What does the pelvic girdle do
The Pelvic Girdle - Structure - Function - Assessment
- 1 Structure of the Pelvic Girdle
- 2 Functions of the Pelvis
- 3 The Greater and Lesser Pelvis
- 3.1 Pelvic Inlet
- 3.2 Pelvic Outlet
- 4 Adaptation for Childbirth
- 5 Clinical Relevance: Assessment of the Female Bony Pelvis
- 5.1 Obstetric Conjugate
- 5.2 Diagonal Conjugate
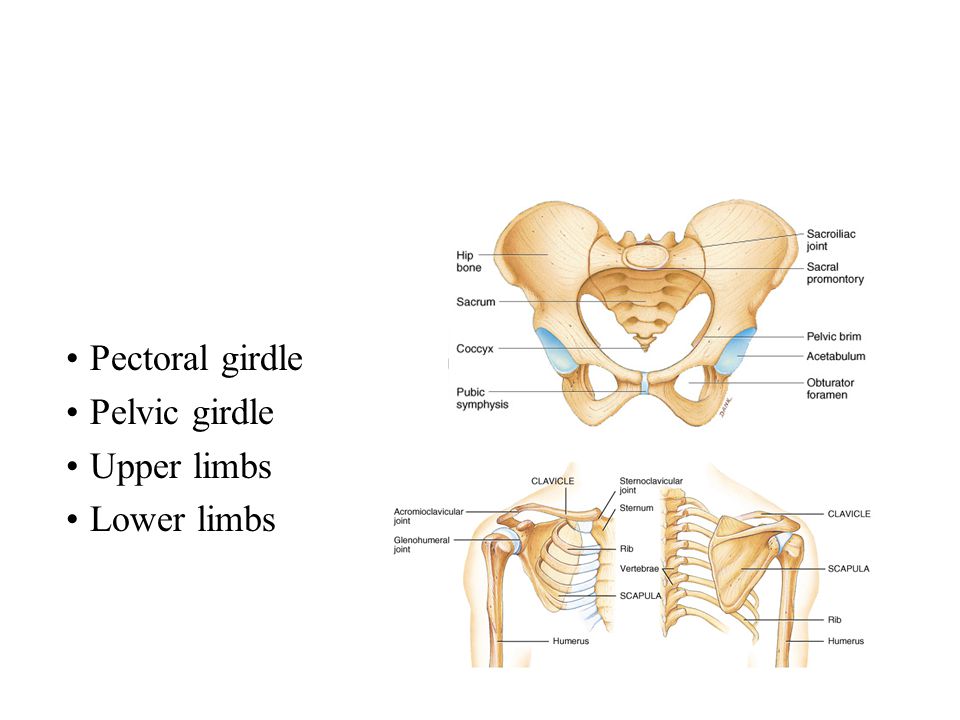
The pelvic girdle is a ring-like bony structure, located in the lower part of the trunk. It connects the axial skeleton to the lower limbs.
In this article, we shall look at the anatomy of the pelvic girdle – its bony landmarks, functions, and its clinical relevance.
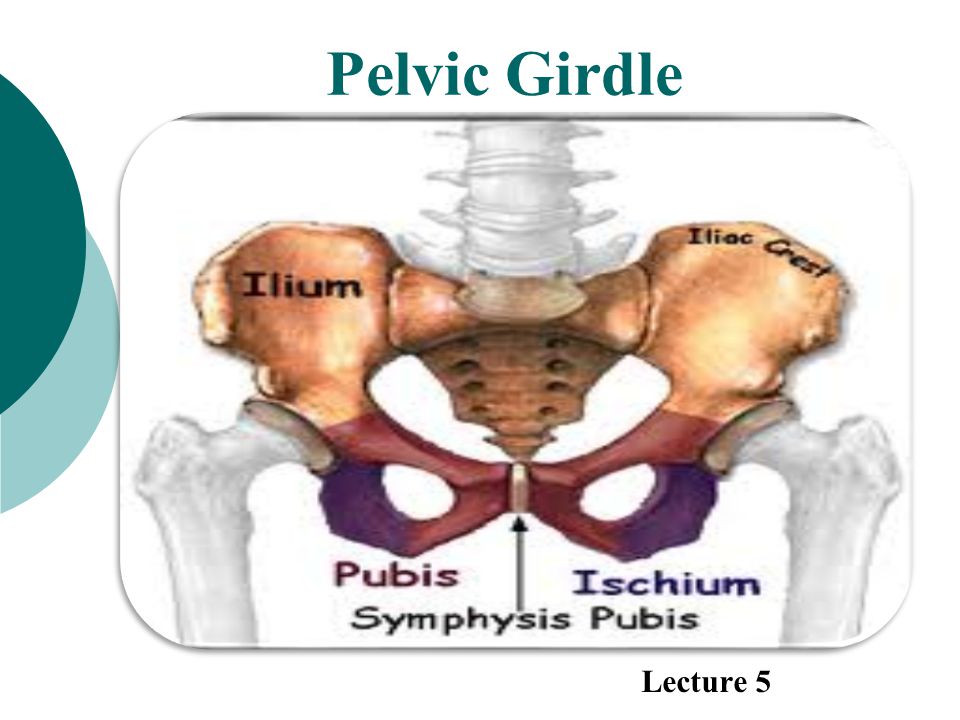
Structure of the Pelvic GirdleThe bony pelvis consists of the two hip bones (also known as innominate or pelvic bones), the sacrum and the coccyx.
There are four articulations within the pelvis:
- Sacroiliac joints (x2) – between the ilium of the hip bones, and the sacrum
- Sacrococcygeal symphysis – between the sacrum and the coccyx.
- Pubic symphysis – between the pubis bodies of the two hip bones.
Ligaments attach the lateral border of the sacrum to various bony landmarks on the bony pelvis to aid stability.
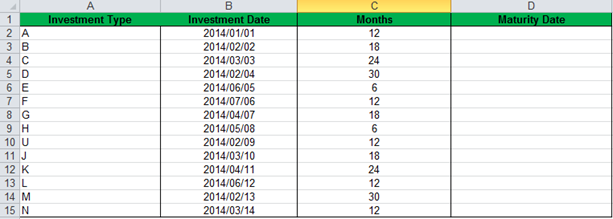
By TeachMeSeries Ltd (2022)
Fig 1 – The pelvic girdle is formed by the hip bones, sacrum and coccyx.
Functions of the PelvisThe strong and rigid pelvis is adapted to serve a number of roles in the human body. The main functions being:
- Transfer of weight from the upper axial skeleton to the lower appendicular components of the skeleton, especially during movement.
- Provides attachment for a number of muscles and ligaments used in locomotion.
- Contains and protects the abdominopelvic and pelvic viscera.
The osteology of the pelvic girdle allows the pelvic region to be divided into two:
- Greater pelvis (false pelvis) – located superiorly, it provides support of the lower abdominal viscera (such as the ileum and sigmoid colon).
 It has little obstetric relevance.
It has little obstetric relevance. - Lesser pelvis (true pelvis) – located inferiorly. Within the lesser pelvis reside the pelvic cavity and pelvic viscera.
The junction between the greater and lesser pelvis is known as the pelvic inlet. The outer bony edges of the pelvic inlet are called the pelvic brim.
By TeachMeSeries Ltd (2022)
Fig 2 – The greater and lesser pelvis. The lesser pelvis is the ‘true’ pelvis and contains the pelvic cavity.
Pelvic InletThe pelvic inlet marks the boundary between the greater pelvis and lesser pelvis. Its size is defined by its edge, the pelvic brim.
The borders of the pelvic inlet:
- Posterior – sacral promontory (the superior portion of the sacrum) and sacral wings (ala).
- Lateral – arcuate line on the inner surface of the ilium, and the pectineal line on the superior pubic ramus.
- Anterior – pubic symphysis.

The pelvic inlet determines the size and shape of the birth canal, with the prominent ridges a key site for attachment of muscle and ligaments.
Some alternative descriptive terminology can be used in describing the pelvic inlet:
- Linea terminalis – the combined pectineal line, arcuate line and sacral promontory.
- Iliopectineal line – the combined arcuate and pectineal lines. This represents the lateral border of the pelvic inlet.
By TeachMeSeries Ltd (2022)
Fig 3 – Looking down onto the pelvis, the borders of the pelvic brim.
Pelvic OutletThe pelvic outlet is located at the end of the lesser pelvis, and the beginning of the pelvic wall.
Its borders are:
- Posterior: The tip of the coccyx
- Lateral: The ischial tuberosities and the inferior margin of the sacrotuberous ligament
- Anterior: The pubic arch (the inferior border of the ischiopubic rami).

The angle beneath the pubic arch is known as the sub-pubic angle and is of a greater size in women.
By TeachMeSeries Ltd (2022)
Fig 4 – The borders of the pelvic outlet.
Adaptation for ChildbirthThe majority of women have a gynaecoid pelvis, as opposed to the male android pelvis. The slight differences in their structures creates a greater pelvic outlet, adapted to aid the process of childbirth. When comparing the two, the gynaecoid pelvis has:
- A wider and broader structure yet it is lighter in weight
- An oval-shaped inlet compared with the heart-shaped android pelvis.
- Less prominent ischial spines, allowing for a greater bispinous diameter
- A greater angled sub-pubic arch, more than 80-90 degrees.
- A sacrum which is shorter, more curved and with a less pronounced sacral promontory.
In addition to the bony adaptations, the sacrotuberous and sacrospinous ligaments can stretch under the influence of progesterone and increase the size of the outlet further.
By TeachMeSeries Ltd (2022)
Fig 5 – Gynaecoid pelvis vs the android pelvis.
Clinical Relevance: Assessment of the Female Bony Pelvis
The lesser pelvis is the bony canal through which the fetus has to pass during childbirth. It is therefore of great importance to determine the diameter of this canal and therefore the childbearing capacity of the mother.
The diameter can be determined by a pelvic examination or radiographically. There are two measurements that are of importance:
Obstetric ConjugateIn order to determine the narrowest fixed distance that the fetus would have to negotiate, the minimum antero-posterior diameter of the pelvic inlet is measured.
This distance is between the sacral promontory and the midpoint of the pubic symphysis (where the pubic bone is thickest) and is known as the obstetric conjugate (or true conjugate).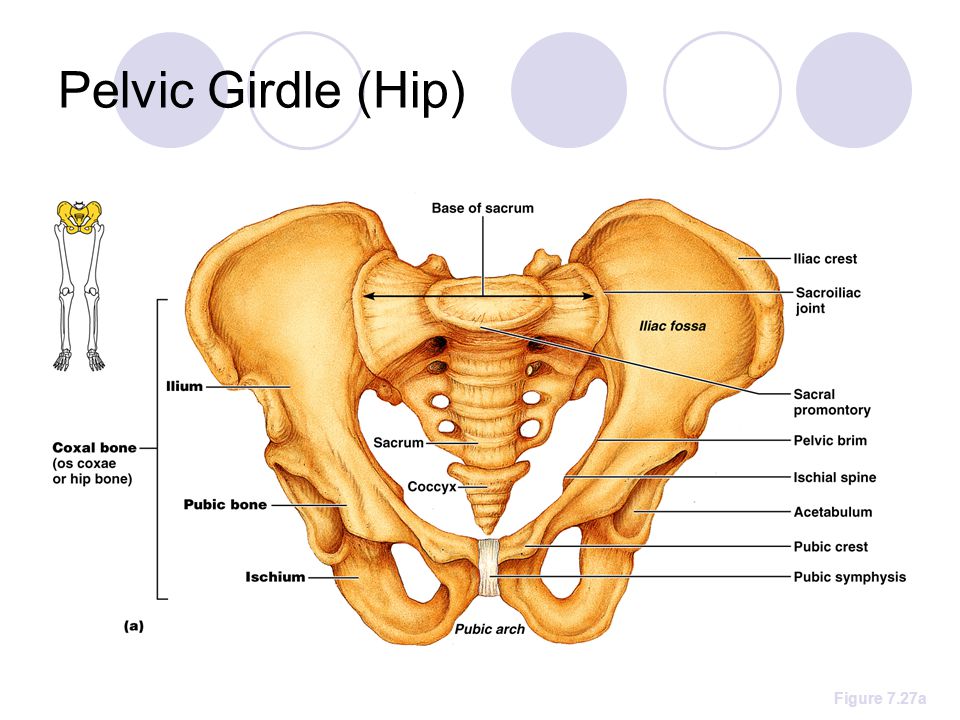 However, this measurement cannot be assessed clinically, due to the presence of the bladder.
However, this measurement cannot be assessed clinically, due to the presence of the bladder.
Diagonal Conjugate
The diagonal conjugate is the alternative, measuring from the inferior border of the pubic symphysis to the sacral promontory and can be measured manually via the vagina.
