Vitamin k jaundice newborn
Dispelling Myths: Vitamin K Injections For Newborns
- Home
- Texas Children's Blog
When a baby is born, parents want nothing more than to love and protect their child. Part of that protection starts right after birth with the administration of a vitamin K injection. Babies are not born with sufficient vitamin K levels and cannot get adequate amounts of vitamin K from breast milk, so this injection, given within the first hour after birth, is crucial because it helps a baby’s blood to clot normally, which prevents vitamin K deficiency bleeding (VKDB) in newborns.
A recent CDC report confirmed that there has been a nationwide increase in parents refusing the vitamin K shot for their newborns--- and this dangerous trend, often based on inaccurate information found online and faulty science, is causing more babies to experience hemorrhaging that is preventable and may cause brain damage or even death in some cases. In the United States, administration of intramuscular vitamin K at birth to prevent all forms of VKDB has been standard practice since first recommended by the American Academy of Pediatrics in 1961. Without the shot, the incidence of early and classical VKDB ranges from 0.25% to 1.7% of births and the incidence of late VKDB ranges from 4.4 to 7.2 per 100,000 infants. The relative risk for developing late VKDB has been estimated at 81 times greater among infants who do not receive intramuscular vitamin K than in infants who do receive it. Early VKBD usually presents in previously healthy appearing infants as unexpected bleeding during the first two weeks of age, usually between the second and fifth day after birth. The bleeding can present as oozing from the umbilical cord area, bleeding from the circumcision site, persistent oozing from puncture sites, gastrointestinal hemorrhage, and/or bleeding into the brain, which can result in significant neurological complications that have a lifelong impact on a child.
 Late VKDB is an indication of severe vitamin K deficiency and presents as unexpected bleeding, including brain bleeds in infants 2-12 weeks of age. Complications of late VKDB may be severe, including death. It classically presents in exclusively breastfed infants who received either no or inadequate neonatal vitamin K. It can also present in infants with intestinal malabosorption defects. One myth about vitamin-k injections is that they are linked to leukemia, but studies show absolutely no relationship between getting vitamin K as a baby and an increased risk of leukemia. Another myth is that the vitamin K injection increases the risk of jaundice---which is inaccurate. Jaundice associated with vitamin K has been observed only in high risk babies (such as premature babies) in doses 30-60 times higher than the dose we give. Some parents also argue that injections cause babies pain, but this pain is very brief and the benefits of the injection are very much worth a short period of discomfort.
Late VKDB is an indication of severe vitamin K deficiency and presents as unexpected bleeding, including brain bleeds in infants 2-12 weeks of age. Complications of late VKDB may be severe, including death. It classically presents in exclusively breastfed infants who received either no or inadequate neonatal vitamin K. It can also present in infants with intestinal malabosorption defects. One myth about vitamin-k injections is that they are linked to leukemia, but studies show absolutely no relationship between getting vitamin K as a baby and an increased risk of leukemia. Another myth is that the vitamin K injection increases the risk of jaundice---which is inaccurate. Jaundice associated with vitamin K has been observed only in high risk babies (such as premature babies) in doses 30-60 times higher than the dose we give. Some parents also argue that injections cause babies pain, but this pain is very brief and the benefits of the injection are very much worth a short period of discomfort.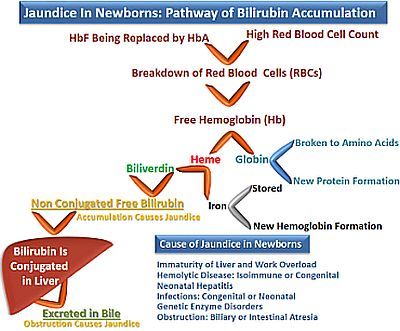 Parents are encouraged to mitigate this brief uncomfortable experience by holding baby skin to skin before and after the injection or allowing the baby to breastfeed before, during and/or after getting the injection. In the not so distant past, infants and children had high rates of dying early in life. During the 20th century alone, the infant mortality rate declined greater than 90% and the maternal mortality rate declined 99%! Much of this is due to advancements in modern medicine. While it might seem nice to do things completely naturally, modern medicine has saved the lives of countless mothers and babies. Update: For more information on this subject, Dr. Lauren Marcewicz, a pediatrician with CDC’s Division of Blood Disorders, speaks about vitamin K deficiency bleeding in infants, the importance of vitamin K prophylaxis at birth, and how healthcare providers can provide the best information to their expectant parents. Listen to the podcast by clicking here now.
Parents are encouraged to mitigate this brief uncomfortable experience by holding baby skin to skin before and after the injection or allowing the baby to breastfeed before, during and/or after getting the injection. In the not so distant past, infants and children had high rates of dying early in life. During the 20th century alone, the infant mortality rate declined greater than 90% and the maternal mortality rate declined 99%! Much of this is due to advancements in modern medicine. While it might seem nice to do things completely naturally, modern medicine has saved the lives of countless mothers and babies. Update: For more information on this subject, Dr. Lauren Marcewicz, a pediatrician with CDC’s Division of Blood Disorders, speaks about vitamin K deficiency bleeding in infants, the importance of vitamin K prophylaxis at birth, and how healthcare providers can provide the best information to their expectant parents. Listen to the podcast by clicking here now.
Author
Dr. Tiffany McKee-Garrett, Neonatologist
Tiffany McKee-Garrett, Neonatologist
Jaundice in Newborns - Dr. Weil's Condition Care Guide
What is newborn jaundice?
Newborn jaundice, or neonatal hyperbilirubinemia, is a condition resulting from excessive amounts of bilirubin in the blood. Bilirubin is a normal breakdown product of red blood cells. Newborn jaundice occurs when bilirubin builds up faster than a baby’s ability to eliminate it from the body. Research shows that jaundice occurs in approximately 60 percent of full term babies and 80 percent of premature babies. Under certain conditions, abnormally high levels of bilirubin can develop and be toxic to newborns, particularly to their nervous systems. Fortunately, most neonatal jaundice resolves over time without any treatment, or with only minimal intervention.
What are the signs and symptoms?
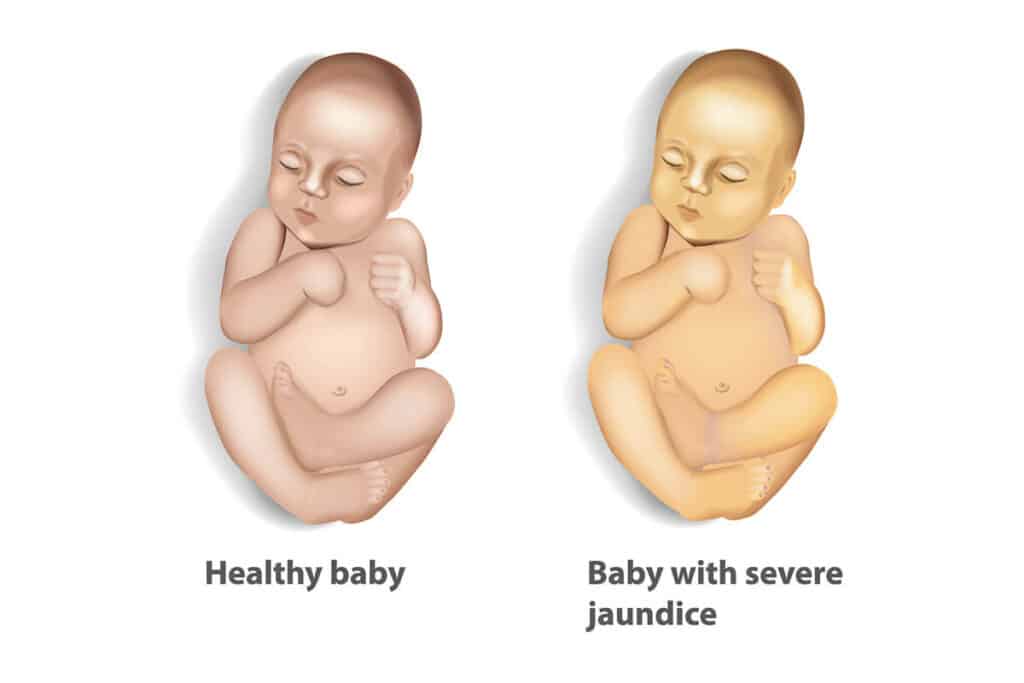
The classic sign of newborn jaundice is yellowing of the skin and sclera (the white part) of the eyes. These babies often look like they have a suntan.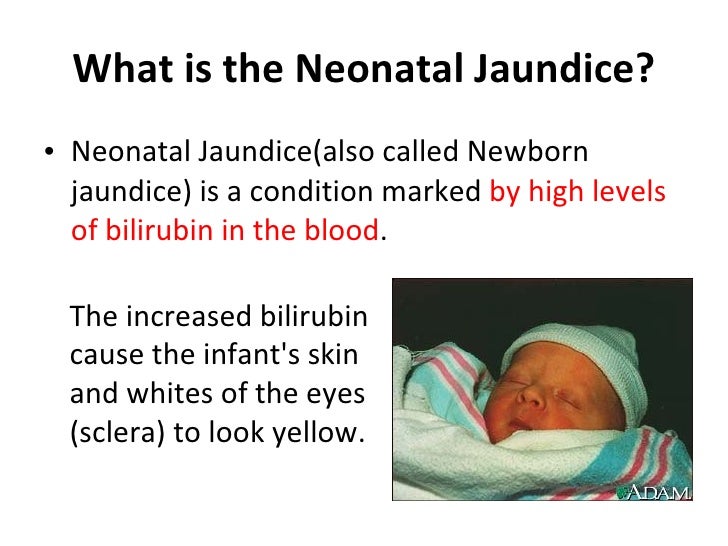 The jaundice can appear in stages, depending on how much bilirubin is circulating. Although not always a true indication of how severe the bilirubinemia is, when the concentration is at around five milligrams per deciliter (mg/dL), only the face appears yellow with the yellowish tint advancing down the body as bilirubin increases. At around 15 mg/dL, it typically moves down to the abdomen; and at over 20 mg/dL, the entire body is yellow including the soles of the feet. A simple way to check for jaundice is to gently press a finger against the baby’s skin. Normally, when you remove your finger, the area will momentarily turn white, but a jaundiced baby’s skin will remain yellow in color.
