How to control diabetes when pregnant
Diabetes During Pregnancy: Diet Tips | Patient Education
Blood sugar control during pregnancy is important for your health and the health of your baby. The following tips will help you control your blood sugar levels during pregnancy. Carbohydrates in food turn into sugar (also called glucose) when digested. Glucose is important for you and your baby, but too much glucose in your blood can lead to problems. It is important to eat the right amount of carbohydrate and to choose healthy foods. Carbohydrates are found in starches, fruits, vegetables, milk and yogurt so these food portions should be measured. Sweets and desserts should be avoided as they may lead to high blood sugar levels.
1. Eat 3 meals and 2–3 snacks per day
Eating too much at one time can cause your blood sugar to go too high. Eat smaller meals and have snacks. You have increased nutritional needs during your pregnancy, and your baby is counting on you to provide balanced nutrition.
2. Measure your servings of starchy foods
Include a starch choice at every meal. A reasonable serving size is about 1 cup of cooked rice, grain, noodles or potatoes, or 2 pieces of bread, per meal.
3. One 8-ounce cup of milk at a time
Milk is a healthy food and it is an important source of calcium. Because it is a liquid, milk sugar is absorbed quickly. Having too much milk at one time can lead to high blood sugar. It is best to limit milk to one cup at a time.
4. One small portion of fruit at a time
Fruits are nutritious, but because they have natural sugars, eat only one serving at a time. A serving of fruit is one small piece of fruit, or ½ large fruit, or about 1 cup of mixed fruit. Avoid fruit that has been canned in syrup. Do not drink fruit juice.
5. Eat more fiber
Try whole grain bread, brown rice, wild rice, whole oats, barley, millet or any other whole grains. Include split peas, lentils and any type of bean: pinto, red, black, or garbanzo. These foods are high in fiber and help to keep your blood sugar levels lower than when you eat refined grains such as white bread and white rice.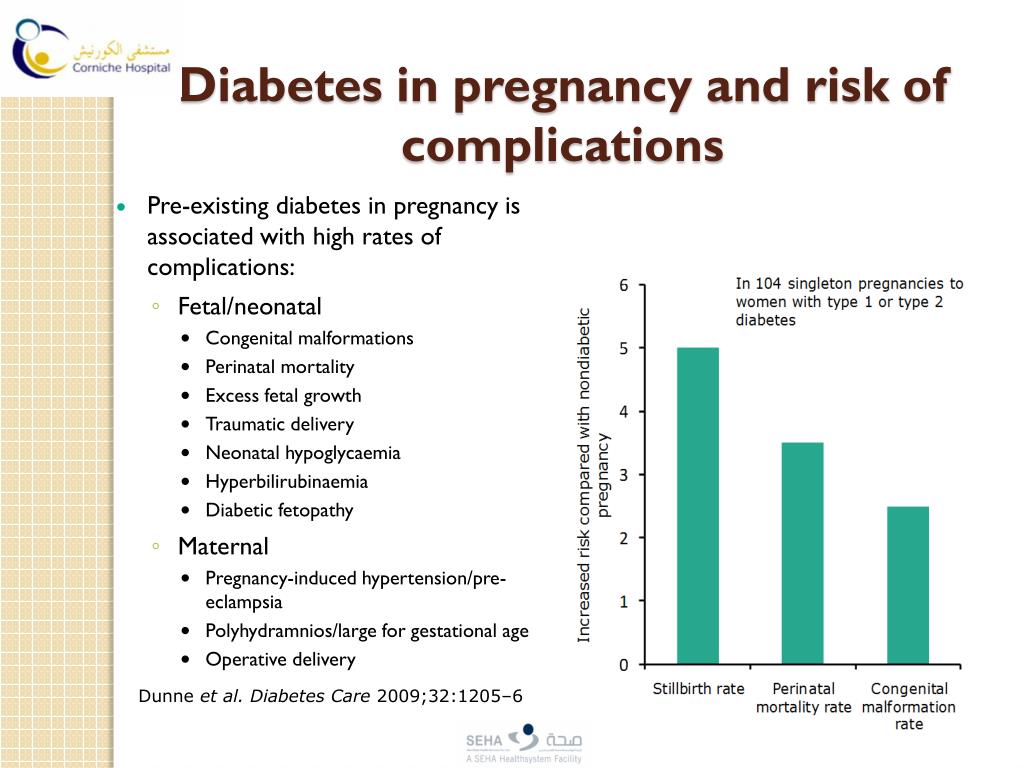
6. Breakfast Matters
Blood sugar can be difficult to control in the morning because that is when pregnancy hormones are very strong. These hormones can cause your blood sugar levels to rise even before you eat.
