Uterus after pregnancy
Your body after baby: The first 6 weeks
Topics
In This Topic
KEY POINTS
Your body changes a lot after you give birth. Some changes are physical and others are emotional.
Learn about common postpartum discomforts and what do to about them. If you’re worried about a discomfort, call your health care provider.
Talk to your provider before you take any medicine to treat a discomfort. If you’re breastfeeding, some medicines aren’t safe for your baby.
Go to all of your postpartum checkups, even if you’re feeling fine. Some health conditions after pregnancy need medical care.
How does your body change in the weeks after giving birth?
Many things are happening in your body right after you have a baby. During pregnancy, your body changed a lot. It worked hard to keep your baby safe and healthy. Now that your baby is here, your body is changing again. Some of these changes are physical, like your breasts getting full of milk. Others are emotional, like feeling extra stress.
Many discomforts and body changes after giving birth are normal. But sometimes they’re signs or symptoms of a health problem that needs treatment. Go to all of your postpartum checkups, even if you’re feeling fine. These are medical checkups you get after having a baby to make sure you’re recovering well from labor and birth. At your checkups, your health care provider can help spot and treat health conditions. Postpartum care is important because new moms are at risk of serious and sometimes life-threatening health complications in the days and weeks after giving birth.
What is perineum soreness?
The perineum is the area between your vagina and rectum. It stretches and may tear during labor and vaginal birth. It’s often sore after giving birth, and it may be more sore if you have an episiotomy. This is a cut made at the opening of the vagina to help let your baby out.
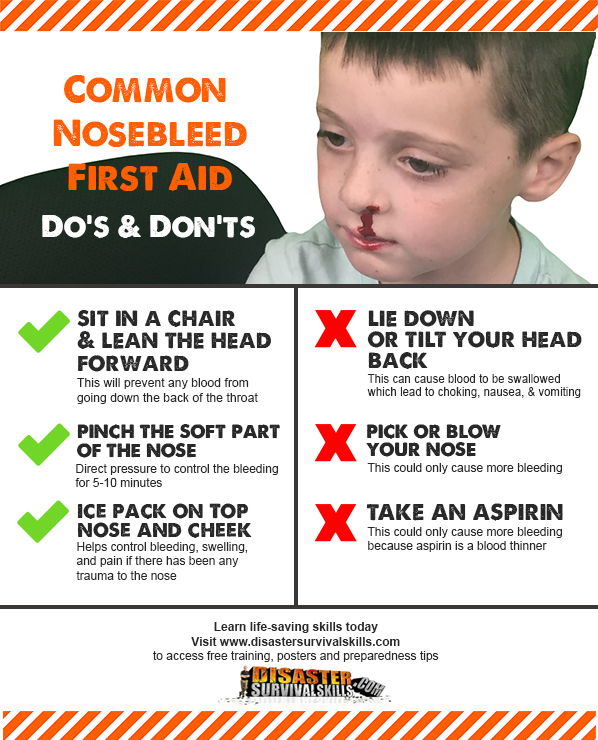
What you can do:
- Do Kegel exercises.
 These exercises strengthen the muscles in the pelvic area. To do Kegel exercises, squeeze the muscles that you use to stop yourself from passing urine (peeing). Hold the muscles tight for 10 seconds and then release. Try to do this at least 10 times in a row, three times a day.
These exercises strengthen the muscles in the pelvic area. To do Kegel exercises, squeeze the muscles that you use to stop yourself from passing urine (peeing). Hold the muscles tight for 10 seconds and then release. Try to do this at least 10 times in a row, three times a day. - Put a cold pack on your perineum. Use ice wrapped in a towel. Or you can buy cold packs that you freeze in your freezer.
- Sit on a pillow or a donut-shaped cushion.
- Soak in a warm bath.
- Wipe from front to back after going to the bathroom. This can help prevent infection as your episiotomy heals.
- Ask your provider about pain medicine.
What are afterbirth pains?
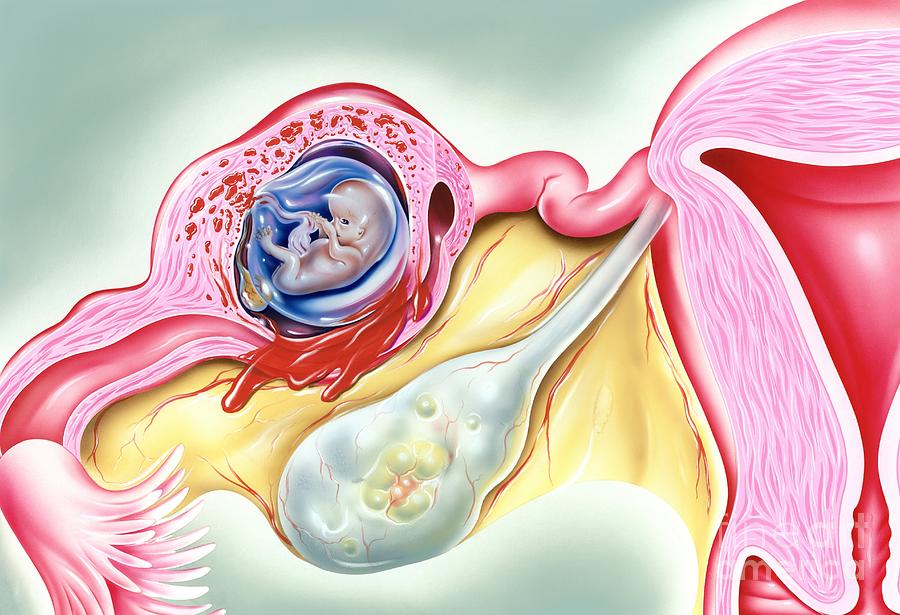
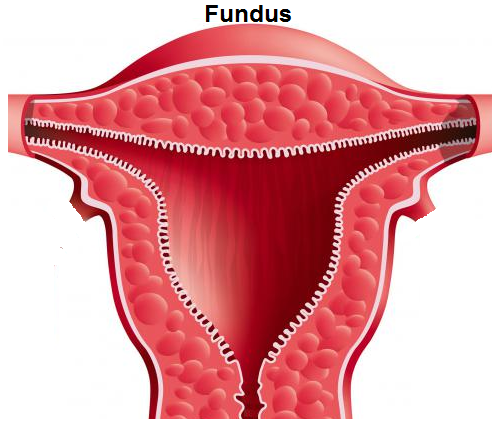
Afterbirth pains are belly cramps you feel as your uterus (womb) shrinks back to its regular size after pregnancy. The cramps should go away in a few days. Right after you give birth, your uterus is round and hard and weighs about 2½ pounds. By about 6 weeks after birth, it weighs only 2 ounces.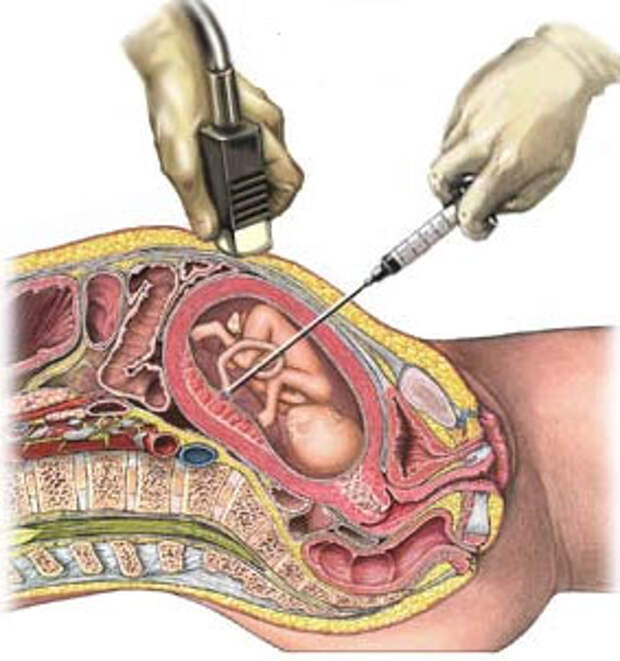
What you can do:
Ask your provider about over-the-counter medicine you can take for pain. Over-the-counter medicine is medicine you can buy without a prescription from your provider.
