Symptoms of unknown pregnancy
False Pregnancy (Pseudocyesis): Causes, Symptoms, and Tests
Written by Stephanie Watson
Reviewed by Traci C. Johnson, MD on August 12, 2022
In this Article
- What Causes False Pregnancy?
- Symptoms of False Pregnancy
- Tests for False Pregnancy
- Treating False Pregnancy
Pregnancy is usually an exciting time for expectant parents. But pregnancy doesn't always end with the anticipated baby. In rare cases, women (or even men) believe they are pregnant, only to find out that their symptoms were caused not by pregnancy, but by something else entirely.
False pregnancy, clinically termed pseudocyesis, is the belief that you are expecting a baby when you are not really carrying a child. People with pseudocyesis have many, if not all, symptoms of pregnancy -- with the exception of an actual fetus. Some men experience a related phenomenon known as couvade, or sympathetic pregnancy. They will develop many of the same symptoms as their pregnant partners, including weight gain, nausea, and backache.
What Causes False Pregnancy?
Only recently have doctors begun to understand the psychological and physical issues that are at the root of pseudocyesis. Although the exact causes still aren't known, doctors suspect that psychological factors may trick the body into "thinking" that it's pregnant.
When a woman feels an intense desire to get pregnant, which may be because of infertility, repeat miscarriages, impending menopause, or a desire to get married, their body may produce some pregnancy signs (such as a swollen belly, enlarged breasts, and even the sensation of fetal movement). The woman's brain then misinterprets those signals as pregnancy, and triggers the release of hormones (such as estrogen and prolactin) that lead to actual pregnancy symptoms.
Some researchers have suggested that poverty, a lack of education, childhood sexual abuse, or relationship problems might play a role in triggering false pregnancy. Having a false pregnancy is not the same as claiming to be pregnant for a benefit (for example, to profit financially), or having delusions of pregnancy (such as in patients with schizophrenia).
Symptoms of False Pregnancy
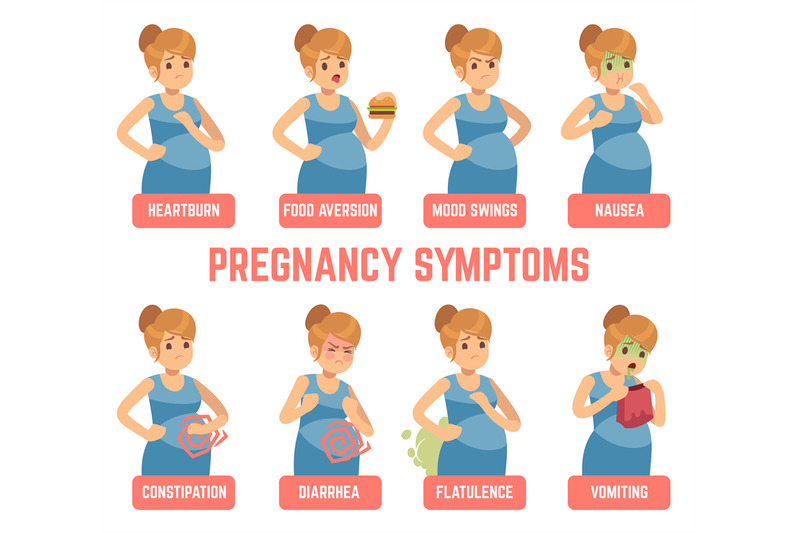
Women with pseudocyesis have many of the same symptoms as those who are actually pregnant, including:
- Interruption of the menstrual period
- Swollen belly
- Enlarged and tender breasts, changes in the nipples, and possibly milk production
- Feeling of fetal movements
- Nausea and vomiting
- Weight gain
These symptoms can last for just a few weeks, for nine months, or even for several years. A very small percentage of patients with false pregnancy will arrive at the doctor's office or hospital with what feels like labor pains.
Tests for False Pregnancy
To determine whether a woman is experiencing a false pregnancy, the doctor will usually evaluate their symptoms, perform a pelvic exam and abdominal ultrasound -- the same tests used to feel and visualize the unborn baby during a normal pregnancy.
