Scrape cervix to induce labor
Risks and effectiveness for inducing labor
Membrane stripping or sweeping is can help induce labor in pregnant people near or past their due date. A doctor inserts their fingers into the cervix and sweeps between the thin membranes of the amniotic sac.
The amniotic sac is the thin-walled sac around the fetus. Membrane stripping or sweeping stimulates hormone and prostaglandin production, compounds that help induce labor.
This article covers the safety, efficacy and potential risks of membrane stripping.
Membrane stripping is usually safe in uncomplicated pregnancies.
However, there are minor risks associated with this technique. These include:
- mild discomfort during the procedure
- minor vaginal bleeding
- irregular contractions
Membrane stripping carries minimal risk, but it may not be suitable for everyone.
Who should not have membrane stripping?
A doctor is likely to decide against membrane stripping if it is unsafe for a person to deliver their baby vaginally. The following factors might also make the procedure unsuitable:
- prior cesarean delivery
- multiple births
- history of preterm delivery
- current bacterial cervical infection
- placenta previa, where the placenta covers the opening of the cervix
- active herpes infection
- vasa previa, a condition in which connective membranes cover the opening of the cervix
- severe fetal abnormalities
- Mullerian duct abnormalities
- abnormal fetal position
- structural pelvic abnormalities
- prior uterine rupture
In most cases, membrane stripping increases the likelihood of spontaneous labor, especially in the 7 days following the procedure. However, a 2020 research review found that membrane stripping does not typically lead to unassisted vaginal birth.
Researchers found 40 studies involving 6,548 women, comparing the rate of labor from membrane stripping versus no intervention. They concluded that membrane stripping can increase the likelihood of spontaneous labor by more than 20%.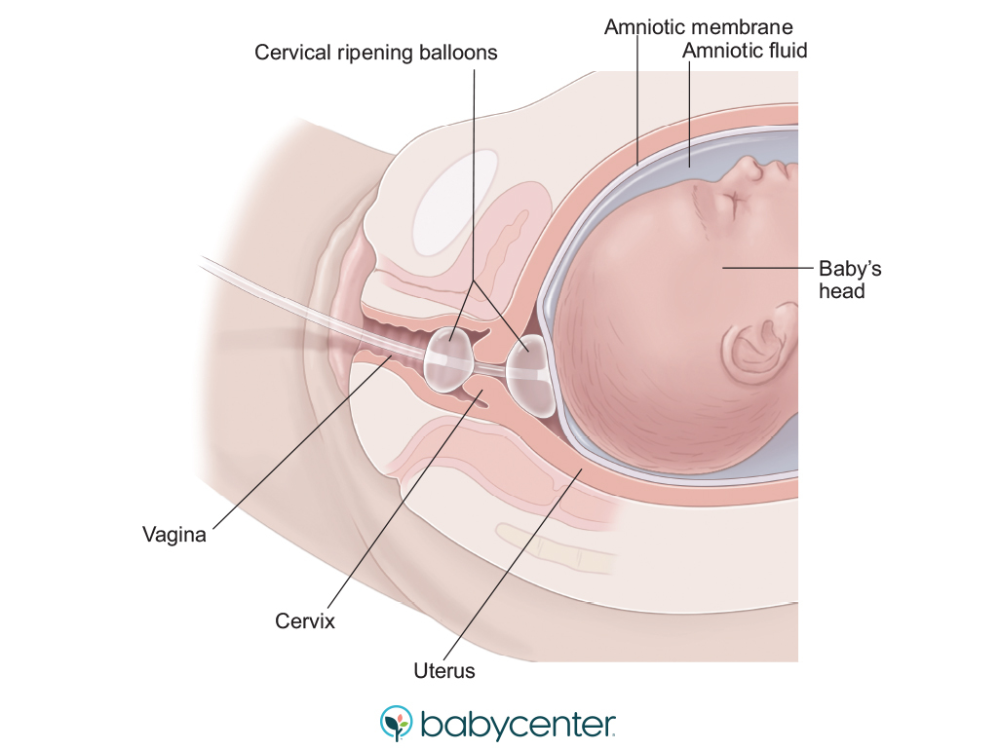
Doctors usually only need to carry out the procedure once to induce labor successfully. However, some women may require multiple stripping procedures.
For example, a 2014 study of 800 women found that membrane stripping, in conjunction with other methods of induction:
- reduces the time between induction and labor
- increases the vaginal delivery rate
- lowers the need for oxytocin, a drug that induces labor
How painful is a membrane strip?
The procedure can be uncomfortable, and most women feel a bit of pain and tenderness afterward. Some women also experience minor bleeding.
It is essential to inform the doctor immediately if severe pain or bleeding occurs during or after the appointment.
What should someone expect before and after a membrane strip?
Women do not generally need to prepare for membrane stripping, which the doctor will carry out as part of a regular examination.
The procedure usually takes place in a doctor’s office. The doctor may need to stimulate the cervix to dilate it, as membrane stripping will not be possible otherwise.
The doctor may need to stimulate the cervix to dilate it, as membrane stripping will not be possible otherwise.
Membrane stripping s a nonsurgical intervention that can induce labor.
Doctors typically perform membrane stripping during the final few weeks of pregnancy, usually between 38 and 41 weeks of gestation.
Membrane stripping is a relatively safe procedure in uncomplicated pregnancies, and study results have shown that it can increase the likelihood of spontaneous labor.
Purpose, Procedure, and What Happens After
I was pregnant with my son during one of the hottest summers on record. By the time the end of my third trimester rolled around, I was so swollen I could barely turn over in bed.
At the time, I worked in our local labor and delivery unit as a nurse, so I knew my doctor well. At one of my checkups, I begged her to do something to help spur my labor.
