Vaccinations are not immunizations
Immunisation or vaccination - what's the difference?
Immunisation or vaccination - what's the difference? | Pregnancy Birth and Baby beginning of content6-minute read
Listen
What is a vaccine?
Vaccination prepares the immune system to fight against a future infection. Vaccines often contain tiny amounts of dead or weakened viruses or bacteria, called antigens. The immune system responds to these antigens without you getting sick, effectively training the immune system to fight the disease if exposed to it in the future.
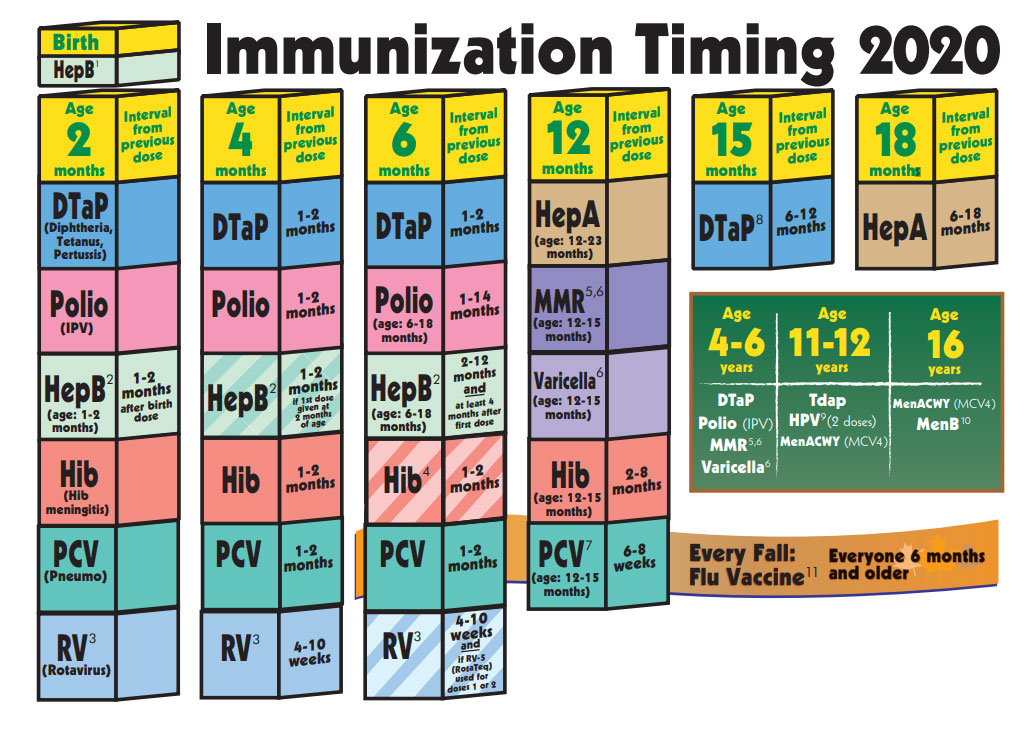
Some vaccines need to be given more than once — known as ‘booster’ vaccinations. Some vaccines, such as the seasonal influenza (flu) vaccine, only work for a short period of time. This is because the virus itself can change over time.
Vaccines are usually given with an injection.
What is in vaccines?
Some vaccines contain a very small dose of a live but weakened form of a virus. Some vaccines contain a very small dose of killed bacteria or small parts of bacteria, and other vaccines contain a small dose of a modified toxin produced by bacteria.
Vaccines may also contain either a small amount of preservative or a small amount of an antibiotic to preserve the vaccine. Some vaccines may also contain a small amount of an aluminium salt, which helps produce a better immune response.
How does immunisation work?
The terms ‘vaccination’ and ‘immunisation’ don’t mean quite the same thing. Vaccination is the term used for getting a vaccine — that is, actually getting the injection or taking an oral vaccine dose. Immunisation refers to the process of both getting the vaccine and becoming immune to the disease following vaccination.
All forms of immunisation work in the same way. When someone is injected with a vaccine, their body produces an immune response in the same way it would following exposure to a disease but without the person getting the disease. If the person comes in contact with the disease in the future, the body is able to make an immune response fast enough to prevent the person developing the disease or developing a severe case of the disease.
If the person comes in contact with the disease in the future, the body is able to make an immune response fast enough to prevent the person developing the disease or developing a severe case of the disease.
What’s the difference between a booster dose and a primary vaccine course?
A primary vaccine course involves the vaccine doses you need for very good protection against a disease.
A booster dose refers to an extra dose of a vaccine that is given after you’ve completed the primary vaccine course.
It gives your immune system a 'boost' and helps provide a higher level of protection from the disease.
Booster doses are common with diseases such as COVID-19, tetanus and whooping cough (pertussis).
How long do immunisations take to work?
In general, the normal immune response takes approximately 2 weeks to work. This means protection from an infection will not occur immediately after immunisation. Most immunisations need to be given several times to build long-lasting protection.
A child who has been given only 1 or 2 doses of the DTPa vaccine is only partially protected against diphtheria, tetanus and pertussis (whooping cough) and may become sick if exposed to these diseases until they have all the doses they need. However, some of the new vaccines, such as the meningococcal ACWY vaccine, provide long-lasting immunity after only one dose.
How long do immunisations last?
The protective effect of immunisations is not always lifelong. Some, like tetanus vaccine, can last up to 10 years depending on your age, after which time a booster dose may be given. Some immunisations, such as whooping cough vaccine, give protection for about 5 years after a full course. Influenza immunisation is needed every year due to frequent changes to the type of flu virus in the community.
Is everyone protected from disease by immunisation?
Even when all the doses of a vaccine have been given, not everyone is protected against the disease. Measles, mumps, rubella, tetanus, polio, hepatitis B and haemophilus influenzae type b (Hib) vaccines protect more than 95% of children who have completed the course. One dose of meningococcal ACWY vaccine at 12 months protects over 90% of children.
One dose of meningococcal ACWY vaccine at 12 months protects over 90% of children.
Three doses of whooping cough vaccine protect about 85% of children who have been immunised, and will reduce the severity of the disease in the other 15% if they do catch whooping cough. Booster doses are needed because immunity decreases over time.
Some vaccinations, like for COVID-19, won’t necessarily prevent you from catching the disease, but can reduce the risk of serious illness.
How are vaccines approved in Australia?
Before a vaccine becomes available in Australia, it must pass the rigorous approval processes of the Therapeutic Goods Administration (TGA). This includes assessing every ingredient in the vaccine for safety, quality and effectiveness.
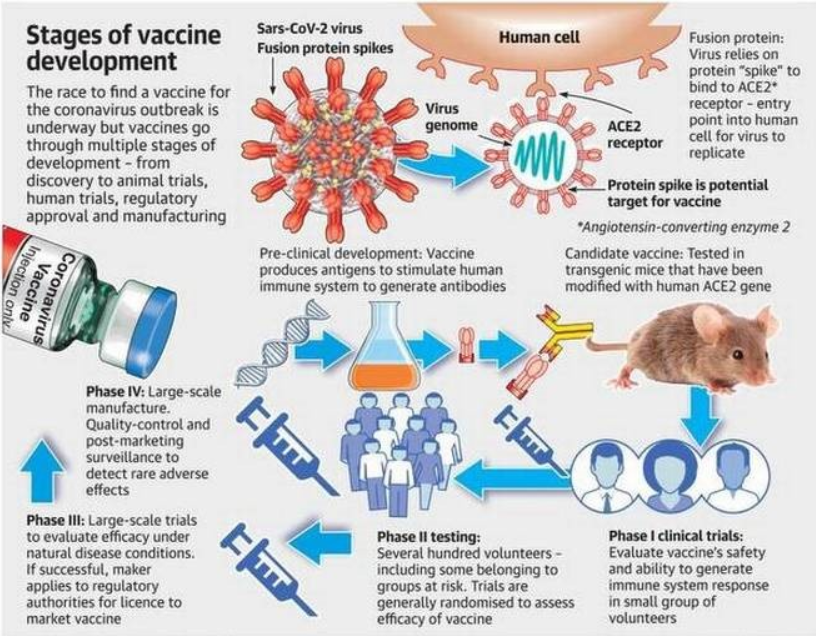
A clinical trial is a scientific study conducted by the makers of a vaccine. Clinical trials of medicines are done in phases.
The TGA carefully assesses the results of clinical trials, as well as the way in which the trials were run.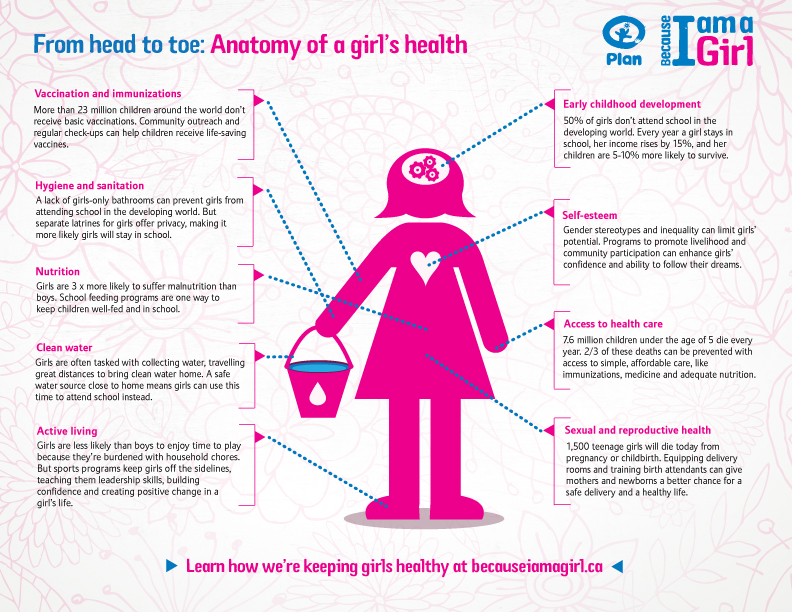 The TGA also checks that the trials involved enough human participants that represented the people for whom the vaccine is intended.
