Watery eyes while pregnant
Vision Changes During Pregnancy - Eye Floaters, Spots & More
By Jill Neimark, reviewed by Valerie Kattouf, OD
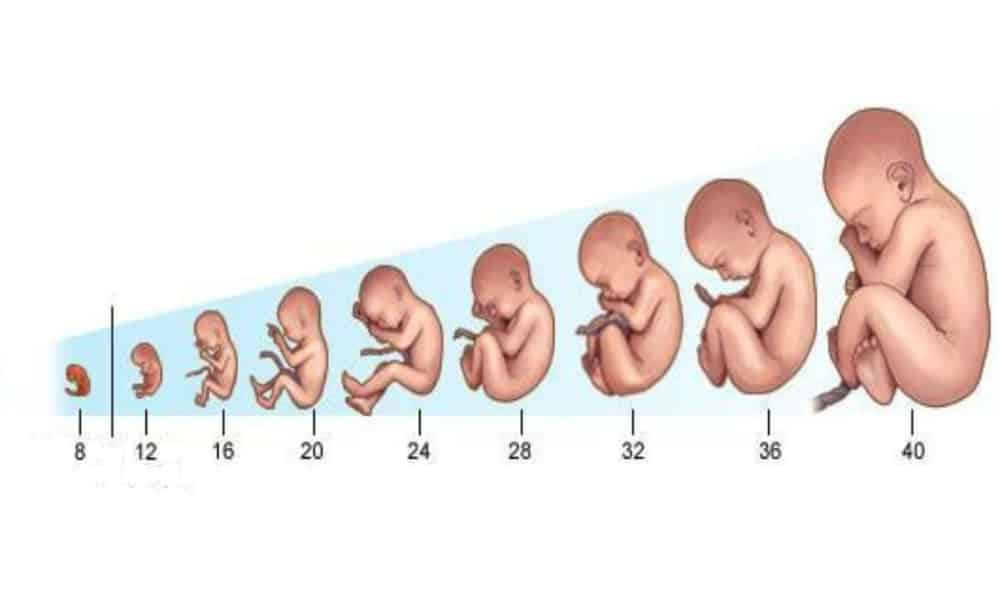
Many of the changes of pregnancy are well understood — hormonal surges, food cravings, shifts in mood, morning sickness, an expanding belly — but not all women know that vision changes can also accompany those 40 weeks of gestation.
The cascade of hormones flooding a pregnant woman’s body affects every tissue and organ, including the eyes.
Most ocular changes are transient and mild and will clear up after delivery, though a few may signal a more serious issue.
Here is an explanation of the most common eye changes of pregnancy, what causes them, and what to do about them.
Blurry vision and dry eyes
The surging hormones of pregnancy can change the quality and amount of tear production in the eye, leading to dry eye syndrome, with symptoms including excessive tearing, intermittent blurry vision and a scratchy, often burning sensation.
This occurs because the tiny, lubricating glands that line the upper and lower eyelid margins (called Meibomian glands) produce less oil to keep the eyes moist. The glands may be temporarily affected by pregnancy’s lower levels of hormones called androgens.
Symptoms of dry eye can often be treated with over-the-counter artificial tears, as well as soothing warm compresses.
Your doctor can also prescribe drops that treat the inflammatory nature of dry eye syndrome. See our informative guide on the best ways to get relief for dry eyes.
LOOKING FOR A DRY EYE SPECIALIST? Find an eye doctor near you who specializes in the treatment of dry eye syndrome.
Refractive changes
Clarity of vision depends on the way our eyes bend, or refract, light. Deviations from the norm of 20/20 are called refractive errors, which can be corrected with glasses or contact lenses.
Pregnancy can change how your eyes refract light because water retention (think of swollen feet, fingers and ankles), can thicken the cornea and alter the front surface of the eye. This may cause changes in vision.
This may cause changes in vision.
Vision will generally return to normal after childbirth.
If changes are minor, experts advise waiting until several weeks postpartum to prescribe new contact lenses or glasses.
Migraines and increased sensitivity to light
Around 40% of women of reproductive age will experience migraines at some point in their lives.
Pregnant women who suffer from migraines often experience some relief in the second and third trimesters of pregnancy, but migraines may flare in the postpartum period because of abrupt declines in estrogen levels.
Sensitivity to light, also called photophobia, is a common symptom of migraines.
