Placenta not working
Placental insufficiency – what it is and how it can affect a pregnancy
Placental insufficiency – what it is and how it can affect a pregnancy | Pregnancy Birth and Baby beginning of content6-minute read
Listen
It’s important to see your doctor or medical team as soon as possible if you have any concerns when you are pregnant. If you have bleeding and/or significant pain, call triple zero (000) for an ambulance or go to your nearest hospital emergency department.
What is placental insufficiency?
The placenta delivers oxygen and nutrients to your baby. Placental insufficiency is when the placenta does not work properly. It’s not very common but it is serious, and can affect the growth and wellbeing of your baby.
If you have placental insufficiency, your baby may not grow as expected, leading to complications during pregnancy or birth.
What causes placental insufficiency?
Placental insufficiency occurs because the placenta doesn’t implant and grow properly in your uterus, or because it’s damaged. Sometimes there is no obvious cause.
The risk of placental insufficiency can be increased if you have medical conditions or other risk factors, such as:
- diabetes
- pre-eclampsia
- blood clotting conditions
- certain infections
- if you smoke drink alcohol or use illegal or recreational drugs
- high blood pressure, kidney problems or heart disease
- if you have had complications earlier in this pregnancy, particularly heavy bleeding
- older age during pregnancy (older than 40 years)
- if you have previously had a small baby, pre-eclampsia or stillbirth
How is placental insufficiency diagnosed?
Placental insufficiency may be picked up during your routine antenatal visits and tests.
Your doctor or midwife will measure and track the growth of your uterus and the baby.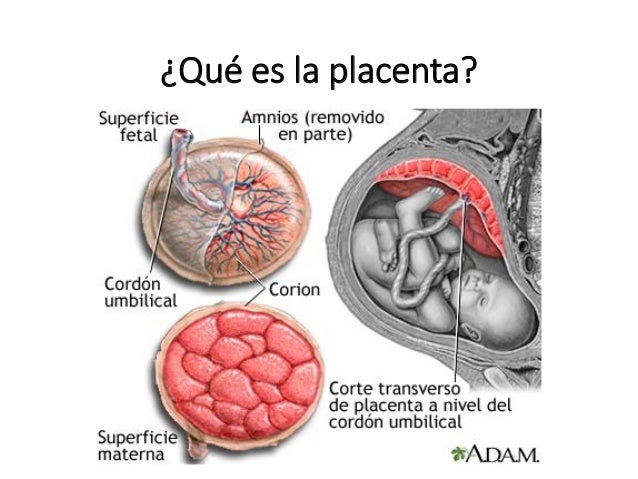 Placental insufficiency may be diagnosed during a routine ultrasound if your baby isn’t growing as expected.
Placental insufficiency may be diagnosed during a routine ultrasound if your baby isn’t growing as expected.
Sometimes pregnant women may notice that their tummy isn’t growing, is smaller than in previous pregnancies or their baby isn’t moving as much. If you have any concerns during your pregnancy, contact your midwife or doctor immediately.
Diagnosing placental insufficiency early is important for the health of the mother and baby.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
What are the risks to you and your baby?
Placental insufficiency can lead to problems both for mother and baby.
For the mother, it can be linked to conditions such as:
- pre-eclampsia
- other problems with the placenta, including placental abruption (when the placenta comes away from the wall of the uterus)
- preterm labour and delivery
If the placenta does not develop properly, it can also lead to problems for your baby. When the baby doesn’t get enough oxygen and nutrients, it can prevent normal growth and development. This is known as fetal growth restriction (FGR).
When the baby doesn’t get enough oxygen and nutrients, it can prevent normal growth and development. This is known as fetal growth restriction (FGR).
Some of the challenges that babies with FGR can have include:
- breathing or heart problems
- low oxygen levels at birth
- difficulty maintaining body temperature
- trouble feeding and gaining weight
- infection
- bleeding on the brain (called ‘intraventricular haemorrhage’)
- problems with their eyes and vision
- problems with their bowel
These conditions are more likely in premature babies.
How is placental insufficiency managed?
If your doctor suspects placental insufficiency, they will keep a close eye on how your baby is growing and developing. They will monitor you and your baby regularly and may arrange for you to give birth in a major hospital with appropriate medical support.
You will be asked to keep a record of your baby's movements and let your medical team know if you notice any changes.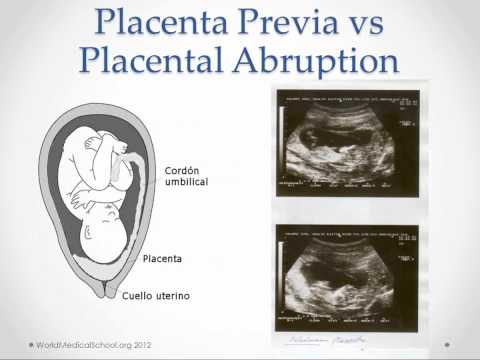
At any stage of your pregnancy, if you are concerned about your baby's movements, contact your midwife or doctor immediately. Do not wait until the next day. A slowing down of movement may be a sign that your baby is unwell.
You will likely need more frequent ultrasounds and have regular monitoring of your baby’s heart rate to assess their growth and wellbeing.
Treatment will depend on the stage of the pregnancy. If you’re under 37 weeks, your doctor may recommend waiting for as long as possible and keeping a close eye on the baby. But if there are signs that your baby is not well, it may be safest to induce labour or deliver your baby with a caesarean.
If your baby hasn’t been growing as expected, they may require additional support from the medical team at birth. The team will care for your baby, keep them warm and may help them to breathe with an oxygen mask or breathing tube.