What body changes can happen after a cesarean section?
Cesarean birth (also called c-section) is surgery in which your baby is born through a cut that your provider makes in your belly and uterus. A c-section is major surgery, so it may take a while for you to recover. You may be really tired for the first few days or weeks after a c-section because you lost blood during the surgery. The incision (cut) on your belly may be sore.
What you can do:
- Ask your provider for pain medicine. Check with him before you take any medicine for pain.
- Ask your partner, family and friends to help you with the baby and around the house.
- Get rest when you can. Sleep when your baby sleeps, even when he naps during the day.
- Don’t lift from a squatting position.
 Don’t lift anything heavier than your baby.
Don’t lift anything heavier than your baby. - Support your belly with pillows when you’re breastfeeding.
- Drink plenty of water to help replace fluids in your body.
What is vaginal discharge?
After your baby is born, your body gets rid of the blood and tissue that was inside your uterus. This is called vaginal discharge or lochia. For the first few days, it’s heavy, bright red and may contain blood clots. Over time, the flow gets less and lighter in color. You may have discharge for a few weeks or even for a month or more.
What you can do:
Use sanitary pads until the discharge stops.
What is breast engorgement?
This is when your breasts swell as they fill with milk. It usually happens a few days after giving birth. Your breasts may feel tender and sore. The discomfort usually goes away once you start breastfeeding regularly. If you’re not breastfeeding, it may last until your breasts stop making milk, usually within a few days.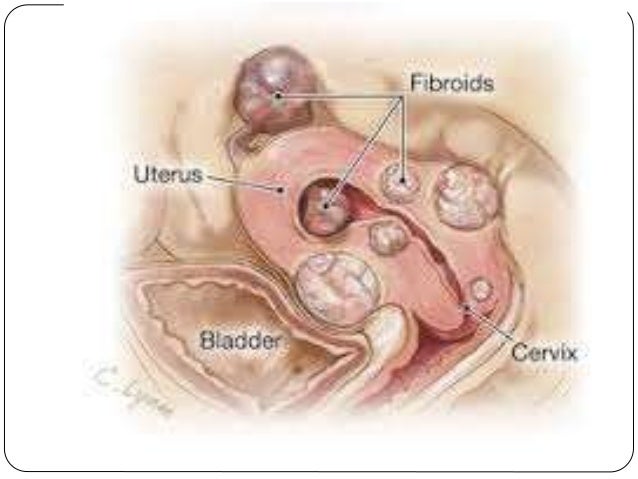
What you can do:
- Breastfeed your baby. Try not to miss a feeding or go a long time between feedings. Don’t skip night feedings.
- Before you breastfeed your baby, express a small amount of milk from your breast with a breast pump or by hand.
- Take a warm shower or lay warm towels on your breasts to help your milk flow. If your engorgement is really painful, put cold packs on your breasts.
- If your breasts are leaking between feedings, wear nursing pads in your bra so your clothes don’t get wet.
- Tell your provider if your breasts stay swollen and are painful.
- If you’re not planning to breastfeed, wear a firm, supportive bra (like a sports bra).
What is nipple pain?
If you’re breastfeeding, you may have nipple plain during the first few days, especially if your nipples crack.
What you can do:
- Talk to your provider or a lactation consultant to be sure your baby is latching on to your breast the right way.
 A lactation consultant is a person trained to help women breastfeed, even women who have breastfeeding problems. Latching on is when your baby’s mouth is securely attached to (placed around) your nipple.
A lactation consultant is a person trained to help women breastfeed, even women who have breastfeeding problems. Latching on is when your baby’s mouth is securely attached to (placed around) your nipple. - Ask your provider about cream to put on your nipples.
- After breastfeeding, massage some breast milk onto your nipples. Let your breasts air dry.
What is swelling?
Lots of women have swelling in their hands, feet and face during pregnancy. It’s caused by extra fluids in your body. It may take time for the swelling to go away after you have your baby.
What you can do:
- Lie on your left side when resting or sleeping.
- Put your feet up.
- Try to stay cool and wear loose clothes.
- Drink plenty of water.
What are hemorrhoids?
Hemorrhoids are painful, swollen veins in and around the anus that may hurt or bleed. Hemorrhoids are common during and after pregnancy.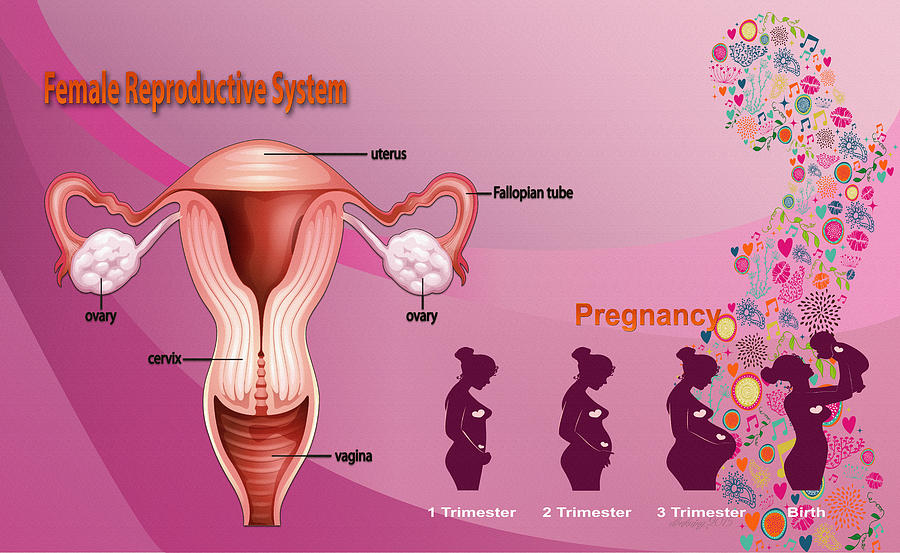
What you can do:
- Soak in a warm bath.