If only they would strip my membranes to induce labor, I reasoned, I could be out of my misery and meet my baby boy sooner.
Here’s a look at how effective membrane stripping is for inducing labor, plus the risks and benefits.
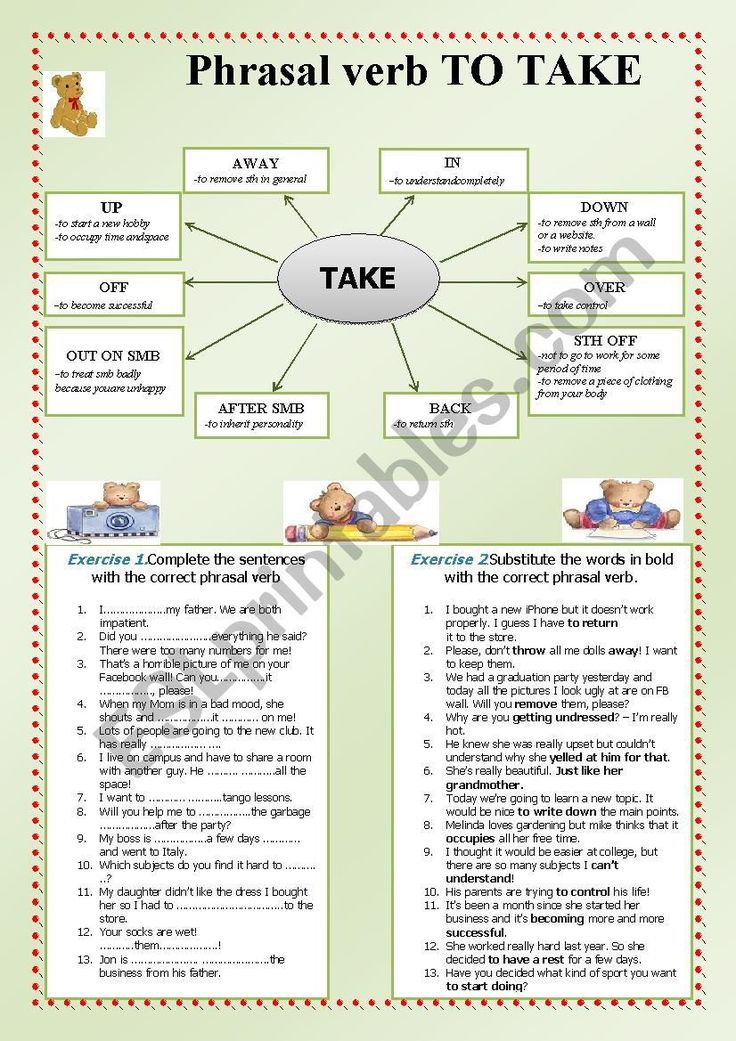
Stripping the membranes is a way to induce labor. It involves your doctor sweeping their (gloved) finger between the thin membranes of the amniotic sac in your uterus. It’s also known as a membrane sweep.
This motion helps separate the sac. It stimulates prostaglandins, compounds that act like hormones and can control certain processes in the body. One of these processes is — you guessed it — labor.
In some cases, your doctor can also gently stretch or massage the cervix to help it start to soften and dilate.
Your doctor may suggest trying a membrane stripping if:
- you’re near or past your due date
- there isn’t a pressing medical reason to induce labor with a faster method
You don’t need to do anything to prepare for a membrane stripping. The procedure can be done in your doctor’s office.
You’ll simply hop up on the exam table like at a normal checkup.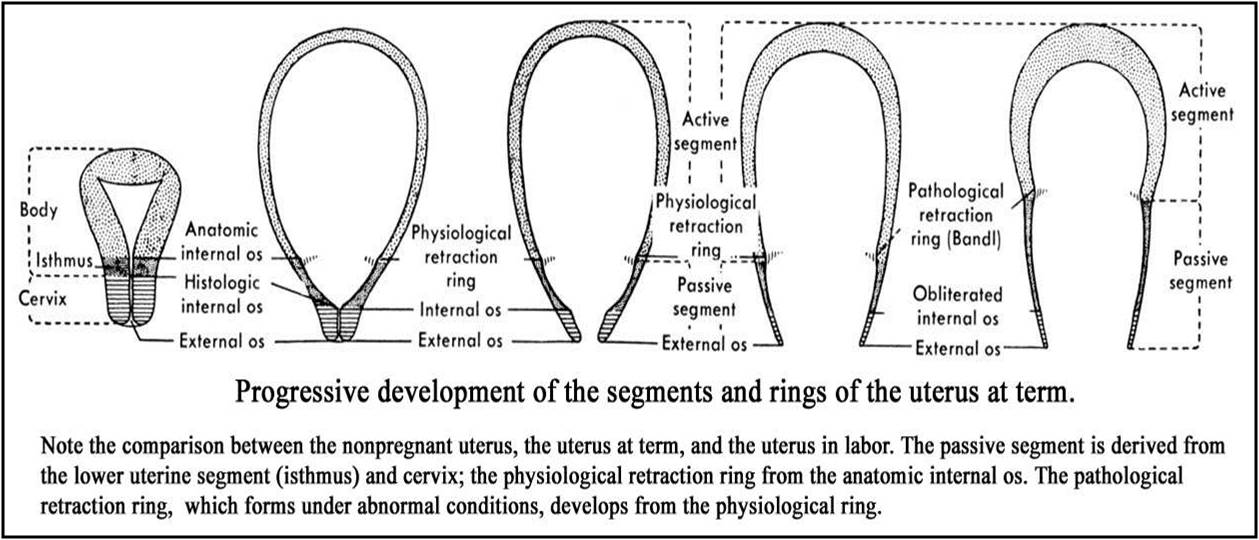 The best thing you can do during the procedure is simply breathe through it and try to relax. Membrane stripping doesn’t take long. The entire procedure will be over in a few minutes.