Your baby may need to be transferred to the neonatal intensive care unit (NICU) or special care nursery for extra care.
It’s important to see your doctor or medical team as soon as possible if you have any concerns when you are pregnant. If you have bleeding and/or significant pain, call triple zero (000) for an ambulance or go to your nearest hospital emergency department.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Department of Health and Aged Care (Fetal growth restriction and well-being), Clinical Medicine Insights: Pediatrics (Intrauterine Growth Restriction: Antenatal and Postnatal Aspects), Elsevier, ScienceDirect (Placental Insufficiency), Perinatal Society of Australia and New Zealand/Stillbirth Centre of Research Excellence (Position Statement: Detection and Management of Fetal Growth Restriction in Singleton Pregnanciex)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Related pages
- About the placenta
- Placenta complications in pregnancy
Need more information?
Causes of Preterm Labour - Miracle Babies
There are many causes of preterm birth
Read more on Miracle Babies Foundation website
Causes - Miracle Babies
Every year in Australia around 48,000 newborn babies require the help of a NICU or SCN, there are many factors linked to premature birth and also many that remain unexplained
Read more on Miracle Babies Foundation website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.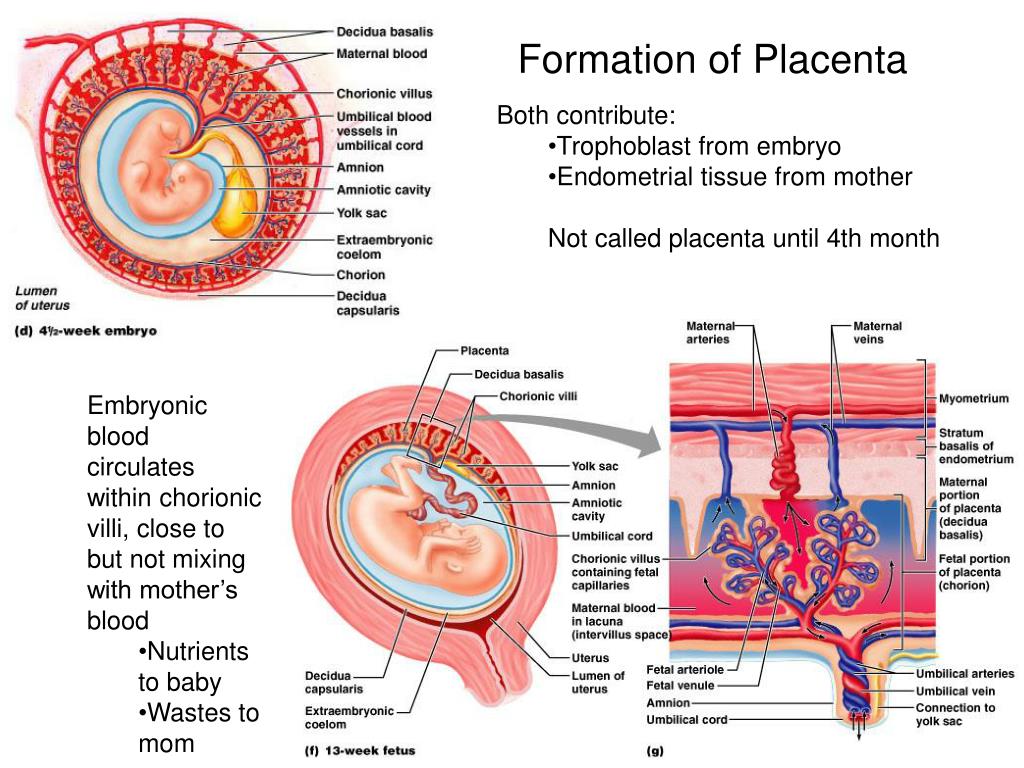
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.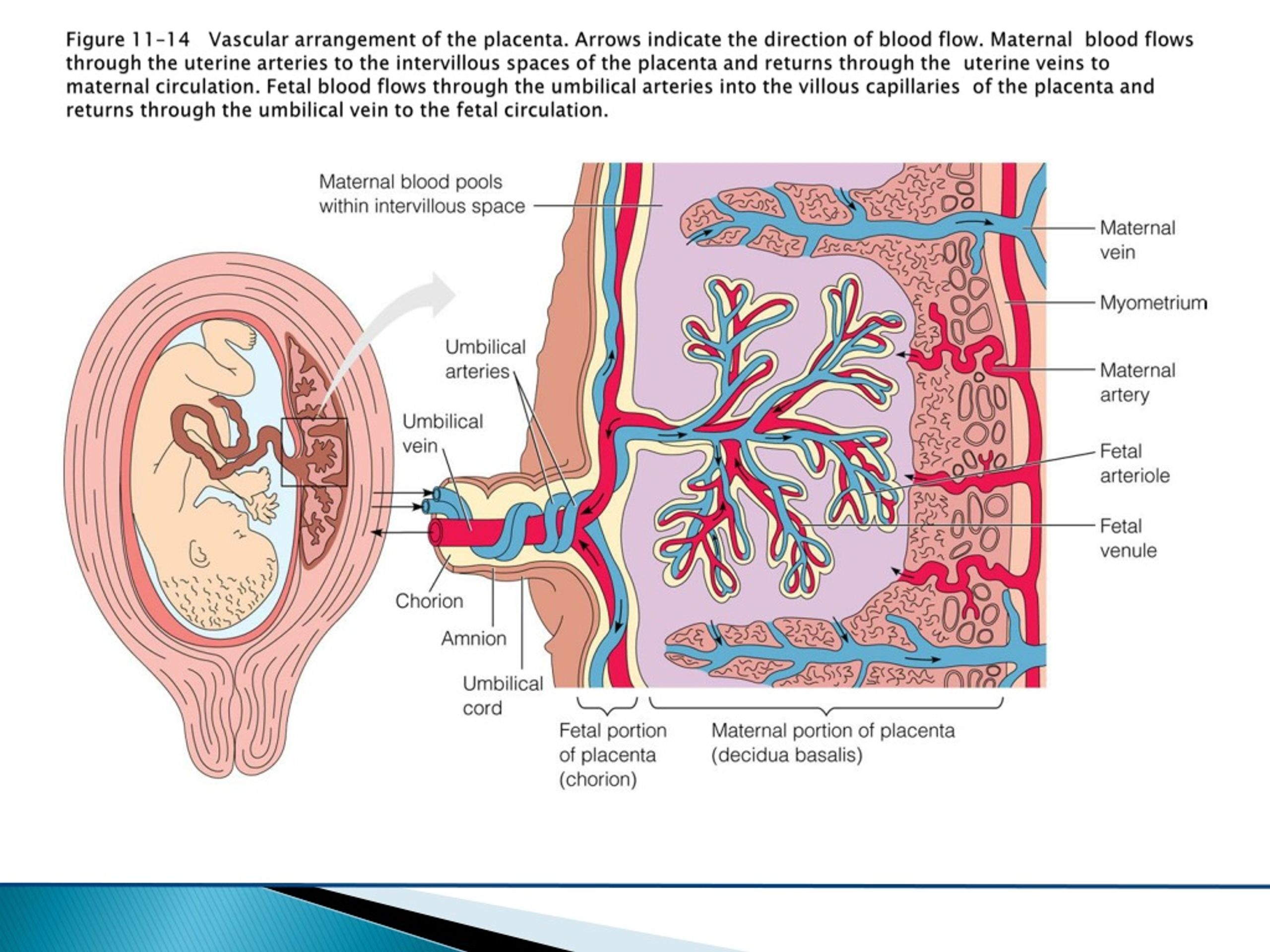
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.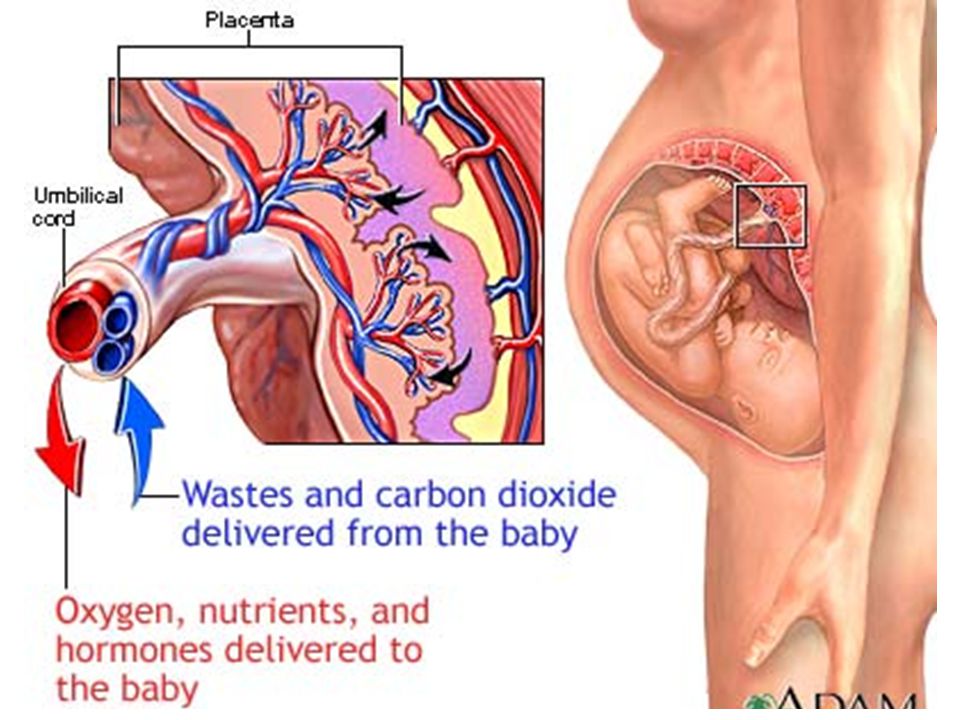
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Placental insufficiency Information | Mount Sinai
Placental dysfunction; Uteroplacental vascular insufficiency; Oligohydramnios
The placenta is the link between you and your baby. When the placenta does not work as well as it should, your baby can get less oxygen and nutrients from you. As a result, your baby may:
As a result, your baby may:
- Not grow well
- Show signs of fetal stress (this means the baby's heart does not work normally)
- Have a harder time during labor
The placenta provides the fetus with oxygen and nutrients and takes away waste such as carbon dioxide via the umbilical cord.
In the placenta, nutrients, wastes, and gases are exchanged between the mothers blood and the babys blood.
Causes
The placenta may not work well, either due to pregnancy problems or social habits. These may include:
- Diabetes
- Going past your due date
- High blood pressure during pregnancy (called preeclampsia)
- Medical conditions that increase the mother's chances of blood clots
- Smoking
- Taking cocaine or other drugs
- Anemia
Certain medicines can also increase the risk for placental insufficiency.
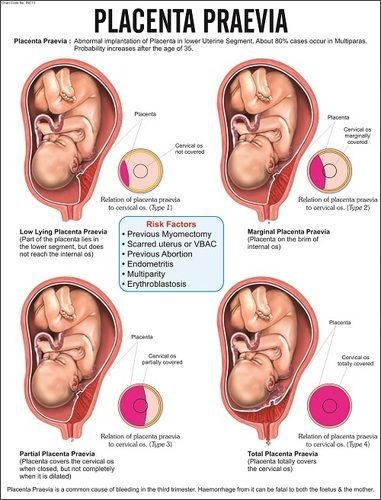
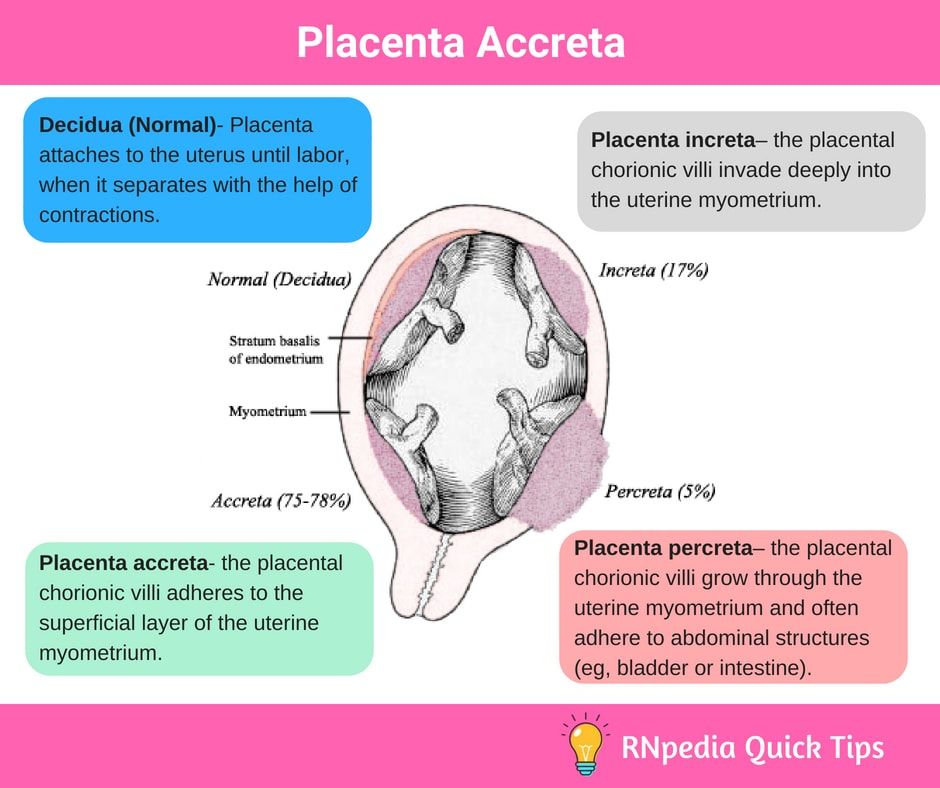
In some cases, the placenta:
- May have an abnormal shape
- May not grow big enough (more likely if you are carrying twins or other multiples)
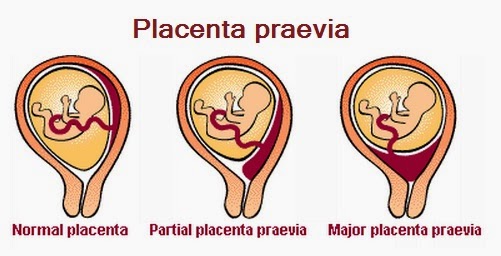
- Does not attach correctly to the surface of the womb
- Breaks away from the surface of the womb or bleeds prematurely
Symptoms
A woman with placental insufficiency usually does not have any symptoms. However, certain diseases, such as preeclampsia, which can be symptomatic, can cause placental insufficiency.
However, certain diseases, such as preeclampsia, which can be symptomatic, can cause placental insufficiency.
Exams and Tests
Your health care provider will measure the size of your growing womb (uterus) at each visit, starting about halfway through your pregnancy.
If your uterus is not growing as expected, a pregnancy ultrasound will be done. This test will measure your baby's size and growth, and assess the size and placement of the placenta.
Other times, problems with the placenta or your baby's growth may be found on a routine ultrasound that is done during your pregnancy.
Either way, your provider will order tests to check how your baby is doing.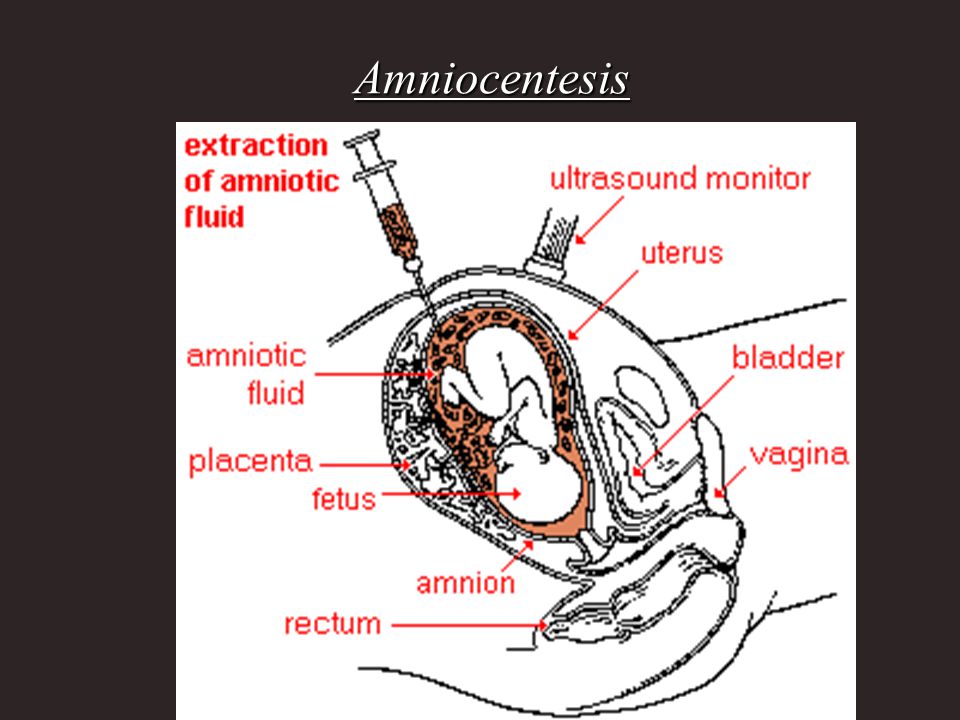 The tests may show that your baby is active and healthy, and the amount of amniotic fluid is normal. Or, these tests can show that the baby is having problems.
The tests may show that your baby is active and healthy, and the amount of amniotic fluid is normal. Or, these tests can show that the baby is having problems.
You may be asked to keep a daily record of how often your baby moves or kicks.
Treatment
The next steps your provider will take depend on:
- The results of tests
- Your due date
- Other problems that may be present, such as high blood pressure or diabetes
If your pregnancy is less than 37 weeks and the tests show that your baby is not under too much stress, your provider may decide to wait longer. Sometimes you may need to get more rest. You will have tests often to make sure your baby is doing well. Treating high blood pressure or diabetes may also help improve the baby's growth.