“We treat migraines with pain medications that are safe for babies,” says obstetrician Keisha R. Callins, MD, MPH, clinical assistant professor at Mercer University School of Medicine in Macon, Georgia.
“We also recommend simple measures like wearing sunglasses or turning lights off in a room,” she adds.
Vision changes may warn of dangerous condition
Your eyes can provide a warning sign of a potentially serious condition during pregnancy: preeclampsia, or dangerously high blood pressure.
This complication affects around 5% of pregnant women and may occur around the 20th week of gestation.
New-onset hypertension and proteinuria (excess protein in the urine) are two cardinal symptoms of preeclampsia, and because blood pressure can soar rapidly and endanger the health of both mother and baby, medical attention is critical.
Obvious eye symptoms include blurred vision, auras of flashing lights, floaters or dark spots in the field of vision, sudden inability to focus the eyes, and even temporary blindness.
More significant eye problems can occur, though, including retinal swelling and bleeding. Headaches and digestive distress are often present.
“It’s critical not to ignore these warning signs,” Dr. Callins says. “If you have these symptoms, go to your doctor to get checked out. Hypertension in pregnancy is the No. 2 cause of maternal mortality.”
Hypertension in pregnancy is the No. 2 cause of maternal mortality.”
Dr. Callins says treatment with blood pressure medications may work, and in some cases, if the pregnancy is far enough along, early delivery is an option.
“I just delivered a baby at 31 weeks,” she says, “because the mother had a blood pressure of 200/100.”
Dr. Callins reports that both baby and mother are fine. She says that if a mother has had an episode of preeclampsia in a previous pregnancy, daily aspirin is recommended.
“It can help alleviate or prevent the problem before it occurs,” Dr. Callins says.
Diabetes and pregnancy present a risk
Mothers-to-be with diabetes must be monitored carefully during pregnancy, Dr. Callins says, because pregnancy can worsen a preexisting eye disease.
Diabetes is known to damage the small blood vessels in the retina at the back of the eye, resulting in diabetic retinopathy.
Signs of diabetic retinopathy include blurry vision, floaters and dark spots in the field of vision; fluctuating vision; dark or empty areas in the field of vision; and impaired color vision.
“Some diabetics on oral insulin may need to be converted to injectable to control their diabetes better,” Dr. Callins says.
She monitors for rare but serious complications such as retinal detachment, which requires immediate laser surgery to repair.
Gestational diabetes — a condition that flares up during pregnancy and then disappears after childbirth — can also cause blurry vision.
LOOKING FOR A VISION & DIABETES SPECIALIST? Find an eye doctor near you who specializes in the treatment of diabetes-related vision issues.
Changes in eye pressure
Our eyes contain clear fluid that is in continuous circulation and helping keep the eye “inflated” just as air keeps a balloon inflated.
Normal eye pressure changes throughout the day, usually between 10 and 21 mmHG (millimeters of mercury).
During pregnancy, eye pressure can decrease slightly.
If a pregnant woman is being treated for glaucoma, she should review her medications with her doctor to be certain they are safe during pregnancy.
Pregnancy and contact lenses
If contact lens wear is uncomfortable during pregnancy, your vision care provider may consider daily disposable soft contact lenses or specialty lenses that can address issues related to dry eye. He/she may also alter your contact lens wearing schedule.
“I often tell my patients not to wear contact lenses, or to take breaks from them, as they can be especially irritating with dry eyes during pregnancy,” says Jessica Cameron, OD, FAAO, an optometrist in the Department of Ophthalmology at the University of Florida in Gainesville.
“I also recommend a good lubrication regimen with artificial tears and ointments,” she adds.
Pregnancy and LASIK: Wait
Doctors do not recommend LASIK (refractive eye surgery) during pregnancy, since these vision changes are often temporary.
Waiting at least six months postpartum is advised for refractive surgery.
“I see these kinds of refractive changes throughout pregnancy,” Cameron says. “If a woman is really bothered, I will change her prescription, but I reassure her that this is expected and all will return to normal after delivery.”
“If a woman is really bothered, I will change her prescription, but I reassure her that this is expected and all will return to normal after delivery.”
Pregnancy and your eyes
Pregnancy is a glorious time when the body is changing rapidly, and it makes sense to nourish your entire body, including your eyes, with healthy foods and an adequate amount of rest.
Make sure to eat well, including lots of leafy green vegetables, fruits, nuts and fish high in omega-3’s, such as salmon and sardines.
