How to stop nipple vasospasms
Vasospasm and breastfeeding - symptoms, causes, management
beginning of content5-minute read
Listen
What is nipple vasospasm?
Vasospasm is what happens when the blood vessels supplying the nipple go into spasm and reduce the blood flow to the nipple. This affects the flow of milk from the nipple.
It is common to feel intense pain if this happens, particularly if the weather is cold. While any of the body's blood vessels can be affected by vasospasm, it can be a particularly painful condition for breastfeeding mothers.
Nipple vasospasm can occur:
- In response to nipple trauma if the baby is not well attached to the breast.
- It can also happen due to Raynaud’s phenomenon, more commonly called ‘Raynauds’ (see below). This is when vasospasm occurs randomly and is unrelated to breastfeeds.
Some women are more likely to have nipple vasospasm, particularly those who tend to have cold fingers and feet and who may already believe they have poor circulation. Sometimes women first experience nipple vasospasm during their pregnancy.
Women who are below average weight for their height are also at greater risk. Cigarette smoking can make vasospasm worse because nicotine constricts the blood vessels.
What does vasospasm with breastfeeding feel like?
Women with vasospasm commonly describe it as an intense, throbbing, burning type of pain in their nipples. When the blood vessels in the nipples are affected by vasospasm, pain can be felt before, during or after breastfeeds. The pain can last for a few seconds or longer. Some women experience vasospasm when they ‘let down’ or their milk ejection reflex has been activated.
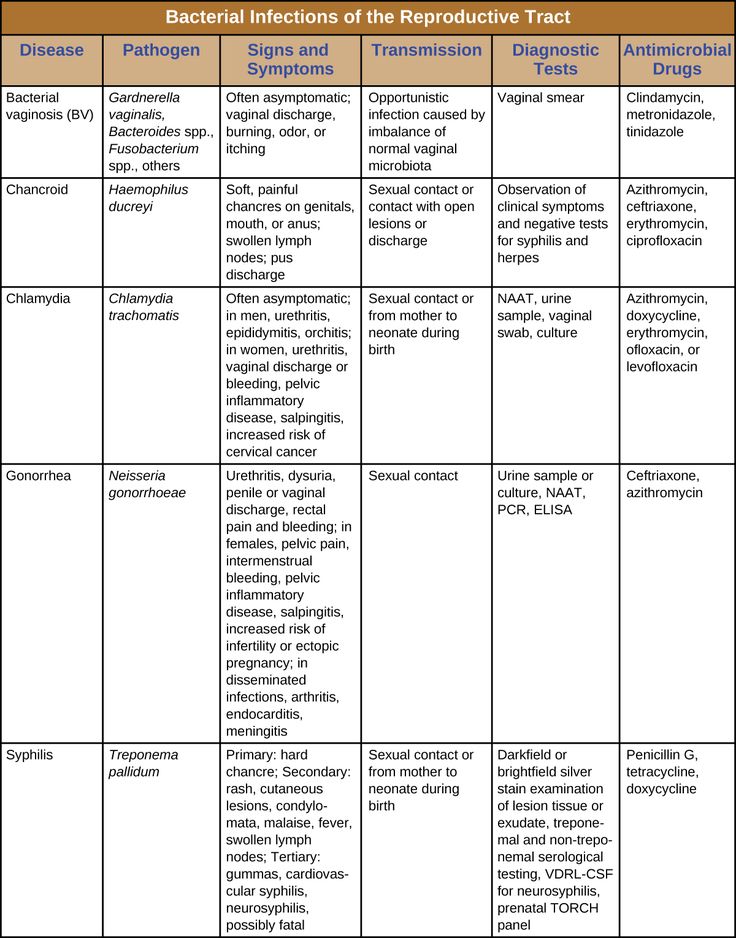
What does vasospasm look like?
