Baby type 2
Newborn screening information for tyrosinemia, type II | Baby's First Test | Newborn Screening
Follow-Up Testing
Your baby’s doctor may ask you if your baby is showing any of the signs of TYR II (see Early Signs below). If your baby has certain signs, your baby’s doctor may suggest starting immediate treatment.
If your baby’s newborn screening result for tyrosinemia, type II (TYR II) was out of the normal range, your baby’s doctor or the state screening program will contact you to arrange for your baby to have additional testing. It is important to remember that an out-of-range screening result does not necessarily mean that your child has the condition. An out-of-range result may occur because the initial blood sample was too small or the test was performed too early. However, as a few babies do have the condition, it is very important that you go to your follow-up appointment for a confirmatory test. Because the harmful effects of untreated TYR II can occur soon after birth, follow-up testing must be completed as soon as possible to determine whether or not your baby has the condition.
Follow-up testing will involve checking your baby’s urine and blood samples for signs of TYR II. Harmful levels of certain substances build up in the body when a child has an amino acid condition, so measuring the amounts of these substances in your baby’s body can help doctors determine if your baby has a condition. A very high amount of tyrosine in the blood might indicate that your baby has TYR II.
About Tyrosinemia, Type II
Early Signs
There are three types of tyrosinemia (I, II, and III). Tyrosinemia, type II (TYR II) tends to affect the skin and eyes. Signs of TYR II usually begin in the first year of life. These signs include:
- Increased tear production
- Sensitivity to light (called photophobia)
- Eye redness
- Skin lesions on the hands and feet
- Behavior changes
- Poor coordination
Many of these signs may occur when your baby eats foods that their body cannot break down. They can be triggered by long periods of time without eating, illnesses, and infections.
If your baby shows any of these signs, be sure to contact your baby’s doctor immediately.
Treatment
Dietary Treatments
Your baby may need to be on a restricted diet in order to avoid certain proteins that their body cannot break down. Babies with tyrosinemia, type II (TYR II) may need to limit certain amino acids (phenylalanine, tyrosine, and methionine) in their diet. Amino acids are the building blocks of protein. These are all found in many proteins, and phenylalanine is also found in artificial sweeteners.
Special foods and formulas for children with TYR II are available. These formulas will likely need to be continued through adulthood.
Medications
Your baby’s doctor might prescribe a drug called NTBC, which helps lower amino acid levels in the blood. Everyone has some amino acids in their blood, but the high levels associated with TYRII can be toxic.
Expected Outcomes
Children who receive early and ongoing treatment for tyrosinemia, type II (TYR II) can have healthy growth and development. This is why newborn screening for TYR II is so important.
This is why newborn screening for TYR II is so important.
About half of the individuals who have been diagnosed with TYR II have intellectual disabilities. Early treatment can reduce the risk of developing intellectual disabilities.
Causes
When we eat food, enzymes help break it down. Some enzymes help break down proteins into their building blocks, called amino acids. Other enzymes break down these amino acids. In tyrosinemia, type II (TYR II), the enzyme tyrosine aminotransferase (TAT) is not working correctly.
TAT’s job is to break down the amino acid tyrosine. Babies with TYR II either make non-working or do not make enough TAT. When TAT is not working correctly, the body cannot break down tyrosine. This causes tyrosine and other amino acids (methionine and phenylalanine) to build up in the body, which can be toxic.
TYR II is an autosomal recessive genetic condition. This means that a child must inherit two copies of the non-working gene for TYR II, one from each parent, in order to have the condition. The parents of a child with an autosomal recessive condition each carry one copy of the non-working gene, but they typically do not show signs and symptoms of the condition. While having a child with TYR II is rare, when both parents are carriers, they can have more than one child with the condition. Learn more about autosomal recessive inheritance.
The parents of a child with an autosomal recessive condition each carry one copy of the non-working gene, but they typically do not show signs and symptoms of the condition. While having a child with TYR II is rare, when both parents are carriers, they can have more than one child with the condition. Learn more about autosomal recessive inheritance.
Support for Tyrosinemia, Type II
Support Services
Support groups can help connect families who have a child or other family member affected with tyrosinemia, type II with a supportive community of people who have experience and expertise in living with the condition. These organizations offer resources for families, affected individuals, health care providers, and advocates:
- Intermountain PKU and Allied Disorders (Facebook page)
- Network of Tyrosinemia Advocates
- Tyrosinemia Society
Accessing Care
Work with your baby’s doctor to determine the next steps for your baby’s care. Your baby’s doctor may help you coordinate care with a doctor who specializes in metabolism, a dietician who can help plan your child’s specialized diet, and other medical resources in your community. Depending on the symptoms your baby experiences, baby’s doctor may work with other doctors who specialize in treating the eyes or skin. Some children with tyrosinemia, type II (TYR II) have developmental delays. If you think that your baby is not meeting their developmental milestones, ask your baby’s doctor about the next steps in accessing a developmental evaluation and care.
Your baby’s doctor may help you coordinate care with a doctor who specializes in metabolism, a dietician who can help plan your child’s specialized diet, and other medical resources in your community. Depending on the symptoms your baby experiences, baby’s doctor may work with other doctors who specialize in treating the eyes or skin. Some children with tyrosinemia, type II (TYR II) have developmental delays. If you think that your baby is not meeting their developmental milestones, ask your baby’s doctor about the next steps in accessing a developmental evaluation and care.
