What does rh d positive mean
Rhesus disease - Causes - NHS
Rhesus disease is caused by a specific mix of blood types between a pregnant mother and her unborn baby.
It can only occur where all of the following happen, where the:
- mother has a rhesus negative (RhD negative) blood type
- baby has a rhesus positive (RhD positive) blood type
- mother has previously been exposed to RhD positive blood and has developed an immune response to it (known as sensitisation)
Blood types
There are several different types of human blood, known as blood groups, with the 4 main ones being A, B, AB and O. Each of these blood groups can either be RhD positive or negative.
Whether someone is RhD positive or RhD negative is determined by the presence of the rhesus D (RhD) antigen. This is a molecule found on the surface of red blood cells.
People who have the RhD antigen are RhD positive, and those without it are RhD negative. In the UK, around 85% of the population are RhD positive.
How blood types are inherited
Your blood type depends on the genes you inherit from your parents. Whether you're RhD positive or negative depends on how many copies of the RhD antigen you've inherited. You can inherit one copy of the RhD antigen from your mother or father, a copy from both of them, or none at all.
You'll only have RhD negative blood if you don't inherit any copies of the RhD antigen from your parents.
A woman with RhD negative blood can have an RhD positive baby if her partner's blood type is RhD positive. If the father has two copies of the RhD antigen, every baby will have RhD positive blood. If the father only has one copy of the RhD antigen, there's a 50% chance of the baby being RhD positive.
Sensitisation
An RhD positive baby will only have rhesus disease if their RhD negative mother has been sensitised to RhD positive blood. Sensitisation occurs when the mother is exposed to RhD positive blood for the first time and develops an immune response to it.
During the immune response, the woman's body recognises that the RhD positive blood cells are foreign and creates antibodies to destroy them.
In most cases, these antibodies aren't produced quickly enough to harm a baby during the mother's first pregnancy. Instead, any RhD positive babies the mother has in the future are most at risk.
How does sensitisation occur?
During pregnancy, sensitisation can happen if:
- small numbers of foetal blood cells cross into the mother's blood
- the mother is exposed to her baby's blood during delivery
- there's been bleeding during the pregnancy
- an invasive procedure has been necessary during pregnancy – such as amniocentesis, or chorionic villus sampling (CVS)
- the mother injures her abdomen (tummy)
Sensitisation can also occur after a previous miscarriage or ectopic pregnancy, or if a RhD negative woman has received a transfusion of RhD positive blood by mistake (although this is extremely rare).
How sensitisation leads to rhesus disease
If sensitisation occurs, the next time the woman is exposed to RhD positive blood her body will produce antibodies immediately.
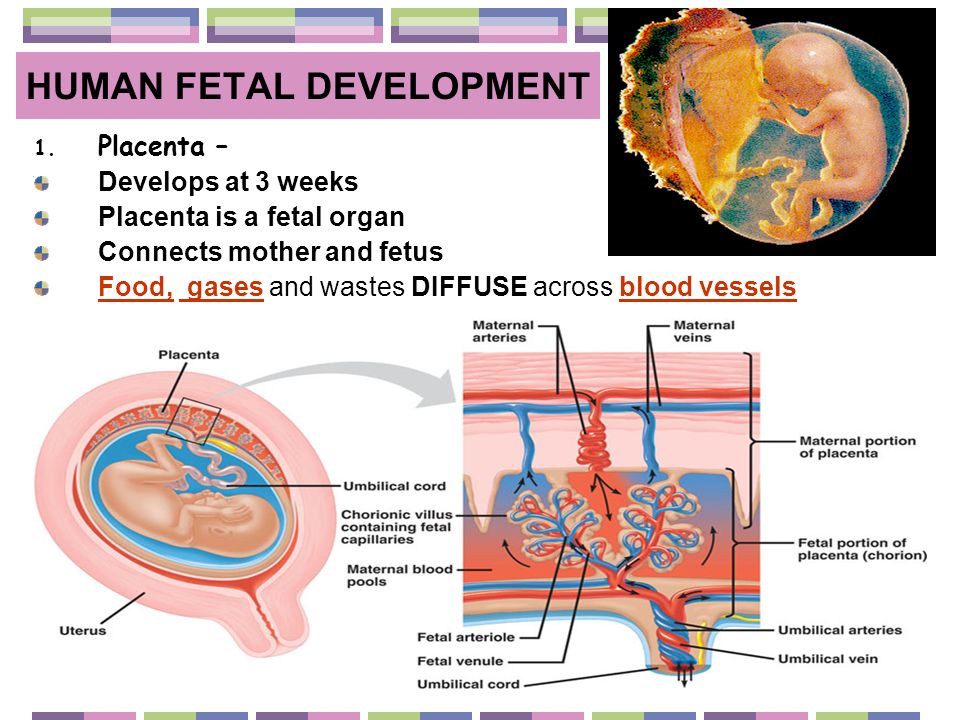
If she's pregnant with an RhD positive baby, the antibodies can lead to rhesus disease when they cross the placenta and start attacking the baby's red blood cells.