Finally, get plenty of rest, keep hydrated, and look forward to the moment you will see, with your own eyes, your newborn baby.
SEE RELATED: Eye twitching during pregnancy
Page published on Friday, August 23, 2019
Pregnancy rhinitis | Pregnancy Birth and Baby
Pregnancy rhinitis | Pregnancy Birth and Baby beginning of content5-minute read
Listen
If you have unexplained breathing problems, see your doctor as soon as possible. If your breathing problems are very bad and come on quickly, call triple zero (000) for an ambulance.
If your breathing problems are very bad and come on quickly, call triple zero (000) for an ambulance.
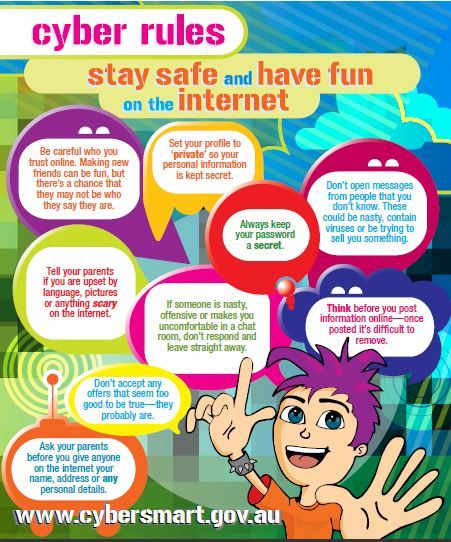
What is pregnancy rhinitis?
Pregnancy rhinitis usually involves a stuffy nose, itchy eyes, and post-nasal drip. These symptoms seem to come out of nowhere during pregnancy. While it's not a life-threatening medical condition, pregnancy rhinitis can be bothersome. There are things you can do to find some relief.
What are the symptoms pregnancy rhinitis?
Symptoms of pregnancy rhinitis are like those of allergic rhinitis (hay fever). These include:
- a runny or congested nose
- sneezing
- itchy eyes
- watery eyes
While it might feel like you are getting a cold, pregnancy rhinitis is not associated with bacterial or viral infection. This means it is not contagious.
CHECK YOUR SYMPTOMS — If you are feeling unwell and not sure what to do next, check your symptoms using the healthdirect Symptom Checker tool.
What causes pregnancy rhinitis?
Rhinitis is an inflammation of the lining of your nose.
People who are affected by allergies may also experience similar symptoms during pregnancy. In these circumstances, symptoms are triggered by one or more allergens. These allergens may be seasonal, such as:
- pollens
- fungi
- moulds
Or they can be perennial (year-round) such as:
- dust mites
- pets
- cockroaches
Rhinitis in pregnancy may also have a non-allergic origin. It's not known exactly why rhinitis occurs more frequently in pregnancy. Some research suggests that factors such as hormones increase the likelihood of rhinitis during pregnancy.
Smoking is also associated with pregnancy rhinitis. It's never too late for future parents to quit smoking.
How is pregnancy rhinitis diagnosed?
Pregnancy rhinitis should be distinguished from other conditions such as infections. Your doctor can do this during a routine visit.
Your doctor can do this during a routine visit.
You may have a breathing problem if:
- you feel you can't get enough air through both your nose and mouth
- you are breathless
- you feel like you're being suffocated
- your chest feels very tight
- you are needing more of your usual asthma or lung medications
If you have unexplained breathing problems, see your doctor as soon as possible. If your breathing problems are very bad and come on quickly, call triple zero (000) for an ambulance.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How long will my symptoms last?
While pregnancy rhinitis can occur at any time during your pregnancy, it is most common during the first trimester.
Symptoms may last for at least 6 weeks. The good news is they usually disappear within 2 weeks of your baby's birth.
How is pregnancy rhinitis treated?
Your pregnancy rhinitis may be triggered by a known allergen. If this is the case, you can try and avoid or limit your exposure to the allergen.
Nasal irrigation is a drug-free technique to clear out air-borne allergens and mucus from blocked nostrils.
Using salt water (saline) nasal sprays can provide relief and is a good solution during pregnancy.
Persistent symptoms are managed individually. If you have itchy-watery eyes, there are certain eye drops that are approved for use during pregnancy. Similarly, specific medicated nasal sprays and antihistamines can be used.
However, always check with your doctor or pharmacist before taking any medicine while pregnant.
Is there an impact on my unborn baby?