Treating high blood pressure or diabetes may also help improve the baby's growth.
If your pregnancy is over 37 weeks or tests show your baby is not doing well, your provider may want to deliver your baby. Labor may be induced (you will be given medicine to make labor start), or you may need a cesarean delivery (C-section).
Outlook (Prognosis)
Problems with the placenta can affect the developing baby's growth. The baby cannot grow and develop normally in the womb if it does not get enough oxygen and nutrients.
Possible Complications
Complications associated with placental insufficiency may include:
- Preeclampsia
- Preterm labor
- Intrauterine growth restriction (IUGR)
- Placental abruption or premature separation of the placenta
- Decreased oxygen delivery to the baby at birth
- Increased risk for fetal loss
Prevention
Getting prenatal care early in pregnancy will help make sure that the mother is as healthy as possible during the pregnancy.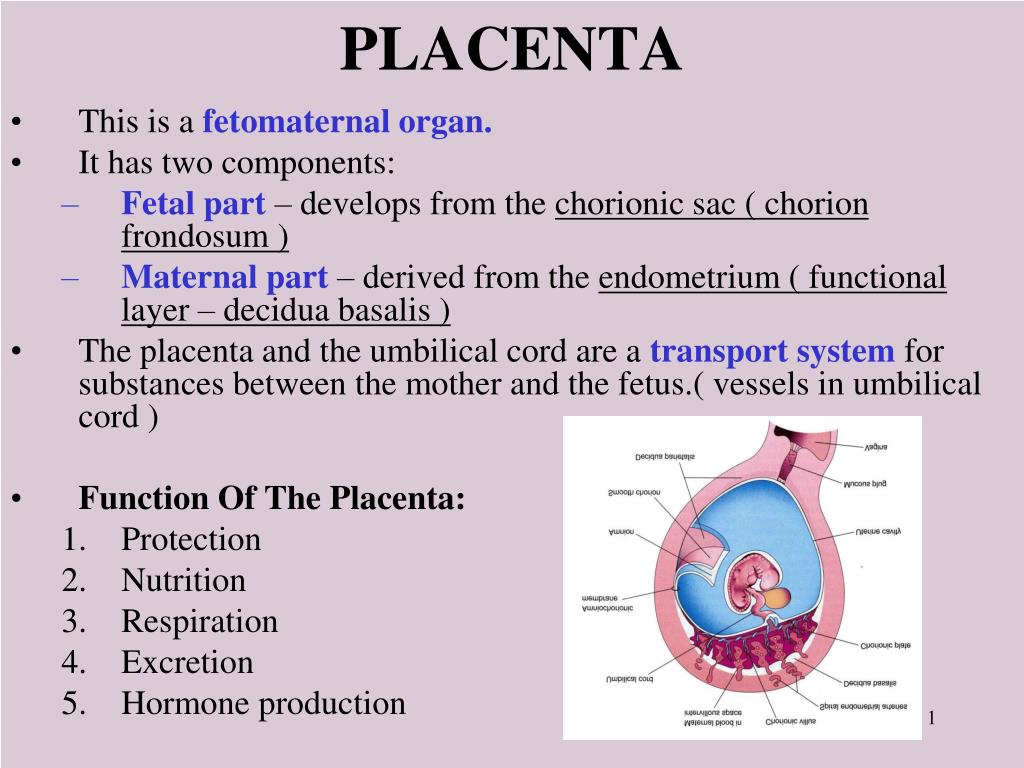
Smoking, alcohol, and other recreational drugs can interfere with the baby's growth. Avoiding these substances may help prevent placental insufficiency and other pregnancy complications.
Benson AE, Branch DW. Collagen vascular diseases in pregnancy. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 51.
Lausman A, Kingdom J; Maternal Fetal Medicine Committee, et al. Intrauterine growth restriction: screening, diagnosis, and management. J Obstet Gynaecol Can. 2013;35(8):741-748. PMID: 24007710 pubmed.ncbi.nlm.nih.gov/24007710/.
Rampersad R, Macones GA. Late- and postterm pregnancy. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies.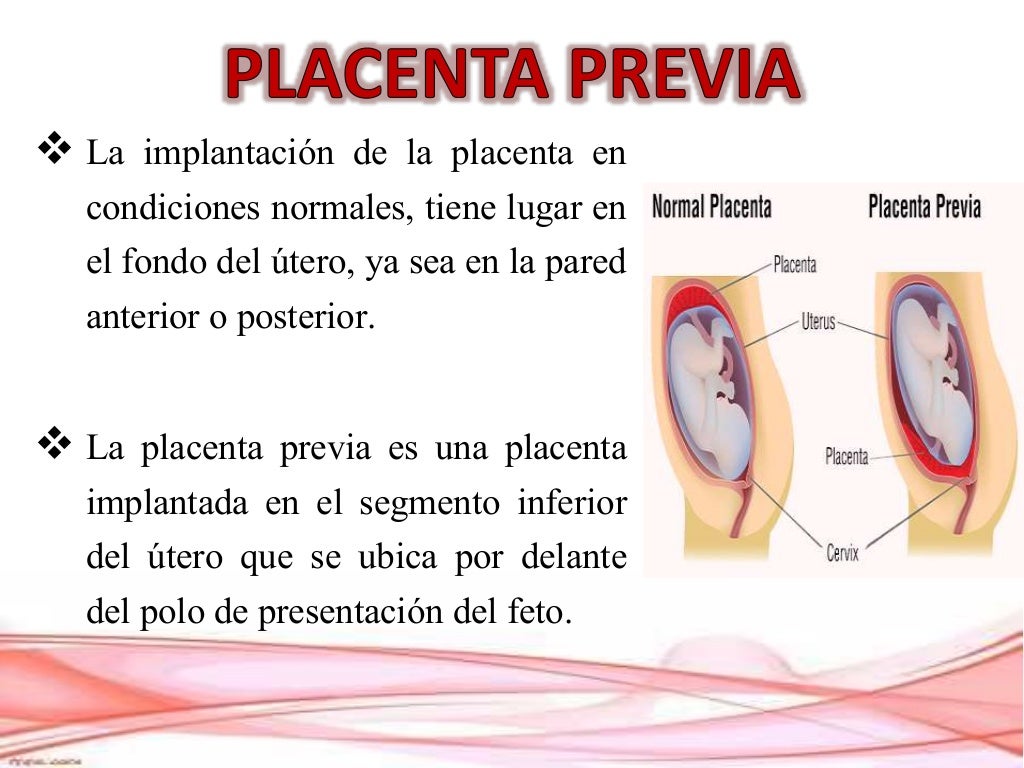 8th ed. Philadelphia, PA: Elsevier; 2021:chap 29.
8th ed. Philadelphia, PA: Elsevier; 2021:chap 29.
Resnik R. Intrauterine growth restriction. In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 47.
Last reviewed on: 12/2/2020
Reviewed by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Placental insufficiency - what is it and how to treat it
- Types and causes of placental insufficiency
- Diagnosis of placental insufficiency
- Treatment of placental insufficiency
Most women know that the placenta connects mother and baby during pregnancy and provides nutrients and oxygen to the baby.
Are there situations when the placenta ceases to perform its function correctly and fully? Is it possible to somehow prevent this?
What is the function of the placenta
So, the placenta is an important organ that is formed only during pregnancy.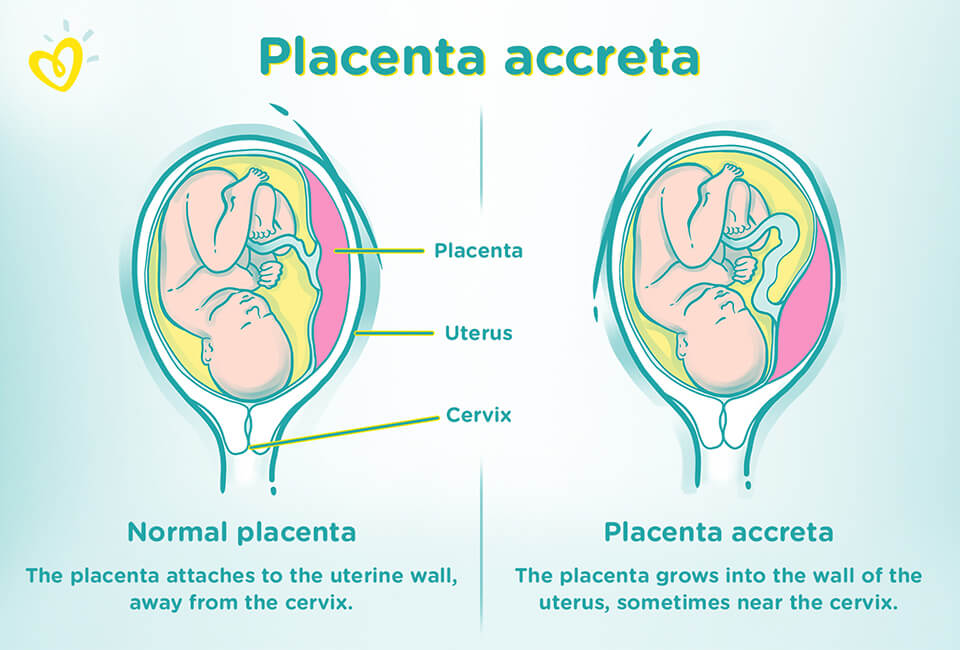 The placenta is formed from the chorion - the embryonic membranes of the fetus. At the very beginning of pregnancy, chorionic villi - outgrowths of the membrane - evenly cover the entire surface of the fetal egg, starting from the second month of pregnancy, on one side of the fetal egg, the villi begin to lengthen, increase in size and form the placenta.
The placenta is formed from the chorion - the embryonic membranes of the fetus. At the very beginning of pregnancy, chorionic villi - outgrowths of the membrane - evenly cover the entire surface of the fetal egg, starting from the second month of pregnancy, on one side of the fetal egg, the villi begin to lengthen, increase in size and form the placenta.
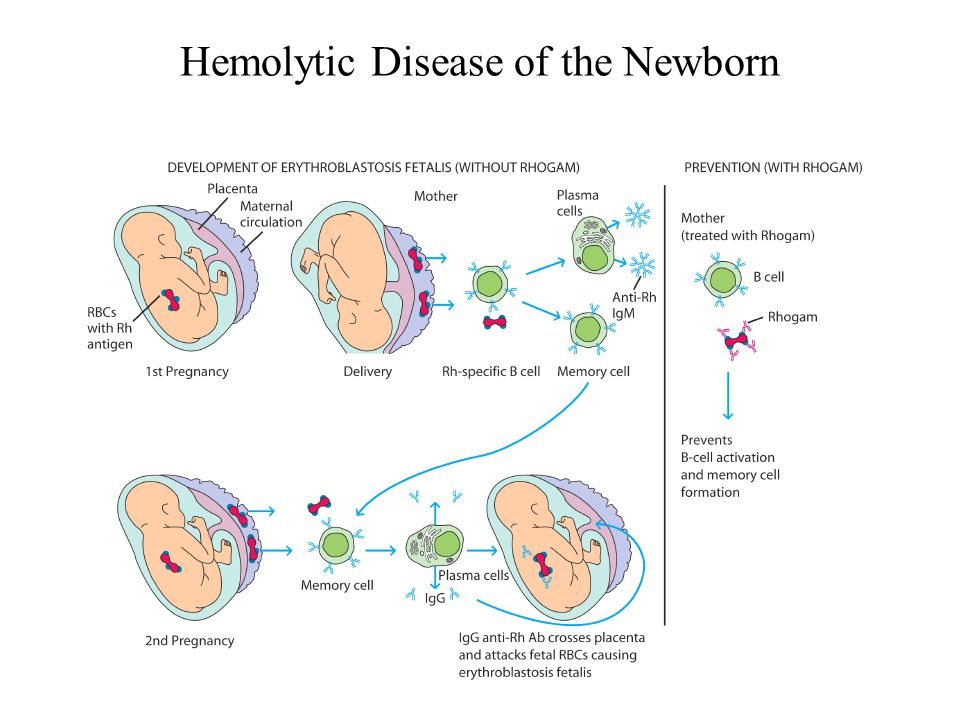
Inside the villi flows the blood of the baby, and outside they are bathed in the blood of the mother. Between the blood flow of mother and baby there is only one layer of cells, which plays the role of a barrier between the body of mother and child. Thanks to this membrane, the blood of the mother and fetus does not mix.