- Ask your provider about using an over-the-counter spray or cream for pain.
- Eat foods that are high in fiber, such as fruits, vegetables and whole-grain breads and cereals.
- Drink lots of water.
- Try not to strain when you’re having a bowel movement (pooping).
What is constipation?
Constipation is when you don’t have bowel movements, you don’t have them often or your stools (poop) are hard to pass. You also may have painful gas. This may happen for a few days after you give birth.
What you can do:
- Eat foods that are high in fiber.
- Drink lots of water.
- Ask your provider about medicine to take.
What urinary problems can happen after giving birth?
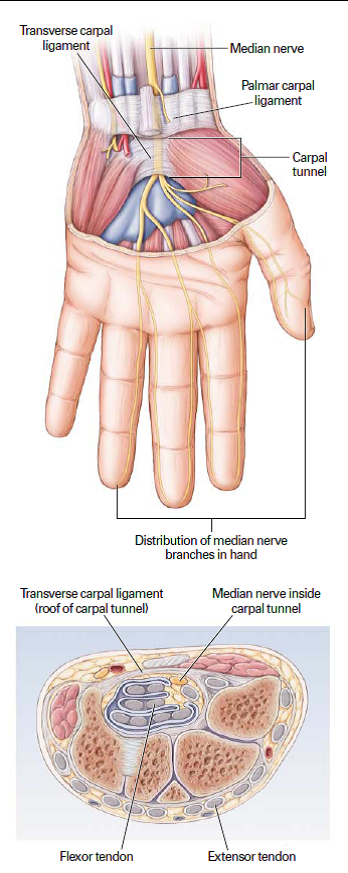
In the first few days after giving birth, you may feel pain or burning when you urinate (pee). Or you may try to urinate but find that you can’t. Sometimes you may not be able to stop urinating. This is called incontinence. It usually goes away as your pelvic muscles become stronger again.
Or you may try to urinate but find that you can’t. Sometimes you may not be able to stop urinating. This is called incontinence. It usually goes away as your pelvic muscles become stronger again.
What you can do for pain, burning or if you have trouble urinating:
- Drink lots of water.
- Run water in the sink when you go to the bathroom.
- Soak in a warm bath.
- If the pain continues, tell your provider.
What you can do for incontinence: Do Kegel exercises to strengthen your pelvic muscles.
Why do you sweat a lot after giving birth?
This happens often to new moms, especially at night. It’s caused by all the changing hormones in your body after pregnancy.
What you can do:
- Sleep on a towel to help keep your sheets and pillow dry.
- Don’t use too many blankets or wear warm clothes to bed.
Why do you feel tired after giving birth?
You may have lost blood during labor and birth.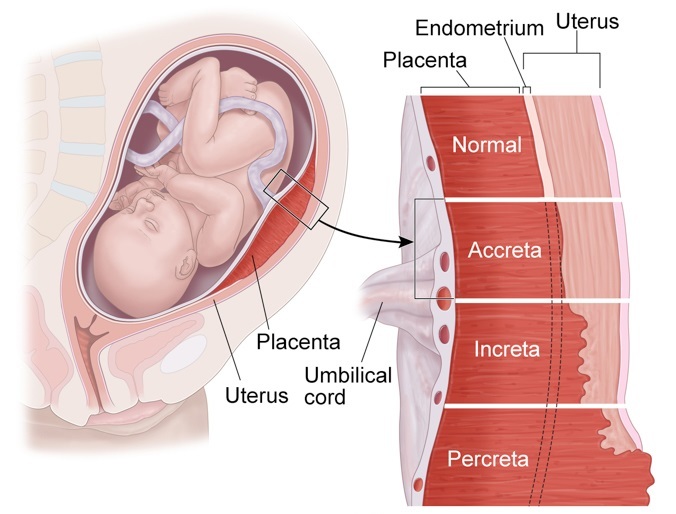 This can make your body tired. And your baby probably doesn’t let you sleep all night!
This can make your body tired. And your baby probably doesn’t let you sleep all night!
What you can do:
- Sleep when your baby sleeps, even when he naps during the day.
- Eat healthy foods, like fruits, vegetables, whole-grain breads and pasta, and lean meat and chicken. Limit sweets and foods with a lot of fat.
- Ask your partner, family and friends for help with the baby and around the house.
- Limit visitors. You’ll have plenty of time for family and friends to meet your new baby when you’re feeling rested.
When can you lose weight after giving birth?
You lose about 10 pounds right away after giving birth and a little more within the first week. This is a great time to get to a healthy weight, no matter how much you weighed before you got pregnant. Eating healthy and being active every day helps boost your energy level and can make you feel better. If you’re at a healthy weight, you’re less likely to have health conditions, like diabetes and high blood pressure, than if you’re over- or underweight.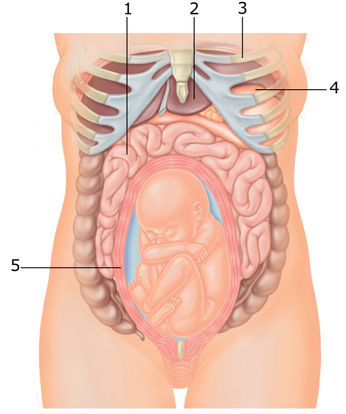 And just in case you get pregnant again, or if you’re planning to have another baby sometime in the future, it’s best to be at a healthy weight before your next pregnancy.
And just in case you get pregnant again, or if you’re planning to have another baby sometime in the future, it’s best to be at a healthy weight before your next pregnancy.
What you can do:
- Talk to your provider about your weight. If you were overweight before pregnancy, you may want to lose more weight than you gained during pregnancy.
- Eat healthy foods. Limit sweets and foods with a lot of fat.
- Drink lots of water.
- Ask your provider about being active, especially if you’ve had a c-section. Begin slowly and increase your activity over time. Walking and swimming are great activities for new moms. Do something active every day.
- Breastfeed your baby. Breastfeeding helps you burn calories. This can help you lose the weight you gained during pregnancy faster than if you weren’t breastfeeding.
- Don’t try to lose too much weight too fast. Your body needs nutrients from food to heal.
 If you’re breastfeeding, losing weight too fast can reduce your milk supply.
If you’re breastfeeding, losing weight too fast can reduce your milk supply. - Don’t feel badly if you don’t lose the weight as quickly as you’d like. It takes time for your body and your belly to get back in shape. Staying fit over time is more important than getting in shape right after giving birth.
What skin changes can happen after giving birth?
You may have stretch marks on your belly where your skin stretched during pregnancy. Some women also get them on their thighs, hips and bottom. They may not disappear after giving birth, but they do fade over time.
What you can do:
Use creams or lotions on your skin. They don’t make stretch marks go away, but they can help reduce itching that comes with stretch marks.