There are insufficient studies to fully understand the impact of pregnancy rhinitis on the growth and development of unborn babies.
However, any condition that reduces your quality of life has the potential to affect your baby. This includes the quality of your sleep during pregnancy.
This includes the quality of your sleep during pregnancy.
If you are concerned about your sleep or breathing during pregnancy, speak to your doctor. They can help you find the best way to clear your breathing passages and improve your sleep.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Auris Nasus Larynx (Medical Management of rhinitis in pregnancy), American Journal of Rhinology & Allergy (Redefining Pregnancy-induced Rhinitis), International Journal of Chemistry, Mathematics and Physics (Chronic Rhinosinusitis and Its Impact on Pregnancy), South Eastern Sydney Local health District/The Royal Hospital for Women (Hay Fever in Pregnancy and Breastfeeding), The Royal Women’s Hospital (Medicines in Pregnancy), Australasian Society of Clinical Immunology and Allergy (ASCIA) (Allergic Rhinitis Clinical Update)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Related pages
- Allergies and hay fever during pregnancy
- Cold and flu during pregnancy and breastfeeding
- Allergies: controlling your environment
- Airborne allergies
- Medicines during pregnancy
Need more information?
Allergic rhinitis - symptoms, causes and treatment - MyDr.com.au
Rhinitis means inflammation of the lining of the nose. Allergic rhinitis means that this inflammation is caused by an allergy.
Read more on myDr website
Allergic rhinitis (hay fever)? - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Allergic rhinitis (commonly known as hay fever) affects around 18% of people in Australia and New Zealand. It can affect children and adults.
It can affect children and adults.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Allergic Rhinitis (hayfever) - Allergy & Anaphylaxis Australia
Allergic rhinitis (hay fever) is one of the most common allergic conditions affecting 1 in 5 people in Australia. It is caused by the body’s immune system reacting to common allergens in the environment such as pollen, house dust mite, moulds and animal danders (skin cells and fur).
Read more on Allergy and Anaphylaxis Australia website
Hay Fever (Allergic Rhinitis) - Australasian Society of Clinical Immunology and Allergy (ASCIA)
The Australasian Society of Clinical Immunology and Allergy (ASCIA) is the peak professional body of clinical immunology and allergy in Australia and New Zealand. ASCIA promotes and advances the study and knowledge of immune and allergic diseases, including asthma.
ASCIA promotes and advances the study and knowledge of immune and allergic diseases, including asthma.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Immunotherapy for Allergic Rhinitis (Hay Fever) - Allergy & Anaphylaxis Australia
Allergen Immunotherapy (AIT) has been used for over 100 years and is a proven treatment providing long-term relief for hay fever. The aim of AIT is to help people react less to their trigger allergen/s that cause symptoms (such as grass pollen/house dust mite). This means having no/less symptoms and a better quality of life.
Read more on Allergy and Anaphylaxis Australia website
Pollen - a trigger for hay fever - National Asthma Council Australia
Plant pollen is well known as a trigger for seasonal allergic rhinitis (hay fever) and seasonal allergic conjunctivitis. Up to four out
Up to four out
Read more on National Asthma Council Australia website
Hay Fever & Asthma | Hay Fever-related Asthma Causes & Symptoms - Asthma Australia
Hay fever is a common allergy, also known as allergic rhinitis, that can also trigger asthma flare-ups. Learn more about hay fever-related asthma & symptoms here.
Read more on Asthma Australia website
Other Allergic Conditions - Allergy & Anaphylaxis Australia
Other Allergic Conditions included: Urticaria (Hives), Eczema (Atopic Dermatitis), Allergic Conjunctivitis, Allergic Rhinitis (hayfever), Sinusitis
Read more on Allergy and Anaphylaxis Australia website
Thunderstorm asthma - Australasian Society of Clinical Immunology and Allergy (ASCIA)
It seems reasonable to think that rain would relieve allergic rhinitis (hay fever) and asthma triggered by pollen, by washing pollen out of the air. However, rain from some thunderstorms can make some people's symptoms worse. Epidemics of thunderstorm asthma in Australia have occurred in Melbourne and Wagga Wagga.