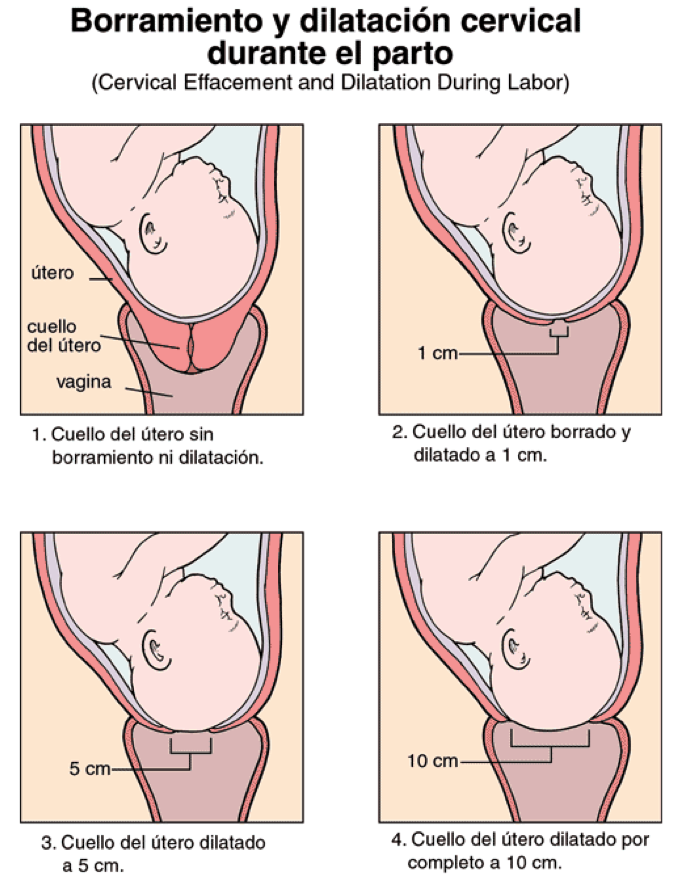
In a case of false pregnancy, no baby will be seen on the ultrasound, and there won't be any heartbeat.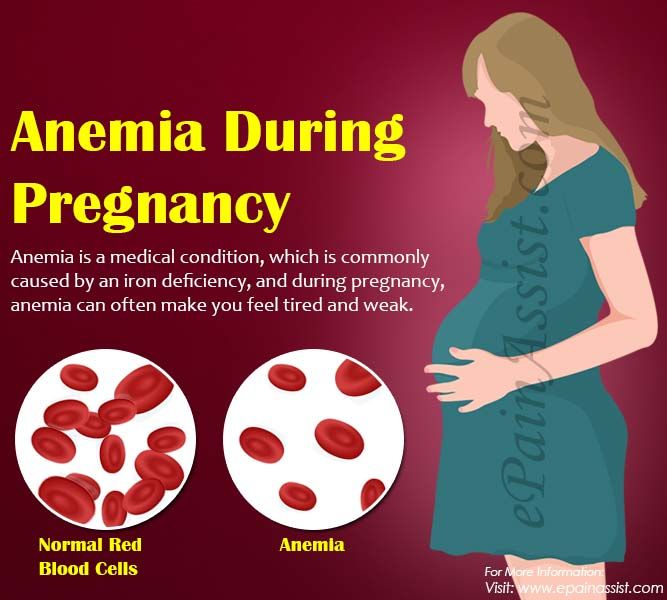 Sometimes, however, the doctor will find some of the physical changes that occur during pregnancy, such as an enlarged uterus and softened cervix. Urine pregnancy tests will always be negative in these cases, with the exception of rare cancers that produce similar hormones to pregnancy.
Sometimes, however, the doctor will find some of the physical changes that occur during pregnancy, such as an enlarged uterus and softened cervix. Urine pregnancy tests will always be negative in these cases, with the exception of rare cancers that produce similar hormones to pregnancy.
Certain medical conditions can mimic the symptoms of pregnancy, including ectopic pregnancy, morbid obesity, and cancer. These conditions may need to be ruled out with tests.
Treating False Pregnancy
When women believe they are pregnant, especially for a period of several months, it can be very upsetting for them to learn that they are not. Doctors need to gently break the news, and provide psychological support, including therapy, to help the patient with pseudocyesis recover from their disappointment.
Can You Be Pregnant and Not Know It?