Because TYR II is a genetic condition, you may want to talk with a genetics specialist. A genetic counselor or geneticist can help you understand the causes of the condition, discuss genetic testing for TYR II, and understand what this diagnosis means for other family members and future pregnancies. Speak with your baby’s doctor about getting a referral. The Clinic Services Search Engineoffered by the American College of Medical Genetics and Genomics (ACMG) and the Find a Genetic Counselor tool on the National Society of Genetic Counselors (NSGC) website are two good resources for you or your baby's health care provider to use to identify local specialists.
Families' Experiences
At this time we have not located a family story for this particular condition. If your family is affected by tyrosinemia, type II (TYR II) and you would like to share your story, please contact us so other families may benefit from your experience.
References & Sources
Visit OrphaNet for more information on tyrosinemia, type II
Visit MedlinePlus Genetics for more condition information
Visit Genetic and Rare Diseases Information Center (GARD) for more information on tyrosinemia, type II
Visit West Virginia's Office of Maternal and Child Health website for more information on tyrosinemia
Visit Genetics Home Reference from the National Library of Medicine for more information on the TAT gene
Your input helps us improve the site for parents and practitioners. Leave us feedback about this page.
Was this page helpful?
Your input helps us improve the site for parents and practitioners. Leave us feedback about this page.
Leave us feedback about this page.
We're sorry to hear that. How can we do to improve it?
Mucopolysaccharidosis Type-II | Baby's First Test | Newborn Screening
Follow-Up Testing
Your baby’s doctor may ask you if your baby is showing any of the signs of mucopolysaccharidosis type II (see Early Signs below). If your baby has certain signs, your baby’s doctor may suggest starting immediate treatment.
If your baby’s newborn screening result for mucopolysaccharidosis type II (MPS II) was out of the normal range, your baby’s doctor or the state screening program will contact you to arrange for your infant to have additional testing. It is important to remember that an out-of-range screening result does not necessarily mean that your child has the condition. An out-of-range result may occur because the initial blood sample was too small or the test was performed too early. However, as a few babies do have the condition, it is very important that you go to your follow-up appointment for a confirmatory test. Because the harmful effects of untreated MPS II can occur soon after birth, follow-up testing must be completed as soon as possible to determine whether or not your baby has a condition.
Because the harmful effects of untreated MPS II can occur soon after birth, follow-up testing must be completed as soon as possible to determine whether or not your baby has a condition.
Follow-up testing will involve checking your baby’s blood and urine for signs of MPS II. When a child has a lysosomal storage disorder, harmful amounts of certain substances build up in the body and enzymes that help the body breakdown sugars are either missing or have reduced activity. Measuring the amounts of these substances in your baby’s body can help doctors determine if your baby has a condition. High levels of sugars called glycosaminoglycans in the urine or deficient activity of the enzyme, iduronate sulfatase (I2S), in the blood may indicate that your baby has MPS II. Your baby’s doctor may also want to confirm the diagnosis with clinical genetic testing.
About Mucopolysaccharidosis Type-II
Early Signs
The age of onset and severity of mucopolysaccharidosis type II (MPS II) differ depending on the form. Signs of severe MPS II usually begin between ages two and four and progress more rapidly than in attenuated MPS II. Individuals with the attenuated form of MPS II usually do not develop signs until age later in childhood, or even adolescence.
Signs of severe MPS II usually begin between ages two and four and progress more rapidly than in attenuated MPS II. Individuals with the attenuated form of MPS II usually do not develop signs until age later in childhood, or even adolescence.
Early signs of MPS II:
- Distinctively large facial features (full lips, large rounded cheeks, broad nose, enlarged tongue)
- Enlargement of vocal cords causing deep, hoarse voice
- Frequent upper respiratory infections
- Short pauses in breathing during sleep (sleep apnea)
- Large head (macrocephaly)
- Swollen abdomen (due to enlarged liver and spleen)
- Soft out-pouching around belly-button (umbilical hernia) or lower abdomen (inguinal hernia)
- Thick, non-stretchy skin
- Pebble-like white growths on back and upper arms
- Hearing loss
- Frequent ear infections
- Poor vision
- Short stature
- Joint stiffness (contractures)
- Severe intellectual disability
- Loss of basic skills, functions, and intelligence (developmental regression)
- Seizures
If your baby shows any of these signs, be sure to contact your baby’s health care provider immediately.
Treatment
There are several treatments your baby’s health care provider may recommend to address the signs of mucopolysaccharidosis type II (MPS II) and help your baby live a healthier life.
Enzyme Replacement Therapy (ERT)
Enzyme replacement therapy (ERT) can be an effective treatment for symptoms of MPS II that do not involve the central nervous system (the brain and spinal cord). This treatment aims to supplement the enzymes that are present at low levels in your baby’s lysosomes.
Therapies
Physical therapy is a very important part of treating the signs and symptoms of MPS II. Consistent physical therapy early on can help preserve mobility and lessen pain and joint stiffness. Some children also may require developmental or occupational therapy to help reach and retain milestones.