However, in recent years it has become known that fetal blood cells still penetrate the placental barrier into the mother's bloodstream, and thanks to this, it has become possible to conduct genetic analyzes and determine chromosomal abnormalities, Rh factor and fetal sex from the blood of a pregnant woman (non-invasive prenatal test) .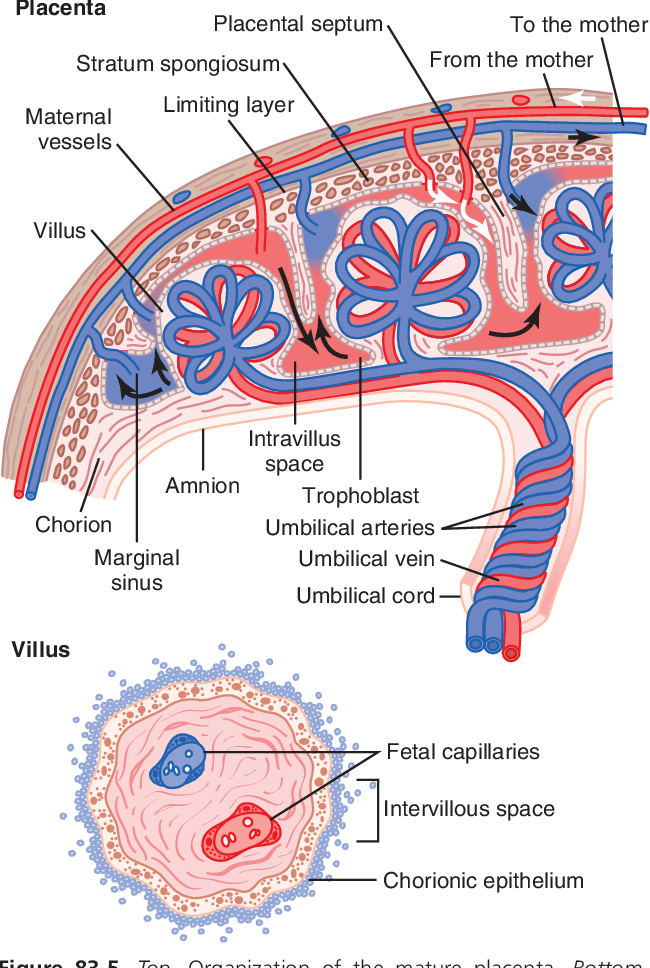
In the placenta, there is a constant exchange of substances between mother and child. Oxygen and nutrients are supplied from the mother's blood to the fetus, carbon dioxide and metabolic products from the fetus back to the mother, to be removed from the body.
The placental barrier performs an immunological function, as it allows some protective antibodies - blood cells that fight infectious agents, in addition, it is impervious to certain harmful substances, viruses and bacteria. Unfortunately, the placental barrier is easily overcome by drugs, alcohol, nicotine, components of many drugs and some viruses.
An important function of the placenta is the production of hormones and biologically active substances. First of all, these are hormones that are important for successful pregnancy, for example, chorionic gonadotropin, placental lactogen, estrogens, etc.
Unfortunately, things don't always go well. Due to a variety of reasons, deviations in the development and functioning of the placenta may occur at different stages of pregnancy.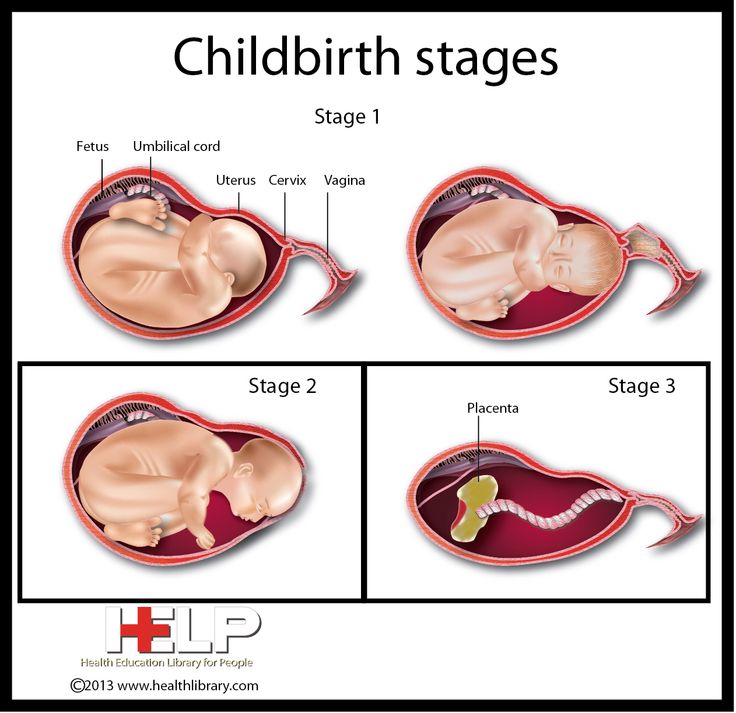 These changes never go unnoticed for mom and baby, and often have dire consequences.
These changes never go unnoticed for mom and baby, and often have dire consequences.
If the placenta ceases to perform its functions to the fullest, the so-called placental insufficiency develops. In fact, it consists in the deterioration of blood circulation in the mother-placenta-fetus system.
Types and causes of placental insufficiency
Doctors distinguish between acute and chronic placental insufficiency:
Acute placental insufficiency
This is a condition that requires urgent medical attention. It is characterized by a rapid deterioration in placental blood flow. Acute placental insufficiency occurs mainly as a result of placental abruption or the death of certain areas of placental tissue, for example, during the formation of blood clots in the vessels. Abdominal trauma, antiphospholipid syndrome can serve as the cause of detachment.
Phospholipids are complex fats that are part of the membranes of all body cells. In some cases, the body's immune system produces a large number of antibodies to some of its own phospholipids and proteins that bind these lipids.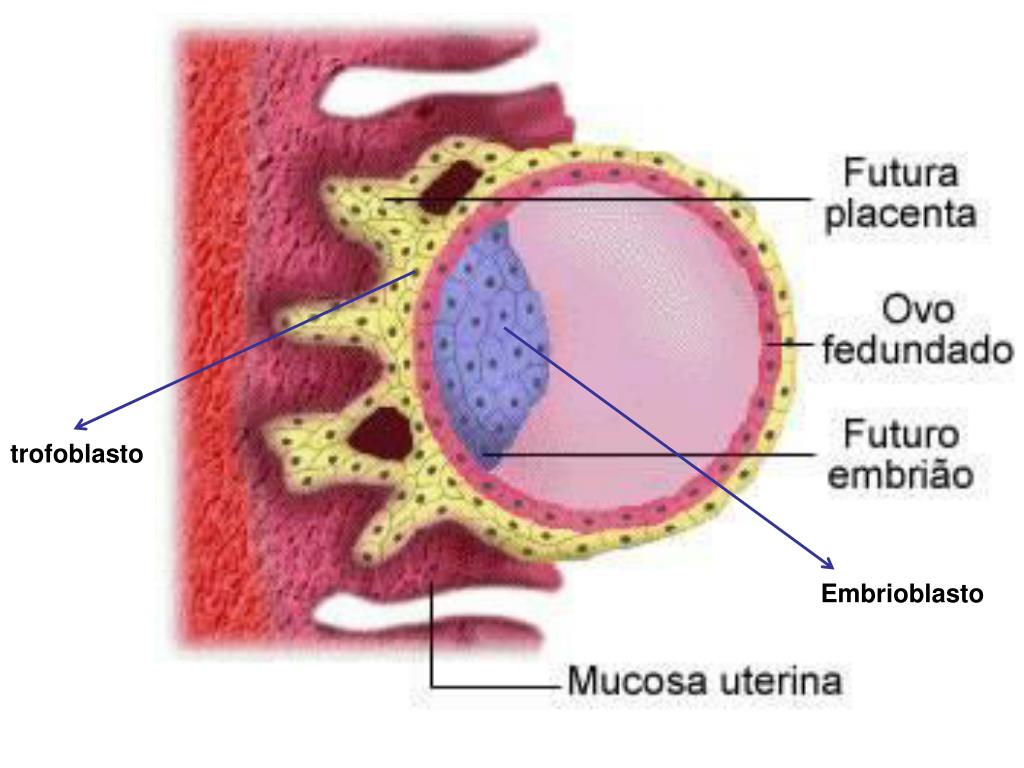 They are called antiphospholipid antibodies and, when interacting with the cells of the body, cause cell damage and activation of the blood coagulation system, which leads to thrombosis.
They are called antiphospholipid antibodies and, when interacting with the cells of the body, cause cell damage and activation of the blood coagulation system, which leads to thrombosis.
Antiphospholipid syndrome is the most common cause of thrombotic complications in pregnancy, including placental abruption and acute placental insufficiency.
A severe course of gestosis, a formidable complication of the second half of pregnancy, manifested by edema, increased pressure and the appearance of protein in the urine, can also cause placental abruption.
Acute placental insufficiency develops when more than 2/3 of the placental surface is detached.
In case of acute placental insufficiency, it is necessary to perform a caesarean section as soon as possible to save the life of the baby and mother.
Chronic placental insufficiency
Chronic placental insufficiency is much more common in pregnant women. In this case, there is a violation of the formation and maturation of the placenta, the uteroplacental and fetal-placental blood flow decreases, gas exchange and metabolism in the placenta are limited, and the synthesis of placental hormones decreases. All these changes determine the insufficient supply of oxygen and nutrients to the baby, cause a delay in the growth and development of the fetus.
All these changes determine the insufficient supply of oxygen and nutrients to the baby, cause a delay in the growth and development of the fetus.
The most common causes of placental insufficiency are previous abortions, especially surgical abortion during the first pregnancy, smoking, while the number and strength of cigarettes smoked do not matter, since tobacco smoke, not nicotine, has a negative effect on the formation of defective placental vessels.
The risk group for the development of placental insufficiency also includes women with chronic diseases such as arterial hypertension, iron deficiency anemia, pyelonephritis, diabetes, thyroid disease.
In recent years, there has been a significant increase in placental insufficiency caused by bacteria, viruses, fungi. The reason for this can be both an acute infection suffered by the expectant mother during pregnancy, and the activation of a chronic infectious process in the body of a pregnant woman.
Of no small importance in the formation of chronic placental insufficiency is the pathology of the uterus: endometriosis, malformations of the uterus (saddle-shaped, bicornuate).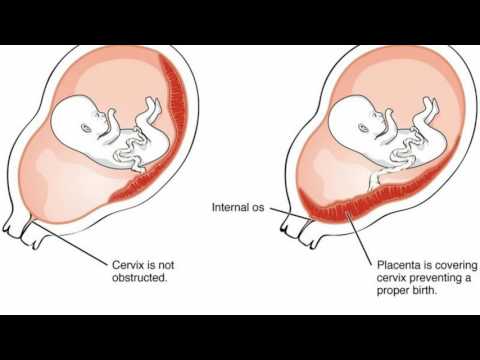 Doctors also consider uterine fibroids to be a risk factor. Of course, a number of drugs have an adverse effect on the formation of the placenta and the development of the fetus. Currently, a list of drugs that are not approved for use during pregnancy has been defined.