The nipple or the tip of the nipple can appear white, or blanched during vasospasm. The colour of the nipple can also change as the blood returns to the vessels and tissues. This can mean there’s a change from white to purple, blue or red as the nipples return to their normal colour.
This can mean there’s a change from white to purple, blue or red as the nipples return to their normal colour.
What is Raynaud’s phenomenon?
Raynaud’s phenomenon, more commonly called ‘Raynauds’ occurs when vasospasm happens randomly and is unrelated to breastfeeds. Vasospasm symptoms can also occur in the fingers and toes in response to cold.
Raynauds is caused by a temporary interruption to normal blood flow in the small blood vessels in the extremities. This is why the fingers and toes, nose, lips and ears are often the most vulnerable body parts being affected.
If you have Raynauds when you are pregnant, you may also experience nipple vasospasm when you are breastfeeding.
How do I know if I have vasospasm?
Breastfeeding should not be painful or uncomfortable. It is common in the early days of breastfeeding for mothers to experience some nipple sensitivity as their body adjusts tp feeding. Women with nipple vasospasm may continue to experience pain when breastfeeding, even when their baby is attached properly and sucking well.
How can vasospasm be treated or managed?
You can manage the effects of nipple vasospasm by reducing your exposure to the air or cold. This will help your blood vessels to stay dilated and avoid becoming restricted. You can make your own decisions about comfort when deciding how many layers of clothing you need to wear. Ideally, you should use light layers which you can take off easily if you feel you’re overheating.
There are other strategies you can try too — for example:
- Apply warmth with a compress or heat pack straight after breastfeeding.
- Use breast warmers made from a reflective material since this can be soothing. Check with your pharmacist to see the options that are available.
- Try massaging olive oil onto your nipples after feeding but without exposing your breast to cold air.
- Try avoiding caffeine — some women report that avoiding this is helpful.
- Avoid exposing your nipples to cold air and wear more layers of clothing to avoid getting cold.
You should also check to make sure your baby is well attached when they are breastfeeding, and that you don’t have any nipple trauma or thrush.
Do supplements help for nipple vasospasm?
Some women find that taking supplements is very helpful in alleviating the symptoms of vasospasm. Before taking any medication or supplements, however, it’s important you speak with a healthcare professional or your pharmacist.
- Fish oil capsules or evening primrose oil (gamma linoleic) may help to improve blood vessel relaxation.
- Magnesium tablets can help to relax the blood vessels.
- Prescription medication may be beneficial — speak with your doctor for more information.
Where can I go for help and advice?
For more help with nipple vasospasm and breastfeeding, speak with:
- your midwife or child health nurse.
- a lactation consultant.
- Australian Breastfeeding Association — Helpline 1800 mum 2 mum, 1800 686 268.
- Pregnancy, Birth and Baby on 1800 882 436 to speak to a maternal child health nurse.
Sources:
ACT Health (Nipple Vasospasm), The Royal Women's Hospital Victoria (Herbal medicines & breastfeeding), The Royal Women's Hospital Victoria (Nipple vasospasm), Australian Breastfeeding Association (Vasospasm)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2021
Back To Top
Related pages
- Mixed feeding
- Breastfeeding your baby
- Diet and medication while breastfeeding
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari.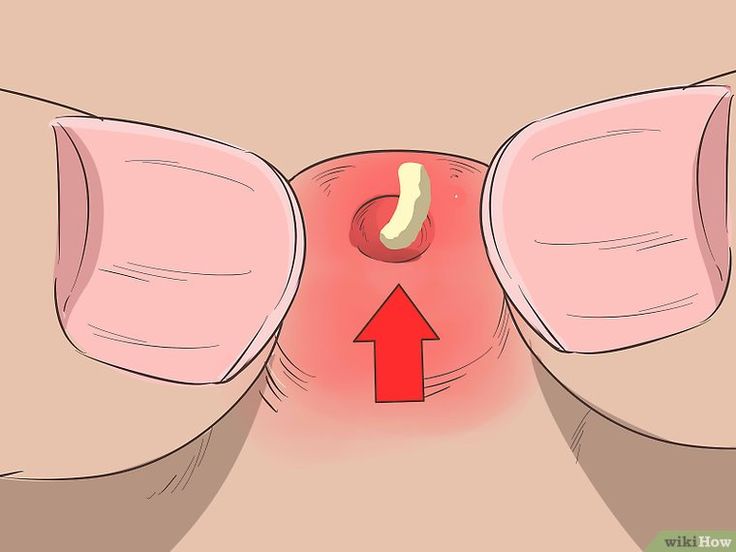 For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
The Ultimate Guide to Nipple Vasospasm
Nipple vasospasm is an oftentimes painful condition that can affect breastfeeding parents. Learn what exactly nipple vasospasm is, what causes it, and how to best treat it so you can find relief.
