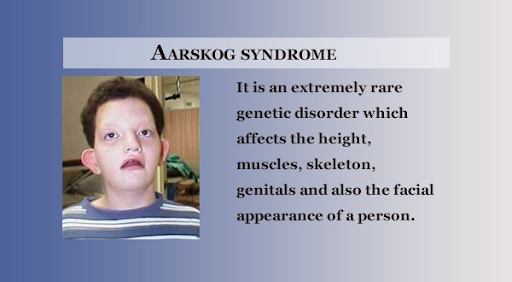
Treatment for baby with conjunctivitis
Pink Eye (Conjunctivitis) in Newborns
Newborns with symptoms of conjunctivitis (pink eye) should see a doctor right away.
Neonatal conjunctivitis is a red eye in a newborn caused by infection, irritation, or a blocked tear duct. When caused by an infection, neonatal conjunctivitis can be very serious.
Symptoms and Causes of Conjunctivitis in Newborns
Newborns with conjunctivitis develop drainage from the eyes within a few days to several weeks after birth. Their eyelids become puffy, red, and tender. The cause of neonatal conjunctivitis is often difficult to determine because, in many instances, the symptoms don’t vary by cause.
Conjunctivitis in a newborn may be caused by a blocked tear duct, irritation produced by the topical antimicrobials given at birth, or infection with a virus or bacterium passed from the mother to her baby during childbirth. Even mothers without symptoms (asymptomatic) at the time of delivery can carry and pass bacteria or viruses to babies during birth.
The most common types of neonatal conjunctivitis include the following:
- Inclusion (chlamydial) conjunctivitis
Chlamydia trachomatis can cause inclusion conjunctivitis and genital infections (chlamydia). A woman with untreated chlamydia can pass the bacteria to her baby during childbirth. Symptoms of inclusion conjunctivitis include redness of the eye(s), swelling of the eyelids, and discharge of pus. Symptoms are likely to appear 5 to 12 days after birth. Symptoms can develop earlier if the amniotic sac is ruptured during delivery. Some newborns with chlamydial conjunctivitis can have the infection in other parts of their bodies. The bacteria can infect the lungs and nasopharynx (where the back of the nose connects to the mouth). - Gonococcal conjunctivitis
Neisseria gonorrhoeae can cause gonococcal conjunctivitis, as well as the sexually transmitted infection called gonorrhea. A woman with untreated gonorrhea can pass the bacteria to her baby during childbirth.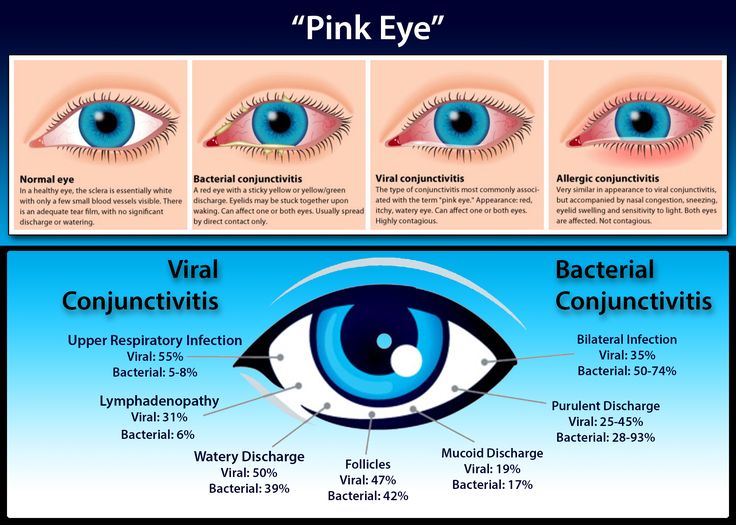 Symptoms usually include red eyes, thick pus in the eyes, and swelling of the eyelids. This type of conjunctivitis usually begins in the first 2-5 days of life. It can also progress to serious infections of the bloodstream (bacteremia) and lining of the brain and spinal cord (meningitis) in newborns.
