the first trimester), drugs (vitamin A, antiepileptic drugs, sulfasalazine, trimethoprim), constant contact with toxic substances ( paints, varnishes). In addition, it must be remembered that maternal factors have a negative impact on intrauterine development: reproductive problems preceding this pregnancy, the presence of diabetes mellitus, phenylketonuria, alcoholism, smoking, age, but also factors from the father's side - age, drug use ( cocaine, marijuana). nine0005
In addition, it must be remembered that maternal factors have a negative impact on intrauterine development: reproductive problems preceding this pregnancy, the presence of diabetes mellitus, phenylketonuria, alcoholism, smoking, age, but also factors from the father's side - age, drug use ( cocaine, marijuana). nine0005
The leading role belongs to the multifactorial theory of the development of congenital heart defects (up to 90%).
Types of congenital heart defects
-
Atrial septal defect (ASD) or open foramen ovale is diagnosed when one or more holes are found in the atrial septum. One of the most common congenital heart defects. Depending on the location of the defect, its size, the strength of the blood flow, more or less pronounced clinical signs are determined. Often ASD is combined with other heart anomalies and is determined in Down's syndrome. nine0005
-
Ventricular septal defect (VSD) - is diagnosed with underdevelopment of the interventricular septum at various levels with the formation of a pathological communication between the left and right ventricles.
 It can occur both in isolation and together with other developmental anomalies. With a small defect, there is often no pronounced lag in physical development. VSD is dangerous because it can lead to the development of pulmonary hypertension, and therefore, it must be promptly corrected by surgery. nine0005
It can occur both in isolation and together with other developmental anomalies. With a small defect, there is often no pronounced lag in physical development. VSD is dangerous because it can lead to the development of pulmonary hypertension, and therefore, it must be promptly corrected by surgery. nine0005 -
Aortic coartation is a segmental narrowing of the aortic lumen with disruption of normal blood flow from the left ventricle to the systemic circulation. Up to 8% of all CHD cases are detected, more often in boys, often combined with other anomalies.
-
An open ductus arteriosus is diagnosed when the Batall duct is not blocked, which is determined in newborns and subsequently overgrows. As a result, there is a partial discharge of arterial blood from the aorta into the pulmonary artery. With this CHD, there are often no severe clinical manifestations, however, the pathology requires surgical correction, since it is associated with a high risk of sudden cardiac death.
 nine0005
nine0005 -
Pulmonary artery atresia - diagnosed underdevelopment (complete or partial) of the cusps of the pulmonary valve with the development of backflow of blood from the pulmonary artery into the cavity of the right ventricle. Subsequently, it leads to insufficient blood supply to the lungs.
-
Pulmonary valve stenosis is an anomaly in which narrowing of the orifice of the pulmonary valve is diagnosed. As a result of the pathology, most often, the valve leaflets, the normal blood flow from the right ventricle to the pulmonary trunk is disturbed. nine0005
-
Tetralogy of Fallot is a complex concomitant CHD. Combines ventricular septal defect, pulmonary artery stenosis, right ventricular hypertrophy, aortic dextraposition. With this pathology, a mixture of arterial and venous blood occurs.
-
Transposition of the great vessels is also a complex CHD. With this pathology, the aorta departs from the right ventricle and carries venous blood, and the pulmonary trunk departs from the left ventricle and carries arterial blood, respectively.
 Parok proceeds hard, is associated with high mortality of newborns. nine0005
Parok proceeds hard, is associated with high mortality of newborns. nine0005 -
Dextrocardia is an anomaly of intrauterine development, characterized by right-sided placement of the heart. Often, there is a "mirror" arrangement of other unpaired internal organs.
-
Ebstein's anomaly is a rare congenital heart disease, diagnosed when the location of the tricuspid valve leaflets changes. Normal - from the atrioventricular fibrous ring, with anomalies - from the walls of the right ventricle. The right ventricle is smaller and the right atrium is elongated, with abnormal valves. nine0005
CHD diagnostic methods
Diagnosis of congenital heart disease is based on the collection of anamnesis data (the presence of malformations, including congenital heart defects, genetic diseases in the next of kin; information about pregnancy and the presence of etiological factors in parents).
When collecting complaints, attention is paid to the child's lag in development, poor weight gain, poor appetite, sluggish sucking from the breast or bottle, refusal of the breast, cyanosis, and frequent respiratory infections. nine0005
nine0005
Physical examination
During a physical examination, pay attention to the color of the skin, determine the pulse and blood pressure (on the right arm and any leg), perform auscultation of the heart, lungs, pay attention to the presence of peripheral edema, conduct pulse oximetry, and determine diuresis.
Instrumentation
However, the leading role in the diagnosis and confirmation, differential diagnosis of CHD is played by instrumental examination methods: X-ray examination of the chest organs, electrocardiography, echocardiography, MRI, CT, catheterization of the heart cavities. nine0005
To accurately diagnose the disease, make an appointment with the specialists of the Family Doctor network.
CHD treatments
In most cases, the treatment of congenital heart defects is surgical, and depending on the anatomy of the defect, the timing and type of intervention are determined.
In order to stabilize the condition before the planned surgical treatment, methods of therapeutic drug treatment of critical conditions and complications of CHD are resorted to.