What hair changes can happen after giving birth?
Your hair may have seemed thicker and fuller during pregnancy. This is because high hormone levels in your body made you lose less hair during pregnancy. After your baby is born, your hair may thin out. You may even lose hair. Hair loss usually stops within 6 months after you give birth. Your hair should regain its normal fullness within a year.
After your baby is born, your hair may thin out. You may even lose hair. Hair loss usually stops within 6 months after you give birth. Your hair should regain its normal fullness within a year.
What you can do:
- Eat lots of fruits and vegetables. The nutrients in fruits and veggies may help protect your hair and help it grow.
- Be gentle with your hair. Don’t wear tight ponytails, braids or rollers. These can pull and stress your hair.
- Use the cool setting on your hair dryer.
When do you get your period again after pregnancy?
If you’re not breastfeeding, your period may start again 6 to 8 weeks after giving birth. If you are breastfeeding, it may not start again for months. Some women don’t have a period again until they stop breastfeeding. When your period returns, it may not be the same as before you were pregnant. It may be shorter or longer than it was. Over time it often returns to the way it was before you got pregnant.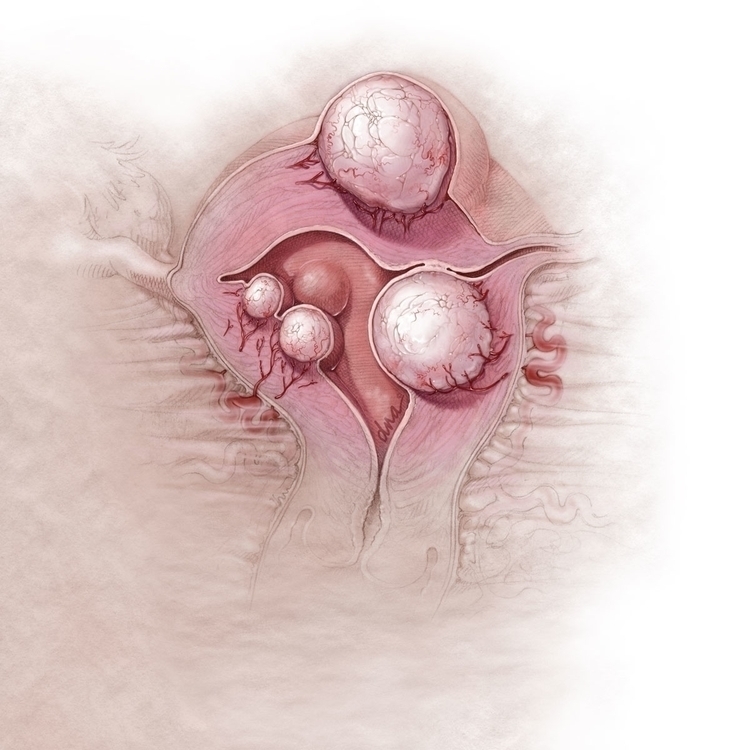
When can you get pregnant again?
Many health care providers recommend waiting 4 to 6 weeks after giving birth to give your body time to heal before you have sex. When you’re ready for sex, be careful – you can get pregnant even before your period starts. This is because you may ovulate (release an egg) before you get your period again.
What you can do:
Use birth control to help make sure you don’t get pregnant again until you’re ready. Birth control helps keep you from getting pregnant. Examples of birth control include intrauterine devices (also called IUDs), implants, the pill and condoms. Talk to your provider about which birth control to use, especially if you’re breastfeeding. Some types of birth control can reduce your milk supply. Breastfeeding is not birth control. It does not prevent pregnancy.
For most women, it’s best to wait at least 18 months (1½ years) between giving birth and getting pregnant again. Too little time between pregnancies increases your risk of premature birth (before 37 weeks of pregnancy). Premature babies are more likely to have health problems than babies born on time. Your body needs time to fully recover from your last pregnancy before it’s ready for your next pregnancy.
Premature babies are more likely to have health problems than babies born on time. Your body needs time to fully recover from your last pregnancy before it’s ready for your next pregnancy.
What can you do about feeling stressed and overwhelmed?
Your baby didn’t come with a set of instructions. You may feel overwhelmed trying to take care of her. Taking care of a baby is a lot to think about.
What you can do:
- Tell your partner how you feel. Let your partner help take care of the baby.
- Ask your friends and family for help. Tell them exactly what they can do for you, like going grocery shopping or making meals.
- Find a support group of new moms. A support group is a group of people who have the same kinds of concerns. They meet together to try to help each other. Ask your provider to help you find a support group of new moms near where you live. Or look for a support group online.
- Eat healthy foods and do something active every day.
- Don’t smoke, drink alcohol or use harmful drugs. All of these things are bad for you and can make it hard for you to handle stress.
What are the baby blues and postpartum depression?
Baby blues (also called postpartum blues) are feelings of sadness a woman may have in the first few days after having a baby. Baby blues can happen 2 to 3 days after you have your baby and can last up to 2 weeks. They usually go away on their own, and you don’t need any treatment.
Postpartum depression (also called PPD) is a kind of depression that some women get after having a baby. It's strong feelings of sadness, anxiety (worry) and tiredness that last for a long time after giving birth. These feelings can make it hard for you to take care of yourself and your baby. PPD is a medical condition that needs treatment to get better. It’s the most common complication for women who have just had a baby.
What you can do about the baby blues:
- Get as much sleep as you can.

- Don’t drink alcohol, use street drugs or use harmful drugs. All of these can affect your mood and make you feel worse. And they can make it hard for you to take care of your baby.
- Ask for help from your partner, family and friends. Tell them exactly what they can do for you.
- Take time for yourself. Ask someone you trust to watch your baby so you can get out of the house.
- Connect with other new moms. Ask your provider to help you find a support group of new moms.
- If you have sad feelings that last longer than 2 weeks, tell your health care provider.
What you can do about postpartum depression:
- If you think you have PPD, tell your provider.
- Learn about risk factors for PPD and signs and symptoms of PPD.
- Ask your provider about treatment for PPD.
- If you’re worried about hurting yourself or your baby, call emergency services (911) right away.
How can you handle going back to work or school?