The TGA also checks that the trials involved enough human participants that represented the people for whom the vaccine is intended.
The TGA ensures that vaccine manufacturers meet manufacturing quality standards. TGA laboratories assess the quality of every batch of a vaccine before it can be supplied in Australia.
Sometimes a ‘provisional approval pathway’ is needed for the temporary registration of promising new medicines and vaccines — where the need for early access outweighs any risks.
Resources and support
In Australia, vaccines are funded by the National Immunisation Program and protect millions of Australians from vaccine-preventable diseases.
If you have any questions, you can speak to your doctor or call healthdirect on 1800 022 222 (known as NURSE-ON-CALL in Victoria).
Sources:
Department of Health (The Australian Immunisation Handbook), Raising Children Network (Immunisation in childhood), Raising Children Network (Immunisation FAQs), Department of Health (National Immunisation Program Schedule), Australian Government Department of Health (COVID-19 vaccines), NSW Health (Booster vaccination - frequently asked questions), Therapeutic Goods Administration (COVID-19 vaccine approval process)Learn more here about the development and quality assurance of healthdirect content.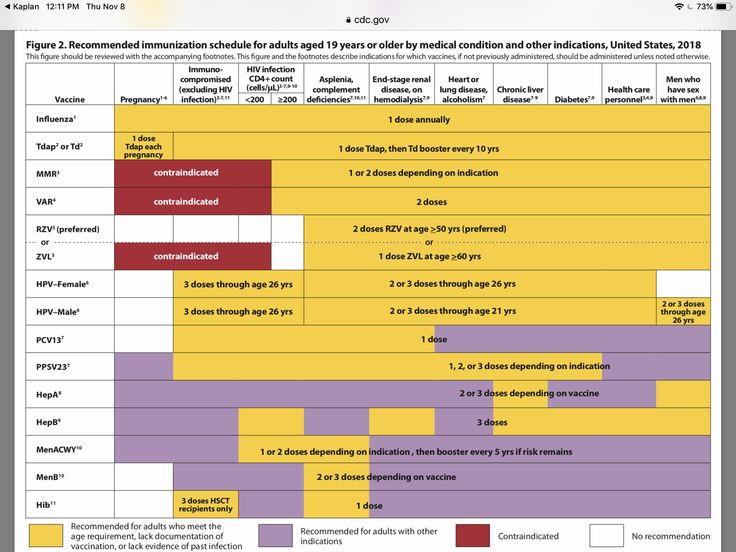
Last reviewed: May 2021
Back To Top
Related pages
- Immunisation and vaccinations for your child
- Vaccinations and pregnancy
Need more information?
Immunisation | Tasmanian Department of Health
Learn about information about immunisation, vaccines and diseases preventable by immunisation in Tasmania.
Read more on Tasmanian Department of Health and Human Services website
Immunisation and vaccinations for your child
Immunisation is a simple, safe and effective way of protecting children against certain diseases. Discover more about childhood vaccinations.
Read more on Pregnancy, Birth & Baby website
Immunisation | SA Health
Information for consumers on vaccines, immunisation programs and immunisation records for you and your children
Read more on SA Health website
Immunisation records | NCIRS
Your immunisation history statement has all your vaccines that have been recorded on the Australian Immunisation Register (AIR)
Read more on National Centre for Immunisation Research and Surveillance (NCIRS) website
What is immunisation? | Australian Government Department of Health and Aged Care
On this page Immunisation or vaccination — what's the difference? Australia's National Immunisation Program Immunisation is a safe and effective way of protecting you and your child against serious diseases.
Read more on Department of Health and Aged Care website
Where can I get immunised? | Australian Government Department of Health and Aged Care
You can get vaccinations from a range of vaccination providers, including your local GP and school-based immunisation programs.
Read more on Department of Health and Aged Care website
Immunisation schedules | NCIRS
The Australian National Immunisation Program (NIP) is funded by the Australian government and implemented by state and territory departments of health
Read more on National Centre for Immunisation Research and Surveillance (NCIRS) website
Kids - Immunisation Coalition
Find out how to protect your kids from infectious diseases.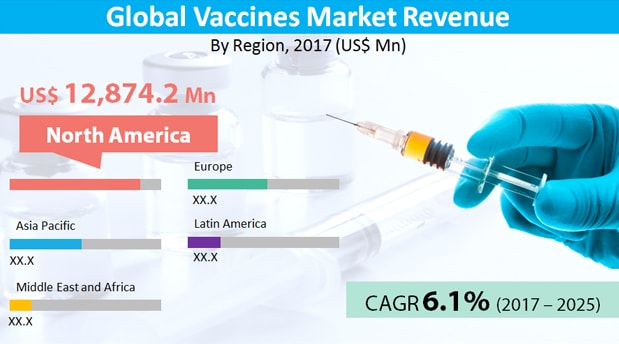 Keep up to date with the Childhood National Immunisation Program schedule.
Keep up to date with the Childhood National Immunisation Program schedule.
Read more on Immunisation Coalition website
Keeping your child’s vaccinations up to date during COVID-19
The COVID-19 pandemic has led to a decrease in children getting their routine childhood vaccinations.
Read more on Pregnancy, Birth & Baby website
Vaccination matters
Ensure your decisions about immunisation are based on fact. When doing your personal reading, make sure your source of information is based on scientific fact.
Read more on Queensland Health website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.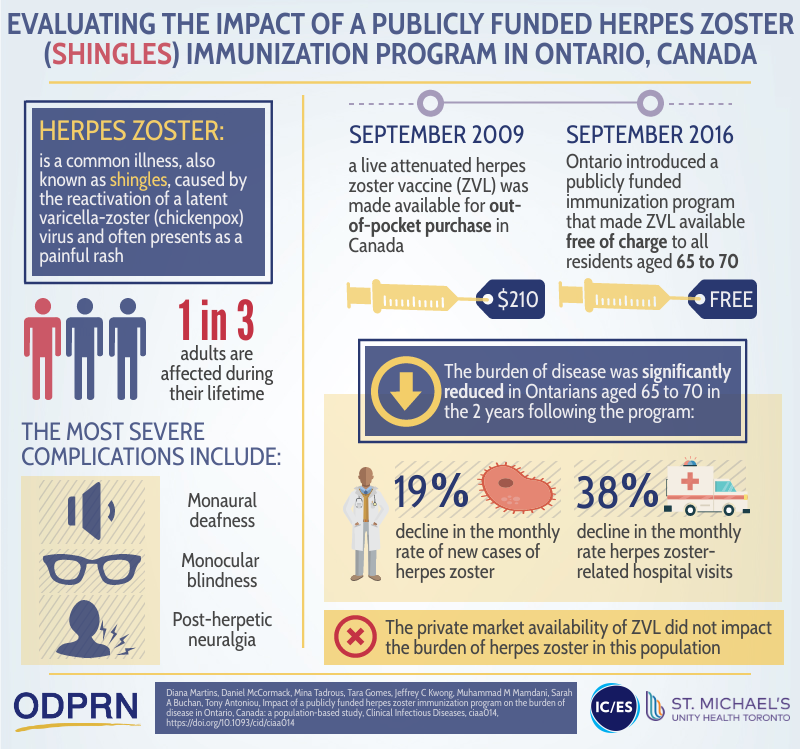
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari.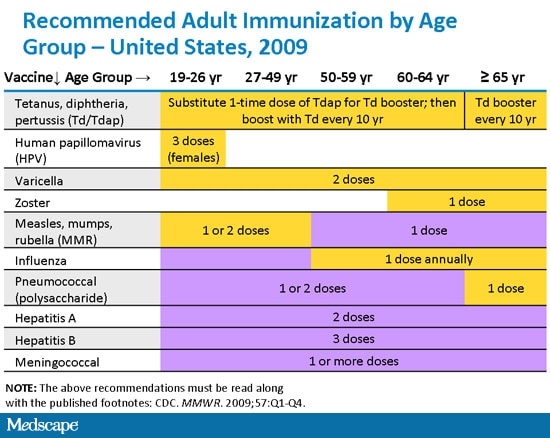 For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Common Questions About Vaccines (for Parents)
What Do Vaccines Do?
Vaccines work by preparing the body to fight illness. Each vaccine contains either a dead or a weakened germ (or parts of it) that causes a particular disease.
The body practices fighting the disease by making
antibodiesthat recognize specific parts of that germ. This permanent or long-lasting response means that if someone is exposed to the actual disease, the antibodies are in place and the body knows how to fight the disease so the person doesn't get sick. This is called immunity.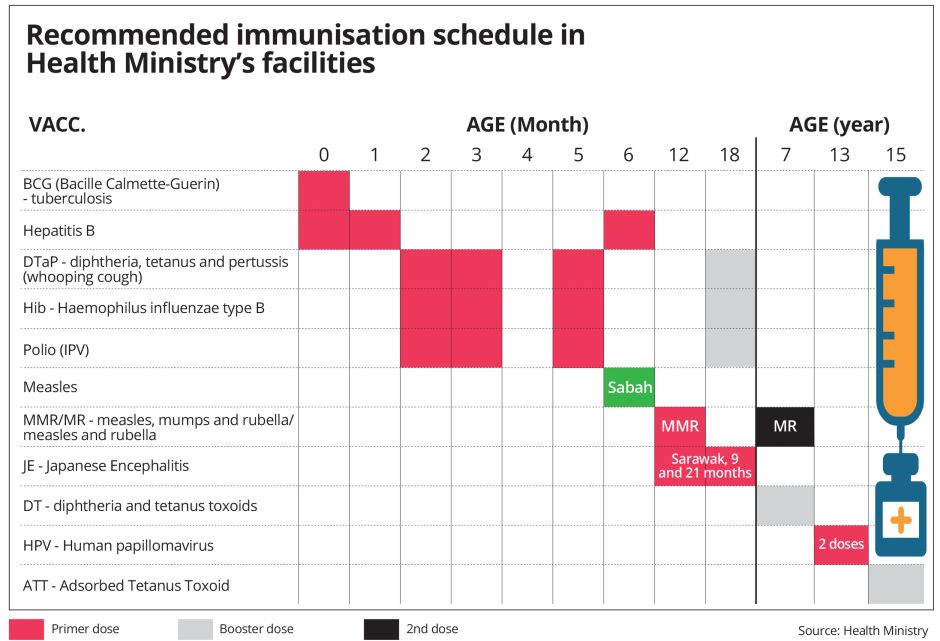 The process by which vaccines create immunity is known as immunization.
