What causes miscarriage at 18 weeks
Late Miscarriage: Causes, Symptoms, and Recovery
Late Miscarriage: Causes, Symptoms, and Recovery- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Kimberly Dishman, MSN, WHNP-BC, RNC-OB — By Diana Wells on August 23, 2016
Overview
Any miscarriage is difficult. But a late miscarriage after week 13 of pregnancy can be even more devastating, both emotionally and physically.
Here’s a look at the causes, symptoms, and how to care for yourself or a loved one who experiences a late miscarriage.
What is a late miscarriage?
Miscarriage is the term used for losing a baby, usually prior to week 20 of your pregnancy. Many early miscarriages are caused by the fetus not developing properly. But there can be other causes, too.
Miscarriages in the first trimester, or before week 13 of your pregnancy, are fairly common. At this stage of pregnancy, many women do not feel symptoms of miscarriage. Also, if it’s very early in the pregnancy, women may not realize that they were pregnant.
A late miscarriage is when you lose a baby after week 13, but before week 20, or during the second trimester.
Causes of a late miscarriage
There are a number of factors that can cause a late miscarriage. Most are related to some abnormality of the fetus’s development. They are usually genetic or structural issues, such as a chromosomal abnormality or heart defect. Trauma can also cause a miscarriage.
They are usually genetic or structural issues, such as a chromosomal abnormality or heart defect. Trauma can also cause a miscarriage.
The cause can be physical as well. One example is a weak cervix that can’t hold the baby inside when it gets bigger. Some medical conditions of the mother can also be a cause for miscarriages, including chronic conditions that aren’t being managed well.
Some of the physical causes of miscarriage include:
- hypertension
- thyroid conditions
- lupus or other immune disorders
- diabetes
- preeclampsia
- other genetic conditions
- some infections
What are the symptoms of a late miscarriage?
While some women may not feel any symptoms of miscarriage, there are some common ones to watch for.
These include:
- not feeling movement of the fetus
- vaginal bleeding or spotting
- cramping or pain in your back and/or abdomen
- unexplained fluid or tissue that passes through the vagina
Keep in mind, not all vaginal spotting is a symptom of a miscarriage. Sometimes you’ll experience some spotting in the first trimester of a healthy pregnancy. See your doctor if you’re concerned.
Sometimes you’ll experience some spotting in the first trimester of a healthy pregnancy. See your doctor if you’re concerned.
Risk factors for a miscarriage
Some miscarriages don’t have a specific cause, or one that can be anticipated. But some women are at a higher risk of miscarriage than others.
The following are risk factors for a miscarriage:
- experiencing two prior miscarriages in a row
- chronic medical conditions
- pregnancy over 35 years old
- being overweight or underweight
- having an abnormally shaped uterus
- a weak cervix
- having invasive prenatal tests (amniocentesis and chorionic villus sampling are examples)
- exposures to substances like alcohol, tobacco, cocaine, NSAIDs, and high levels of caffeine
- low folate level
- untreated celiac disease
While these conditions suggest a higher risk of miscarriage, it doesn’t mean that you can’t have a healthy pregnancy. Cutting out harmful substances like alcohol and drugs and properly managing other conditions can give you a good chance at a healthy pregnancy.
Recovery after a late miscarriage
Physical needs and care after a late miscarriage
Physically, your body may recover fairly quickly after a miscarriage. But it depends on how far along you were in your pregnancy and what type of miscarriage you experienced. For those who go through labor and delivery of the miscarriage, it can take several weeks to recover.
You’ll experience some bleeding and cramps similar to getting your period. Most of all, you’ll feel very tired as your body recovers.
Contact your doctor if your pain, bleeding, or exhaustion becomes worse or continues longer than several weeks. Another potentially upsetting part of your recovery may be that your body begins producing milk. If this causes pain or discomfort, be sure to talk to your doctor about taking some type of pain reliever or other ways to help.
You should also talk to your doctor about when you’ll physically be ready to return to work. Every situation is different, and your doctor can help determine when it’s safe and reasonable for you to return.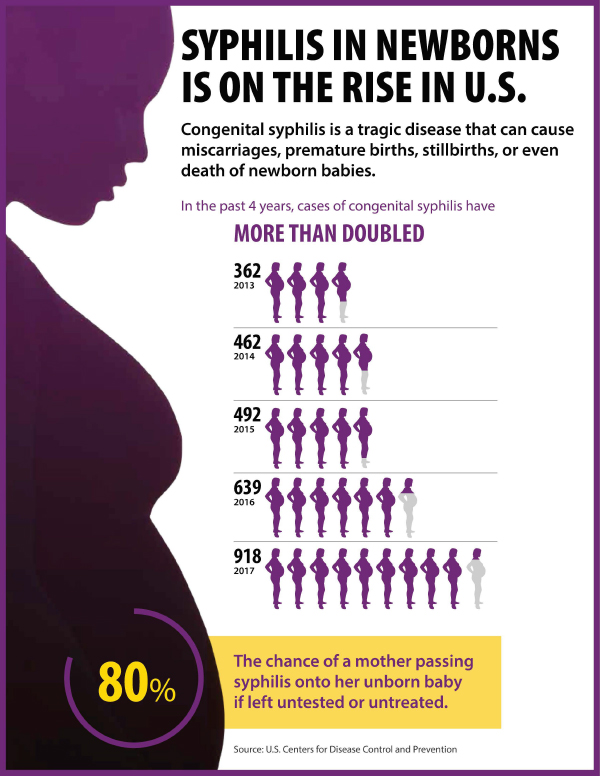
Emotional needs and care after a late miscarriage
The emotional needs after a late miscarriage shouldn’t be ignored. Losing a baby at any stage of pregnancy is difficult, but even more so in the second trimester.
Every woman will react differently and have different emotions. For some, talking about it helps. For others, moving on and not talking about it may help. It’s important to find what feels right for you and get the support you need. Your doctor can usually direct you to support groups or counselors that specialize in helping you work through all of your emotions after your miscarriage.
You’ll likely feel a wide range of emotions after your miscarriage.
These might include:
- anger
- guilt
- jealousy of others who or pregnant or have babies
- sadness
It is also important to remember that people will not always know what to say. This can sometimes mean they say the wrong things. Being prepared for these times might help soften the emotional impact.
Consider seeking out others who have experienced miscarriages, particularly late miscarriages, who you can talk to or cry with. Knowing that someone else understands can help you tremendously as you recover.
Getting pregnant again after a late miscarriage
Thinking about getting pregnant again can be scary or stressful. You may also not know how long you should wait before trying again. The first step is to be sure that you’re emotionally ready for another pregnancy and that your partner is, too. Be sure that you’ve completed the grieving process for your miscarriage.
Physically, you’re usually able to have sex two to six weeks following a miscarriage. But it’s important to talk to your doctor about when your body may be physically ready to become pregnant again.
What are the chances of having a second late miscarriage?