Surgeries
As your child grows, your child’s health care provider may recommend surgeries to improve quality of life. Removal of the tonsils and adenoids and insertion of ventilating tubes can prevent some upper respiratory infections and may reduce hearing loss. In children with attenuated to severe MPS II who develop a build-up of fluid in the brain (hydrocephaly), a surgery to relieve the pressure inside the skull may be recommended. Other surgeries would not take place until later in life, if at all. Joint replacement surgery and surgery to treat carpal tunnel syndrome can improve mobility and lessen pain. Heart valve replacement may prevent later heart complications.
In children with attenuated to severe MPS II who develop a build-up of fluid in the brain (hydrocephaly), a surgery to relieve the pressure inside the skull may be recommended. Other surgeries would not take place until later in life, if at all. Joint replacement surgery and surgery to treat carpal tunnel syndrome can improve mobility and lessen pain. Heart valve replacement may prevent later heart complications.
Diet
A dietician can help you create a nutrition plan to help your baby control diarrhea and constipation, which may occur in those with severe MPS II. There is no diet that can prevent the storage of GAGs because they are actually created by the body.
Expected Outcomes
For some babies with MPS II, detecting the condition early and beginning proper treatment may help prevent or delay some of the severe health outcomes associated with the condition. This is why newborn screening for MPS II is so important.
Though treatment may improve the length and quality of life for children with MPS II, those affected with the severe form often die before reaching their mid-teens from heart disease or airway obstruction. Those with the attenuated form usually live into adulthood, although they may have a shortened lifespan.
Those with the attenuated form usually live into adulthood, although they may have a shortened lifespan.
Causes
Structures called lysosomes are the recycling centers within our cells. Lysosomes contain enzymes that help the cell breakdown and reuse certain materials from the foods we eat. Some enzymes help the lysosome breakdown complex sugars, specifically. One of these enzymes is called iduronate 2-sulfatase (I2S).
If your baby has Mucopolysaccharidosis type II (MPS II), their body is missing or making non-working copies of I2S enzymes. When these enzymes are not working correctly, your baby’s body cannot break down large sugar molecules called glycosaminoglycans (GAGs) into smaller components. This causes sugar molecules and other harmful substances to build up in cells throughout the body, resulting in the many signs and symptoms of MPS II.
MPS II is an X-linked recessive condition. This means a male must inherit one copy of the non-working gene from his mother to have the condition. Although rare, females have been diagnosed with MPS II. A female must inherit two copies of the non-working gene, one from each parent, in order to have the condition. In X-linked conditions, the gene is carried on the X sex chromosome, and the condition generally affects males. While having a child with MPS II is rare, when one or both parents carry the non-working gene for the condition, they can have more than one child with the condition. Learn more about X-linked recessive inheritance.
Although rare, females have been diagnosed with MPS II. A female must inherit two copies of the non-working gene, one from each parent, in order to have the condition. In X-linked conditions, the gene is carried on the X sex chromosome, and the condition generally affects males. While having a child with MPS II is rare, when one or both parents carry the non-working gene for the condition, they can have more than one child with the condition. Learn more about X-linked recessive inheritance.
Support for Mucopolysaccharidosis Type-II
Support Services
Support groups can help connect families who have a child or other family member affected with mucopolysaccharidosis type II with a supportive community of people who have experience and expertise in living with the condition. These organizations offer resources for families, affected individuals, health care providers, and advocates.
- National MPS Society
- Canadian Society for Mucopolysaccharide and Related Diseases, Inc.

- Society for Mucopolysaccharide Diseases
Accessing Care
Work with your baby’s health care provider to determine the next steps for your baby’s care. Your baby’s doctor may help you coordinate care with a dietician or nutritionist, physical therapists, neurologists, physicians that specialize in metabolism, cardiology, and pulmonology, and other medical resources in your community. Some children with mucopolysaccharidosis type II (MPS II) have developmental delays. If you think that your baby is not meeting their developmental milestones, ask your baby’s doctor about the next steps in accessing a developmental evaluation and care.
Because MPS II is a genetic condition, you may want to talk with a genetics specialist. A genetic counselor or geneticist can help you understand the causes of the condition, discuss genetic testing for MPS II, and understand what this diagnosis means for other family members and future pregnancies. Speak with your baby’s doctor about getting a referral. The Clinic Services Search Engine offered by the American College of Medical Genetics and Genomics (ACMG) and the Find a Genetic Counselor tool on the National Society of Genetic Counselors (NSGC) website are two good resources for you or your baby's health care provider to use to identify local specialists.
The Clinic Services Search Engine offered by the American College of Medical Genetics and Genomics (ACMG) and the Find a Genetic Counselor tool on the National Society of Genetic Counselors (NSGC) website are two good resources for you or your baby's health care provider to use to identify local specialists.
Families' Experiences
Caleb is a happy, energetic boy living with MPS II. Read about Caleb and how enzyme replacement therapy has helped him live a more normal life.
The MPS Society (UK) gathers stories about families affected by MPS II and related disorders. Read them here.
References & Sources
Visit GeneReviews for more information on MPS II
Visit MedlinePlus Genetics for more condition information
Your input helps us improve the site for parents and practitioners. Leave us feedback about this page.
