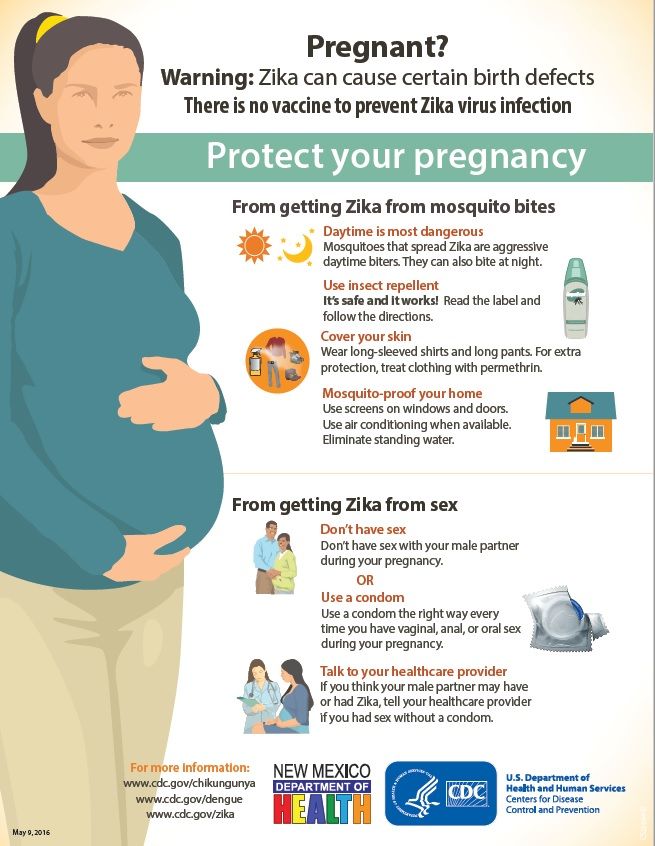
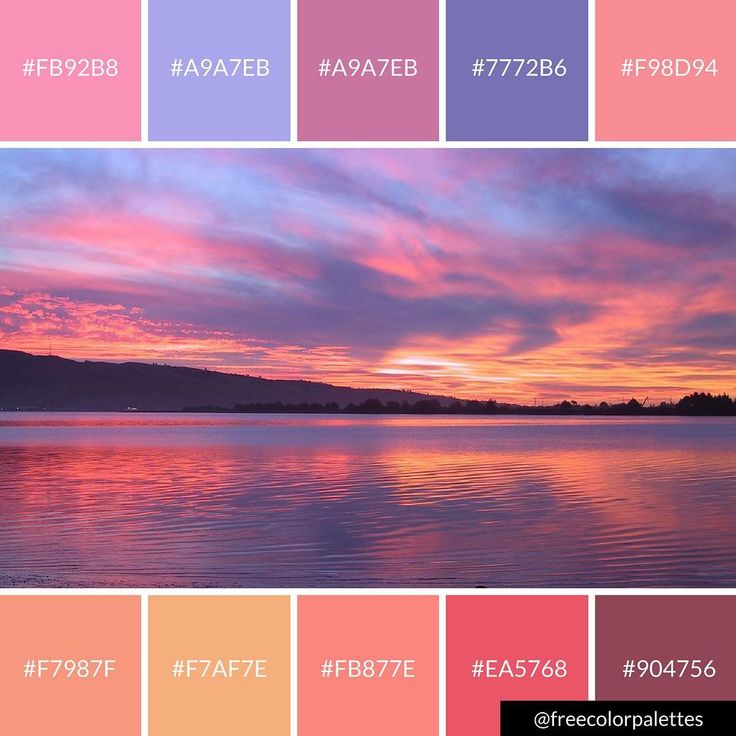
Waters breaking pink colour
When your waters break - BabyCentre UK
In this article
- What causes my waters to break?
- When will my waters break?
- What will it feel like when my waters break?
- How can I tell if my waters have broken or I’ve peed?
- Is it my waters breaking or is it discharge?
- What should I do when my waters break?
- My waters have broken and I’m having contractions. What will happen?
- What happens if my waters break before I go into labour?
- Why would my midwife break my waters?
Your waters breaking is usually a sign that labour is on the way or you’re in early labour (Scorza 2018, Lowth 2017). During pregnancy, your growing baby is cushioned inside a fluid-filled bag (amniotic sac) in your womb (uterus). When your baby is ready to be born, the sac breaks and the fluid comes out through your vagina (NHS 2018a). This is your waters breaking. You may feel a slight trickle or a sudden gush of water (NHS 2018a) and it can be hard to tell if your waters have broken or if you’ve peed. Get the lowdown on what happens when your waters break and how to tell when it's happened.
What causes my waters to break?
We don't know exactly what the trigger is, but your waters breaking is usually a sign that you are ready to go into labour, or are in early labour (Scorza 2018, Lowth 2017).