It should be noted that the majority of women will only have one miscarriage. It’s less common to have two or more. So your chances are very good of your next pregnancy being normal, healthy, and full-term.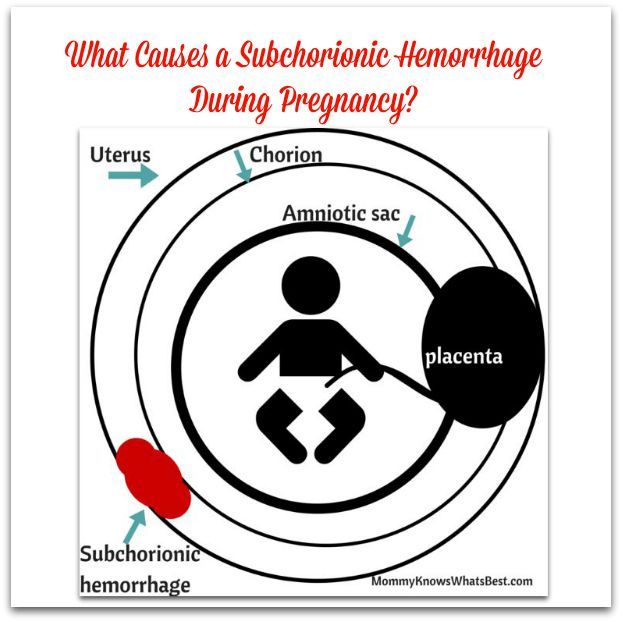 But that depends on any physical issues or medical conditions you have.
But that depends on any physical issues or medical conditions you have.
If you’ve had more than one miscarriage, your doctor may want to complete some tests prior to approving you to start trying to get pregnant again. Even if you do have a medical or physical condition that makes pregnancy riskier, there are usually steps that the doctor can advise you to take to increase your chances of a healthy pregnancy.
Next steps
If you experience a late miscarriage, it’s important that you seek out support to help you through both the physical and emotional healing processes. Your doctor can be a great resource for helping you find the support you need and helping you prepare for your next pregnancy.
Q:
What can a woman who had a late miscarriage do in subsequent pregnancies to stay healthy?
Anonymous patient
A:
Stay healthy by meeting with and discussing your
pregnancy desires with all of your healthcare providers. If you have a chronic
If you have a chronic
medical problem, like diabetes or thyroid disease, follow directions to manage
the condition carefully for optimal health before and during pregnancy.
Extremes of weight are other aspects of health that can be modified. Obese and
underweight women have an increased risk of spontaneous abortion or
miscarriage. Sometimes, a physical problem with the maternal body may need to
be corrected, like a septum, or wall, in the uterus. Also, be aware of the
damage that can happen to a pregnancy by viruses, medications, and other
environmental exposures. Talk to your doctor about how to have a safe
pregnancy.
Kimberly Dishman, MSN, WHNP-BC, RNC-OB
Answers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
Last medically reviewed on August 23, 2016
- Parenthood
- Pregnancy
- Pregnancy Complications
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations.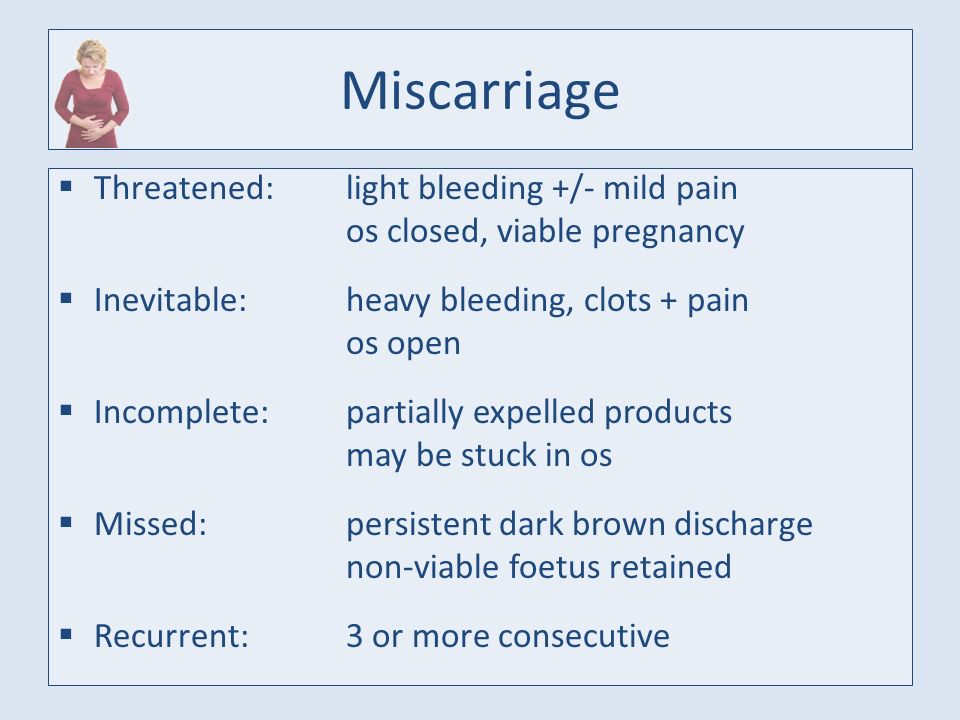 We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Late miscarriage: second trimester loss. (2011)
miscarriageassociation.org.uk/wp/wp-content/leaflets/Late-Miscarriage.pdf - Mayo Clinic Staff. (2016, July). Miscarriage
mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/home/ovc-20213664 - Mayo Clinic Staff. (2016, March). Pregnancy after miscarriage: What you need to know
mayoclinic.org/healthy-lifestyle/getting-pregnant/in-depth/pregnancy-after-miscarriage/art-20044134 - Murry, M. M. (2008, March). Miscarriage brings silent anguish
mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/expert-blog/pregnancy-loss-miscarriage/bgp-20055824 - Understanding second trimester loss. (2015)
ucdmc.ucdavis.edu/obgyn/services/FP/trimester_loss.html
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.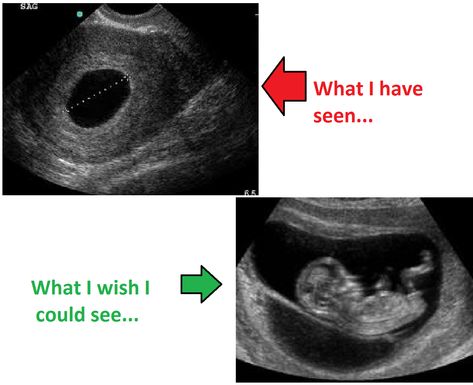
Current Version
Aug 23, 2016
Written By
Diana Wells
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Kimberly Dishman, MSN, WHNP-BC, RNC-OB
Share this article
Medically reviewed by Kimberly Dishman, MSN, WHNP-BC, RNC-OB — By Diana Wells on August 23, 2016
related stories
Pregnancy After Miscarriage: Answers to Your Questions
How to Tell if You’re Having a Miscarriage Without Bleeding
Everything You Need to Know About Miscarriage
Depression After a Miscarriage
How Long Does a Miscarriage Last?