Page last reviewed: 16 November 2021
Next review due: 16 November 2024
What is my rhesus status, and how will it affect my pregnancy?
In this article
- What is my rhesus status?
- What does it mean if I'm rhesus negative?
- How does rhesus disease affect my baby during pregnancy and after birth?
- What do anti-D injections do?
- Is there a way to avoid having an anti-D injection?
- How could my baby's blood get into my blood?
- What happens if I already have antibodies in my blood?
- Where does anti-D come from, and is it safe?
- What happens after my baby is born?
What is my rhesus status?
When you have your first antenatal appointment your midwife will offer you a number of routine blood tests.
One of these tests is to find out your blood group (A, B, AB or O) and your rhesus status (positive or negative) (NCCWCH 2008, NHS 2018).
Your rhesus status is fixed by your genes:
- If you're rhesus positive (RhD positive), it means that a protein (D antigen) is found on the surface of your red blood cells. Most people are RhD positive.
- If you’re rhesus negative (RhD negative), you do not have the D antigen on your blood cells. (NHS BT 2017, NHS 2018)
What does it mean if I'm rhesus negative?
Rhesus status only matters if you are RhD negative and the baby you’re carrying is RhD positive (NHS BT 2016, NHS 2018). Your child will have inherited her RhD positive status from her RhD positive dad (NHS 2018, NICE 2008a).
Your baby's dad can have a blood test to check his rhesus status, if he’s not already aware of it from a previous health check, or from being a blood donor (NCCWCH 2008, NHS 2018).
If some of your RhD positive baby's blood enters your bloodstream, your immune system may react to the D antigen on your baby's blood cells. It will be treated as a foreign invader and your body will produce antibodies against it (NHS 2018, NICE 2008a). This is known as a sensitising event, or being sensitised (NHS BT 2016, NHS 2018).
Sensitising is not usually harmful if it is your first pregnancy. But it can cause problems if you become pregnant again with another RhD positive baby. The antibodies that your body made in your first pregnancy can quickly multiply, cross the placenta and attack the blood cells of your baby (NHS BT 2016, NHS 2018).
The good news is that, because of routine injections of a substance called anti-D immunoglobulin (anti-D) to guard against the harmful effects of antibodies, complications are rare (NHS 2018).