Dry cereals, fruits, and milk are not the best choices for breakfast because they are digested very quickly and can cause blood sugar levels to rise quickly.
A breakfast of whole grains plus a protein food is usually best.
7. Avoid fruit juice and sugary drinks
It takes several pieces of fruit to make a glass of juice. Juice is high in natural sugar. Because it is liquid, it raises blood sugar levels quickly. Avoid regular sodas and sugary soft drinks for the same reason. You may use diet drinks and Crystal Light.
8. Strictly limit sweets and desserts
Cakes, cookies, candies, and pastries are high in sugar and are likely to raise blood sugar levels too much. These foods often contain a lot of fat and offer very little nutrition.
9. Stay away from sugars
Do not add any sugar, honey, or syrup to your foods.
10. These artificial sweeteners are safe in pregnancy
- Aspartame; Equal, NutraSweet, NatraTaste
- Acesulfame K; Sunett
- Sucralose; Splenda
- Stevia; Truvia, Purevia
11. Look out for sugar-alcohols in sugar-free foods
Sugar alcohol is often used to make sugar-free desserts and syrups. These products can be labeled "sugar free" but may contain the same amount of carbohydrate as the versions made with regular sugar. Look at food labels to see the grams of total carbohydrate.
Sugar alcohols may have a laxative effect, or cause gas and bloating. The following are examples of sugar-alcohols: mannitol, maltitol, sorbitol, xylitol, isomalt, and hydrogenated starch hydrolysate.
Gestational Diabetes and Pregnancy | CDC
Gestational diabetes is a type of diabetes that is first seen in a pregnant woman who did not have diabetes before she was pregnant.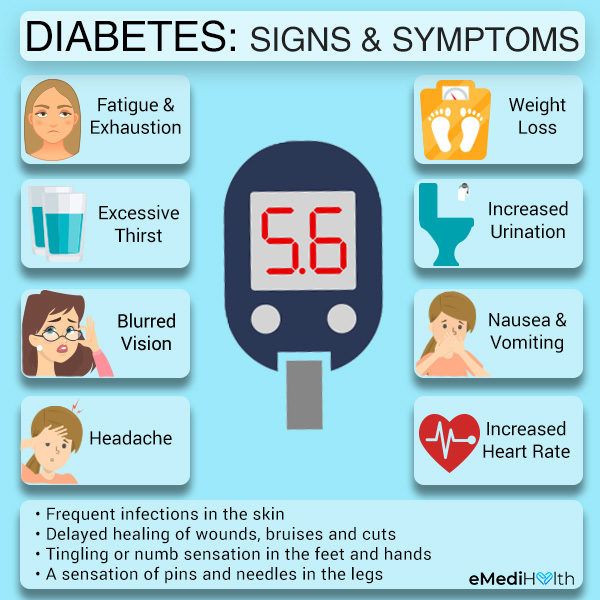 Some women have more than one pregnancy affected by gestational diabetes. Gestational diabetes usually shows up in the middle of pregnancy. Doctors most often test for it between 24 and 28 weeks of pregnancy.
Some women have more than one pregnancy affected by gestational diabetes. Gestational diabetes usually shows up in the middle of pregnancy. Doctors most often test for it between 24 and 28 weeks of pregnancy.
Often gestational diabetes can be managed through eating healthy foods and regular exercise. Sometimes a woman with gestational diabetes must also take insulin.
Learn more about Diabetes Self-Management Education and Support Services
Blood sugar that is not well controlled in a woman with gestational diabetes can lead to problems for the pregnant woman and the baby:
An Extra-Large Baby
Diabetes that is not well controlled causes the baby’s blood sugar to be high. The baby is “overfed” and grows extra-large. Besides causing discomfort to the woman during the last few months of pregnancy, an extra-large baby can lead to problems during delivery for both the mother and the baby. The mother might need a C-Section to deliver the baby. The baby can be born with nerve damage due to pressure on the shoulder during delivery.