The best thing you can do during the procedure is simply breathe through it and try to relax. Membrane stripping doesn’t take long. The entire procedure will be over in a few minutes.
Researchers on a study published in the Journal of Clinical Gynecology and Obstetrics (JCGO) didn’t find any increased risks for negative side effects in women undergoing membrane stripping.
Women who have their membrane swept aren’t more likely to have a cesarean delivery (commonly referred to as a C-section) or other complications.
The study concluded that membrane stripping is safe and that, in most cases, women will only need to have the procedure one time for it to work.
Experts still question whether or not membrane stripping is really effective. A 2011 review of available studies concluded that the efficacy depends on how far along in pregnancy a woman is, and whether or not she uses other induction methods. It’s most effective if she doesn’t.
The JCGO study reported that after a membrane sweep, 90 percent of women delivered by 41 weeks compared to women who didn’t receive the membrane sweep.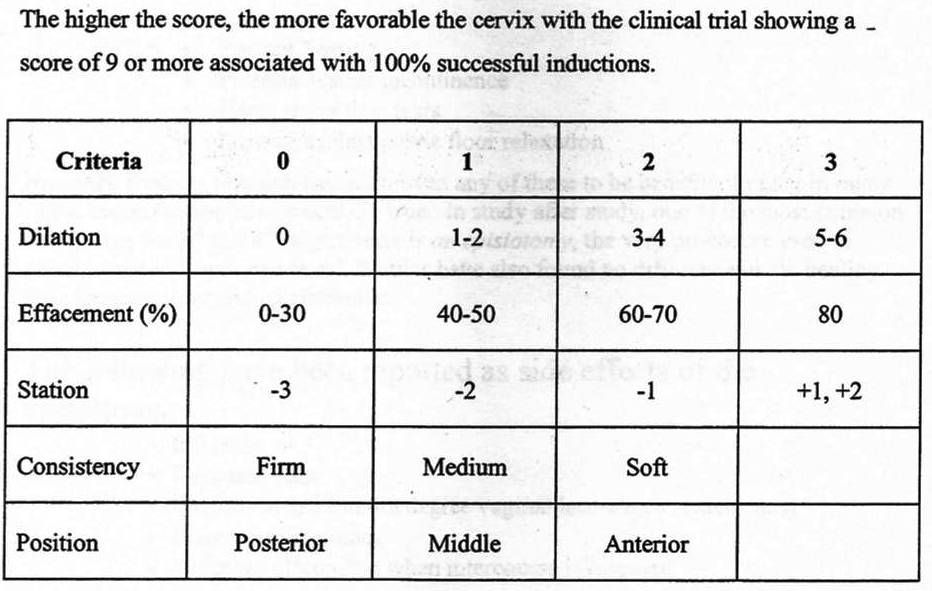 Of these, only 75 percent delivered by 41 weeks’ gestation. The goal is to stimulate labor and safely deliver before the pregnancy is beyond 41 weeks, and membrane stripping may occur as early as 39 weeks.
Of these, only 75 percent delivered by 41 weeks’ gestation. The goal is to stimulate labor and safely deliver before the pregnancy is beyond 41 weeks, and membrane stripping may occur as early as 39 weeks.
Membrane stripping might be most effective for women who are past their due dates. One study found that membrane sweeping could increase the likelihood of spontaneous labor within 48 hours.
Membrane stripping isn’t as effective as other types of induction, such as using medications. It’s generally only used in situations when there really isn’t a pressing medical reason to induce.
Advice from a nurse educator This procedure does cause some discomfort and should only be done by an experienced doctor. You may experience bleeding and cramping for a few days following the procedure. But if it works, it could save you from having your labor induced with medication.
Advice from a Nurse Educator
This procedure does cause some discomfort and should only be done by an experienced doctor.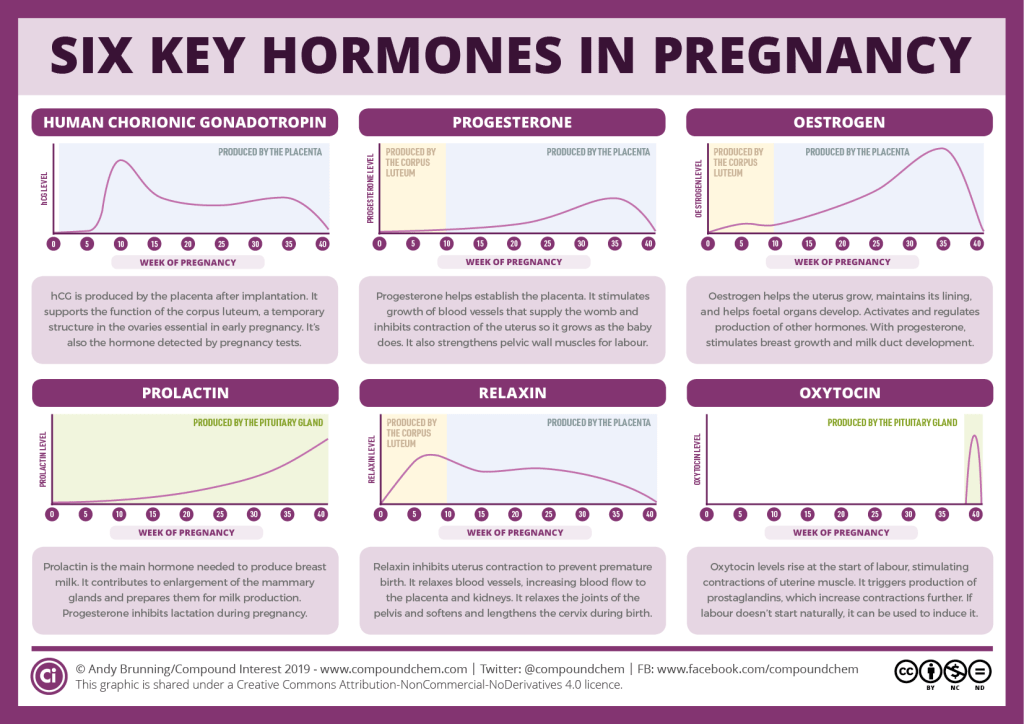 You may experience bleeding and cramping for a few days following the procedure. But if it works, it could save you from having your labor induced with medication.