Was this page helpful?
Your input helps us improve the site for parents and practitioners.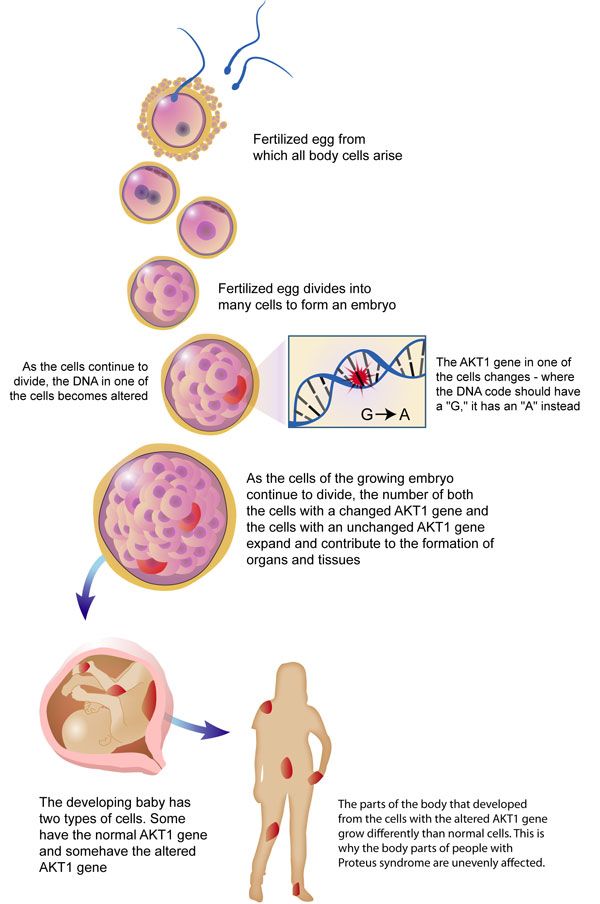 Leave us feedback about this page.
Leave us feedback about this page.
We're sorry to hear that. How can we do to improve it?
Temperament of the child - types of temperament in children
Problem with an asterisk. Given: a pair of parents and two same-sex children. Parents are the same, conditions and upbringing are the same, so why are children so different?
For example, they did not buy another toy in the store. The older child took it for granted and after a while forgot it, and the younger one screams and rolls on the floor due to the parents' refusal.
Parents are perplexed, they say, how is it that the eldest son was not like that at all.
The answer lies in the type of child's temperament, which just manifests itself in atypical situations. The answer to our problem: the eldest child is sanguine, the youngest is choleric.
What is temperament? What is the difference between temperament and character?
Temperament is an invariable innate feature of people, responsible for the manifestation of emotions and energy.
Temperament is often confused with character, but these are fundamentally different concepts:
- Character is formed by the environment and circumstances, temperament is a given from birth.
- Temperament appears immediately. About what character the baby has, you can find out in a couple of years.
- Temperament influences the development of certain character traits (for example, sociability). But thanks to the character, you can learn to restrain some of the unfavorable manifestations of temperament.
- Character may change throughout life, but temperament may not.
Types of temperament in children
Hippocrates spoke about temperament for the first time. He singled out four types depending on which "vital juices" in a person are more:
- if the blood is sanguine;
- red-yellow bile - choleric;
- mucus - phlegmatic;
- black bile - melancholic.
And although ideas about the cause of temperament have changed, the names given by Hippocrates have remained.
- Sanguine. Children of this type of temperament will stick with conversations to everyone and on any occasion. Sanguine people never sit still. Their games are often active and change as quickly as the mood of little fidgets.
- Choleric. Choleric children are not subject to their own emotions, which break out of them and are always visible to others. Choleric people are just as active and sociable as sanguine people. They love to lead and direct.
- Phlegmatic. Calm and balanced phlegmatic people are never in a hurry, they are very slow. Determined - if they are passionate about something, they will try to find out everything about it. They can be entrusted with painstaking work - they will do it in the best possible way. Always follow orders. Before making friends with someone, they look closely.
- Melancholic. Vulnerable and sensitive children are often thoughtful and in a sad mood.
 They are indecisive and lack of initiative, new acquaintances are given to them with difficulty. It takes a long time to get used to the new team.
They are indecisive and lack of initiative, new acquaintances are given to them with difficulty. It takes a long time to get used to the new team.
Why determine the type of child's temperament?
Why do some children quickly get used to an unfamiliar environment and find entertainment for themselves, while others do not leave their parents a single step?
Temperament controls the type of thinking and the output of the child's emotions. Therefore, sanguine and choleric people will quickly get used to a new place, and phlegmatic and melancholic people will adapt for a long time.
Parents should determine the child's temperament in order to understand and accept it. For example, instead of making a scandal and rushing a phlegmatic child to go for a walk because of long preparations.
In childhood, it is possible to correct the manifestations of temperament and teach the child to interact with the outside world within the framework of his innate characteristics.
Parents, having learned which levers to press, will be able to interest the child, develop his talents, calculate physical and mental stress.
How to determine the temperament of a child?
To determine the type of child's temperament, answer the questions. Don't forget to check your answer options.