(To do this you use the tip of your middle finger to measure the sacral promontory and then using the other hand to mark the level of the inferior margin of the pubic symphysis on the examining hand. You then use the distance between the index finger and the pubic symphysis to measure the diagonal conjugate, ideally 11cm or greater)
In addition to measuring the diagonal conjugate, a mid-pelvis check is carried out. Here, the clinician is testing for straight side walls and measuring the bispinous diameter which is narrowest part of the pelvic canal. The width of the subpubic angle at the pelvic outlet can be determined by the distance between the ischial tuberosities.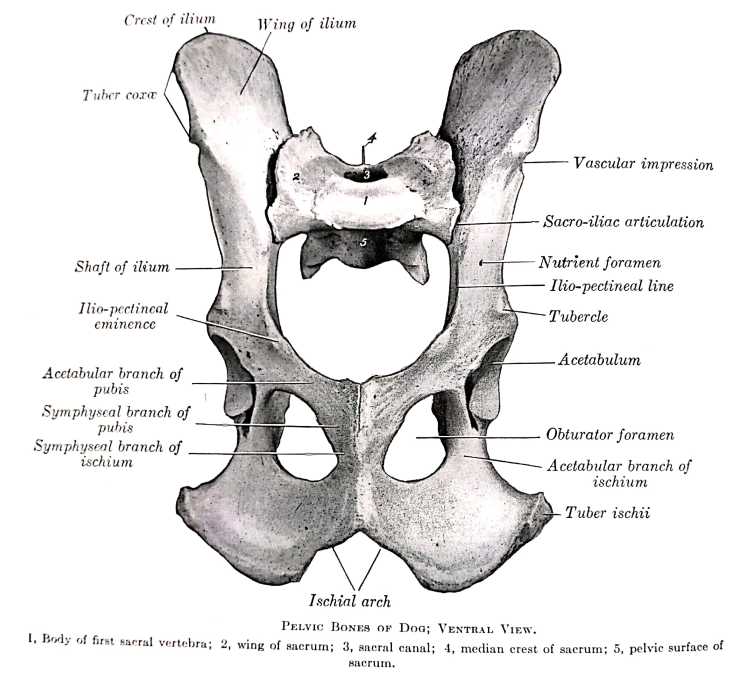
By TeachMeSeries Ltd (2022)
Fig 6 – Assessment of the female pelvis, via the diagonal conjugate
printPrint this Article
The Pelvic Girdle and Pelvis – Anatomy & Physiology
The Appendicular Skeleton
OpenStaxCollege
Learning Objectives
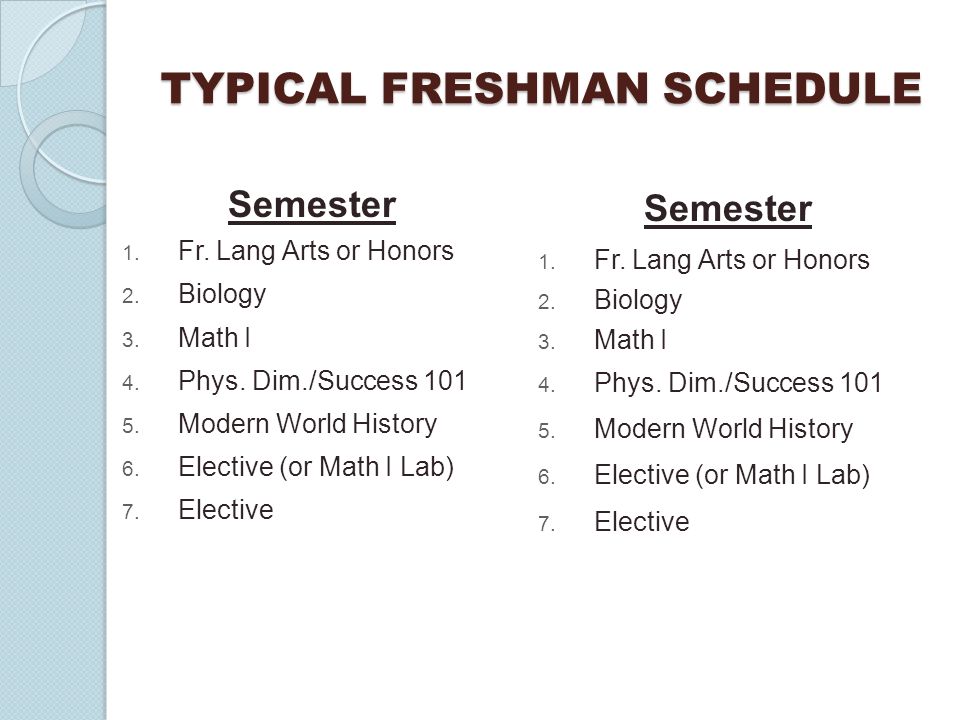
By the end of this section, you will be able to:
- Define the pelvic girdle and describe the bones and ligaments of the pelvis
- Explain the three regions of the hip bone and identify their bony landmarks
- Describe the openings of the pelvis and the boundaries of the greater and lesser pelvis
The pelvic girdle (hip girdle) is formed by a single bone, the hip bone or coxal bone (coxal = “hip”), which serves as the attachment point for each lower limb. Each hip bone, in turn, is firmly joined to the axial skeleton via its attachment to the sacrum of the vertebral column. The right and left hip bones also converge anteriorly to attach to each other. The bony pelvis is the entire structure formed by the two hip bones, the sacrum, and, attached inferiorly to the sacrum, the coccyx ([link]).
The bony pelvis is the entire structure formed by the two hip bones, the sacrum, and, attached inferiorly to the sacrum, the coccyx ([link]).
Unlike the bones of the pectoral girdle, which are highly mobile to enhance the range of upper limb movements, the bones of the pelvis are strongly united to each other to form a largely immobile, weight-bearing structure. This is important for stability because it enables the weight of the body to be easily transferred laterally from the vertebral column, through the pelvic girdle and hip joints, and into either lower limb whenever the other limb is not bearing weight. Thus, the immobility of the pelvis provides a strong foundation for the upper body as it rests on top of the mobile lower limbs.
Pelvis
The pelvic girdle is formed by a single hip bone. The hip bone attaches the lower limb to the axial skeleton through its articulation with the sacrum. The right and left hip bones, plus the sacrum and the coccyx, together form the pelvis.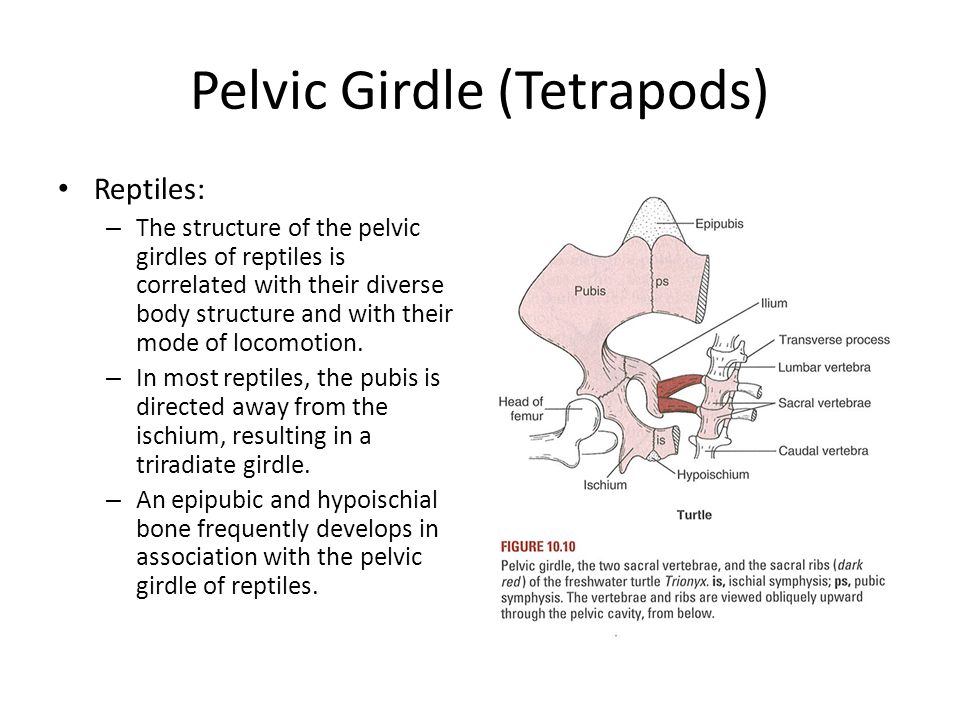
The hip bone, or coxal bone, forms the pelvic girdle portion of the pelvis. The paired hip bones are the large, curved bones that form the lateral and anterior aspects of the pelvis. Each adult hip bone is formed by three separate bones that fuse together during the late teenage years. These bony components are the ilium, ischium, and pubis ([link]). These names are retained and used to define the three regions of the adult hip bone.
The Hip Bone
The adult hip bone consists of three regions. The ilium forms the large, fan-shaped superior portion, the ischium forms the posteroinferior portion, and the pubis forms the anteromedial portion.
The ilium is the fan-like, superior region that forms the largest part of the hip bone. It is firmly united to the sacrum at the largely immobile sacroiliac joint (see [link]). The ischium forms the posteroinferior region of each hip bone. It supports the body when sitting. The pubis forms the anterior portion of the hip bone. The pubis curves medially, where it joins to the pubis of the opposite hip bone at a specialized joint called the pubic symphysis.
The pubis curves medially, where it joins to the pubis of the opposite hip bone at a specialized joint called the pubic symphysis.
Ilium
When you place your hands on your waist, you can feel the arching, superior margin of the ilium along your waistline (see [link]). This curved, superior margin of the ilium is the iliac crest. The rounded, anterior termination of the iliac crest is the anterior superior iliac spine. This important bony landmark can be felt at your anterolateral hip. Inferior to the anterior superior iliac spine is a rounded protuberance called the anterior inferior iliac spine. Both of these iliac spines serve as attachment points for muscles of the thigh. Posteriorly, the iliac crest curves downward to terminate as the posterior superior iliac spine. Muscles and ligaments surround but do not cover this bony landmark, thus sometimes producing a depression seen as a “dimple” located on the lower back. More inferiorly is the posterior inferior iliac spine.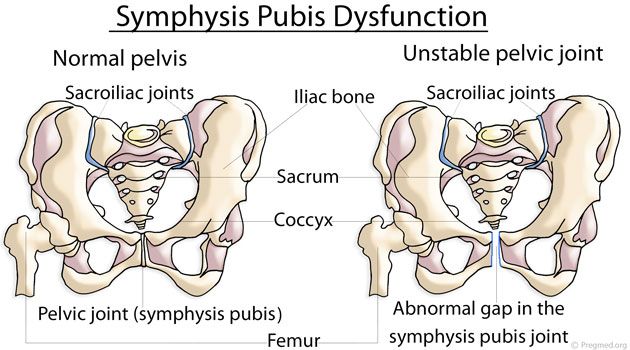 This is located at the inferior end of a large, roughened area called the auricular surface of the ilium. The auricular surface articulates with the auricular surface of the sacrum to form the sacroiliac joint. Both the posterior superior and posterior inferior iliac spines serve as attachment points for the muscles and very strong ligaments that support the sacroiliac joint.
This is located at the inferior end of a large, roughened area called the auricular surface of the ilium. The auricular surface articulates with the auricular surface of the sacrum to form the sacroiliac joint. Both the posterior superior and posterior inferior iliac spines serve as attachment points for the muscles and very strong ligaments that support the sacroiliac joint.
The shallow depression located on the anteromedial (internal) surface of the upper ilium is called the iliac fossa. The inferior margin of this space is formed by the arcuate line of the ilium, the ridge formed by the pronounced change in curvature between the upper and lower portions of the ilium. The large, inverted U-shaped indentation located on the posterior margin of the lower ilium is called the greater sciatic notch.
Ischium
The ischium forms the posterolateral portion of the hip bone (see [link]). The large, roughened area of the inferior ischium is the ischial tuberosity.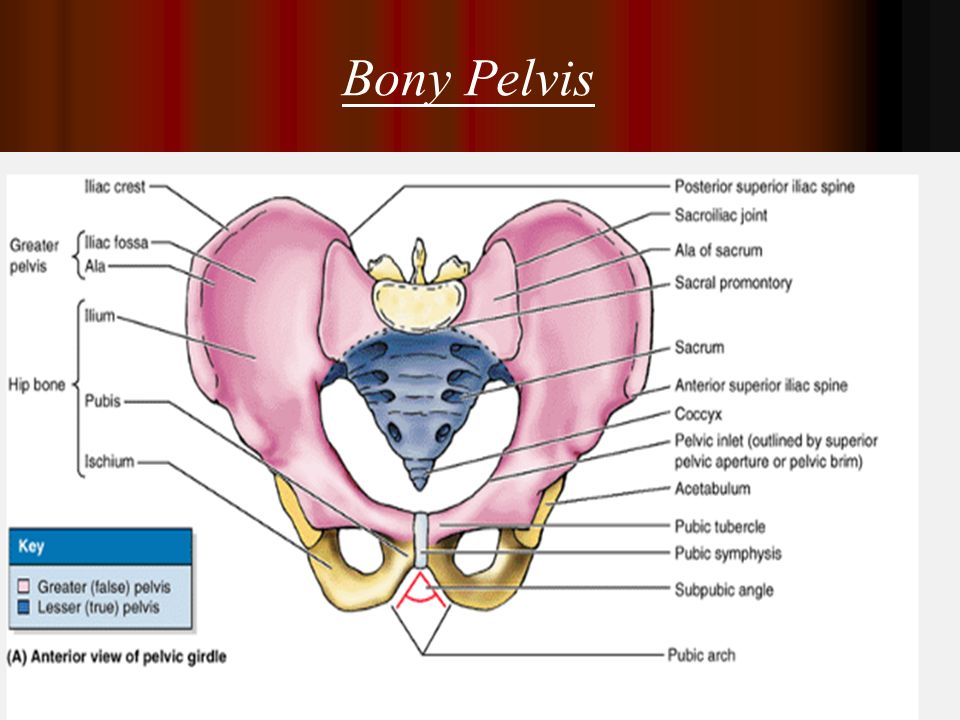 This serves as the attachment for the posterior thigh muscles and also carries the weight of the body when sitting. You can feel the ischial tuberosity if you wiggle your pelvis against the seat of a chair. Projecting superiorly and anteriorly from the ischial tuberosity is a narrow segment of bone called the ischial ramus. The slightly curved posterior margin of the ischium above the ischial tuberosity is the lesser sciatic notch. The bony projection separating the lesser sciatic notch and greater sciatic notch is the ischial spine.
This serves as the attachment for the posterior thigh muscles and also carries the weight of the body when sitting. You can feel the ischial tuberosity if you wiggle your pelvis against the seat of a chair. Projecting superiorly and anteriorly from the ischial tuberosity is a narrow segment of bone called the ischial ramus. The slightly curved posterior margin of the ischium above the ischial tuberosity is the lesser sciatic notch. The bony projection separating the lesser sciatic notch and greater sciatic notch is the ischial spine.
