Swollen and itchy vag lips in pregnancy
Vaginal thrush during pregnancy | Pregnancy Birth and Baby
Vaginal thrush during pregnancy | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Most women experience occasional bouts of a common yeast infection known as vaginal thrush. It causes itching, irritation and swelling of the vagina and surrounding area, sometimes with a creamy white cottage cheese-like discharge.
Vaginal thrush is fairly harmless, but it can be uncomfortable and it can keep coming back, which is known as recurrent thrush.
Thrush is a yeast infection, usually caused by a yeast-like fungus called 'Candida albicans'.
Many women have Candida in their vagina without it causing any symptoms. Hormones in vaginal secretions and 'friendly' vaginal bacteria keep the fungus under control. Problems arise when the natural balance in the vagina is upset and Candida multiplies.
Vaginal thrush can sometimes be passed on during sex but is not considered a sexually transmitted infection (STI). However, if you have thrush it’s best to avoid having sex until you’ve completed a course of treatment and the infection has cleared up.
During pregnancy
You are more at risk of getting thrush while you're pregnant. Changes in the levels of female hormones, such as oestrogen, increase your chances of developing thrush and make it more likely to keep coming back.
There is no evidence that thrush affects your chances of getting pregnant.
If you're pregnant or breastfeeding and you have thrush, you should avoid taking oral anti-thrush treatments. Instead, use vaginal pessaries, plus an anti-thrush cream if necessary.
Treatment
If you have thrush and you're pregnant or breastfeeding, you should always visit your doctor rather than buying anti-thrush medication over the counter from a pharmacy.
You won’t be prescribed oral treatment because it may affect your baby. An anti-thrush pessary, such as clotrimazole, nystatin or miconazole will probably be prescribed to be used for about 3 to 7 days.
If you're pregnant, take care when inserting a pessary because there's a risk of injuring your cervix (neck of the womb). To reduce the risk, it may be better to insert the pessaries by hand instead of using the applicator.
If you have symptoms around your vulva, such as itching and soreness, you may also be prescribed an anti-thrush cream.
Not all of these products are safe to use at different stages of pregnancy, so it's important to talk to your doctor and pharmacist before using any products.
What can I do to prevent vaginal thrush?
There are a number of simple things you can do:
- Wear cotton or silk underwear rather than synthetics and change daily. Wear tights or stockings for as short a time as possible.
- Wash underwear in hot water and pure soap and double rinse to make sure any irritants are removed before you wear them.
- Change out of damp swimming costumes or sports clothes as soon as possible after swimming or exercise.
- If using pads, change them regularly and avoid perfumed or deodorised pads.
- Avoid tight fitting clothes such as jeans as this creates a moist, warm environment that encourages the overgrowth of bacteria and yeasts.
- Never douche — except if it is specifically prescribed by a doctor to treat an infection. Douching increases your risk of vaginal irritation and is not recommended during pregnancy. A healthy vagina does not need a vaginal deodorant.
- Avoid using soaps, bubble baths, bath salts, perfumes and perfumed talcs around the vaginal area. And never ever use anything harsh such as disinfectants — even diluted, near your vagina.
- A gentle moisturiser like aqueous cream may be advised. Use water or soap substitutes to wash the area.
- Always wipe from the front to the back after going to the toilet since this stops bowel organisms being swept into the vagina.
 Don’t use perfumed toilet paper because it can cause irritation.
Don’t use perfumed toilet paper because it can cause irritation.
Sources:
Mater Mother’s Hospital (Pregnancy – information for women and families), MotherSafe: NSW Medications in Pregnancy and Breastfeeding Service (Thrush in pregnancy), Women and Children’s Health Network (Common health problems in pregnancy – vaginal thrush)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: November 2020
Back To Top
Need more information?
Thrush | SA Health
Thrush or Candidiasis is a common vaginal infection, caused by an overgrowth of yeasts and is not considered to be a sexually transmitted infection
Read more on SA Health website
Vaginal discharge during pregnancy
Almost all women have more vaginal discharge in pregnancy as it helps prevent any infections travelling up from the vagina to the womb.