When your waters break, the fluid-filled amniotic sac, which protects and cushions your baby in your womb (uterus), tears. The amniotic fluid then leaks out via your cervix and vagina (NHS 2018a).
The bag of waters is made up of two layers of membranes, which explains why midwives and doctors often describe waters breaking as "ruptured membranes" (NHS 2018a).
When will my waters break?
It's most likely they'll break once you've started having contractions (Scorza 2018, Simkin and Ancheta 2011).
Bear in mind that your waters breaking isn't necessarily a clear staging post in labour. It can happen at any point over quite a long time span, either before labour starts in earnest, or, more often, as you progress through the first or second stages of labour.
It can happen at any point over quite a long time span, either before labour starts in earnest, or, more often, as you progress through the first or second stages of labour.
You can't control when your waters break, but it's probably helpful if they go towards the end of the first stage of labour (Jackson et al 2014, Simkin and Ancheta 2011) because:
- It can protect you and your baby from infection (Simkin and Ancheta 2011).
- It may take the edge off your contractions (Jackson et al 2014, Simkin and Ancheta 2011) by spreading the pressure through your womb.
- It may help your baby to move her head more easily into a good position for birth (Simkin and Ancheta 2011).
Sometimes, waters break before any other signs of labour, including contractions. This happens for about one woman in 10 at term (NCCWCH 2008, NHS Digital 2018).
For about two in 100 women, their waters break earlier than this, before they are 37 weeks pregnant (NHS Digital 2018, Tommy's 2016). (If this happens to you, call your maternity unit straight away. See our section below What should I do when my waters break? for more information.)
(If this happens to you, call your maternity unit straight away. See our section below What should I do when my waters break? for more information.)
If you’re concerned about your waters breaking when you’re out, keep a couple of maternity pads in your bag from around 37 weeks of pregnancy. At night, pop a waterproof cover, or even a cheap shower curtain, under your sheet. You may also find it comes in handy after the birth, if your breasts leak milk while you sleep.
What will it feel like when my waters break?
Every woman is different, so it’s hard to say. It won't hurt (Tommy's 2017). You may feel a slight trickle or a large gush, depending on where the bag of waters has torn and whether your baby's head is engaged (NHS 2018a).
By the end of pregnancy, there can be about 600ml (1.1 pints) of fluid (Bailey 2014, Vorvick 2016). Your body continues to make more throughout labour, so you may be surprised to find that you continue to lose fluid, even after your waters have broken (Bailey 2014, Tommy's 2016).
You may feel your waters breaking with a pop or you may only realise that your waters have gone when you feel fluid coming out of your vagina or dampness in your underwear (Tommy's 2017).
If you’re having contractions, you may notice that they start to feel more intense once your waters have broken (Jackson et al 2014, Simkin and Ancheta 2011).
How can I tell if my waters have broken or I’ve peed?
Unlike pee, amniotic fluid shouldn't have a strong smell and you won't be able to control its flow (NHS 2017, Tommy's 2017). It's 99 per cent water, so it's normally clear with a yellow tinge (Bailey 2014) or sometimes a pink tinge, if there are traces of blood (NHS 2017, Tommy's 2016).
Is it my waters breaking or is it discharge?
Amniotic fluid is different from vaginal discharge, which can get quite heavy as you approach labour, and is milky and musky-smelling (NHS 2018b).
If you’re close to or past your due date, your waters may contain some of your baby's first poo (meconium) (Newson 2015). This may give the waters a green tinge, or you may be able to see green or brown meconium (Newson 2015, NCCWCH 2014).
Always phone your maternity unit for advice after your waters have broken, and phone immediately if you are worried about the colour of your waters.
How to stay calm during labour
Worried about feeling stressed when in labour? Learn how these mums managed to keep calm. More labour and birth videos
What should I do when my waters break?
Call your maternity unit (NHS 2017, 2018a). What happens next depends how far along you are when your waters break, and whether you're already in labour.
If your waters break before 37 weeks
Call the unit without delay, as you may need swift treatment to protect your baby (Thomson, RCOG 2019). The number for the unit should be in your maternity notes.
The number for the unit should be in your maternity notes.
You'll need extra support and care from the hospital team. Your doctor or midwife will recommend that you:
- Have a course of antibiotics for 10 days or until you're in active labour, whichever is sooner. This is to protect you and your baby from infection.
- Have a course of steroids if you're between 24 weeks and 34 weeks pregnant, and possibly up to 36 weeks pregnant. This is to protect your baby's lungs, if he's born early.
- Have blood tests and extra monitoring of your baby, to check for infection.
- Meet a neonatologist and have a look around the neonatal care unit in case your baby arrives early and needs extra care.
- Wait to see if labour starts on its own. You may be able to go home, if all's well after a period of monitoring in hospital. You need to contact your doctor or midwife if you have symptoms of an infection, such as high temperature, tummy pain or your baby moving less than usual.