Written by Kimberly Goad
Reviewed by Dan Brennan, MD on March 31, 2022
You’ve probably heard a story about it at least once: a woman who didn’t know they were pregnant until they went into labor. Your first thought? How is it possible to not know you’re carrying a baby?
Your first thought? How is it possible to not know you’re carrying a baby?
It’s not out of the question, says Michael Cackovic, MD, an OB/GYN at The Ohio State University Wexner Medical Center. “There are women who don’t have routine sex, don’t have routine periods, and don’t regularly see a doctor,” he says. Under those circumstances, it’s possible you could not realize you’re pregnant.
Other women have mental health problems that keep them from recognizing or accepting that they’re going to have a baby.
A few studies have estimated that one in 400 or 500 women are 20 weeks, or about 5 months, into their pregnancy before they realize they are pregnant.
One in 2,500 women make it all the way to labor before they understand they’re going to have a baby. That’s about three times more common than a woman’s chance of having triplets.
How It Happens
A number of things could keep a woman from noticing the changes in their body:
Fear or stress. The thought of becoming a mother is so stressful for some women that they go into deep denial -- so deep that they don’t know they’re pregnant. “Denial is a very powerful defense mechanism, making it possible to talk yourself out of every symptom you may have. The movement in your abdomen is ‘just gas,’ for instance,” Cackovic says.
The thought of becoming a mother is so stressful for some women that they go into deep denial -- so deep that they don’t know they’re pregnant. “Denial is a very powerful defense mechanism, making it possible to talk yourself out of every symptom you may have. The movement in your abdomen is ‘just gas,’ for instance,” Cackovic says.
For example, a teenager may deny or ignore a pregnancy because they don’t want their parents to know they have had sex. A married woman may do the same because they got pregnant by someone other than their partner. Some women may have a denied pregnancy because of a mental health problem, like bipolar disorder or schizophrenia.
No symptoms. For some women, the physical tip-offs of pregnancy, like weight gain, morning sickness, heartburn, or fatigue, don’t happen. Or they’re so mild that a woman just doesn’t notice them. Depending on their body type, “it’s reasonable for a woman to make it to 30 weeks without looking pregnant,” Cackovic says.
Weight changes. If a woman is overweight or their size often goes up and down, they might not notice the extra baby weight. If they’re obese, Cackovic says, they may not “have the physical feelings of being pregnant” that non-obese women feel.
Period problems. A woman can have irregular periods because of stress, some medications (like birth control pills or drugs for epilepsy), obesity, or health problems like polycystic ovary syndrome (PCOS), uncontrolled diabetes, or an eating disorder. So when their period is a no-show, their first thought may not be pregnancy.
They can’t feel the baby move. Usually a mom-to-be will start to feel their baby kicking or rolling between 18 to 20 weeks of pregnancy. But if the placenta happens to be in the front of their uterus, they may not feel those movements, Cackovic says.
Research suggests a well-adjusted woman can have a denied pregnancy and still go on to be a good mother, especially if they’re able to come to grips with the fact that they’re going to have a baby, Cackovic says. For example, some women understand and accept it when they see an ultrasound image of their child. But doctors usually recommend a mental health evaluation to figure out what caused them to deny their pregnancy. It’s also an important step to prevent child abuse and neglect, which are more common after denied pregnancies than normal ones.
For example, some women understand and accept it when they see an ultrasound image of their child. But doctors usually recommend a mental health evaluation to figure out what caused them to deny their pregnancy. It’s also an important step to prevent child abuse and neglect, which are more common after denied pregnancies than normal ones.
Why It Matters
Women can and do deliver healthy babies after a denied pregnancy, Cackovic says. But there are risks to not knowing you’re pregnant:
- You could miss out on the prenatal care that can ensure that you and your baby are healthy, like physical exams, blood tests, and ultrasound scans.
- You won’t know your or your baby’s risk for complications, like anemia, a type of high blood pressure called preeclampsia, gestational diabetes, or birth defects.
- You won’t know it’s time to make healthy changes that help your baby grow and thrive, like getting good nutrition, avoiding alcohol, and stopping certain medications.