Share this content
Nipple vasospasm occurs when the blood vessels supplying the nipple contract. The narrowed vessels limit the supply of blood and oxygen while reducing the flow of milk. Breastfeeding mothers who experience nipple vasospasm often feel intense pain. Although some people are naturally predisposed to nipple vasospasm, environmental and behavioral factors can increase the risk. The good news is that it’s often possible to reduce or eliminate nipple vasospasm symptoms with gentle care and the right treatment.
The good news is that it’s often possible to reduce or eliminate nipple vasospasm symptoms with gentle care and the right treatment.
What are the Symptoms of Nipple Vasospasm?
It’s normal for blood vessels to expand and contract, but sometimes they contract too much and for too long. When this happens in the tissue surrounding the nipples, they don’t get enough blood. The nipple will often blanch, making it look paler than usual. When the blood returns, it can also look darker or redder than usual.
The nipple itself may feel sore, and some moms report a burning or stabbing sensation. Breastfeeding mothers can also experience pain deep in the breast tissue near their nipples. This pain can occur before, during, or after feeding. It can also happen between feeds if there are risk factors that increase the likelihood of vasospasm.
What Causes Nipple Vasospasm?
If you experience nipple vasospasm as a breastfeeding mother, it’s most likely because your baby is having latching difficulties during their nursing sessions. An ineffective latch can hurt your nipple and cause the blood vessels to constrict. Learning to latch, however, is common for newborns – and, though many moms will experience soreness or discomfort as a result, not all moms will experience nipple vasospasm. If you are prone to poor circulation (tip: do you frequently have cold hands or feet, even if the temperature is warmer?), this makes nipple vasospasm more likely.
Other factors that may make nipple vasospasm more likely include:
- Exposing your nipples to cold temperatures.
- Cracked nipples.
- Infections, including thrush.
Nipple Vasospasm and Reynaud's Syndrome
Raynaud’s Syndrome causes some parts of the body to be particularly prone to vasospasm. People with this condition experience numbness, cold, and sometimes pain in their hands, feet, ears, and other body parts when smaller arteries supplying blood to the skin narrow in response to cold or stress and cause decreased blood flow to these areas. Breastfeeding mothers with Reynaud’s Syndrome are significantly more likely to suffer from nipple vasospasm.
How to Treat Nipple Vasospasm
If your nipple vasospasm symptoms started when you began to breastfeed, it could be the result of nipple damage from improper latching. You may be able to reduce the pain associated with nipple vasospasm by ensuring your baby is properly latched to your breast while nursing. You can learn more about correctly latching your little one by working with a Lactation Consultant.
Other strategies that can be tried in tandem with working alongside a lactation specialist include:
- Avoiding cold environments when breastfeeding.
- Don’t expose your nipples to cold air – if you’re nursing your little one outside in cooler temperatures, make sure to keep yourself and your baby warm and cozy while they feed!
- Wear an extra layer of breastfeeding-friendly clothing to keep warm in or out of your home.
- Cover your chest as soon as your baby comes off the breast so you can maintain warmth.