- Plan a hospital birth at 37 weeks, unless there are complications that mean that it's safer for your baby to be born sooner.
- Have magnesium sulfate fed through a fine tube (drip) into your vein if you're between 24 weeks and 30 weeks pregnant and are in active labour, or are having a planned preterm birth within the next day. Having magnesium sulphate can help to reduce the risk of cerebral palsy, which may affect some babies who are born too soon.
(Thomson, RCOG 2019)
If you tested positive for group B streptococcus (GBS) during pregnancy, your doctor or midwife will offer you an induction as soon as possible, along with antibiotics via drip (RCOG 2017, Scorza 2018). This will help to protect your baby from contracting a GBS infection. Infection of newborns by GBS is unusual, but can be harmful if it happens (RCOG 2017).
If your waters break at full term
Call your maternity unit for advice on what to do. You midwife may ask for the following information:
You midwife may ask for the following information:
- How many weeks pregnant you are.
- If this is your first baby.
- If your pregnancy has been straightforward.
- If your waters broke with a gush or a trickle.
- What time your waters broke.
- What colour the fluid was.
- If you have signs of contractions starting, such as cramps.
- Whether your baby’s movements have changed since your waters broke.
Your midwife will advise you to wear a maternity pad, rather than a sanitary towel, in case the fluid needs to be checked. Sanitary towels tend to lock fluid away, which makes it harder to check the colour of the fluid. Don't use a tampon either, as this can increase the risk of infection (Tommy's 2017).
After assessing you over the phone, your midwife should have a good picture of what needs to happen next. If your contractions haven't started, but you're healthy and doing well, she may reassure you that you can stay at home for another 12 hours to 24 hours to see what happens. At least 60 per cent of women go into labour within 24 hours of their waters breaking (NCCWCH 2014, Pintucci et al 2014) and most of the rest go into labour within 48 hours (Pintucci et al 2014).
At least 60 per cent of women go into labour within 24 hours of their waters breaking (NCCWCH 2014, Pintucci et al 2014) and most of the rest go into labour within 48 hours (Pintucci et al 2014).
My waters have broken and I’m having contractions. What will happen?
If you're having contractions, or there's doubt over whether your waters really have broken, you midwife will probably ask you to come to the hospital or birth centre. If you're coming in by car, you or your birth partner could pop a bin liner and clean towel on the seat to protect it, just in case.
Once you arrive at the unit, your midwife will listen to your baby's heartbeat to make sure your baby is well (NCCWCH 2014). She may ask to swab your vagina to check for amniotic fluid, or give you a special pad that can detect the fluid (NCCWCH 2014).
Your midwife may also ask to carry out a vaginal examination to see if your cervix has started to change. She may need to use a speculum, which opens your vagina wider, so she can see your cervix more clearly (NCCWCH 2014, Tommy's 2017). If it's hard for her to tell if there's a tear in the amniotic sac, she may ask you to cough. This can help the waters pass through your cervix (NCCWCH 2014, Tommy's 2017).
She may need to use a speculum, which opens your vagina wider, so she can see your cervix more clearly (NCCWCH 2014, Tommy's 2017). If it's hard for her to tell if there's a tear in the amniotic sac, she may ask you to cough. This can help the waters pass through your cervix (NCCWCH 2014, Tommy's 2017).
What happens if my waters break before I go into labour?
The chance of you, or your baby, developing an infection does increase if your waters have broken and there's a delay to labour starting. But you're both likely to remain well while waiting a day for contractions to get under way (NCCWCH 2014, Pintucci et al 2014, Scorza et al 2018).
If your labour hasn't started after 24 hours, your midwife or doctor will recommend that you have your labour induced with an artificial hormone called Syntocinon (NCCWCH 2014). Hospitals recommend a cut-off of about 24 hours because waiting for longer raises the risk of infection further (NCCWCH 2014, NICE 2016).
If you're worried about waiting even for 24 hours, or are just keen to get labour going, talk to your midwife or doctor about having an induction sooner.
On the other hand, if you'd prefer not to have an induction after waiting for 24 hours, you'll need to:
- Have your baby's heart rate and movements checked by a midwife or doctor every 24 hours.
- Check your temperature every four hours.
- Check for changes in the colour and smell of your waters, as you’re likely to continue to lose fluid.
- Stay focused on your baby's movements to be sure he's moving around as usual.
(NCCWCH 2014)
You may need to change your plans if you had been hoping to have your baby in a birth centre or at home. Even if you're both well, your midwife or doctor will advise you to have your baby in hospital if it's more than 24 hours from when your waters break to the start of your labour.
If you’re waiting at home, call the hospital immediately if you:
- Have signs of infection, such as raised temperature, shivering and skin flushing.