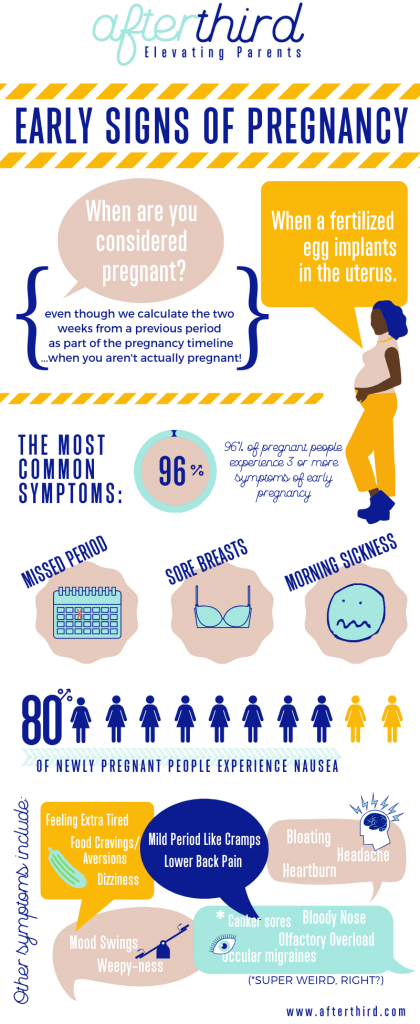
Know the Early Signs
It’s hard to predict who could have a denied pregnancy. But if you think you might miss some of the classic signs, like weight gain or a missing period, you can watch out for other early signals, such as:
- Tender, swollen breasts
- Peeing more often
- Feeling very tired
- Nausea, sometimes with vomiting
- Can’t stand certain foods or smells
Ectopic pregnancy - causes and treatment
If the fixation and subsequent development of the ovum occurs outside the uterus, then the pregnancy is called ectopic (ectopic). It occurs in 2% of all pregnancies. The embryo can be fixed on the ovary, in the abdominal cavity, in the cervix, in the fallopian tubes. An ectopic pregnancy in the early stages is no different from a normal one.
An egg is released from the ovary during ovulation and enters the fallopian tube. Fertilization occurs when a sperm and an egg meet in the ampulla of the fallopian tube. Normally, at the end of the first week after fertilization, the embryo enters the uterine cavity and implantation occurs. A fertilized egg can develop normally only in the uterus.
Normally, at the end of the first week after fertilization, the embryo enters the uterine cavity and implantation occurs. A fertilized egg can develop normally only in the uterus.
Types
- tubal - the embryo develops in the fallopian tubes;
- abdominal - the embryo is attached to the walls of the peritoneum;
- ovarian - the embryo is attached to the walls of the cervix;
- cervical - the embryo is attached to the cavity of the ovary.
Very rare bilateral ectopic pregnancy, as well as heterotopic pregnancy (combination of uterine and ectopic). An ectopic pregnancy of any type is considered a medical emergency.
Let's take a look at tubal pregnancy next, because it is the most common and accounts for 98-99% of all pregnancies outside the uterus.
Signs of ectopic pregnancy
Until the fetal egg overstretches the wall of the fallopian tube, pregnancy is no different from normal and is characterized by standard signs:
- delayed menstruation;
- positive test;
- early toxicosis;
- drowsiness;
- breast enlargement and soreness;
- change in taste preferences.

During menstruation, scanty dark-colored blood discharge is possible. It is impossible for a woman to determine an ectopic pregnancy at home, and diagnostics and specialist advice are required.
Until a certain point, the fertilized egg develops normally. But the embryo grows and it ceases to have enough nutrients. At some point, he ruptures the fallopian tube and bleeding occurs. At the same time, the blood practically does not flow out, only small spotting discharges may appear, the main bleeding occurs in the abdominal cavity.
An ectopic pregnancy may show symptoms after 2 weeks of delayed menstruation. A woman may feel:
- weakness, dizziness;
- pain in rectum radiating to back;
- loss of appetite;
- pain in the lower abdomen, sometimes with nausea and vomiting;
- scanty spotting.
Particular attention should be paid to pain in the lower abdomen. This symptom is also characteristic of a normal uterine pregnancy. But in a normal pregnancy, the pain is temporary. With tubal, as a rule, the pain increases, intensifies and does not stop.
But in a normal pregnancy, the pain is temporary. With tubal, as a rule, the pain increases, intensifies and does not stop.
If you experience any of the symptoms listed, seek medical attention immediately. The condition can worsen sharply at any moment, which threatens the health and life of a woman.