Read this next
Pregnancy After Miscarriage: Answers to Your Questions
Medically reviewed by Amanda Kallen, MD
Getting pregnant after a miscarriage can be an emotional experience, filled with joy but also anxiety and guilt. Learn more about pregnancy after…
READ MORE
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.
 D., MSN, R.N., CNE, COI
D., MSN, R.N., CNE, COIA miscarriage is also known as a pregnancy loss. These are the symptoms, causes, and a look at how to move forward.
READ MORE
Everything You Need to Know About Miscarriage
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
A miscarriage is the loss of a fetus during pregnancy. It’s also an event that’s more common than you think. Learn about causes, types, symptoms, and…
READ MORE
Depression After a Miscarriage
Medically reviewed by Janine Kelbach, RNC-OB
It’s not uncommon to experience depression after the sudden loss of a pregnancy. Learn how to cope with the depression associated with miscarriage.
READ MORE
How Long Does a Miscarriage Last?
Medically reviewed by Holly Ernst, PA-C
The loss of a pregnancy before 20 weeks is considered a miscarriage.
 The length of time a miscarriage lasts varies from woman to woman, as do the risk…
The length of time a miscarriage lasts varies from woman to woman, as do the risk…READ MORE
Everything You Need to Know About Miscarriage
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
A miscarriage is the loss of a fetus during pregnancy. It’s also an event that’s more common than you think. Learn about causes, types, symptoms, and…
READ MORE
Identifying and Treating a Missed Abortion
A missed abortion is another term for a missed miscarriage or a silent miscarriage. We’ll explore symptoms, causes, and treatment options.
READ MORE
Is There a Link Between Endometriosis and Miscarriage?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Does endometriosis increase your risk for miscarriage? We explain the connection.
READ MORE
Can Taking Prometrium Vaginally Prevent Miscarriage?
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Progesterone is known as the “pregnancy hormone.” Without enough progesterone, a woman’s body can’t continue to grow a fertilized egg. If you’ve…
READ MORE
Abortion with Septic Shock
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Septic shock occurs when an infection overtakes your body and causes very low blood pressure. Abortion with septic shock can be a dangerous…
READ MORE
Understanding Second Trimester Loss | Obstetrics and Gynecology
Pregnancy loss in the second trimester can be the result of a very preterm delivery (like a spontaneous miscarriage in the second trimester) or death of the fetus (called a fetal demise). About 2-3% of pregnancies will be lost in the second trimester, a rate that is much lower than in the first trimester. Once a pregnancy gets to about 20 weeks gestation, less than 0.5% will end in a fetal demise.
About 2-3% of pregnancies will be lost in the second trimester, a rate that is much lower than in the first trimester. Once a pregnancy gets to about 20 weeks gestation, less than 0.5% will end in a fetal demise.
A loss at this time in pregnancy is most often a hard and sad experience. Many friends and family already know you are pregnant. What do you do? What do you say? For most women and their partners, the process of grieving is no different than losing a person who has been in your life for some time. You often have hopes and dreams about your child before that child is born, and losing the pregnancy in the second or third trimester is certainly a loss for a family.
Why see a UC Davis Health specialist?
Our specialists can evaluate you quickly in an office setting. Any laboratory testing or ultrasound examinations that need to be done can be performed easily and conveniently. We perform our own ultrasound examination in the office and can share the results with you immediately. Treatment of a second trimester loss is very different than early miscarriage, and our specialists can provide all options to you and your family. We understand that losses at this time require both emotional and medical support. We are happy to review all treatment options but also know that you may need some time. It is also important for you to know that a fetal demise in the second trimester is not a medical emergency so treatment is not immediately indicated.
Treatment of a second trimester loss is very different than early miscarriage, and our specialists can provide all options to you and your family. We understand that losses at this time require both emotional and medical support. We are happy to review all treatment options but also know that you may need some time. It is also important for you to know that a fetal demise in the second trimester is not a medical emergency so treatment is not immediately indicated.
If you are having very heavy vaginal bleeding or are feeling very sick, you should go to the Emergency Room to see our physicians.
Symptoms of a second trimester loss
- Bleeding: Most commonly, bleeding is a sign of a problem with the placenta and does not indicate a fetal demise. But, bleeding can be a sign that the cervix is opening without labor (called cervical insufficiency). With cervical insufficiency, the cervix begins to open early without contractions; as the cervix opens more, contractions then follow.

- Cramping: Pregnancy losses in the second trimester can be due to early labor.
- Loss of fetal movement: This can indicate a fetal demise. Most women can feel the baby moving by the 20th week. If the baby has been moving and you no longer feel that same movement, it is important to contact the doctor’s office immediately to make sure the baby is fine. Decreased fetal movement is more commonly a sign that there is a problem with the pregnancy and only rarely does it mean the fetus has died.
Most women less than 20 weeks of pregnancy do not notice any symptoms of a fetal demise.
The test used to check for a fetal demise in the second trimester is an ultrasound examination to see if the baby is moving and growing. Fetal demise is diagnosed when the ultrasound examination shows no fetal heart activity.
What causes a second trimester loss?
The causes of a pregnancy loss in the second trimester are very different than early pregnancy loss. There are medical conditions that increase the risk for cervical insufficiency or preterm labor before viability which include:
There are medical conditions that increase the risk for cervical insufficiency or preterm labor before viability which include:
- Prior surgery to the cervix
- Use of illicit drugs, especially cocaine
- Fetal abnormalities (genetic or structural problems)
- Uterine infection (this is more common in developing countries and less common in the United States)
- Physical problems with the uterus, including fibroids or abnormalities in the shape of the uterus
There are also some medical conditions that are associated with fetal death in the second trimester which include:
- Fetal abnormalities (genetic or structural problems)
- Poorly controlled maternal cnoditions like thyroid disease, diabetes or hypertension
- Lupus (systemic lupus erythematosus)
- Autoimmune or genetic conditions that increase a woman’s risk of forming blood clots in her legs or her lungs (like antiphospholipid syndrome)
- Very early pre-eclampsia or eclampsia of pregnancy
- Trauma
The specialists at UC Davis Health will review with you what testing is indicated to help learn more about why a second trimester loss occurred. Despite the testing that is available, about half of the time there is no identifiable reason for a second trimester loss. We can work with you to figure out what may be helpful with a next pregnancy or to learn more about medical issues that are important for your future.
Despite the testing that is available, about half of the time there is no identifiable reason for a second trimester loss. We can work with you to figure out what may be helpful with a next pregnancy or to learn more about medical issues that are important for your future.