You may experience bleeding and cramping for a few days following the procedure. But if it works, it could save you from having your labor induced with medication.
The bottom line is you’ll need to balance your discomfort with other adverse effects.
— Debra Sullivan, PhD, MSN, RN, CNE, COI
To be honest, a membrane stripping isn’t a comfy experience. It can be uncomfortable to go through, and you may feel a bit sore afterward.
Your cervix is highly vascular, meaning it has a lot of blood vessels. You may also experience some light bleeding during and after the procedure, which is completely normal. However, if you’re experiencing a lot of bleeding or in a lot of pain, be sure to go to the hospital.
Membrane stripping is most effective if a woman:
- is over 40 weeks in their pregnancy
- doesn’t use any other type of labor-inducing techniques
In those cases, the JCGO study found that women on average went into labor on their own about a week earlier than women who didn’t have their membranes swept.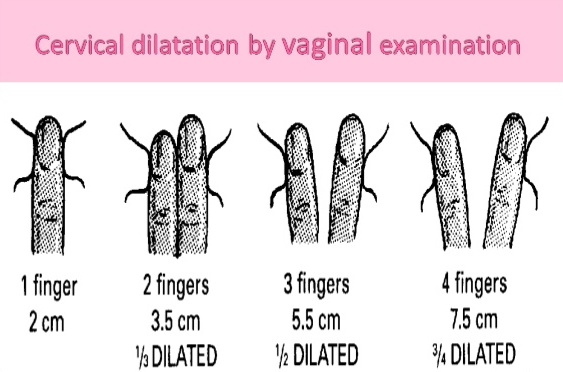
If you’re reaching a stage in your pregnancy where you’re feeling miserable, talk to your doctor about the pros and cons of a membrane induction. Remember that unless there’s a medical concern, it’s usually best to let your pregnancy progress naturally.
But if you’re past your due date and you don’t have a high-risk pregnancy, a membrane stripping might be a very effective and safe way to help put you into labor naturally. And hey, it might be worth a shot, right?
What will help in childbirth - articles from the specialists of the clinic "Mother and Child"
Vovk Lyudmila Anatolyevna
Reproductologist, Obstetrician-gynecologist
Lapino-1 Clinical Hospital "Mother and Child"
We walk and dance
If earlier in the maternity hospital, with the onset of labor, a woman was put to bed, now, on the contrary, obstetricians recommend that the expectant mother move . For example, you can just walk: the rhythm of steps soothes, and gravity helps the neck to open faster.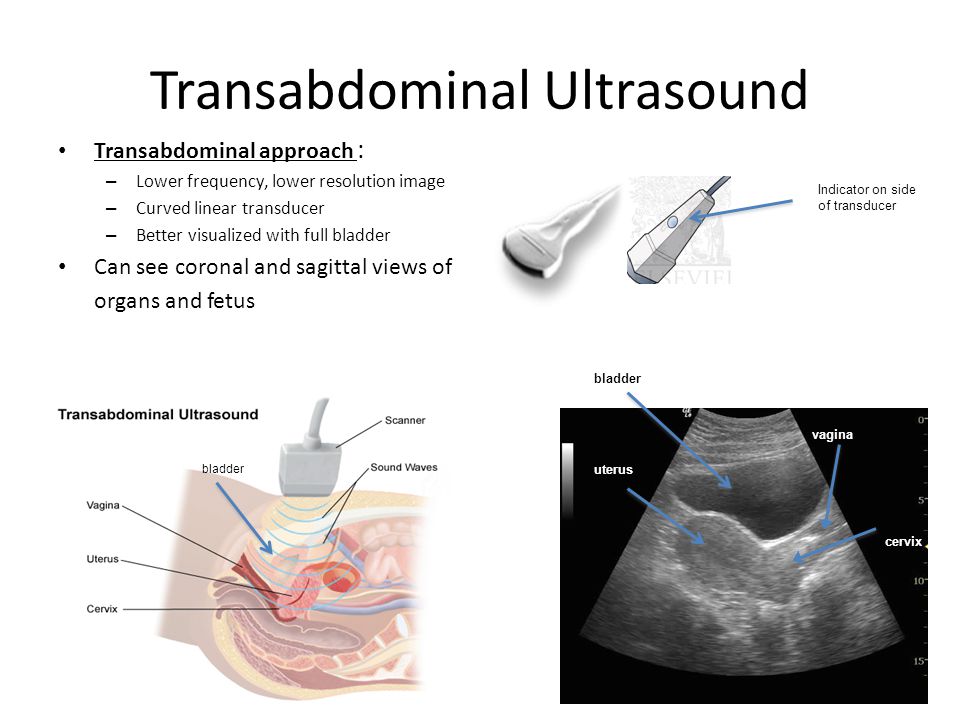 You need to walk as fast as it is convenient, without sprinting up the stairs, it’s better to just “cut circles” along the corridor or ward, from time to time (during the aggravation of the fight) resting on something. The gait does not matter - you can roll over like a duck, rotate your hips, walk with your legs wide apart. It is worth trying and dancing, even if you think that you do not know how. For example, you can swing your hips back and forth, describe circles and figure eights with your fifth point, sway in a knee-elbow position. The main thing is to move smoothly and slowly, without sudden movements. nine0003