Causes of ectopic pregnancy
Causes are all conditions that disrupt the movement of a fertilized egg into the uterine cavity:
- chronic inflammatory processes of the pelvic organs;
- violation of patency - the appearance of adhesions and scarring of tissues;
- violation of the peristalsis of the fallopian tube
- the exit from the pipe is closed;
- endometrial pathology;
- transferred infectious diseases;
- congenital factor - pipes are twisted and very long;
- single fallopian tube.
Risk factors:
- history of ectopic pregnancy;
- adhesive process in the small pelvis;
- interventions on the fallopian tubes;
- intrauterine contraception;
- surgery;
- pregnancy after prolonged infertility, after IVF procedure;
- anatomical features;
- bad habits;
- age from 35 years;
- hormonal and endocrine disorders.
Diagnosis
It is very difficult to detect a tubal pregnancy during a routine gynecological examination. Methods for diagnosing ectopic pregnancy:
- beta-hCG test is the only biochemical indicator for diagnosing ectopic pregnancy. In a normal course, the increase in hCG should double every 2-3 days. Suspicion will be a sluggish increase in hCG, no more than 1.5 times every 2-3 days. A low rise in beta-hCG may be with an undeveloped uterine or ectopic pregnancy;
- An early ultrasound of an ectopic pregnancy should be transvaginal to determine where the embryo has attached. It is desirable to carry out for 5-7 days after the delay of menstruation.
Blood progesterone testing is not indicated for the diagnosis of tubal pregnancy. Only according to the beta-hCG data, it is impossible to make a diagnosis, it is necessary to do a transvaginal ultrasound.
Complications
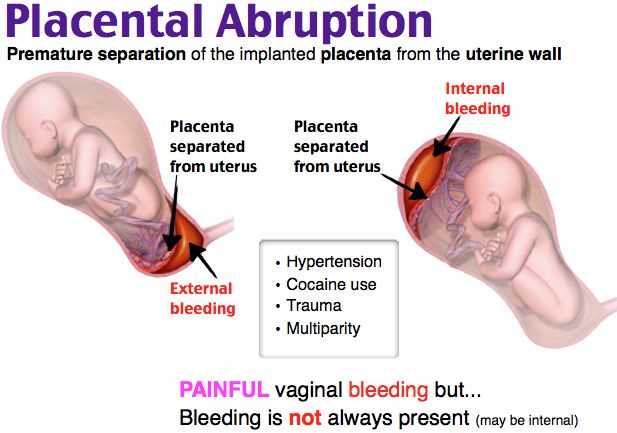
Termination of an ectopic pregnancy usually occurs for 4-6 weeks and develops as a rupture of the tube or as a tubal abortion.
Signs of interruption by type of tube rupture:
- delayed menstruation;
- intra-abdominal bleeding, characterized by a sharp decrease in blood pressure, pallor, cold sweat, dizziness, fainting, nausea, vomiting;
- sharp and very severe pain in the abdomen.
May occur after 6 weeks of pregnancy. An extremely dangerous situation for a woman's life and require immediate surgical intervention.
Signs of interruption by type of tubal abortion:
- delayed menstruation;
- bleeding from labia;
- constant aching, dull pain in the lower abdomen, may radiate to the lower back, groin, rectum.
Tubal abortion proceeds for a long time, without acute manifestations. With detachment of the fetal from the fallopian tube, blood enters the abdominal cavity in small portions and therefore there are no sharp symptoms. On gynecological examination, an increase in the size of the uterus and appendages, pain on palpation of the posterior fornix of the vagina is determined.
What complications can be:
- severe bleeding;
- repeated ectopic pregnancy;
- infertility.
Ectopic pregnancy and consequences
- probability of normal pregnancy and childbirth - about 50%;
- repeated ectopic pregnancy - about 20%;
- 15-20% miscarriages;
- 25% infertility.
Ectopic pregnancy, what treatment is used
If an ectopic pregnancy is suspected, a woman should be urgently hospitalized in a hospital, even if there are no complaints of well-being. The main threat is that the pregnancy can be terminated at any time.
The effectiveness of treatment is determined by timely diagnosis at an early stage and the choice of using laparoscopic access.