- Use dry heat, such as a breast warmer or heat pack.
- Avoid caffeine, nicotine, and alcohol, all of which can also make vasospasm more likely.
Breastfeeding Vasospasm - Milk Fairies
Some breastfeeding moms experience nipple discomfort during and after feeding their baby. Discomfort and pain can occur for various reasons, and one of them is vasospasm .
Vasospasm of the nipples is often correlated with Raynaud's syndrome - a disease characterized by a disorder of arterial circulation mainly in the vessels of the extremities (feet and hands) under the influence of cold or emotional excitement.
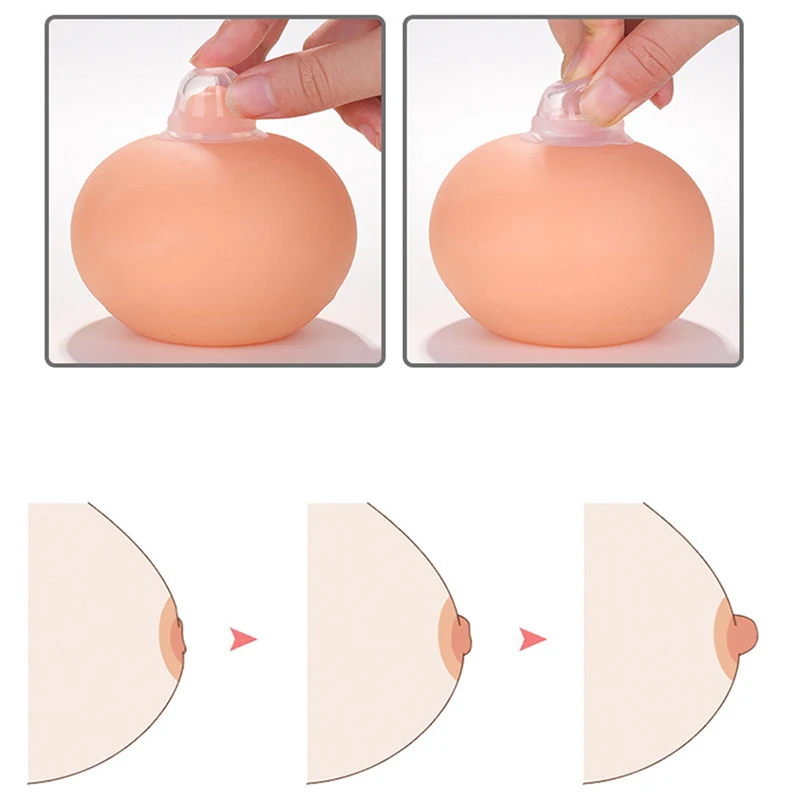
Vasospasm of the nipple occurs when the vessels in the upper part of the nipple spasm so much that all the blood drains from its tip, as a result of which the nipple turns white (as an option - successively turns white - blue - purple), and then, when the spasm passes , and the blood rushes back, turns pink again. Vasospasm can occur on one or both breasts at once and last from a few minutes to an hour or more. Soreness can be of a different nature.
Vasospasm can occur on one or both breasts at once and last from a few minutes to an hour or more. Soreness can be of a different nature.
The mother may feel burning, throbbing, stabbing or burning pain; moreover, pain and external manifestations of vasospasm can occur both immediately after feeding and between them [5]. Some moms feel Shooting pain that starts from the nipple and radiates deep into the chest, so vasospasm is often misdiagnosed as a yeast infection.
Vasospasm can occur on its own or as a result of infections or injuries to the nipple - this is how the nipple signals a problem. Often, a mother notices that it has become painful to feed, and after the feeding is completed, she finds that the nipple has become white. Usually injuries and damage to the nipples during lactation are associated with features breastfeeding the baby - in order to prevent or alleviate the symptoms of vasospasm, you must first make sure that the baby is properly attached to the breast and does not injure it when sucking.