The process by which vaccines create immunity is known as immunization.
Since the start of widespread vaccinations in the United States, cases of once common childhood illnesses like measles and diphtheria have dropped greatly. Vaccines have protected millions of kids from dangerous diseases and saved thousands of lives.
In fact, some diseases are so rare now that parents sometimes ask if vaccines for them are even needed. But most diseases that can be prevented by vaccines do still exist in the world, even in the United States, although they happen very rarely.
Will the Immune System Be Weaker By Relying on a Vaccine?
No, the immune system makes antibodies against a germ, like the chickenpox virus, whether it encounters it naturally or through a vaccine. Being vaccinated against one disease does not weaken the immune response to another disease.
Can a Vaccine Give Someone the Disease It's Supposed to Prevent?
It's impossible to get the disease from any vaccine made with dead (killed) bacteria or viruses or just part of the bacteria or virus.
Only those vaccines made from weakened (also called attenuated) live viruses — like the chickenpox (varicella) and measles-mumps-rubella (MMR) vaccines — could possibly make a child develop a mild form of the disease. But it's almost always much less severe than if a child became infected with the disease-causing virus itself. However, for kids with weak immune systems, such as those being treated for cancer, these vaccines may cause problems.
The risk of disease from vaccination is very small. One live virus vaccine that's no longer used in the United States is the oral polio vaccine (OPV). The success of the polio vaccination program made it possible to replace OPV with the inactivated polio vaccine (IPV), which contains a killed virus form. This change means that polio disease cannot be spread by vaccinated U.S. children. OPV is still used in many other countries, though, with great success in reducing the number of cases worldwide.
Does My Child Need Vaccines if All the Other Kids in School Are Immunized?
It is true that a single child's chance of catching a disease is low if everyone else is fully vaccinated (immunized). But your child is also exposed to people other than those at school. And if one person thinks about skipping vaccines, chances are that others are thinking the same thing. Each child who isn't immunized gives highly contagious diseases one more chance to spread.
But your child is also exposed to people other than those at school. And if one person thinks about skipping vaccines, chances are that others are thinking the same thing. Each child who isn't immunized gives highly contagious diseases one more chance to spread.
Although vaccination rates are fairly high in the United States, there's no sure way to know if everyone your child has contact with has been vaccinated. That's especially true now that so many people travel to and from other countries. During travel, someone could be exposed to people who got OPV in other countries, which can be risky for anyone who didn't get all their polio vaccines. So the best way to protect your kids is through vaccination.
Can Getting So Many Vaccines at One Time Harm My Baby?
Babies have stronger immune systems than you might think, and they can handle far more germs than what they receive from vaccines. In fact, the amount of germs in vaccines is just a small percentage of the germs babies' immune systems deal with every day.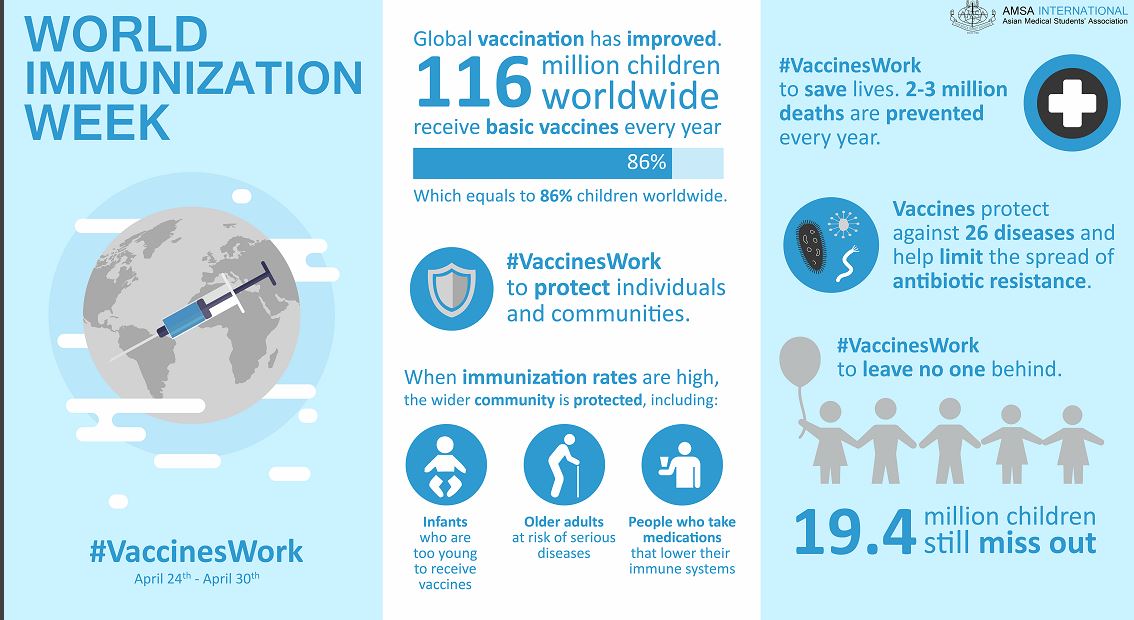
Sometimes, kids can have a reaction to a vaccine like a mild fever or rash. But the risk of serious reactions is small compared with the health risks from the often-serious diseases they prevent, and do not happen because the baby got several vaccines at once.
A lot of consideration and research went into creating the immunization schedule most doctors use, and it has been proven safe time and time again. Still, some parents choose to use alternative schedules (spreading or "spacing out" vaccines) because they're concerned about the number of shots their babies get at each checkup. This is actually more likely to make a baby sick. Studies show that many babies on alternative immunization schedules never get all the vaccines they need.
Plus, alternative schedules can be a real hassle. Spacing out vaccines over more doctor visits means that you'll have to take your child to the doctor — and your child will have to get a shot — more often.
Why Should My Child Get a Painful Shot if Vaccines Aren't 100% Effective?
Few things in medicine work 100% of the time. But vaccines are one of the most effective weapons we have against disease — they work in 85% to 99% of cases. They greatly reduce your child's risk of serious illness (particularly when more and more people are vaccinated) and give diseases fewer chances to take hold in a population.
But vaccines are one of the most effective weapons we have against disease — they work in 85% to 99% of cases. They greatly reduce your child's risk of serious illness (particularly when more and more people are vaccinated) and give diseases fewer chances to take hold in a population.
It can be hard to watch kids get a shot, but the short-term pain is nothing compared with suffering through a potentially deadly bout of diphtheria, whooping cough, or measles.
Why Do Healthy Kids Need to Be Immunized?
Vaccinations are intended to help keep healthy kids healthy. Because vaccines work by protecting the body before disease strikes, if you wait until your child gets sick, it will be too late for the vaccine to work. The best time to immunize kids is when they're healthy.
Can Vaccines Cause a Bad Reaction in My Child?
The most common reactions to vaccines are minor and include:
- redness and swelling where the shot was given
- fever
- soreness at the site where the shot was given
In rare cases, vaccines can trigger more serious problems, such as seizures or severe allergic reactions.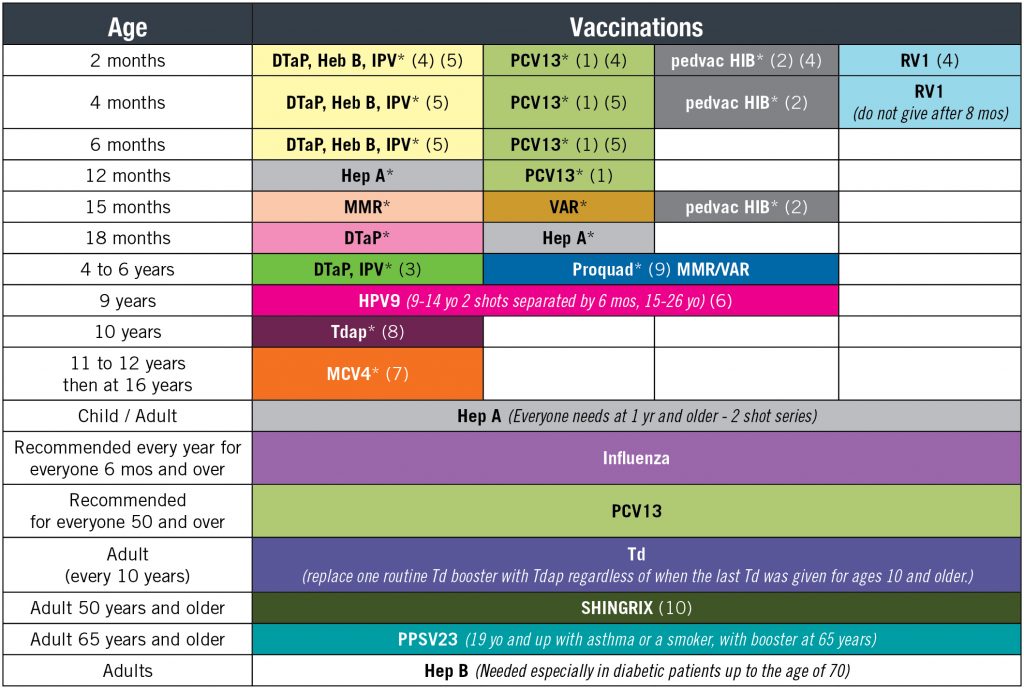 If your child has a history of allergies to food or medicine, or has had a problem with a vaccine before, let the doctor know before any vaccines are given. Every year, millions of kids are safely vaccinated and very few experience serious side effects.