It may be hard for you to leave your baby with a caregiver all day, even if it’s a family member or a close friend.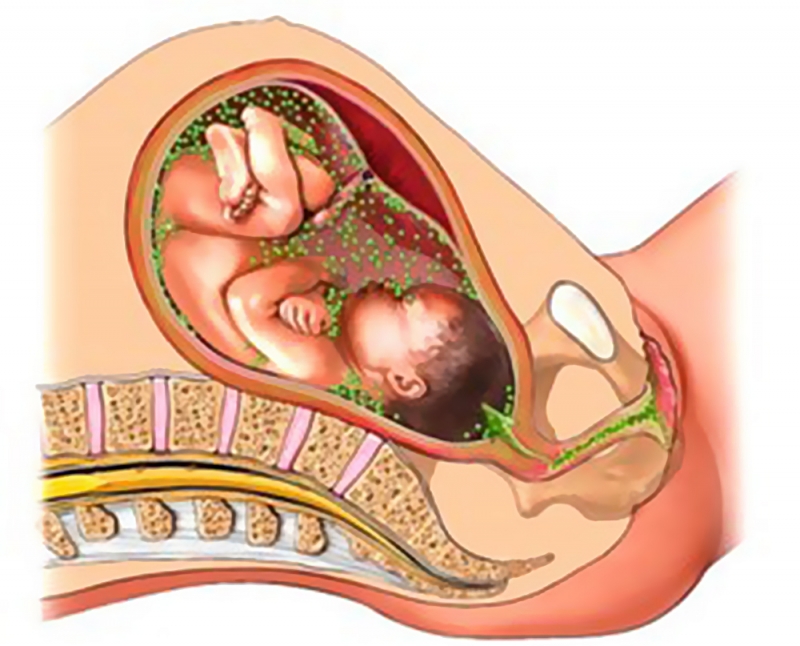 It also may be hard to find a caregiver you trust. You and your partner may disagree about what type of child care is best for your baby. You may be upset that you can’t stay home with your baby all the time.
It also may be hard to find a caregiver you trust. You and your partner may disagree about what type of child care is best for your baby. You may be upset that you can’t stay home with your baby all the time.
What you can do:
- Talk to your partner about child care. Figure out how much you can spend and what kind of care you want. For example, you can have a caregiver come to your home to take care of your baby. Or you can take your baby to a child care center.
- Ask friends and family about child care they use. Maybe you can use the same person or service.
- If you’re using a child care center, ask for names and phone numbers of people who use the center. Call to ask how they feel about the center’s care.
- Ask your boss if you can ease back into work. Maybe you can work a few hours a day at first, or just a few days a week.
How can you and your partner get used to being new parents?
Both you and your partner are getting used to having a baby around. Your partner may be just as stressed and nervous about being a parent as you are. Rely on each other to figure things out.
Your partner may be just as stressed and nervous about being a parent as you are. Rely on each other to figure things out.
What you can do:
- Learn about taking care of your baby together. Read baby-care books and go to baby-care classes.
- Let your partner help with the baby. Don’t try to do everything yourself.
- Talk to each other. Talking about your feelings can help keep you from feeling hurt and frustrated.
- Make time for just the two of you. Go for a walk or out to dinner. Ask someone you trust to take care of the baby for an hour or two.
- Tell your partner what your provider says about how long to wait to have sex again. Ask your provider to talk to your partner, if you think that’s helpful.
Last reviewed: July, 2018
See also: Your postpartum checkups, Warning signs and symptoms of health problems after giving birth, Pregnancy-related death, maternal death and maternal mortality, Postpartum depression, Baby blues after pregnancy, Keeping breast milk safe and healthy, Birth control, How long should you wait before getting pregnant again
') document. write('
write('
Nutrition, weight & fitness
') document.write('') }
') document.write('') }
Postpartum recovery: Bleeding, headaches, exercise, and more
Postpartum recovery is different for everyone. It may take several weeks (or months) to lose your postpartum belly, for example. And postpartum weight loss may take anywhere from 6 to 12 months or more. When you get your first postpartum period will depend in part on whether – and how much – you're breastfeeding. Just like adjusting to your new life with your baby, taking care of your changing postpartum body can seem like a lot, but you'll feel more and more like yourself every day as you recover.
Just as every pregnancy, labor, and delivery is unique, so is every postpartum recovery experience. Postpartum women share many of the same postpartum experiences, though, and they have similar questions – about everything from their postpartum belly and postpartum headaches to postpartum weight loss and exercise, for example.
Here are some of the most frequently asked questions about postpartum recovery, but remember that your healthcare provider is just a call away, too. Don't hesitate to call them for more information or for answers to your less frequently asked questions.
How long is postpartum recovery?
Every mom is different. Postpartum recovery depends on a number of factors, such as your age and general health, the type of pregnancy you had (with or without pregnancy complications), and the type of labor and delivery you had (vaginal or c-section, assisted with forceps or a vacuum or not, long and difficult or – relatively – easy, and medicated or non-medicated).
Most moms, though, feel somewhat "back to normal" by about six to eight weeks after delivery. If you're exclusively formula feeding, you may even have your first postpartum period by then.
That's not to say all of your symptoms will take that long to subside. Postpartum bleeding should slow within days, for example, and afterpains should disappear within a week or so. Perineal pain may quickly disappear, or it may linger – depending on whether you had perineal tearing or an episiotomy. On the other hand, some things may take longer than eight weeks. Your normal hair patterns (growing and resting phases), for example, will take 6 to 15 months to return to normal.
Perineal pain may quickly disappear, or it may linger – depending on whether you had perineal tearing or an episiotomy. On the other hand, some things may take longer than eight weeks. Your normal hair patterns (growing and resting phases), for example, will take 6 to 15 months to return to normal.
What essentials should I have in my postpartum recovery kit?
Prepare a postpartum recovery kit well in advance of your due date (maybe along with your hospital bag.) Here are the most important things to include:
- Maxi pads. You'll have some postpartum bleeding (lochia) right after delivery. In the first few days, the flow might be similar to a heavy period, so stock up on some extra-large pads for those days. You can switch to smaller pads as your flow lightens. Because of the risk of infection, you can't use tampons or menstrual cups.
- Disposable underwear. You may at first want to stick with disposable underwear (usually expandable mesh, which they'll give you at the hospital).
 These are perfect for holding large sanitary pads, and you won't have to worry about staining regular undies. Some can be washed a few times and reused. Many moms wear them until they're done bleeding. Some like to wear incontinence panties instead of postpartum disposables. You may need to wear pads with them at first, until your bleeding slows down.
These are perfect for holding large sanitary pads, and you won't have to worry about staining regular undies. Some can be washed a few times and reused. Many moms wear them until they're done bleeding. Some like to wear incontinence panties instead of postpartum disposables. You may need to wear pads with them at first, until your bleeding slows down. - Postpartum underwear. When you're no longer bleeding enough to need large sanitary pads, you may want to graduate from the disposables to something more like regular underwear. Choose postpartum underwear that's very comfortable (soft and larger than you'd normally wear), stretchy, and absorbent. If you had a c-section, you'll want them to be high waisted to avoid irritating the scar area. Some specially designed postpartum underwear have absorbent panels so that you don't need to wear a pad once your flow is light. Compression postpartum underwear can be used for light support, but don't make them too tight or they'll interfere with healing.
- An ice pack. Ice can numb pain, reduce swelling, and be very soothing for perineal pain. A normal ice pack won't be comfortable, but there are products on the market that are designed specifically to use on your perineum. These gel packs are shaped like sanitary pads so you can tuck them in your underwear, and they'll conform to your body.