Read more on Pregnancy, Birth & Baby website
Contraception: vaginal ring - MyDr.com.au
The vaginal ring (brand name NuvaRing) is a type of hormonal contraception. When used properly, the vaginal ring is an effective and safe way of preventing pregnancy.
Read more on myDr website
Urinary tract infections (UTIs) during pregnancy
A urinary tract infection (UTI) is the most common bacterial infection women get in pregnancy, but there are ways to lower the risk of developing one.
Read more on Pregnancy, Birth & Baby website
Gestational diabetes: Q and A - MyDr.com.au
Gestational diabetes is a form of diabetes that develops during pregnancy. It is different from having known diabetes before pregnancy and then getting pregnant.
It is different from having known diabetes before pregnancy and then getting pregnant.
Read more on myDr website
Anatomy of pregnancy and birth - perineum and pelvic floor
The perineum – the skin between the vagina and anus - stretches during childbirth and can sometimes tear. Learn here how to prepare the perineum for the birth.
Read more on Pregnancy, Birth & Baby website
Pregnancy - signs and symptoms - Better Health Channel
All women experience pregnancy differently, and you will experience different symptoms at different stages of your pregnancy.
Read more on Better Health Channel website
STIs and pregnancy
Sexually transmitted infections (STIs), if left untreated, can cause serious problems for both mother and child.
Read more on Pregnancy, Birth & Baby website
Episiotomy
An episiotomy is a procedure performed during labour to assist with the delivery of your baby.
Read more on Pregnancy, Birth & Baby website
Menstrual cycle: normal - MyDr.com.au
All you need to know about periods, including what's normal and what's not. Plus, see what happens inside your body during the different phases of a normal menstrual cycle.
Read more on myDr website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
How to Ease Vaginal Swelling During Pregnancy
Swelling is a common side effect of pregnancy, especially when it comes to your feet and hands. But there’s one area that can also swell during pregnancy that doesn’t get a lot of attention: Your vagina. If you notice you have a swollen vagina during pregnancy, know you’re not the only woman going through this! Still, we’re guessing you might have questions about why this is happening. Here’s what you need to know, plus how to minimize the swelling and ease any discomfort.
In this article:
Symptoms of vaginal swelling during pregnancy
What causes vaginal swelling during pregnancy?
How to reduce vaginal swelling during pregnancy
How to prevent vaginal swelling during pregnancy
Symptoms of Vaginal Swelling During Pregnancy
Every woman and every pregnancy is different—which means the symptoms of vaginal swelling during pregnancy can differ from person to person. In general, though, you might experience the following:
In general, though, you might experience the following:
• Noticeable swelling. You’re probably familiar on at least some level with what your vulva and vaginal area usually feels like. If it’s swollen, it can feel noticeably bigger or puffier, says Frederick Friedman, Jr., MD, associate professor of obstetrics, gynecology and reproductive science at the Icahn School of Medicine at Mount Sinai in New York City. “There may just be a general feeling of swelling or fullness in the vaginal area,” adds Julie Lamppa, APRN, CNM, a certified nurse midwife at Mayo Clinic, which can lead to overall discomfort.
• Bumps. Some women who experience vaginal swelling during pregnancy can have varicose veins surface in their vulvar area, which can cause swelling and a bumpy feel down there, Lamppa says.
• Itchiness. This isn’t the case for every woman, but itchiness can sometimes accompany vaginal swelling, Lamppa says.
What Causes Vaginal Swelling During Pregnancy?
There are several reasons why you might develop vaginal swelling in pregnancy. Here are some of the most common ones:
Here are some of the most common ones:
• An increase in blood volume. Your blood volume increases during pregnancy to help support the growing baby. As your uterus grows, there’s also an increase in pressure of the blood vessels in your pelvis, Lamppa explains. The combination of these two things can lead to swelling.