Pubis
The pubis forms the anterior portion of the hip bone (see [link]). The enlarged medial portion of the pubis is the pubic body. Located superiorly on the pubic body is a small bump called the pubic tubercle. The superior pubic ramus is the segment of bone that passes laterally from the pubic body to join the ilium. The narrow ridge running along the superior margin of the superior pubic ramus is the pectineal line of the pubis.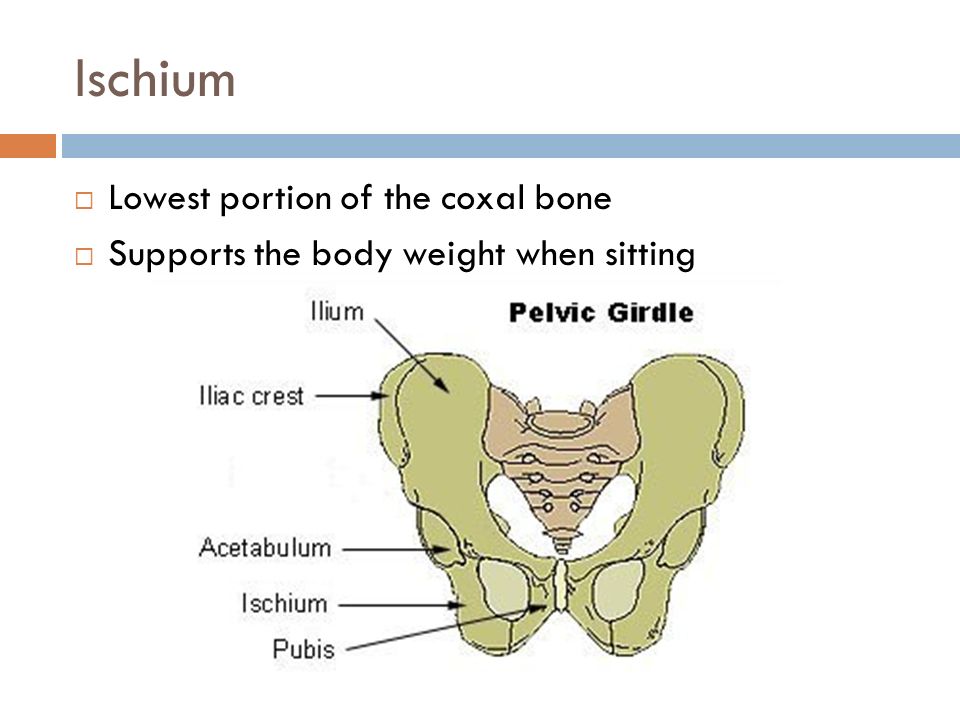
The pubic body is joined to the pubic body of the opposite hip bone by the pubic symphysis. Extending downward and laterally from the body is the inferior pubic ramus. The pubic arch is the bony structure formed by the pubic symphysis, and the bodies and inferior pubic rami of the adjacent pubic bones. The inferior pubic ramus extends downward to join the ischial ramus. Together, these form the single ischiopubic ramus, which extends from the pubic body to the ischial tuberosity. The inverted V-shape formed as the ischiopubic rami from both sides come together at the pubic symphysis is called the subpubic angle.
The pelvis consists of four bones: the right and left hip bones, the sacrum, and the coccyx (see [link]). The pelvis has several important functions. Its primary role is to support the weight of the upper body when sitting and to transfer this weight to the lower limbs when standing. It serves as an attachment point for trunk and lower limb muscles, and also protects the internal pelvic organs.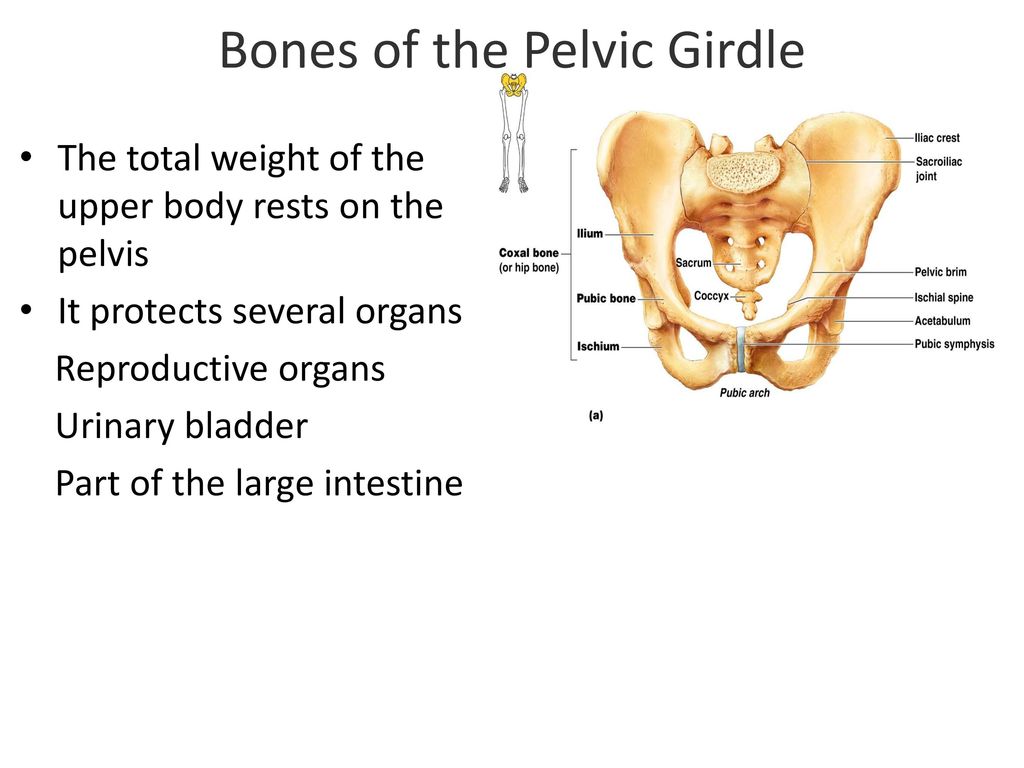 When standing in the anatomical position, the pelvis is tilted anteriorly. In this position, the anterior superior iliac spines and the pubic tubercles lie in the same vertical plane, and the anterior (internal) surface of the sacrum faces forward and downward.
When standing in the anatomical position, the pelvis is tilted anteriorly. In this position, the anterior superior iliac spines and the pubic tubercles lie in the same vertical plane, and the anterior (internal) surface of the sacrum faces forward and downward.
The three areas of each hip bone, the ilium, pubis, and ischium, converge centrally to form a deep, cup-shaped cavity called the acetabulum. This is located on the lateral side of the hip bone and is part of the hip joint. The large opening in the anteroinferior hip bone between the ischium and pubis is the obturator foramen. This space is largely filled in by a layer of connective tissue and serves for the attachment of muscles on both its internal and external surfaces.
Several ligaments unite the bones of the pelvis ([link]). The largely immobile sacroiliac joint is supported by a pair of strong ligaments that are attached between the sacrum and ilium portions of the hip bone. These are the anterior sacroiliac ligament on the anterior side of the joint and the posterior sacroiliac ligament on the posterior side.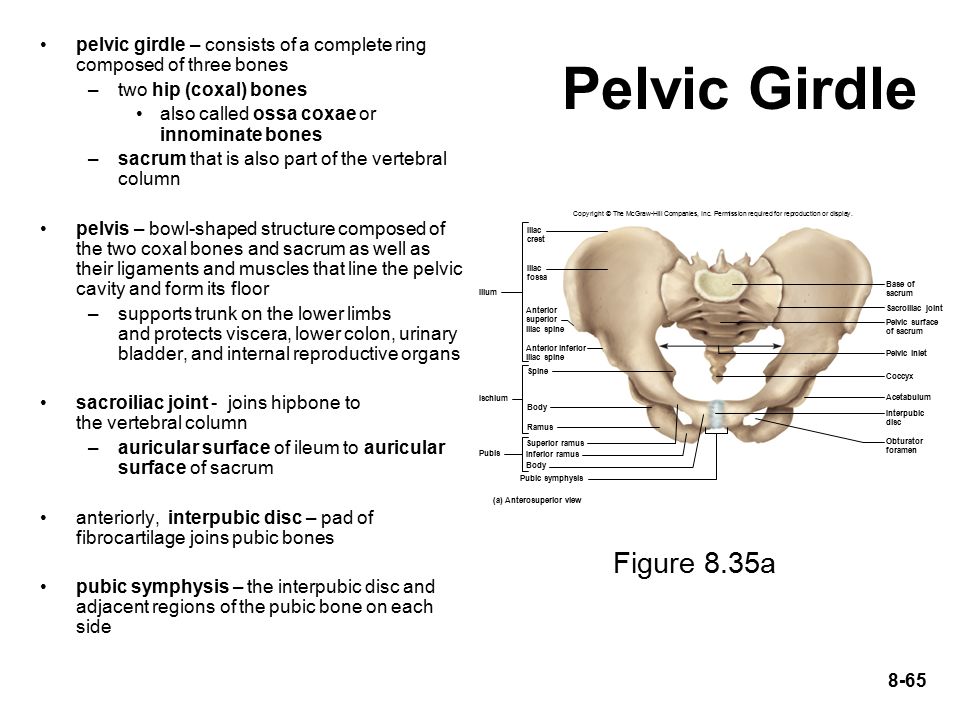 Also spanning the sacrum and hip bone are two additional ligaments. The sacrospinous ligament runs from the sacrum to the ischial spine, and the sacrotuberous ligament runs from the sacrum to the ischial tuberosity. These ligaments help to support and immobilize the sacrum as it carries the weight of the body.
Also spanning the sacrum and hip bone are two additional ligaments. The sacrospinous ligament runs from the sacrum to the ischial spine, and the sacrotuberous ligament runs from the sacrum to the ischial tuberosity. These ligaments help to support and immobilize the sacrum as it carries the weight of the body.
Ligaments of the Pelvis
The posterior sacroiliac ligament supports the sacroiliac joint. The sacrospinous ligament spans the sacrum to the ischial spine, and the sacrotuberous ligament spans the sacrum to the ischial tuberosity. The sacrospinous and sacrotuberous ligaments contribute to the formation of the greater and lesser sciatic foramens.
Watch this video for a 3-D view of the pelvis and its associated ligaments. What is the large opening in the bony pelvis, located between the ischium and pubic regions, and what two parts of the pubis contribute to the formation of this opening?
The sacrospinous and sacrotuberous ligaments also help to define two openings on the posterolateral sides of the pelvis through which muscles, nerves, and blood vessels for the lower limb exit.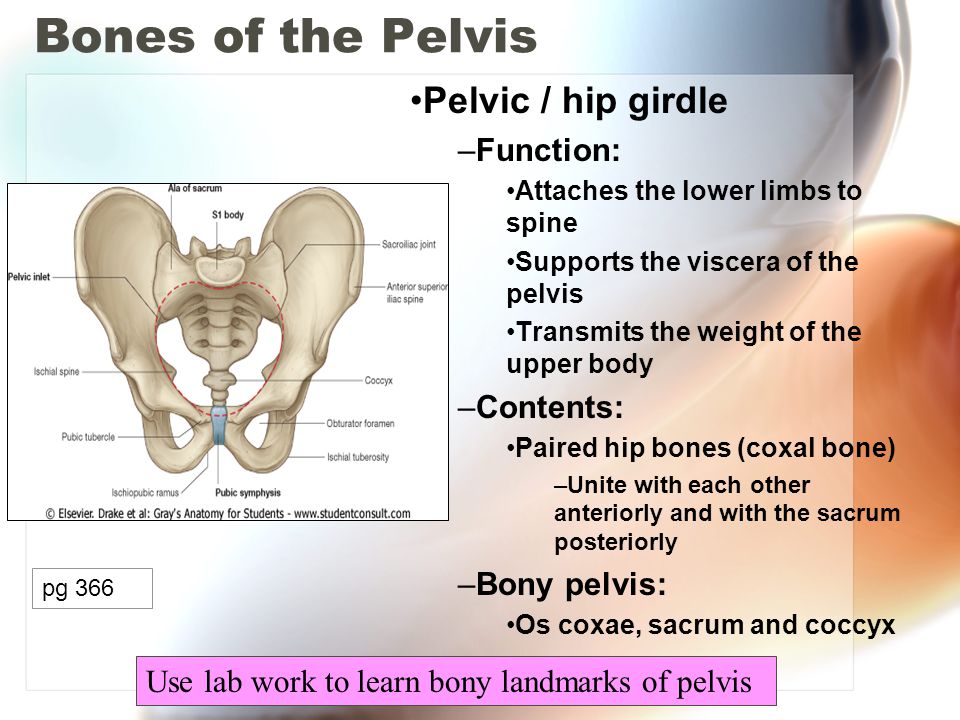 The superior opening is the greater sciatic foramen. This large opening is formed by the greater sciatic notch of the hip bone, the sacrum, and the sacrospinous ligament. The smaller, more inferior lesser sciatic foramen is formed by the lesser sciatic notch of the hip bone, together with the sacrospinous and sacrotuberous ligaments.
The superior opening is the greater sciatic foramen. This large opening is formed by the greater sciatic notch of the hip bone, the sacrum, and the sacrospinous ligament. The smaller, more inferior lesser sciatic foramen is formed by the lesser sciatic notch of the hip bone, together with the sacrospinous and sacrotuberous ligaments.