- Squirt/rinse bottle. An occasional perineal rinse with water can be soothing and help you avoid infection. (Besides, the last thing you'll want to do is wipe with toilet paper.) Peri bottles are specially designed for postpartum use – they spray upside down and usually have a narrow, angled neck to make it easy to reach where you need to. You can add a couple drops of witch hazel to the water, if you like, for added cleansing and soothing.
- Hemorrhoid pads. These are especially helpful if you're dealing with postpartum hemorrhoids, but – because they help shrink blood vessels – they also help with general perineal pain.

- Perineal spray. If you're uncomfortable or itchy as stitches or wounds heal, a perineal spray – which numbs the area – may be very helpful.
- Sitz bath. Taking a sitz bath in warm or cool water can clean and sooth the perineal, vaginal, and rectal area.
- An OTC pain reliever. Both acetaminophen and ibuprofen are generally considered safe postpartum, even if you're breastfeeding. Your provider may recommend you alternate between them for maximum relief. Don't exceed the recommended dosages.
- Stool softener. Postpartum constipation is very common, and there are many things you can do to ease it naturally (such as drinking plenty of water and walking). But if nothing else is working, you may want to take an OTC stool softener. Talk with your practitioner before taking it, however.
- Support band. A support band provides compression and support and can be especially helpful for moms who have had a c-section or moms who have diastasis recti (a vertical bulge in your abdomen where the muscles have widened to make room for your baby).

- Postpartum pillow. Also called a donut cushion, a postpartum pillow helps take pressure off the perineal area when sitting. It's especially helpful if you have hemorrhoids or perineal pain.
If you're breastfeeding, you'll also want to stock up on:
- Nipple cream. If your nipples are dry, cracked, itchy, or bleeding, nipple cream can moisturize and heal them safely. Some moms also find nipple cream useful for lubricating the flanges of their breast pumps.
- Nursing pads. Tuck these in your nursing bra to catch leaks. They're especially helpful in the early days, when your breasts are figuring out when and how much milk to produce. Nursing pads (also called breast pads) also protect sensitive nipples from rubbing and chafing. You can purchase reusable or disposable pads.
- Nursing pillows. Specially designed nursing pillows help you position your baby comfortably each nursing session.
 Some parents also use them while bottle feeding and as little loungers for their babies.
Some parents also use them while bottle feeding and as little loungers for their babies. - Nursing bras. You'll want a few nursing bras, which make it easy for you to breastfeed your baby comfortably. Choose them according to your needs, whether that's something supportive, something to sleep in, or a bra that you can also use for pumping.
Watch our video on 6 things you'll need for breastfeeding for ideas. For help choosing everything from ice packs to pumping bras, see some of the best postpartum products.
How long do you bleed after having a baby?
Postpartum vaginal bleeding typically lasts for four to eight weeks total. But it's not the same continuous flow of blood. For the first few days after birth, you'll bleed quite a bit, like a heavy period. The blood, combined with tissue from the lining of the uterus and mucus, is called lochia.
The discharge will lighten each day, and around two to four days after delivery it may be watery and pinkish.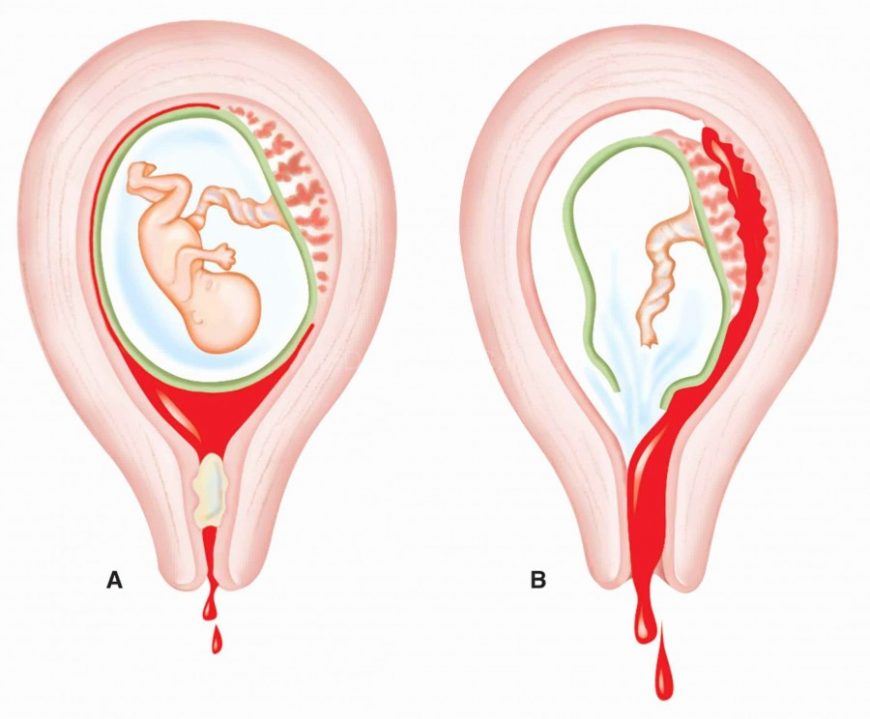 It'll continue to taper off, and by 10 days postpartum you might only have a small amount of white or yellowish discharge, though you may still have spurts of bleeding occasionally (a few times a day). The bleeding should be completely finished in another two to four weeks.
It'll continue to taper off, and by 10 days postpartum you might only have a small amount of white or yellowish discharge, though you may still have spurts of bleeding occasionally (a few times a day). The bleeding should be completely finished in another two to four weeks.
Some women bleed more than this, and it's a medical emergency. Profuse bleeding withing the first 24 hours of delivery is considered primary postpartum hemorrhage (PPH). When it happens in the days or weeks after delivery, it's a late (or delayed or secondary) PPH. If you have any signs of PPH (bright red bleeding that lasts more than a few days after delivery, bleeding that soaks more than one sanitary pad in an hour, blood clots bigger than a golf ball), call your provider right away. Also call if you develop new, significant bleeding after your initial bleeding slowed down.
Some women have a small amount of postpartum rectal bleeding, which is usually caused by hemorrhoids. Taking steps to ease constipation may help, because straining during a bowel movement or passing hard stools can cause the swollen hemorrhoid veins to bleed.
When will my postpartum belly go away?
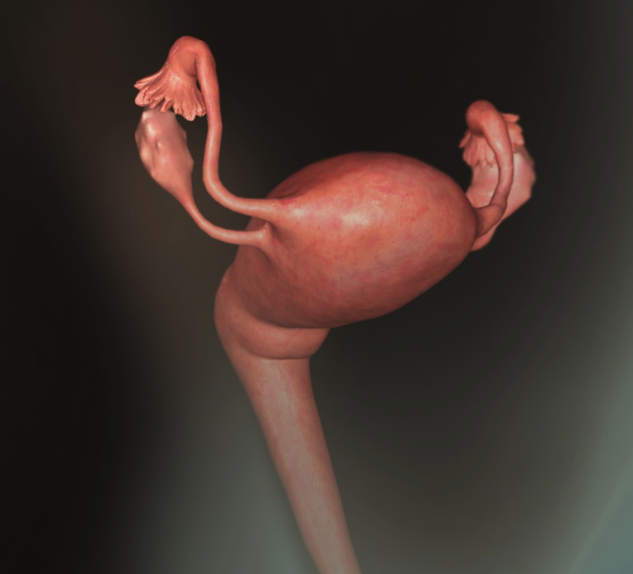
It may depend on a number of factors – such as your weight gain during pregnancy, how active you are, and your genes. Your uterus needs to shrink back to its pre-pregnancy size, you need to lose all that pregnancy fluid (through sweat, urine, and vaginal secretions), and you need to burn off the extra weight you put on to nourish your baby during pregnancy. Hormonal changes after delivery will help with the process, but it can take months.