If your child has a history of allergies to food or medicine, or has had a problem with a vaccine before, let the doctor know before any vaccines are given. Every year, millions of kids are safely vaccinated and very few experience serious side effects.
Research continually improves vaccine safety. The American Academy of Pediatrics (AAP) now advises doctors to use a diphtheria, tetanus, and pertussis vaccine that includes only specific parts of the pertussis cell instead of the entire killed cell. This vaccine, called DTaP, has been associated with even fewer side effects.
Do Vaccines or Thimerosal Cause Autism?
No. Many studies have found no link between vaccines and autism. Likewise, a groundbreaking 2004 report from the Institute of Medicine (IOM) found that thimerosal (an organic mercury compound that's been used as a preservative in vaccines since the 1930s) does not cause autism.
Still, some parents have opted not to have their children immunized, putting them at great risk for deadly diseases.
The MMR vaccine, especially, has come under fire even though many scientific reports have found no evidence linking the vaccine to autism. In fact, the study that suggested a possible link between autism and the MMR vaccine was retracted in 2004 and the doctor who published it lost his medical license. Even before it was discredited and declared fraudulent, the study was rejected by all major health organizations, including the AAP, the National Institutes of Health (NIH), the Centers for Disease Control and Prevention (CDC), and the World Health Organization (WHO).
There's also no reason to believe that thimerosal is linked to autism, according to the 2004 IOM report. Still, in an effort to reduce childhood exposure to mercury and other heavy metals, thimerosal began being removed from kids' vaccines in 1999. Now, vaccines for infants and young children contain no or very little thimerosal. And recent studies have not shown any cognitive and behavioral problems in babies who might have gotten these thimerosal-containing vaccines.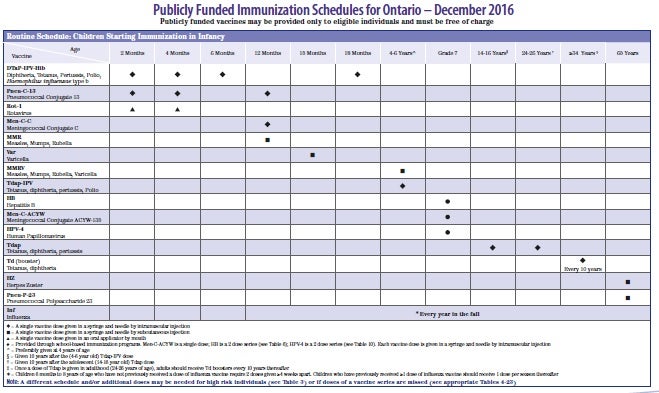
So what could explain the increased rates of autism in recent years? First, a broader definition of autism now can apply to more kids who show varying degrees of symptoms. A greater awareness of the condition among health professionals also has led to more diagnoses.
And while the number of children diagnosed with autism may be increasing, the rates of MMR vaccination are not. In London, diagnoses of autistic disorders have been on the rise since 1979, but rates of MMR vaccination haven't increased since routine MMR vaccination began in 1988.
Also, the average age of diagnosis of autism is the same both in children who have and who have not gotten the MMR vaccine. What many researchers are seeing is that a child might have subtle signs of autism before the first birthday — sometimes even in early infancy — but these aren't noticed by parents until they become more obvious.
Wasn't There a Problem With the Rotavirus Vaccine?
Rotavirus is one of the most common causes of diarrhea in young children. In 1999, a rotavirus vaccine was taken off the market because it was linked to an increased risk for intussusception, a type of bowel problem, in babies.
In 1999, a rotavirus vaccine was taken off the market because it was linked to an increased risk for intussusception, a type of bowel problem, in babies.
Now, two different rotavirus vaccines (RotaTeq and Rotarix) are available and are very safe. Some studies suggest that they have a very small increased risk for intussusception, but that problem is rare. These vaccines have been shown to prevent most cases of rotavirus infection and almost all severe cases.
The vaccine is now on the regular immunization schedule to be given orally to infants as a liquid during standard vaccination visits — RotaTeq at ages 2 months, 4 months, and 6 months, or Rotarix at ages 2 months and 4 months. Your doctor will have the most current information.
Do Vaccines Cause SIDS, Multiple Sclerosis, Or Other Problems?
There are concerns, many of which circulate on the Internet, linking some vaccines to multiple sclerosis, sudden infant death syndrome (SIDS), and other problems. To date, studies have not shown any connection between vaccines and these conditions.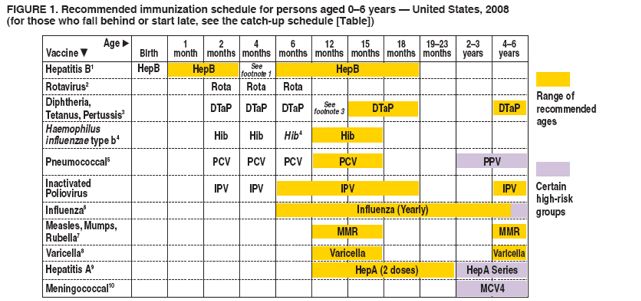 The number of SIDS cases has actually fallen by more than 50% in recent years, while the number of vaccines given yearly continues to rise.
The number of SIDS cases has actually fallen by more than 50% in recent years, while the number of vaccines given yearly continues to rise.
Why Do Kids Need Vaccines for a Disease That's Been Eliminated?
Diseases that are rare or wiped out in the United States, like measles and polio, still exist in other parts of the world. Doctors continue to vaccinate against them because it's easy to come into contact with illnesses through travel — either when Americans travel abroad or when people who aren't fully immunized come to the United States.
In recent years, there have been measles outbreaks in many different states, even though measles was declared eliminated from the U.S. in 2000. (Elimination means that the disease has not been transmitted continuously for over a year, but it doesn’t mean there aren't outbreaks.) These cases were mostly among people who did not get vaccinated. Other preventable diseases that had recent outbreaks include whooping cough (pertussis) and mumps.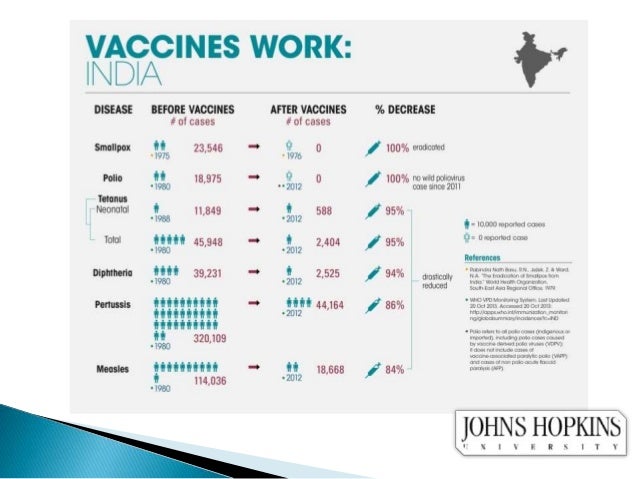
It's only safe to stop vaccinations for a particular disease when that disease has been eliminated worldwide, as with smallpox.
How Long Does Immunity Last After Getting a Vaccine?
A few vaccines, like the two for measles or the series for hepatitis B, may make you immune for your entire life. Others, like tetanus, last for many years but require periodic shots (boosters) for continued protection against the disease.
The whooping cough (pertussis) vaccine also does not give lifelong immunity, and that may be one reason why outbreaks still happen. Whooping cough isn't a serious problem for older kids and adults, but it can be for infants and young children. Because of this, teens and adults now get a pertussis booster along with the tetanus and diphtheria booster (Tdap) — an important step in controlling this infection, particularly for pregnant women and other adults who will be around newborn babies.
It's important to keep a record of vaccinations so the doctor knows when your kids are due for a booster.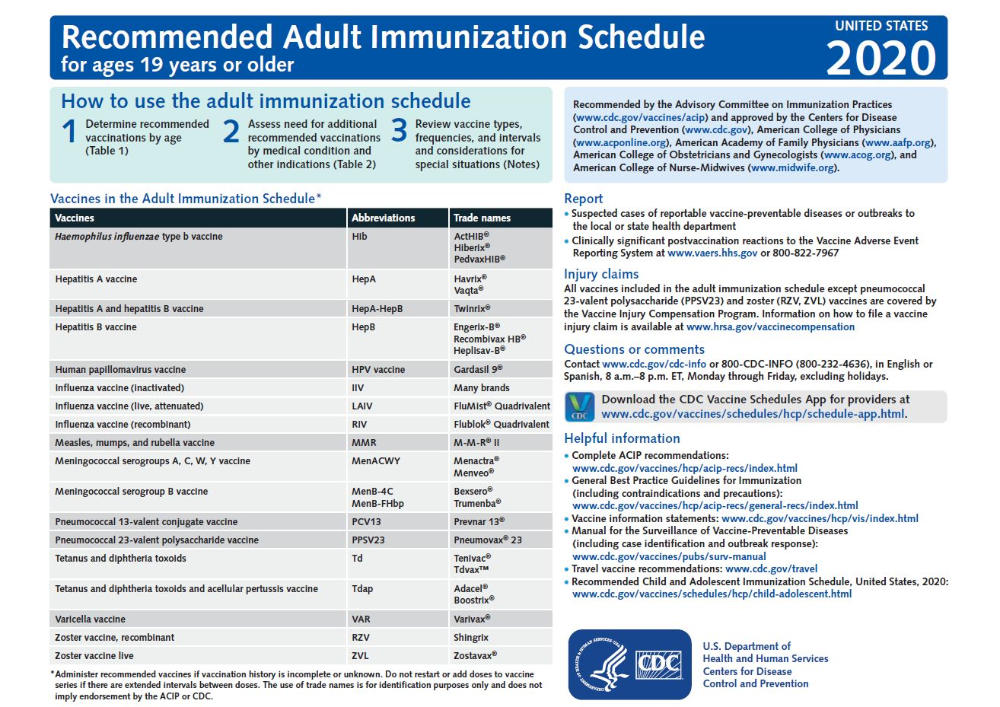 Also make sure your kids get the flu vaccine each year. Last year's flu vaccine won't protect someone from getting the flu this year because flu viruses constantly change. The vaccine is updated each year to include the most current strains of the virus.