The space enclosed by the bony pelvis is divided into two regions ([link]). The broad, superior region, defined laterally by the large, fan-like portion of the upper hip bone, is called the greater pelvis (greater pelvic cavity; false pelvis). This broad area is occupied by portions of the small and large intestines, and because it is more closely associated with the abdominal cavity, it is sometimes referred to as the false pelvis. More inferiorly, the narrow, rounded space of the lesser pelvis (lesser pelvic cavity; true pelvis) contains the bladder and other pelvic organs, and thus is also known as the true pelvis. The pelvic brim (also known as the pelvic inlet) forms the superior margin of the lesser pelvis, separating it from the greater pelvis. The pelvic brim is defined by a line formed by the upper margin of the pubic symphysis anteriorly, and the pectineal line of the pubis, the arcuate line of the ilium, and the sacral promontory (the anterior margin of the superior sacrum) posteriorly. The inferior limit of the lesser pelvic cavity is called the pelvic outlet. This large opening is defined by the inferior margin of the pubic symphysis anteriorly, and the ischiopubic ramus, the ischial tuberosity, the sacrotuberous ligament, and the inferior tip of the coccyx posteriorly. Because of the anterior tilt of the pelvis, the lesser pelvis is also angled, giving it an anterosuperior (pelvic inlet) to posteroinferior (pelvic outlet) orientation.
Male and Female Pelvis
The female pelvis is adapted for childbirth and is broader, with a larger subpubic angle, a rounder pelvic brim, and a wider and more shallow lesser pelvic cavity than the male pelvis.
Comparison of the Female and Male Pelvis
The differences between the adult female and male pelvis relate to function and body size.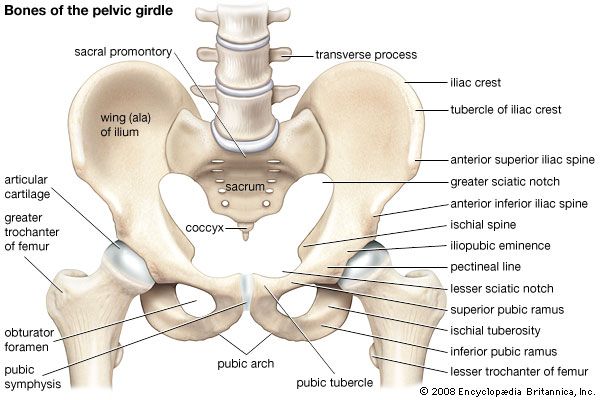 In general, the bones of the male pelvis are thicker and heavier, adapted for support of the male’s heavier physical build and stronger muscles. The greater sciatic notch of the male hip bone is narrower and deeper than the broader notch of females. Because the female pelvis is adapted for childbirth, it is wider than the male pelvis, as evidenced by the distance between the anterior superior iliac spines (see [link]). The ischial tuberosities of females are also farther apart, which increases the size of the pelvic outlet. Because of this increased pelvic width, the subpubic angle is larger in females (greater than 80 degrees) than it is in males (less than 70 degrees). The female sacrum is wider, shorter, and less curved, and the sacral promontory projects less into the pelvic cavity, thus giving the female pelvic inlet (pelvic brim) a more rounded or oval shape compared to males. The lesser pelvic cavity of females is also wider and more shallow than the narrower, deeper, and tapering lesser pelvis of males.
In general, the bones of the male pelvis are thicker and heavier, adapted for support of the male’s heavier physical build and stronger muscles. The greater sciatic notch of the male hip bone is narrower and deeper than the broader notch of females. Because the female pelvis is adapted for childbirth, it is wider than the male pelvis, as evidenced by the distance between the anterior superior iliac spines (see [link]). The ischial tuberosities of females are also farther apart, which increases the size of the pelvic outlet. Because of this increased pelvic width, the subpubic angle is larger in females (greater than 80 degrees) than it is in males (less than 70 degrees). The female sacrum is wider, shorter, and less curved, and the sacral promontory projects less into the pelvic cavity, thus giving the female pelvic inlet (pelvic brim) a more rounded or oval shape compared to males. The lesser pelvic cavity of females is also wider and more shallow than the narrower, deeper, and tapering lesser pelvis of males.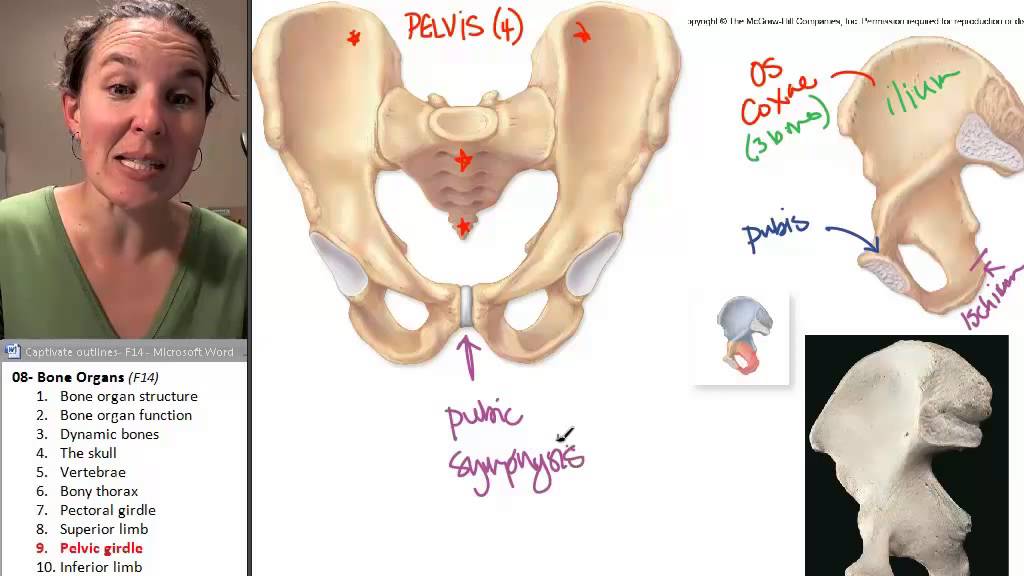 Because of the obvious differences between female and male hip bones, this is the one bone of the body that allows for the most accurate sex determination. [link] provides an overview of the general differences between the female and male pelvis.
Because of the obvious differences between female and male hip bones, this is the one bone of the body that allows for the most accurate sex determination. [link] provides an overview of the general differences between the female and male pelvis.
| Overview of Differences between the Female and Male Pelvis | ||
|---|---|---|
| Female pelvis | Male pelvis | |
| Pelvic weight | Bones of the pelvis are lighter and thinner | Bones of the pelvis are thicker and heavier |
| Pelvic inlet shape | Pelvic inlet has a round or oval shape | Pelvic inlet is heart-shaped |
| Lesser pelvic cavity shape | Lesser pelvic cavity is shorter and wider | Lesser pelvic cavity is longer and narrower |
| Subpubic angle | Subpubic angle is greater than 80 degrees | Subpubic angle is less than 70 degrees |
| Pelvic outlet shape | Pelvic outlet is rounded and larger | Pelvic outlet is smaller |
Career Connection
Forensic Pathology and Forensic Anthropology
A forensic pathologist (also known as a medical examiner) is a medically trained physician who has been specifically trained in pathology to examine the bodies of the deceased to determine the cause of death.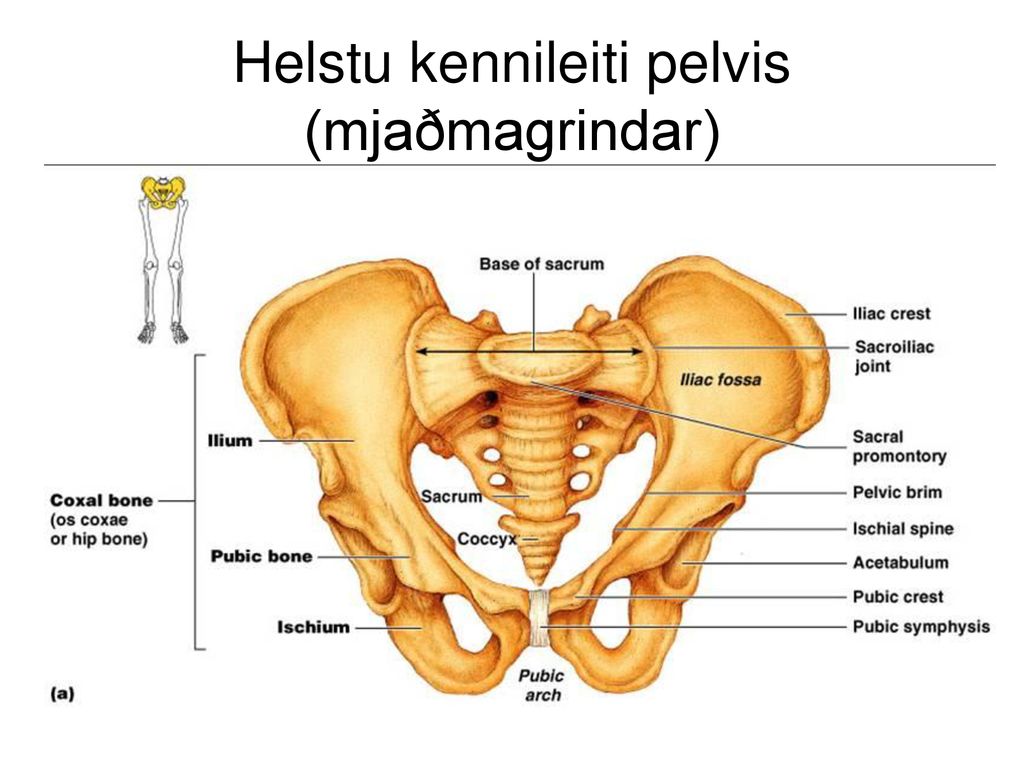 A forensic pathologist applies his or her understanding of disease as well as toxins, blood and DNA analysis, firearms and ballistics, and other factors to assess the cause and manner of death. At times, a forensic pathologist will be called to testify under oath in situations that involve a possible crime. Forensic pathology is a field that has received much media attention on television shows or following a high-profile death.
A forensic pathologist applies his or her understanding of disease as well as toxins, blood and DNA analysis, firearms and ballistics, and other factors to assess the cause and manner of death. At times, a forensic pathologist will be called to testify under oath in situations that involve a possible crime. Forensic pathology is a field that has received much media attention on television shows or following a high-profile death.
While forensic pathologists are responsible for determining whether the cause of someone’s death was natural, a suicide, accidental, or a homicide, there are times when uncovering the cause of death is more complex, and other skills are needed. Forensic anthropology brings the tools and knowledge of physical anthropology and human osteology (the study of the skeleton) to the task of investigating a death. A forensic anthropologist assists medical and legal professionals in identifying human remains. The science behind forensic anthropology involves the study of archaeological excavation; the examination of hair; an understanding of plants, insects, and footprints; the ability to determine how much time has elapsed since the person died; the analysis of past medical history and toxicology; the ability to determine whether there are any postmortem injuries or alterations of the skeleton; and the identification of the decedent (deceased person) using skeletal and dental evidence.
Due to the extensive knowledge and understanding of excavation techniques, a forensic anthropologist is an integral and invaluable team member to have on-site when investigating a crime scene, especially when the recovery of human skeletal remains is involved. When remains are bought to a forensic anthropologist for examination, he or she must first determine whether the remains are in fact human. Once the remains have been identified as belonging to a person and not to an animal, the next step is to approximate the individual’s age, sex, race, and height. The forensic anthropologist does not determine the cause of death, but rather provides information to the forensic pathologist, who will use all of the data collected to make a final determination regarding the cause of death.
The pelvic girdle, consisting of a hip bone, serves to attach a lower limb to the axial skeleton. The hip bone articulates posteriorly at the sacroiliac joint with the sacrum, which is part of the axial skeleton.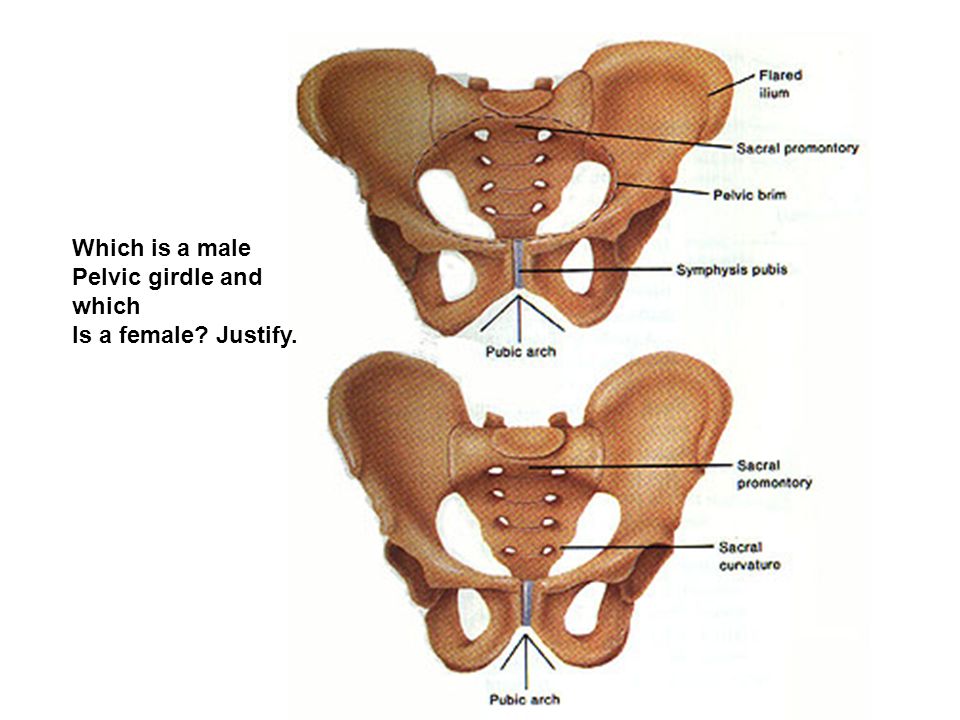 The right and left hip bones converge anteriorly and articulate with each other at the pubic symphysis. The combination of the hip bone, the sacrum, and the coccyx forms the pelvis. The pelvis has a pronounced anterior tilt. The primary function of the pelvis is to support the upper body and transfer body weight to the lower limbs. It also serves as the site of attachment for multiple muscles.