However, rain from some thunderstorms can make some people's symptoms worse. Epidemics of thunderstorm asthma in Australia have occurred in Melbourne and Wagga Wagga.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Allergy Treatments - Australasian Society of Clinical Immunology and Allergy (ASCIA)
The Australasian Society of Clinical Immunology and Allergy (ASCIA) is the peak professional body of clinical immunology and allergy in Australia and New Zealand. ASCIA promotes and advances the study and knowledge of immune and allergic diseases, including asthma.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.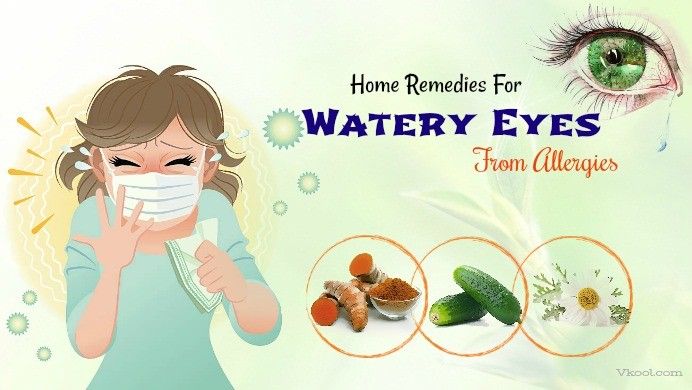
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.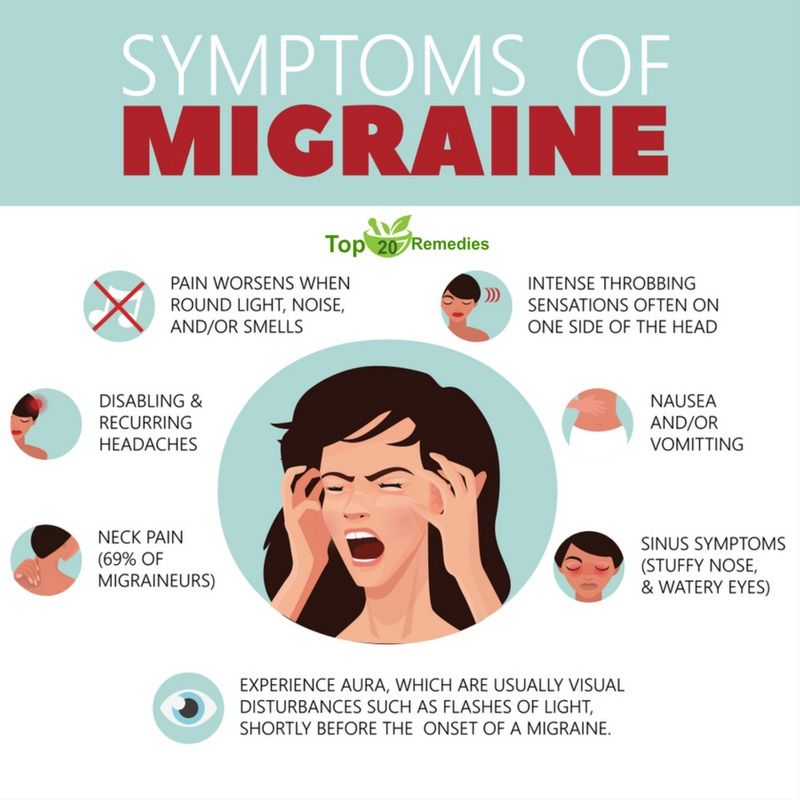
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
why vision falls and deteriorates
Our doctors
Horonenko
Elena
ValerievnaNurse of the highest qualification category More about the doctor All doctors of the clinic
Ask a question to the doctors of the clinic
Patients' reviews
Ilona-AirisKuopio-Finland /25
Davydova Irina Vasilievna performed an operation on me. Thanks to everyone, all the staff are very polite! The doctor is especially good. Eyes checked, explained. Vision returned 100% While it is slightly painful to see, but I see everything as in childhood. I am very excited! Very good clinic!
Thanks to everyone, all the staff are very polite! The doctor is especially good. Eyes checked, explained. Vision returned 100% While it is slightly painful to see, but I see everything as in childhood. I am very excited! Very good clinic!
All reviews
- Home
- For patients
- Useful materials
- What happens to vision during pregnancy
During pregnancy, a woman's body is rebuilt, because its main goal now is to support the life of the fetus and prepare for childbirth . This process affects all organs and systems, including the optical one. Pregnancy affects the condition of the eyes in different ways:
- the physiology of the organ of vision changes, but, as a rule, temporarily;
- eye diseases occur;
- existing pathologies are aggravated;
- common systemic diseases give complications to the eyes.