Symptoms usually include red eyes, thick pus in the eyes, and swelling of the eyelids. This type of conjunctivitis usually begins in the first 2-5 days of life. It can also progress to serious infections of the bloodstream (bacteremia) and lining of the brain and spinal cord (meningitis) in newborns. - Chemical conjunctivitis
When eye drops are given to newborns to help prevent a bacterial infection, the newborn’s eye(s) may become irritated. This may be diagnosed as chemical conjunctivitis. Symptoms of chemical conjunctivitis usually include mildly red eye(s) and some swelling of the eyelids. Symptoms are likely to last for only 24 to 36 hours. - Other neonatal conjunctivitis
Viruses and bacteria other than Chlamydia trachomatis and Neisseria gonorrhoeae can cause conjunctivitis. For example, bacteria that normally live in a woman’s vagina and are not sexually transmitted can cause conjunctivitis. Additionally, the viruses that cause genital and oral herpes can cause neonatal conjunctivitis and severe eye damage.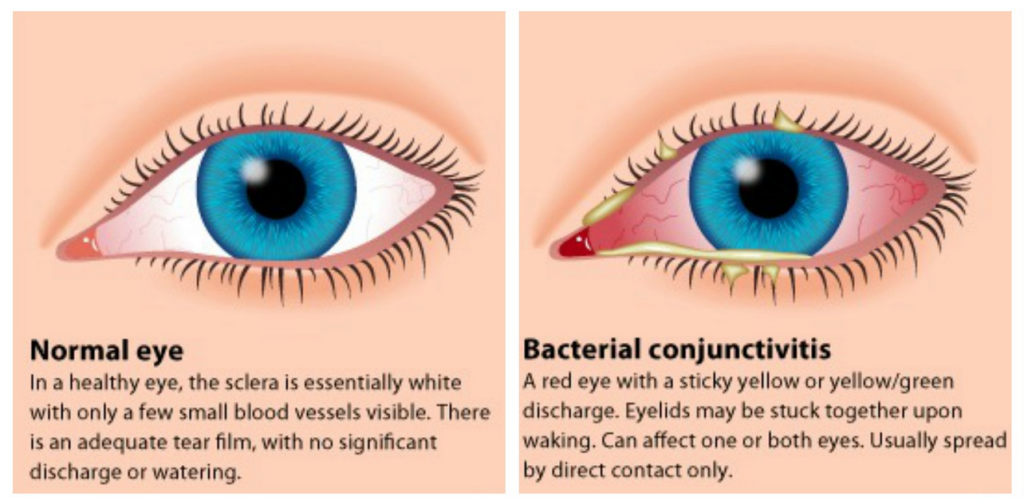 The mother may pass such viruses to her baby during childbirth. However, herpes conjunctivitis is less common than conjunctivitis caused by gonorrhea and chlamydia. Symptoms usually include red eye(s) and swollen eyelids with some pus.
The mother may pass such viruses to her baby during childbirth. However, herpes conjunctivitis is less common than conjunctivitis caused by gonorrhea and chlamydia. Symptoms usually include red eye(s) and swollen eyelids with some pus.
Prevention and Treatment of Conjunctivitis in Newborns
To prevent neonatal conjunctivitis, most states have laws requiring providers to put drops or ointment in a newborn’s eyes, typically within 2-3 hours of birth. In the past, hospitals used silver nitrate; now hospitals mostly use antibiotic eye drops, typically erythromycin. During pregnancy and prior to giving birth, women with genital herpes should consult with their physician about ways to minimize the chances of spread to their newborn baby.
Doctors may treat neonatal conjunctivitis caused by a bacterial infection with antibiotics. It will depend on the severity of the infection and the bacteria that caused it. Some antibiotics are applied as an eye drop or ointment in the eye (topical).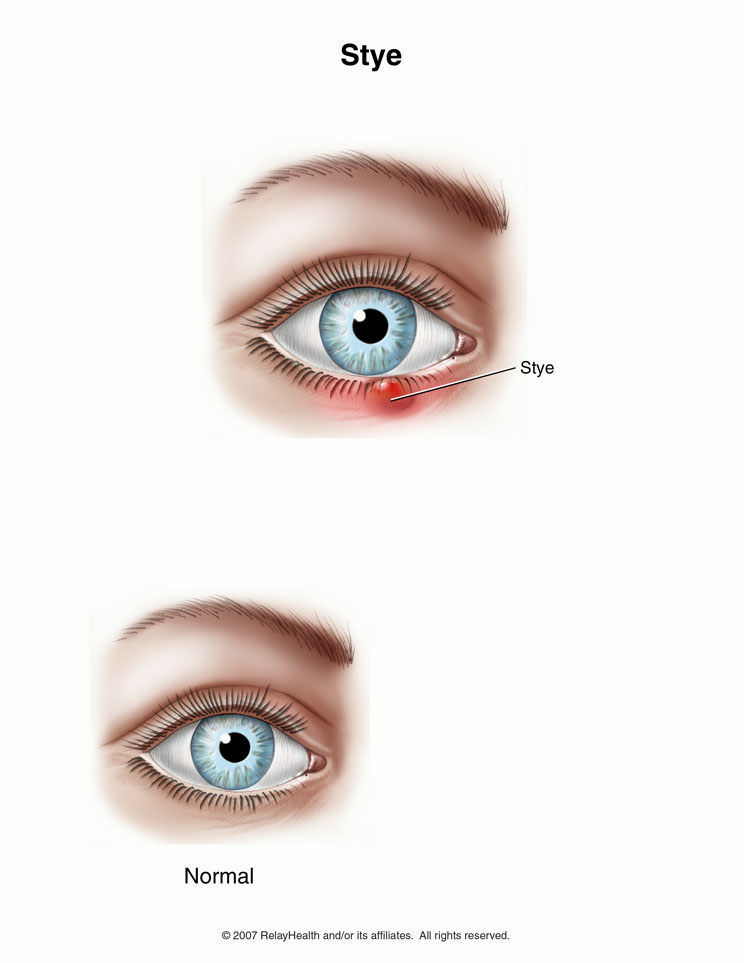 Other antibiotics are given by mouth (orally), through a vein (intravenous), or as a shot (intramuscular). Doctors may treat a newborn’s conjunctivitis with a combination of topical, and either oral, intravenous, or intramuscular antibiotics. Rinsing the newborn’s infected eye with a saline solution will remove any debris that may develop in response to the infection.