• Varicose veins in your vulva. Varicose veins are swollen, bumpy veins that develop when valves let blood pool in one spot or flow backward. Just like you can develop varicose veins in your legs, you can also develop these in your vulva during pregnancy, Lamppa says. “These aren’t dangerous, but they can be alarming to women when they suddenly show up.”
• A yeast infection. Yeast infections are common among moms-to-be, and they can also lead to a swollen vagina during pregnancy, Friedman says. “The inflammation that results from the infection can cause more swelling,” he explains.
• Excess fluid. Excess fluid can get trapped in your body’s tissues during pregnancy, and that can cause swelling down there, Friedman says.
Excess fluid can get trapped in your body’s tissues during pregnancy, and that can cause swelling down there, Friedman says.
How to Reduce Vaginal Swelling During Pregnancy
If you suspect that your vaginal swelling is due to excess fluid, compression or support stockings might help. “There are products on the market that you can buy that give vulvar support,” Lamppa says. (Just check in with your doctor first to make sure it’s okay for you to use.)
For direct relief, Lamppa recommends applying a cool pack directly to your vulva. That should help with discomfort as well as cut down on some of the swelling.
If you’re experiencing vaginal swelling along with symptoms of a yeast infection—such as an itchy vaginal area during pregnancy, accompanied by white vaginal discharge—Lamppa recommends seeing your doctor for an evaluation. If they determine that you do, in fact, have a yeast infection, your care provider will likely recommend that you use an over-the-counter cream.
How to Prevent Vaginal Swelling During Pregnancy
Sorry, but there isn’t a ton you can do to lower the odds you’ll experience vaginal swelling during pregnancy, given that it’s a normal side effect of being pregnant, Lamppa says. However, doing your best to avoid sitting or standing for long periods of time may be helpful, Friedman suggests.
While it’s pretty common, it’s a good idea to flag any vaginal swelling during pregnancy for your care provider so they can help pinpoint the cause and get you sweet relief ASAP.
Updated January 2020
Expert bios:
Frederick Friedman, Jr., MD, is an associate professor of obstetrics, gynecology and reproductive science at the Icahn School of Medicine at Mount Sinai. He also serves as director for both the division of obstetrics and the division of generalists in the department of obstetrics, gynecology and reproductive science at the Mount Sinai Health System, and maintains a clinical practice in general obstetrics and gynecology.
Julie Lamppa, APRN, CNM, is a certified nurse midwife and medical editor at Mayo Clinic, and maintains a midwifery practice in Rochester, New York.
*Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances. *
Plus, more from The Bump:
Swelling in Pregnancy: Why It Happens and How to Deal
How Your Vaginal Discharge Can Change During Pregnancy
10 Surprising Pregnancy Symptoms No One Warned You About
Changes in a woman's body during pregnancy
From the very first days of pregnancy, the body of a pregnant woman undergoes profound transformations. These transformations are the result of the coordinated work of almost all body systems, as well as the result of the interaction of the mother's body with the child's body.
During pregnancy, many internal organs undergo significant restructuring. These changes are adaptive in nature, and, in most cases, are short-lived and completely disappear after childbirth. Consider the changes in the basic systems of the vital activity of a woman's body during pregnancy.
The respiratory system during pregnancy works hard. The respiratory rate increases. This is due to an increase in the need of the mother and fetus for oxygen, as well as in the limitation of the respiratory movements of the diaphragm due to an increase in the size of the uterus, which occupies a significant space of the abdominal cavity.