The jaundice can appear in stages, depending on how much bilirubin is circulating. Although not always a true indication of how severe the bilirubinemia is, when the concentration is at around five milligrams per deciliter (mg/dL), only the face appears yellow with the yellowish tint advancing down the body as bilirubin increases. At around 15 mg/dL, it typically moves down to the abdomen; and at over 20 mg/dL, the entire body is yellow including the soles of the feet. A simple way to check for jaundice is to gently press a finger against the baby’s skin. Normally, when you remove your finger, the area will momentarily turn white, but a jaundiced baby’s skin will remain yellow in color.
High concentrations of bilirubin can lead to poor feeding and lethargy (extreme sleepiness). At levels over 25 mg/dL, there is a risk for hearing loss, mental retardation, spastic paralysis and, if left untreated, even death. Kernicterus (permanent brain damage) is a condition caused by excessively high levels of bilirubin that are left untreated. This is extremely rare in developed nations, however, due to early recognition and treatment.
This is extremely rare in developed nations, however, due to early recognition and treatment.
What are the causes?
Hemoglobin is the pigment in red blood cells (RBCs) that carries oxygen and gives blood its color. As RBCs age and are broken down they release their hemoglobin, which is processed a number of times before it is removed by the body. Bilirubin is a yellowish-orange pigment produced during the processing of hemoglobin in the liver. Normally, bilirubin passes through the liver and is excreted as bile into the intestines, where it is eliminated from the body through the bowels. Because newborns have immature livers, they often are unable to remove bilirubin as quickly as they make it, which results in the yellowish skin tone. This is called physiologic jaundice. It is very common and typically presents between the second and third day of life, peaks by day four, and resolves without intervention within 2 weeks.
Breastfeeding jaundice and breast milk jaundice are variants of jaundice related to nursing babies.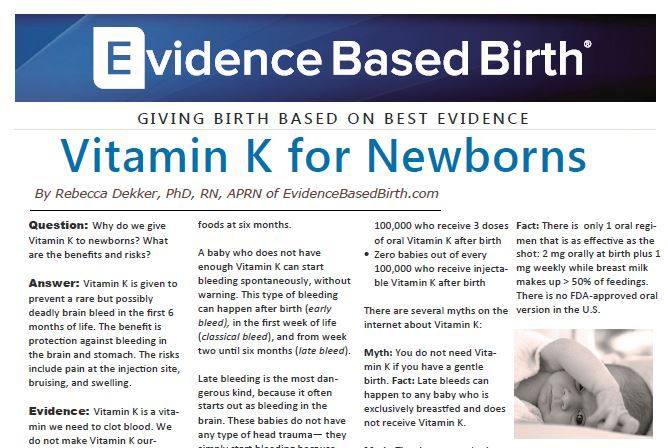 Approximately 13% of breast-fed newborns will become jaundiced during the first seven days. This is typically seen when babies are not nursing as much as their bodies require, leading to reduced numbers of stools and decreased excretion of bilirubin through the bowels. Breast milk jaundice, on the other hand, usually presents after the first week of life. This is less common. It affects about one in 200 babies, and there is still uncertainty as to what its cause might be; possibly, enzymes in mother’s milk may allow bilirubin to be reabsorbed from the GI tract back into the blood. Another theory suggests that certain fats in mother’s milk may be processed preferentially by the liver, allowing concentrations of bilirubin to rise. Regardless, breast milk jaundice usually peaks at weeks two or three, and resolves without treatment.
Approximately 13% of breast-fed newborns will become jaundiced during the first seven days. This is typically seen when babies are not nursing as much as their bodies require, leading to reduced numbers of stools and decreased excretion of bilirubin through the bowels. Breast milk jaundice, on the other hand, usually presents after the first week of life. This is less common. It affects about one in 200 babies, and there is still uncertainty as to what its cause might be; possibly, enzymes in mother’s milk may allow bilirubin to be reabsorbed from the GI tract back into the blood. Another theory suggests that certain fats in mother’s milk may be processed preferentially by the liver, allowing concentrations of bilirubin to rise. Regardless, breast milk jaundice usually peaks at weeks two or three, and resolves without treatment.
There are many less common causes of jaundice in newborns. Any event or condition that raises the number of RBCs that need to be processed by the liver can cause jaundice.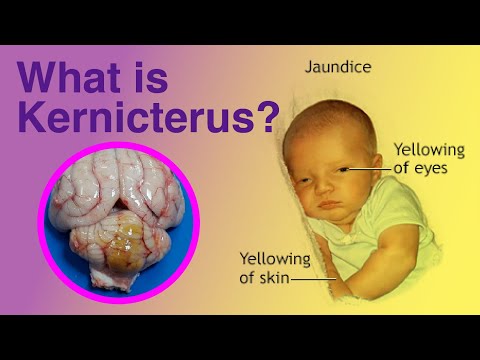 Sometimes the natural trauma during a difficult childbirth can produce significant bruising and excessive damage to red blood cells result. The use of suction to the baby’s head in vacuum-assisted deliveries often results in the formation of a hematoma and consequently increased RBCs that need to be processed. A baby can also swallow blood during childbirth, which travels to the intestines and is reabsorbed into the bloodstream. Abnormal blood cell shapes and children born with polycythemia (a disease in which the proportion of blood volume made up of RBCs increases) can create an overload of RBCs to be processed. In mother-baby blood incompatibility (also called Rh incompatibility), maternal antibodies that pass through the umbilical cord to the baby will attack fetal blood cells causing bilirubin levels to rise significantly.
Sometimes the natural trauma during a difficult childbirth can produce significant bruising and excessive damage to red blood cells result. The use of suction to the baby’s head in vacuum-assisted deliveries often results in the formation of a hematoma and consequently increased RBCs that need to be processed. A baby can also swallow blood during childbirth, which travels to the intestines and is reabsorbed into the bloodstream. Abnormal blood cell shapes and children born with polycythemia (a disease in which the proportion of blood volume made up of RBCs increases) can create an overload of RBCs to be processed. In mother-baby blood incompatibility (also called Rh incompatibility), maternal antibodies that pass through the umbilical cord to the baby will attack fetal blood cells causing bilirubin levels to rise significantly.
Sometimes jaundice can be a sign of a serious underlying problem. Any condition that interferes with the body’s ability to process hemoglobin can abnormally raise bilirubin levels such as prematurity, hypoxia (lack of oxygen), thyroid insufficiency, certain enzyme deficiencies, and infection.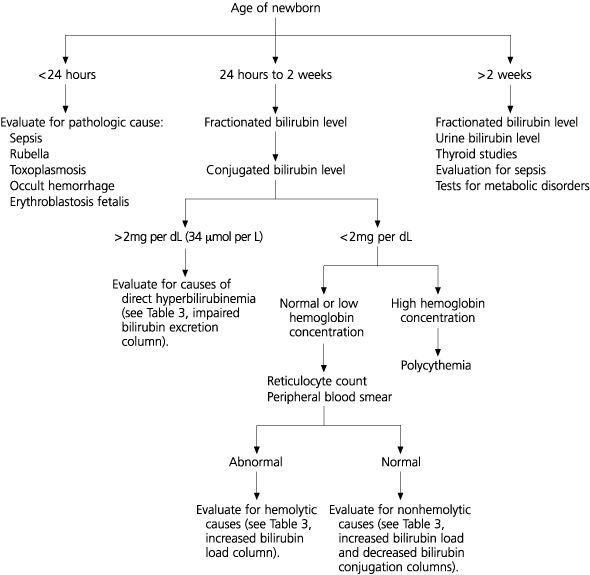 Pitocin, a drug commonly used to induce delivery, is associated with increased bilirubin levels in newborns. Additionally, supplementing with vitamin K during pregnancy can sometimes increase the risk of neonatal jaundice, as can mothers who are diabetic during pregnancy.
Pitocin, a drug commonly used to induce delivery, is associated with increased bilirubin levels in newborns. Additionally, supplementing with vitamin K during pregnancy can sometimes increase the risk of neonatal jaundice, as can mothers who are diabetic during pregnancy.
What is the conventional treatment?
When the jaundice is caused from breastfeeding, typically it will resolve on its own. Supplementing breast milk with formula for one to two days often increases stooling and causes the levels to fall quickly, and they generally do not rise again once breastfeeding is resumed. If the baby is well enough, even though bilirubin levels may be elevated, the doctor may want mom to simply increase feedings to avoid interrupting breastfeeding and the bond it creates between mother and child.
UV light helps in the breakdown of bilirubin, and if bilirubin levels rise between 15-20 mg/dL, phototherapy may be indicated The newborn is placed under special blue lights (with protective eyewear) that assist in the processing of bilirubin into lumirubin, a compound with a different structural formula that is more easily eliminated by the baby.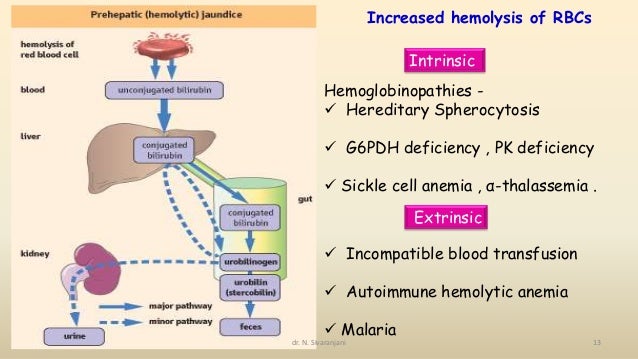
A different type of light therapy can be used at home. A “bili-blanket” is a fiberoptic blanket that is placed against the baby’s bare back and works similarly to phototherapy. Once levels normalize, they usually will not become elevated again. Cases of physiologic jaundice almost never require treatment beyond phototherapy.