The right and left hip bones converge anteriorly and articulate with each other at the pubic symphysis. The combination of the hip bone, the sacrum, and the coccyx forms the pelvis. The pelvis has a pronounced anterior tilt. The primary function of the pelvis is to support the upper body and transfer body weight to the lower limbs. It also serves as the site of attachment for multiple muscles.
The hip bone consists of three regions: the ilium, ischium, and pubis. The ilium forms the large, fan-like region of the hip bone. The superior margin of this area is the iliac crest. Located at either end of the iliac crest are the anterior superior and posterior superior iliac spines. Inferior to these are the anterior inferior and posterior inferior iliac spines. The auricular surface of the ilium articulates with the sacrum to form the sacroiliac joint. The medial surface of the upper ilium forms the iliac fossa, with the arcuate line marking the inferior limit of this area. The posterior margin of the ilium has the large greater sciatic notch.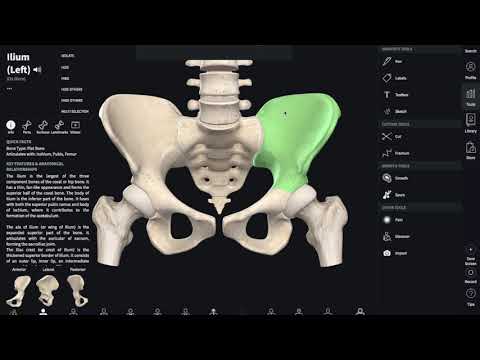
The posterolateral portion of the hip bone is the ischium. It has the expanded ischial tuberosity, which supports body weight when sitting. The ischial ramus projects anteriorly and superiorly. The posterior margin of the ischium has the shallow lesser sciatic notch and the ischial spine, which separates the greater and lesser sciatic notches.
The pubis forms the anterior portion of the hip bone. The body of the pubis articulates with the pubis of the opposite hip bone at the pubic symphysis. The superior margin of the pubic body has the pubic tubercle. The pubis is joined to the ilium by the superior pubic ramus, the superior surface of which forms the pectineal line. The inferior pubic ramus projects inferiorly and laterally. The pubic arch is formed by the pubic symphysis, the bodies of the adjacent pubic bones, and the two inferior pubic rami. The inferior pubic ramus joins the ischial ramus to form the ischiopubic ramus. The subpubic angle is formed by the medial convergence of the right and left ischiopubic rami.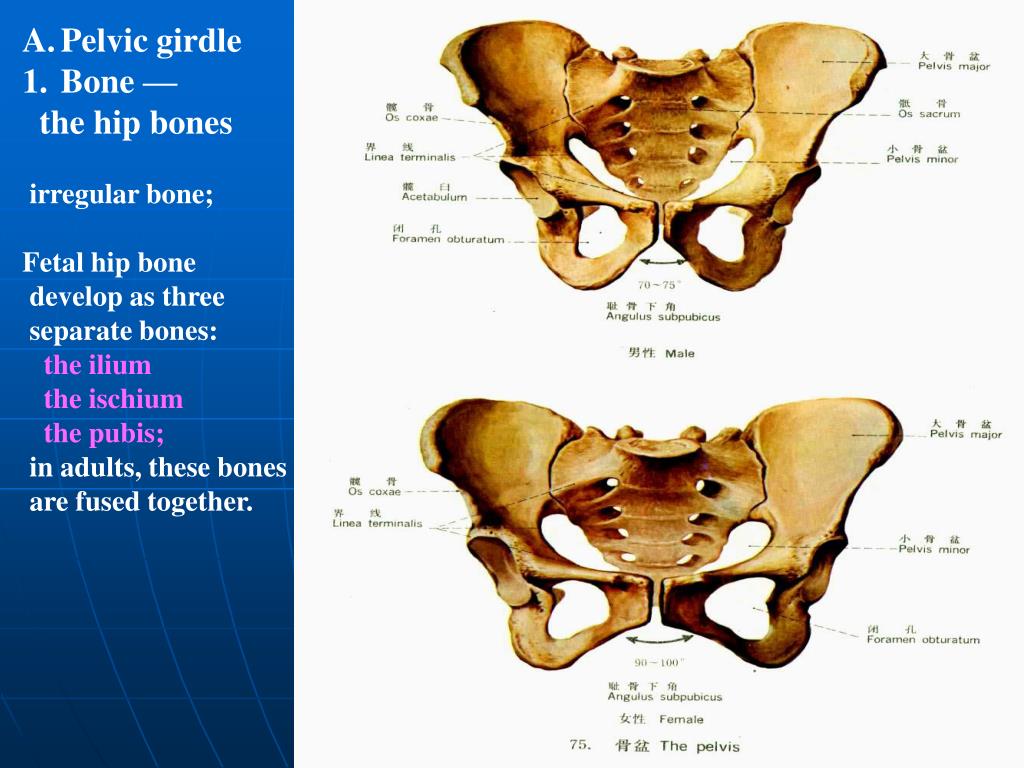
The lateral side of the hip bone has the cup-like acetabulum, which is part of the hip joint. The large anterior opening is the obturator foramen. The sacroiliac joint is supported by the anterior and posterior sacroiliac ligaments. The sacrum is also joined to the hip bone by the sacrospinous ligament, which attaches to the ischial spine, and the sacrotuberous ligament, which attaches to the ischial tuberosity. The sacrospinous and sacrotuberous ligaments contribute to the formation of the greater and lesser sciatic foramina.
The broad space of the upper pelvis is the greater pelvis, and the narrow, inferior space is the lesser pelvis. These areas are separated by the pelvic brim (pelvic inlet). The inferior opening of the pelvis is the pelvic outlet. Compared to the male, the female pelvis is wider to accommodate childbirth, has a larger subpubic angle, and a broader greater sciatic notch.
Watch this video for a 3-D view of the pelvis and its associated ligaments. What is the large opening in the bony pelvis, located between the ischium and pubic regions, and what two parts of the pubis contribute to the formation of this opening?
The obturator foramen is located between the ischium and the pubis.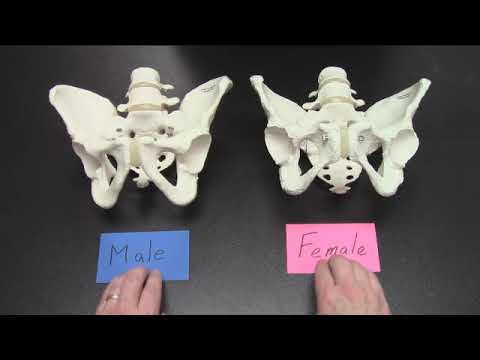 The superior and inferior pubic rami contribute to the boundaries of the obturator foramen.
The superior and inferior pubic rami contribute to the boundaries of the obturator foramen.
How many bones fuse in adulthood to form the hip bone?
- 2
- 3
- 4
- 5
B
Which component forms the superior part of the hip bone?
- ilium
- pubis
- ischium
- sacrum
A
Which of the following supports body weight when sitting?
- iliac crest
- ischial tuberosity
- ischiopubic ramus
- pubic body
B
The ischial spine is found between which of the following structures?
- inferior pubic ramus and ischial ramus
- pectineal line and arcuate line
- lesser sciatic notch and greater sciatic notch
- anterior superior iliac spine and posterior superior iliac spine
C
The pelvis ________.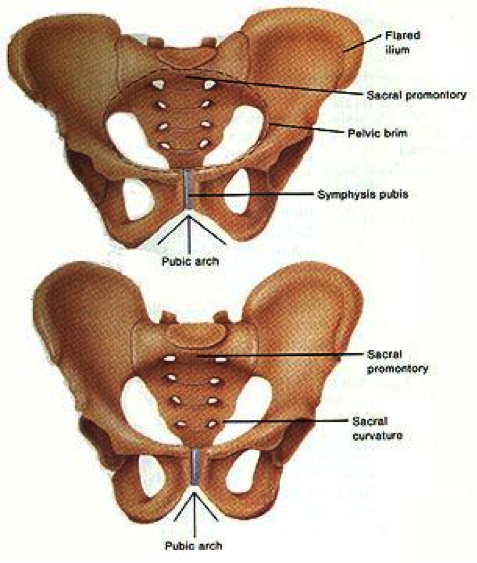
- has a subpubic angle that is larger in females
- consists of the two hip bones, but does not include the sacrum or coccyx
- has an obturator foramen, an opening that is defined in part by the sacrospinous and sacrotuberous ligaments
- has a space located inferior to the pelvic brim called the greater pelvis
A
Describe the articulations and ligaments that unite the four bones of the pelvis to each other.
The pelvis is formed by the combination of the right and left hip bones, the sacrum, and the coccyx. The auricular surfaces of each hip bone articulate with the auricular surface of the sacrum to form the sacroiliac joint. This joint is supported on either side by the strong anterior and posterior sacroiliac ligaments. The right and left hip bones converge anteriorly, where the pubic bodies articulate with each other to form the pubic symphysis joint. The sacrum is also attached to the hip bone by the sacrospinous ligament, which spans the sacrum to the ischial spine, and the sacrotuberous ligament, which runs from the sacrum to the ischial tuberosity.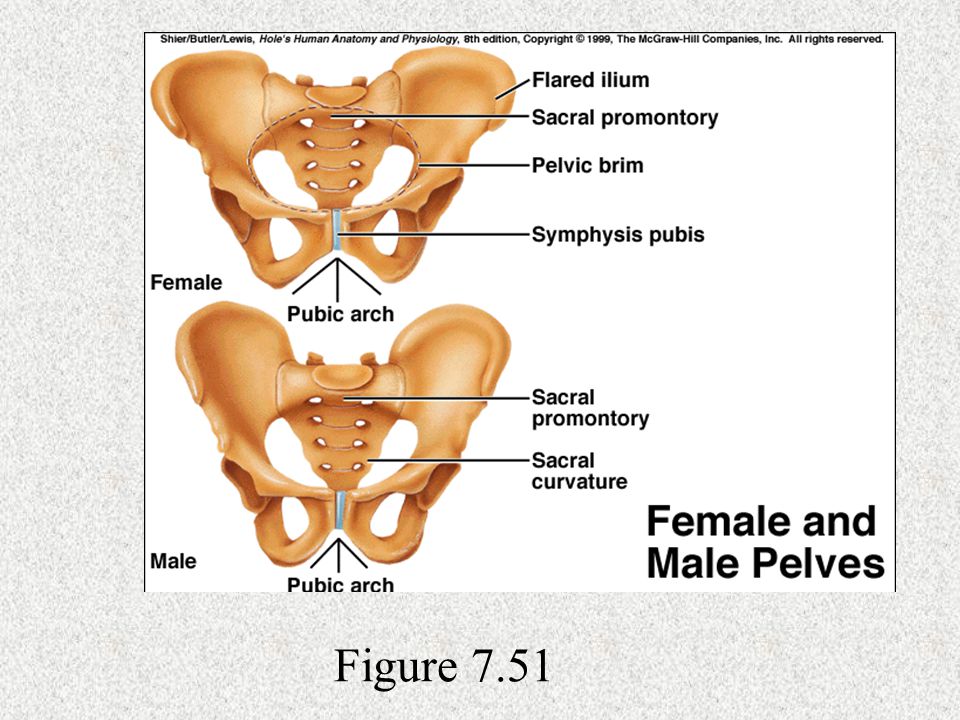 The coccyx is attached to the inferior end of the sacrum.
The coccyx is attached to the inferior end of the sacrum.
Discuss the ways in which the female pelvis is adapted for childbirth.