C-Section (Cesarean Section)
A C-section is an operation to deliver the baby through the mother’s belly. A woman who has diabetes that is not well controlled has a higher chance of needing a C-section to deliver the baby. When the baby is delivered by a C-section, it takes longer for the woman to recover from childbirth.
High Blood Pressure (Preeclampsia)
When a pregnant woman has high blood pressure, protein in her urine, and often swelling in fingers and toes that doesn’t go away, she might have preeclampsia. It is a serious problem that needs to be watched closely and managed by her doctor. High blood pressure can cause harm to both the woman and her unborn baby. It might lead to the baby being born early and also could cause seizures or a stroke (a blood clot or a bleed in the brain that can lead to brain damage) in the woman during labor and delivery. Women with diabetes have high blood pressure more often than women without diabetes.
Low Blood Sugar (Hypoglycemia)
People with diabetes who take insulin or other diabetes medications can develop blood sugar that is too low. Low blood sugar can be very serious, and even fatal, if not treated quickly. Seriously low blood sugar can be avoided if women watch their blood sugar closely and treat low blood sugar early.
Low blood sugar can be very serious, and even fatal, if not treated quickly. Seriously low blood sugar can be avoided if women watch their blood sugar closely and treat low blood sugar early.
If a woman’s diabetes was not well controlled during pregnancy, her baby can very quickly develop low blood sugar after birth. The baby’s blood sugar must be watched for several hours after delivery.
5 Tips for Women with Gestational Diabetes
- Eat Healthy Foods
Eat healthy foods from a meal plan made for a person with diabetes. A dietitian can help you create a healthy meal plan. Learn more about diabetes meal planning. - A dietitian can also help you learn how to control your blood sugar while you are pregnant. To find a registered dietician near you, please visit The Academy of Nutrition and Dietetics website.
- Exercise Regularly
Exercise is another way to keep blood sugar under control. It helps to balance food intake.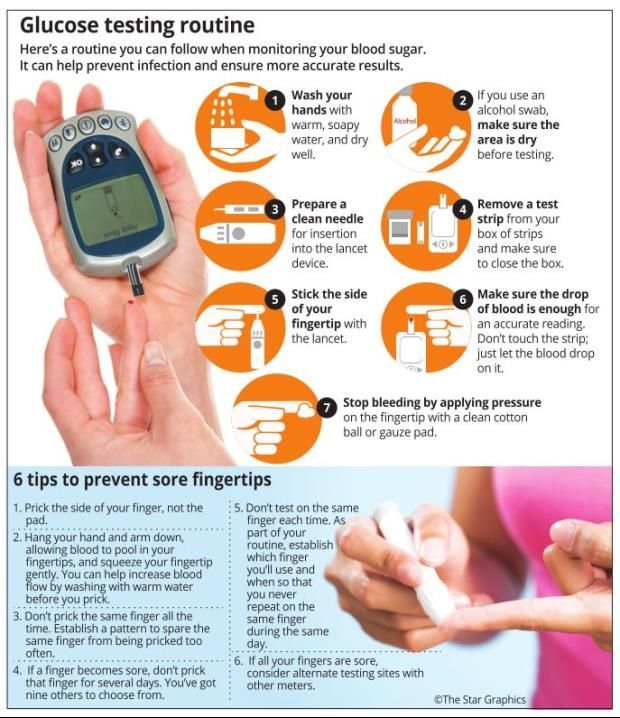 After checking with your doctor, you can exercise regularly during and after pregnancy. Get at least 30 minutes of moderate-intensity physical activity at least five days a week. This could be brisk walking, swimming, or actively playing with children.Learn more about physical activity during pregnancy »
After checking with your doctor, you can exercise regularly during and after pregnancy. Get at least 30 minutes of moderate-intensity physical activity at least five days a week. This could be brisk walking, swimming, or actively playing with children.Learn more about physical activity during pregnancy » - Monitor Blood Sugar Often
Because pregnancy causes the body’s need for energy to change, blood sugar levels can change very quickly. Check your blood sugar often, as directed by your doctor. - Take Insulin, If Needed
Sometimes a woman with gestational diabetes must take insulin. If insulin is ordered by your doctor, take it as directed in order to help keep blood sugar under control. - Get Tested for Diabetes after Pregnancy
Get tested for diabetes 6 to 12 weeks after your baby is born, and then every 1 to 3 years.For most women with gestational diabetes, the diabetes goes away soon after delivery. When it does not go away, the diabetes is called type 2 diabetes. Even if the diabetes does go away after the baby is born, half of all women who had gestational diabetes develop type 2 diabetes later. It’s important for a woman who has had gestational diabetes to continue to exercise and eat a healthy diet after pregnancy to prevent or delay getting type 2 diabetes. She should also remind her doctor to check her blood sugar every 1 to 3 years.