In addition, vasospasm may occur in women who have had breast or nipple surgery in the past, possibly due to tissue and nerve damage. Also, some drugs (eg, fluconazole and oral contraceptives [3]) and some substances, including nicotine and caffeine, can contribute to vasospasm [9].].
How to help yourself during vasospasm?
During the vasospasm itself, to stop the pain, you can try to restore blood flow to the tip of the nipple by gently squeezing the nipple at its base. [8] Gentle massage with light squeezing movements (you can lubricate your fingers with cosmetic or vegetable oil) will help to quickly restore blood supply to the nipple and reduce pain until it disappears completely.
In the case of prolonged and severe pain, you can take (on consultation with your doctor!) an anesthetic that is compatible with breastfeeding, such as Ibuprofen or Paracetamol. [1
How to prevent vasospasm?
To avoid or reduce the intensity of vasospasms, in the first place - do not overcool ! [2] Put on a warm vest or carry your baby in your arms for a while after feeding.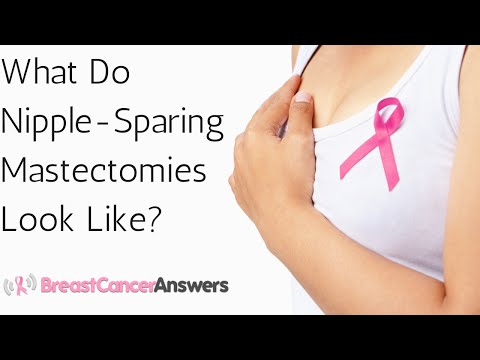 Some mothers find it helpful to put a warm diaper on the nipple as soon as the baby releases the breast. Some people use a hair dryer on warm air, blowing it on their breasts. Similarly, any warm dry and wet compresses help or even your own warm hand covering the nipple immediately after breastfeeding.
Some mothers find it helpful to put a warm diaper on the nipple as soon as the baby releases the breast. Some people use a hair dryer on warm air, blowing it on their breasts. Similarly, any warm dry and wet compresses help or even your own warm hand covering the nipple immediately after breastfeeding.
If painful vasospasm continues despite non-traumatic breastfeeding and heat application after feedings, then medication prevention and treatment of vasospasm (only prescribed by your physician!) may be an option. For example, you can ask the doctor to prescribe vitamin B6, calcium and magnesium as a preventive measure and relieve vasospasm .
Some doctors recommend applying a moderate amount of nitroglycerin ointment or 2% spray to the nipples after each feed for the first 24 hours and then whenever symptoms of vasospasm begin [6]. However, its use can cause a side effect in the form of headaches, and only about half of the patients confirm the effectiveness of such an ointment for vasospasm.
One tablet Nifedipine long-acting tablets per day for two weeks may also help. Nifedipine is a calcium channel blocker commonly used to treat hypertension and is not excreted in breast milk. [7] Nifedipine therapy has been shown to be effective in vasospasm and has no side effects in the baby [4]. 9
 & Pitman, T. The Ultimate Breastfeeding Book of Answers. Roseville, California: Prima 2000
& Pitman, T. The Ultimate Breastfeeding Book of Answers. Roseville, California: Prima 2000 Soreness of the nipples is a frequent companion of the formation of lactation in nursing mothers. Just managed to move away from the fights, as a new misfortune - "grabs" the nipples . Some women disappointedly say that they were not at all ready for such pain during feeding. “ It would be better if I gave birth again than to endure such a ,” they say.
Most often, these symptoms occur in the first week after childbirth, when the skin of the nipples gets used to the intensive sucking from the baby who is training to latch on. It is not always possible to insert the breast deeply or the baby lies in an uncomfortable position and literally hangs on the tip of the mother's nipple. As soon as the mother changes the position in which she feeds (the position from under the arm helps especially), the soreness gradually disappears.