Doctors also consider uterine fibroids to be a risk factor. Of course, a number of drugs have an adverse effect on the formation of the placenta and the development of the fetus. Currently, a list of drugs that are not approved for use during pregnancy has been defined.
Also of great importance in the development of placental insufficiency is thrombophilia - an increased tendency of the body to form blood clots - blood clots in the vessels.
In some cases, placental insufficiency may be due to the presence of chromosomal abnormalities in the fetus, in particular in Down syndrome (the presence of an additional chromosome 21 in the fetus) or Edwards syndrome (an additional chromosome 18 in the fetus), placental dysfunction is diagnosed already in the early stages of pregnancy.
It should be noted that among the complications of pregnancy, most often leading to the development of chronic placental insufficiency, a significant factor is preeclampsia (or late preeclampsia) - a complication of the second half of pregnancy, manifested by edema, increased pressure and the appearance of protein in the urine.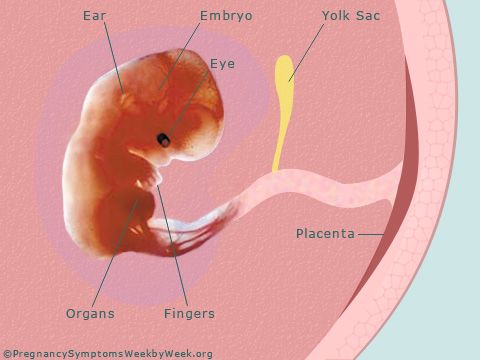
Regardless of the factors contributing to the development of placental insufficiency, it is based on circulatory disorders in the uterine-placental complex, leading to disruption of all functions of the placenta. Consequently, the symptoms of chronic placental insufficiency will be due to a lack of oxygen and nutrients to the fetus.
This is, first of all, intrauterine fetal growth retardation - a lag in the size of the fetus and a slowdown in its growth. Often there is a change in the motor activity of the fetus. At first there may be some increase in movements, and then a decrease. Violation of the protective function of the placenta leads to intrauterine infection of the fetus under the action of pathogenic (pathogenic) microorganisms penetrating the placenta. The fetus, the development of which occurs in conditions of placental insufficiency, is much more at risk of trauma during childbirth, they have a violation of adaptation to extrauterine life, increased morbidity in the first year of life.
According to the time of occurrence, doctors divide placental insufficiency into early and late.
Early (or primary) placental insufficiency
Develops before 16 weeks of gestation. It occurs already at the stage of placenta formation and is associated with diseases of a pregnant woman that are present before pregnancy, for example, with uterine pathology, chronic arterial hypertension, and endocrinological diseases. In this case, the formation of defective vessels in the placenta occurs.
Late (or secondary) placental insufficiency
Occurs after 16 weeks of pregnancy and is most often associated with diseases that have already occurred during pregnancy. Most often, these are iron deficiency anemia (that is, a decrease in the concentration of hemoglobin and iron in the blood), gestational diabetes mellitus (that is, a violation of the absorption of glucose by the body that occurred during pregnancy), past viral and bacterial infections.
It is important to subdivide placental insufficiency into compensated and decompensated forms.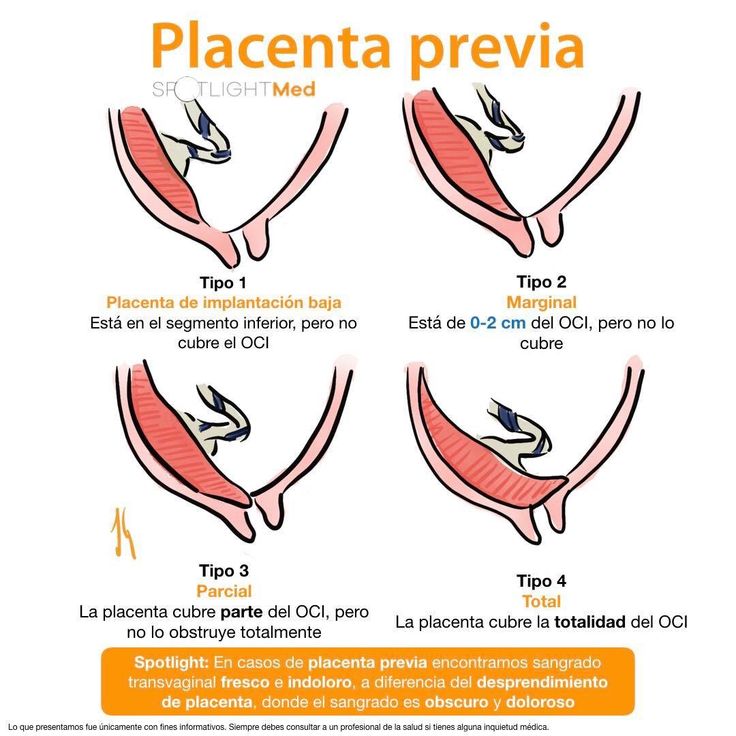
Compensated placental insufficiency
It develops, for example, with the threat of abortion and mild forms of late preeclampsia, if these complications are successfully amenable to medical correction.
Decompensated placental insufficiency
Causes the development of fetal growth retardation, chronic intrauterine hypoxia, up to fetal death.
Learn more about services:
- Ultrasound for pregnant women
- Ultrasound of the 1st trimester of pregnancy
- Ultrasound of vessels during pregnancy
- Consultation with a gynecologist
Diagnosis of placental insufficiency
It is almost impossible to treat an already developed placental insufficiency, so doctors actively seek to identify pregnant women who are at risk of developing placental dysfunction. If placental insufficiency is detected in the 3rd trimester of pregnancy, there is no effective treatment, unfortunately. Therefore, all methods of identifying in the early stages of pregnancy those women whose formation of the placenta has been disturbed are being very actively used.
Therefore, all methods of identifying in the early stages of pregnancy those women whose formation of the placenta has been disturbed are being very actively used.
First of all, when registering for pregnancy, the most significant risk factors are identified - smoking, abortions, aggravated heredity (low birth weight, tendency to thrombosis), the presence of chronic diseases of the heart, blood vessels, diabetes mellitus.
Preventive measures against the development of placental insufficiency are especially relevant and necessary until 16-17 weeks of pregnancy, when the formation of placental structures occurs.
Significant assistance in assessing the risk of developing placental insufficiency is provided by prenatal screening, which is carried out at 11-14 weeks of pregnancy. It is carried out to detect Down syndrome, Edwards syndrome and other chromosomal diseases in the fetus. Currently, the most relevant is to conduct a comprehensive early screening of a pregnant woman to predict the risk of developing placental insufficiency, preeclampsia and intrauterine growth retardation.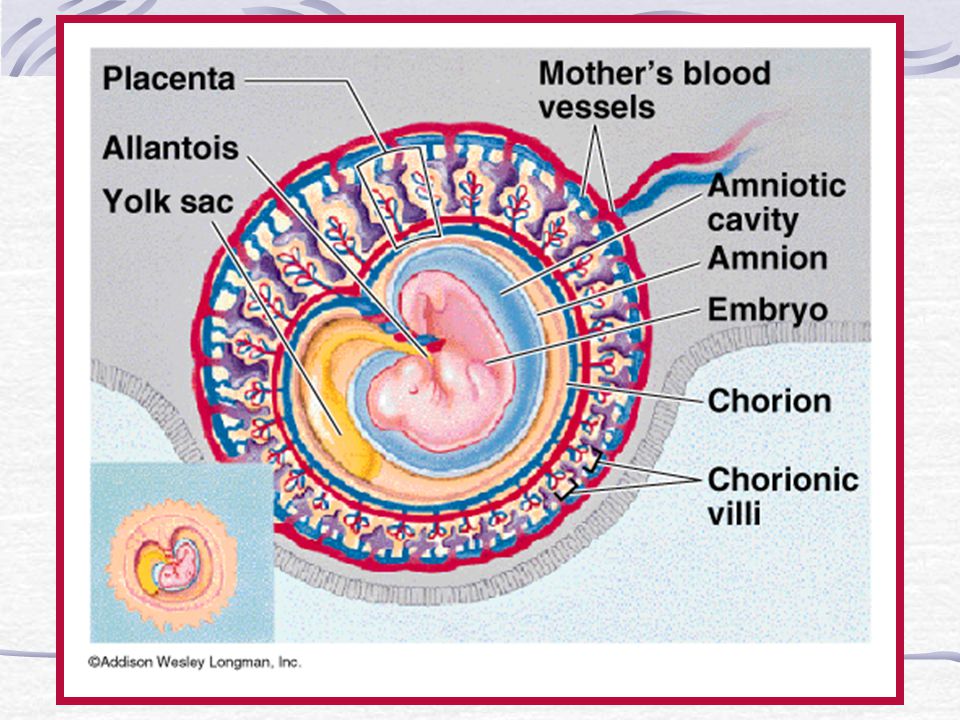 Since this type of diagnostics is one of the most modern and advanced, unfortunately, it is not yet included in the list of services provided in the antenatal clinic within the framework of compulsory medical insurance, but is available to everyone in prenatal diagnostic centers.
Since this type of diagnostics is one of the most modern and advanced, unfortunately, it is not yet included in the list of services provided in the antenatal clinic within the framework of compulsory medical insurance, but is available to everyone in prenatal diagnostic centers.
Determination of proteins produced by the placenta
First of all, the PAPP-A protein is determined, it is also a marker of chromosomal abnormalities of the fetus. A decrease in the concentration of PAPP-A in the blood at 11-14 weeks of gestation occurs in pregnant women who have a high risk of placental insufficiency and fetal growth retardation.
The second placental hormone that helps in assessing the risk of placental insufficiency is PIGF (placental growth factor). Its concentration in the blood decreases long before the first manifestations of placental insufficiency. Its definition is not as widely used as PAPP-A, but many laboratories have already included this protein in 1st trimester prenatal screening.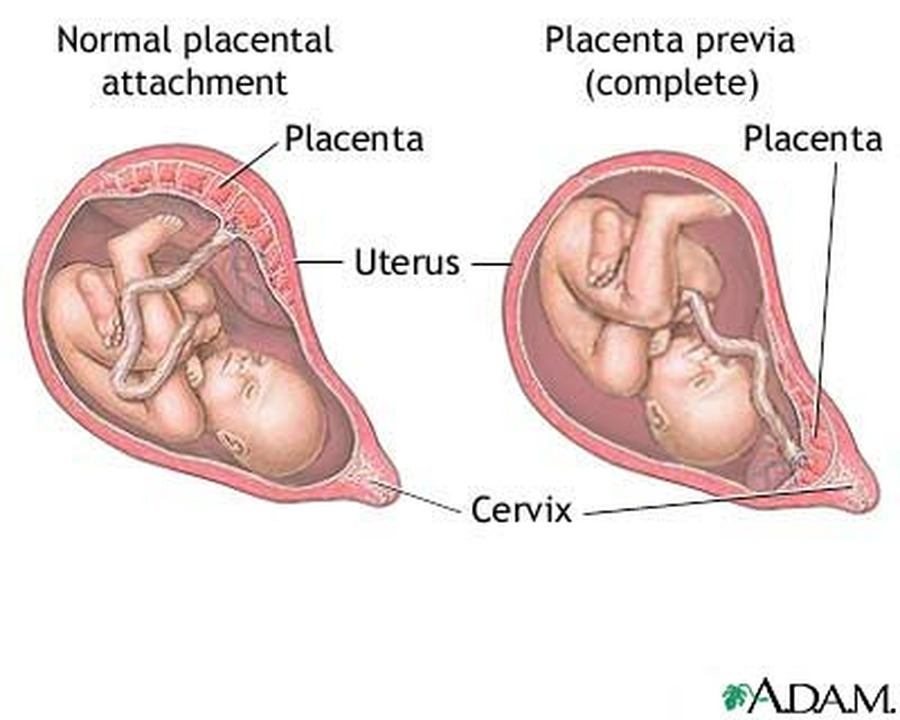 It is extremely important when screening the 1st trimester to measure blood flow in the vessels of the uterus. It has been unambiguously proven that the narrowing of the vessels of the uterus, determined during the study, indicates the inferiority of the formation of the placenta, which will worsen with increasing gestational age and lead to a decrease in the nutrition of the baby and the supply of oxygen, that is, to the development of placental insufficiency and fetal growth retardation. With normal sizes of uterine vessels at 11-14 weeks of gestation, the risk of severe placental insufficiency is negligible.