Other antibiotics are given by mouth (orally), through a vein (intravenous), or as a shot (intramuscular). Doctors may treat a newborn’s conjunctivitis with a combination of topical, and either oral, intravenous, or intramuscular antibiotics. Rinsing the newborn’s infected eye with a saline solution will remove any debris that may develop in response to the infection.
If a blocked tear duct causes conjunctivitis, a gentle, warm massage between the eye and nasal area may help. If the blocked tear duct does not clear by 1 year of age, the newborn may require surgery.
Treatments for the common causes of neonatal conjunctivitis are as follows:
- Inclusion (chlamydial) conjunctivitis
Doctors usually use oral antibiotics to treat inclusion conjunctivitis. - Gonococcal conjunctivitis
Doctors give intravenous (IV) or intramuscular (IM) antibiotics to treat gonococcal conjunctivitis. If untreated, the newborn could develop corneal ulcerations (open sores in the cornea) and blindness.
- Chemical conjunctivitis
Since this type of conjunctivitis is caused by chemical irritation, treatment is usually not required. The newborn will usually get better in 24 to 36 hours. - Other bacterial and viral conjunctivitis
Doctors usually give antibiotic drops or ointments to treat conjunctivitis caused by other bacteria For both bacterial and viral conjunctivitis, a warm compress to the eye may relieve swelling and irritation. Be sure to wash hands before and after touching the infected eyes.
Pinkeye (Conjunctivitis) (for Parents) - Nemours KidsHealth
What Is Pinkeye?
The eye infection conjunctivitis (kun-junk-tih-VY-tus) — often called pinkeye — is common in young kids. It's usually contagious, and breakouts can sweep through preschools and playgrounds. But even teens and adults can get pinkeye.
Pinkeye is an inflammation of the conjunctiva, the white part of the eye and the inner eyelids.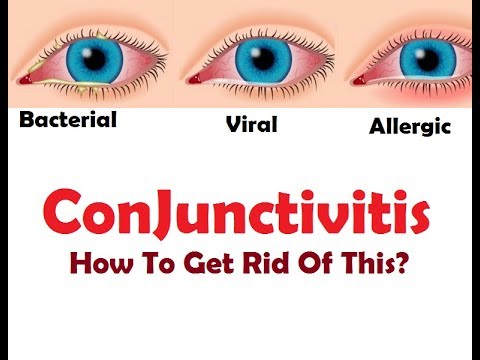 It's a minor infection and although it might look bad, usually isn't serious.
It's a minor infection and although it might look bad, usually isn't serious.
Still, if your child shows signs of pinkeye, it's important to see a doctor. Some kinds of pinkeye go away on their own, but others need treatment.
What Causes Pinkeye?
Infectious pinkeye (the kind that can spread to others) can be caused by many of the bacteria and viruses responsible for colds and other infections — including ear infections, sinus infections, and sore throats. Sometimes it's caused by the same types of bacteria that cause chlamydia and gonorrhea, two sexually transmitted diseases (STDs).
Some kinds of pinkeye are noninfectious, such as:
- allergic conjunctivitis, which happens more often in kids with other allergic conditions, like hay fever. Triggers include grass, ragweed pollen, animal dander, and dust mites.
- irritant conjunctivitis, caused by anything that irritates the eyes, such as air pollution or chlorine in pools
Pinkeye in Newborns
Newborns are at risk for pinkeye and can develop serious health problems if it's not treated. If a pregnant woman has an STD, during delivery the bacteria or virus can pass from the birth canal into the baby's eyes, causing pinkeye. To prevent this, doctors give antibiotic ointment or eye drops to all babies right after birth. Occasionally, this treatment causes a mild chemical conjunctivitis, which usually clears up on its own. Doctors also can screen pregnant women for STDs and treat them during pregnancy to prevent spreading the infection to the baby.
If a pregnant woman has an STD, during delivery the bacteria or virus can pass from the birth canal into the baby's eyes, causing pinkeye. To prevent this, doctors give antibiotic ointment or eye drops to all babies right after birth. Occasionally, this treatment causes a mild chemical conjunctivitis, which usually clears up on its own. Doctors also can screen pregnant women for STDs and treat them during pregnancy to prevent spreading the infection to the baby.