- Notice a decrease in your baby's movements.
(NCCWCH 2014)
If your midwife or doctor finds an infection, you'll need to have antibiotics via a drip (NCCWCH 2014). You may also need to have your labour induced straight away, depending on your circumstances (NCCWCH 2008, RCOG 2017). Although this may sound alarming, these measures will help to protect your baby.
Your baby may also be vulnerable to infection after he has been born, so you'll need to stay in hospital for at least 12 hours after the birth (NCCWCH 2014). If you have any concerns about your baby's health in the first five days after birth, phone your midwife immediately, so your baby can be checked promptly (NCCWCH 2014).
Why would my midwife break my waters?
Your midwife may offer to break your waters for you, to induce labour if you’re overdue (NHS 2016), or to speed up labour (NCCWCH 2014).
Read what mums say about induced labour.
References
Bailey J. 2014. The placenta. In: Marshall JE, Raynor MD. eds. Myles Textbook for Midwives. 16th ed. Edinburgh: Churchill Livingstone, 101-23
Jackson K, Marshall JE, Brydon S. 2014. Physiology and care during the first stage of labour. In: Marshall JE, Raynor MD. eds. Myles textbook for midwives. 16th ed. Edinburgh: Churchill Livingstone, 327-66
Lowth M. 2017. Labour: childbirth. Patient, patient.info [Accessed September 2019]
Middleton P, Shepherd E, Fenady V, et al. 2017. Planned early birth versus expectant management (waiting) for prelabour rupture of membranes at term (37 weeks or more). Cochrane Database of Systematic Reviews (1): CD005302. www.cochranelibrary.com [Accessed September 2019]
NCCWCH. 2008. Induction of labour. National Collaborating Centre for Women's and Children's Health, Clinical guideline 70. www.nice. org.uk [Accessed September 2019]
org.uk [Accessed September 2019]
NCCWCH. 2014. Intrapartum care: care of healthy women and their babies during childbirth. Updated February 2017. National Collaborating Centre for Women's and Children's Health, Clinical guideline, 190. www.nice.org.uk [Accessed September 2019]
Newson L. 2015. Meconium aspiration. Patient, Professional articles. patient.info [Accessed September 2019]
NHS. 2016. Choices when pregnancy reaches 41 weeks. NHS, National Institute for Health Research. www.nhs.uk [Accessed September 2019]
NHS. 2017. Am I in labour? NHS, Health A-Z, Pregnancy and baby. www.nhs.uk [Accessed September 2019]
NHS. 2018a. What is the amniotic sac? NHS, Common health questions, pregnancy. www.nhs.uk [Accessed September 2019]
NHS. 2018b. Vaginal discharge in pregnancy NHS, Health A-Z, Pregnancy and baby. www.nhs.uk [Accessed September 2019]
NHS Digital. 2018. Table 7.d: Delivery complications recorded by length of gestation, 2017-18. NHS Maternity Statistics, 2017-2018, HES NHS maternity statistics tables. digital.nhs.uk [Accessed September 2019]
NHS Maternity Statistics, 2017-2018, HES NHS maternity statistics tables. digital.nhs.uk [Accessed September 2019]
NICE. 2016. Sepsis: recognition, diagnosis and early management. National Institute for Health and Care Excellence, NICE guideline 51. www.nice.org.uk [Accessed September 2019]
Pintucci A, Meregalli V, Colombo P, et al. 2014. Premature rupture of membranes at term in low risk women: how long should we wait in the "latent phase"? J Perinat Med 42(2):189-96
RCOG. 2017. Information for you: group B streptococcus (GBS) in pregnancy and newborn babies. Royal College of Obstetricians and Gynaecologists. www.rcog.org.uk [Accessed September 2019]
Scorza WE. 2018. Management of prelabour rupture of the fetal membranes at term. UpToDate 03 Jan
Simkin P, Ancheta R. 2011. The labor progress handbook: early interventions to prevent and treat dystocia. 3rd ed. Chichester: Wiley Blackwell
Thomson AJ, on behalf of the Royal College of Obstetricians and Gynaecologists. 2019. Care of women presenting with suspected preterm prelabour rupture of membranes from 24+0 weeks of gestation. BJOG obgyn.onlinelibrary.wiley.com [Accessed June 2019]
2019. Care of women presenting with suspected preterm prelabour rupture of membranes from 24+0 weeks of gestation. BJOG obgyn.onlinelibrary.wiley.com [Accessed June 2019]
Tommy's. 2016. Waters breaking early (PPROM). Tommy's – the baby charity. www.tommys.org [Accessed September 2019]
Tommy's. 2017. What to expect when your waters break. Tommy's – the baby charity. www.tommys.org [Accessed September 2019]
Vorvick L. 2016. Amniotic fluid. MedlinePlus. medlineplus.gov [Accessed September 2019]
Show references Hide references
Waters breaking early (PPROM) | Tommy's
This page covers waters breaking early before 37 weeks. Read more about what to expect when your waters break after 37 weeks.