Compared to the male, the female pelvis is wider to accommodate childbirth. Thus, the female pelvis has greater distances between the anterior superior iliac spines and between the ischial tuberosities. The greater width of the female pelvis results in a larger subpubic angle. This angle, formed by the anterior convergence of the right and left ischiopubic rami, is larger in females (greater than 80 degrees) than in males (less than 70 degrees). The female sacral promontory does not project anteriorly as far as it does in males, which gives the pelvic brim (pelvic inlet) of the female a rounded or oval shape. The lesser pelvic cavity is wider and more shallow in females, and the pelvic outlet is larger than in males. Thus, the greater width of the female pelvis, with its larger pelvic inlet, lesser pelvis, and pelvic outlet, are important for childbirth because the baby must pass through the pelvis during delivery.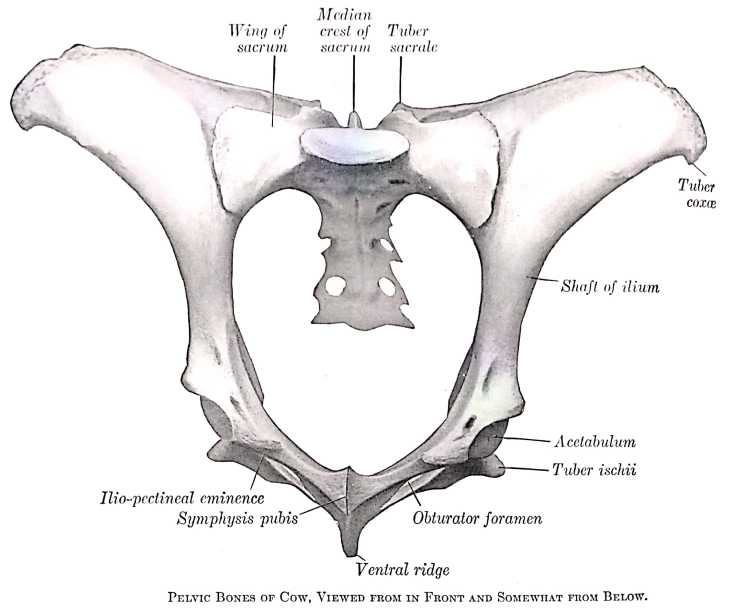
Glossary
- acetabulum
- large, cup-shaped cavity located on the lateral side of the hip bone; formed by the junction of the ilium, pubis, and ischium portions of the hip bone
- anterior inferior iliac spine
- small, bony projection located on the anterior margin of the ilium, below the anterior superior iliac spine
- anterior sacroiliac ligament
- strong ligament between the sacrum and the ilium portions of the hip bone that supports the anterior side of the sacroiliac joint
- anterior superior iliac spine
- rounded, anterior end of the iliac crest
- arcuate line of the ilium
- smooth ridge located at the inferior margin of the iliac fossa; forms the lateral portion of the pelvic brim
- auricular surface of the ilium
- roughened area located on the posterior, medial side of the ilium of the hip bone; articulates with the auricular surface of the sacrum to form the sacroiliac joint
- coxal bone
- hip bone
- greater pelvis
- (also, greater pelvic cavity or false pelvis) broad space above the pelvic brim defined laterally by the fan-like portion of the upper ilium
- greater sciatic foramen
- pelvic opening formed by the greater sciatic notch of the hip bone, the sacrum, and the sacrospinous ligament
- greater sciatic notch
- large, U-shaped indentation located on the posterior margin of the ilium, superior to the ischial spine
- hip bone
- coxal bone; single bone that forms the pelvic girdle; consists of three areas, the ilium, ischium, and pubis
- iliac crest
- curved, superior margin of the ilium
- iliac fossa
- shallow depression found on the anterior and medial surfaces of the upper ilium
- ilium
- superior portion of the hip bone
- inferior pubic ramus
- narrow segment of bone that passes inferiorly and laterally from the pubic body; joins with the ischial ramus to form the ischiopubic ramus
- ischial ramus
- bony extension projecting anteriorly and superiorly from the ischial tuberosity; joins with the inferior pubic ramus to form the ischiopubic ramus
- ischial spine
- pointed, bony projection from the posterior margin of the ischium that separates the greater sciatic notch and lesser sciatic notch
- ischial tuberosity
- large, roughened protuberance that forms the posteroinferior portion of the hip bone; weight-bearing region of the pelvis when sitting
- ischiopubic ramus
- narrow extension of bone that connects the ischial tuberosity to the pubic body; formed by the junction of the ischial ramus and inferior pubic ramus
- ischium
- posteroinferior portion of the hip bone
- lesser pelvis
- (also, lesser pelvic cavity or true pelvis) narrow space located within the pelvis, defined superiorly by the pelvic brim (pelvic inlet) and inferiorly by the pelvic outlet
- lesser sciatic foramen
- pelvic opening formed by the lesser sciatic notch of the hip bone, the sacrospinous ligament, and the sacrotuberous ligament
- lesser sciatic notch
- shallow indentation along the posterior margin of the ischium, inferior to the ischial spine
- obturator foramen
- large opening located in the anterior hip bone, between the pubis and ischium regions
- pectineal line
- narrow ridge located on the superior surface of the superior pubic ramus
- pelvic brim
- pelvic inlet; the dividing line between the greater and lesser pelvic regions; formed by the superior margin of the pubic symphysis, the pectineal lines of each pubis, the arcuate lines of each ilium, and the sacral promontory
- pelvic girdle
- hip girdle; consists of a single hip bone, which attaches a lower limb to the sacrum of the axial skeleton
- pelvic inlet
- pelvic brim
- pelvic outlet
- inferior opening of the lesser pelvis; formed by the inferior margin of the pubic symphysis, right and left ischiopubic rami and sacrotuberous ligaments, and the tip of the coccyx
- pelvis
- ring of bone consisting of the right and left hip bones, the sacrum, and the coccyx
- posterior inferior iliac spine
- small, bony projection located at the inferior margin of the auricular surface on the posterior ilium
- posterior sacroiliac ligament
- strong ligament spanning the sacrum and ilium of the hip bone that supports the posterior side of the sacroiliac joint
- posterior superior iliac spine
- rounded, posterior end of the iliac crest
- pubic arch
- bony structure formed by the pubic symphysis, and the bodies and inferior pubic rami of the right and left pubic bones
- pubic body
- enlarged, medial portion of the pubis region of the hip bone
- pubic symphysis
- joint formed by the articulation between the pubic bodies of the right and left hip bones
- pubic tubercle
- small bump located on the superior aspect of the pubic body
- pubis
- anterior portion of the hip bone
- sacroiliac joint
- joint formed by the articulation between the auricular surfaces of the sacrum and ilium
- sacrospinous ligament
- ligament that spans the sacrum to the ischial spine of the hip bone
- sacrotuberous ligament
- ligament that spans the sacrum to the ischial tuberosity of the hip bone
- subpubic angle
- inverted V-shape formed by the convergence of the right and left ischiopubic rami; this angle is greater than 80 degrees in females and less than 70 degrees in males
- superior pubic ramus
- narrow segment of bone that passes laterally from the pubic body to join the ilium
Pelvic girdle
Hip bone ( os coxae ) up to 16 years old consists of iliac, ischial and pubic bones, which then merge into one.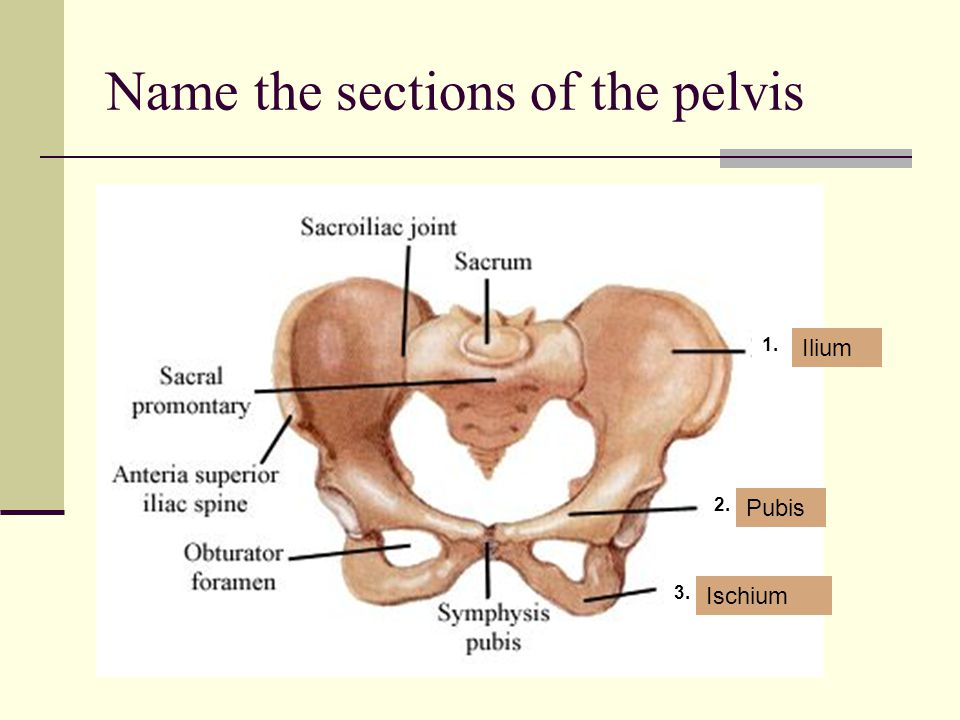 fusion sites their bodies - acetabulum , where includes the head of the femur.
fusion sites their bodies - acetabulum , where includes the head of the femur.
Iliac bone consists of a body and a wing, which ends with a comb. front - two protrusions: superior and inferior iliac awns, behind the same awns, but less expressed. Wing recess - iliac hole . The bone has an ear-shaped surface, gluteal and arcuate lines.
Ischial bone consists of body and branch , has ischial tuberosity and ischial tuberosity awn . Above and below the awn - a large and small clippings .
pubic bone has body , upper and lower branches . Together with the ischial branch bone limit obturator hole closed with connective tissue membrane.
Connections pelvis. Behind the bones are connected by a sedentary sacroiliac joint , flat in shape, firmly fixed bundles. Front - pubic articulation – symphysis (half-joint).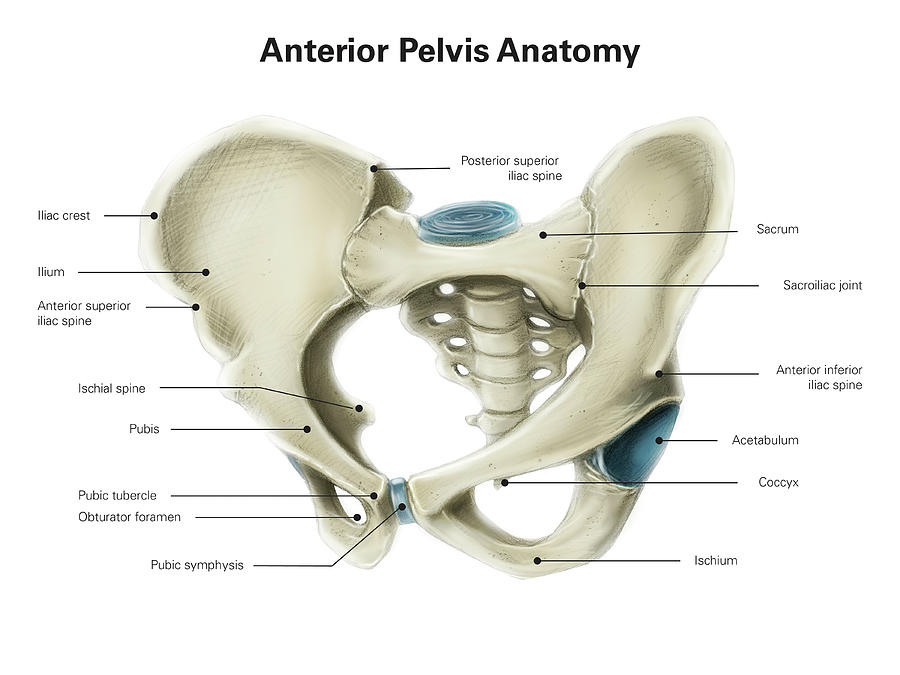 Own ligaments of the pelvis : sacrotuberous and sacrospinous. They form with ischial notches large and small ischial foramen through which muscles, blood vessels, nerves.
Own ligaments of the pelvis : sacrotuberous and sacrospinous. They form with ischial notches large and small ischial foramen through which muscles, blood vessels, nerves.
Taz formed by pelvic bones, sacrum and coccyx. Distinguish between large and small pelvis
Large the pelvis is formed by the wings of the ilium bones and is a support for internal abdominal organs.
Small pelvis - inside the large one. It distinguishes: entrance, exit and cavity. In the pelvis urinary organs and rectum are located intestine (rectum).
Sex differences : in women, the pelvis is wider than in men, in men, the cape protrudes into the cavity pelvis, in women the subpubic angle is obtuse, the cape does not protrude, the sacrum is wide, short (features of the birth canal).
B size matters in obstetrics pelvis.
Large pelvis:
-
spinous distance = 26 cm (between the front superior iliac spines)
d. spinarum
-
ridge distance = 29 cm (between remote iliac crest points) d. cristarum
-
spit distance = 31 cm (between skewers thigh bones) d. trochanterica
-
straight outer dimension = 21 cm (between the top edge of the symphysis and fossa of the lumbosacral joints)
Small pelvis:
-
external conjugate = 20 cm (from symphysis to junction V lumbar vertebra with sacrum)
-
diagonal conjugate = 12.5-13 cm (from the bottom edge symphysis to the cape - with vaginal research)
-
gynecological conjugate = 10.5-11 cm (the size of the outer conjugates - 9-10 cm or diagonal - 2 cm = 10.5 cm)
-
straight pelvic outlet size = 10 cm (lower edge of symphysis to apex coccyx)
Femoral bone ( femur ) most long tubular bone. Distinguish body, proximal and distal epiphyses. Ball head facing to the medial side. Below - the neck, under her large and small skewers, behind - intertrochanteric ridge. The body is located with a bulge anteriorly. Along the back surface - rough line. At the distal end - lateral and medial condyles, laterally above them - epicondyles with supracondylar fossa. Above the fossa is the popliteal surface. The condyles articulate with the tibial bone.
Distinguish body, proximal and distal epiphyses. Ball head facing to the medial side. Below - the neck, under her large and small skewers, behind - intertrochanteric ridge. The body is located with a bulge anteriorly. Along the back surface - rough line. At the distal end - lateral and medial condyles, laterally above them - epicondyles with supracondylar fossa. Above the fossa is the popliteal surface. The condyles articulate with the tibial bone.
Patella ( patella ) - bone, included in the tendon of the quadriceps thigh muscles involved in the formation knee joint.
Bones lower leg: tibia and fibula.
Tibial bone ( tibia ) has body and two ends. Upper - medial and lateral condyle with intercondylar elevation. On the outside lateral condyle - articular head articulation platform fibula. trihedral body shape, with a protruding front edge, at the top passes into tuberosity.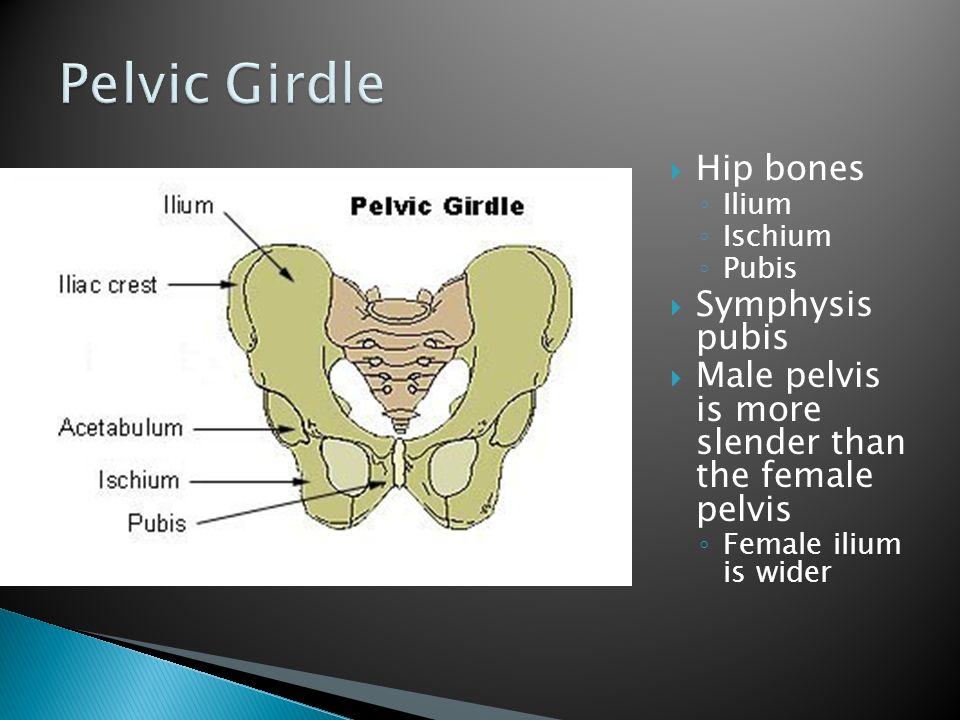 On the the lower end is the medial malleolus. On the lateral side - articular platform for articulation with the fibula bone, from below - a surface for articulation with the talus.