In the most severe cases of jaundice, an exchange transfusion is required. In this procedure, small amounts of the baby’s blood are replaced with fresh donated blood, thus diluting the bilirubin and (in the case of Rh incompatibility) maternal antibodies if present. This is a specialized procedure typically performed in facilities that care for critically ill children. Recently, promising studies have shown that treating severely jaundiced babies with intravenous immunoglobulin is very effective at reducing bilirubin levels to safe ranges.
What does Dr. Weil recommend for newborn jaundice?
Early detection of rising bilirubin levels is key to preventing problems.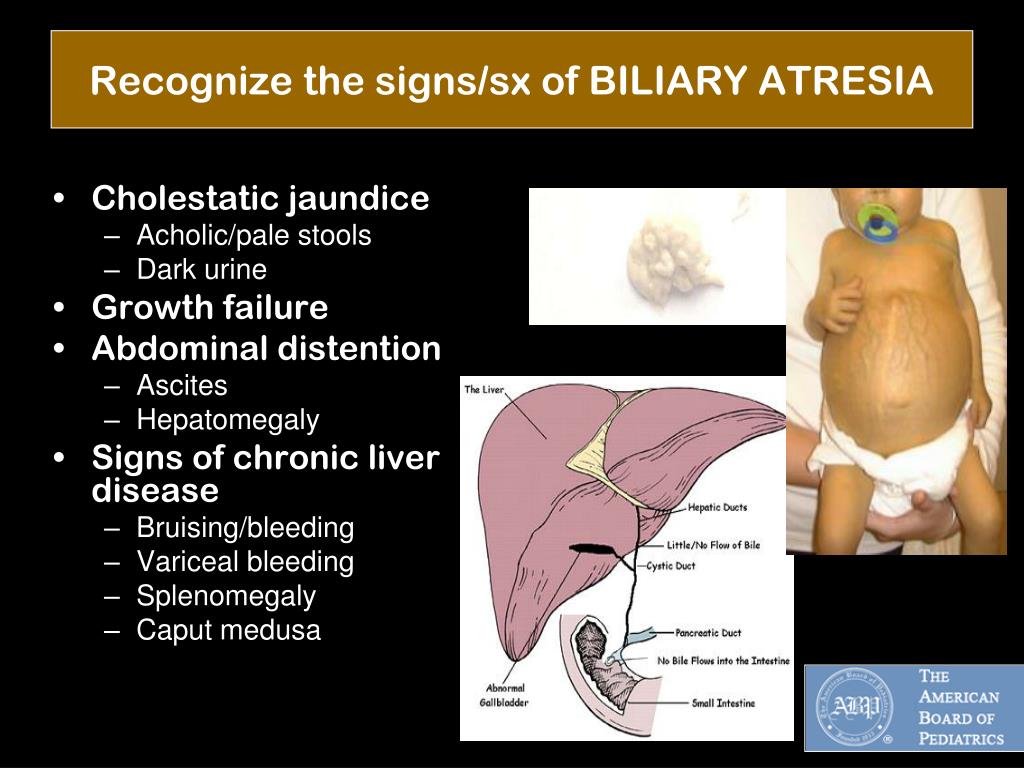 Any premature child, and all full term infants that are discharged home on the first day after delivery should be seen by a doctor or trained health care professional during the next few days.
Any premature child, and all full term infants that are discharged home on the first day after delivery should be seen by a doctor or trained health care professional during the next few days.
In newborns, some degree of jaundice is normal, not preventable and is not a health risk. The risk of significant jaundice can often be reduced by feeding babies at least eight to 12 times a day for the first several days and by carefully identifying infants at highest risk. All pregnant women should be tested for blood type and unusual antibodies. If the mother is Rh negative, follow-up testing on the infant’s cord blood is absolutely required.
Lactation consultants can offer helpful suggestions if breastfeeding mothers have issues or concerns. Sometimes unbundling a sleepy infant completely can allow better feeding than when the child is too cozy. Exposing infants to mild amounts of sunlight by sitting them near the window or outside for twenty minutes can also help break down bilirubin. Obviously, this works better in summertime than in winter.
Obviously, this works better in summertime than in winter.
Physiological jaundice of newborns - maternity hospital "Leleka"
Even in the maternity hospital, in the second or third life of a newborn, the child's skin may become yellowish. This is a manifestation of physiological jaundice in newborns. We immediately hasten to reassure young mothers: this is not a disease, but a symptom that has nothing to do with jaundice in liver diseases in adults.
What is physiological jaundice and where does it come from
As you know, human blood contains erythrocytes - red blood cells that carry oxygen between tissues and organs. They live for a relatively short time, and then break down into components that are excreted from the body by the liver and kidneys. One of the components is bilirubin, a pigmenting substance. With the massive breakdown of red blood cells, bilirubin accumulates in the tissues and gives the skin and whites of the eyes a yellowish tint. The icteric color of the skin in adults is diagnosed with liver dysfunction. nine0003
The icteric color of the skin in adults is diagnosed with liver dysfunction. nine0003
A massive breakdown of erythrocytes also occurs in the body of a newborn. Inside the womb, when the baby is not breathing with lungs, it needs more red blood cells to fully supply oxygen. When a child is born, more oxygen enters the blood, some of the red blood cells are released and quickly destroyed. This produces bilirubin. And the liver of a newborn cannot yet remove a large amount of bilirubin at the same time, it accumulates in the skin, and the baby becomes yellowish. nine0003
How to treat physiological jaundice in newborns
Physiological jaundice is a normal condition for a newborn baby, it is not contagious, goes away on its own after a few days, and does not affect the general condition of the body. But you can help the baby's body to quickly cope with the withdrawal of bilirubin. There are several factors that stimulate jaundice:
- Retention of meconium in the body;
- Fasting;
- Hypothermia.
 nine0021
nine0021 - Premature birth;
- Medical stimulation of the labor process, administration of oxytocin;
- Congenital disorders of the biliary tract;
- Rh-conflict of mother and child;
- Maternal diabetes mellitus;
- Infectious diseases;
- Internal hemorrhages in a child; nine0016
- Cracked nipples in mother and blood in baby's digestive tract;
- Other reasons.
- WHEC UPDATE
- Violence against women
- Obstetrics
- Newborn care
- Medicine Diseases during pregnancy
- Diagnostic Ultrasound
- Infectious diseases during pregnancy nine0015 Pain management during work and delivery
- Gynecology
- Focus on mental health
- Gynecological and Cytopathology
- Gynecological Oncology
- Uro/Gynecology
- Obstetric fistula
- Health Policy & Women's Health nine0015 Glossary
- Main page (Russian)
- Editorial
- List of articles
- Overview of the
blood clotting system This overview simplifies the understanding of the blood clotting system as a whole, and also discusses various abnormalities that can affect the operation of perioperative and intensive care units (ICUs). Coagulation is a dynamic process and understanding of the blood coagulation system has evolved in recent years in anesthesia practice. Although the traditional classification of coagulation gives a more reliable description of the same. The coagulation process is usually under the inhibitory control of several inhibitors, which limit the formation of a clot, thereby preventing the spread of a thrombus. This delicate balance is upset whenever the procoagulant activity of clotting factors increases or the activity of natural inhibitors decreases. An imbalance between the two components predisposes the patient to bleeding or thrombosis. Therefore, it is necessary to understand the physiology of the same in order to predict the pathological and clinical consequences of the same before any pharmacological interventions are carried out. Accurate reporting of PT/INR results has a direct impact on the management of patients receiving vitamin K antagonist therapy. An appropriate standardization process can greatly improve the accuracy of reported results.