However, if you are not treated with anti-D, the immune response in your second pregnancy will be stronger than the first pregnancy and can cause rhesus disease in your baby (NHS BT 2016, NICE 2008a).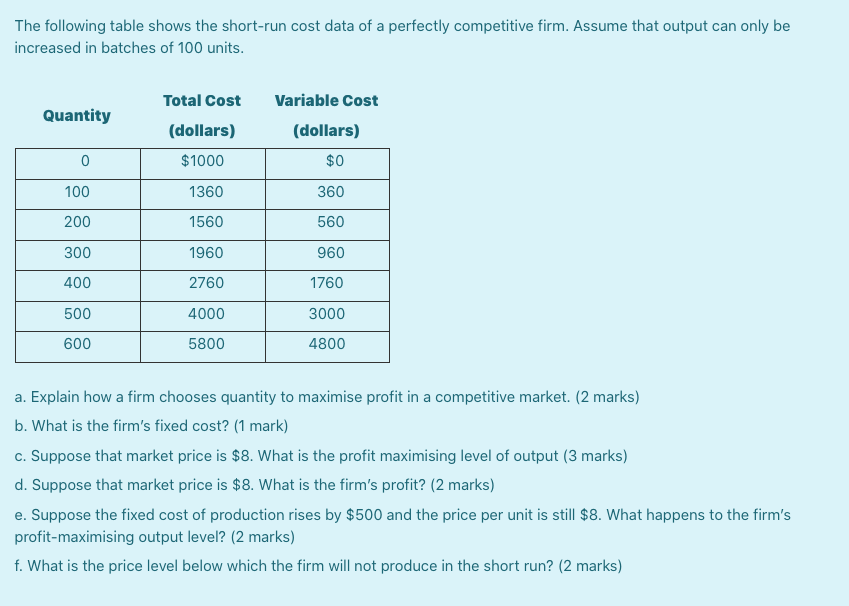 Your antibodies start to attack your baby's blood cells during pregnancy and can carry on attacking them for a few months after the birth (NHS 2018).
Your antibodies start to attack your baby's blood cells during pregnancy and can carry on attacking them for a few months after the birth (NHS 2018).
How does rhesus disease affect my baby during pregnancy and after birth?
When your baby's blood cells are attacked, rhesus disease causes anaemia. If the anaemia becomes severe, it can lead to life-threatening problems for your unborn baby, such as heart failure, fluid retention and swelling (NHS 2018, NICE 2008b).
After she’s born, your baby's liver won't be able to cope with the volume of blood cells that need breaking down. She may then become jaundiced, which is a sign of haemolytic disease of the fetus and newborn (HDFN), or haemolytic disease of the newborn (HDN).
In severe cases, HDFN can cause permanent brain damage and neurological problems in your baby, such as cerebral palsy, and physical or speech problems (NICE 2008b).
It's simple to avoid the possibility of HDFN affecting your baby, as long as you go to your antenatal appointments and have the treatment your midwife offers (NHS BT 2016, NICE 2008a, b, Qureshi et al 2014).
What do anti-D injections do?
Having an injection of anti-D can prevent your system from making antibodies (McBain et al 2015, NICE 2008a). It's important to prevent antibodies from being made, because once they're produced, they stay in your blood forever.
Anti-D works by rapidly destroying any fetal blood cells in your circulation before you can make antibodies. This means that you will not have antibodies in your system to cause haemolytic disease (HDFN) in this or your next pregnancy (NHS BT 2016).
Your midwife will inject anti-D into your upper arm, usually straight into your muscle but sometimes the injection goes into a vein (NHS BT 2016).
Your midwife is likely to offer you an anti-D jab at 28 weeks and 34 weeks of pregnancy (NHS BT 2016, NHS 2018, Qureshi et al 2014). Some maternity units offer one high-dose injection of anti-D at 28 weeks to 30 weeks pregnancy instead (NHS BT 2016, NHS 2018, Qureshi et al 2014).
You should also have anti-D within 72 hours of any possible sensitising event, when there’s a risk your baby's blood has mixed with yours (NICE 2008b, Qureshi et al 2014). See the next section for more information on what a sensitising event could be.
Is there a way to avoid having an anti-D injection?
It depends where you live. It's routine on the NHS to give anti-D to all women who are RhD negative – just in case their baby is RhD positive.
However, you only need anti-D if your baby definitely is RhD positive. Usually, you'll only find out her rhesus status after she's born. So if she turns out to be RhD negative, you'll have had anti-D needlessly. Some NHS antenatal clinics offer High-throughput, non-invasive prenatal testing (NIPT) to check your unborn baby's rhesus status.