What is preterm prelabour rupture of membranes (PPROM)?
Your baby develops inside a bag of fluid called the amniotic sac. When your baby is ready to be born, the sac breaks and the fluid comes out through your vagina. This is your waters breaking. It is also known as rupture of the membranes.
This is your waters breaking. It is also known as rupture of the membranes.
Normally your waters break shortly before or during labour. If your waters break before labour at less than 37 weeks of pregnancy, this is known as preterm prelabour rupture of membranes or PPROM. If this happens, it can (but does not always) trigger early labour.
If your waters break early, the risks and treatment depend on your stage of pregnancy.
Is PPROM common in pregnancy?
PPROM happens in about 3% of pregnancies.
What causes PPROM?
We don’t always know why PPROM happens. But it may be caused by infection, or placental problems, such as placental insufficiency or a blood clot (haematoma) behind the placenta or membranes. Other risk factors may include if you:
- have had a premature birth or PPROM before
- have had any vaginal bleeding in pregnancy
- have had any direct trauma to the stomach
- have had cervical surgery or have a short cervix
- have experienced placental abruption before
- have extra fluid around the baby in the amniotic sac (polyhydramnios)
- are pregnant with more than 1 baby.

It is important to remember that PPROM is not caused by anything you did or didn’t do in pregnancy.
How will I know if my waters have broken?
Your waters breaking may feel like a mild popping sensation, followed by a trickle or gush of fluid that you can’t stop, unlike when you wee. The amount of fluid you lose may vary. You may not have any sensation of the actual ‘breaking’, and then the only sign that your waters have broken is the trickle of fluid. It doesn’t hurt when your waters break.
You can read more about what to expect when your waters break.
What should I do if my waters break early?
If you think your waters may have broken, you should contact your midwife or labour ward and go to the hospital for a check-up straight away.
Amniotic fluid is clear and a pale straw colour. It may be a little pinkish if it contains some blood, or it may be clear. You must tell your healthcare professional if:
- the waters are smelly or coloured
- you are losing blood.
This could mean that you and your baby need urgent attention.
If you think that you are leaking fluid from the vagina, wear a pad not a tampon so your doctor or midwife can check the amount and colour of your waters.
“I had cervical incompetence and PPROM. I was put on hospital bedrest, antibiotics and had regular scans on the remaining water levels. Despite the antibiotics my infection markers were getting worse and I had to be induced at 24 weeks because they didn't think my baby would survive much longer in an infected womb. He survived birth, spent 7 months in hospital and then came home. He's now almost 5 years old and starting school in September.”
Rachel
What happens at the hospital?
When you arrive at hospital, your healthcare professional will assess you to see if your waters have broken. This will also include a check on your general health including your temperature, pulse and blood pressure. They will also check your baby’s heartbeat and may do a urine test to check for infection.
Your healthcare professional will talk to you about what has happened, how you are feeling and your pregnancy history.
How is PPROM diagnosed?
Your healthcare professional will likely ask to do an internal vaginal examination (they will ask for your permission before doing so).
You may have what’s called a speculum examination. This is when a small instrument covered in gel is inserted into the vagina. The healthcare professional will then be able to see if there is any fluid pooling in the vagina. They will also take a swab to test for infection and a swab to test for group B strep infection. This will help confirm if your waters have broken. This test isn’t painful but it can sometimes be uncomfortable.
If it isn’t clear from the speculum examination, they may do a swab test of the fluid. They may also do an ultrasound scan to estimate the amount of fluid around your baby.
What happens next?
If your waters have broken, you will usually be advised to stay in hospital where you and your baby will be closely monitored for signs of infection. This may be for a few days or maybe longer. You will have your temperature, blood pressure and pulse taken regularly, as well as blood tests to check for infection. Your baby’s heart rate will also be monitored regularly.
This may be for a few days or maybe longer. You will have your temperature, blood pressure and pulse taken regularly, as well as blood tests to check for infection. Your baby’s heart rate will also be monitored regularly.
If your waters have not broken, you should be able to go home.
If only a very small amount of amniotic fluid is leaking, it is not always possible to see it during an examination and it can be difficult to confirm whether your waters have broken.
If you continue to leak fluid at home, you should return to the hospital for a further check-up.
What could PPROM mean for me and for my baby?
If your waters have broken early, your healthcare professional will discuss with you the possible outcomes for your baby. These will depend on how many weeks pregnant you are when this happens and your individual circumstances.
Infection
The membranes form a protective barrier around the baby. After the membranes break, there is a risk that you may develop an infection. This can cause you to go into labour early or cause you or your baby to develop sepsis (a life-threatening reaction to an infection).