Coagulation is a dynamic process and understanding of the blood coagulation system has evolved in recent years in anesthesia practice. Although the traditional classification of coagulation gives a more reliable description of the same. The coagulation process is usually under the inhibitory control of several inhibitors, which limit the formation of a clot, thereby preventing the spread of a thrombus. This delicate balance is upset whenever the procoagulant activity of clotting factors increases or the activity of natural inhibitors decreases. An imbalance between the two components predisposes the patient to bleeding or thrombosis. Therefore, it is necessary to understand the physiology of the same in order to predict the pathological and clinical consequences of the same before any pharmacological interventions are carried out. Accurate reporting of PT/INR results has a direct impact on the management of patients receiving vitamin K antagonist therapy. An appropriate standardization process can greatly improve the accuracy of reported results. nine0016
nine0016 - Vitamin K deficiency bleeding
Prevention of early vitamin K deficiency bleeding (VKHD) in the newborn with onset at birth before 2 weeks of age (previously known as classical hemorrhagic disease of the newborn) by oral or parenteral vitamin K is common practice. Vitamin K is essential for the synthesis of several blood clotting factors. Infants can easily develop vitamin K deficiency due to poor placental transfer, low vitamin K content in breast milk, and poor intestinal absorption due to immature intestinal flora and malabsorption. VKDB in infancy is classified depending on the time of presentation: early (within 24 hours), classic (within 1 week after birth) and late (from 2 weeks to 6 months). Prophylactic administration of vitamin K to prevent VKDB has been practiced in the United States for decades in both term and preterm infants. A single dose (1.0 mg) of intramuscular (IM) vitamin K after birth is effective in preventing classic VKD in term infants. Both intramuscular (1.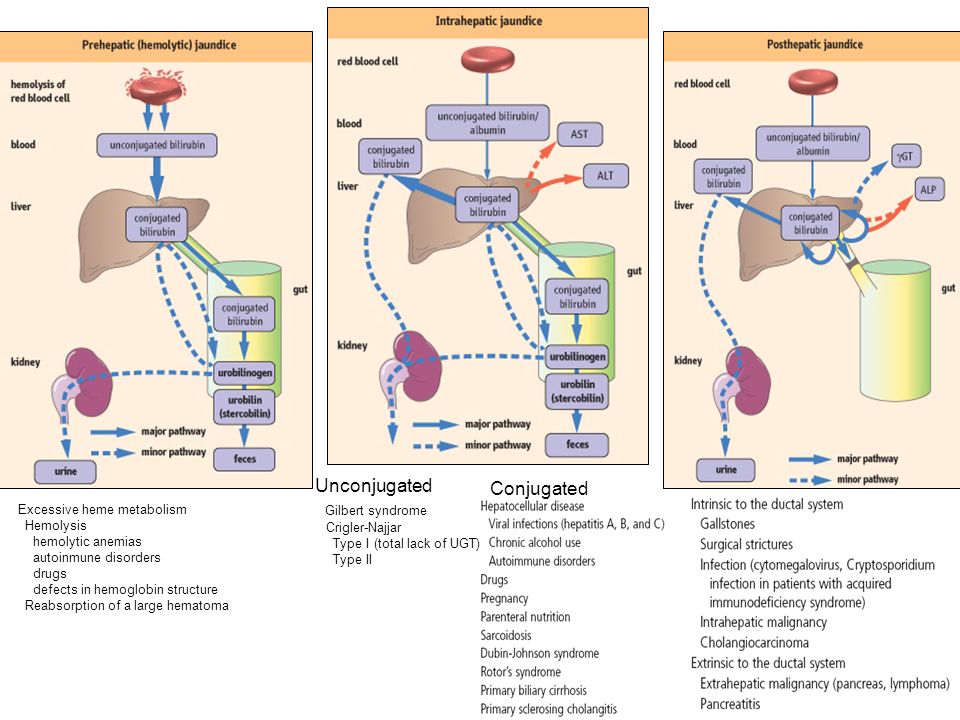 0 mg) and oral vitamin K prophylaxis improve biochemical parameters of blood coagulation for a period of one to seven days. This review provides updated recommendations for the use of vitamin K for the prevention of early and late VKDB. nine0016
0 mg) and oral vitamin K prophylaxis improve biochemical parameters of blood coagulation for a period of one to seven days. This review provides updated recommendations for the use of vitamin K for the prevention of early and late VKDB. nine0016 - Neonatal seizures
Neonatal seizures usually indicate a serious underlying disorder. Neonatal seizures differ in clinical description from seizures in adults, and seizures in preterm infants differ from seizures in term infants. The organization of the cerebral cortex, synaptogenesis, and myelination of cortical efferent pathways in newborns are poorly developed, which leads to weakly spreading fragmentary seizures, the electrical activity of which may not extend to the EEG surface electrodes. There are four recognizable clinical types of seizures: subtle; clonic; Tonic; and myoclonic. The neonatal period is a period of intense physiological synaptic excitability, since the synaptogenesis that occurs at this point in time is completely dependent on activity.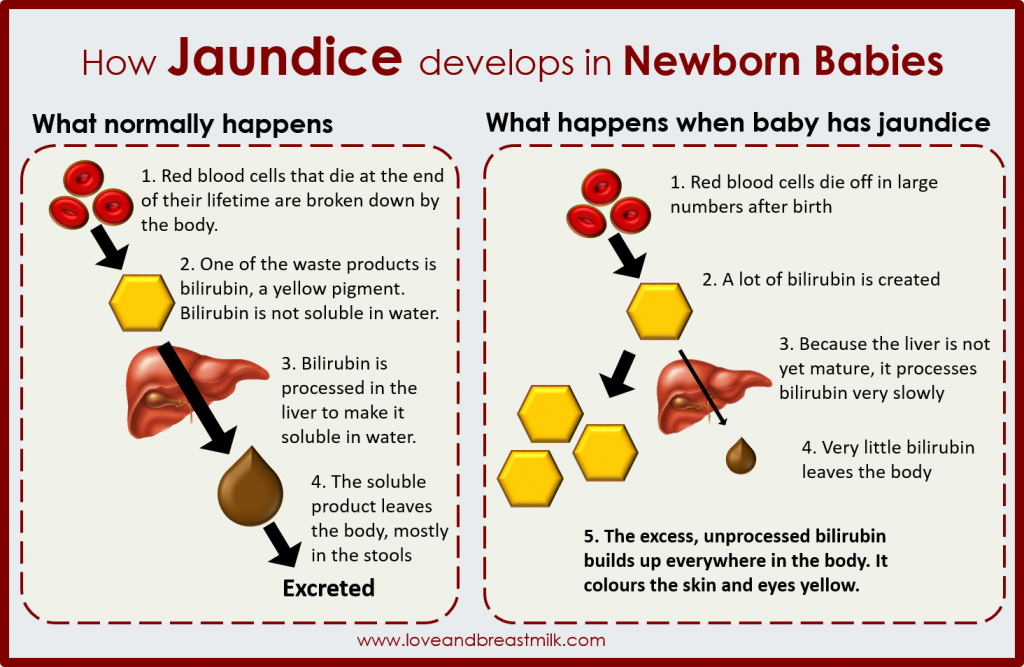 In humans, the density of synapses and dendritic vertebrae peaks during gestation and in the first month of life. Recognition often helps in prognosis and treatment; the most common is hypoxic-ischemic encephalopathy (HIE). Patients generally have a poor prognosis, with most developing severe encephalopathy and epilepsy. A review of the literature indicates that neonatal seizures and their etiology have a significant impact on the developing brain; It is very important to recognize seizures at an early stage and start immediate antiepileptic therapy. Continuous computerized simultaneous video electroencephalograph (EEG) monitoring is required; Infants at risk often have electrographic seizures without clinical manifestations. The poor prognosis for preterm infants with seizures is reflected in high rates of subsequent long-term disability and mortality. The severity and timing of the pathological process continue to be major determinants of outcome. Although there are antiepileptic treatments for seizures in newborns, they are ineffective in more than 35% of cases.
In humans, the density of synapses and dendritic vertebrae peaks during gestation and in the first month of life. Recognition often helps in prognosis and treatment; the most common is hypoxic-ischemic encephalopathy (HIE). Patients generally have a poor prognosis, with most developing severe encephalopathy and epilepsy. A review of the literature indicates that neonatal seizures and their etiology have a significant impact on the developing brain; It is very important to recognize seizures at an early stage and start immediate antiepileptic therapy. Continuous computerized simultaneous video electroencephalograph (EEG) monitoring is required; Infants at risk often have electrographic seizures without clinical manifestations. The poor prognosis for preterm infants with seizures is reflected in high rates of subsequent long-term disability and mortality. The severity and timing of the pathological process continue to be major determinants of outcome. Although there are antiepileptic treatments for seizures in newborns, they are ineffective in more than 35% of cases.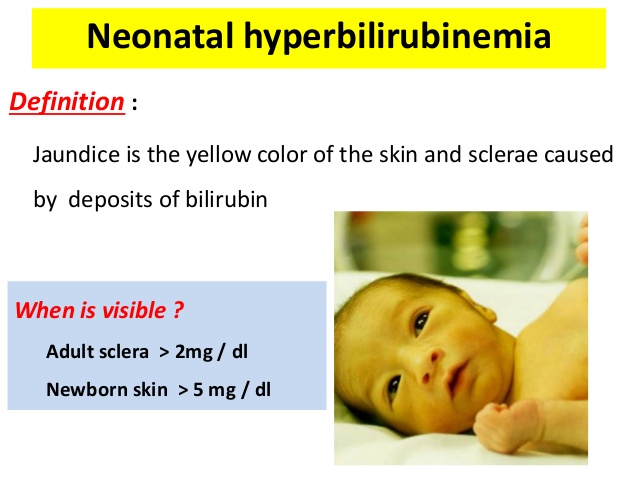 The prognosis is determined primarily by etiology. The aim of the study should be to develop more effective treatments for neonatal seizures, regardless of etiology. nine0016
The prognosis is determined primarily by etiology. The aim of the study should be to develop more effective treatments for neonatal seizures, regardless of etiology. nine0016 - Group B neonatal streptococcal infection
Group B streptococcal infection (GBS) remains the most common cause of early-onset neonatal sepsis and an important cause of late sepsis in infants. This review reviews the epidemiology, microbiology, pathogenesis of the disease, and treatment strategies for neonatal early- and late-onset GBS infection. While most children recover from GBS infection, some are born stillborn, others die in the first weeks of life, and others suffer lifelong disabilities. Prevention strategies (antibiotic prophylaxis during labor) for early invasive GBS in infants are currently limited to developed countries and only during labor. GBS recurrence in newborns and young children may occur after completion of appropriate treatment of the primary infection. There are no good prospective studies to indicate the optimal choice of therapy in a neonate with possible sepsis, but ampicillin and gentamicin are usually appropriate based on the usual susceptibility of the predominant organisms causing early sepsis.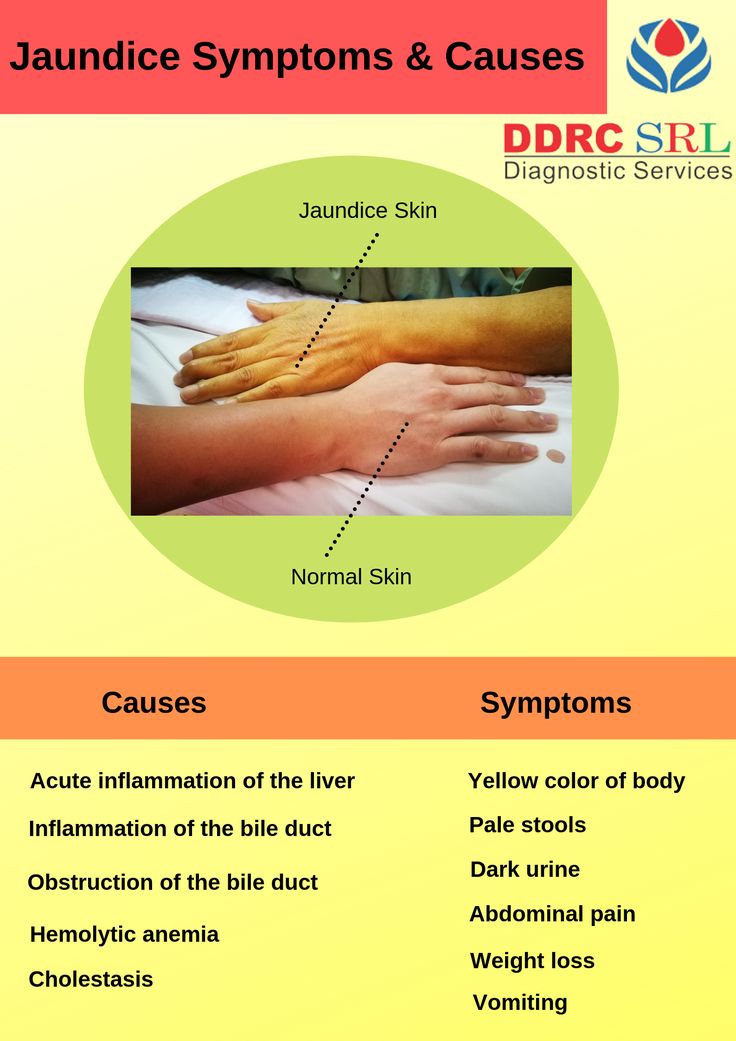 GBS vaccination will be acceptable for most women, and GBS vaccines are in the early stages of development. While most children recover from GBS infection, some are born stillborn, others die in the first weeks of life, and others suffer lifelong disabilities. nine0016