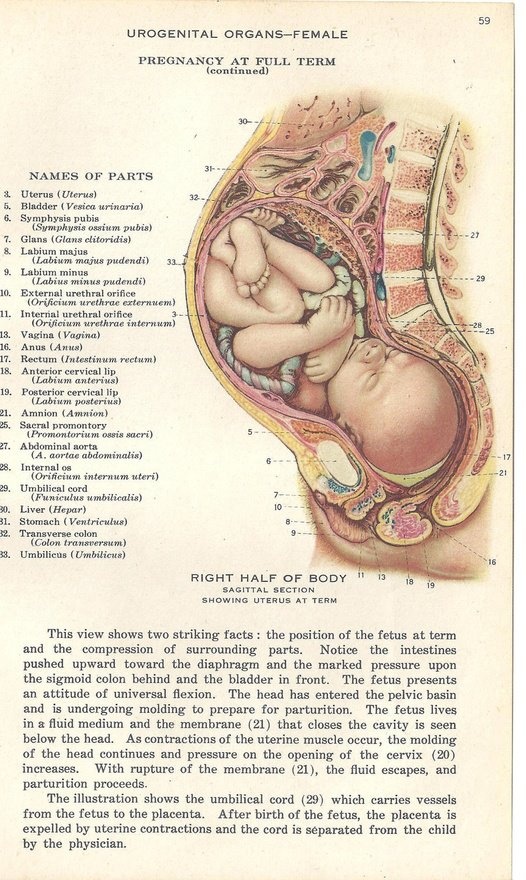
Within minutes of your baby's birth, contractions cause your uterus to shrink, its crisscrossed fibers tightening just like they did during labor. These contractions also help the placenta detach from the uterine wall. After the placenta is delivered, uterine contractions close off the open blood vessels where the placenta was attached. You may feel cramps, known as afterpains, as this happens.
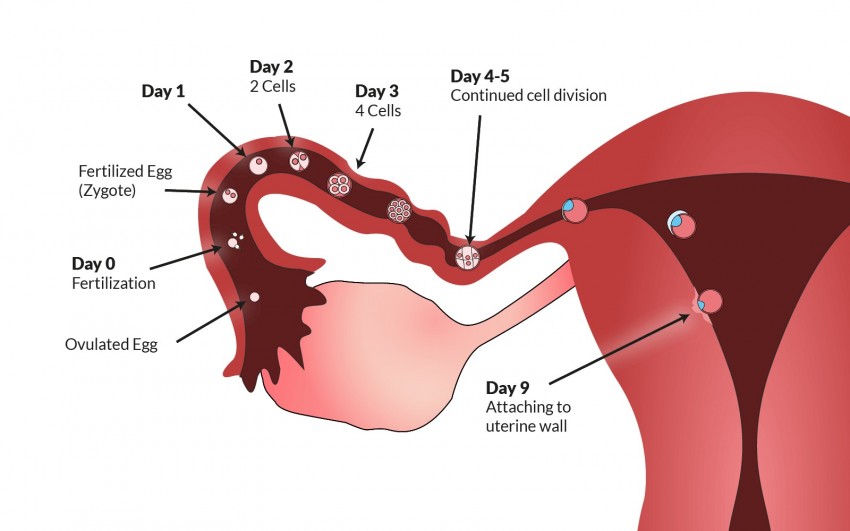
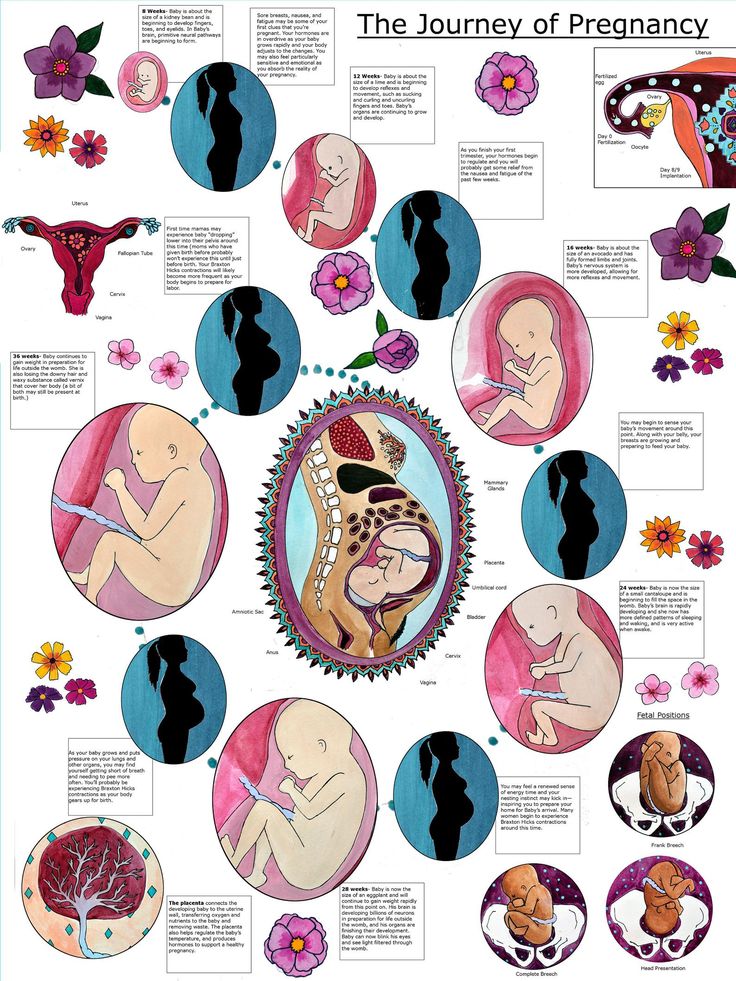
For the first couple of days after giving birth, you'll be able to feel the top of your uterus near your belly button. In a week, your uterus will be half the size it was just after you gave birth. After two weeks, it will be back inside your pelvis. By about four weeks, it should be close to its pre-pregnancy size. This process is called involution of the uterus.
In a week, your uterus will be half the size it was just after you gave birth. After two weeks, it will be back inside your pelvis. By about four weeks, it should be close to its pre-pregnancy size. This process is called involution of the uterus.