What Are the Signs & Symptoms of Pinkeye?
Besides the telltale red or pink color that gives pinkeye its name, eye discomfort is a common symptom. Kids might say that it feels like there's sand in the eye. Often, there's some discharge from the eye, and pain and swelling of the conjunctiva. Some kids have swollen eyelids or sensitivity to bright light. Pinkeye can affect one or both eyes.
In cases of allergic conjunctivitis, itchiness and watery eyes are common symptoms.
Is Pinkeye Contagious?
Pinkeye is contagious if it's caused by bacteria or a virus:
- Pinkeye that's caused by bacteria can spread to others as soon as symptoms appear and for as long as there's discharge from the eye — or until 24 hours after antibiotics are started.

- Pinkeye that's caused by a virus is generally contagious before symptoms appear and can remain so as long as the symptoms last.
Allergic conjunctivitis and irritant conjunctivitis are not contagious.
A child can get pinkeye by touching an infected person or something an infected person has touched, such as a used tissue. In the summertime, pinkeye can spread when kids swim in contaminated water or share contaminated towels. It also can spread through coughing and sneezing.
Also, someone who has pinkeye in one eye can spread it to the other eye by rubbing or touching the infected eye, then touching the other eye.
How Is Pinkeye Diagnosed?
If you think your child has pinkeye, it's important to see your health care provider to learn what's causing it and how to treat it. Other serious eye conditions can have similar symptoms, so a child who complains of severe pain, changes in eyesight, swelling around the eyes, or sensitivity to light should be examined.
If you can't get an in-person visit, you might be able to do a "video visit" instead. Telehealth — when patients and health care providers use technology for the remote diagnosis and treatment of some health conditions — is becoming more and more popular. Ask your health care provider if his or her practice participates in telemedicine, and check with your insurance provider to see if this option is covered.
How Is Pinkeye Treated?
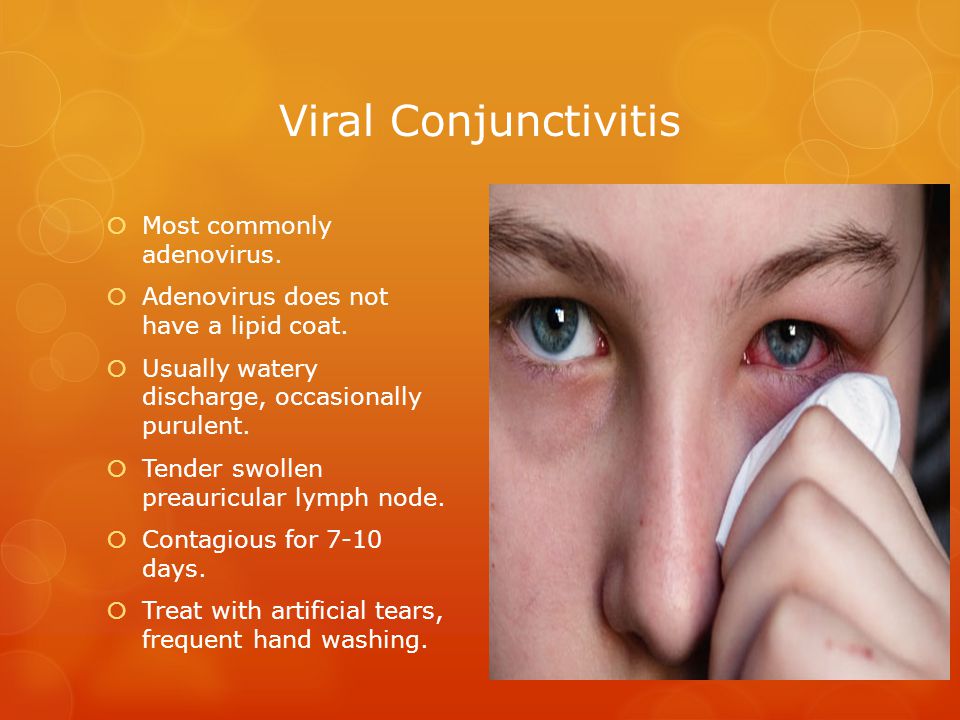
Pinkeye caused by a virus usually goes away without any treatment. Pinkeye caused by bacteria is treated with antibiotic eye drops or ointment.
It can be hard to get kids to tolerate eye drops several times a day. If you're having trouble, put the drops on the inner corner of your child's closed eye — when your child opens the eye, the medicine will flow into it. If you still have trouble with drops, ask the doctor about antibiotic ointment, which can be placed in a thin layer where the eyelids meet, and will melt and enter the eye.
If your child has allergic conjunctivitis, your doctor may prescribe anti-allergy medicine, either as pills, liquid, or eye drops.
You also can give acetaminophen or ibuprofen to relieve discomfort (check instructions for correct amount).
How Can Parents Help?