Treatment of a second trimester loss
It is typically not safe for a woman to wait for the pregnancy to deliver on its own with a second trimester loss. There is a high chance of having significant bleeding when a pregnancy in the second trimester delivers on its own at home. In the case of fetal demise, a dead fetus that has been in the uterus for 4 weeks can cause changes in the body’s clotting system. These changes can put a woman at a much higher chance of significant bleeding if she waits for a long time after the fetal demise to deliver the pregnancy.
Our doctors are committed to providing all available treatment options. Testing to figure out the cause of the pregnancy loss can be performed regardless of the method a woman chooses for termination.
We understand that a second trimester loss is an emotional and stressful time and we want to ensure that the emotional needs of you and your family are met as well. We understand this is a time that you need support and we are sensitive to your wishes for remembrances and religious preferences. We will discuss these issues with you before any treatment.
When a diagnosis of fetal demise in the second or third trimester is made, options include:
- Surgical evacuation: This procedure, called a dilation and evacuation, can be performed in the second trimester, typically up to about 24 weeks. Surgical evacuation is the most common treatment women choose and involves removing the pregnancy through the cervix in the operating room while you are asleep. The cervix needs to be opened about 1-2 inches in diameter. The doctors can use different ways to open the cervix based on how far along the pregnancy is and your individual circumstance. The goal is to provide the safest care for each patient.
 After a surgical evacuation, normal activity can typically be resumed the following day. Opening or preparing the cervix for surgical evacuation of the pregnancy may involve:
After a surgical evacuation, normal activity can typically be resumed the following day. Opening or preparing the cervix for surgical evacuation of the pregnancy may involve: - Medicines (tablets) that are put in the vagina a few hours to one day before the procedure.
- Medicine (tablets) that you hold between your cheek and gums for 30 minutes before swallowing. You would use this medicine a few hours before the procedure.
- Placing thin sticks in your cervix, called osmotic dilators, to absorb water from the cervix which causes the dilator sticks to swell slowly over 4-24 hours. Having the osmotic dilators placed is similar to getting a Pap test.
Labor induction: This treatment uses medicines to cause the uterus to go into labor. For women with pregnancies beyond 24 weeks, this is commonly the only option. If you choose this option, you will be in the Labor and Delivery Unit at UC Davis Medical Center and will have all of the same pain treatments available to you as a woman who is naturally in labor (like IV pain medications or an epidural). The treatment typically starts with swallowing a pill to make the uterus more sensitive to the medications to induce labor. About 24 hours later, you are admitted to the Labor and Delivery Unit and will have medicine (tablets) put in the vagina every few hours to cause labor. Sometimes, women need medicine through an IV to also help get labor started. It may take 1-2 days for the uterus to go into labor and for the delivery to be complete. Up to 5% of women in the second trimester do not go into labor and need a surgical evacuation.
The treatment typically starts with swallowing a pill to make the uterus more sensitive to the medications to induce labor. About 24 hours later, you are admitted to the Labor and Delivery Unit and will have medicine (tablets) put in the vagina every few hours to cause labor. Sometimes, women need medicine through an IV to also help get labor started. It may take 1-2 days for the uterus to go into labor and for the delivery to be complete. Up to 5% of women in the second trimester do not go into labor and need a surgical evacuation.
Your doctor will be able to explain more details about the pros and cons of each treatment.
After treatment of a second trimester loss
Bleeding may continue for several weeks after a labor induction but tends to be much lighter with a surgical evacuation. Any bleeding may change in color from bright red to pink or brown. Lower abdominal cramping in the few days after treatment is also common. You should contact a doctor right away if the bleeding gets heavier instead of lighter over time, if a fever develops, or if vaginal discharge or a strange or unpleasant vaginal odor occurs. Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant, it will be very important to start an effective method of contraception.
Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant, it will be very important to start an effective method of contraception.
FAQs about second trimester loss
Q: What is cervical insufficiency?
A: This diagnosis is made when a woman has dilation of the cervix during the second trimester without having any contractions or signs of a uterine infection. Some studies suggest that some types of surgeries performed when women have advanced pre-cancerous changes in the cervix can increase the risk of cervical insufficiency. These surgeries include cervical conization (also known as a “cone biopsy”) or if a patient has had multiple LEEP procedures. With these surgeries, part of the cervix is removed to get rid of the pre-cancerous changes. Having these procedures increases the risk of having a second trimester loss by about 1%. In women who have these types of procedures, the chance of having cervical insufficiency is about 1.5%.
In women who have these types of procedures, the chance of having cervical insufficiency is about 1.5%.
Q: What treatments are available if one of the tests shows I have a medical problem that increased the chance of a second trimester loss?
A: Our specialists will work with you to maximize your health status before you try to get pregnant again. For some women, this may mean treatment of a thyroid condition, improved control of diabetes, or changing medications being used for chronic illnesses. Some conditions may require blood thinners like aspirin or injectable medications that should be started early in the next pregnancy (after a normal pregnancy is seen with an early ultrasound exam).
Q: In my last pregnancy, I didn’t get any genetic testing and had a second trimester demise related to a genetic abnormality. What genetic testing is available for my next pregnancy to help figure out if the pregnancy is normal so I can learn earlier if the pregnancy is genetically normal?
A: It will be important to meet with a genetic counselor, if possible, before your next pregnancy, who can also review the details of the available tests. The counselor can also talk with you more about your history and your family history to make sure no genetic or familial medical problems are missed. There are a few different tests, all of which can be performed early in pregnancy, depending on what is right for you. Screening for some of the most common chromosomal abnormalities just from your blood (called NIPT or non-invasive prenatal testing). First trimester screening can be performed between 11 and 14 weeks which involves a blood test and an ultrasound examination. In some situations, chorionic villus sampling (a biopsy of the placenta) or expanded prenatal screening may be indicated. Our specialists and genetic counselors can work with you and your family to help you understand all of these tests and figure out what approach is right for you.
The counselor can also talk with you more about your history and your family history to make sure no genetic or familial medical problems are missed. There are a few different tests, all of which can be performed early in pregnancy, depending on what is right for you. Screening for some of the most common chromosomal abnormalities just from your blood (called NIPT or non-invasive prenatal testing). First trimester screening can be performed between 11 and 14 weeks which involves a blood test and an ultrasound examination. In some situations, chorionic villus sampling (a biopsy of the placenta) or expanded prenatal screening may be indicated. Our specialists and genetic counselors can work with you and your family to help you understand all of these tests and figure out what approach is right for you.
Q: After a second trimester loss, how long should I wait before I try to conceive again?
A: There is really no good information available to show the absolute right answer to that question. First, it may take a month or two to have any testing completed to help figure out why you had a second trimester loss. We know that it takes some time for your uterus and your body to get back to normal. The specialists at UC Davis usually recommend waiting at least 3 months after a second trimester loss before trying again to get pregnant.
First, it may take a month or two to have any testing completed to help figure out why you had a second trimester loss. We know that it takes some time for your uterus and your body to get back to normal. The specialists at UC Davis usually recommend waiting at least 3 months after a second trimester loss before trying again to get pregnant.