Also make sure your kids get the flu vaccine each year. Last year's flu vaccine won't protect someone from getting the flu this year because flu viruses constantly change. The vaccine is updated each year to include the most current strains of the virus.
The flu vaccine reduces the average person's chances of catching the flu by up to 80%. It can't prevent infection by all viruses that can cause flu-like symptoms, though, so it's not a guarantee that someone won't get sick during flu season. Still, if a person who got the vaccine gets the flu, their symptoms usually will be fewer and milder.
How Are Vaccines Studied and Improved?
The FDA's Center for Biologics Evaluation and Research is the government agency that regulates vaccines in the United States. Working with the CDC and the NIH, they continuously research and monitor vaccine safety and effectiveness.
New vaccines are licensed only after thorough lab studies and clinical trials, and safety monitoring continues even after they're approved. There continue to be improvements (such as those already made to the DTaP and polio vaccines) that ease potential side effects and ensure the best possible safety standards.
There continue to be improvements (such as those already made to the DTaP and polio vaccines) that ease potential side effects and ensure the best possible safety standards.
Where Can I Get Affordable Vaccines for My Child?
Vaccines are one of the best tools we have to keep kids healthy. But they work best when everyone gets them. Vaccines are now required to be covered by health insurance plans at no cost to the patient. Some plans only cover vaccines when they are given by your doctor or at specific locations. So check with your insurance company to make sure. You can also get inexpensive or free vaccines through many local public health clinics and community health centers, and campaigns to vaccinate kids often hold free vaccination days.
The U.S. government's Vaccines for Children program covers Medicaid-eligible, uninsured Alaskan and Native American populations, and some underinsured kids for routine vaccinations up to 18 years of age. The vaccines are provided by the government and given in a doctor's office.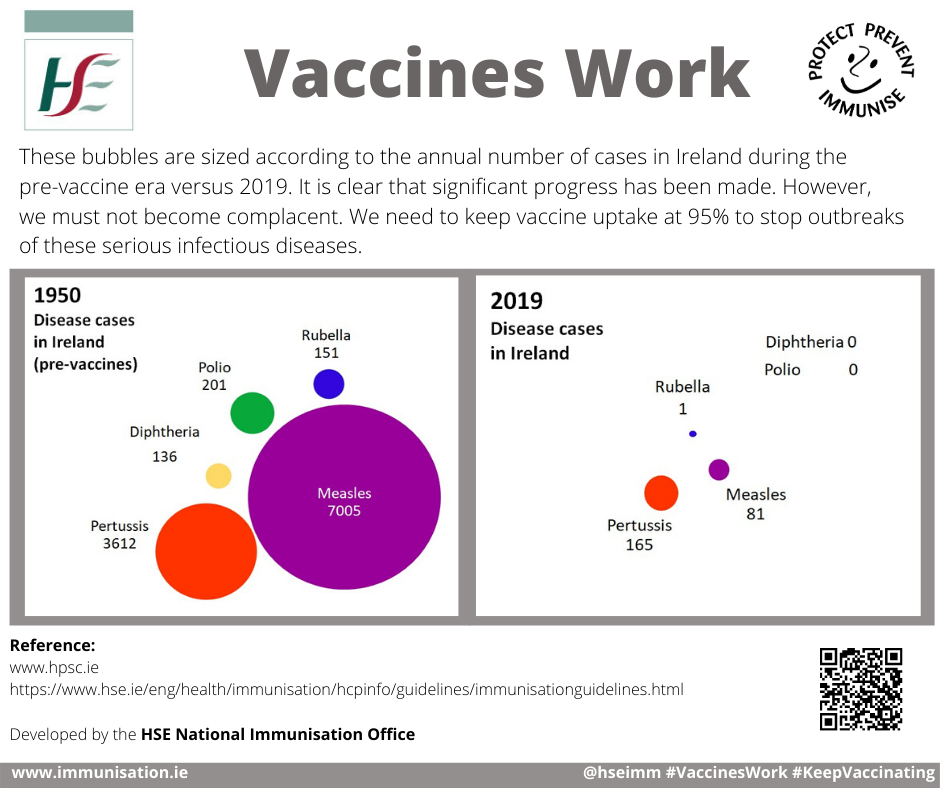 But the doctor's visit itself is not covered (unless the child has insurance, including Medicaid). Some public health clinics may cover both the visit and the vaccinations.
But the doctor's visit itself is not covered (unless the child has insurance, including Medicaid). Some public health clinics may cover both the visit and the vaccinations.
Where Can I Learn More About Vaccines?
Read this article for details about each recommended vaccine. You also can visit the CDC's National Immunization Program website for more information about vaccinations.
And talk with your doctor about which vaccines your kids need. Working together, you can help keep your family healthy.
Vaccinations: to be or not to be?
The question of whether to vaccinate a child worries many parents. This topic is associated with many fears, myths and doubts. We asked the most exciting questions to the pediatrician of EUROMED Clinic - Elena Sergeevna Kochetkova.
- Elena Sergeevna, can there be two opinions on the question of whether to vaccinate a child?
- Definitely not! Vaccination is the only way to protect your child from many dangerous (and sometimes deadly) infections. Many parents are afraid of complications after vaccinations, but I assure you, the risk of complications from past infections is many times higher. If we talk about complications after vaccinations, then first we need to distinguish between unwanted side effects and really real complications. Side effects are usually easily tolerated by the child and pass quickly. As for serious complications after vaccinations, I can say that in my more than 30 years of practice, I have only twice encountered really unpredictable and serious complications in children. And even then it cannot be said that they were completely criminal.
Many parents are afraid of complications after vaccinations, but I assure you, the risk of complications from past infections is many times higher. If we talk about complications after vaccinations, then first we need to distinguish between unwanted side effects and really real complications. Side effects are usually easily tolerated by the child and pass quickly. As for serious complications after vaccinations, I can say that in my more than 30 years of practice, I have only twice encountered really unpredictable and serious complications in children. And even then it cannot be said that they were completely criminal.
Usually, complications can be avoided by preparing the child for vaccination, taking into account his history, diseases, and allergies he has.
- In what cases is the vaccine not given for medical reasons?
- Most of our medical exemptions are purely Russian reinsurance, a concession to anxious parents. Abroad, for example, a high temperature will be considered the basis for a temporary refusal to vaccinate, and we even have a runny nose, which was three days ago for many, is a reason to postpone vaccination. In most cases, vaccination does not affect recovery, just as recovery does not affect vaccination. But we have accepted everything that happens to the child for a long time after the introduction of the vaccine, to write off the vaccination. We forget the golden rule: “after” does not mean “due to”.
In most cases, vaccination does not affect recovery, just as recovery does not affect vaccination. But we have accepted everything that happens to the child for a long time after the introduction of the vaccine, to write off the vaccination. We forget the golden rule: “after” does not mean “due to”.
Of course, there are cases when it is better to postpone vaccination. This is an acute condition in case of allergies (during the remission period, vaccination for allergy sufferers is not only possible, but must be done), high fever, acute respiratory viral infections, and some neurological diseases. A separate case when vaccination is recommended to be postponed is the presence of benign neutropenia in a child under one year old. This condition is associated with the adaptation of the child to our urban conditions, modern loads; It is manifested by the fact that an insufficient number of neutrophils is observed in the blood test. Moreover, this amount does not fit either into the norm or into the state of illness, but is in the average value.In such a situation, it is better not to burden the body additionally, its immune forces are now already weakened, and all forces are aimed at adapting to the environment.
- Is it possible to vaccinate children prone to allergies, often ill?
- First of all! Of course, in an acute condition, vaccinations are not given. But in a state of remission, it is necessary to be vaccinated. Judge for yourself, if a child who is often ill, weakened, becomes infected with some serious infection, how will he get sick? With a high degree of probability - very difficult, most likely with complications. As for allergy sufferers, an additional problem will arise with them - how to treat them, how they will react to the disease, to medications. Again, there is a high risk that the disease will be severe.
Therefore, allergy sufferers, often ill children, patients with heart disease need to be vaccinated.
- There is an opinion that vaccination can provoke the development of allergies in a child. This is true?
This is true?
- There is no direct connection here, of course. But if the child has a predisposition to allergies, the introduction of a vaccine can serve as an impetus for the development of the disease. In this situation, it is difficult to assume which is more dangerous, because the infection itself or medications can also provoke the development of allergies.
- Many parents wonder whether it is worth vaccinating against hepatitis B and tuberculosis right away in the maternity hospital - after all, the newborn baby is still so weak. Perhaps it would be wiser to give him time to adapt, and give these vaccinations later - say, at 3-6 months?
- A child immediately after birth (and even while still in the womb!) Faces hundreds of microorganisms, and successfully processes them. So the additional couple of antigens that he will be injected with during vaccination do not play a special role against this background.
The immune response to BCG (vaccination against tuberculosis) develops within 2-3 months. Given that tuberculosis occurs in absolutely all social strata, including among very prosperous and wealthy people, then when should a child be vaccinated in order to provide him with reliable protection?
Given that tuberculosis occurs in absolutely all social strata, including among very prosperous and wealthy people, then when should a child be vaccinated in order to provide him with reliable protection?
Hepatitis B is a disease that does not have the concept of “recovery” in childhood. If an adult becomes ill with hepatitis B, then he has a chance to control it - with the help of an appropriate lifestyle and medications. For children, this is not possible. They grow and therefore their hepatitis can only actively progress.
In childhood, the main route of infection with hepatitis B is during medical procedures. And no one can know when a child will need medical attention: an emergency operation, a blood transfusion after an injury, an accident. Girls now have their ears pierced very early - and this is also a risk of contracting hepatitis.