Cardio The mother's vascular system has to pump more blood during pregnancy to ensure an adequate supply of nutrients and oxygen to the fetus. In this regard, during pregnancy, the thickness and strength of the heart muscles increase, the pulse and the amount of blood pumped by the heart in one minute increase. In addition, the volume of circulating blood increases. In some cases, blood pressure increases. The tone of the blood vessels during pregnancy decreases, which creates favorable conditions for enhanced
In addition, the volume of circulating blood increases. In some cases, blood pressure increases. The tone of the blood vessels during pregnancy decreases, which creates favorable conditions for enhanced
to supply tissues with nutrients and oxygen. During pregnancy, the network of vessels of the uterus, vagina, and mammary glands decreases sharply. On the external genital organs, in the vagina, the lower extremities are often observed varicose veins, sometimes the formation of varicose veins. Heart rate decreases in the second half of pregnancy. It is generally accepted that the rise in blood pressure over 120-130 and a decrease to 100 mm Hg. signal the occurrence of pregnancy complications. But it is important to have data on the initial level of blood pressure. and changes in the blood system. During pregnancy, blood formation increases, the number of red blood cells, hemoglobin, plasma and bcc increases. BCC by the end of pregnancy increases by 30-40%, and erythrocytes by 15-20%. Many healthy pregnant women have a slight leukocytosis. ESR during pregnancy increases to 30-40. Changes occur in the coagulation system that contribute to hemostasis and prevent significant blood loss during childbirth or placental abruption and in the early postpartum period.
Many healthy pregnant women have a slight leukocytosis. ESR during pregnancy increases to 30-40. Changes occur in the coagulation system that contribute to hemostasis and prevent significant blood loss during childbirth or placental abruption and in the early postpartum period.
Kidneys work hard during pregnancy. They secrete decay products of substances from the body of the mother and fetus (the waste products of the fetus pass through the placenta into the mother's blood).
Changes in the digestive system are represented by increased appetite (in most cases), craving for salty and sour foods. In some cases, there is an aversion to certain foods or dishes that were well tolerated before the onset of pregnancy. Due to the increased tone of the vagus nerve, constipation may occur.
The most significant changes, however, occur in the genitals of pregnant women. These changes prepare the woman's reproductive system for childbirth and breastfeeding.
The uterus of a pregnant woman increases significantly in size. Its mass increases from 50 g - at the beginning of pregnancy to 1200 g - at the end of pregnancy. The volume of the uterine cavity by the end of pregnancy increases by more than 500 times! The blood supply to the uterus is greatly increased. In the walls of the uterus, the number of muscle fibers increases. The cervix is filled with thick mucus that clogs the cavity of the cervical canal. The fallopian tubes and ovaries also increase in size. In one of the ovaries, there is a "corpus luteum of pregnancy" - a place for the synthesis of hormones that support pregnancy.
The walls of the vagina will loosen and become more elastic.
External genitalia (labia minor and major) also increase in size and become more elastic. The tissues of the perineum are loosened. In addition, there is an increase in mobility in the joints of the pelvis and a divergence of the pubic bones. The changes in the genital tract described above are of extremely important physiological significance for childbirth. Loosening the walls, increasing the mobility and elasticity of the genital tract increases their throughput and facilitates the movement of the fetus through them during childbirth.
The changes in the genital tract described above are of extremely important physiological significance for childbirth. Loosening the walls, increasing the mobility and elasticity of the genital tract increases their throughput and facilitates the movement of the fetus through them during childbirth.
Skin in the genital area and in the midline of the abdomen usually becomes darker in color. Sometimes "stretch marks" form on the skin of the lateral parts of the abdomen, which turn into whitish stripes after childbirth.
Mammary glands increase in size, become more elastic, tense. When pressing on the nipple, colostrum (first milk) is released. Changes of the bone skeleton and muscular system . An increase in the concentration of the hormones relaxin and progesterone in the blood contributes to the leaching of calcium from the skeletal system. This accomplishes two goals. On the one hand, this helps to reduce the rigidity of the joints between the pelvic bones (especially the pubic joint) and increase the elasticity of the pelvic ring.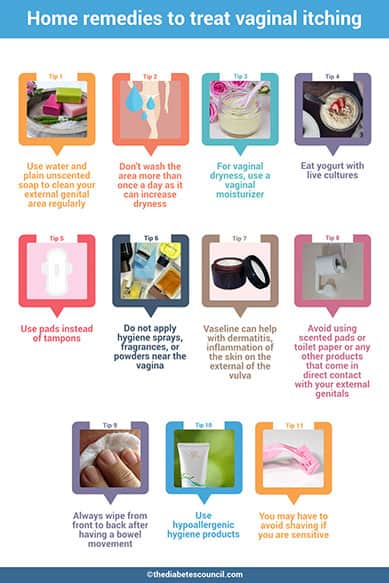 Increasing the elasticity of the pelvis is of great importance in increasing the diameter of the internal bone ring in the first stage of labor and further reducing the resistance of the birth tract to fetal movement in the second stage of labor. Secondly, calcium, washed out of the mother's skeletal system, is used to build the skeleton of the fetus.