Using cool or warm compresses on the eyes may make your child more comfortable. Clean the edges of the infected eye carefully with warm water and gauze or cotton balls. This can also remove the crusts of dried discharge that make the eyelids stick together in the morning.
If your child wears contact lenses, your doctor or eye doctor may recommend that the lenses not be worn until the infection is gone. Then, disinfect the lenses and their storage case at least twice before letting your child wear them again. If your child wears disposable contact lenses, throw away the current pair and use a new pair after the infection is gone.
Doctors usually recommend keeping kids with contagious conjunctivitis out of school, childcare, or summer camp for a short time.
Can Pinkeye Be Prevented?
Infectious conjunctivitis is highly contagious, so teach kids to wash their hands well and often with warm water and soap. They also should not share eye drops, tissues, eye makeup, washcloths, towels, or pillowcases.
Be sure to wash your own hands well after touching an infected child's eyes, and throw away items like gauze or cotton balls after they've been used. Wash towels and other linens that the child has used in hot water separately from the rest of the family's laundry to avoid contamination.
If you know your child is prone to allergic conjunctivitis, keep windows and doors closed on days when the pollen is heavy, and dust and vacuum often to limit allergy triggers. Irritant conjunctivitis can only be prevented by avoiding the irritating causes.
Screening and treating pregnant women for STDs can prevent many cases of pinkeye in newborns. A pregnant woman may have bacteria in her birth canal even if she shows no symptoms, which is why prenatal screening is important.
When Should I Call the Doctor?
If the pinkeye does not improve after 2 to 3 days of treatment, or after a week if untreated, call your doctor.
If your child has increased swelling, redness, and tenderness in the eyelids and around the eye, along with a fever, call your doctor. Those symptoms may mean the infection has started to spread beyond the conjunctiva and will need more treatment.
Reviewed by: Rachel S. Schare, MD
Date reviewed: November 2020
Conjunctivitis in children - treatment, symptoms of viral conjunctivitis
Our doctors
Gracheva
Larisa
Alekseevna Anesthesiologist-resuscitator of the highest category, candidate of medical sciences. More about the doctor All doctors of the clinic
Ask a question to the doctors of the clinic
Reviews of patients
Maria
Thank you has no boundaries! I did laser correction and I want to say thank you to all the hospital staff for their qualified help, top-level service, thank you for giving me the opportunity to see the world with my own eyes, without glasses and lenses, it's just an inexpressible feeling, gratitude has no boundaries, to everyone I recommend your clinic, where such wonderful people work, thanks again to everyone!!! nine0003
All reviews
- Home
- For patients
- Useful materials
- Conjunctivitis
Conjunctivitis is an inflammation of the mucous membrane lining the inner surface of the eyelid and the eyeball. When it becomes inflamed, the blood vessels enlarge, the eye becomes red, and the eyelids swell. The child complains of pain in the eyes, pain, itching.
When it becomes inflamed, the blood vessels enlarge, the eye becomes red, and the eyelids swell. The child complains of pain in the eyes, pain, itching.
Causes of conjunctivitis
Pathology is often found in children who are alien to the rules of hygiene. Toddlers often rub their eyes with dirty hands, causing an infection. The causes of the disease can be different, these are:
- viruses;
- bacteria, most often staphylococci and streptococci - purulent discharge from the eyes is characteristic of such an infection;
- allergens;
- other irritants, eg pool reagent.
Bacterial and viral conjunctivitis in children are contagious and can spread to other family members if proper hygiene is not followed.
It is difficult to determine the cause of the disease on your own, therefore, at the first manifestations of the inflammatory process, the child should be shown to an ophthalmologist. The clinic for laser eye microsurgery at Maerczak employs oculists who specialize in the treatment of childhood eye diseases. nine0003
nine0003
Treatment of conjunctivitis in children
Inflammation goes away quickly if the right medicines are chosen. The doctor determines how to treat conjunctivitis in a child, based on the cause of the disease and the condition of the baby.
- In case of bacterial conjunctivitis, antibiotics are prescribed in the form of drops, ointments, less often tablets. Even if the symptoms disappear in the first days, it is important to take the medication for as long as the doctor has prescribed without changing the dosage. Otherwise, there is a risk of developing resistance to antibiotics: bacteria will become immune to this drug. nine0020
- If the inflammation is caused by a virus, ophthalmologists advise constantly rinsing the child's eyes and removing dry discharge. Warm compresses can help relieve symptoms. Make sure that the child does not touch sore eyes - this increases irritation and spreads the disease.
- To relieve the symptoms of allergic conjunctivitis, you need to limit contact with the allergen.
 Antihistamines reduce inflammation.
Antihistamines reduce inflammation.