It is extremely important when screening the 1st trimester to measure blood flow in the vessels of the uterus. It has been unambiguously proven that the narrowing of the vessels of the uterus, determined during the study, indicates the inferiority of the formation of the placenta, which will worsen with increasing gestational age and lead to a decrease in the nutrition of the baby and the supply of oxygen, that is, to the development of placental insufficiency and fetal growth retardation. With normal sizes of uterine vessels at 11-14 weeks of gestation, the risk of severe placental insufficiency is negligible.
The next mandatory screening ultrasound is at 20-21 weeks of gestation. In this case, measurements of the fetus must be carried out in order to assess whether there is a lag in growth. After all, with oxygen starvation, the growth rate of the fetus slows down and its size begins to lag behind the norm for each period of pregnancy. In addition, the doctor must evaluate the condition and maturity of the placenta.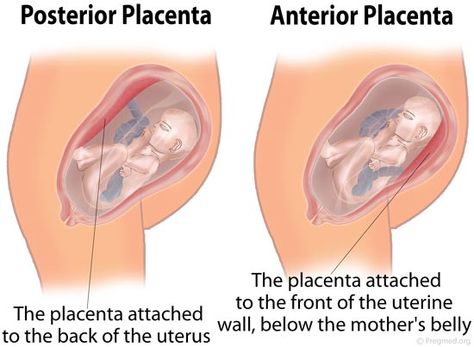 During ultrasound, dopplerometry of the uterine vessels is also performed to detect early changes that precede the clinical manifestations of placental insufficiency.
During ultrasound, dopplerometry of the uterine vessels is also performed to detect early changes that precede the clinical manifestations of placental insufficiency.
In patients belonging to the high-risk group, in addition to ultrasound and dopplerometry, daily monitoring of blood pressure fluctuations is also carried out, the amount of protein in the urine sample collected per day is determined, and the indicators of the blood coagulation system are evaluated.
The third ultrasound is performed for all expectant mothers at 30-34 weeks of pregnancy. The doctor measures the circumference of the head and abdomen of the crumbs, the length of the bones of his arms and legs, and calculates the estimated weight of the fetus. These measurements allow the doctor to make sure that the baby is developing normally. The structure of the placenta is also important, the presence of signs of aging in it, as a result of which it usually ceases to fully supply the baby with blood, which means that it ceases to have enough oxygen and nutrients and the development of the child is disturbed.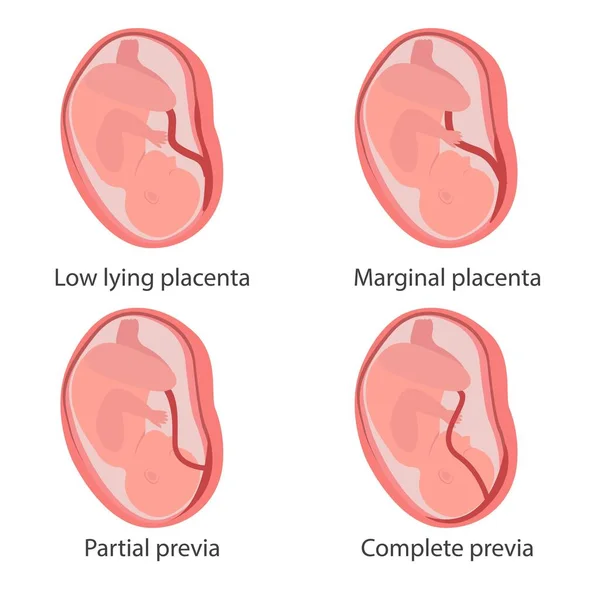 During ultrasound, the amount and type of amniotic fluid is assessed, which can also change with intrauterine fetal suffering.
During ultrasound, the amount and type of amniotic fluid is assessed, which can also change with intrauterine fetal suffering.
Doppler
Doppler of the placental and umbilical cord vessels (method of studying blood flow velocities in these vessels) also allows you to assess the well-being of the baby. The doctor examines the blood flow in the arteries of the uterus, umbilical cord, heart and brain of the child. This study allows you to determine whether the placenta is working well, whether there are signs of a lack of oxygen in the baby, or the development of preeclampsia in the mother. With a decrease in the speed of blood flow in any vessel, one can speak of fetal malnutrition of varying severity.
A well-timed examination makes it possible to identify the initial stages of blood supply deficiency. In such cases, treatment can prevent formidable complications, such as hypoxia and intrauterine growth retardation of the baby. Dopperometry is carried out at 20-21 weeks and at 30-32 weeks of pregnancy, if there are changes, control is carried out at least every two weeks.
Cardiotocography
This is an important method for assessing the condition of the fetus. CTG is performed at a gestational age of 33 weeks or more, since only at this stage of the intrauterine development of the baby is a complete regulation of the activity of the cardiovascular system of the fetus established by the centers of the spinal cord and brain. Recording of fetal heartbeats is carried out for 20-40 minutes, and if necessary, the study can be extended up to 1.5 hours.
The device registers and records the baby's heart rate. The obstetrician-gynecologist evaluates the heartbeat recording curve, episodes of slowing down and a sharp increase in the fetal heart rate, and based on these data, makes a conclusion about how comfortable the baby feels in the mother's stomach. For example, with a decrease in the concentration of oxygen in the blood of the fetus, its supply to the cells of the nervous system also decreases, which in turn affects the heart rate. In the normal course of pregnancy, CTG is performed after 33 weeks 1 time in 10-14 days, sometimes more often.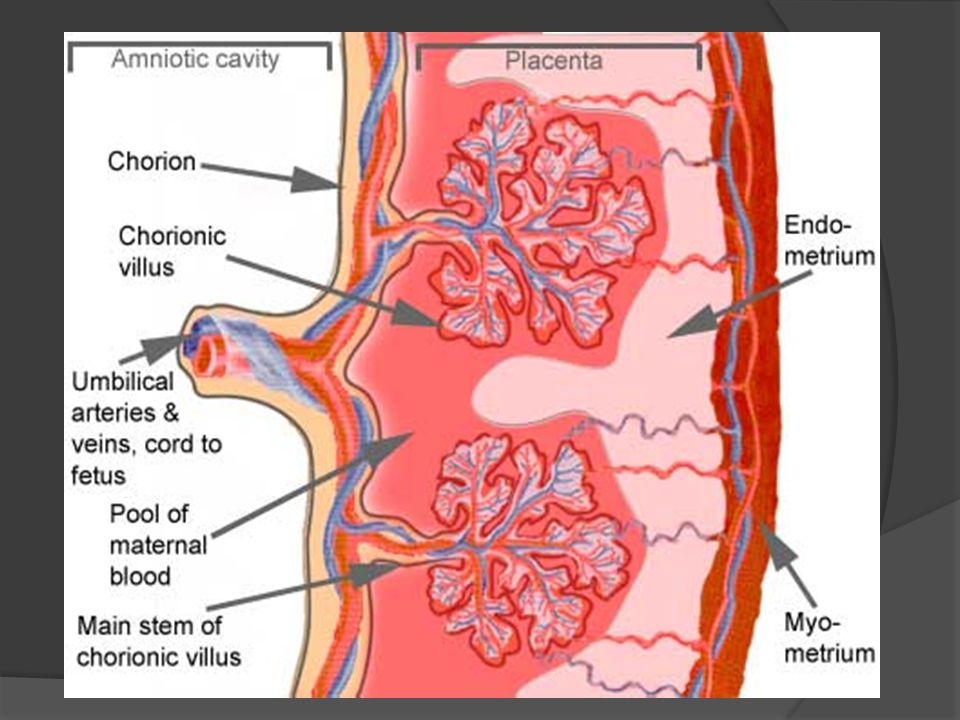 Some clinics currently offer the service of continuous CTG monitoring, which becomes relevant in the presence of signs of placental insufficiency. A pregnant woman is given a monitor that records changes in the baby's heart activity and these data are transmitted via the Internet to the attending physician.
Some clinics currently offer the service of continuous CTG monitoring, which becomes relevant in the presence of signs of placental insufficiency. A pregnant woman is given a monitor that records changes in the baby's heart activity and these data are transmitted via the Internet to the attending physician.
Treatment of placental insufficiency
There are currently no specific treatments for placental insufficiency because there are no drugs that selectively improve uteroplacental blood flow. That is why all measures to combat placental insufficiency are aimed at prevention. If the patient is at high risk for the development of placental insufficiency, from early pregnancy she is prescribed drugs whose effectiveness is well proven and which prevent the early development of severe placental dysfunction.
If during the additional methods of assessing the condition of the fetus, initial disturbances in the supply of oxygen to the baby are detected, drug treatment is carried out aimed at increasing the flow of blood and oxygen through the placenta and mandatory control examinations against the background of ongoing therapy.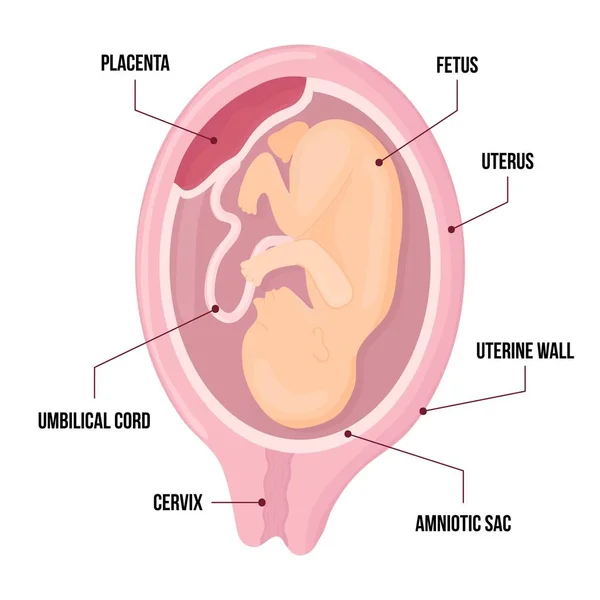 If the changes are serious and the baby experiences a pronounced deficiency of oxygen and nutrients, his condition suffers, then in such cases an emergency delivery is performed.
If the changes are serious and the baby experiences a pronounced deficiency of oxygen and nutrients, his condition suffers, then in such cases an emergency delivery is performed.
Pathogenesis and etiology in placental insufficiency: causes and diagnosis
Placental insufficiency is one of the main problems of obstetrics and neonatology. Placental dysfunction often leads to fetal hypoxia, delayed fetal development, and serious perinatal complications. In especially severe cases, pathology causes intrauterine death of the child. Obstetric tactics in case of placental insufficiency depends on the etiology, severity of the condition of the embryo and associated complications. Timely therapy helps to stop the progression of the pathology and keep the pregnancy until the due date.
What are the functions of the placenta?
The placenta is a temporary organ that is formed only during the period of gestation. The process of formation of the placenta is completed by the 16th week of pregnancy and from this period until the very birth, it is fully responsible for the metabolism between the mother and the embryo.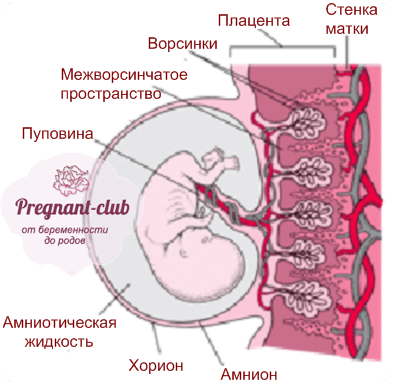
The health of the child directly depends on the normal functioning of the placenta. Thanks to the gas exchange function, oxygen enters the embryo through the blood vessels, and carbon dioxide is excreted in the opposite direction. The trophic function is responsible for the delivery of nutrients necessary for the development of the child, and the excretory function is responsible for the removal of the products of its metabolism.