Physiological changes are one of the causes of visual impairment during pregnancy
The structure of the eye changes due to the restructuring of the hormonal, hemodynamic, metabolic and immune systems of the body:
- The eyeball lengthens. Associated with this is some deterioration in vision during pregnancy, which usually recovers after lactation is completed.
- In expectant mothers, the secretion of the lacrimal gland decreases, which is manifested by signs of the "dry eye" syndrome.
- redness, dryness, burning sensation, foreign body sensation, increased photosensitivity. To relieve discomfort, the ophthalmologist prescribes special drops.
- Reduced sensitivity of the cornea, which is fraught with injury.
- Conversely, the curvature and thickness of the cornea increase. Together with a change in the lens, this gives blurred vision with glasses and contact lenses, in which the patient felt normal before pregnancy.
 After lactation, this should pass, so it makes no sense to do laser correction or change glasses while expecting a baby.
After lactation, this should pass, so it makes no sense to do laser correction or change glasses while expecting a baby. - Intraocular pressure decreases, and this should be taken into account by the doctor if the patient has a diagnosis of glaucoma.
Visual defects occurring during pregnancy
Ophthalmic pathologies usually do not appear on their own, but develop against the background of hypertension, preeclampsia, eclampsia. A woman may complain of visual disturbances: blurred vision, photopsy, loss of part of the visual field, double vision, decreased central vision. In most cases, after childbirth, the symptoms disappear. leads to the restoration of vision.
Various brain tumors, inflammatory and autoimmune diseases, multiple sclerosis, diabetes can cause ophthalmic pathologies in pregnant women. Such women must be observed by an ophthalmologist.
The technologies used in the Laser Eye Microsurgery Clinic can correct or stop serious malfunctions of the optical system. Competent and timely assistance of an ophthalmologist will preserve your vision.
Competent and timely assistance of an ophthalmologist will preserve your vision.
Eye health during pregnancy
Pregnancy is a special period in a woman's life. Organs adapt to new conditions and function differently. The eyes are no exception. In the past, cesarean sections were often prescribed by eye doctors due to poor eyesight and eye diseases, but it has been scientifically proven that only in rare cases are women unable to give birth themselves due to eye diseases.
Nowadays, there are no strict guidelines for examining the condition of the eyes during pregnancy. However, all pregnant women should visit an ophthalmologist, especially if there are visual impairments, such as myopia, and also if there have been injuries, diseases or eye surgeries.
One of the most common reasons why a caesarean section was previously prescribed due to vision problems is retinal disease. During childbirth, when the baby comes out, there is a strong muscle tension, which causes pressure in the eyes. A lot of force and pressure on the retina can affect its condition and create more severe damage if there was any previous retinal disease.
A lot of force and pressure on the retina can affect its condition and create more severe damage if there was any previous retinal disease.
Therefore, regardless of whether a woman wears glasses every day or does without them, it would be advisable for every pregnant woman to check the condition of the retina before childbirth. Since the eye and vision test does not pose a risk to the expectant mother or baby, it can be done as early as the first trimester of pregnancy. If the eye doctor sees changes in the retina during the visit, the pregnant woman still has enough time before the birth to prevent them in time, and most likely the birth can be natural. The high-risk group also includes women with a high degree of myopia, which is characterized by various degenerative processes in the retina and vascular tract; pregnant women with diabetes mellitus, autoimmune diseases, high blood pressure, toxicosis.
If the eye doctor detects damage to the retina during the visit, the patient can undergo laser photocoagulation of the retina, which limits the location of the lesion, the retinal tissue is fixed.
It is also advisable to check the eyes after childbirth to assess whether retinal tears have formed during childbirth. If changes in the retina have already formed before childbirth, it is recommended to visit an eye doctor as soon as possible to make sure that damage to the retina does not progress and immediate treatment is not required.
What is the retina?
The retina is the inner lining of the eyeball. It consists of neurons that perceive light stimulation, which allows us to see. If the retina is torn, it can begin to flake off, resulting in impaired or even loss of vision.
If a retinal tear is diagnosed in time, it can be limited with a laser, thus preventing retinal detachment. Sudden flashes of light, flies, or spots in the field of vision may indicate a retinal tear. If detachment has already occurred, the laser can no longer be used - surgery is required. Therefore, it is especially important to detect a retinal tear as soon as possible.