You need to walk as fast as it is convenient, without sprinting up the stairs, it’s better to just “cut circles” along the corridor or ward, from time to time (during the aggravation of the fight) resting on something. The gait does not matter - you can roll over like a duck, rotate your hips, walk with your legs wide apart. It is worth trying and dancing, even if you think that you do not know how. For example, you can swing your hips back and forth, describe circles and figure eights with your fifth point, sway in a knee-elbow position. The main thing is to move smoothly and slowly, without sudden movements. nine0003
Showering and bathing
For many people, water is a great way to relieve fatigue and tension, and it also helps with painful contractions. You can just stand in the shower, or you can lie down in the bath. Warm water will warm the muscles of the back and abdomen, they will relax, and the birth canal will relax - as a result, the pain may decrease. Well, if it does not decrease, then in any case, the water will relieve stress and at least for a while distract from the pain.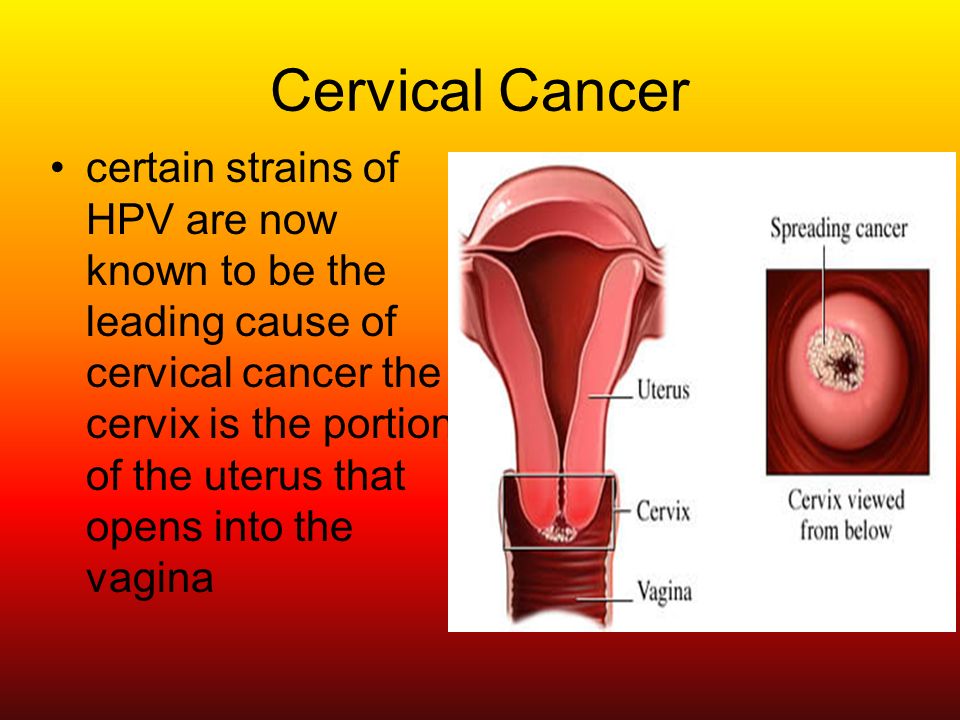 So if there is a shower or jacuzzi bath in the delivery room, do not be shy and try this method of pain relief for contractions. The only thing is that the water should not be too hot, even if it seems that heat helps to better endure contractions. nine0003
So if there is a shower or jacuzzi bath in the delivery room, do not be shy and try this method of pain relief for contractions. The only thing is that the water should not be too hot, even if it seems that heat helps to better endure contractions. nine0003
Swinging on the ball
Until recently, fitball (rubber inflatable ball) in the rodblock was something outlandish, and today is found in many maternity hospitals. And if you find a fitball in your rodblock, be sure to use it. You can sit on the ball astride and swing, rotate the pelvis, spring, roll from side to side. You can also kneel down, lean on the ball with your hands and chest and sway back and forth. All these movements on the ball will relax the muscles, increase the mobility of the pelvic bones, improve the opening of the neck, and reduce the pain of contractions. And while the woman is sitting on the ball, her partner (usually her husband) can massage her neck area for additional relaxation.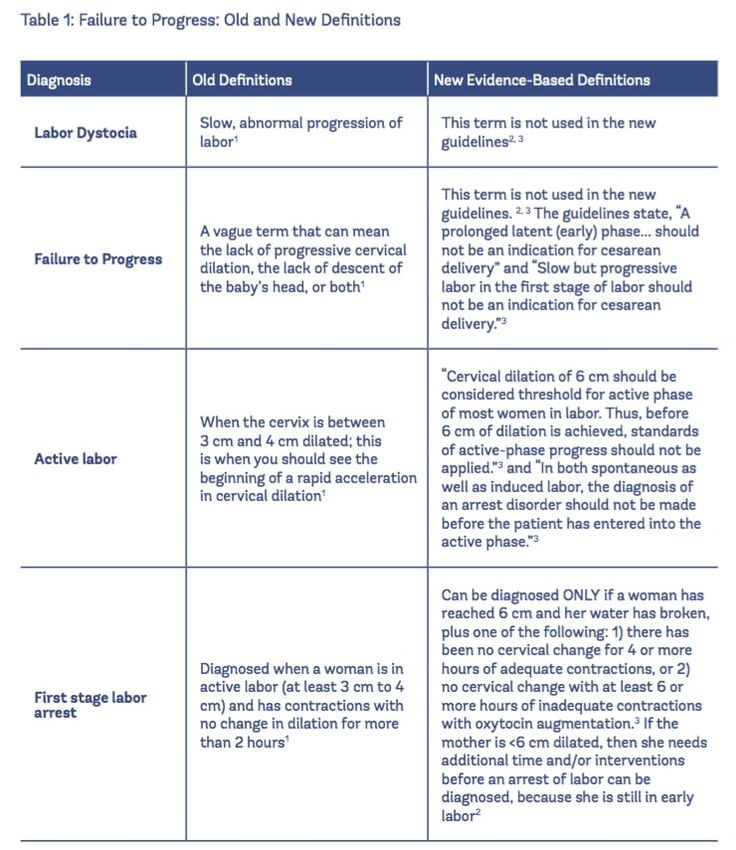 nine0003
nine0003
To be more comfortable, the ball should be soft, slightly deflated, and large, with a diameter of at least 75 cm.