NIPT detects your baby's DNA in your bloodstream. The DNA can be analysed to show whether your baby is RhD positive, in which case you'll need anti-D, or RhD negative, in which case you won't.
Ask your midwife whether you can have High-throughput NIPT to discover your unborn baby's rhesus status. If you're not in an area where the NHS is offering High-throughput NIPT yet for RhD negative mums, you could pay to have it done privately.
How could my baby's blood get into my blood?
Your baby's RhD positive blood would not normally mix with your Rhd negative blood at any time during your pregnancy. The placenta usually acts as a barrier between your red blood cells and your baby’s. However, even if your pregnancy is going well, it’s possible for small amounts of your baby’s blood to cross into your bloodstream (a sensitising event).
What does the placenta do?
Find out more about how the placenta supports your unborn baby.More pregnancy videos
This is most likely to happen when you give birth. Your blood and your baby's blood can mix whether you have a straightforward vaginal birth, an assisted birth or give birth by caesarean section (Qureshi et al 2014).
Mixing of your baby’s blood with yours can happen during pregnancy, though this is less likely. For example, a small area of the placenta may detach from your womb wall, causing an unnoticed bleed. This is called a concealed placental abruption (NHS BT 2016).
There are more obvious ways your blood and your baby's blood could mix. Tell your midwife if you experience any of the following:
- Vaginal bleeding.
- A threatened miscarriage. You may have bleeding and cramps in early pregnancy, but your pregnancy continues.
- A blow to your tummy, such as if you have a fall, or are involved in a car collision. (NHS BT 2016, Qureshi et al 2014)
Some procedures carry a slight risk of causing a sensitising event:
- Chorionic villus sampling (CVS) or amniocentesis.
- External cephalic version (ECV) which is performed to turn breech babies to a head-down position. (NHS BT 2016, Qureshi et al 2014)
What happens if I already have antibodies in my blood?
Your midwife will check for antibodies when you have your routine blood tests in early pregnancy, and again at 28 weeks (NCCWCH 2008).
Sometimes, a previous termination, ectopic pregnancy, or miscarriage may have caused a sensitising event without you realising (NHS BT 2016, Qureshi et al 2014).
If antibodies are detected in your blood, your midwife will not give you anti-D. Anti-D is only useful in preventing antibodies from being made. It cannot remove antibodies that are already there.
Instead, your midwife or doctor will refer you to a fetal medicine specialist, an obstetrician who is highly trained in treating unborn babies (NCCWCH 2008). You may have to travel to a different hospital if your local one doesn’t have a fetal medicine unit.
Your specialist will monitor your baby throughout your pregnancy to watch for signs of rhesus disease. Rhesus disease can cause your baby to have too few red blood cells, making her anaemic (NHS 2018).
Your specialist will use a type of ultrasound scan called a Doppler scan to check the blood flow to your baby’s brain. If your baby is affected by rhesus disease, her blood may be thinner and flow more quickly.
If your baby's blood is flowing too fast, your specialist may ask to carry out a procedure called foetal blood sampling (FBS). FBS checks whether your baby is anaemic. You’ll have a local anaesthetic to numb your belly. Your specialist will then insert a fine needle through your belly to remove a small sample of blood from your baby. You’ll be able to go home from the hospital on the same day.
There's a small chance that FBS could cause a miscarriage, so your specialist will only recommend it if he thinks it’s the best way to help your baby (NHS 2018).
If your baby is found to have severe anaemia, she can be treated by blood transfusions, even before she’s born (NHS 2018). Transfusion helps to improve the health of most unborn babies. However, it's better for some babies to be born early via induction or caesarean section, so that treatment can start earlier (NHS 2018).
After your baby is born, she is likely to be cared for in a neonatal unit. If she has jaundice after the birth, the neonatal team can treat her with phototherapy and more blood transfusions (NHS 2018, NICE 2008b). These treatments will help your baby's liver to process blood cells (NHS 2018, NICE 2008b).
These treatments will help your baby's liver to process blood cells (NHS 2018, NICE 2008b).