Even if the diabetes does go away after the baby is born, half of all women who had gestational diabetes develop type 2 diabetes later. It’s important for a woman who has had gestational diabetes to continue to exercise and eat a healthy diet after pregnancy to prevent or delay getting type 2 diabetes. She should also remind her doctor to check her blood sugar every 1 to 3 years.
Women who had gestational diabetes or who develop prediabetes can also learn more about the National Diabetes Prevention Program (National DPP), CDC-recognized lifestyle change programs. To find a CDC-recognized lifestyle change class near you, or join one of the online programs.
More Information
Gestational Diabetes and Pregnancy [PDF – 1 MB]
View, download, and print this brochure about gestational diabetes and pregnancy.
For more information on gestational diabetes, visit the American Diabetes Association’s website.
- Diabetes
- Before Pregnancy
- Healthy Pregnancy
- Birth Defects
- CDC’s National Center on Birth Defects and Developmental Disabilities
Gestational diabetes in pregnancy | OneTouch®
Gestational Diabetes
2What Causes Gestational Diabetes?
Doctors don't know exactly what causes gestational diabetes, but they have some ideas about it.
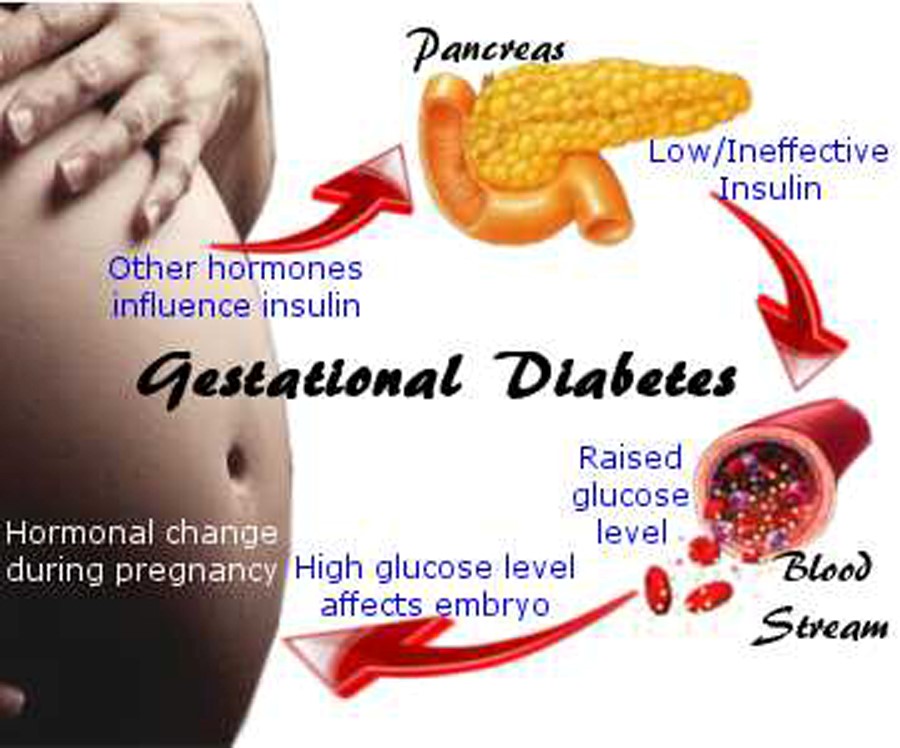
The placenta supports and nourishes the baby as it grows. Hormones from the placenta help the baby develop. But these same hormones also block the action of insulin, reducing its effectiveness. Gestational diabetes occurs when your body is no longer able to produce and use all the insulin it needs during pregnancy, resulting in high blood glucose levels if left untreated.
Some women are at higher risk of developing gestational diabetes. The following factors increase the risk of developing gestational diabetes:
- Being overweight before pregnancy
- Too much weight gain during pregnancy (more than the recommended amount)
- Age over 25
- History of gestational diabetes
- Presence of diabetes in close relatives
- African American, Asian, Hispanic or Native American
How is gestational diabetes diagnosed?