It is no coincidence that hepatitis B vaccination is given on the first day after birth - precisely because no one is immune from urgent medical intervention.
- What other vaccinations, in addition to those listed in the vaccination calendar, can be recommended for a child?
- Vaccination against rotavirus infection. Rotavirus is very dangerous in the first years of a child's life. More than 90% of children with rotavirus infection are hospitalized in an infectious diseases hospital. In general, according to statistics, more than half of the hospitalizations of children with acute intestinal diseases are associated with rotavirus infection. The disease is accompanied by high fever, severe vomiting and diarrhea (diarrhea), which leads to dehydration, and for young children this can be very dangerous. In addition, children can get sick with this infection repeatedly, since it has a lot of varieties. The vaccine protects against rotavirus and greatly facilitates the course of the disease with related viruses (norovirus, astrovirus, etc.).
The vaccination course includes three vaccinations with an interval of 4-10 weeks, the vaccine is administered orally (that is, drops in the mouth). The first vaccination is given at the age of 6 to 12 weeks (not later!), the last vaccination must be given no later than 8 months. After a full course of vaccination, the child develops immunity to rotavirus infection, which lasts up to 5 years. Revaccination is not required.
The first vaccination is given at the age of 6 to 12 weeks (not later!), the last vaccination must be given no later than 8 months. After a full course of vaccination, the child develops immunity to rotavirus infection, which lasts up to 5 years. Revaccination is not required.
Chickenpox vaccination. This vaccination is not included in the Russian vaccination calendar, unlike many foreign countries, but I recommend doing it. You can get vaccinated against chickenpox from the age of the child.
Many parents ask themselves: why is it needed, because if a child gets chickenpox in childhood, then he will have immunity for life anyway? Everything is so simple. In childhood, chicken pox is usually quite easily tolerated, especially if the child's mother is immune to this infection, and, accordingly, the mother's antibodies still remain in the small child. In older adults, chickenpox, most often, proceeds quite severely and with a large number of complications.
Many years of experience allows us to make the following observations: now chickenpox mutates quite strongly.Even 15 years ago, most doctors treated chickenpox quite calmly, arguing in the same way: they had been ill with fairly predictable consequences, and immunity was formed. Now the virus is becoming more aggressive, deaths and serious complications are recorded every year! Rashes appear not only on the skin, but also on the mucous membranes, on the internal organs: the surface of the intestines, bronchi, and this can lead to the development of severe complications.
In addition, it is important to consider that chickenpox is caused by a generalized herpes infection. And after that, herpes does not leave the body. Often, after 40 years, the virus wakes up and manifests itself in the form of a neurological reaction: shingles in the intercostal spaces. This is usually associated with stress, with a decrease in immunity.
Thus, the relevance of vaccination against chickenpox is no longer in doubt.
Vaccination against HPV. Human papillomavirus (HPV) is the main cause of cervical cancer. Accordingly, timely vaccination of girls against HPV is a reliable protection against the development of cancer. HPV immunization is recommended for girls and young women who are not yet infected with HPV. It is advisable to vaccinate before the onset of sexual activity, it is usually recommended for teenage girls at 12 years of age. The standard vaccination course consists of 3 doses and is carried out according to the scheme (0-2-6 months): the second dose - 2 months after the first; the third dose - 6 months after the first.
Accordingly, timely vaccination of girls against HPV is a reliable protection against the development of cancer. HPV immunization is recommended for girls and young women who are not yet infected with HPV. It is advisable to vaccinate before the onset of sexual activity, it is usually recommended for teenage girls at 12 years of age. The standard vaccination course consists of 3 doses and is carried out according to the scheme (0-2-6 months): the second dose - 2 months after the first; the third dose - 6 months after the first.
This vaccine can be recommended for all girls. But if there is a family history (oncology in one of the close relatives, especially cancer of the cervix, vulva, vagina), then this vaccine is especially needed!
Boys are also recommended to be vaccinated. Firstly, in order to protect their future beloved women, since boys can be carriers of HPV. Secondly, HPV can be one of the factors in the development of oncology of the reproductive system in men, although this is much less common.
Thus, we repeat once again: only vaccination is a reliable protection against many serious infections. Let's not experiment on our children, testing their resistance to infections and playing Russian roulette: they will easily get sick or get severe complications from a disease from which we could easily protect them just by vaccinating.
- Vaccination
- is the most effective way to protect your child from infectious diseases. With the help of vaccinations, they successfully fight measles, rubella, mumps (mumps), chicken pox, polio, hepatitis B, rotavirus infection and bacteria that cause tuberculosis, diphtheria, whooping cough, tetanus, hemophilic infection.
The essence of vaccination lies in the fact that a child is vaccinated with a weakened or killed pathogen (or artificially synthesized, similar to the present one) in order to stimulate the body to produce antibodies to it.
- Immunization calendar
- is a list of vaccines and a scheme for their administration, approved by the Ministry of Health of the Russian Federation.
The vaccination schedule regulates scheduled vaccinations and vaccinations that are given according to epidemiological indications.
Scheduled vaccinations are given against mass infections that are severe, have a high probability of adverse consequences or death. They are carried out, starting from the birth of a child, according to a special schedule. In addition to the vaccinations approved in the calendar, you can separately vaccinate against certain serious infections if you wish: chicken pox, human papillomavirus, rotavirus infection, etc.
Vaccinations according to epidemic indications are given in case of outbreaks of certain infections; people living or visiting epidemiologically disadvantaged areas; workers of certain specialties (medical workers, teachers, etc.). For example, all residents of the Novosibirsk region are recommended to be vaccinated against tick-borne encephalitis, a dangerous infection that can be contracted by a tick bite.
| Categories and age of citizens subject to preventive vaccinations | Name of vaccination | Notes |
|---|---|---|
| Newborns in the first 24 hours of life | First vaccination against viral hepatitis B | |
| Newborns on 3-7 days of life | Tuberculosis vaccination | |
| Children at 1 month | Second vaccination against viral hepatitis B | |
| Children at 2 months | Third vaccination against viral hepatitis B | According to indications, only if the child is at risk. |
| First vaccination against pneumococcal infection (provides protection against pneumonia, bronchitis, otitis and moderate SARS) | ||
| Children at 3 months | First vaccination against diphtheria, whooping cough, tetanus | |
| First vaccination against Haemophilus influenzae (purulent otitis media, meningitis) | The course of vaccination against hemophilic infection for children aged 3 to 6 months consists of 3 injections of 0.5 ml with an interval of 1-1.5 months. | |
| First polio vaccination | ||
| Children at 4, 5 months | Second vaccination against diphtheria, whooping cough, tetanus | It is carried out for children who received the first vaccination at 3 months |
| Second vaccination against Haemophilus influenzae | It is carried out for children who received the first vaccination at 3 months | |
| Second polio vaccination | It is carried out for children who received the first vaccination at 3 months | |
| Children at 6 months | Third vaccination against diphtheria, whooping cough, tetanus | It is carried out for children who received the first and second vaccinations at 3 and 4. 5 months, respectively. 5 months, respectively. |
| Third vaccination against viral hepatitis B | It is carried out for children who do not belong to risk groups who received the first and second vaccinations at 0 and 1 months, respectively. | |
| Third vaccination against Haemophilus influenzae | It is carried out for children who received the first and second vaccinations at 3 and 4.5 months, respectively. | |
| Third polio vaccination | ||
| Children at 12 months | Vaccination against measles, rubella, mumps | |
| Fourth hepatitis B vaccination | Conducted for children at risk | |
| Children at 18 months | First revaccination against diphtheria, whooping cough, tetanus | |
| First revaccination against polio | ||
| Revaccination against Haemophilus influenzae | Revaccinations are carried out once for children vaccinated in the first year of life. | |
| Children at 20 months | Second revaccination against polio | |
| Children at 6 years old | Revaccination against measles, rubella, mumps | Conducted to children who have received vaccinations against measles, rubella, mumps |
| Children at 6-7 years old | Second revaccination against diphtheria, tetanus | |
| Children at 7 years old | Revaccination against tuberculosis | |
| Third revaccination against diphtheria, tetanus | ||
| Third revaccination against polio | ||
| Revaccination against tuberculosis | ||
| Adults over 18 years old | Revaccination against diphtheria, tetanus | Carried out in accordance with the instructions for the use of antigen-reduced toxoids in adults over 18 years of age every 10 years from the last revaccination |
Services
Child vaccination Extensive vaccination for injuries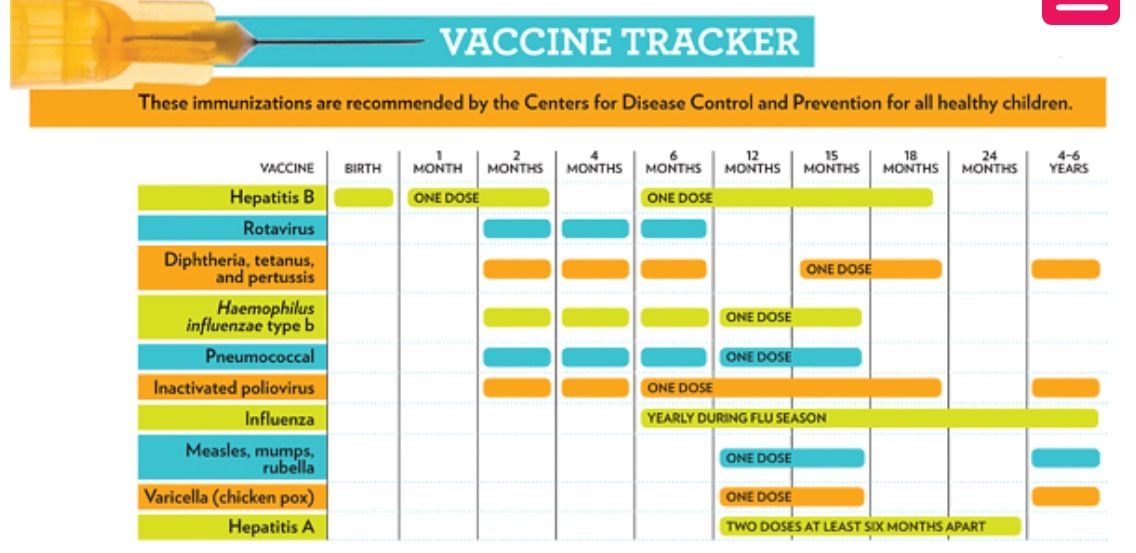 Popular Topics
Popular Topics - Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- 298
- I
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center/ 9029eight
- Questions and answers /
- Questions and answers /
- Vaccines and immunization: What is vaccination?