This can cause you to go into labour early or cause you or your baby to develop sepsis (a life-threatening reaction to an infection).
The symptoms of infection include:
- a raised temperature
- an unusual vaginal discharge with an unpleasant smell
- a fast pulse rate
- pain in your lower stomach.
Your baby’s heart rate may also be faster than normal. If there are signs that you have an infection, your baby may need to be born straight away. This is to try to prevent both you and your baby becoming more unwell.
PPROM and premature birth
About 50% of women with PPROM will go into labour within 1 week after their waters break. The further along you are in your pregnancy, the more likely you are to go into labour within 1 week of your waters breaking. PPROM is associated with 3-4 out of every 10 premature births.
Babies born prematurely have an increased risk of health problems and may need to spend time a neonatal unit. Find out more about premature birth.
Find out more about premature birth.
Cord prolapse
This is when the umbilical cord falls through your cervix into the vagina. This is an emergency complication and can be life-threatening for your baby, but it is uncommon.
Pulmonary hypoplasia
This is when your baby’s lungs fail to develop normally because of a lack of fluid around them. It is more common if your waters break very early on in pregnancy (less than 24 weeks) when your baby’s lungs are still developing.
Placental abruption
This when your placenta separates prematurely from your uterus. It can cause heavy bleeding and can be dangerous for both you and your baby. Find out more about placental abruption.
If you experience PPROM, sometimes your baby sadly may not survive. There is a higher risk of this happening if your waters break very early, if the baby is born very prematurely or, in some cases, following infection or cord prolapse.
Are there any treatments for PPROM?
It is not possible to ‘fix’ or heal the membranes once they are broken. But you may be offered treatment to reduce the risks to your baby. This could include:
But you may be offered treatment to reduce the risks to your baby. This could include:
- a short course of antibiotics to reduce the risk of an infection and delay labour
- a course of steroid injections (corticosteroids) to help with your baby’s development and to reduce the chance of problems caused by being born prematurely
- magnesium sulphate once you are in labour, which can reduce the risk of your baby developing cerebral palsy if they are born very premature.
If you do go into premature labour, you may be offered intravenous antibiotics (where the antibiotics are given through a needle straight into a vein) to reduce the risk of early-onset group B strep infection.
Do I need to stay in hospital?
You will usually be advised to stay in hospital for 5 to 7 days after your waters break, to monitor your and your baby’s wellbeing. You may be allowed to go home after that if you are not considered at risk for giving birth early.
When should I seek help if I go home?
Contact your healthcare professional and return to the hospital immediately if you experience any of the following:
- raised temperature
- flu-like symptoms (feeling hot and shivery)
- vaginal bleeding
- if the leaking fluid becomes greenish or smelly
- contractions or cramping pain
- abdominal pain or back pain
- if you are worried that the baby is not moving as normal.
 Contact your midwife or maternity unit immediately if you think your baby’s movements have slowed down, stopped or changed.
Contact your midwife or maternity unit immediately if you think your baby’s movements have slowed down, stopped or changed.
You should be given clear advice on how to take your pulse and temperature at home. You’ll probably also be advised to avoid having sex during this time.
What follow-up should I have?
You should have regular check-ups with your healthcare professional (usually once or twice a week).
During these check-ups, your baby’s heart rate will be monitored, your temperature, pulse and blood pressure will be checked and you will have blood tests to look for signs of infection. Your doctor will work with you to make an ongoing plan for your pregnancy, including regular ultrasound scans to check on your baby’s growth.
Your mental health
Experiencing PPROM can be stressful and cause a lot of anxiety. Coping with new symptoms and complications in pregnancy can sometimes be overwhelming. You could try our top 10 tips to relax.
If you’re feeling low, talk to your partner, family or friends about how you are feeling. You can also talk to your midwife. You won’t be judged for how you feel. They will help you stay well so you can look after yourself and your baby. They may also be able to signpost you to more help and support if you need it.
You can also call the Tommy’s midwives for a free, confidential chat on 0800 014 7800 (Monday to Friday, 9am to 5pm), or email us at [email protected].
When is the right time to give birth?
If you and your baby are both well with no signs of infection, you may be advised to wait until 37 weeks to give birth. This is because it can reduce the risks associated with being born prematurely.
If you are carrying the GBS bacteria, then you may be advised to give birth from 34 weeks because of the risk of GBS infection for your baby.
Your healthcare professional will talk to you about what they think is best and ask you what you want to do. Don’t be afraid to ask as many questions as you need to in order to feel comfortable and able to make informed decisions about your care.
Will I be able to have a vaginal birth after PPROM?
This is possible, but it depends on when you go into labour, the position your baby is lying, and your own individual circumstances and choices.
Your healthcare professional will discuss this with you.
Will I have PPROM again a future pregnancy?
Possibly. Having PPROM or giving birth prematurely means that you are at an increased risk of having a preterm birth in any future pregnancies, but it doesn’t mean that you definitely will.