The placenta also performs an immunological function: it protects the embryo from harmful substances and dangerous viruses, passing only maternal antibodies to it to suppress infections. An important role is also played by the hormonal function, due to which the synthesis of hormones necessary for the normal course of pregnancy and fetal development takes place.
If the blood supply to an organ deteriorates for some reason, placental insufficiency occurs. Due to impaired functionality, the placenta is no longer able to provide the necessary metabolism between mother and child, which leads to fetal hypoxia and intrauterine growth retardation.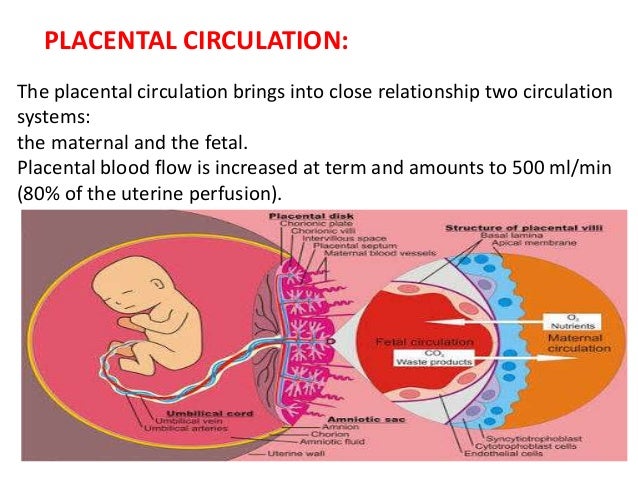
Diagnosis of FPI
The main danger of placental insufficiency is that it can be asymptomatic for a long time and it is possible to recognize the pathology only after the manifestation of complications, which are accompanied by intrauterine hypoxia. That is why it is important for a pregnant woman not to miss scheduled examinations and visits to an obstetrician-gynecologist. Modern diagnostic methods help to identify placental insufficiency in the early stages and establish the etiology of the disorder. This allows you to adjust obstetric tactics and stabilize pathological processes even before the appearance of serious complications.
Laboratory diagnostics
The method is based on a comprehensive study of the level of hormones in the patient's blood. Laboratory diagnostics is good because it allows you to detect placental insufficiency and determine its etiology even before the first clinical symptoms appear. This helps to develop the correct obstetric tactics and reduce the risk of perinatal complications.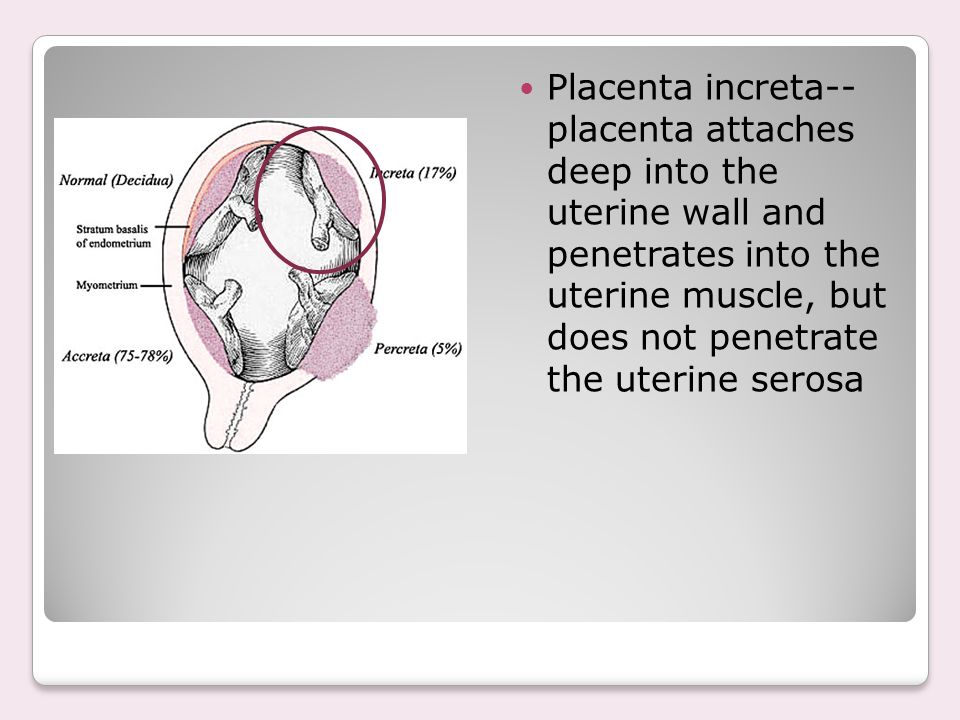
In the first trimester, pathology can be detected by analyzing hCG and progesterone. If their concentration is below normal, this indicates problems with the activity of the corpus luteum and indicates hormonal placental insufficiency. Another early sign of FPI is a violation of the synthesis of hormones of the fetoplacental complex, which play an important role in the intrauterine development of the fetus and affect the gestational process as a whole.
When performing hormonal and biochemical analyzes, it is important to consider that most of them have a wide range of possible fluctuations and low specificity. These factors reduce the reliability of the results obtained, causing problems with choosing the right obstetric tactics. Therefore, for accurate diagnosis and clarification of the etiology of disorders, it is better to use more informative methods of examination.
Ultrasound
Ultrasound is performed to determine the baby's fetometric parameters and then compare the results with standard values, which depend on the gestational age.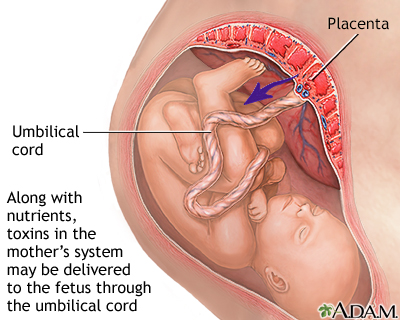 The specialist measures the distance between the temples of the embryo, the circumference of the head and chest, and the length of the thigh. If the obtained indicators do not meet the standards, this indicates an intrauterine growth retardation of the fetus, which requires special obstetric tactics. Depending on the etiology and severity of the deviation, there are three stages of the syndrome:
The specialist measures the distance between the temples of the embryo, the circumference of the head and chest, and the length of the thigh. If the obtained indicators do not meet the standards, this indicates an intrauterine growth retardation of the fetus, which requires special obstetric tactics. Depending on the etiology and severity of the deviation, there are three stages of the syndrome:
- I degree - the embryo lags behind in development by 2 weeks;
- II degree - 2-4 weeks behind;
- III degree - the delay is more than 4 weeks.
The doctor also performs a placenta to determine the thickness, maturity and location of the placenta. There are four degrees of organ maturity, each of which corresponds to a certain gestational age:
- 0 degree - the initial stage of maturation, in which the organ is fully functional and works without deviations. Observed at gestational age up to 30 weeks.
- Grade 1 - at this stage, slight echogenic inclusions appear in the tissues of the placenta, which is considered normal from 27 to 34 weeks of pregnancy.
- 2 degree - characterized by an increase in pathological inclusions in the structure of the placenta, which is acceptable in the period of 34-38 weeks and is dangerous if detected at an earlier gestational age.
- 3 degree - the placenta reaches its maximum maturity and its functions gradually fade away. Physiological aging of the organ occurs after 37 weeks of gestation.
Fetoplacental insufficiency is often indicated by the presence of calcifications and other pathological inclusions in placental tissues, which are signs of organ overmaturity. Regardless of the etiology, premature aging of the placenta poses a serious threat to the health of the embryo and requires the development of individual obstetric tactics. Due to the deterioration of its functions, the child does not receive the necessary nutrients and oxygen, which leads to hypoxia and intrauterine growth retardation.
Dopplerography
Dopplerography is the most informative and accurate method for diagnosing uteroplacental blood flow, which allows to detect FPI at the initial stage and establish the etiology of the disorder.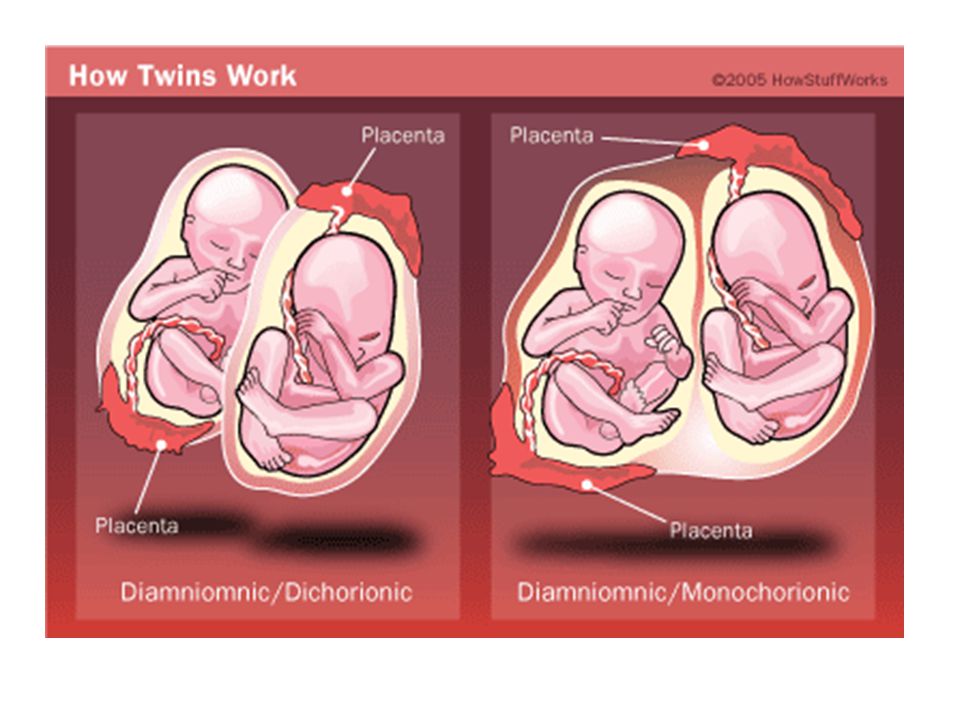 During the examination, the doctor analyzes the condition of large blood vessels: the umbilical and uterine arteries, as well as the middle cerebral artery of the embryo. Reduced blood flow in any of these vessels indicates dysfunction of the fetoplacental system, which leads to hypoxia and intrauterine growth retardation.
During the examination, the doctor analyzes the condition of large blood vessels: the umbilical and uterine arteries, as well as the middle cerebral artery of the embryo. Reduced blood flow in any of these vessels indicates dysfunction of the fetoplacental system, which leads to hypoxia and intrauterine growth retardation.
According to the severity and etiology, hemodynamic disorders are classified as follows:
- IA degree - a mild form of dysfunction that occurs due to a deterioration in blood flow only in the uterine arteries and does not pose a danger to the child. Occurs with extragenital pathologies or preeclampsia due to a persistent increase in blood pressure.
- IB degree - circulatory disturbance is observed only in the umbilical artery, in other large vessels the state of blood flow remains normal. This form of placental insufficiency is more common in early pregnancy, when the placenta is not yet fully formed.
- II degree - a more serious type of disorder, in which the state of the fetal-placental and utero-placental blood flow worsens.
 At this stage, deviations do not yet exceed critical values, however, they require careful medical supervision to track the dynamics of development and determine further obstetric tactics.