If the child wears lenses, it is worth abandoning them for the duration of treatment and switching to glasses. nine0003
Bacterial conjunctivitis in a child - treatment, causes, symptoms
Conjunctivitis occupies one of the leading positions among the pathologies of the eyeball membrane. The disease is an inflammation of the mucous membrane of the eye with characteristic symptoms: swelling, itching, hyperemia. In severe cases, the pathology is complicated by damage to the cornea and a violation of the visual function of the organ. Doctors are faced in practice with viral, bacterial, allergic and other types of conjunctivitis. nine0003
Bacterial conjunctivitis in children is one of the most dangerous both in terms of the course of pathology and prognosis. The disease is common due to high contagiousness, changes in the composition of the microflora and the addition of a combined infection of viral etiology or fungal conjunctivitis. Especially often recorded inflammation of the conjunctiva in children with weakened immune systems.
Especially often recorded inflammation of the conjunctiva in children with weakened immune systems.
Causes
The direct cause of inflammation is the penetration of the causative agent of bacterial conjunctivitis. Among the pathogenic microflora recently found:
- hemolytic streptococcus;
- gonococcus;
- Pseudomonas aeruginosa;
- Staphylococcus epidermidis;
- E. coli;
- chlamydial infection.
The level of bacterial infections of the mucous membrane of the eyes caused by Staphylococcus aureus remains traditionally high. It is he who is most often found in laboratories when taking an analysis for pathogenic microflora.
The factors in the spread of purulent conjunctivitis in children are different and vary depending on age. The conjunctiva is inhabited by various microflora from birth. It is the balance between immunity and pathogenic microbiota that holds back many pathologies, including inflammatory ones.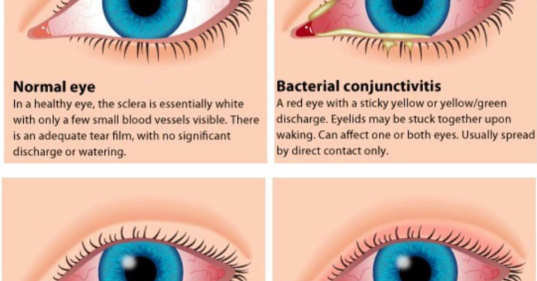 If the balance is disturbed and the number of harmful microorganisms is exceeded, the process of inflammation of the mucous membrane starts. nine0003
If the balance is disturbed and the number of harmful microorganisms is exceeded, the process of inflammation of the mucous membrane starts. nine0003
Newborns are more likely to get the pathogen when passing through the birth canal. Weakened immunity, prematurity and other aggravating factors play an important role. In the first 2-4 days of a child's life, signs of gonococcal conjunctivitis or chlamydial infection are usually recorded.
In infancy, the leading factor in the development of conjunctival inflammation is weak local immunity, stress, hypothermia or overheating. An important indicator is the number of pathogens that have fallen on the mucous membrane. The body copes with a small amount on its own, washing them away with tears, but with a high concentration of pathogenic microflora, infection is practically inevitable. The disease in infants is associated with a herpes infection, and at this age they also suffer from adenovirus and diphtheria conjunctivitis. nine0003
The organs of vision are arranged in such a way that the eye and its appendages provide mechanical protection against the penetration of pathogenic agents. The eye is constantly washed with tears, thereby removing dust, microbes and traces of their vital activity from the surface. While maintaining the integrity of the cells of the mucous membrane, they represent a powerful barrier and protect against microbes in case of bacterial damage. Together, this helps to resist the development of infection.
The eye is constantly washed with tears, thereby removing dust, microbes and traces of their vital activity from the surface. While maintaining the integrity of the cells of the mucous membrane, they represent a powerful barrier and protect against microbes in case of bacterial damage. Together, this helps to resist the development of infection.
Violation of the integrity of the membrane becomes additional risk factors for damage to the conjunctiva:
- anomalies of the eyelids, drying of the mucosa and microcracks;
- obstruction of the lacrimal ducts;
- violation of the precorneal film;
- superficial eye injuries;
- rare blinking, dry eye syndrome.
These conditions increase the risk of infection and bacterial conjunctivitis in a child.
Differences of bacterial conjunctivitis from other types of pathology
Unlike different types of infectious conjunctivitis, the bacterial form has its own characteristic features that help to make a diagnosis. In most cases, the pathology develops rapidly, as in acute infectious diseases. nine0003
In most cases, the pathology develops rapidly, as in acute infectious diseases. nine0003
The difference between bacterial conjunctivitis and other types and in the symptoms of the disease. In children, severe hyperemia is observed, the eyelids swell, the transitional folds of the eyeball swell. Despite this, the cornea remains clear, does not acquire a yellowish tint and does not thicken, as with symptoms of allergic inflammation. A key sign of pathology is the appearance of mucous secretions with a transition to purulent, which causes the eyelids to stick together, crusts appear between the eyelashes.
Incubation period of pathogen
The incubation period of the pathogen ranges from several hours to several days. Latent pathology develops no longer than 4 days, but the incubation period of adenovirus infection is about 8 days.
This is a typical characteristic of acute conjunctivitis. The manifestation of an inflammatory disease provokes vivid symptoms in a child, with which parents go to the clinic.