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection? nine0004
- Rules for patients
- Online doctor's consultation
- to corporative clients
- The documents
A miscarriage is always associated with severe consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule. An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child. nine0033
An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child. nine0033
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, bruise, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this.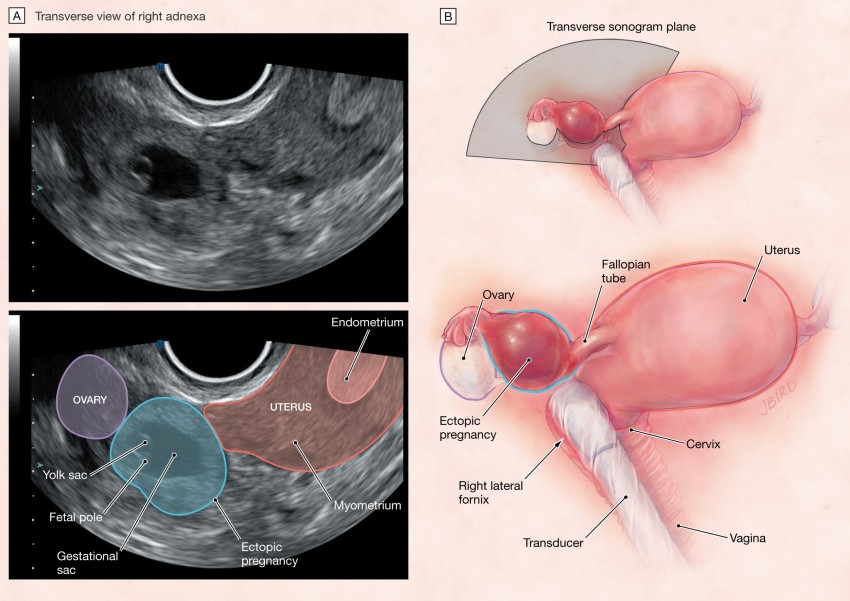 However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same. nine0033
However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same. nine0033
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap.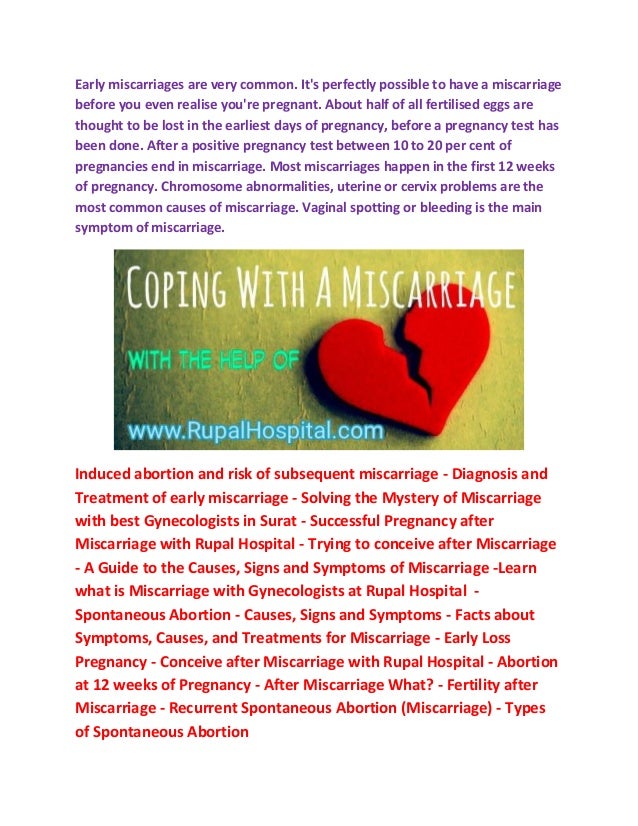 The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss. nine0033
The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss. nine0033
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it. nine0033
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies.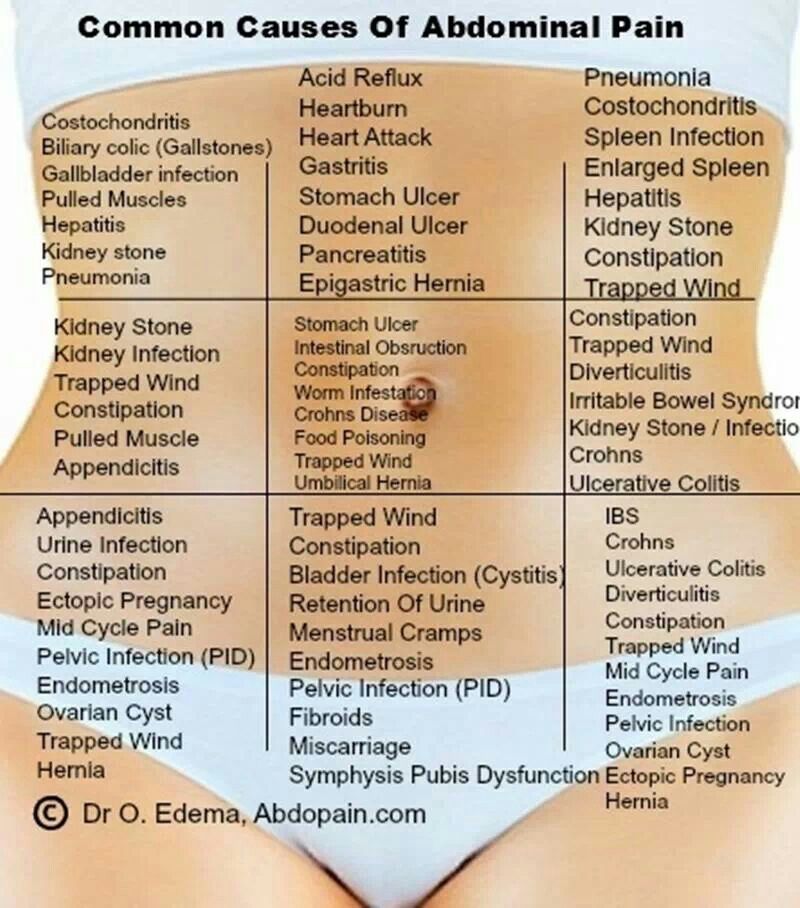 You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage. Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful. nine0033
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage in this period is also considered early. Its most common causes are:
Endocrine disorders
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage. nine0033
nine0033
Imbalance of hormones in a woman's body is very likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time. nine0033
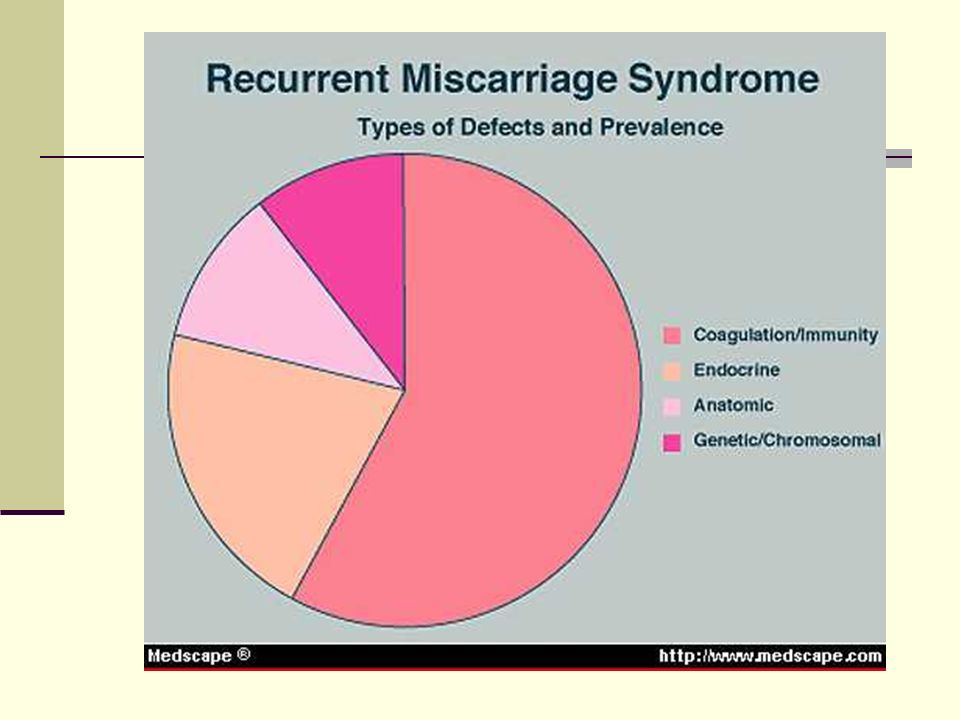
An excess of male sex hormones that suppress the production of estrogen and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor. nine0033
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 about C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections. nine0033
Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections. nine0033
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance. Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect. nine0033
Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect. nine0033
Reduced immunity
Reduced immunity during pregnancy also refers to immune causes. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage between 12 and 22 weeks
Such a miscarriage is considered late.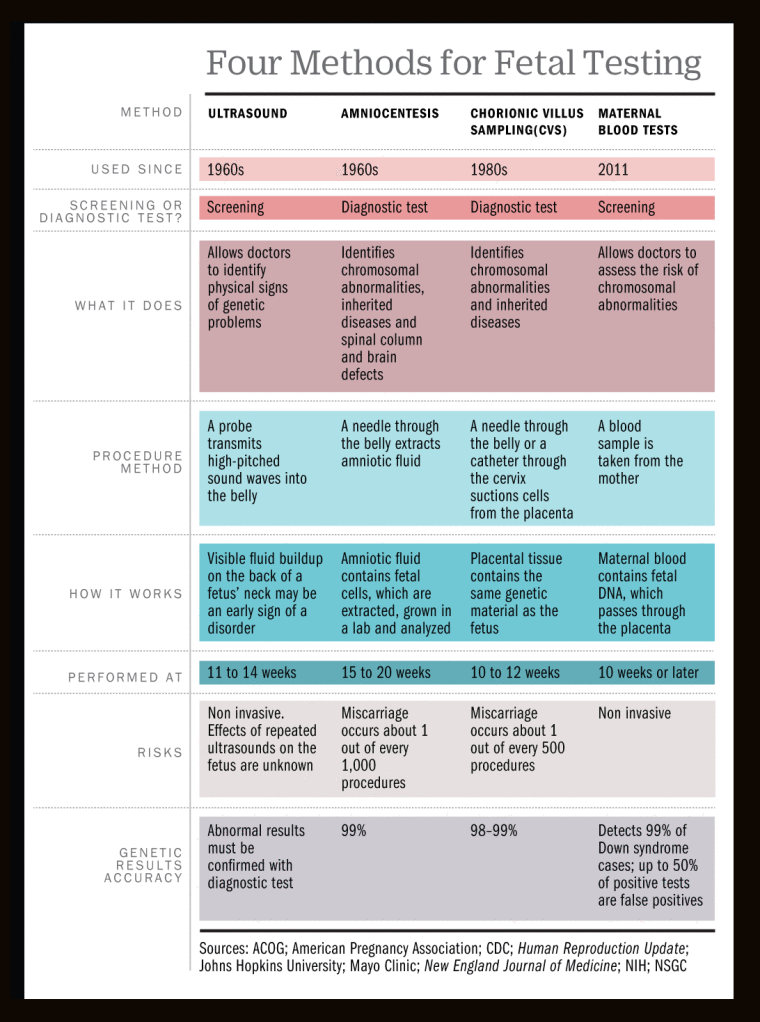 Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth. nine0033
In isthmic-cervical insufficiency, there is only one method of treatment - mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina.:max_bytes(150000):strip_icc()/hemorrhage-in-miscarriage-meaning-2371523-FINAL-f2ab04cab1cc491e964a45e682f93da5.png) The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor. nine0033