We hang on a rope or wall bars
When the contractions become very strong and painful, you can take poses in which the stomach is, as it were, in a “suspended” state. Some advanced maternity hospitals have wall bars and ropes attached to the ceiling for this. During contraction, you can hang on them, as a result, the weight of the uterus will put less pressure on large blood vessels, and this will improve uteroplacental blood flow. In addition, in the “suspended” position, the load from the spine will be removed, which will also reduce pain. nine0003
Do not hang on a rope or a wall only if there is a desire to push, and the cervix has not yet opened and the efforts must be restrained.
Lying comfortably
If during childbirth a woman wants not to move, but, on the contrary, to lie down, then, of course, she can lie down.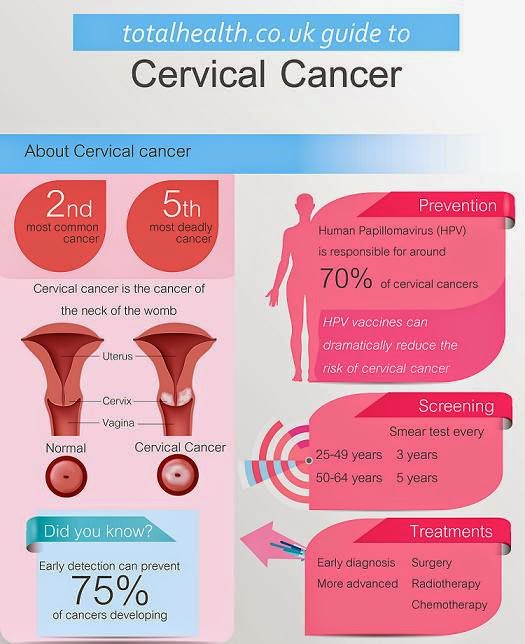 In modern maternity hospitals, instead of traditional ones, there are transforming beds: you can change their height, lower or raise the headboard or foot end, adjust the tilt level, push or push some part of the bed. There are also handrails in transforming beds (to use them to rest or even hang on them), and leg supports, and retractable pillows, and special backs - in general, everything in order to fit the bed under you and take it with it comfortable position. Moreover, this can be done without any physical effort - using the remote control. nine0003
In modern maternity hospitals, instead of traditional ones, there are transforming beds: you can change their height, lower or raise the headboard or foot end, adjust the tilt level, push or push some part of the bed. There are also handrails in transforming beds (to use them to rest or even hang on them), and leg supports, and retractable pillows, and special backs - in general, everything in order to fit the bed under you and take it with it comfortable position. Moreover, this can be done without any physical effort - using the remote control. nine0003
We use everything we have
In any road block, even if it is minimally equipped, you can still find something useful. For example, if during a fight you want to take a position with a support, you can lean forward and rest against something that turns up under your arm - a table, a headboard, a window sill. The main thing is that the support must be very stable. You can also get on all fours in the “cat pose” and focus on your hands, and to make it more convenient, put a pillow and a folded blanket under your chest. If you want to hang on something (and there is no rope or wall) and your husband will be nearby, you can use postures that allow you to transfer body weight to him: for example, hang on your husband’s neck. In general, it is worth showing imagination and adapting any item in the rodblock to your needs. nine0003
If you want to hang on something (and there is no rope or wall) and your husband will be nearby, you can use postures that allow you to transfer body weight to him: for example, hang on your husband’s neck. In general, it is worth showing imagination and adapting any item in the rodblock to your needs. nine0003
And don't be afraid to look stupid during childbirth. No one in the delivery room cares about how you move or lie down as long as it helps you get through your contractions, so calmly find your comfortable position.
Giving birth in an uncomfortable position is both difficult and inefficient. So memorize and rehearse some poses beforehand, and if there are any fixtures in the rodblock, try using them. Something of this will definitely help you to comfortably and easily survive childbirth.
When we move, take various postures, the blood supply to the uterus improves, as a result, it contracts better, and the cervix opens faster. In addition, uteroplacental blood flow improves, and therefore the baby does not suffer from hypoxia
strength to push
By clicking on the send button, I consent to the processing of personal data
Induction of labor or induction of labor
The purpose of this information material is to familiarize the patient with the induction of labor procedure and to provide information on how and why it is performed.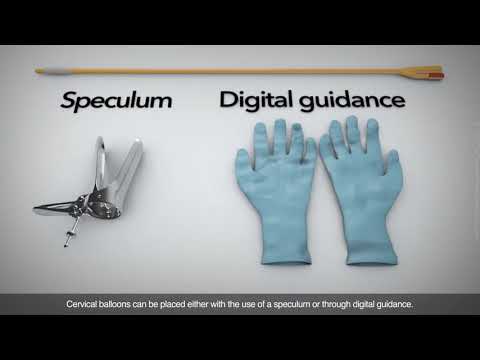
In most cases, labor begins between the 37th and 42nd weeks of pregnancy. Such births are called spontaneous. If medications or medical devices are used before the onset of spontaneous labor, then the terms "stimulated" or "induced" labor are used in this case. nine0003
Labor should be induced when further pregnancy is for some reason unsafe for the mother or baby and it is not possible to wait for spontaneous labor to begin.