Most women who receive good medical care during pregnancy are regularly screened for gestational diabetes between the 24th and 28th weeks of pregnancy.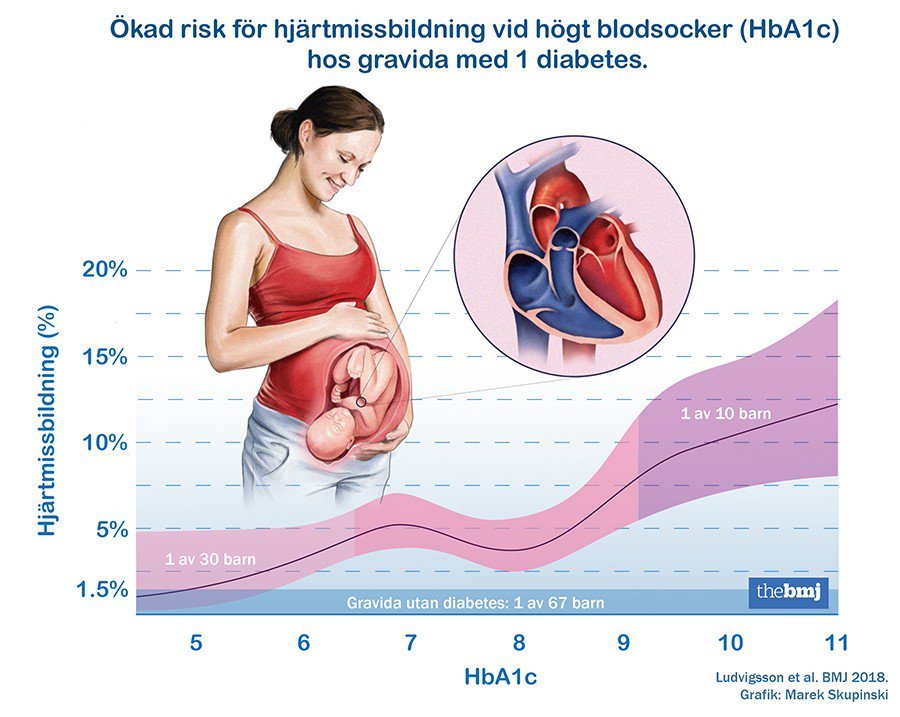 If you are at high risk of developing gestational diabetes, your doctor may test you earlier and/or more than once during your pregnancy.
If you are at high risk of developing gestational diabetes, your doctor may test you earlier and/or more than once during your pregnancy.
As part of the Gestational Diabetes Test, your doctor will ask you to drink a sugary drink, and you will have a blood sample taken before and after you drink the drink. If the results show that the blood glucose level at the specified time is above the recommended limits, the diagnosis of gestational diabetes is confirmed. Your doctor will tell you about a plan for treating gestational diabetes.
Why is it important to treat gestational diabetes?
A mother instinctively protects her child. It is important for the health of both mother and child that treatment for gestational diabetes be started as soon as the diagnosis is made. If left untreated, gestational diabetes can cause problems that include the following:
- An increased chance of having a large baby weighing more than 4 kg - this condition is called macrosomia.
 It increases the likelihood
It increases the likelihood - complications and injuries during vaginal delivery;
- caesarean section. (K-section)
- Your baby is at high risk for preterm labor and breathing problems (respiratory distress)
- Your baby is at high risk for low blood sugar (hypoglycemia) shortly after birth
- You are more likely to have preeclampsia (high blood pressure and liver or kidney problems)
Following your doctor's instructions and carefully managing your gestational diabetes can greatly reduce your risk of developing these complications.
What to expect if you are diagnosed with gestational diabetes?
If you have been diagnosed with gestational diabetes:
- Your doctor will recommend a healthy carbohydrate-controlled diet and exercise. In many cases, these measures will be sufficient to control blood glucose levels throughout pregnancy.
- You may need help from a dietitian in developing a healthy eating plan.
 A nutritionist can teach you how to control the amount and types of carbohydrates in your food so that you can manage your blood glucose levels while still meeting the needs of your growing child. You may also be asked to keep a food journal and monitor your weight.