August 30, 2021 | FAQ
Revised August 10, 2021
What is vaccination?
Vaccination is a simple, safe and effective way to protect against diseases before a person comes into contact with their pathogens.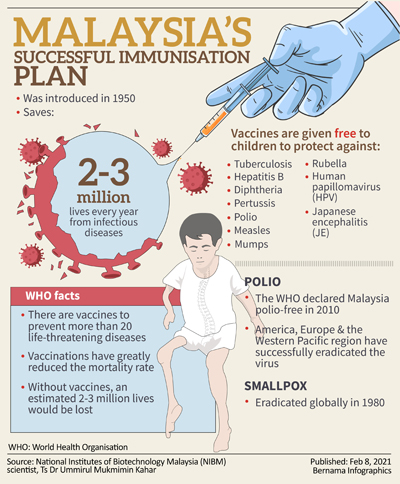 Vaccination activates the body's natural defense mechanisms to build resistance to a range of infectious diseases and makes your immune system stronger.
Vaccination activates the body's natural defense mechanisms to build resistance to a range of infectious diseases and makes your immune system stronger.
Like diseases, vaccines train the immune system to produce specific antibodies. However, vaccines contain only killed or attenuated forms of the causative agents of a particular disease - viruses or bacteria - that do not lead to the disease and do not create the risk of complications associated with it.
Most vaccines are given by injection, although some are given by mouth. vaccines (given by mouth), and nasal spray vaccines (given through the nose).
What is the principle of the vaccine?
Vaccines reduce the risk of disease by activating natural defense mechanisms to build immunity to the pathogen. Vaccination provokes the body's immune response. Immune system:
- Recognizes pathogens such as viruses or bacteria.
- Starts production of antibodies. Antibodies are proteins naturally produced by the body's immune system to fight disease.
- Remembers the causative agent of the disease in order to deal with it in the future. If this pathogen enters the body again, the immune system will quickly destroy it, preventing the development of the disease.
Thus, vaccination is a safe and rational way to induce an immune response in the body without the need to infect it with a particular disease.
Our immune system has a memory. By receiving one or more doses of a vaccine, we are usually protected against a particular disease for many years, decades, or even a lifetime. This is what makes vaccines so effective. Vaccines keep us from getting sick, which is much better than having to treat the disease when it has already begun.
When should I get vaccinated (or have my child vaccinated)?
Vaccines protect us throughout our lives and at all ages - from birth, through childhood, through adolescence and into old age. In most countries, people are given vaccination cards that show which vaccinations an adult or child has received and when the next vaccinations are due. It is important that all indicated vaccinations are up to date.
It is important that all indicated vaccinations are up to date.
By delaying vaccination, we put ourselves at risk of becoming seriously ill. If we wait until the moment when a vaccine is urgently needed - for example, if an outbreak of a disease has begun - then it may be too late to get the desired effect of vaccination or all the necessary doses of the vaccine.
Why do I need to be vaccinated?
Without vaccination, we are at risk of serious diseases such as measles, meningitis, pneumonia, tetanus and polio. Many of these diseases are life threatening. The WHO estimates that childhood vaccines alone save more than 4 million lives each year.
Although some diseases are becoming less common, their pathogens continue to circulate in some or all regions of the world. In today's world, infectious diseases can easily cross borders and infect anyone who lacks immunity to them.
There are two main reasons to get vaccinated: to protect yourself and to protect others.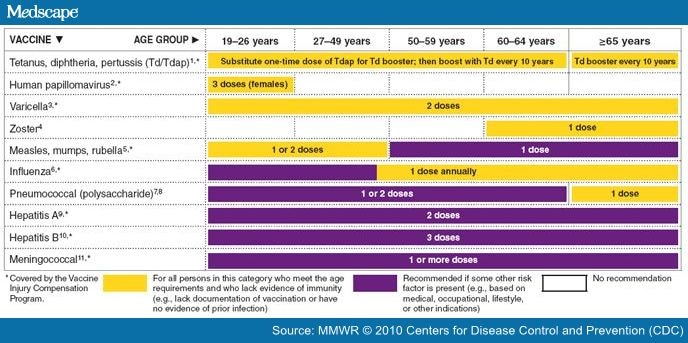 Since some people, such as newborns and people with serious illnesses or those with certain allergies, may not be vaccinated, their protection against vaccine-preventable diseases depends on the availability of vaccinations in others.
Since some people, such as newborns and people with serious illnesses or those with certain allergies, may not be vaccinated, their protection against vaccine-preventable diseases depends on the availability of vaccinations in others.
Who should not be vaccinated?
Almost anyone can get vaccinated. However, for people with certain diseases and conditions, some vaccinations are contraindicated or should be deferred to a later date. These diseases and conditions may include:
- chronic diseases or treatments (eg chemotherapy) that suppress the immune system;
- extremely rare acute and life-threatening allergic reactions to vaccine components;
- severe illness at the time of vaccination. However, these children should be vaccinated as soon as they recover. Moderate malaise or subfebrile temperature is not a contraindication for vaccination.
Often the need to consider these factors depends on the type of vaccine. If you are not sure whether you or your child should get a particular vaccine, ask your doctor.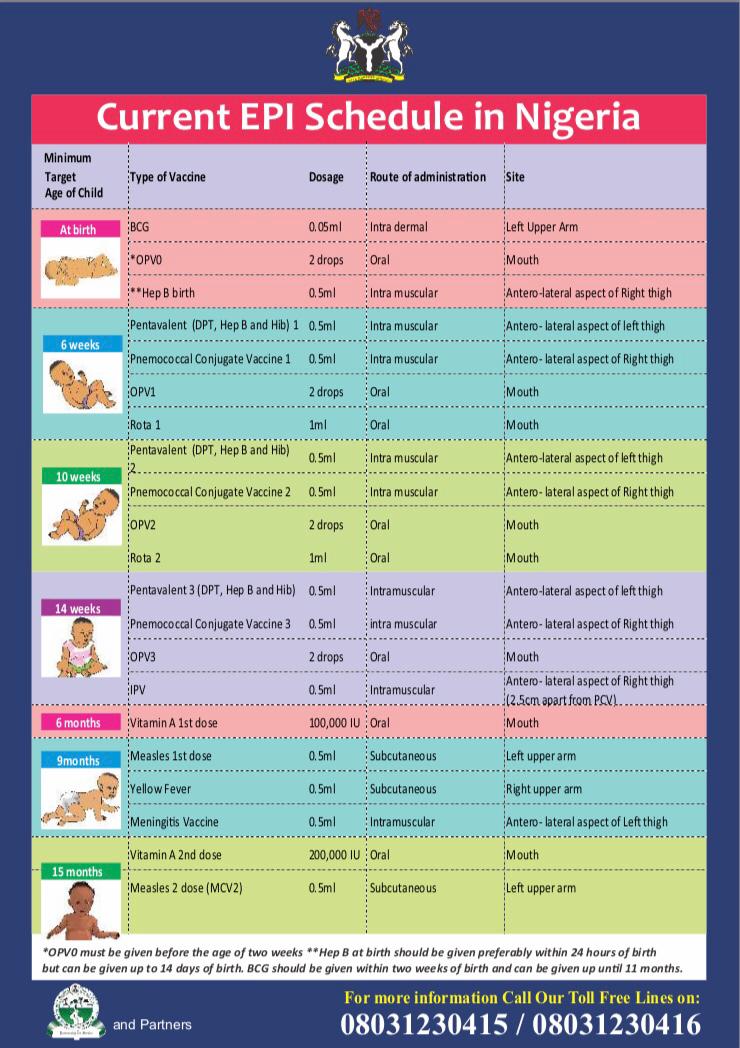 Your doctor will help you make an informed decision about your or your child's vaccinations.
Your doctor will help you make an informed decision about your or your child's vaccinations.
A number of vaccines for some other diseases, including Ebola or malaria, are currently under development or experimental use, but these vaccines have not yet been introduced in mass use throughout the world.
Not all vaccinations may be required in your country. Vaccinations against certain diseases may only be required for people who travel to certain countries or who are at increased risk due to their professional activities. Ask your doctor what vaccinations you and your family members need.
Why are vaccinations started at such an early age?
In their daily lives, young children may find themselves in many different places and come into contact with a wide variety of people, thereby exposing them to a serious risk of infection. The WHO-recommended immunization schedule allows infants and young children to be protected as early as possible against a range of diseases. Often, infants and young children are most at risk of illness because their immune systems are not yet fully developed and their bodies are less able to fight off infections. Therefore, it is extremely important to vaccinate children according to the recommended schedule.
Often, infants and young children are most at risk of illness because their immune systems are not yet fully developed and their bodies are less able to fight off infections. Therefore, it is extremely important to vaccinate children according to the recommended schedule.
What is included in the vaccine?
All components of a vaccine play an important role in its safety and efficacy. The composition of vaccines, in particular, includes the following components:
- Antigen. This is a killed or weakened form of any microorganism - a virus or a bacterium - on which our body learns to recognize and destroy the causative agent of the disease if it encounters it in the future.
- Adjuvants that help enhance the body's immune response. Without them, vaccines would be less effective.
- Preservatives to keep vaccines effective.
- Stabilizers to preserve the vaccine during storage and transport.