You will probably have specialist care in your next pregnancy. If you are not offered specialist care, you can ask for it. Remember that you can always talk to your midwife if you have any concerns about your care.
Why did the water in Argentina turn pink?
Residents of the Argentinean province of Chubut are worried that the river of the same name near their homes turned pink a few days ago. Once upon a time, this place was a good place to relax, but for several years, local people have been complaining about bad smells and other environmental problems around the river. As it turned out, the unusual color of the water is associated with emissions from a nearby fish factory. Once in the river, a chemical that destroys bacteria is used to store shrimp before transporting them to other cities and countries. The journalists shared photos of the place poisoned by the plant, so let's look at the pictures and find out what kind of chemical we are talking about and what caused the release. In fact, the plant poured waste into the local water quite deliberately, finding itself in a stalemate. But this is not a reason to remove the blame from her for what she did.
As it turned out, the unusual color of the water is associated with emissions from a nearby fish factory. Once in the river, a chemical that destroys bacteria is used to store shrimp before transporting them to other cities and countries. The journalists shared photos of the place poisoned by the plant, so let's look at the pictures and find out what kind of chemical we are talking about and what caused the release. In fact, the plant poured waste into the local water quite deliberately, finding itself in a stalemate. But this is not a reason to remove the blame from her for what she did.
Argentina's Chubut River turned pink due to chemical waste
River pollution in Argentina
According to Science Alert, the chemical found in the river is sodium sulfite. This antibacterial product is used in fish processing plants to treat sewage. After use, it and fish waste must be properly disposed of, but local companies have not been able to do this. The fact is that a few weeks ago, residents of the neighboring town of Rawson blocked the roads along which trucks with waste were moving.
Dozens of trucks come to us every day, it annoys the residents,” explained local resident Lada.
Trucks used this route to go to the treatment plant, but now they don't have that option. Therefore, the waste was dumped into the river. But to do this, no matter how difficult the situation was, was not worth it. After all, we are talking about the cleanliness of the environment, with which at the moment we already have serious problems.
Bird's-eye view of the Chubut River
Sodium sulfite damage
At the end of July, the water in the river was colored pink, which made the locals very upset. Once upon a time, people rested on the banks of Chubut, but today hardly anyone will dare to do this. According to the head of the local environmental control center Juan Micheloud, the substance that got into the water does not harm living organisms and the unnatural color will disappear in a few days. But other people do not agree with him, because traces of such severe damage cannot simply disappear.
Sodium sulfite turned the water pink
Apparently, each side is at least slightly wrong. Juan Michelud is right that sodium sulfite cannot seriously harm living organisms. The fact is that it is a food preservative and is referred to as E221 in various products. It is an effective bleach and is even used in food as a color stabilizer. There is no reason to believe that it is completely safe for health, but there is no obvious harm and it is approved for use in Russia and Europe.
No one knows when the water will restore its natural color
Read also: Why did the meteorite lake in India change its color dramatically?
The future of the poisoned river
Whether the plant will suffer any punishment is unknown. About 600,000 people live in the province of Chubut, and many of them work at this plant. If something happens to him, thousands of people may be left without work, which will certainly entail very unpleasant consequences. Local residents believe that it would be nice to build a recycling center somewhere nearby. But this will require large financial investments and take quite a lot of time. What the plant will do with waste further is also not clear.
Local residents believe that it would be nice to build a recycling center somewhere nearby. But this will require large financial investments and take quite a lot of time. What the plant will do with waste further is also not clear.
Links to interesting articles, funny memes and a lot of other interesting information can be found on our telegram channel. Subscribe!
It is worth noting that there are waters in the world that are colored pink for more natural reasons. The most striking example is Lake Hillier, located in Australia. For a long time it was believed that algae painted it in an unusual color. But in 1950, scientists analyzed the water and found no traces of plants capable of this. But in 2016, the study was re-conducted as part of the Extreme Microbiome Project. It turned out that the unusual color of the water is really the merit of the algae. We are talking about Dunaliella saline ( Dunaliella salina ), which is abundant in Lake Hillier. You can read more about the unusual lake at this link.
You can read more about the unusual lake at this link.
EnvironmentEcology
To send a comment, you must either
Pink color. Unusual pink lakes
At the end of the series of articles about the pink color, as always, an article about some interesting "pink" fact. this time it is not connected with fashion and beauty, but it is connected with the beauty of nature =). Well, if you want, you can see how pink (the color of the lake) is combined with blue (the sky)
We are talking about pink... lakes .
Source http://log-in.ru/articles/8-udivitelnykh-rozovykh-ozer-nasheiy-planety/ I will comment on something in italics.