A nutritionist can teach you how to control the amount and types of carbohydrates in your food so that you can manage your blood glucose levels while still meeting the needs of your growing child. You may also be asked to keep a food journal and monitor your weight. - You may need to check your blood glucose daily with a glucometer. Ask your doctor or diabetes consultant to recommend a glucometer that is right for you. Checking and tracking your blood glucose levels will help you and your doctor manage your gestational diabetes.
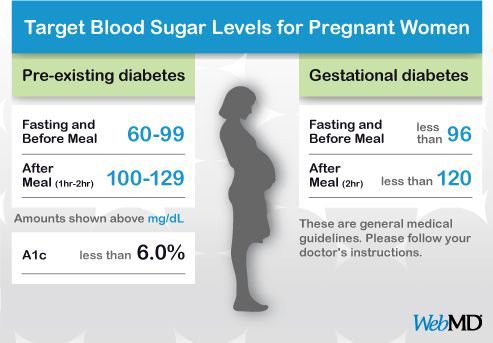
As a rule, blood glucose levels should be checked at least 4 times a day, usually on an empty stomach, and then 1-2 hours after a meal. Your doctor or healthcare professional will tell you how often you should test and what your target blood glucose range is. Remember to record your blood glucose measurements, including the time and results of the test, before or after a meal, and how long after a meal the test was taken.
- Light exercise during pregnancy will help your body make better use of its own insulin and help control blood glucose levels.
 Types of exercise that can be safely performed by pregnant women include brisk walking and swimming. Talk to your doctor for advice on safe exercise during pregnancy.
Types of exercise that can be safely performed by pregnant women include brisk walking and swimming. Talk to your doctor for advice on safe exercise during pregnancy.
At your appointment, the midwife can check your blood pressure and take a urine sample. You will also talk to your doctor about your blood glucose test results, how you eat, how much exercise you do, and how much weight you have gained. Your growing child will also be closely monitored. All this will help determine if the prescribed treatment plan for gestational diabetes is working and if it needs to be adjusted.
If dietary changes and exercise don't help control your blood glucose, your doctor may prescribe medication—pills or insulin—for the rest of your pregnancy.
Medication (pills, insulin)
Just because your doctor prescribes pills or insulin doesn't mean you can't manage your gestational diabetes. In some cases, your body may simply not be able to produce enough insulin on its own that your body needs as your baby grows. It is very important to follow your doctor's recommendations to protect yourself and your baby. You may be able to stop taking antidiabetic drugs after the baby is born.
It is very important to follow your doctor's recommendations to protect yourself and your baby. You may be able to stop taking antidiabetic drugs after the baby is born.
If your doctor prescribes insulin for gestational diabetes, you can get it by injection or by other means, such as an insulin pump. Someone in your family can learn this with you and help you take your insulin as prescribed by your doctor. Fortunately, today, thanks to insulin syringes with small, thin needles, injections are virtually painless. Your doctor will tell you when and how much insulin you should take each time, and may recommend adjusting your insulin intake during your pregnancy.
Refs:
2 IDF Diabetes Atlas (Version 8) (2017). International Diabetes Federation: Brussels, Belgium. Online version dated May 5, 2018 at http://diabetesatlas.org/IDF_Diabetes_Atlas_8e_interactive_EN/
You may be interested
What is diabetes?
PREGNANCY AND DIABETES IS A FOOD OF MISTAKE — "InfoMedPharmDialog"
Skip to content PREGNANCY AND DIABETES ARE A FIELD OF DELUSIONSPREGNANCY AND DIABETES ARE A FIELD OF DELUSIONS
This article carries more emotional than semantic load, but I think many doctors share my point of view.
Surely, patients come to every specialist with some strange ideas inspired by the Internet, television shows, neighbors on the bench in the yard. But the worst thing is that some of these attitudes are cultivated by doctors and harm at least the quality of life of the patient, and at the maximum - his health. Today I would like to discuss one of the most defenseless groups of endocrine patients - pregnant women with diabetes. The most difficult, of course, is for women with type 1 diabetes who are planning a child or come to the antenatal clinic already pregnant. Their whole diabetic life passes in a series of myths imposed by society, and it is good if these women have the strength and knowledge to resist them.
Yuliya A. Manuylova, senior researcher, endocrinologist, Moscow State University M.V. Lomonosov, Ph.D.
Myth 1 - Women with diabetes should not give birth
Reality You can give birth.