On the the lower end is the medial malleolus. On the lateral side - articular platform for articulation with the fibula bone, from below - a surface for articulation with the talus.
fibula bone ( fibula ) fine, located outside of the tibia bones. The top end is the head articulates with the tibia. The body is triangular. The lower end is thickened ( lateral malleolus ), adjacent to talus outside. Between big and fibula - interosseous membrane.
Bones feet ( ossa pedis ) bones of the tarsus, metatarsus and phalanges fingers.
Bones tarsus: talus, calcaneus, cuboid, navicular and three cuneiform. These are short spongy bones. Ramming bone together with the bones of the lower leg forms ankle. The heel bone articulates with talar joint.
Bones metatarsus - five short tubular bones. Consists of base, body and heads.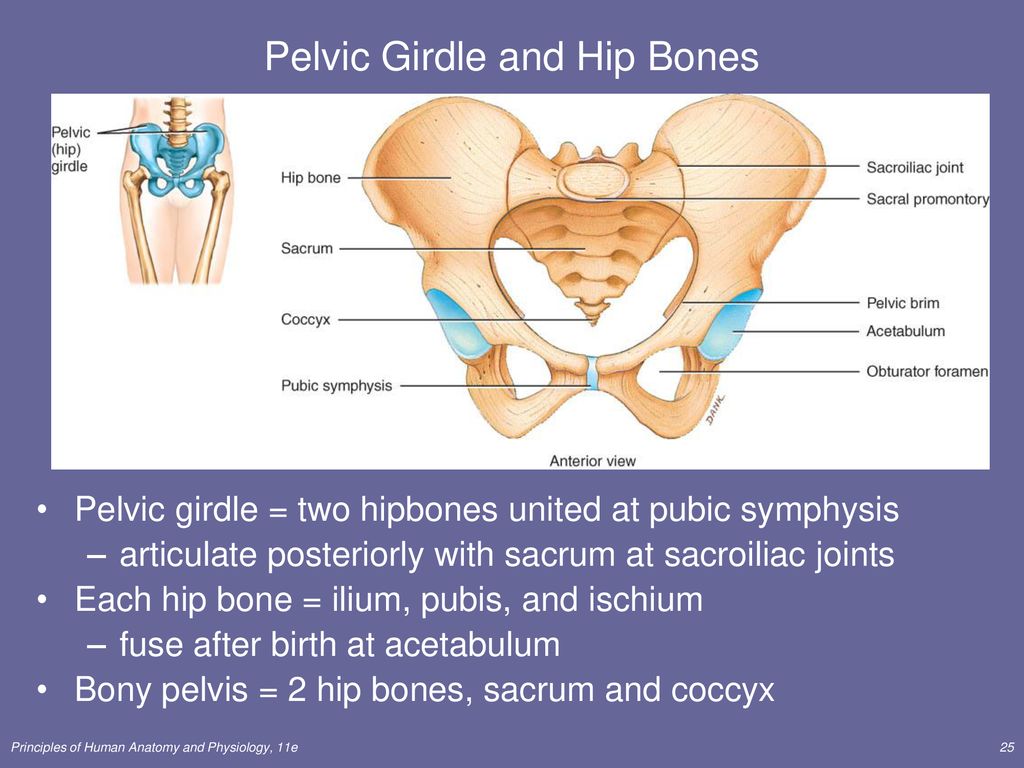 They articulate with the tarsus and phalanges of the fingers.
They articulate with the tarsus and phalanges of the fingers.
Fingers legs, as on the hand have three phalanges, except for the first (in him two).
Foot features conditioned the role of the supporting apparatus in the vertical body position. The foot performs support and spring function. Longitudinal spine feet are almost at right angles to the axis of the leg and thigh. The bones of the foot form transverse and longitudinal vaults facing concavity towards the sole, and convexity - to the rear of the foot (relies only on the tubercle calcaneus and metatarsal heads). The outer edge of the foot is lower (support arch), internal raised (spring vault).
Connections bones of the free lower limb
Hip joint formed acetabulum and femoral head bones. By the edge of the cavity is the articular lip. it spherical joint, reinforced with ligaments:
-
iliofemoral - inhibits extension, retention vertical position of the body;
-
pubic capsular and ischiocapsular come from superior branch of the pubic bone and body sciatic, weaving into the articular capsule, attached to a large and small spit;
-
bundle femoral head - inside the cavity joint.
 It carries nerves and blood vessels to head of the femur. movements any.
It carries nerves and blood vessels to head of the femur. movements any.
Knee joint formed femoral tibial bone and patella. In the joint cavity - menisci between the condyles of the femur and tibia. outer edge the meniscus is thickened and fused with the capsule. Attached by ligaments to the intercondylar elevation of the tibia. The anterior edges of the meniscus are connected cross link. Menisci - shock absorbers. Inside the cavity - front and posterior cruciate ligaments - connects the femur and tibia bones. Synovial membrane of the capsule forms a series of synovial bags, which communicate with the joint cavity. The most large - patella bag . Joint strengthen strong lateral ligaments. Movements: flexion, extension, small rotation.
Ankle joint formed lower leg bones and ram bone, reinforced with ligaments from the lower leg passing to the talus, scaphoid and heel bones. The articular bag is thin.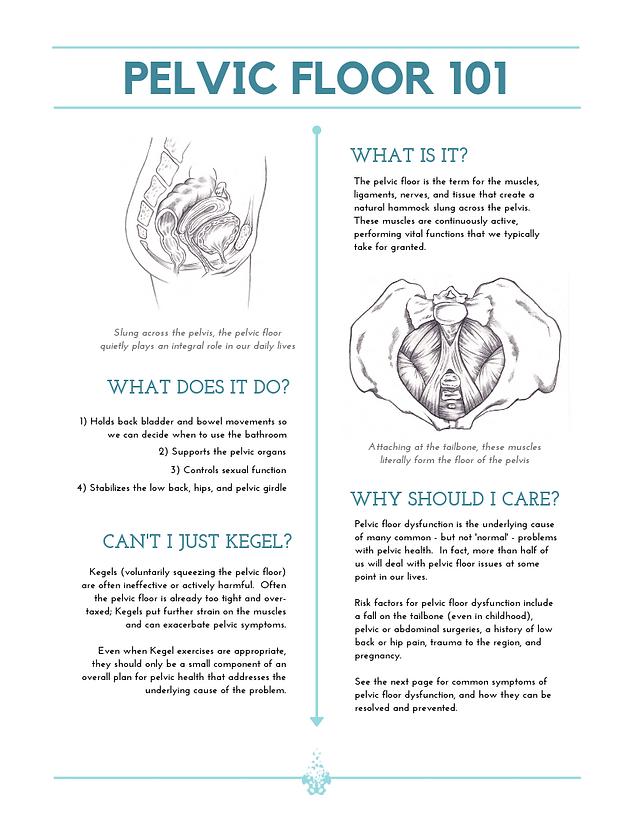 Movements: flexion and extension of the foot, slight abduction and adduction of the feet.
Movements: flexion and extension of the foot, slight abduction and adduction of the feet.
Joints and foot ligaments:
-
articulation (Chopart joint) combines talonavicular and calcaneocuboid. These joints are strengthened by the forked ligament on the back of the foot.
-
Tarsus-metatarsals joints (Lisfranc joint) - from the rear and soles - ligaments.
-
Set The feet are reinforced with muscles and ligaments. Basic - long sole bundle comes from the calcaneus fusiform to the base of all metatarsal bones and to the cuboid.
lecture No. 5
Pelvic tilt - treatment, symptoms, causes, diagnosis
The pelvis is one of the most important, although sometimes overlooked, parts of the skeleton.
The pelvis is shaped like a basket with a tip and contains many vital organs, including the intestines and bladder.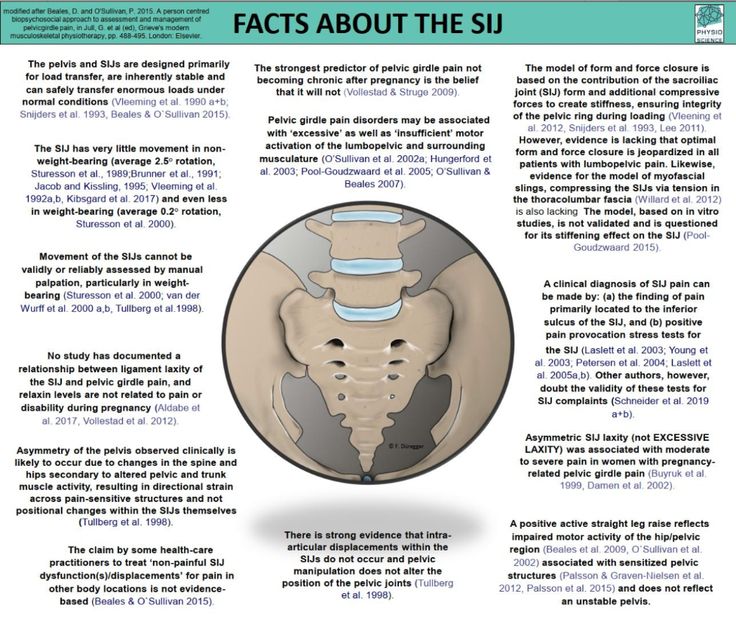 In addition, the pelvis is in the center of gravity of the skeleton. If the body is compared to a pencil balancing horizontally on a finger, its point of balance (center of gravity) will be the pelvis.
In addition, the pelvis is in the center of gravity of the skeleton. If the body is compared to a pencil balancing horizontally on a finger, its point of balance (center of gravity) will be the pelvis.
It is therefore clear that the position of the pelvis has a great influence on posture. This is the same as if the central block in the tower is displaced, in which case all blocks above the displacement are at risk of falling. And if you compare the central unit with a box, then the tilt can lead to the box falling out. Similar mechanisms take place when the pelvis is tilted, and the contents of the pelvis are shifted forward. As a result, there is a protruding abdomen and bulging of the buttocks. Since the pelvis is the junction of the upper and lower torso, it plays a key role in body movement and balance. The pelvic bones support the most important supporting part of the body - the spine. In addition, the pelvis allows the lower limbs and torso to move in a coordinated manner (in tandem).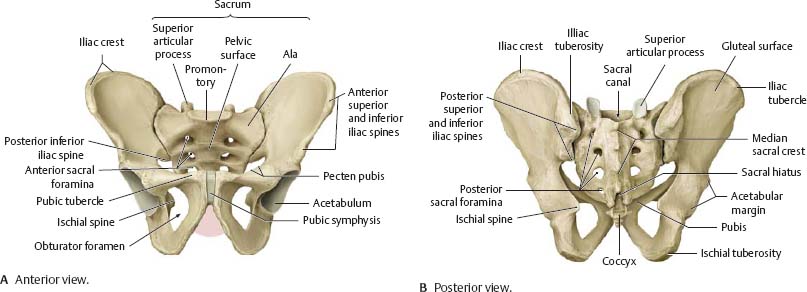 When the pelvis is in a normal position, various movements are possible, twisting, tilting and movement biomechanics are balanced and the distribution of load vectors is even. Displacement (skew) of the pelvis from normal positions causes dysfunctional disorders of the spine, as there is a change in the axis of distribution of loads during movement. For example, if there is an axle shift in a car, then the wheels wear out quickly. Something similar happens in the spine, there are leverage effects and excessive load on certain points, which lead to rapid wear of the structures of the spine. Therefore, often the main cause of pain in the back and neck is a change in the position of the pelvis (displacement, distortion). A change in position changes biomechanics, which can lead to degenerative changes in the spine, to disc herniation, scoliosis, osteoarthritis, spinal canal stenosis, sciatica, etc. Pelvic tilt also leads to pain and dysfunction in the neck, neck pain radiating to the shoulders, arms, contributes to the development of carpal tunnel syndrome and other problems in the limbs.