As soon as the mother changes the position in which she feeds (the position from under the arm helps especially), the soreness gradually disappears.
spasm of the vessels of the nipple - the so-called Raynaud's syndrome , or vasospasm.
Until the end, the causes of this condition have not been clarified, but Dr. Jack Newman (his article below) suggested that pain in the nipples could be precisely because of this, and spasm of the vessels of the nipple occurs due to a sharp change in air temperature, when the baby releases the breast.
“These conditions [sore, white nipples] are caused by spasms in the blood vessels, blocking the flow of blood to certain parts of the body, usually the extremities, although not necessarily. They often occur due to a sharp drop in temperature. Most often, Raynaud's syndrome occurs in the fingers, for example, when a person steps out of a warm room into the street on a cold day. The fingers turn white, and due to poor blood flow to their tips, pain appears. Raynaud's syndrome is more common in women and often occurs in association with "autoimmune" diseases such as rheumatoid arthritis."
Raynaud's syndrome is more common in women and often occurs in association with "autoimmune" diseases such as rheumatoid arthritis."
i.e. when the baby releases the breast, the nipple turns white after a few seconds. In this case, a woman may experience acute burning pain, and then the nipple gradually acquires its previous color, and the pain becomes throbbing. As a rule, vasospasm occurs after the end of feeding, when the baby has already left the breast.
Treatment is to eliminate the root cause of pain - incorrect grip, thrush, etc.
What else can help relieve breast pain while breastfeeding?
- Do not leave the breast to dry after feeding, but immediately cover it with your arm or bra.
- Rub in olive oil immediately after feeding.
- Use warm compresses (except alcohol).
- Massage the chest (but not the chest) several times - massage the muscles between the collarbone and chest after feeding or when pain occurs.

If you suspect that you have vasospasm and cannot solve the problem even with the suggested measures, contact a lactation consultant or doctor.
============================================== ===============
Vasospasm and Raynaud's Syndrome
Dr. J. Newman
These conditions are caused by spasms in the blood vessels certain parts of the body, usually to limbs , although not necessarily. They often occur due to a sharp drop in temperature. Most often, Raynaud's syndrome occurs in the fingers, for example when a person leaves a warm room outside on a cold day. The fingers turn white, and due to poor blood flow to their tips, pain appears. More often, Raynaud's syndrome affects women, and it often occurs against the background of "autoimmune" diseases, such as rheumatoid arthritis.
Here we will refer to both of these conditions (vasospasm and Raynaud's syndrome - translator's note) by the word vasospasm. Vasospasm can also occur in the nipples. In fact, this is a much more common occurrence than is commonly believed. It may occur along with any other sore nipple problems and is often caused by nipple injuries, but sometimes it occurs on its own and is not associated with any other cause of nipple soreness.
Vasospasm can also occur in the nipples. In fact, this is a much more common occurrence than is commonly believed. It may occur along with any other sore nipple problems and is often caused by nipple injuries, but sometimes it occurs on its own and is not associated with any other cause of nipple soreness.
As a rule, vasospasm occurs after the end of feeding, when the baby has already left the breast. Most likely, the air outside is colder than in the child's mouth. When the baby releases the breast, the nipple looks normal, but soon, within minutes or even seconds, it begins to turn white. Perhaps the reason is that the nipple dries out very quickly. Usually mothers say that when the nipple turns white, they experience a burning pain. After some time, the nipple may return to its normal color (when the blood returns to the nipple), and then the mothers notice a throbbing pain. We offer you to watch our video, where the mother's nipple turns white, and then turns pink again. The color of the nipple (and the nature of the pain) can change from one side to the other within a few minutes or even an hour or two after feeding. Sometimes mothers note that the nipple does not turn white, but changes color from pink to red to purple and becomes pink again. We are not concerned about the change in color of the nipple, but the pain that accompanies this phenomenon. It is noteworthy that in some mothers, vasospasm is not accompanied by pain.