The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor. nine0033
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children. nine0033
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.
Miscarriages due to hemostasis disorders
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis). nine0033
Blood coagulation disorders leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (bleeding tendencies). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can appear even in childhood in the form of increased bleeding during cuts, tooth extractions, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop. nine0033
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of disorders in the blood coagulation system.
When planning a pregnancy, a genetic examination should be carried out and, if necessary, treatment should be initiated.
It is advisable to be examined for hidden hemostasis defects even for those who consider themselves healthy. This will allow you to predict the occurrence of complications and prevent loss. Early therapy can prevent miscarriage at 98% of cases. If defects in hemostasis are already detected during pregnancy, it can be difficult to maintain it.
What to do after a miscarriage?
Find the cause! The ideal option is to be examined by future parents: it is much more reasonable to postpone conception and spend two or three months to identify the causes than to risk getting pregnant again, spend two months waiting, and then lose everything again and still go to the doctors.
Until you understand the reason, it will not evaporate. In most cases, the answers lie on the surface. Take care of your health and your future baby. nine0033
Sign up for a consultation with an obstetrician-gynecologist by phone +7 (495) 150-60-01
Tyan Oksana Alexandrovna
Head of the department, obstetrician-gynecologist Doctor of the highest category Work experience: 26 years
Volkova Polina Dmitrievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the highest category Experience: 35 years
Postnikova Nadezhda Anatolyevna
Obstetrician-gynecologist, ultrasound specialist Work experience: 35 years
Moiseeva Alla Vitalievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the first category Work experience: 37 years
Zabolotnova Olga Valentinovna
Obstetrician-gynecologist Doctor of the first category Experience: 26 years
Shchelokova Elena Nikolaevna
Obstetrician-gynecologist Doctor of the highest category Experience: 38 years
Maksimova Tamara Anatolyevna
Obstetrician-gynecologist Experience: 7 years
Dear patients!