Pink Lake is a lake that has a reddish or pink color due to the presence of algae that produce carotenoids (organic pigments). These include algae such as Dunaliella salina, which is a type of halophile green microalgae that lives in particularly salty sea water. Thanks to their pink color, these lakes are becoming more and more popular among tourists and photographers from all over the world.
1. Lake Hillier, Australia
This body of water is located on the edge of Middle Island. The peculiarity of the lake is its bright pink color. The color of the water is constant and does not change if water is poured into a container. The length of the lake is about 600 meters. It is separated from the ocean by a narrow strip of land, consisting of sand dunes covered with vegetation.
For the first time people discovered an unusual lake in 1802. Then the British navigator Matthew Flinders decided to stop on the island on his way to Sydney. What was the surprise of the traveler when, among the dense forests of the island, he stumbled upon a pink reservoir. The lake is surrounded by white salt deposits and dense forests of eucalyptus trees. To the north, sand dunes separate the lake from the Southern Ocean. (*when most of us were in school - there was no "southern ocean", now some single out it - this is the ocean around Antarctica*)
The lake is very popular and tourists tend to get there, even passengers of planes flying over the lake take pictures it is a miracle of nature.
2. Retba, Senegal
Lake Retba or Pink Lake is located to the east of the Cap Vert peninsula in Senegal, northeast of Dakar, the capital of Senegal. It got its name because of the color of the water in which Dunaliella salina algae grow.
There is a small salt mining business on the lake. Many workers who collect salt work 6-7 hours a day in the lake, which has a salt content of about 40%. To protect their skin, they rub "Beurre de Karité" (Shea butter, obtained from shea nuts harvested from the shea tree) into it, which softens the skin and prevents tissue damage. that was the lagoon. But the Atlantic surf gradually washed up the sand, and in the end the channel that connected the lagoon with the ocean turned out to be covered up. For a long time, Retba remained an unremarkable salt lake.
But in the 70s of the last century, a series of droughts hit Senegal, Retba became very shallow and the extraction of salt, which lay in a thick layer at the bottom, became quite profitable. At the same time, the water in the lake acquired a pink hue due to microorganisms that can exist in a saturated saline solution. In addition to them, there is no other organic life in Retba - for algae, not to mention fish, such a salt concentration is detrimental. It is here almost one and a half times higher than in the Dead Sea - three hundred and eighty grams per liter!
At the same time, the water in the lake acquired a pink hue due to microorganisms that can exist in a saturated saline solution. In addition to them, there is no other organic life in Retba - for algae, not to mention fish, such a salt concentration is detrimental. It is here almost one and a half times higher than in the Dead Sea - three hundred and eighty grams per liter!
Amazing color water and charming boats completely cover the two-kilometer coastline of Pink Lake, or Lake Retba, as it is called in the language of the Wolof people, the largest ethnic group in Senegal. ( *about the Wolof language - far from a fact, because the Senegalese themselves (both Wolof - the ethnic majority, and Peul, the people who specifically live there) call it Lac Rose and they don’t understand the name Retba, they can’t translate, although with languages there certain troubles - for example, a native urban resident of the Wolof people usually speaks a mixture of Wolof, French and Arabic and may not know some terms in the "rural" Wolof *)
3. Torrevieja Salt Lake (Alina de Torrevieja), Spain
Torrevieja Salt Lake (Alina de Torrevieja), Spain
Torrevieja Salt Lake and La Mata Salt Lake are salt lakes surrounding Torrevieja, a seaside town in southeastern Spain. The microclimate created by the largest salt lakes in Europe - Torrevieja and La Mata, is declared one of the healthiest in Europe, according to the World Health Organization.
A special type of algae grows in the water, which gives the water a pink hue. The pink color of Lake Torrevieja, caused by the presence of algae and salt, gives it a "science fiction" look. Just like in the Dead Sea in Israel, here you can also just lie on the surface of the water. In addition, it will bring great benefits for the prevention and treatment of diseases of the skin and lungs.
4. Hutt Lagoon, Australia
Hutt Lagoon is an elongated salt lake located off the coast north of the mouth of the Hutt River in midwestern Western Australia. It is located in the dunes adjacent to the coast.
It is located in the dunes adjacent to the coast.
Hutt Lagoon was once the mouth of the 60km (37 miles) Hutt River, but at some point in the prehistoric past, the river changed its course and the mouth remained isolated from both the river and the sea.
This lagoon is home to the world's largest microalgae farm. The total area of small artificial ponds in which Dunaliella saline is bred is 250 hectares.
5. Masazirgol Lake, Azerbaijan
Masazir Lake is a salt lake in the Karadag region, near Baku, Azerbaijan. The total area of the lake is 10 square kilometers. The ionic composition of water contains large amounts of chloride and sulfate.
6. Dusty Rose Lake, Canada
This pink lake, located in British Columbia, Canada, is quite unusual, little known and possibly unique. The water in this lake is not at all salty, and does not contain algae, but it still has a pink color.