The purpose of stimulation is to start labor by stimulating uterine contractions.
When inducing labor, the patient must be in the hospital so that both mother and baby can be closely monitored.
Labor induction methods
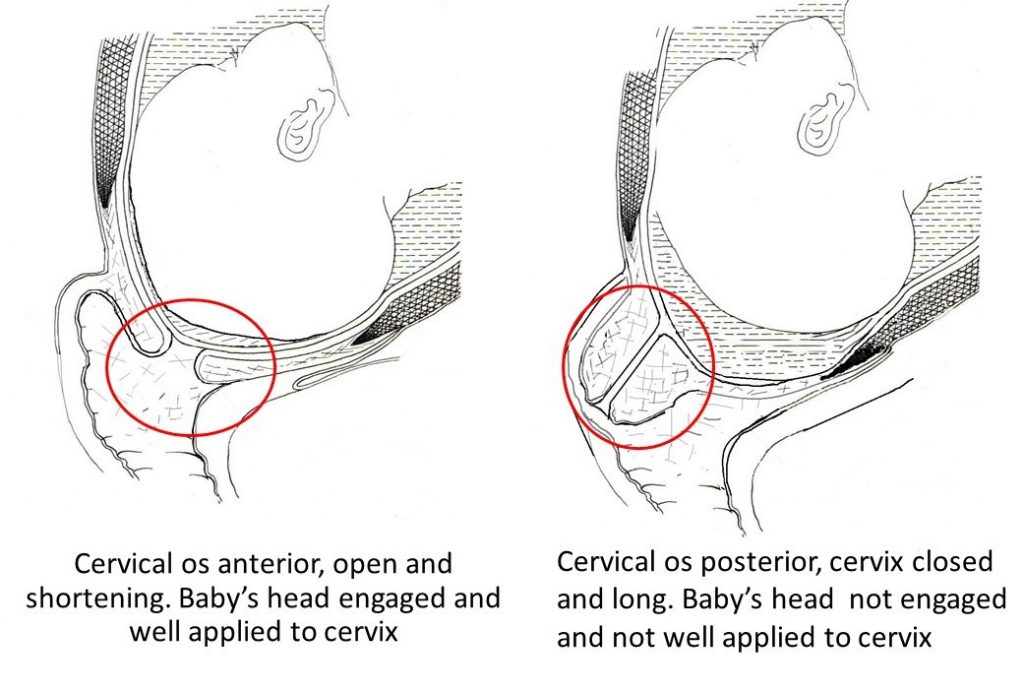
The choice of labor induction method depends on the maturity of the cervix in the patient, which is assessed using the Bishop scale (when viewed through the vagina, the position of the cervix, the degree of its dilatation, consistency, length, and the position of the presenting part of the fetus in the pelvic area are assessed).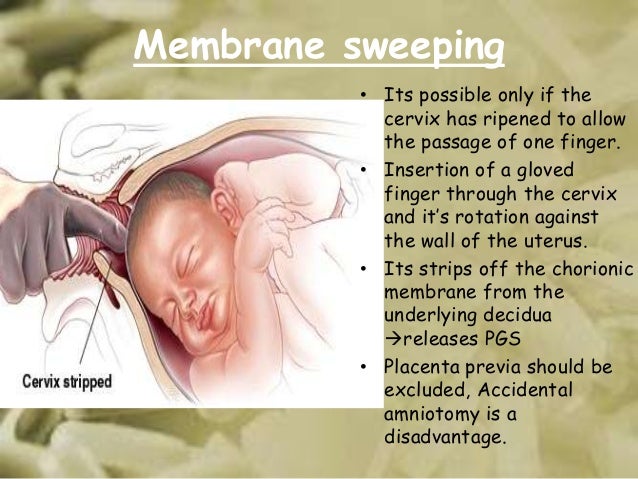 Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
The following methods are used to induce (stimulate) labor:
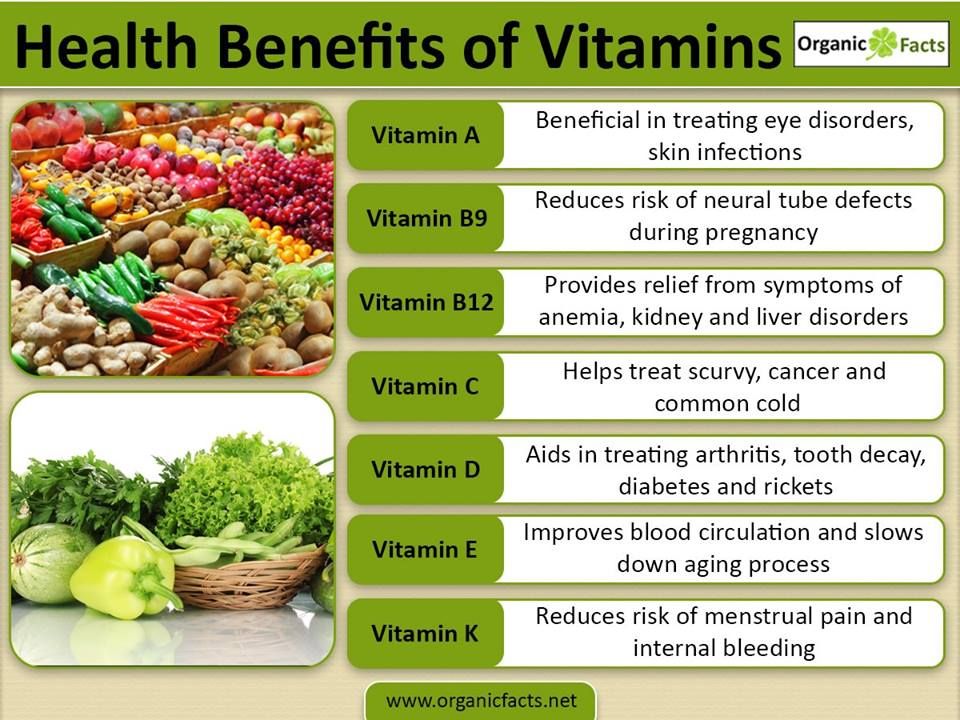
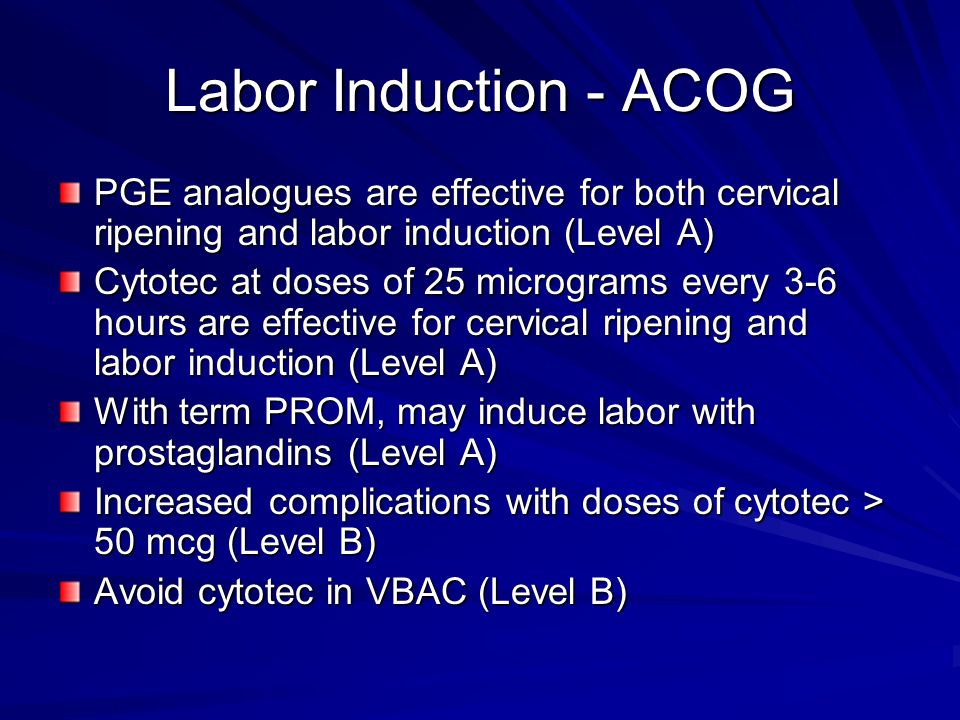
- Oral misoprostol is a drug that is a synthetic analogue of prostaglandins found in the body. It prepares the body for childbirth, under its action the cervix becomes softer and begins to open.
- Balloon Catheter - A small tube is placed in the cervix and the balloon attached to the end of the tube is filled with fluid to apply mechanical pressure to the cervix. When using this method, the cervix becomes softer and begins to open. The balloon catheter is kept inside until it spontaneously exits or until the next gynecological examination. nine0096
- Amniotomy or opening of the fetal bladder - in this case, during a gynecological examination, when the cervix has already sufficiently dilated, the fetal bladder is artificially opened. When the amniotic fluid breaks, spontaneous uterine contractions will begin, or intravenous medication may be used to stimulate them.