GBS vaccination will be acceptable for most women, and GBS vaccines are in the early stages of development. While most children recover from GBS infection, some are born stillborn, others die in the first weeks of life, and others suffer lifelong disabilities. nine0016 - Neonatal hearing loss detection and intervention
Hearing loss can affect a child's ability to develop communication, language and social skills. The sooner children with hearing loss receive services, the more likely they are to reach their full potential. The most important time for a child to learn a language is during the first 3 years of life when the brain develops and matures. In fact, children begin to learn speech and language in the first 6 months of life. In 2017, the Early Hearing Detection and Intervention Act (EHDI) reauthorizes the Health Resources and Services Administration (HRSA) to continue funding awards to states, territories, and healthcare providers to support continuous improvement in EHDI programs. These projects help to identify effective strategies to address screening, loss to follow-up diagnosis and services, inclusion in early intervention services, and family engagement. A variety of communication and intervention options are available for children with hearing loss. With the help of health professionals and intervention specialists, families can choose the options that best suit their needs. nine0016
These projects help to identify effective strategies to address screening, loss to follow-up diagnosis and services, inclusion in early intervention services, and family engagement. A variety of communication and intervention options are available for children with hearing loss. With the help of health professionals and intervention specialists, families can choose the options that best suit their needs. nine0016 - Neonatal Withdrawal Syndrome
Neonatal Withdrawal Syndrome (NAS) is the result of the sudden cessation of fetal exposure to substances used or abused by the mother during pregnancy. Withdrawal from legal or illicit substances is becoming more common among newborns in both developed and developing countries. Opioids such as morphine or methadone are recommended as first-line therapy, and phenobarbital or clonidine as add-on therapy. Further research is needed to determine best practice in the assessment, non-pharmacological intervention, and pharmacological management of infants with NAS to improve outcomes.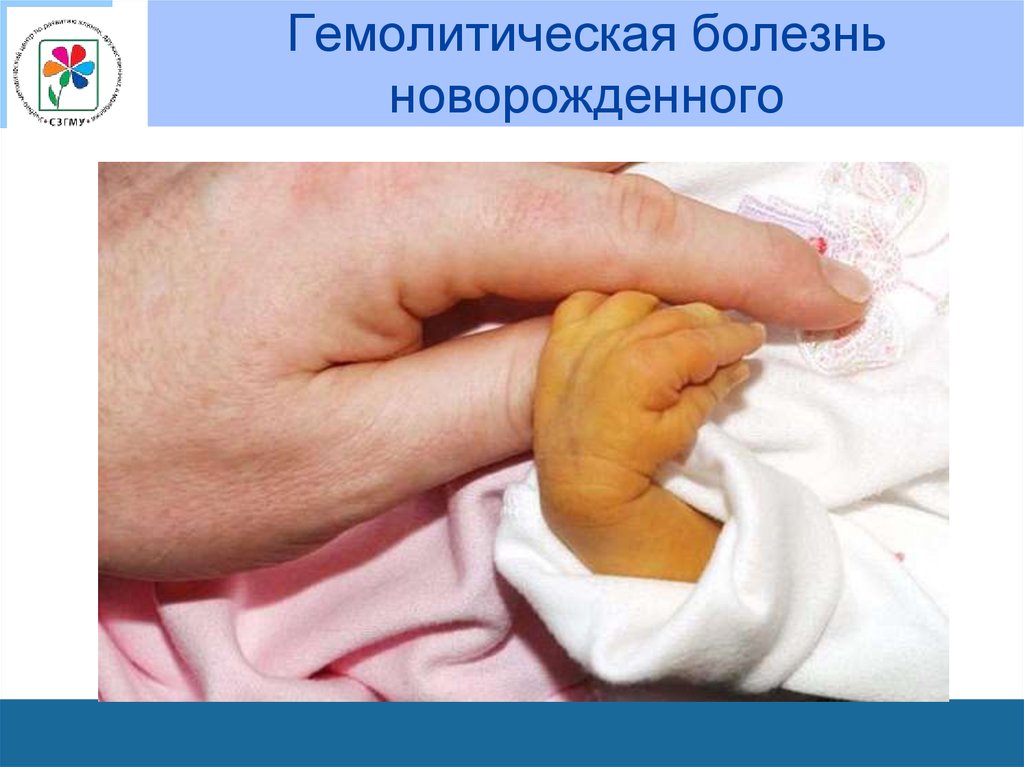 Lessons learned from prenatal alcohol exposure may be relevant to opioids. Full consideration should be given to the postpartum environment of children with prenatal opioid exposure, which may include social and economic difficulties adversely affecting the development of the child. It is more appropriate to prescribe opioids after caesarean section, given the individual needs for opioids in the hospital or the general decision-making model. During breastfeeding, give preference to acetaminophen and ibuprofen. nine0016
Lessons learned from prenatal alcohol exposure may be relevant to opioids. Full consideration should be given to the postpartum environment of children with prenatal opioid exposure, which may include social and economic difficulties adversely affecting the development of the child. It is more appropriate to prescribe opioids after caesarean section, given the individual needs for opioids in the hospital or the general decision-making model. During breastfeeding, give preference to acetaminophen and ibuprofen. nine0016 - Birth trauma: neonatal brachial plexus injury
The review focuses on neonatal brachial plexus palsy (NBPP) with particular emphasis on its pathophysiology, causation and treatment. Several strategies are included that demonstrate either a reduction in NBPP or an increase in the rate of successful resolution of shoulder dystocia. The main goal in the presence of clinically recognizable shoulder dystocia remains to deliver the fetus before the fetal brain experiences hypoxic-ischemic injury. Perinatal disorders are prone to malpractice litigation. NBPP results from stretching of the nerves in the perinatal period and can lead to paresis or paralysis and loss of sensation in the affected hand. Knowledge about NBPP is constantly evolving. What is known at this time with reasonable certainty is that NBPP occurs infrequently and may be caused by maternal (endogenous) forces or applied (exogenous) clinician forces, or a combination of the two. Do interdisciplinary shoulder dystocia exercises regularly. Caesarean section reduces, but does not eliminate, the risk of birth trauma and NSAIDs associated with macrosomia. In general, in terms of surgical treatment, primary surgery includes surgical procedures involving nerve transfer, and the ulnar, median, and phrenic nerves are used as grafts/donors in this type of surgery. nine0016
Perinatal disorders are prone to malpractice litigation. NBPP results from stretching of the nerves in the perinatal period and can lead to paresis or paralysis and loss of sensation in the affected hand. Knowledge about NBPP is constantly evolving. What is known at this time with reasonable certainty is that NBPP occurs infrequently and may be caused by maternal (endogenous) forces or applied (exogenous) clinician forces, or a combination of the two. Do interdisciplinary shoulder dystocia exercises regularly. Caesarean section reduces, but does not eliminate, the risk of birth trauma and NSAIDs associated with macrosomia. In general, in terms of surgical treatment, primary surgery includes surgical procedures involving nerve transfer, and the ulnar, median, and phrenic nerves are used as grafts/donors in this type of surgery. nine0016 - Sudden Infant Death Syndrome
Significant new information has been received in recent decades about sudden infant death and early childhood apnea. Sudden Infant Death Syndrome (SIDS), also known as Sudden Unexpected Infant Death (SUID) and Sudden Unexpected Death in Infancy (SUDI), are terms used to describe the unexpected death of an infant under 12 months of age. The cause of death could not be explained after a thorough investigation, examination of the place of death and examination of the medical history. The sleep position for each sleep campaign has helped educate millions of caregivers, parents, grandparents, aunts, uncles, nannies, child care providers, health care providers, and others about ways to reduce the risk of reducing SIDS and other sleep-related causes of childhood death. Belly time describes the time you place your baby on your stomach while he is awake and someone is watching. Belly time is important. Newborn safety should be regularly taught in obstetric curricula, and the Women's Health and Education Center (WHEC) is collaborating with the United Nations (UN) and the World Health Organization (WHO) to distribute updated literature and guidance to healthcare professionals regarding newborns.