Increasing the elasticity of the pelvis is of great importance in increasing the diameter of the internal bone ring in the first stage of labor and further reducing the resistance of the birth tract to fetal movement in the second stage of labor. Secondly, calcium, washed out of the mother's skeletal system, is used to build the skeleton of the fetus.
It should be noted that calcium compounds are washed out of all bones of the maternal skeleton (including the bones of the foot and spine). As shown earlier, a woman's weight increases during pregnancy by 10 -12 kg. This additional load against the background of a decrease in bone stiffness can cause foot deformity and the development of flat feet. A shift in the center of gravity of the body of a pregnant woman due to an increase in the weight of the uterus can lead to a change in the curvature of the spine and the appearance of pain in the back and pelvic bones. Therefore, for the prevention of flat feet, pregnant women are advised to wear comfortable shoes with low heels. It is advisable to use insoles that support the arch of the foot. For the prevention of back pain, special physical exercises are recommended that can unload the spine and sacrum, as well as wearing a comfortable bandage. Despite an increase in calcium loss by the bones of the skeleton of a pregnant woman and an increase in their elasticity, structure and bone density (as is the case with osteoporosis in older women).
It is advisable to use insoles that support the arch of the foot. For the prevention of back pain, special physical exercises are recommended that can unload the spine and sacrum, as well as wearing a comfortable bandage. Despite an increase in calcium loss by the bones of the skeleton of a pregnant woman and an increase in their elasticity, structure and bone density (as is the case with osteoporosis in older women).
Changes in the nervous system . In the first months of pregnancy and at the end of it, there is a decrease in the excitability of the cerebral cortex, which reaches its greatest degree by the time of the onset of childbirth. By the same period, the excitability of the receptors of the pregnant uterus increases. At the beginning of pregnancy, there is an increase in the tone of the vagus nerve, in connection with which various phenomena often occur: changes in taste and smell, nausea, increased salivation, etc.
Active endocrine glands there are significant changes that contribute to the proper course of pregnancy and childbirth. Changes in body weight. By the end of pregnancy, a woman's weight increases by about 10-12 kg. This value is distributed as follows: fetus, placenta, membranes and amniotic fluid - approximately 4.0 - 4.5 kg, uterus and mammary glands -1.0 kg, blood - 1.5 kg, intercellular (tissue) fluid - 1 kg , an increase in the mass of adipose tissue of the mother's body - 4 kg.
Changes in body weight. By the end of pregnancy, a woman's weight increases by about 10-12 kg. This value is distributed as follows: fetus, placenta, membranes and amniotic fluid - approximately 4.0 - 4.5 kg, uterus and mammary glands -1.0 kg, blood - 1.5 kg, intercellular (tissue) fluid - 1 kg , an increase in the mass of adipose tissue of the mother's body - 4 kg.