Symptoms of pathology
Conjunctivitis has a distinctive set of symptoms that does not depend on the causative agent of infection, but there are also characteristic signs of pathology. For a disease of any form, whether it is allergic chlamydial conjunctivitis, the following symptoms are typical:
- swelling of the eyelids;
- redness of the conjunctiva;
- lacrimation;
- petechial hemorrhages;
- feeling of dryness, irritation;
- photophobia;
- general malaise;
- cutting sensations in the eyes;
- headache;
- blurred vision;
- fever;
- soreness of the eyeballs. nine0027
- topical anti-inflammatory and antipruritic drugs are used; nine0020
- instill eyewash solutions;
- use antibacterial drugs of local and general action;
- eye drops-tear substitutes are prescribed in case of dryness.
- mucosal lesions with the development of dry eye syndrome;
- corneal inflammation and clouding;
- decreased quality of vision;
- occurrence of scars, deformities;
- eyelid fusion.
- do not touch the face, eyes with dirty hands, as the infection is transmitted by contact;
- wash hands after outdoor contact with pets; nine0020
- avoid contact with sick children because bacterial conjunctivitis is contagious;
- timely treat infectious pathologies;
- use individual towels;
- strengthen immunity;
- replace handkerchiefs with disposable wipes.
The listed signs are typical for conjunctivitis of any etiology of the disease, the symptoms are complex and increase in the first days of the disease. A specific sign of a bacterial infection is purulent discharge, which is not present in viral infections. Herpetic conjunctivitis is characterized by a rash, allergic is characterized by redness of the mucous membrane, sharp signs of eye irritation, severe itching, nasal congestion, swelling of the conjunctiva.
Treatment of bacterial conjunctivitis in children
When examining a sick child and diagnosing acute bacterial conjunctivitis with purulent discharge and typical clinical manifestations of the disease, the main task for the doctor is to prescribe an effective and adapted treatment. It is important to choose a drug with good tolerance, which will not cause discomfort during therapy, and also will not cause side effects.
For the treatment of bacterial conjunctivitis:
Doctors make their choice in the treatment of bacterial conjunctivitis in children on a group of broad-spectrum antimicrobials. They are also recommended for bacterial complication of viral conjunctivitis. It is best to prescribe antibacterial drugs after a laboratory study of purulent discharge in order to target the pathogen. For example, with fungal infections, antimycotic drugs will be more effective, and with viral lesions, antibiotics are completely useless, unless a bacterial infection has joined. nine0003
For example, with fungal infections, antimycotic drugs will be more effective, and with viral lesions, antibiotics are completely useless, unless a bacterial infection has joined. nine0003
If the diagnosis of conjunctivitis for the type of pathogen was not carried out, then doctors rely on clinical signs of inflammatory pathology. For treatment, drugs of the penicillin or erythromycin series are prescribed for suspected streptococcal conjunctivitis, and the therapy of the gonococcal form is carried out by local and systemic methods. If the disease proceeds with frequent exacerbations, corneal lesions and is difficult to treat, then doctors prescribe antibiotics of the fluoroquinolone and vancomycin series. nine0003