Sudden Infant Death Syndrome (SIDS), also known as Sudden Unexpected Infant Death (SUID) and Sudden Unexpected Death in Infancy (SUDI), are terms used to describe the unexpected death of an infant under 12 months of age. The cause of death could not be explained after a thorough investigation, examination of the place of death and examination of the medical history. The sleep position for each sleep campaign has helped educate millions of caregivers, parents, grandparents, aunts, uncles, nannies, child care providers, health care providers, and others about ways to reduce the risk of reducing SIDS and other sleep-related causes of childhood death. Belly time describes the time you place your baby on your stomach while he is awake and someone is watching. Belly time is important. Newborn safety should be regularly taught in obstetric curricula, and the Women's Health and Education Center (WHEC) is collaborating with the United Nations (UN) and the World Health Organization (WHO) to distribute updated literature and guidance to healthcare professionals regarding newborns. security. nine0016
security. nine0016 - Neonatal jaundice: part I
Jaundice (hyperbilirubinemia) occurs in most newborns. Jaundice is a benign disease in most newborns, but because of the potential toxicity of bilirubin, newborns must be monitored to identify those who may develop severe hyperbilirubinemia and, in rare cases, acute bilirubin encephalopathy or kernicterus. Based on expert consensus and a review of available evidence, a universal pre-discharge bilirubin screening is recommended. This can be achieved by measuring total serum bilirubin (ideally during routine metabolic screening) or transcutaneous bilirubin and plotting the result on an hourly nomogram to determine the risk of subsequent hyperbilirubinemia requiring treatment. If the child is discharged before 24 hours of postnatal age, bilirubin should be rechecked within 48 hours. These guidelines provide a framework for the prevention and treatment of hyperbilirubinemia in neonates aged 35 weeks or more of pregnancy. Kernicterus is discussed in detail in the book Jaundice of the Newborn: Part II.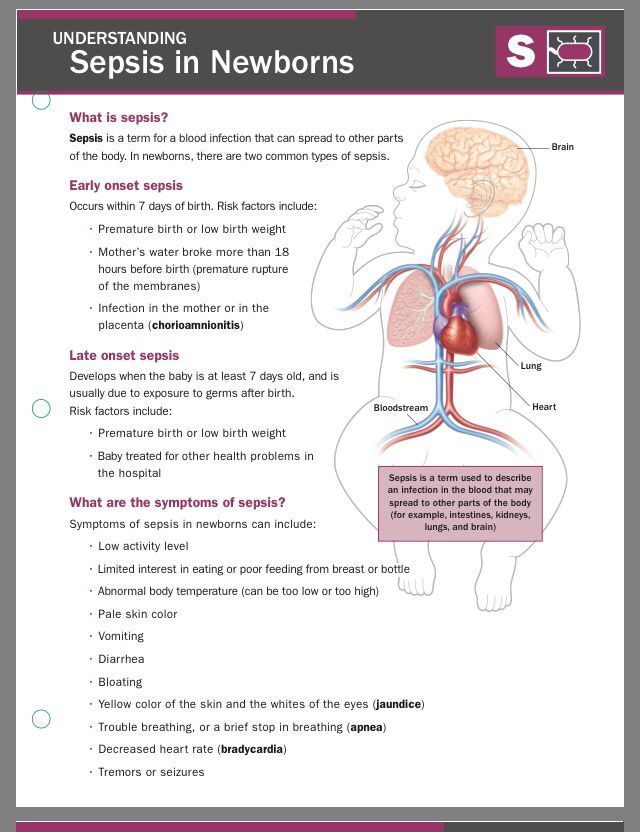 The Women's Health and Education Center (WHEC) recommends that every child: 1) encourage and support successful breastfeeding; 2) Perform a systematic pre-discharge assessment for risk of severe bilirubinemia; 3) Provide early and targeted follow-up based on risk assessment; and when indicated 4) Treat neonates with phototherapy or exchange transfusion to prevent the development of severe hyperbilirubinemia and possibly bilirubin encephalopathy (kernicterus). nine0016
The Women's Health and Education Center (WHEC) recommends that every child: 1) encourage and support successful breastfeeding; 2) Perform a systematic pre-discharge assessment for risk of severe bilirubinemia; 3) Provide early and targeted follow-up based on risk assessment; and when indicated 4) Treat neonates with phototherapy or exchange transfusion to prevent the development of severe hyperbilirubinemia and possibly bilirubin encephalopathy (kernicterus). nine0016 - Neonatal jaundice: part II
The term kernicterus literally means yellow poison, with the nucleus indicating the most commonly affected area of the brain (ie, the nuclear area). Historically, the term refers to an anatomical diagnosis made at autopsy based on the characteristic staining pattern found in children who were noted to have hyperbilirubinemia prior to their death. This document discusses the overview, clinical management, and treatment of kernicterus. Despite the lack of a clear causal relationship between jaundice and the degree of hyperbilirubinemia. Laboratory studies have shown that bilirubin is neurotoxic at the cellular level. Prevention of hyperbilirubinemia is the best way to minimize the incidence of kernicterus. However, because some infants develop kernicterus with relatively modest bilirubin levels, there is no known absolute bilirubin level below which an infant is completely safe. In addition, since other factors contribute to the ability of bilirubin to cross the blood-brain barrier, proper consideration must be given to the management of these components. Any child at risk for significant hyperbilirubinemia and possible neurotoxicity should be cared for in a nursery capable of providing adequate care for hyperbilirubinemia and any associated diagnoses. Developmental potential can be maximized by early detection and intervention of neurological deficits. nine0016
Laboratory studies have shown that bilirubin is neurotoxic at the cellular level. Prevention of hyperbilirubinemia is the best way to minimize the incidence of kernicterus. However, because some infants develop kernicterus with relatively modest bilirubin levels, there is no known absolute bilirubin level below which an infant is completely safe. In addition, since other factors contribute to the ability of bilirubin to cross the blood-brain barrier, proper consideration must be given to the management of these components. Any child at risk for significant hyperbilirubinemia and possible neurotoxicity should be cared for in a nursery capable of providing adequate care for hyperbilirubinemia and any associated diagnoses. Developmental potential can be maximized by early detection and intervention of neurological deficits. nine0016 - Newborn male circumcision
Newborn male circumcision is a surgical procedure that removes the foreskin, the skin that covers the tip of the penis. In the United States, a large percentage of male newborns are circumcised.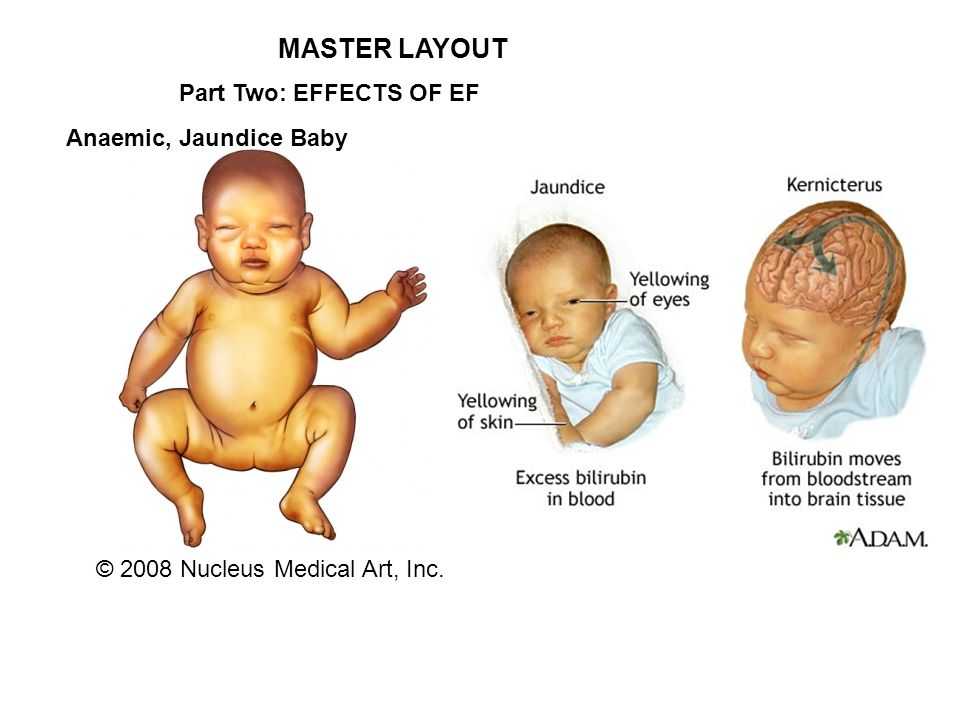 While circumcision has known medical benefits, the procedure is usually performed for family, religious, or cultural reasons. Existing scientific evidence suggests potential medical benefits of newborn male circumcision. However, these data are insufficient to recommend routine neonatal circumcision. Circumcision is a safe and simple procedure, but it comes with risks and potential complications. In the United States, this is often done before the new baby leaves the hospital. Possible benefits include a lower risk of urinary tract infections, penile cancer, and sexually transmitted diseases. There is a low risk of bleeding or infection. The child may also feel some pain. The Women's Health and Education Center (WHEC) recommends that parents discuss circumcision with their child's primary care physician. The World Health Organization (WHO) program on male circumcision and HIV prevention is also being discussed. Parents should make a decision based on the benefits and risks, as well as their own religious, cultural and personal preferences.