Most cases of rhesus disease are mild and respond well to minimal treatments (NHS 2018). However, if severe, your baby may also need an injection of a solution of antibodies to help stop her blood cells from being destroyed (NHS 2018).
Where does anti-D come from, and is it safe?
Anti-D comes from plasma, the clear yellowish fluid part of blood (NHS BT 2016). Anti-D won't harm your baby (Qureshi et al 2014).
The blood is screened for HIV, hepatitis B and hepatitis C (Qureshi et al 2014). It is also treated to inactivate any viruses, such as variant Creutzfeldt-Jakob disease (vCJD) (Qureshi et al 2014). The chance of passing on any infection is very low (NHS BT 2016).
Allergic reactions to anti-D in pregnant women are rare and unlikely to be serious (NHS 2018, Qureshi et al 2014). However, if you know you have an allergy to immunoglobulin A (IgA), you may develop a severe allergic or anaphylactic reaction, as the anti-D injection may contain trace amounts of IgA.
You should stay in the health centre or doctor's surgery for 20 minutes after having the injection and say immediately if you feel unwell.
What happens after my baby is born?
When your baby is born, a sample of her blood will be taken from the umbilical cord. This is so that her blood group and rhesus status can be determined (NHS 2018, Qureshi et al 2014). Your midwife will also ask to take a sample of blood from a vein in your arm just after you give birth, to look for antibodies (Qureshi et al 2014).
If your baby is RhD positive, your doctor or midwife will give you another injection of anti-D. You need this within 72 hours of birth to stop your immune system from reacting to your baby’s blood (NHS BT 2016, NHS 2018, Qureshi et al 2014).
If large amounts of fetal blood are found in your system, you may need a bigger dose of anti-D (Qureshi et al 2014). If your baby is RhD negative and you are too, then you will not need to have anti-D.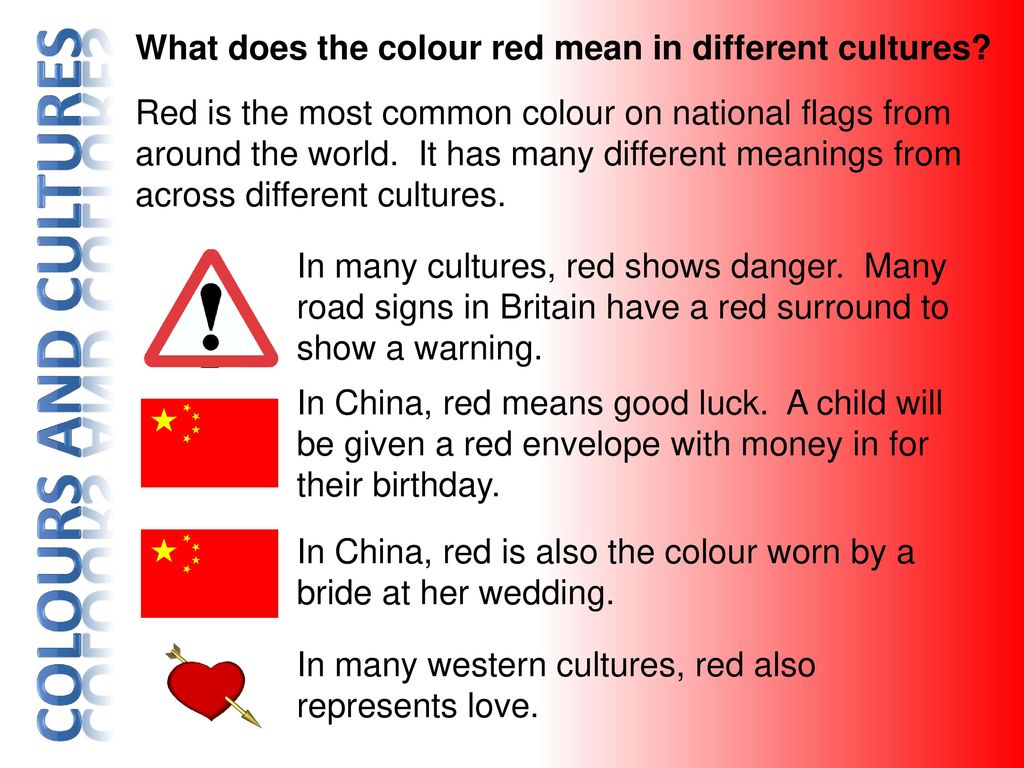
More information
- Find out when anti-D isn't necessary.