1. How does the child react to the comments of caregivers and parents?
A. Listens and agrees with the remarks, but soon forgets about the said remark.
B. He reacts violently, makes excuses and tries to explain the reasons for the misconduct.
V. Listens with complete equanimity. He admits he was wrong.
D. Gets upset, worries, may be offended and cry.
2. The children started a team game “fun starts”. Characteristic behavior for your baby:
A. Holds himself confidently, supports everyone, prompts.
B. He pushes everyone, shouts, points out mistakes.
B. Thinks about actions and calmly performs.
D. He is insecure, very agitated. May refuse to play.
3. In an argument with children, your child:
A. Lets others speak, but defends his own opinion.
B. Considers only his own opinion to be true, does not allow others to say, interrupts.
B. Speaks confidently, without superfluous emotions, consistent in presenting his thoughts.
D. Does not dare to express an opinion.
4. How quickly does fatigue appear in a child?
A. Can run all day. Tired only in the evening.
B. Sometimes very active, and then suddenly tired.
V. Not very mobile, medium energy. Rarely complains of fatigue.
D. Gets tired quickly.
Gets tired quickly.
5. What emotions does a child experience if he knows that he will have to enter a new team (class, group, team)?
А. Looking forward to new interesting acquaintances.
B. Shows excitement, agitated.
W. Does not show concern, seems indifferent.
D. Worries a lot, wants to stay at home.
6. Features of your baby's speech:
А.
B. Speaks in raised tones, speech is broken and fast.
B. Carefully chooses words, speaks measuredly.
D. Speaks quietly, sometimes inaudibly, allows himself to be interrupted.
7. In a children's company your child:
A. A recognized leader, joker.
B. Tries to take the lead, gets irritated when it fails.
V. Medium roles.
Medium roles.
D. Listens to the majority.
8. When your child is left without company, he...
A. Complains of being bored.
B. Finds things to do quickly.
V. Plays quietly and peacefully.
D. Feels great. Finds something to his liking.
9. What kind of games does your baby prefer?
A. Outdoor team games.
B. Noisy with pampering.
B. Logic.
D. Board games without competition, noisy - only with close people.
10. Your child is visiting someone or visiting a doctor for the first time. How does he behave?
A. Soon adapts, gets to know everyone with interest, behaves lively.
B. Begins to get nervous, is in an excited state.
V. Serenely looks at the new surroundings and furnishings.
Serenely looks at the new surroundings and furnishings.
G. Shy, keeps only close to relatives, does not make contact.
Count the number of answers. What are the most?
If " A " prevails, your child's temperament is close to the sanguine type. If there are more answers « B ”, most likely, your baby is a choleric, “ B ” is a phlegmatic and “ D ” is a melancholic.
Choleric child
Choleric child fills the whole space, as he is very active and noisy. Quickly lights up with an idea, but can quit what he started if he does not succeed. Often children of this type of temperament speak quickly and abruptly, because they have no time.
Because of the haste in the classroom, they can make mistakes, although they know the correct answer.
Positive aspects of choleric people: activity, sociability, purposefulness.
Negative aspects of choleric people: excessive emotionality, hysteria, irritability, rejection of criticism.
How to help:
Parents need to teach their children to identify their emotions. Due to the fact that the emotions overwhelm the choleric, he cannot cope with them. Ask the child what he feels now, and then name this emotion “you are angry, baby”, “you are annoyed because it didn’t work out the first time, let’s try again.” The child will learn to understand their own emotions and control them.
Sanguine child
Children of this type of temperament are also active and sociable, but, unlike choleric, they are also balanced. They easily find a common language with everyone, are recognized leaders and ringleaders.
Sanguine people often break discipline in the classroom.
Positive aspects of sanguine people: cheerfulness, openness, versatility
Negative aspects of sanguine people: quick jumping from one to another, superficiality.
How to help:
Parents need to teach their child to finish what they start. Teach your child to plan their day. Show that a big goal is achieved by persistent small steps. Praise the child, but let the praise be well-deserved.
Teach your child to plan their day. Show that a big goal is achieved by persistent small steps. Praise the child, but let the praise be well-deserved.
Phlegmatic child
Emotional recluse, calm, calm and very kind. Children with this type of temperament are balanced, but do not know how to share their experiences with others.
The slow pace of work does not allow them to complete assignments in class on time.
Positive aspects of phlegmatic people: constancy, purposefulness, good nature.
Negative aspects of phlegmatic people: stubbornness, slowness, lack of emotion.
How to help:
Parents need to teach their child to show and express their feelings. You can entrust your child with taking care of a pet.
Many are annoyed by the slowness of the baby. In fact, this is how his restraint is manifested. It is in the power of parents to develop the speed of the reaction of the child and teach him to cope with some things faster.
Melancholic child
Timid and shy kids who get lost when they drop out of their usual life. They are very vulnerable and always worry too much. But, unlike choleric children, melancholic children cannot bring their feelings out and suffer greatly about this.
It is very difficult for children of this temperament to concentrate, so they are distracted in class.
Positive aspects of melancholic people: accuracy, sincerity, obligation, diligence, responsibility.
Negative aspects of melancholic people: anxiety, isolation, indecision, slowness.