While circumcision has known medical benefits, the procedure is usually performed for family, religious, or cultural reasons. Existing scientific evidence suggests potential medical benefits of newborn male circumcision. However, these data are insufficient to recommend routine neonatal circumcision. Circumcision is a safe and simple procedure, but it comes with risks and potential complications. In the United States, this is often done before the new baby leaves the hospital. Possible benefits include a lower risk of urinary tract infections, penile cancer, and sexually transmitted diseases. There is a low risk of bleeding or infection. The child may also feel some pain. The Women's Health and Education Center (WHEC) recommends that parents discuss circumcision with their child's primary care physician. The World Health Organization (WHO) program on male circumcision and HIV prevention is also being discussed. Parents should make a decision based on the benefits and risks, as well as their own religious, cultural and personal preferences.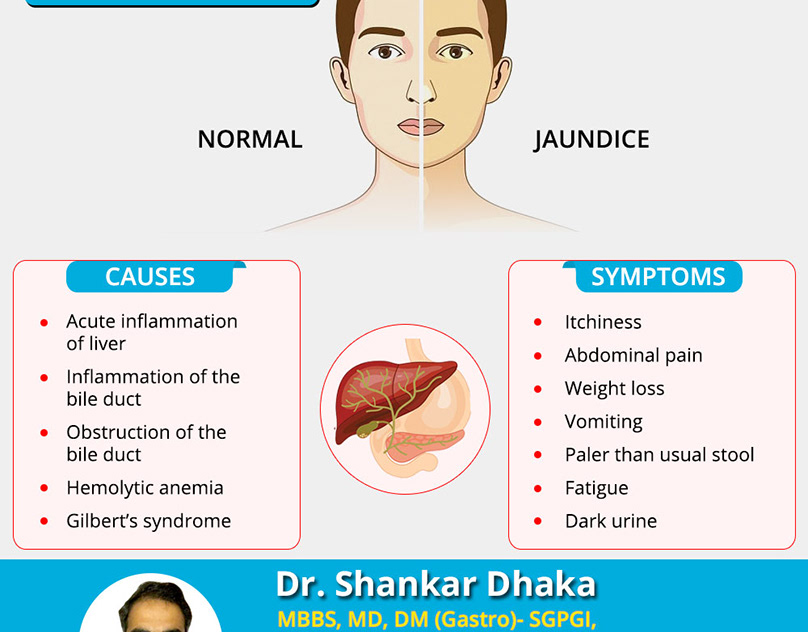 As with most surgeries, the best results are achieved by practitioners who are well trained, perform the procedure under supervision until their experience is sufficient, and follow the correct protocol throughout the entire operation. nine0016
As with most surgeries, the best results are achieved by practitioners who are well trained, perform the procedure under supervision until their experience is sufficient, and follow the correct protocol throughout the entire operation. nine0016 - Newborn nutrition
The breastfeeding landscape has changed over the past few decades as more women begin breastfeeding in the postpartum period and hospitals are designated as baby-friendly hospitals following the evidence-based Ten Steps to Successful Breastfeeding. Breast milk feeding supports optimal growth and development of the newborn while reducing the risk of acute and chronic diseases. The use of donor breast milk is increasing for high-risk infants, mainly for infants born weighing less than 1500 g or those with severe intestinal disorders. Pasteurized donor milk may be considered in situations where the supply of mother's milk is insufficient. Intramuscular vitamin K1 (phytonadione) at a dose of 0.5 to 1.0 mg should be given regularly to all newborns on the first day to reduce the risk of hemorrhagic disease of the newborn. Vitamin D deficiency/insufficiency and rickets increased in all infants due to decreased exposure to sunlight secondary to changes in lifestyle, dressing habits, and use of topical sunscreen preparations. Supplemental fluoride should not be given for the first 6 months. From 6 months to 3 years of age, fluoride supplementation should be limited to infants living in communities where the concentration of fluoride in the water is
Vitamin D deficiency/insufficiency and rickets increased in all infants due to decreased exposure to sunlight secondary to changes in lifestyle, dressing habits, and use of topical sunscreen preparations. Supplemental fluoride should not be given for the first 6 months. From 6 months to 3 years of age, fluoride supplementation should be limited to infants living in communities where the concentration of fluoride in the water is - US Newborn Screening Program
Newborn screening is the largest screening program in the United States, with approximately four million newborns performed each year. This is an approved public health program designed to identify disorders in children. It aims to provide rapid diagnosis and enable early therapy for specific metabolic, infectious, and other genetic disorders for which early intervention reduces disability and death. This important practice usually occurs before the development of signs or symptoms of the disease. Newborn screening programs consist of a comprehensive integrated clinical service of education, screening, diagnosis, monitoring, evaluation, and often long-term management.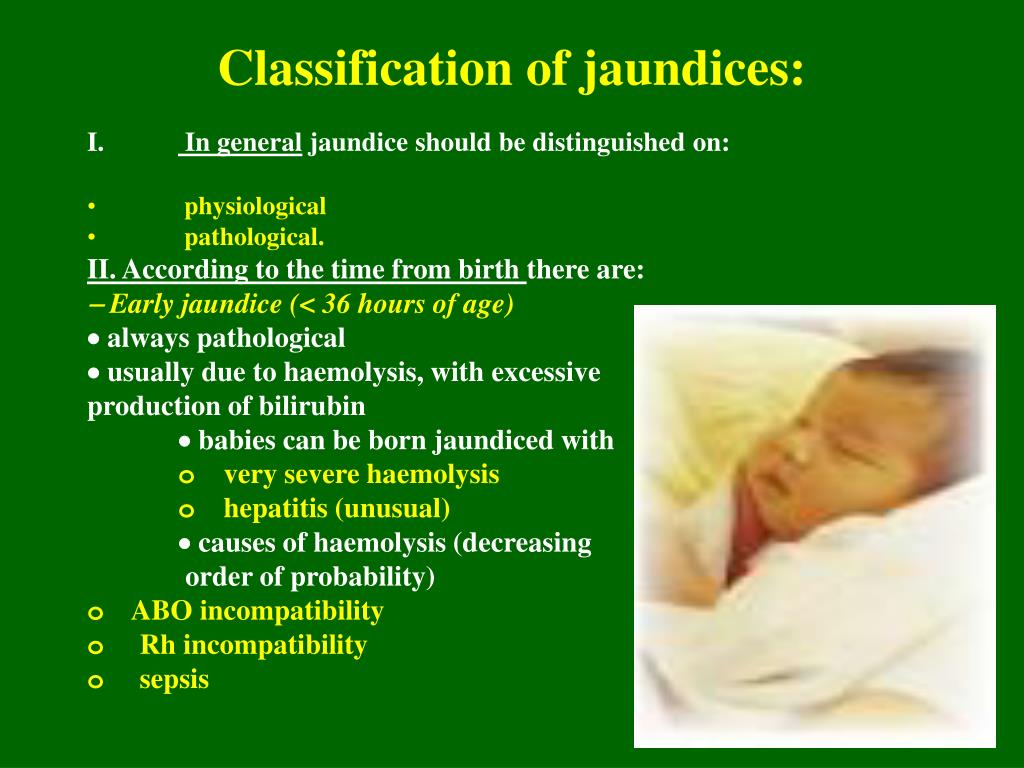 The list of recommended conditions for newborn screening programs is constantly being evaluated. Integrating education about newborn screening into prenatal care allows parents to be prepared for their child to be screened and to receive newborn screening results. In addition, parents often view their transition from prenatal management through pediatrics as continuous care with no difference in medical services. This can be achieved at various points in antenatal care: 1) during a new first trimester birth and include written or web-based information along with other patient education materials; 2) later in pregnancy with other educational information regularly shared, such as during streptococcal glucose or group B screening in the third trimester, 3) during discussions of past adverse pregnancy outcomes associated with a positive newborn screening test or birth defect, in the same time as options for prenatal or preimplantation genetic screening or diagnostic testing. nine0016
The list of recommended conditions for newborn screening programs is constantly being evaluated. Integrating education about newborn screening into prenatal care allows parents to be prepared for their child to be screened and to receive newborn screening results. In addition, parents often view their transition from prenatal management through pediatrics as continuous care with no difference in medical services. This can be achieved at various points in antenatal care: 1) during a new first trimester birth and include written or web-based information along with other patient education materials; 2) later in pregnancy with other educational information regularly shared, such as during streptococcal glucose or group B screening in the third trimester, 3) during discussions of past adverse pregnancy outcomes associated with a positive newborn screening test or birth defect, in the same time as options for prenatal or preimplantation genetic screening or diagnostic testing. nine0016 - Apgar score
The purpose of this document is to put the Apgar score in its proper perspective. The Apgar score describes the condition of a newborn infant immediately after birth and, when used correctly, is a standardized assessment tool. It also provides a mechanism for recording the transition from fetus to newborn. Apgar scores do not predict individual mortality or adverse neurological outcome. However, based on population studies, Apgar scores less than 5 at the 5-minute and 10-minute readings clearly indicate an increased relative risk of cerebral palsy, and the degree of anomaly correlates with the risk of cerebral palsy. However, most infants with a low Apgar score will not develop cerebral palsy. The Apgar score depends on many factors, including gestational age, maternal medications, resuscitation, cardiorespiratory and neurological conditions. If the Apgar score at 5 minutes is 7 or more, peripartum hypoxia-ischemia is unlikely to cause neonatal encephalopathy. Recommendations for the neonatal resuscitation program (NRP), Apgar score, and subsequent neurological dysfunctions are also discussed.