When the pelvis is in a normal position, various movements are possible, twisting, tilting and movement biomechanics are balanced and the distribution of load vectors is even. Displacement (skew) of the pelvis from normal positions causes dysfunctional disorders of the spine, as there is a change in the axis of distribution of loads during movement. For example, if there is an axle shift in a car, then the wheels wear out quickly. Something similar happens in the spine, there are leverage effects and excessive load on certain points, which lead to rapid wear of the structures of the spine. Therefore, often the main cause of pain in the back and neck is a change in the position of the pelvis (displacement, distortion). A change in position changes biomechanics, which can lead to degenerative changes in the spine, to disc herniation, scoliosis, osteoarthritis, spinal canal stenosis, sciatica, etc. Pelvic tilt also leads to pain and dysfunction in the neck, neck pain radiating to the shoulders, arms, contributes to the development of carpal tunnel syndrome and other problems in the limbs.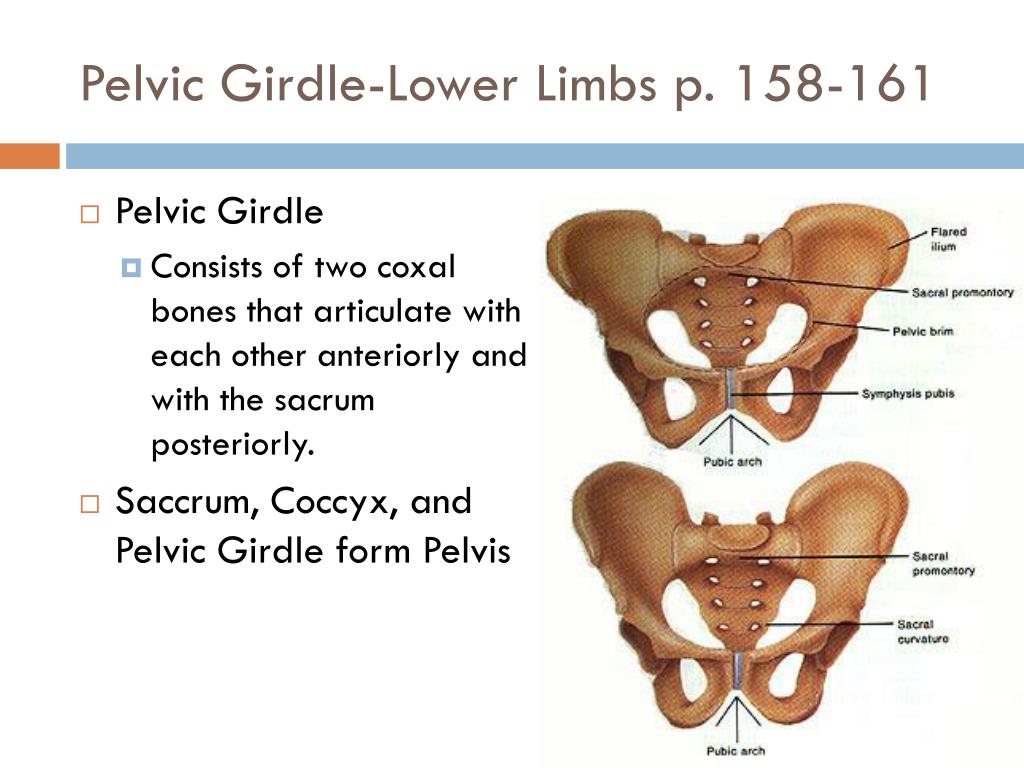
Causes of misalignment (displacement) of the pelvis
First of all, misalignment of the pelvis is caused by a normal muscle imbalance. Technology is developing very quickly and a sedentary lifestyle is one of the main reasons for the development of imbalance, because our body requires a certain amount of movement that it does not receive. Prolonged sitting and low physical activity are sufficient conditions for the development of muscle imbalances leading to pelvic tilt and, as a result, the appearance of dysfunctional disorders in the spine and the occurrence of back pain.
Accidents and injuries are common causes of pelvic tilt , such as side impact, heavy lifting while twisting, falling to one side, carrying heavy loads from the side, such as carrying a child on the hip or carrying a heavy bag constantly on one shoulder. In women, the pelvis is less stable from birth than in men, since a certain flexibility and elasticity of the pelvic structures is necessary for the normal course of pregnancy and childbirth. Therefore, pregnancy is often the main cause of pelvic displacement in women.
Therefore, pregnancy is often the main cause of pelvic displacement in women.
Injury to the pelvic muscles is the most common cause of misalignment. Injured muscles tend to thicken and shift in order to protect the surrounding structures. If the muscles in the pelvic area, such as the sacrum, are damaged, then the tightening of the muscles will lead to an effect on the ligaments attached to the pelvis and joints. As a result, structures such as the sacroiliac joints will also have a certain disposition. Muscle compaction after damage persists until the muscle is fully restored and during this period of time the pelvis remains in an abnormal position.
Differences in leg length can also cause pelvic tilt and in such cases the tilt can be from right to left or vice versa. But the displacement can also be forward or backward, or it can be twisting of the pelvis.
Many conditions can lead to muscle spasms that cause pelvic twist. Disc herniation can cause muscle spasm of an adaptive nature and, in turn, antalgic scoliosis with functional pelvic tilt . Active people often experience tension in the calf muscles, which in turn creates tension around the pelvis. Surgery such as hip replacement can also cause the pelvis to reposition itself.
Active people often experience tension in the calf muscles, which in turn creates tension around the pelvis. Surgery such as hip replacement can also cause the pelvis to reposition itself.
Since the pelvis is one of the most stressed areas of the body due to movement and weight support, movements that cause pain and stiffness are a clear indicator of pelvic alignment problems. Back pain in particular is a common indicator of pelvic tilt . In addition to participation in the movement in the pelvic cavity are: part of the digestive organs, nerves, blood vessels, reproductive organs. Therefore, in addition to back pain, there may be other symptoms, such as numbness, tingling, bladder and bowel problems, or reproductive problems. Most often, changes in the following muscles lead to pelvic disposition:
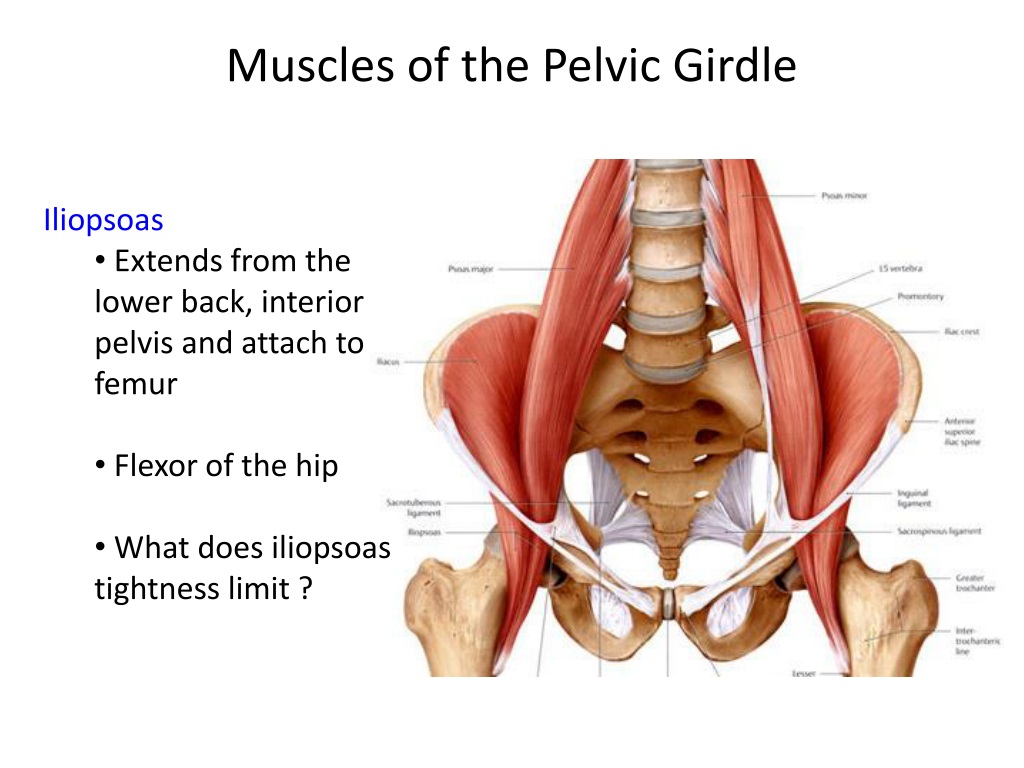
M. Psoas major (lumbar muscle) anatomically can lead to extension and flexion of the hip, which leads to an anterior displacement of the pelvis.
M.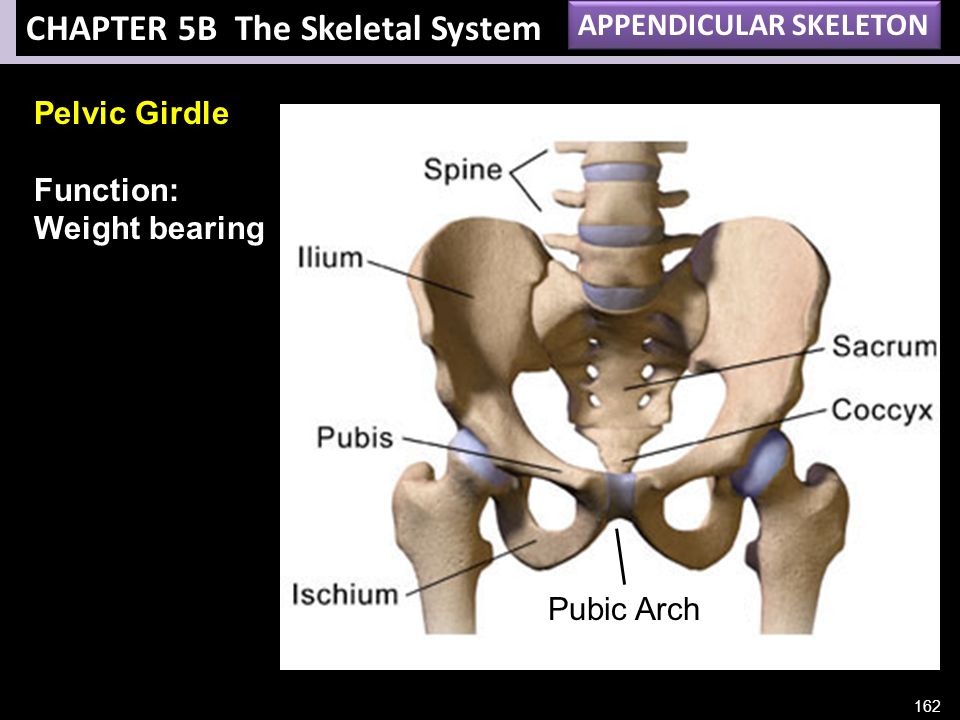 Quadriceps (quadriceps), especially the rectus muscle, can lead to hip flexion.
Quadriceps (quadriceps), especially the rectus muscle, can lead to hip flexion.
M.Lumbar erectors may cause lumbar extension.
M.Guadratus lumborum with bilateral induration may cause increased lumbar extension.
M.Hip adductors (adductors of the thigh) can cause the pelvis to tilt forward as a result of internal rotation of the hip. This leads to shortening of the adductor muscles.
M. Gluteus maximus (gluteus maximus) is responsible for hip extension and is an antagonist of the psoas major muscle.
M.Hamstrings The muscle of the back of the thigh, this muscle can be hardened. The muscle can be weak, at the same time hardened due to the fact that it is a synergist of the gluteus maximus muscle and this may be of a compensatory nature. The deep muscles of the abdominal wall, including the transversus abdominis and internal obliques, may become tense due to weakening of the muscles of the lumbar erectors
Symptoms
Symptoms of a misaligned pelvis can be moderate or severe and significantly impair the functionality of the body.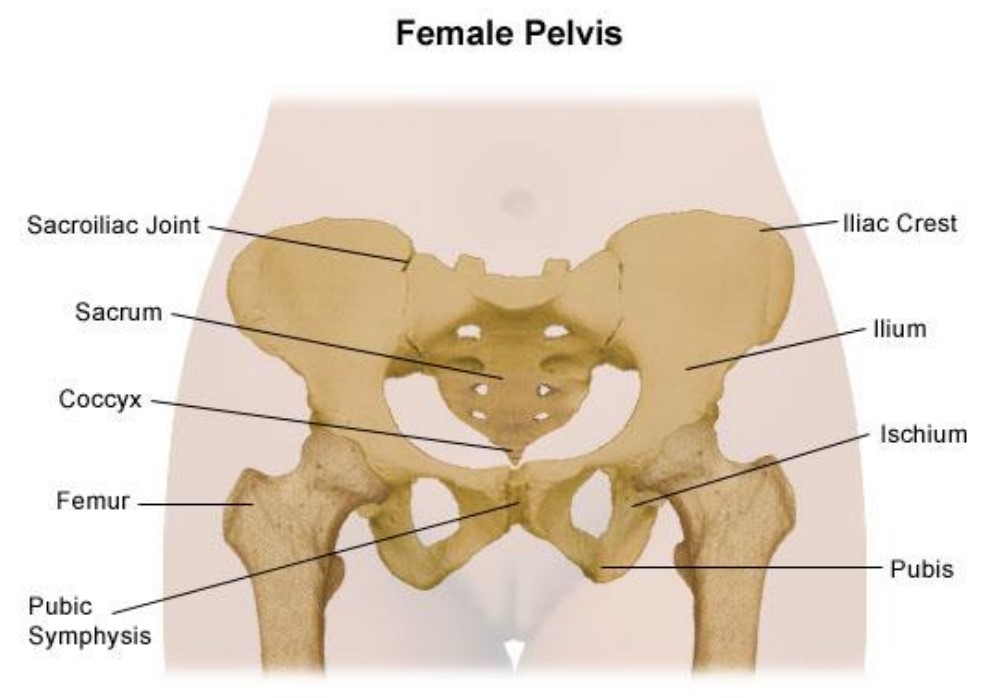 With moderate misalignment, a person may feel unsteady when walking or frequent falls are possible.
With moderate misalignment, a person may feel unsteady when walking or frequent falls are possible.
The most common symptoms are pain:
- In the lower back (radiating to the leg)
- Pain in the hip, sacroiliac joints or groin
- Pain in the knee, ankle or foot Achilles tendon
- Pain in shoulders, neck
If the pelvis is displaced for a long time, then the body will correct and compensate for the biomechanical disturbance and asymmetry and the corresponding adaptation of the muscles, tendons and ligaments will occur. Therefore, treatment may take some time. In addition, pelvic tilt can be difficult to correct, as a pathological stereotype of movements is formed over time. The longer the period of pelvic tilt, the longer it takes to restore normal muscle balance.
Diagnosis and treatment
Pelvic tilt is usually well diagnosed on physical examination of the patient. If it is necessary to diagnose changes in the spine or hip joints, instrumental examination methods are prescribed, such as radiography or MRI (CT).