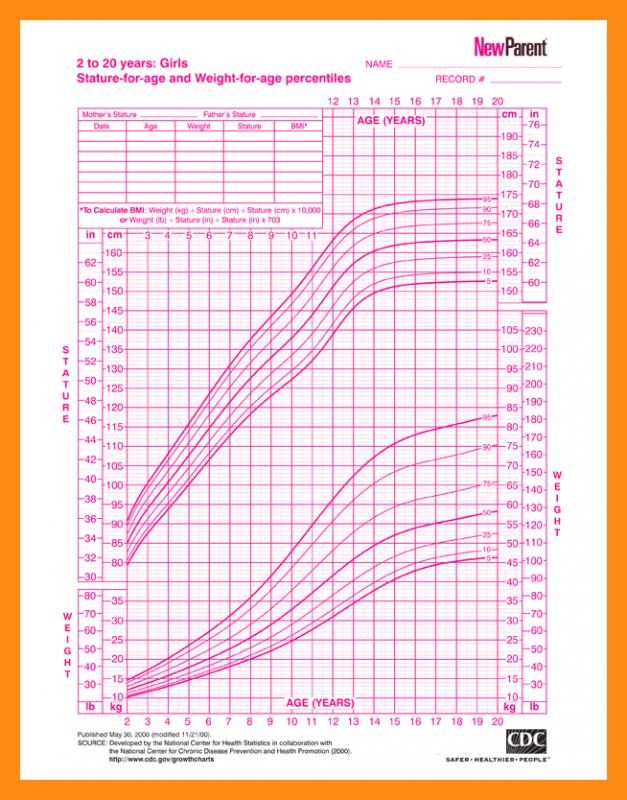
But ... It is necessary to plan pregnancy, have well-compensated diabetes mellitus (ideally, the level of glycated hemoglobin should be less than 6% at least six months before pregnancy). During pregnancy, you will have to carefully control glycemia: measure blood sugar 6-12 times a day, monitor nutrition, take regular tests, and be prepared for frequent correction of insulin doses. Yes, women with diabetes require a lot of effort during pregnancy, but it's worth it. None of the women I know with diabetes regretted pregnancy, all passed this test with dignity and calmness, and some of them more than once.
Myth 2 - Give birth as soon as possible
Reality Everything must be within reason. If a 17-year-old girl is told: “Give birth faster. This is your last chance" - then, probably, this is not entirely true. What is meant in this case: with a long history of diabetes, the risk of diabetic complications is higher, and it is best to carry a pregnancy with no complications or with minimal ones.
Therefore, if a woman is ready for pregnancy, then there is no point in postponing. But it is not necessary to rush into motherhood too much - with good compensation for diabetes, the risk of complications is low, so there is time for reflection and for finding a beloved dad for the unborn baby.
Myth 3 - Parents with type 1 diabetes will definitely develop diabetes in their child
Reality This is the biggest horror story for all mothers. In reality, type 1 diabetes is not hereditary, and the risk of diabetes in a child is only 2% if the mother is ill, 6% if the father is ill, and about 30% if both parents have diabetes.
(from previous myth)
Myth 4 - In a child with a parent with type 1 diabetes, blood sugar should be monitored
Reality As we have already found out, type 1 diabetes very rarely occurs in children, despite the illness of their parents.
What's more, type 1 diabetes is NEVER to be missed, it progresses so fast, with so much deterioration in well-being and so many symptoms that it is impossible not to pay attention to it. Therefore, just poking a child’s finger with a needle and looking at glucose, and even more so taking blood from a vein for glucose once a month, is, in my opinion, a crime. The child is in a lot of pain, he is nervous, his mother is nervous, the procedural nurse is nervous, that is, several people suffer, and this act of vandalism does not carry any information. I have a patient who developed diabetes only 2 or 3 years before pregnancy. Naturally, she was very worried about her daughter and once, at a monthly appointment with a pediatrician, she asked for a referral for a capillary blood test for sugar. Received glucose 6.8 mmol / l. Note that the baby is breastfed, eats every 2-3 hours, that is, the result is not obtained on an empty stomach. And then ... The mother's panic, the doctor's restless state, the child's torment (starvation, pain from venous blood sampling).
As a result, everything ended well, the child does not have diabetes. But all this could have been avoided by simply not needlessly not taking tests.