How to help:
This type of child, like no other, needs the approval and praise of adults. They are very insecure, they believe that they have only flaws. The task of parents is to teach the melancholic to believe in himself and in his success.
Temperament is never found in its pure form, however, by looking closely at the child, you can determine the leading type. Adhere to raising a child according to the type of temperament, smoothing out sharp corners and honing the positive sides. And most importantly - love your child, and then a harmonious and loving person will grow out of him.
Adhere to raising a child according to the type of temperament, smoothing out sharp corners and honing the positive sides. And most importantly - love your child, and then a harmonious and loving person will grow out of him.
Emotional intelligence for children
We introduce children to the types of emotions, how to manage them and how to express themselves in teamwork, through situational games
learn more
Autism spectrum disorders in children
home
Articles
Diseases
Alpatsky Dmitry Alexandrovich Neurologist, epileptologist, EEG doctor
12/07/2015
Often, mothers come to the doctor with complaints of delayed speech development in a child. But in some children, with a close look, the specialist, in addition to this, sees the features of the child's behavior that differ from the norm and are alarming .
Consider a clinical example:
Boy S. Age 2 years 9 months. According to the mother, the child's vocabulary is no more than 20 separate words, consisting of two or three syllables. There are no phrases. Mom says that the child often has tantrums, is restless, it is difficult to fall asleep. The child's mother has no other complaints. On examination, the doctor notices that the child does not look into the eyes, is constantly in motion, reacts with a cry if something is not given or forbidden to him. You can calm the child only by giving him a mobile phone or tablet. Shows interest not in children's toys, but more in shiny pieces of furniture and interior. Starting to play something, quickly loses interest and switches to something else. Asking the mother, it turns out that the child is very selective in food. Not accustomed to the potty, defecation only in a diaper in a standing position. Difficulty falling asleep and waking up during sleep. The child underwent Electroencephalography and consultations with a clinical psychologist and a speech therapist.
Age 2 years 9 months. According to the mother, the child's vocabulary is no more than 20 separate words, consisting of two or three syllables. There are no phrases. Mom says that the child often has tantrums, is restless, it is difficult to fall asleep. The child's mother has no other complaints. On examination, the doctor notices that the child does not look into the eyes, is constantly in motion, reacts with a cry if something is not given or forbidden to him. You can calm the child only by giving him a mobile phone or tablet. Shows interest not in children's toys, but more in shiny pieces of furniture and interior. Starting to play something, quickly loses interest and switches to something else. Asking the mother, it turns out that the child is very selective in food. Not accustomed to the potty, defecation only in a diaper in a standing position. Difficulty falling asleep and waking up during sleep. The child underwent Electroencephalography and consultations with a clinical psychologist and a speech therapist. Based on the results of the diagnosis and the clinical picture, the diagnosis was made - Autism Spectrum Disorder.
Based on the results of the diagnosis and the clinical picture, the diagnosis was made - Autism Spectrum Disorder.
Autism Spectrum Disorders (ASD) are complex disorders of mental development that are characterized by social maladaptation and inability to social interaction, communication and behavioral stereotypy (multiple repetitions of monotonous actions).
Back in the middle of the last century, autism was a fairly rare disease. But over time, more and more children suffering from this disorder began to appear. Statistics show that the incidence of ASD in children over the past 30-40 years in countries where such statistics are carried out has risen from 4-5 people per 10,000 children to 50-116 cases per 10,000 children. At the same time, boys are more susceptible to this disease than girls (approximately 4:1 ratio).
Causes of RAS.
All over the world, until today, scientists studying the causes of autism have not come to a consensus. Many assumptions are put forward. Among the possible factors for the appearance of this disorder in children are some hypotheses:
Many assumptions are put forward. Among the possible factors for the appearance of this disorder in children are some hypotheses:
- genetic predisposition hypothesis
- a hypothesis based on disorders of the development of the nervous system (autism is considered as a disease caused by disorders of brain development in the early stages of a child's growth).
- hypotheses about the influence of external factors: infections, chemical effects on the mother's body during pregnancy, birth trauma, congenital metabolic disorders, the influence of certain drugs, industrial toxins.
But whether these factors really can lead to the appearance of autism in children has not yet been clarified.
Features of the mental development of children with ASD.
To understand and recognize the presence of autism in a child, parents need to carefully monitor the behavior of the child, notice unusual signs that are not characteristic of the age norm. Most often, these signs can be detected in children under the age of 3 years.
Most often, these signs can be detected in children under the age of 3 years.
Childhood autism is considered as a developmental disorder that affects all areas of the child's psyche: intellectual, emotional, sensitivity, motor sphere, attention, thinking, memory, speech.
Disorders of speech development : at an early age, the absence or weak cooing and babbling can be noted. After a year, it becomes noticeable that the child does not use speech to communicate with adults, does not respond to a name, and does not follow verbal instructions. By the age of 2, children have a very small vocabulary. By the age of 3 they do not build phrases or sentences. At the same time, children often stereotypically repeat words (often incomprehensible to others) in the form of an echo. Some children have a lack of speech development. For others, speech continues to develop, but there are still communication impairments. Children do not use pronouns, address, speak about themselves in the third person. In some cases, there is a regression of previously acquired speech skills.