- Learn which other routine blood tests your midwife or doctor should offer you during pregnancy.
References
McBain RD, Crowther CA, Middleton P. 2015. Anti-D administration in pregnancy for preventing Rhesus alloimmunisation. Cochrane Database Syst Rev (9):CD000020. www.cochranelibrary.com [Accessed April 2019]
NCCWCH. 2008. Antenatal care: routine care for the healthy pregnant woman. National Collaborating Centre for Women's and Children's Health, Clinical guideline. www.nice.org.uk [Accessed April 2019]
NHS BT. 2016. Protecting women and babies with anti-D immunoglobulin. NHS Blood and Transplant. hospital.blood.co.uk [Accessed April 2019]
NHS BT. 2017. Blood group basics. NHS Blood and Transplant. www.blood.co.uk [Accessed April 2019]
NHS. 2018. Rhesus disease. NHS, Health A-Z. www.nhs. uk [Accessed April 2019]
uk [Accessed April 2019]
NICE. 2008a. Understanding NICE guidance: routine antenatal anti-D prophylaxis for women who are rhesus D negative. National Institute for Health and Clinical Excellence. www.nice.org.uk [Accessed April 2019]
NICE. 2008b. Routine antenatal anti-D prophylaxis for women who are rhesus D negative. National Institute for Health and Care Excellence, Technology appraisal guidance, 156. www.nice.org.uk [Accessed April 2019]
NICE. 2016. New blood test for pregnant women could help thousands avoid unnecessary treatment. National Institute for Health and Care Excellence, News and features. www.nice.org.uk [Accessed April 2019]
Qureshi H, Massey E, Kirwan D, et al. 2014. BCSH guideline for the use of anti-D immunoglobulin for the prevention of haemolytic disease of the fetus and newborn. Transfus Med 24(1):8-20. onlinelibrary.wiley.com [Accessed April 2019]
RCOG. 2011. Antepartum haemorrhage. Royal College of Obstetricians and Gynaecologists, Green-top guideline, 63. www.rcog.org.uk [Accessed April 2019]
Show references Hide references
Rh factor
Rh factor is a protein that can be found on the surface of human red blood cells. It is of great importance in the management of pregnancy and blood transfusion.
Synonyms Russian
Rh-affiliation, Rh.
Synonyms English
Rh, Rh type, Rh typing, Rh-factor, rhesus factor.
Test method
Agglutination test.
What biomaterial can be used for research? nine0006
Venous blood.
How to properly prepare for an examination?
- Eliminate fatty foods for 24 hours before the test.
- Do not smoke for 30 minutes before the test.