- Intravenously injected synthetic oxytocin - acts similarly to the hormone of the same name produced in the body. The drug is given by intravenous infusion when the cervix has already dilated (to support uterine contractions). The dose of the drug can be increased as needed to achieve regular uterine contractions. nine0096
When should labor be induced?
Labor induction is recommended when the benefits outweigh the risks.
Induction of labor may be indicated in the following cases:
- The patient has a comorbid condition complicating pregnancy (eg, high blood pressure, diabetes mellitus, preeclampsia, or some other condition).
- The duration of pregnancy is already exceeding the norm - the probability of intrauterine death of the fetus increases after the 42nd week of pregnancy. nine0096
- Fetal problems, eg, fetal development problems, abnormal amount of amniotic fluid, changes in fetal condition, various fetal disorders.
- If the amniotic fluid has broken and uterine contractions have not started within the next 24 hours, there is an increased risk of inflammation in both the mother and the fetus. This indication does not apply in case of preterm labor, when preparation of the baby's lungs with a special medicine is necessary before delivery. nine0096
- Intrauterine fetal death.
What are the risks associated with labor induction?
Labor induction is not usually associated with significant complications.
Occasionally, after receiving misoprostol, a patient may develop fever, chills, vomiting, diarrhea, and too frequent uterine contractions (tachysystole). In case of too frequent contractions to relax the uterus, the patient is injected intravenously relaxing muscles uterus medicine. It is not safe to use misoprostol if you have had a previous caesarean section as there is a risk of rupture of the uterine scar.