Conclusion. Summarizing the facts concerning changes in a woman's body during pregnancy, it is worth emphasizing that these changes reflect the processes of physiological adaptation of the mother's body to the process of intrauterine development of the fetus. Therefore, measures aimed at preventing the pathology of pregnancy should be, first of all, natural, physiological. This is a proper and balanced diet, smoking cessation, a sufficient level of physical activity and fluid intake. In a healthy woman, such approaches ensure the normal course of pregnancy and adequate preparation of the mother's body for childbirth and breastfeeding.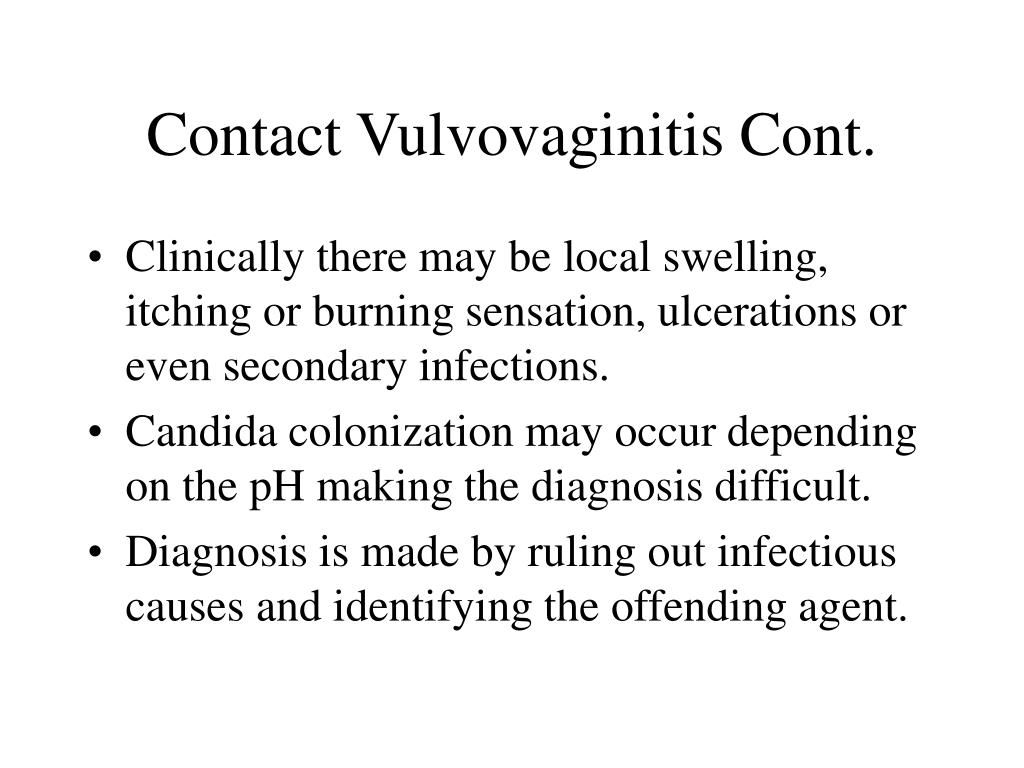
Prepared by: Head of the Pregnancy Pathology Department Teressa Ivanovna Vorobieva.
Why does the skin itch during pregnancy?
Skin itching during pregnancy is not a very common phenomenon. Most often, the skin begins to itch unbearably (as after mosquito bites) in the evening, closer to night, which can provoke insomnia and generally worsen a woman’s mood. Usually itching does not harm the baby and goes away after childbirth. However, it is still worth consulting with a gynecologist and dermatologist.
What does it come from?
The cause of itching during pregnancy in most cases is a violation of the liver: the production and outflow of bile, a general increase in the level of bilirubin in the blood. This is due to a hormonal failure in the body of the future mother - a violation of the synthesis of estrogens, as well as due to fetal pressure on the bile ducts. The fatty acids produced in large quantities enter the woman's skin with the bloodstream and irritate the nerve endings, causing excruciating itching. Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus.
Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus.
Who is predisposed?
Itching during pregnancy is usually observed in women with chronic diseases of the biliary tract and with high levels of cholesterol in the blood. Such future mothers need to regularly (at least once a month) do a biochemical blood test to exclude toxic effects on liver cells.
How to fight?
A pregnant woman should tell her gynecologist about the discomfort associated with skin itching. In some cases, itching can be a sign of the development of such a dangerous disease as hepatitis. The doctor will conduct appropriate examinations. If, according to an objective examination, itching does not pose any danger, it is often possible to get rid of discomfort simply by following a diet aimed at lowering cholesterol levels, limiting the intake of fatty, spicy and salty foods that prevent the liver from coping with the function of bile secretion, as well as drinking plenty of water - it is necessary to eliminate dry skin.