(continuation of the previous two)
Myth 5 - Do not give sweets to children with type 1 diabetes (and children whose parents have diabetes)
Reality On the one hand, the restriction of children (absolutely any, without reference to diabetes) in sweets is right, it forms a normal eating behavior, maintains an ideal body weight. But diabetes has nothing to do with it. The first type of diabetes does not arise from an excess amount of sweets, and for children with the first type already existing, there is a simple rule: count the amount of XE, prick an adequate dose of insulin and eat a carbohydrate (including dessert). Why am I writing this? Indeed, a REASONABLE restriction in confectionery products is useful. Yes, that's right, but the key word is REASONABLE.
Children who are not allowed sweets suffer, eat them without their parents knowing, inject insufficient doses of insulin (and live with elevated glucose levels), deliberately cause hypoglycemia to get sugar, and with the advent of pocket money and the weakening of supervision, they begin to consume forbidden sweets tons.
Myth 6 - A child with diabetes or a healthy child of parents with diabetes should not be vaccinated
Reality Not only possible, but necessary. A healthy child has no contraindications to vaccinations at all. Moreover, today the main cause of type 1 diabetes is considered to be a viral infection (for example, measles and rubella). That is, vaccination for a child is, to some extent, prevention of diabetes. And a child with diabetes who is not vaccinated according to the schedule has an increased risk of infection, resulting in loss of glucose control (because during any inflammatory disease, the need for insulin increases and, as a result, blood sugar levels).
And we have to fight not only with the serious condition caused by the infection, but also with the decompensation of diabetes.
Myth 7 - A woman with diabetes will have a child with a developmental defect
Reality Indeed, the risk of fetopathy, miscarriage and complications in a woman in labor increases with decompensated diabetes. That is why we are talking about the need to plan and prepare for pregnancy, carefully monitoring your condition for all 9 months. However, if the recommendations of doctors are followed, the pregnancy ends safely.
Myth 8 — If you have diabetes, you cannot give birth on your own, they will do a caesarean section. Very high risk of death in childbirth
Reality In pregnant women with diabetes, the indications for operative delivery are the same as in women without diabetes. That is, if the pregnancy proceeds normally, there are no complications of diabetes or pregnancy that would threaten the normal course of childbirth, a woman with diabetes may well give birth herself.
I’m not even talking about death in childbirth, in principle, anyone can die. The risk in a compensated patient with diabetes is no higher than in another woman.
Myth 9 - Mothers with diabetes should not breastfeed
Reality Of course you can. Yes, it will be necessary to adjust insulin doses, because at this time there is a greater risk of hypoglycemia, but diabetes is by no means a contraindication for breastfeeding.
An ideal picture of the world
Here I have tried to list the main misconceptions of both patients and healthcare professionals regarding the planning and management of pregnancy in patients with diabetes. As a conclusion, I would like to briefly describe how I imagine the ideal picture. So, what would you like to see everywhere:
- Compulsory pregnancy planning for all diabetic women and achievement of carbohydrate metabolism compensation before pregnancy.
- Obtaining adequate information from doctors (not intimidation and insistence on termination of pregnancy, but an explanation of the rules for bearing a healthy child).
- Timely examination and assistance to pregnant women with diabetes.
- Absence of myths that harm the mental and physical health of mothers with diabetes and their children.
Of course, most modern doctors follow the principles of smart strategies, and their patients are happy, socially active, beautiful and healthy. But I really want all women with diabetes to be able to receive adequate care based on world medical experience.
IMPORTANT TO REMEMBER
There is another type of diabetes that occurs only during pregnancy - gestational. And here the situation is reversed: for some reason, this diabetes is not given enough attention, although the risks of adverse events for a pregnant woman and a child with uncompensated gestational diabetes are rather big.
![]()
What the guidelines say:
- Assess venous plasma glucose in the first trimester and perform an oral glucose tolerance test at 24–28 weeks (unless contraindicated).
- A pregnant woman's reference glucose values are lower than those of any other person.
- Gestational diabetes does not require confirmation: the diagnosis is established even with a single detected glycemia that meets the diagnostic criteria.
- When gestational diabetes is detected, treatment is started: diet therapy for a week, if there is no effect, insulin therapy.
What happens in practice:
- The oral glucose tolerance test is not available for all pregnant women.
- Blood glucose levels are not always taken into account.
Even if gestational diabetes is diagnosed, action may not be taken. I was recently approached by a patient from a small town with a diagnosis of gestational diabetes.