In the hospital, after 48-72 hours, repeat ultrasound, determine the level of beta-hCG and conduct a gynecological examination. If the increase in beta-hCG is less than 50% in 48-72 hours and the fetal egg is not detected, then the patient will be shown a diagnostic laparoscopy.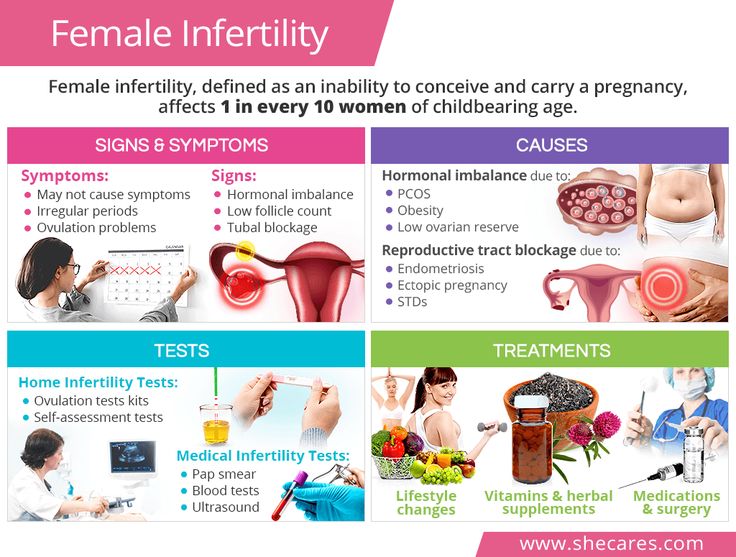 Such diagnostics will help not to wait for the rupture of the tube, blood loss and shock.
Such diagnostics will help not to wait for the rupture of the tube, blood loss and shock.
Currently in Russia, ectopic pregnancy is treated only surgically:
- radical (tubectomy) - removal of the tube along with ectopic pregnancy. It is used for rupture or overstretching of the pipe;
- organ-preserving (tubotomy) - the tube is cut and the fetal egg is removed. The method is used with timely detection and slight stretching of the pipe.
Only surgery can remove a fertilized egg that has attached itself outside the uterine cavity. The most common is laparoscopy. The surgeon removes the fetal egg and partially or completely the fallopian tube through small punctures. After 3 days, the woman is allowed to go home.
Opening of the abdominal cavity is usually used when laparoscopic access is difficult (pronounced adhesive process, a large amount of blood in the abdominal cavity, obesity).
The nature of the operation depends on the condition of the woman, the volume of blood loss, location and size of the ovum.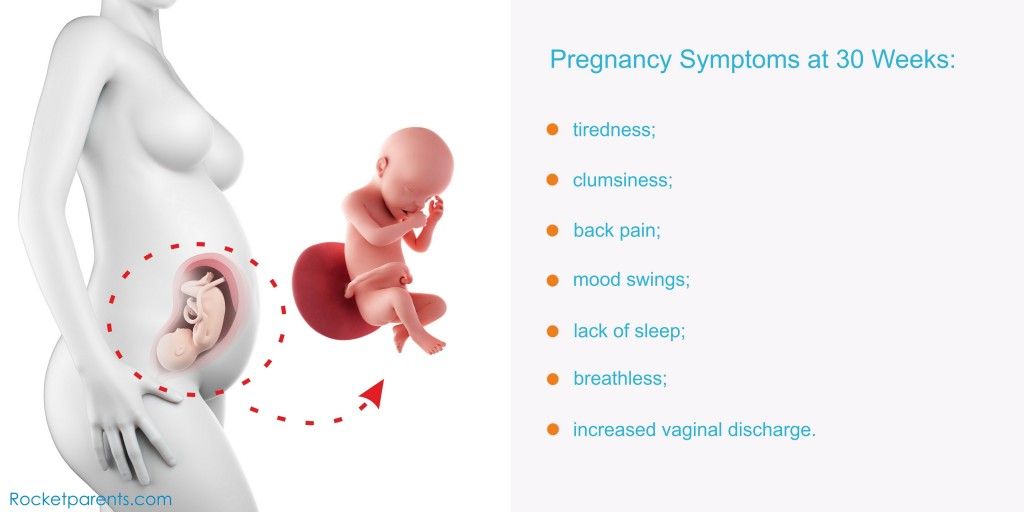 With laparoscopic access, the incidence of recurrent ectopic pregnancy is lower than with laparotomy.