The color of the nipple (and the nature of the pain) can change from one side to the other within a few minutes or even an hour or two after feeding. Sometimes mothers note that the nipple does not turn white, but changes color from pink to red to purple and becomes pink again. We are not concerned about the change in color of the nipple, but the pain that accompanies this phenomenon. It is noteworthy that in some mothers, vasospasm is not accompanied by pain.
Treatment for vasospasm is to address the underlying cause of the pain (improper grip, thrush, etc.). See materials Breastfeeding , Candida Protocol and Painful Nipples, and our video clips. Almost always, as other causes of nipple soreness are eliminated, the pain caused by vasospasm will decrease, but more slowly. Addressing the root cause of pain (fixing a seizure, treating candidiasis) should be at the heart of treatment. In some mothers, as a result of pain during feeding, they stop, some of these pains did not exist initially. There are also mothers in whom vasospasm begins already during pregnancy. If the pain is not severe, it may not need treatment, it is only necessary to support and reassure the woman. But in some cases, it is worth prescribing treatment, especially if the pain bothers the mother and especially if it does not go away during feeding, as a significant decrease in the blood supply to the nipple can slow down the healing process.
There are also mothers in whom vasospasm begins already during pregnancy. If the pain is not severe, it may not need treatment, it is only necessary to support and reassure the woman. But in some cases, it is worth prescribing treatment, especially if the pain bothers the mother and especially if it does not go away during feeding, as a significant decrease in the blood supply to the nipple can slow down the healing process.
Treatment of Raynaud's syndrome (whitening of the nipples)
- Identify and treat the root cause of the pain : i.e. improper grip and/or thrush.
- Stop leaving breasts uncovered to dry. When the baby releases the breast, immediately cover the nipple with a warm hand while you put on the bra. After showering, do not leave the shower cabin until the chest is completely covered and warm, away from the cold air.
- Olive oil Warm the oil between your fingers and gently massage your nipples during the burning, this can greatly relieve the pain.
 We have heard from many mothers that such a massage immediately reduces the symptoms of vasospasm and, in general, vasospasm occurs less frequently during this procedure. It is very important to rub the oil into the nipples, and not just smear it.
We have heard from many mothers that such a massage immediately reduces the symptoms of vasospasm and, in general, vasospasm occurs less frequently during this procedure. It is very important to rub the oil into the nipples, and not just smear it. - Vitamin B6 Multicomplex . No studies have yet been done to prove that it works, however we have many anecdotal evidence that vitamin B6 helps, at least in some cases. He is completely harmless. It is best not to take vitamin B6 alone, but to take a vitamin B complex, which also includes niacin. It is necessary to take such a number of capsules that the dose of B6 is 100 mg 2 times a day, for several weeks. So, for example, if a vitamin B complex tablet contains 125 mg, but it only contains 50 mg of vitamin B6, then mom should take 2 capsules at a time, twice a day. It should be taken until several weeks pass without pain. The course can be repeated if necessary. If the pain hasn't returned within a week or two, try stopping vitamin B6.
 If vitamin B6 has not worked in a week, it may not help.
If vitamin B6 has not worked in a week, it may not help. - Warm dry compresses can be very effective in treating vasospasm when it occurs and in relieving pain. If the mother lies down after feeding and puts warm heating pads on her nipples for a few minutes, this can help a lot. At the same time, she will rest and, perhaps, this will also help to cope with the pain.
- Magnesium with calcium as follows: 300 mg magnesium/200 mg calcium (gluconate) twice daily. Or take separately 2 times a day 300 mg of magnesium and 2 times a day 200 mg of calcium daily.
- After correcting the grip, a method perhaps as effective as all of the above is to massage the chest muscles between the collarbone and chest after feeding, or if there is pain in the nipples or breasts. Massage should be intense and strong, it should be done in the chest area, it is not necessary to massage the chest itself. Mom can also massage herself under the pectoral muscles, in the armpit, but such a massage should be done gently.