General information about the study
Rh factor is a protein found on the surface of red blood cells in some people. The blood of those who have it is called Rh-positive, those who do not - Rh-negative. The presence or absence of this protein is an individual feature, not a pathology. Positive Rh factor occurs in 85% of people, respectively, negative - in 15%. nine0003
The presence or absence of this protein is an individual feature, not a pathology. Positive Rh factor occurs in 85% of people, respectively, negative - in 15%. nine0003
The Rh factor is of particular importance during pregnancy. If the mother has a positive Rh factor, then her blood will in any case be compatible with the blood of the child, if it is negative, options are possible: in the case when the father of the child also has a negative Rh factor, the mother’s blood will be compatible with the will inherit a negative Rh, but when the father has a positive Rh factor, and the mother has a negative one, with a probability of 50%, incompatibility of the blood of the mother and child may occur - an Rh conflict that threatens with complications. nine0003
This happens as follows: when the blood of the fetus enters the mother's bloodstream, antibodies to its positive Rh in her body begin to be produced, since the proteins on the erythrocyte molecules are perceived by the mother's body as something alien. This is not dangerous for a woman, but antibodies through the placenta penetrate the fetal bloodstream, which threatens him with negative consequences: the antibodies “stick” to the fetal red blood cells and can cause them to stick together. This process is called hemolysis. Hemolysis during pregnancy can lead to fetal developmental disorders and, in some cases, to miscarriage, and after birth, to the so-called hemolytic jaundice of the newborn, in which a significant number of red blood cells are destroyed in the baby's blood. At the same time, the skin of the newborn turns yellow, since the breakdown products of red blood cells are colored precisely in yellow. Most often the brain is affected, dropsy may develop. In severe cases, the baby needs a blood transfusion. nine0003
This is not dangerous for a woman, but antibodies through the placenta penetrate the fetal bloodstream, which threatens him with negative consequences: the antibodies “stick” to the fetal red blood cells and can cause them to stick together. This process is called hemolysis. Hemolysis during pregnancy can lead to fetal developmental disorders and, in some cases, to miscarriage, and after birth, to the so-called hemolytic jaundice of the newborn, in which a significant number of red blood cells are destroyed in the baby's blood. At the same time, the skin of the newborn turns yellow, since the breakdown products of red blood cells are colored precisely in yellow. Most often the brain is affected, dropsy may develop. In severe cases, the baby needs a blood transfusion. nine0003
What is research used for?
- To determine a possible Rh conflict between mother and fetus. If its high probability is determined, the woman is given injections of a serum containing anti-Rh immunoglobulin, which binds to the fetal red blood cells and "hides" them from the mother's immune system, which prevents the production of antibodies to the fetal red blood cells.
- To find a donor for a safe blood transfusion. It is important to make sure that the donated blood is compatible with the recipient's blood. If the donor blood or its components contain antibodies to the protein contained on the recipient's erythrocytes, a severe transfusion reaction may develop, caused by the destruction of erythrocytes in the vascular bed. Currently, only the transfusion of blood that matches the group and Rh factor of the donor and the recipient is allowed. nine0034
When is the examination scheduled?
- During pregnancy, to confirm the woman's blood type, Rh factor and anti-Rh antibodies. This information is of great importance in the management of pregnancy.
- When donating blood. Most often, a blood transfusion is needed for:
- severe anemia,
- bleeding occurring in a patient during or after surgery,
- severe injuries, nine0033 significant blood loss,
- cancer and side effects of chemotherapy,
- bleeding disorders, in particular hemophilia.
What do the results mean?
If the woman is Rh-negative and positive for anti-Rh antibodies, the blood type and Rh factor of the child's father must be determined. If the father has a negative Rh factor, no further examination is required, if it is positive, further monitoring of the dynamics of the level of anti-Rh antibodies in the mother's blood is carried out. With its increase, a timely decision on therapy should be made. nine0003
Important notes
- Rh incompatibility between mother and fetus is currently not an obstacle to the birth of a healthy baby.
- During the first pregnancy, Rh conflict usually does not occur, since antibodies are produced slowly and in small quantities. With repeated pregnancy and subsequent, the likelihood of a Rh conflict increases.
Also recommended
- Blood type AB0
- Alloimmune anti-erythrocyte antibodies (including anti-Rhesus), titer
Who orders the examination?
Obstetrician-gynecologist, therapist, general practitioner, hematologist, transfusiologist, surgeon.
About Blood Types - Blood Center
When a doctor talks about your blood type, he usually means two things: your ABO blood type and your Rh (rhesus factor).
A person's blood group is determined by antigens found on his red blood cells. An antigen is a structure on the surface of a cell. If it is foreign to the body, then the human defense system will react to it. Therefore, it is necessary to take into account blood groups when transfusing: the donor's blood group is determined at the Blood Center, and the patient's blood group is determined before transfusion. nine0003
AB0 system
The most important is the ABO blood group system, according to which blood is divided into groups A, B, O and AB. It is determined by two antigens located on the surface of red blood cells:
- group A - only antigen A is present on the surface of erythrocytes
- group B - only antigen B is present on the surface of erythrocytes
- group AB - both A and B antigens are on the surface of erythrocytes
- group O - on the surface of erythrocytes there is neither antigen A nor antigen B.