In some cases, there is a regression of previously acquired speech skills.
Difficulties in communication and lack of emotional contact with others: Such children eschew tactile contact, almost completely absent eye contact, there are inadequate facial reactions and difficulties in using gestures. Children most often do not smile, do not reach out to their parents and resist attempts by adults to take them in their arms. Children with autism lack the ability to express their emotions, as well as to recognize them in the people around them. There is a lack of empathy for other people. The child, along with the adult, does not focus on one activity. Children with autism do not make contact with other children or avoid it, they find it difficult to cooperate with other children, most often they tend to retire (difficulties in adapting to the environment).
H disruption of exploratory behavior: children are not attracted by the novelty of the situation, they are not interested in the environment, they are not interested in toys. Therefore, children with autism most often use toys in an unusual way, for example, a child may not roll the whole car, but turn one of its wheels monotonously for hours. Or not understanding the purpose of the toy to use it for other purposes.
Therefore, children with autism most often use toys in an unusual way, for example, a child may not roll the whole car, but turn one of its wheels monotonously for hours. Or not understanding the purpose of the toy to use it for other purposes.
Eating disorders : a child with autism can be extremely selective in the offered products, food can cause the child to be disgusted, dangerous, often children begin to sniff food. But along with this, children may try to eat an inedible thing.
Violation of self-preservation behavior: due to a large number of fears, the child often finds himself in a situation that is dangerous for himself. The cause can be any external stimulus that causes an inadequate reaction in the child. For example, a sudden noise may cause a child to run in a random direction. Also, the reason is ignoring real threats to life: a child can climb very high, play with sharp objects, cross the road without looking.
Disturbance of motor development: as soon as the child begins to walk, he is noted for clumsiness. Also, some children with autism are inherent in walking on their toes, a very noticeable violation of the coordination of hands and feet. It is very difficult for such children to teach everyday actions, it is rather difficult for them to imitate. Instead, they develop stereotypical movements (performing the same actions for a long time, running in circles, swinging, flapping “like wings” and circular movements with their arms), as well as stereotypical manipulations with objects (tweaking small details, lining them up). Children with autism have significant difficulty in learning self-care skills. Pronounced motor awkwardness.
Also, some children with autism are inherent in walking on their toes, a very noticeable violation of the coordination of hands and feet. It is very difficult for such children to teach everyday actions, it is rather difficult for them to imitate. Instead, they develop stereotypical movements (performing the same actions for a long time, running in circles, swinging, flapping “like wings” and circular movements with their arms), as well as stereotypical manipulations with objects (tweaking small details, lining them up). Children with autism have significant difficulty in learning self-care skills. Pronounced motor awkwardness.
Perception disorders: difficulties in orientation in space, fragmentation in the perception of the environment, distortion of a holistic picture of the objective world.
Difficulty in concentrating: children have difficulty concentrating on one thing, there is high impulsivity and restlessness.
Poor memory: often both parents and professionals notice that children with autism remember well what is meaningful to them (this may cause them pleasure or fear). Such children remember their fear for a long time, even if it happened a very long time ago.
Such children remember their fear for a long time, even if it happened a very long time ago.
Features of thinking: experts note difficulties in arbitrary learning. Also, children with autism do not focus on understanding the cause-and-effect relationships in what is happening, there are difficulties in transferring the acquired skills to a new situation, the concreteness of thinking. It is difficult for a child to understand the sequence of events and the logic of another person.
Behavioral problems: negativism (refusal to listen to the instructions of an adult, to perform joint activities with him, leaving the learning situation). Often accompanied by resistance, screams, aggressive outbursts. A huge problem is the fears of such children. Usually they are incomprehensible to others, because often children cannot explain them. The child may be frightened by sharp sounds, some specific actions. Another behavioral disorder is aggression. Any disorder, violation of a stereotype, interference of the outside world in a child's life can provoke aggressive (hysteria or physical attack) and auto-aggressive outbursts (damage to oneself).
Each case of the disease is very individual: autism can have most of the listed signs in an extreme degree of manifestation, and it can manifest itself only in some barely noticeable features.
Diagnosis of autism spectrum disorders
To diagnose autism, specialists use the criteria of 2 international classifications: ICD-10 and DSM-5.
But the main three criteria (“triad” of violations) that can be distinguished are:
- violation of social adaptation
- violations in the communication sphere
- stereotypical behavior
The main diagnostic steps include:
- examination of the child by a psychiatrist, neurologist, psychologist
- observation of the child and filling out the "Autism Rating Scale", which can be used to determine the severity of the disorder
- conversation with parents
- filling in questionnaires by parents - "Questionnaire for the diagnosis of autism"
PAC species
There are several existing classifications of ASD, and the separation often occurs on completely different grounds, which, of course, can bring some inconvenience to a person who is initially little familiar with medicine or psychology; therefore, the most basic and frequently encountered types of ASD will be highlighted below: - Kanner's syndrome (Early childhood autism) - characterized by a "triad" of the main violations: difficulty in establishing contacts with the outside world, stereotypical behavior, as well as a delay or violation of the communicative functions of speech development . It is also necessary to note the condition of the early onset of these symptoms (up to about 2.5 years)
It is also necessary to note the condition of the early onset of these symptoms (up to about 2.5 years)
It manifests itself in children in 4 forms, depending on the degree of fencing off from the outside world:
Complete detachment from what is happening. This group is characterized by the absence of speech and the inability to organize the child (to establish eye contact, to achieve the implementation of instructions and assignments). When trying to interact with the child, he shows the greatest discomfort and impaired activity.