Chronic form, herpetic conjunctivitis and other types of pathology are recommended to be treated with the addition of steroids. They increase the effectiveness of antibiotic therapy, but the use of hormones in acute forms of the disease is unacceptable.
Treatment of conjunctivitis with antibiotic eye ointments and eye drops takes an average of 5–7 days.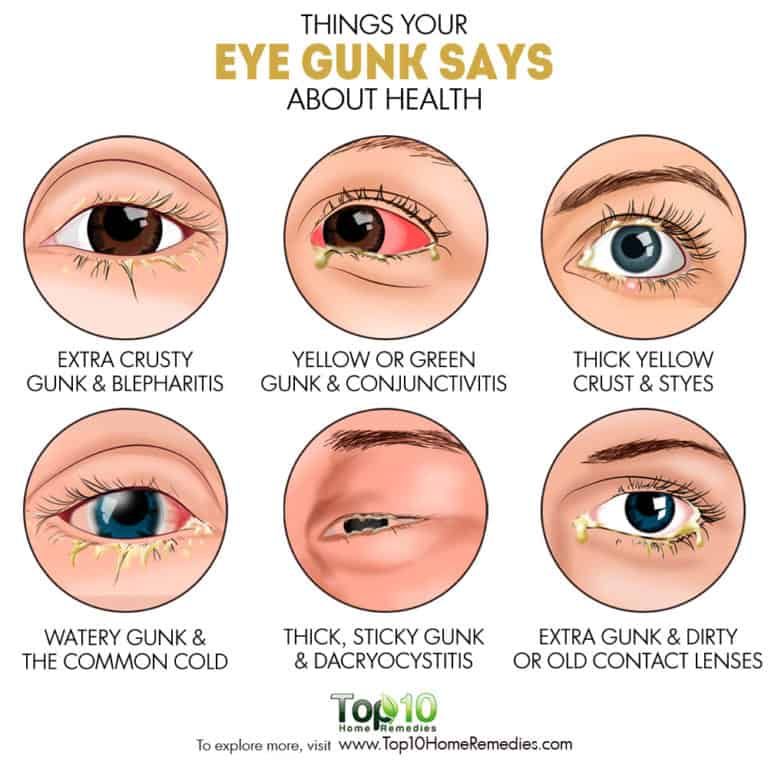 In order not to develop secondary bacterial conjunctivitis, therapy is carried out in full. Strictly follow the recommendations of a specialist, do not skip the processing time, do not reduce or increase the number of instillations. Otherwise, the slightest pathology of the eyes with a weakened immune system causes a secondary infection. In the absence of a clinical effect of the drug and for the prevention of dangerous complications within 2-3 days, the regimen is changed. nine0003
In order not to develop secondary bacterial conjunctivitis, therapy is carried out in full. Strictly follow the recommendations of a specialist, do not skip the processing time, do not reduce or increase the number of instillations. Otherwise, the slightest pathology of the eyes with a weakened immune system causes a secondary infection. In the absence of a clinical effect of the drug and for the prevention of dangerous complications within 2-3 days, the regimen is changed. nine0003
During the treatment of conjunctivitis in children, it is important to ensure the outflow of copious purulent discharge, eliminate redness and swelling of the mucous membrane, ensure timely toileting of the eyelids, and prevent stagnation of abundant discharge in the corners. Do not allow the baby to rub his eyes, shade the room so as not to irritate the eyesight with bright light. A sick child with signs of inflammation and the appearance of purulent discharge must be isolated from the children's team.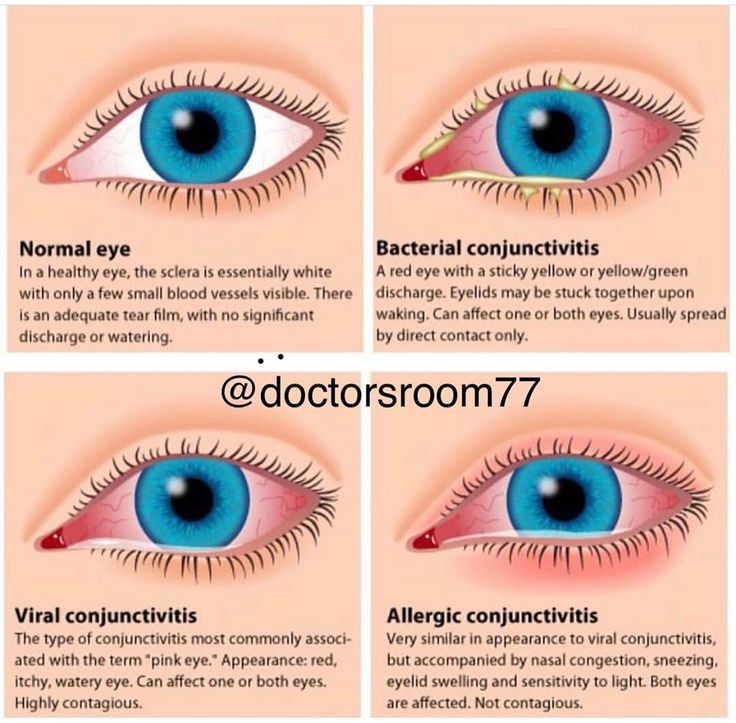 Complete recovery from various infectious lesions of an acute nature is possible in 7-14 days, chronic pathologies last 2-3 months. nine0003
Complete recovery from various infectious lesions of an acute nature is possible in 7-14 days, chronic pathologies last 2-3 months. nine0003
Complications and consequences
Among the most common dangerous diseases that occur after suffering conjunctivitis, there may be dacryocystitis and phlegmon of the lacrimal sac. The cause of dacryocystitis is tissue inflammation, and in chronic conjunctivitis of the eyes, when purulent discharge is in the lacrimal sac for a long time, phlegmon develops. In the absence of proper drug therapy, the pathological process extends to the periorbital tissue, followed by inflammatory edema. nine0003
Among the complications associated with the misuse of drugs or late visits to the doctor, note:
If the disease is accompanied by complications, the duration of therapy is prolonged, and the pediatric ophthalmologist will change the recommendations and prescribe drugs to combat the consequences. nine0003
nine0003
Prevention of bacterial conjunctivitis
Prevention of the development of conjunctivitis is, first of all, strict hygiene, because most conjunctivitis is caused by pathogenic microorganisms. Simple rules of hygiene will help eliminate the factors for the development of pathology. Remind children of elementary recommendations:
These precautions can protect the child from infection. Not only parents, but also educators and teachers should lead by example. It is imperative that there are no cases of adult conjunctivitis in preschool and school settings.