With laparoscopic access, the incidence of recurrent ectopic pregnancy is lower than with laparotomy.
Recovering from an ectopic pregnancy
It is important to have a complete examination to understand the cause of an ectopic pregnancy and eliminate it. Observe physical and sexual rest for at least a month after surgery. Measures should be aimed at restoring reproductive function after surgery:
- prevention of adhesions - physiotherapy, reflexology, injections of longidase, lidase;
- oral contraceptives are recommended for the duration of rehabilitation therapy. As a rule, 6 months after an ectopic pregnancy, you can become pregnant again.
If a tubal pregnancy was diagnosed in time, then the chances of conceiving and carrying a healthy child are quite high. When planning a pregnancy, be sure to consult a doctor.
How to avoid ectopic pregnancy
Prevention involves reducing the likelihood of the causes that lead to the development of ectopic pregnancy:
- timely treatment of inflammatory diseases of the genital organs;
- reliable contraception as abortion prevention;
- use of contraceptives strictly under medical supervision;
- pregnancy planning, complete examination;
- treatment of hormonal disorders.
Regular visits to the gynecologist and examination for various infections are also important. If you suspect pregnancy, contact the MEDICA Fetal Medicine Center, experienced specialists will consult, diagnose and determine the type of pregnancy.
If you suspect pregnancy or you are concerned about a delay, then contact the Medica Fetal Medicine Center, experienced specialists will consult, diagnose and determine the type of pregnancy.
Finding the most effective management for pregnancy of unknown location - NIH study
08/05/2021
Non-developing pregnancy of unknown location - a clinical situation in which the result of a pregnancy test is positive, but using instrumental methods of examination it is impossible to confirm the localization of pregnancy in the uterine cavity or outside it. A study supported by the National Institutes of Health (NIH) assessed the hypothesis that preventive treatment for missed pregnancy of unknown location is a more rational tactic than treating symptoms as they appear.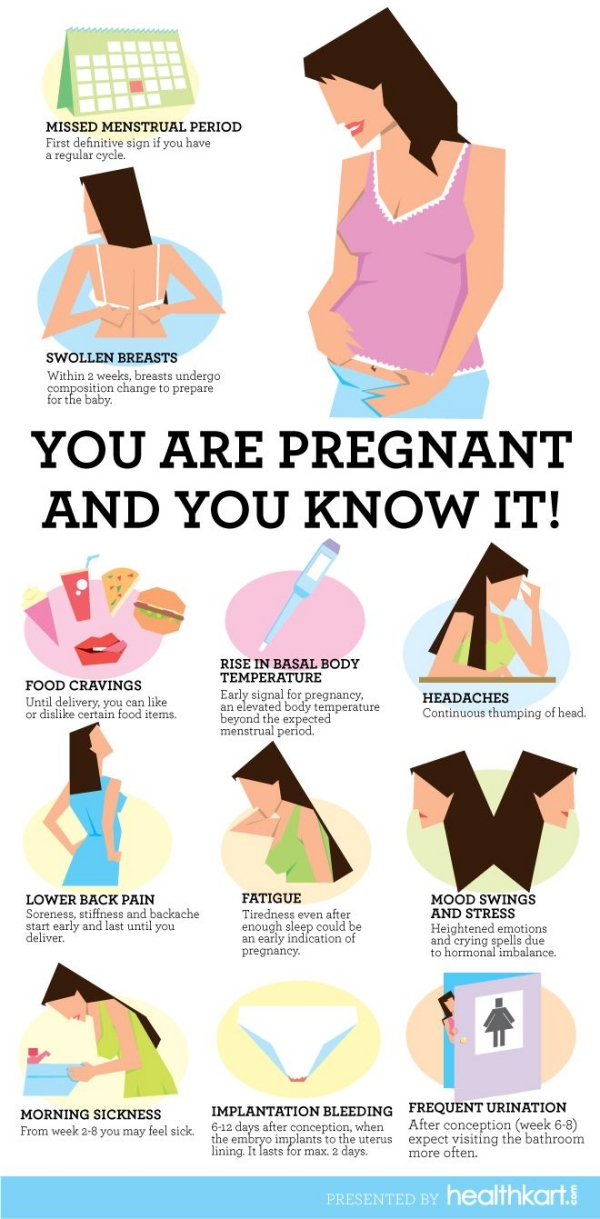 However, both clinical treatment approaches carry similar risks of side effects, mainly vaginal bleeding or when the pregnancy is later determined to be ectopic (pregnancy outside the uterus), fallopian tube rupture.