For your convenience and prompt provision of all the information you need, please leave your application during opening hours clinics.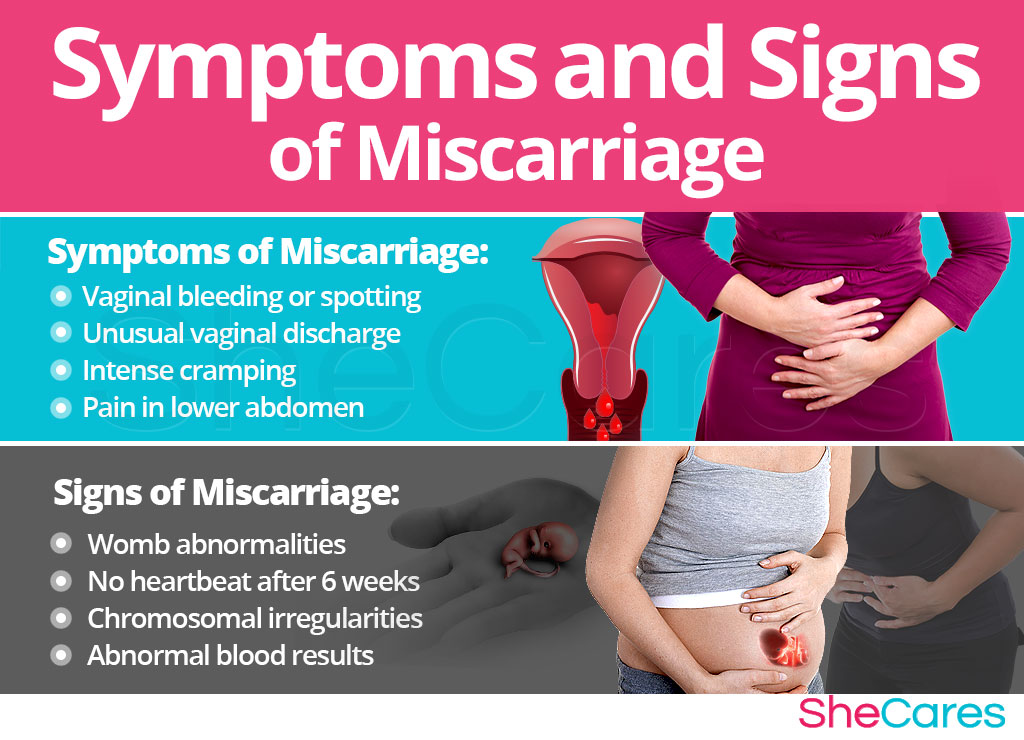
Miscarriage and miscarriage
Over the past 10 years, the number of spontaneous miscarriages has been growing rapidly. The International Histological Classification Organization (FIGO) has declared an epidemic of the situation with an increase in the frequency of miscarriages.
Spontaneous miscarriage is the termination of pregnancy before the fetus reaches a viable term (up to 22 weeks of pregnancy and fetal weight 500g.).
Most miscarriages (about 80%) occur before 12 weeks of gestation. Moreover, in the early stages up to 8 weeks of pregnancy, the cause of miscarriage is chromosomal abnormalities in 50% of cases. It turns out that nature eliminates the defective product of conception. And these causes are difficult to prevent, especially in the presence of hereditary diseases. Fortunately, accidental breakdowns are much more common than genetically determined ones. Therefore, subsequent pregnancies usually end happily.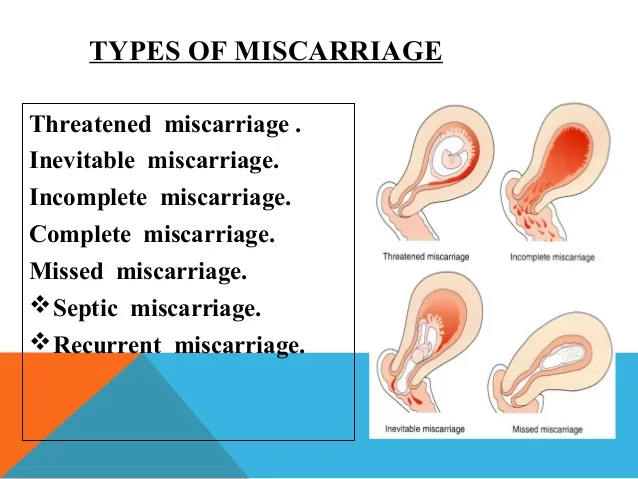 nine0083 But the remaining 50% of miscarriages have completely real and removable causes. They can be easily identified at the stage of preparation for pregnancy by a gynecologist.
nine0083 But the remaining 50% of miscarriages have completely real and removable causes. They can be easily identified at the stage of preparation for pregnancy by a gynecologist.
What are the reasons?
- chronic diseases: inflammatory diseases of the uterus and appendages, polycystic ovary syndrome, uterine fibroids, endometriosis, malformations of the genital organs.
- infections: toxoplasmosis, listeriosis, genital tuberculosis, sexual infections - chlamydia, mycoplasma, ureaplasma, syphilis. nine0177 - antiphospholipid syndrome.
- endocrine diseases: diabetes, thyroid disease.
- metabolic disorders in the body: obesity, folic acid deficiency, iron deficiency, vitamin D deficiency.
- male factor.
Of course, these causes are identified and eliminated before the planned conception.
There are harmful factors that can affect the development of the fetus in the early stages of pregnancy and lead to miscarriage:
- alcohol consumption. nine0177 - use of caffeine (4-5 cups of coffee per day).
nine0177 - use of caffeine (4-5 cups of coffee per day).
- smoking (more than 10 cigarettes per day).
- drug use.
- taking medications with a teratogenic effect (for example: aspirin, nise and others from this group of drugs; antifungals; antidepressants; some antibiotics and a number of other drugs).
- toxins and occupational hazards: ionizing radiation, pesticides, inhalation of anesthetic gases.
What are the signs of possible pregnancy loss? nine0084
These are complaints of pain in the lower abdomen and lower back, bloody discharge from the genital tract. It is necessary to consult a doctor to rule out an ectopic pregnancy and conduct an additional examination (hCG test, blood test for progesterone, ultrasound).
In early pregnancy, with dubious ultrasound data or suspected non-developing (missing) pregnancy, expectant management is chosen with a repetition of the gynecologist's examination, ultrasound, tests after 7-10 days. If the diagnosis was made and the fact of uterine pregnancy was confirmed, with a threatened miscarriage, preservation therapy is carried out in an outpatient day hospital. A miscarriage that has begun requires hospitalization in the gynecological department. In the case of a non-developing pregnancy, an abortion is performed. nine0033
A miscarriage that has begun requires hospitalization in the gynecological department. In the case of a non-developing pregnancy, an abortion is performed. nine0033
In accordance with the clinical treatment protocol approved by the Ministry of Health of the Russian Federation dated 07.06.2016. Preference is given to drug therapy aimed at terminating pregnancy with prostaglandin analogues (misoprostol) with or without prior use of an antiprogestin (mifepristone). In case of need for surgical treatment (with incomplete miscarriage with infected miscarriage), it is recommended to use aspiration curettage (with an electric vacuum source or a manual vacuum aspirator). What has a significant advantage over curettage of the uterine cavity because it is less traumatic and can be performed on an outpatient basis. nine0033
All women who have had a miscarriage need treatment to prevent complications and prevent recurrent miscarriages. Why is rehabilitation therapy necessary?