At this stage, deviations do not yet exceed critical values, however, they require careful medical supervision to track the dynamics of development and determine further obstetric tactics. - III degree - the most severe form of pathology, in which the blood flow in the umbilical artery deteriorates to critical levels. This condition indicates decompensated placental insufficiency and severe fetal hypoxia.
Cardiotocography
This test measures the heart rate and fetal movement. Cardiotocography is prescribed after the 32nd week of pregnancy, when the nervous system is responsible for the regulation of the cardiac activity of the embryo, due to which it is possible to analyze the functionality of several systems at once. Also during this period, the child stabilizes the cycle of activity and rest, in which he is active for an average of 50-60 minutes and is at rest for about 20-30 minutes. It is not recommended to do CTG at earlier dates due to the high probability of false results.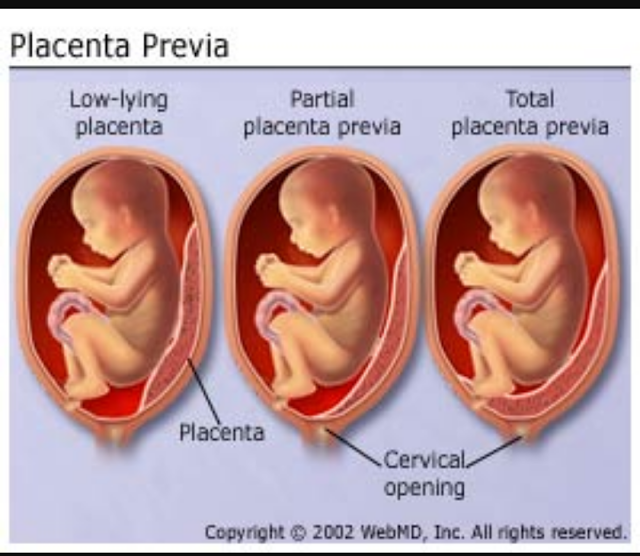
Cardiotocography takes into account the following parameters of the fetal heartbeat:
- basal rhythm and its variability;
- the presence of heart rate deviations from the average;
- periods of deceleration and acceleration;
- non-stress test scores.
Based on the data obtained, the doctor evaluates the child's condition and decides on further obstetric tactics.
Analysis of the biophysical profile of the fetus
If placental insufficiency and intrauterine hypoxia are suspected, special importance in obstetric tactics is given to the assessment of the biophysical profile of the fetus, which is formed according to the results of CTG and ultrasound diagnostics. The study takes into account 6 parameters:
- Respiratory movements of the embryo.
- Non-stress test results.
- Stage of placental maturity.
- Fetal muscle tone.
- Volume of amniotic fluid.
- Fetal motor activity.
Each of the indicators is estimated from 0 to 2 points, depending on the identified violations. The total result of 7 points and above indicates a satisfactory condition of the embryo and the absence of deviations in its development. With a lower assessment, obstetric tactics depend on the etiology of the disorder, the maturity of the fetus, and the readiness of the mother's body for preterm birth.
Etiology of placental insufficiency
Given the multifactorial etiology, there are three main groups of causes that lead to placental insufficiency and intrauterine growth retardation:
Maternal:
- genetic and constitutional characteristics of the mother;
- haematological and autoimmune disorders;
- socio-economic and age factor;
- chronic pulmonary, renal, endocrine or cardiovascular diseases;
- unbalanced diet;
- smoking, alcohol abuse and other bad habits;
- taking strong drugs.
Fruit:
- genetic and constitutional features of the fetus;
- intrauterine infections;
- chromosomal aneuploidy;
- pathologies of embryonic development (congenital defects of the heart muscle, absence of one of the umbilical arteries, etc.)
Uteroplacental:
- abnormal development of the uterus;
- necrosis of placental tissues due to poor blood supply;
- multiple pregnancy;
- placental mosaicism.
Risk factors
Considering the etiology of placental insufficiency, it is impossible not to mention the risk factors that increase the likelihood of pathology. Conventionally, they can be divided into the following categories:
Complications of pregnancy:
- anomalies in the location of the placenta;
- carrying two or more embryos;
- threatened miscarriage;
- urinary infections;
- post-pregnancy;
- preeclampsia.
Extragenital pathologies of the mother:
- endocrine - pathologies of the adrenal glands, diabetes mellitus, hypothyroidism, thyrotoxicosis;
- cardiovascular - arterial hypotension or hypertension, varicose veins, congenital heart defects;
- haematological - anemia, thrombophilia;
- renal - pyelonephritis, glomerulonephritis;
- autoimmune - scleroderma, systemic lupus erythematosus;
- infectious diseases in the acute or chronic stage.
Social factors:
- age under 17 or over 35;
- patient underweight;
- malnutrition;
- sleep disorder;
- frequent stress;
- bad ecology;
- harmful working conditions;
- heavy physical work;
- pathological addictions.
Gynecological disorders:
- endometriosis and other pathologies of the endometrium;
- history of pregnancy complications;
- uterine infantilism;
- primary infertility;
- benign/malignant tumors in the pelvic organs, etc.
Extragenital pathologies and complications that develop during pregnancy represent the greatest risk. It is these factors of etiology that most often cause placental insufficiency and intrauterine growth retardation of the child.
Pathogenesis of placental insufficiency
In the early stages of gestation, FPI often develops due to an enzymatic deficiency of the internal mucous membrane of the uterus, the tissues of which undergo significant changes during pregnancy under the influence of hormones. As a result of the violation, problems arise with the introduction of the trophoblast into the uterine endometrium. In most cases, the etiology of enzymatic deficiency is anomalies in the location and structure of the placenta or ovarian dysfunction.
Primary placental insufficiency can also be caused by malformations of the chorion or blood vessel defects. In the first trimester, pathology often leads to early intrauterine death of the embryo due to serious abnormalities in its development.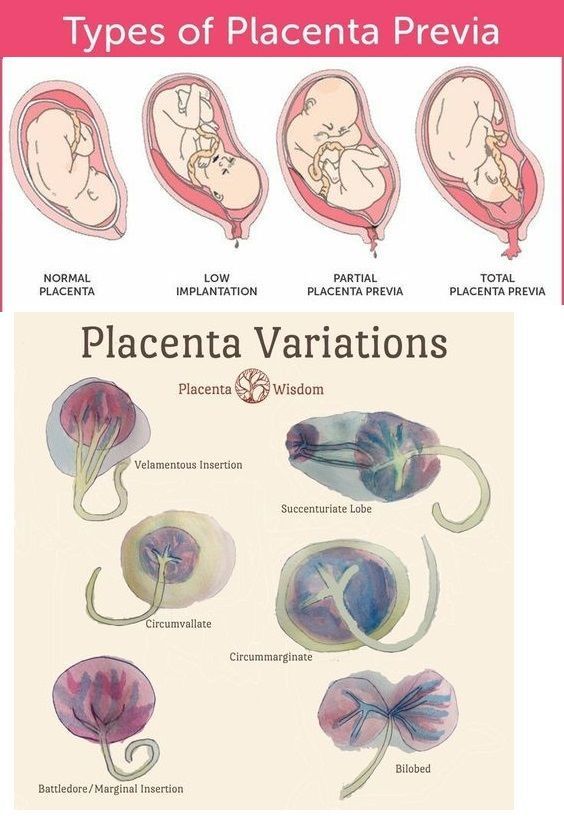
According to the clinical course, two stages of placental insufficiency are distinguished - acute and chronic. The acute form occurs with placental abruption or infarction and poses a serious threat to pregnancy due to the rapid development and increased risk of embryo death. The severity of the course of the chronic form of pathology depends on the etiology and compensatory capabilities of the maternal organism. If it cannot adapt to pathological changes, this leads to severe fetal hypoxia and serious perinatal complications.
The etiology of placental insufficiency can also be disorders of uteroplacental circulation and various microcirculatory disorders that develop with placental infarction, poor blood flow in the chorionic villi, problems with venous outflow, etc.
functions of the placenta, due to which the child experiences a lack of oxygen and lacks the nutrients necessary for growth. There is intrauterine hypoxia, which increases the risk of fetal growth retardation, and in especially severe cases leads to its intrauterine death.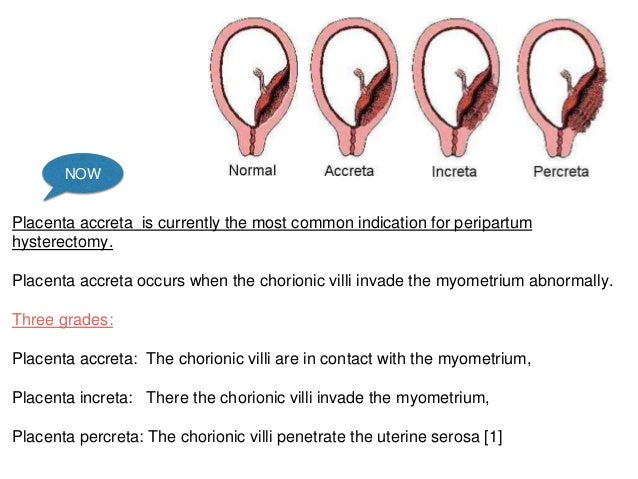
Obstetric tactics in placental insufficiency
Obstetric tactics in the detection of FPI is aimed at improving the condition of the fetus by normalizing the uteroplacental and fetal-placental circulation. The main goal of therapy is to eliminate the etiology of the disorder and maintain pregnancy until the due date.
Patients at high risk in early gestation should be treated prophylactically to prevent placental dysfunction. When a mild degree of intrauterine hypoxia is detected in the II and III trimester, obstetric tactics involves drug therapy, the effect of which improves fetal-placental blood flow.
Evaluate the effectiveness of obstetric tactics allow control examinations: CTG and Doppler. If therapy does not help and the child's condition worsens, the woman is hospitalized in a hospital for a comprehensive diagnosis, clarification of the etiology of disorders and a change in treatment tactics.
Indications for urgent hospitalization:
- decompensated form of FPI;
- subcompensated form of FPI;
- threatened preterm labor;
- development of placental insufficiency against the background of preeclampsia or exacerbation of extragenital diseases.

There is no single treatment regimen for placental insufficiency. Obstetric tactics depend on the etiology of disorders, the condition of the embryo and the severity of the pathology:
- IA degree - with a mild stage of FPI, a woman is recommended to walk more in the fresh air, eat well, take vitamins, and also establish sleep and wakefulness. For dynamic monitoring, CTG and dopplerometry procedures are prescribed. If the patient's condition has stabilized and the pregnancy proceeds without deterioration, early delivery is not required.
- IB degree - this stage of the pathology requires constant medical supervision, which is possible only during hospitalization. In order to monitor hemodynamic parameters and the general condition of the fetus, obstetric tactics include CTG and Doppler diagnostics every 2-3 days. To improve blood flow, a woman is prescribed drug therapy.
- II degree - dopplerometry and CTG are performed every 2 days. With a deterioration in blood flow, obstetric tactics provide for early delivery.
- III degree - the most severe form of pathology, in which prolongation of pregnancy does not make sense. In this case, obstetric tactics involves an emergency caesarean section to save the life of the child.
The effectiveness of therapy increases when a woman completes the first course before 26 weeks of gestation and repeats treatment in the third trimester. At a later date, correctly chosen obstetric tactics help the embryo adapt to conditions of oxygen starvation and thereby improve its condition.
Unfortunately, even after a full course of treatment, it is impossible to recover from fetoplacental insufficiency. Existing treatment regimens are aimed at stabilizing the already identified pathology and maintaining the compensatory capabilities of the maternal organism until the required delivery date.
That is why in obstetric tactics such an important role is given to preventive measures. Timely treatment of chronic diseases, maintaining a healthy lifestyle and following the recommendations of an obstetrician-gynecologist helps reduce the risk of placental insufficiency and increases the chances of enduring and giving birth to a healthy baby on time.