However, both clinical treatment approaches carry similar risks of side effects, mainly vaginal bleeding or when the pregnancy is later determined to be ectopic (pregnancy outside the uterus), fallopian tube rupture.
If the pregnancy does not develop properly and cannot be visualized using ultrasonography (ultrasound) and other instrumental examination methods, a pregnancy of unknown location is confirmed by the determination of human chorionic gonadotropin (hCG), a hormone secreted by cells that later become the placenta. Treatment is usually offered when hCG levels remain consistently low, indicating a lack of fetal development and persistence of residual cells.
If the pregnancy is later determined to be ectopic, if left untreated, it can be complicated by severe bleeding and maternal death. Similarly, an undeveloped pregnancy of any location can lead to bleeding or scarring of the uterus, which can complicate a subsequent pregnancy.
The study was conducted by Kurt T.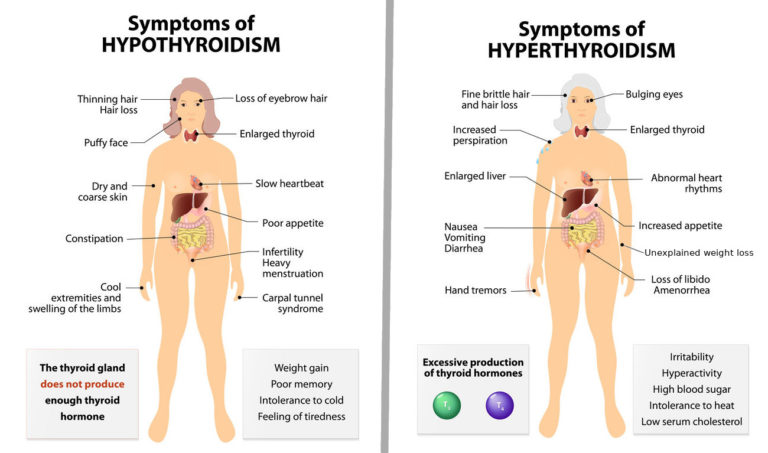 Barnhart, M.D. of the University of Pennsylvania and colleagues. The results are published in the Journal of the American Medical Association. The study was funded by the National Institute of Child Health and Human Development. Eunice Kennedy Shriver (NIH's Eunice Kennedy Shriver National Institute of Child Health and Human Development - NICHD).
Barnhart, M.D. of the University of Pennsylvania and colleagues. The results are published in the Journal of the American Medical Association. The study was funded by the National Institute of Child Health and Human Development. Eunice Kennedy Shriver (NIH's Eunice Kennedy Shriver National Institute of Child Health and Human Development - NICHD).
According to study author Esther Eisenberg, MD, MPH, NICHD Fertility and Infertility Branch, the data show that treatment can be tailored to the wishes and needs of each individual patient.
According to the results of the study, it was found that participants in all study groups rated the treatment received as satisfactory and acceptable.
Little research has been done to date on the most effective treatments for pregnancy of unknown location. Treatment options include the drug methotrexate, curettage of the uterine mucosa, or expectant management—monitoring the patient closely and stopping treatment if no symptoms develop.
The current study included 253 patients. The researchers found that those who received methotrexate with or without uterine curettage recovered faster without the need for additional treatment compared to those in the expectant management group. Of the total number of patients studied, 5 patients underwent surgery for ectopic pregnancy: 2 in the expectant management group, 2 after curettage of the uterine cavity, and 1 received methotrexate.
Patients were randomized to expectant management, uterine curettage followed by methotrexate if needed, or two doses of methotrexate alone. Traditionally, curettage of the uterus is performed to determine the localization of an undeveloped pregnancy. If placental cells are not detected in the uterus, the pregnancy is regarded as ectopic with the further appointment of methotrexate.
Patients could opt out of randomization and choose to participate in a different treatment arm. About 27% abandoned the expectant management, 48% refused to empty the uterus, and 42% abandoned the two-dose regimen.