The Apgar score describes the condition of a newborn infant immediately after birth and, when used correctly, is a standardized assessment tool. It also provides a mechanism for recording the transition from fetus to newborn. Apgar scores do not predict individual mortality or adverse neurological outcome. However, based on population studies, Apgar scores less than 5 at the 5-minute and 10-minute readings clearly indicate an increased relative risk of cerebral palsy, and the degree of anomaly correlates with the risk of cerebral palsy. However, most infants with a low Apgar score will not develop cerebral palsy. The Apgar score depends on many factors, including gestational age, maternal medications, resuscitation, cardiorespiratory and neurological conditions. If the Apgar score at 5 minutes is 7 or more, peripartum hypoxia-ischemia is unlikely to cause neonatal encephalopathy. Recommendations for the neonatal resuscitation program (NRP), Apgar score, and subsequent neurological dysfunctions are also discussed. The review also looks at the occurrence of a 5-minute Apgar score of 0 and seizures or severe neurological dysfunction. Perinatal asphyxia is the main cause of neurological complications in newborns. The Apgar score is useful in conveying information about the general status of the newborn and response to resuscitation. However, if necessary, resuscitation should be initiated prior to the 1-minute score. Therefore, the Apgar score is not used to determine if the necessary resuscitation steps are necessary or when to use them. nine0016
The review also looks at the occurrence of a 5-minute Apgar score of 0 and seizures or severe neurological dysfunction. Perinatal asphyxia is the main cause of neurological complications in newborns. The Apgar score is useful in conveying information about the general status of the newborn and response to resuscitation. However, if necessary, resuscitation should be initiated prior to the 1-minute score. Therefore, the Apgar score is not used to determine if the necessary resuscitation steps are necessary or when to use them. nine0016 - Neonatal care: initial assessment and resuscitation
Approximately 10% of term patients and preterm infants require some assistance to start breathing, which includes stimulation at birth; less than 1% will require extensive resuscitation. Although the vast majority do not require intervention to transition from intrauterine to extrauterine life, due to the high total number of births, a significant number of infants will require some degree of resuscitation.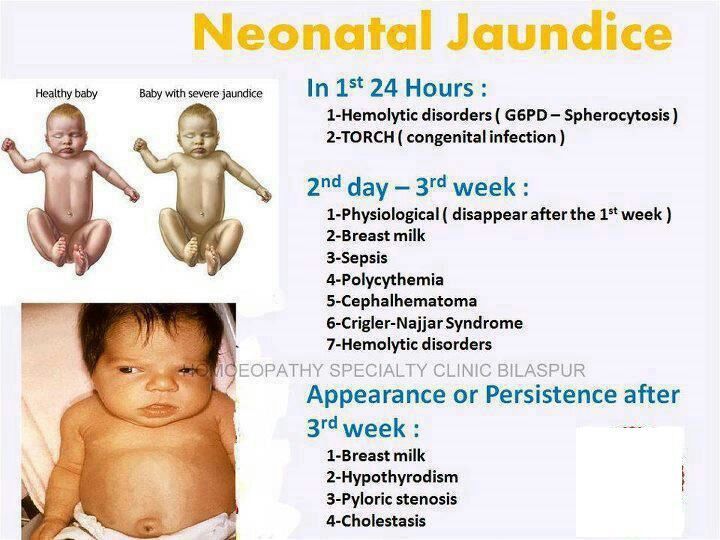 Recognition and immediate resuscitation of a problem newborn infant requires an organized plan of action that includes the immediate availability of appropriate equipment and qualified personnel on site. Expected problems with the newborn should be communicated in detail by the obstetric care provider to the responsible leader of the resuscitation team. Evaluation and resuscitation of the infant at birth should be provided in accordance with the principles of the guidelines for resuscitation of newborns. Most of the principles apply during the neonatal period and early infancy. Each hospital should have a policy and procedures for neonatal care and resuscitation, including the qualifications of doctors and other medical practitioners who provide this care. The Women's Health and Education Center (WHEC), with its partners, launched the Newborn Care series to disseminate updated literature and guidance to health care providers regarding the care and safety of newborns. Current recommendations are summarized in this section.
Recognition and immediate resuscitation of a problem newborn infant requires an organized plan of action that includes the immediate availability of appropriate equipment and qualified personnel on site. Expected problems with the newborn should be communicated in detail by the obstetric care provider to the responsible leader of the resuscitation team. Evaluation and resuscitation of the infant at birth should be provided in accordance with the principles of the guidelines for resuscitation of newborns. Most of the principles apply during the neonatal period and early infancy. Each hospital should have a policy and procedures for neonatal care and resuscitation, including the qualifications of doctors and other medical practitioners who provide this care. The Women's Health and Education Center (WHEC), with its partners, launched the Newborn Care series to disseminate updated literature and guidance to health care providers regarding the care and safety of newborns. Current recommendations are summarized in this section.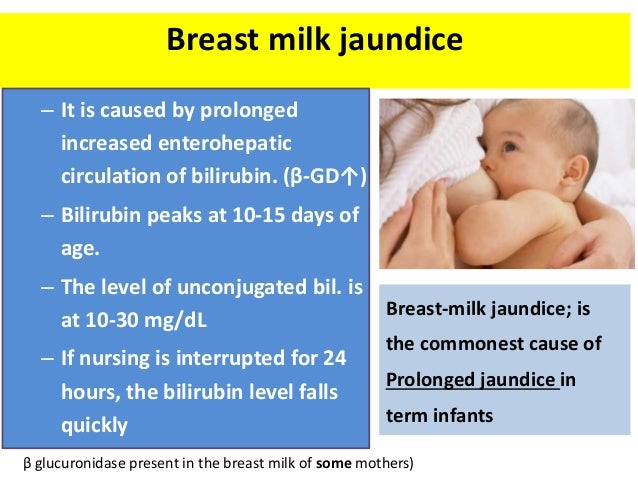
Meconium is the original feces, it is formed in the intestines of the baby from the digested amniotic fluid that the baby swallows in the womb. The exit of meconium is evidence that the baby's digestive system has started and begins to work normally. In order for meconium to come out faster, it is necessary to put the newborn to the breast from the very moment of birth. Even drops of colostrum will have a beneficial effect on the child's immunity and start intestinal motility, after which meconium will come out.
Early attachment to the breast also keeps the baby from starving. In the first days of life, there is no need to feed the child. Even if the mother has little milk, the baby should be applied to the breast more often. So the baby will feed on the mother's milk drop by drop, and the breast will switch to the mode of normal milk production. nine0003
Hypothermia is another possible cause of intense jaundice. But nowadays babies are more often dressed too warm than left undressed. So you can’t leave your child naked in the fresh air for a long time, but there’s no need to wrap him in a blanket either. A good rule of thumb is that the baby should have one more layer of clothing than the mother. If the mother is wearing a summer sundress, a baby's undershirt and sliders, a light envelope or a blanket are enough for the child.
So you can’t leave your child naked in the fresh air for a long time, but there’s no need to wrap him in a blanket either. A good rule of thumb is that the baby should have one more layer of clothing than the mother. If the mother is wearing a summer sundress, a baby's undershirt and sliders, a light envelope or a blanket are enough for the child.
Pathological neonatal jaundice
Fewer than 1% of children have abnormal neonatal jaundice. Here are the reasons why it develops most often:
To distinguish between normal and pathological neonatal jaundice, the baby is closely monitored for the first two or three days. With prolonged intense jaundice, negative consequences for the central nervous system are possible. Therefore, the infant may be given phototherapy. When the sun's rays fall on the baby's body, bilirubin breaks down into components that are excreted from the body much faster. nine0003
With prolonged intense jaundice, negative consequences for the central nervous system are possible. Therefore, the infant may be given phototherapy. When the sun's rays fall on the baby's body, bilirubin breaks down into components that are excreted from the body much faster. nine0003
The simplest phototherapy is sunbathing. The baby is undressed and laid out for 10-15 hours in the open sun, in extreme cases - on the windowsill. Important: the baby should not freeze, this will only increase the jaundice. If it is not hot in the maternity hospital, it is better not to undress the child completely, to expose only the arms and legs. And of course, you can not place a baby under the scorching rays of the sun in the summer, especially in the south. It is better to spend sunbathing in the morning and in the evening.
Modern maternity hospitals often offer sunbathing with photolamps. In these special devices, the wavelength of light is chosen so as to break down bilirubin as much as possible into safe components.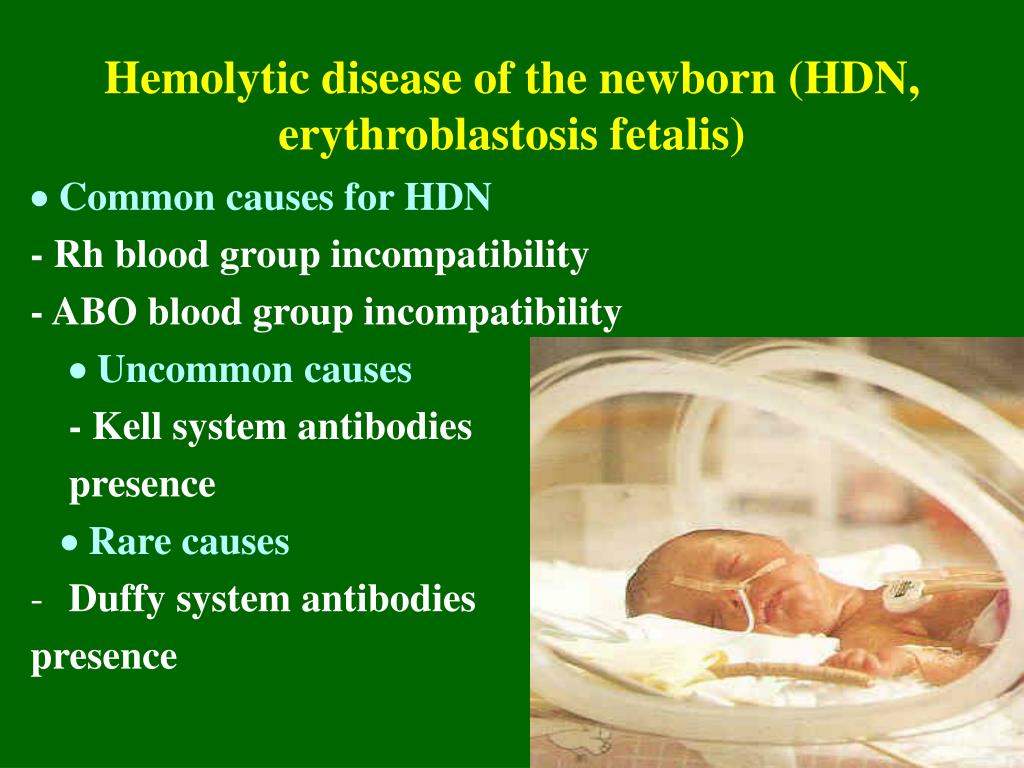 When combined with breastfeeding, phototherapy can be quite effective. But in the most severe cases, infusion therapy and blood transfusion may be needed. nine0003
When combined with breastfeeding, phototherapy can be quite effective. But in the most severe cases, infusion therapy and blood transfusion may be needed. nine0003