According to the decision of the XVIII World Congress of Obstetricians and Gynecologists , the diagnosis of chronic endometritis should be made to absolutely all women who have had an undeveloped pregnancy.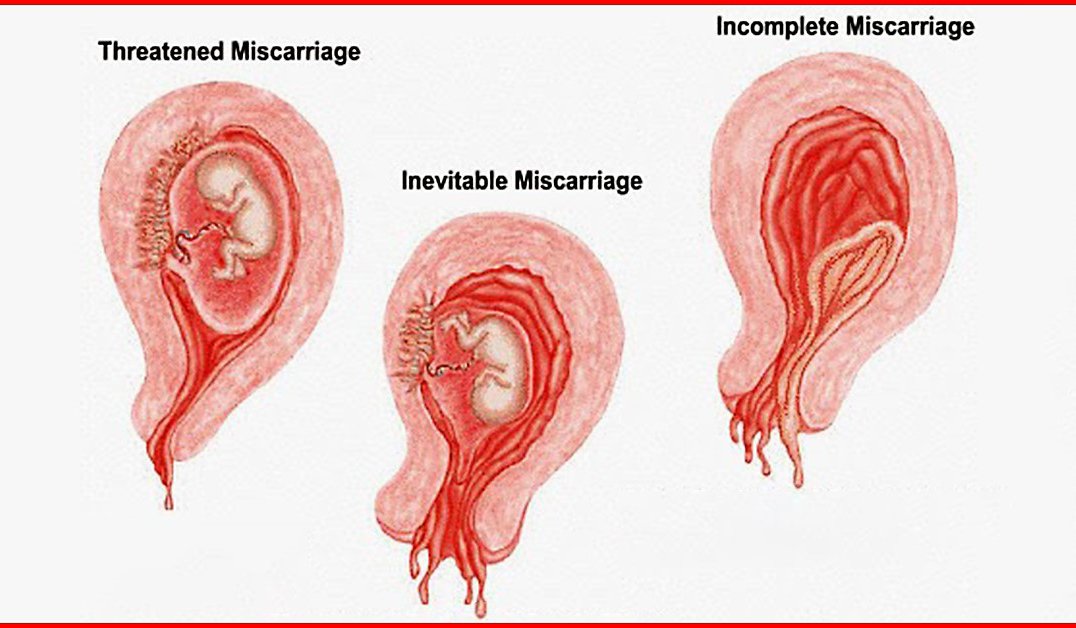 Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy. nine0177 If time is missed, it is necessary to conduct additional diagnostics: endometrial biopsy with histological examination and examination for infections, including tuberculosis. Then, taking into account the results obtained, symptomatic anti-inflammatory therapy is carried out (immunomodulators, antibacterial drugs, physiotherapy, gynecological massage, mud therapy). In parallel, an examination is prescribed to identify other causes of miscarriage (male factor, chronic maternal diseases, genital infections, antiphospholipid syndrome). nine0177 In the medical center "Mifra-Med" at the level of modern requirements of medicine, all the possibilities for a complete adequate examination have been created: all types of tests, ultrasound, hysteroscopy, aspiration biopsy, consultations of narrow specialists (endocrinologist, therapist, neurologist, urologist).
Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy. nine0177 If time is missed, it is necessary to conduct additional diagnostics: endometrial biopsy with histological examination and examination for infections, including tuberculosis. Then, taking into account the results obtained, symptomatic anti-inflammatory therapy is carried out (immunomodulators, antibacterial drugs, physiotherapy, gynecological massage, mud therapy). In parallel, an examination is prescribed to identify other causes of miscarriage (male factor, chronic maternal diseases, genital infections, antiphospholipid syndrome). nine0177 In the medical center "Mifra-Med" at the level of modern requirements of medicine, all the possibilities for a complete adequate examination have been created: all types of tests, ultrasound, hysteroscopy, aspiration biopsy, consultations of narrow specialists (endocrinologist, therapist, neurologist, urologist).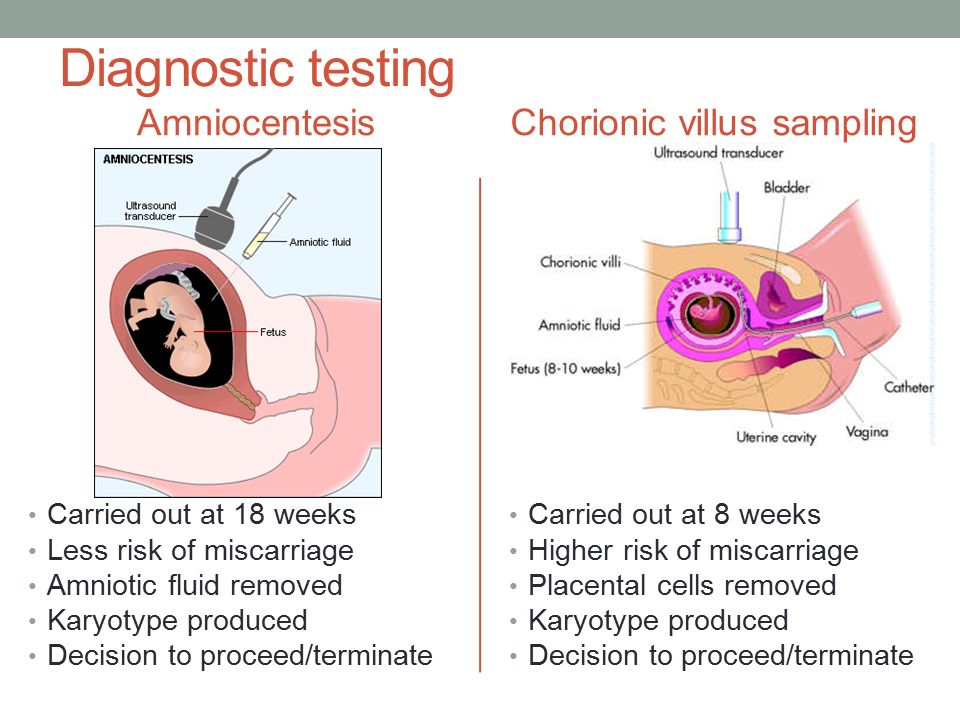

:strip_icc():format(jpeg)/kly-media-production/medias/2785562/original/028627600_1556001360-shutterstock_1019963743.jpg)