The names of vaccine components written on vaccine packages can be confusing.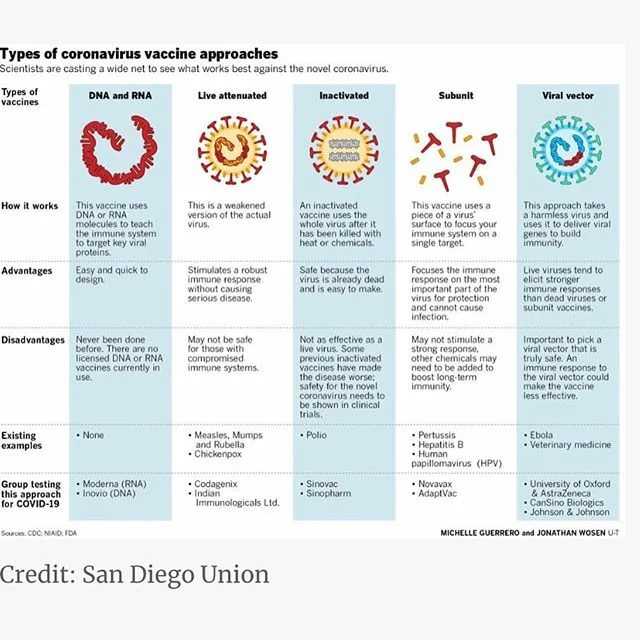 However, many of them are naturally present in the body, environment and food. All of the components of vaccines, like the vaccines themselves, are subject to rigorous testing and monitoring for their safety.
However, many of them are naturally present in the body, environment and food. All of the components of vaccines, like the vaccines themselves, are subject to rigorous testing and monitoring for their safety.
Are vaccines safe?
Vaccination is safe and usually causes minor and temporary side effects, such as arm pain or mild fever. More serious side effects are possible, but they are extremely rare.
Any licensed vaccine is rigorously tested through several phases of clinical trials before it is approved for use and regularly evaluated after introduction. Scientists are also constantly monitoring information from a range of sources for signs that a given vaccine may pose a health risk.
It must be remembered that the risk of serious harm to health from a vaccine-preventable disease is much greater than the risk associated with vaccination. For example, tetanus can cause severe pain, convulsions and thrombosis, and measles can lead to encephalitis (infection of the brain) and blindness.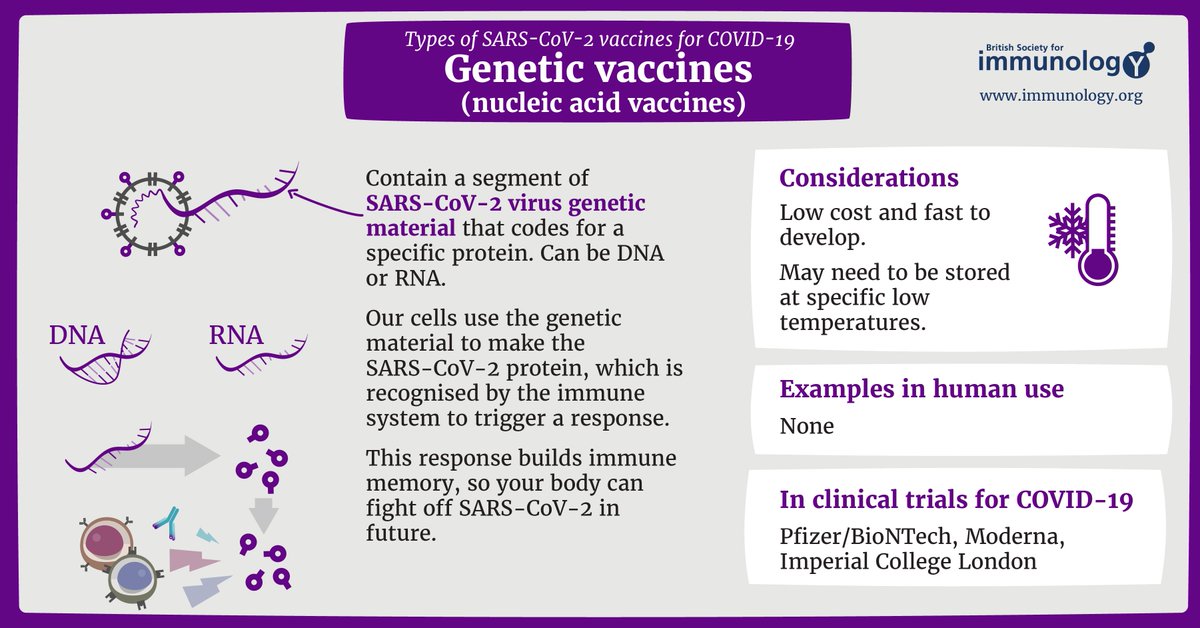 Many vaccine-preventable diseases can even be fatal. The benefits of vaccination far outweigh the risks, and without vaccines, the world would experience an order of magnitude more illness and death.
Many vaccine-preventable diseases can even be fatal. The benefits of vaccination far outweigh the risks, and without vaccines, the world would experience an order of magnitude more illness and death.
My child did not receive the recommended vaccinations on time. Is it too late to get the missing vaccinations?
In most cases, it is never too late to get the missing shots. Ask your doctor how and when you or your child can get the missing shots.
Do vaccines have side effects?
Like all medicines, vaccines can cause mild side effects such as low grade fever and pain or redness at the injection site. These symptoms usually go away on their own within a few days.
Severe or long-term side effects are extremely rare. The chance of experiencing a serious adverse body reaction to a vaccine is 1 in a million.
The safety of vaccines is constantly monitored and is continuously monitored for rare adverse reactions.
How are vaccines developed and tested?
The most commonly used vaccines have been in use for decades, and every year millions of people receive them safely. Like all medicines, every vaccine must undergo extensive, rigorous testing to assess its safety before it can be introduced in countries.
Like all medicines, every vaccine must undergo extensive, rigorous testing to assess its safety before it can be introduced in countries.
Experimental vaccines are first tested in animals to evaluate their safety and ability to prevent disease. They are then tested in human clinical trials, which consist of three phases.
• During the first phase of the trial, the vaccine is given to a small number of volunteers to evaluate its safety, make sure it generates an immune response, and determine the correct dose.
• During the second phase of the trial, the vaccine is typically administered to hundreds of volunteers, who are closely monitored for any side effects and further evaluation of its ability to generate an immune response. Data on disease outcomes are also collected at this stage whenever possible, but these data are usually not sufficient to provide a clear picture of the impact of the vaccine on the disease. Participants in this phase of the trial share the same characteristics (such as age and gender) as the people for whom the vaccine is intended. At this stage, some volunteers receive the vaccine and others do not, allowing comparisons to be made and conclusions about the vaccine to be made.
At this stage, some volunteers receive the vaccine and others do not, allowing comparisons to be made and conclusions about the vaccine to be made.
• During the third phase of the trial, the vaccine is administered to thousands of volunteers, some of whom receive the study vaccine and some do not, as in the second phase of the trial. The data from both groups are carefully compared to determine whether the vaccine is safe and effective in protecting against the disease it is intended to target.
Following clinical trial results, a number of steps must be taken before a vaccine can be included in a national immunization program, including efficacy, safety, and manufacturing reviews for regulatory approval and public health policy approval.
After the introduction of the vaccine, careful monitoring continues to detect any unexpected unwanted side effects and further evaluate its effectiveness under conditions of regular use in even more people, which will allow understanding how to best use the vaccine to ensure the greatest protective effect. For more information on vaccine development and safety, click here.
For more information on vaccine development and safety, click here.
Can a child have more than one vaccine at a time?
Scientific evidence shows that the simultaneous administration of several vaccines does not have negative consequences. Every day, children are exposed to several hundred foreign substances that trigger the body's immune response. A simple meal is accompanied by the entry of new microorganisms into the body, and many bacteria live in the nose and mouth.
The ability to combine multiple vaccines (such as diphtheria, whooping cough and tetanus) reduces the number of injections and reduces discomfort for the child. In addition, it allows you to know for sure that the child received the right vaccinations at the right time and will not catch a potentially fatal disease.
Is there a link between vaccination and autism?
There is no evidence of any association between vaccination and autism spectrum disorders. This conclusion was drawn from the results of many studies conducted on very large groups of people.
In 1998, a study was published raising concerns about a possible link between the measles, mumps, and rubella (MMR) vaccine and autism, but the study later found a number of serious misrepresentations and falsified information. The journal that published this work later withdrew it, and the doctor who wrote it lost his license to practice medicine. Unfortunately, due to fears caused by this publication, vaccination rates in some countries dropped sharply, which subsequently led to outbreaks of these diseases.
We all have a responsibility to take the necessary steps to disseminate only reliable, science-based information about vaccines and the diseases that vaccines help prevent.
Does my daughter need to be vaccinated against the human papillomavirus (HPV)?
Almost all cases of cervical cancer are caused by sexually transmitted HPV infection. Vaccination against HPV before a person comes into contact with this virus is the most effective means of protection against this disease. Studies in Australia, Belgium, Sweden, Germany, New Zealand, the United Kingdom, the United States of America and Sweden showed that vaccination reduced the number of HPV infections among adolescent girls and young women to almost 90%.
Studies in Australia, Belgium, Sweden, Germany, New Zealand, the United Kingdom, the United States of America and Sweden showed that vaccination reduced the number of HPV infections among adolescent girls and young women to almost 90%.
Studies have proven the safety and efficacy of the HPV vaccine. WHO recommends that all girls aged 9–14 years be vaccinated with two doses of the HPV vaccine, and that women be periodically screened for cervical cancer later in life.
I have questions about vaccinations. Who should I contact?
If you have any questions about vaccinations, be sure to ask your doctor. He or she will be able to give you evidence-based information about vaccinations, including the recommended vaccination schedule in your country for you and your family members.
When looking for information about vaccines on the Internet, look only to trusted sources. To help you find these sources, WHO has reviewed and "certified" many websites in many languages around the world to contain only information based on sound scientific evidence and independent analysis by leading technical experts.