If a person has blood type A, B or 0, then in his blood plasma there are also antibodies that destroy those antigens that the person himself does not have. Examples: If you have type A blood, then you cannot be transfused with type B blood, because in this case there are antibodies in your blood that fight against B antigens. If you have blood type 0, then your blood contains antibodies that fight like against antigens A and against antigens B.
If a person has blood type AB, then he does not have such antibodies, so he can be transfused with blood of any group. Therefore, the carrier of the AB blood group can be called universal patient.
A carrier of blood group 0 with a negative Rh factor, in turn, is called a universal donor, , since his red blood cells are suitable for all patients.
Rhesus (Rh ) accessory
Rh factor (Rh) can be positive (+) and negative (-). It depends on the presence of the D antigen on the surface of the red blood cells. If the D antigen is present, the person is considered Rh-positive, and if the D antigen is absent, then the person is Rh-negative. nine0003
It depends on the presence of the D antigen on the surface of the red blood cells. If the D antigen is present, the person is considered Rh-positive, and if the D antigen is absent, then the person is Rh-negative. nine0003
If a person is Rh negative, contact with Rh positive blood (for example, during pregnancy or blood transfusion) may form antibodies. These antibodies can cause pregnancy problems in an Rh-negative woman if she is carrying an Rh-positive baby.
In addition to the ABO and Rh systems, about thirty more blood group systems have been discovered to date. Clinically, the most important of these are the Kell, Kidd and Duffy systems. According to the Kell system, donor blood is also examined. nine0003
How is blood type determined?
To determine the blood type, it is mixed with a reagent containing known antibodies.
Three drops of blood taken from one person are applied to the base: the anti-A test reagent is added to one drop, the anti-B test reagent to the other, and the anti-D test reagent to the third, i. e. Rh test reagent. If blood clots form in the first drop, i.e. erythrocytes stick together (agglutination), then the person has antigen A. If erythrocytes do not stick together in another drop, therefore the person does not have antigen B; and if agglutination occurs in the third drop, then this indicates a positive Rh factor. In this example, the donor has blood type A and is Rh positive. nine0003
e. Rh test reagent. If blood clots form in the first drop, i.e. erythrocytes stick together (agglutination), then the person has antigen A. If erythrocytes do not stick together in another drop, therefore the person does not have antigen B; and if agglutination occurs in the third drop, then this indicates a positive Rh factor. In this example, the donor has blood type A and is Rh positive. nine0003
Donor and recipient blood group compatibility is extremely important, otherwise the recipient may have dangerous reactions to the blood transfusion.
Inheritance of blood groups
A person inherits from his father and from his mother to the same extent. Therefore, the hereditary substance has a double structure: one part from the mother and the other from the father. Speaking about the inheritance of blood groups, it must be borne in mind that:
- Most of our genes exist in two copies
- Each parent gives (based on random selection) one of these copies to their children.
- Genes occur in different versions (alleles)
- Some versions of the gene are stronger than others
| ABO system | System Rh |
| In the AB0 system, antigens are presented in three versions A, B and 0. Given that the hereditary substance includes two parts, six different combinations can occur: nine0186 | |
| Genes | |
| AA | |
| A0 | |
| AB | |
| B0 | |
| BB | |
| 00 |
The stronger part appears, both equally or a combination of them. In the AB0 system, genes A and B are stronger than 0, which affects the formation of the blood group as follows:
| Genes | Blood type | |
| AA | A | |
| A0 | A | |
| AB | AB | |
| B0 | B | |
| BB | B | |
| 00 | 0 | |
Example: The mother has a combination of A0 genes in hereditary substance, and her blood type is A (at the same time, she is a carrier of the blood type 0 gene, and there is a possibility that she will pass it on to her child).