Active rejection. It is characterized by more active contact with the environment than the first group. There is no such detachment, but there is rejection of a part of the world that is unacceptable to the child. The child shows selective behavior (in communication with people, in food, in clothes)
Preoccupation with autistic interests. It is characterized by the formation of overvalued addictions (for years a child can talk on the same topic, draw the same plot). The gaze of such children is directed at the face of a person, but they look "through" this person. Such children enjoy the stereotyped reproduction of individual impressions.
The gaze of such children is directed at the face of a person, but they look "through" this person. Such children enjoy the stereotyped reproduction of individual impressions.
Extreme difficulty in organizing communication and interaction. Autism at its mildest. Children are characterized by increased vulnerability, contact with the world stops at the slightest sensation of obstacles. These children can make eye contact.
- Asperger's Syndrome. Formed from birth. Children have an early onset of speech development, a rich vocabulary, developed logical thinking, and there are no disorders in mental development. But at the same time, the communicative side of speech suffers: such children do not know how to establish contact with other people, do not listen to them, can talk to themselves, do not keep a distance in communication, and do not know how to empathize with other people.
- Rett syndrome. Its peculiarity lies in the fact that the development of a child up to 1-1. 5 years proceeds normally, but then the newly acquired speech, motor and subject-role skills begin to disintegrate. Characteristic for this condition are stereotypical, monotonous movements of the hands, rubbing, wringing, while not carrying a purposeful character. The rarest of the presented diseases, occurring almost always only in girls.
5 years proceeds normally, but then the newly acquired speech, motor and subject-role skills begin to disintegrate. Characteristic for this condition are stereotypical, monotonous movements of the hands, rubbing, wringing, while not carrying a purposeful character. The rarest of the presented diseases, occurring almost always only in girls.
- Childhood psychosis. The first manifestation of symptoms before 3 years of age. It is characterized by violations of social behavior, communication disorders. There are stereotypes in behavior (children run in a monotonous circle, sway while standing and sitting, fingering their fingers, shaking their hands). These children have eating disorders: they can swallow food without chewing. Their unclear speech can sometimes be an incoherent collection of words. There are times when children freeze in place, like dolls.
- Atypical autism. It differs from autism in terms of age manifestation and the absence of one criterion from the “triad” of major disorders.
Correction of patients with ASD
One of the most important sections of habilitation for children with ASD is undoubtedly the provision of psycho-correctional and social rehabilitation assistance, with the formation of social interaction and adaptation skills. Comprehensive psycho-correctional work, which includes all sections and types of rehabilitation assistance, which will be described below, is, along with drug therapy, an effective means of stopping the negative symptoms of ASD, and also contributes to the normal inclusion of the child in society. Types of RAS correction:
1) Psychological correction - the most common and well-known type; It is characterized by a fairly wide range of methods, of which the TEACCH and ABA-therapy programs are most widely used and recognized in the world.
The first program is based on the following principles:
- The characteristics of each individual child are interpreted on the basis of observations of him, and not from theoretical ideas;
- increasing adaptation is carried out both by learning new skills and by adapting existing ones to the environment;
- Creation of an individual training program for each child; use of structured learning; holistic approach to intervention.
The second program is largely based on learning, which depends on the consequences that have arisen after the behavior. Consequences can be in the form of punishment or reward. In this model, it is necessary to highlight the main methods, such as the procedure for creating a contour and reinforcing behavior similar to the target; method of teaching chains of behavior; method of teaching discrimination of stimuli.
2) Neuropsychological correction - this type includes a set of exercises consisting of stretching, breathing, oculomotor, facial and other exercises for the development of the communicative and cognitive sphere, and the exercises themselves differ markedly in time and quantity.
3) Work with the child's family and environment - first of all, this type of correction is aimed at alleviating emotional tension and anxiety among family members, since parents of children with ASD often also need help, including psychotherapeutic support and training programs (such programs are mainly aimed at developing feelings of understanding of the problem, the reality of its solution and the meaningfulness of behavior in the current family situation).
4) Psychosocial therapy - in fact, work with the child himself to form the cognitive, emotional and motivational-volitional resources of the individual for the possibility of further social adaptation, the need for which becomes more pronounced as the child with ASD grows older.
5) Logopedic correction - given the fact that speech development disorder is one of the cardinal manifestations of ASD, this type of work with a child will be an integral part of the correction program. It is characterized by a focus on the formation of vocabulary, the development of auditory attention, as well as phonetic and speech hearing.
6) Medical correction of RAS. In some forms of autism, medication is needed for the child. For example, to improve concentration and perseverance, a doctor may prescribe vitamins and nootropic drugs that improve thinking processes and stimulate speech development. And with high impulsivity, aggression, negativism, pronounced signs of "withdrawal into oneself", psychotropic drugs can help.