Even after your uterus shrinks back to its normal size, you may continue to look pregnant for several weeks or even months. That's because your abdominal muscles get stretched out during pregnancy, and it takes time – and regular exercise – to get those muscles back in shape. (Some women may never be able to get rid of their "pregnancy pouch" entirely.)
If you notice a vertical bulge down the center of your abdomen, you may have diastasis recti. This means that the muscles in your abdomen have separated, leaving a gap. Your provider can confirm if you have the condition, and you can do abdominal rehab to help close it.
Keep in mind that you might not be able to return to your pre-pregnancy belly – or shape, for that matter. Your hips may be wider, your waistline larger, and your belly softer than they were before becoming pregnant. Try to embrace that and appreciate your postpartum belly and your body for its ability to carry and deliver your little one.
Your hips may be wider, your waistline larger, and your belly softer than they were before becoming pregnant. Try to embrace that and appreciate your postpartum belly and your body for its ability to carry and deliver your little one.
By the way, your stretch marks (which happen as your belly and breasts grow quickly during pregnancy) won't completely disappear. By about six to 12 months postpartum, they should be lighter, though. If you have linea nigra (a dark line down your abdomen), that line will also fade over the course of a year, though it may not completely go away.
When will I lose the baby weight?
You may be able to lose the baby weight around 6 to 12 months after your baby arrives. But that's not a guarantee. Some women take longer, and many never return to their pre-pregnancy weight.
Postpartum weight loss begins right after delivery, when you'll already be about 13 pounds lighter. You'll lose the amount your baby weighed (usually 7 or 8 pounds), about a pound of placenta, and another few pounds of blood and amniotic fluid.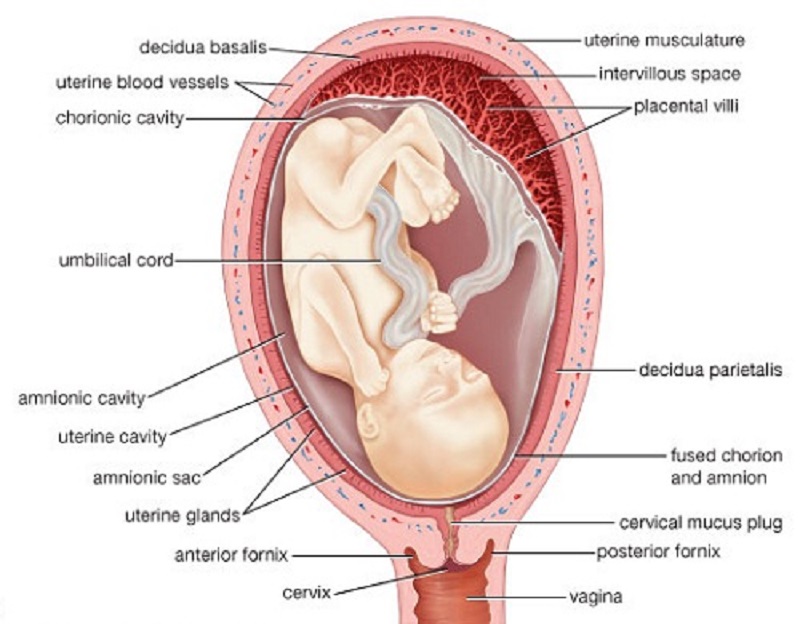 You'll continue to lose about 4 to 6 pounds of water weight in your first week postpartum.
You'll continue to lose about 4 to 6 pounds of water weight in your first week postpartum.
By about 6 weeks postpartum, most moms lose half of their baby weight. And this is a good time to start thinking about calorie reduction, if you like. But take your time (no crash dieting) and include exercise in your diet plan, too.
If you're breastfeeding, wait at least two months to begin dieting. The good news is that breastfeeding – which burns about 400 to 500 calories daily – might help you lose some of those extra pounds. Significant calorie restriction can lead to a dip in milk supply, so start slow.
Read more about diet for healthy post-baby weight loss.
Will my vagina be the same postpartum?
Though you will regain vaginal muscle tone, if you give birth vaginally, your postpartum vagina will probably remain a little larger than it was before.
Right after delivery, your vagina is stretched open and may be swollen and bruised. How much depends on a number of factors, such as:
- How big your baby was
- Whether you had an assisted birth
- How much relaxin you produced (Relaxin is the hormone that loosens the joints, ligaments, and tissues in your pelvis and vagina in preparation for delivery)
- How long you pushed during delivery (even moms with a c-section might have pushed some first)
- Your age (your muscles loosen as you age)
- How many births you've had (more deliveries mean more laxity)
Over the next few days, swelling starts to go down, and your vagina begins to regain muscle tone. In the next few weeks, it will gradually get smaller. Most moms with an uncomplicated vaginal delivery can regain full pelvic floor tightness in about six months. For moms with multiple vaginal births or a birth injury during delivery, it may take a bit longer. Doing Kegel exercises regularly can restore muscle tone. Some women find pelvic floor therapy even more helpful.
In the next few weeks, it will gradually get smaller. Most moms with an uncomplicated vaginal delivery can regain full pelvic floor tightness in about six months. For moms with multiple vaginal births or a birth injury during delivery, it may take a bit longer. Doing Kegel exercises regularly can restore muscle tone. Some women find pelvic floor therapy even more helpful.
You'll need to wait until your postpartum checkup to get your provider's go-ahead for sex if you've had a c-section, episiotomy, or perineal tear. Otherwise, many providers recommend you wait about four weeks after childbirth. That said, it may be much longer before you're interested, and that's perfectly fine. Take as much time as you need to adjust physically and emotionally to motherhood.
Find out when it's safe to start having sex again.
Are postpartum headaches normal?
Yes, about 40 percent of women experience headaches in the postpartum period.
Causes of postpartum headaches include:
- Sleep deprivation
- Hormonal changes
- Psychological stress
- Postpartum fatigue
- Physiological changes
- An epidural during labor and delivery.
 About 1 in 100 women develop a spinal headache in the days after having an epidural.
About 1 in 100 women develop a spinal headache in the days after having an epidural.
Postpartum migraines are also common. Migraine in women is closely linked to hormonal changes. A drop in estrogen levels (just before a menstrual period or right after birth) can trigger a migraine. According to the American Migraine Foundation, about one in four women will experience a migraine within two weeks of delivery, and almost half will have migraine attacks within the first month. About 5 percent of women who have never experienced migraine get their first one in the postpartum period.
Most causes of postpartum headaches aren't dangerous, but headaches can be a warning sign of postpartum preeclampsia. Call your provider if you have a headache that:
- Gets worse over time or won't go away
- Is very intense
- Lasts even after taking medication and fluids
- Starts suddenly, like a thunderclap
- Throbs and is on one side of your head or above your ear
- Is accompanied by blurred vision or dizziness
- Goes away when you're lying down and you've had an epidural
How can I take care of myself postpartum?
After your baby arrives, it's important – for both of you – that you take care of yourself by eating well, getting enough rest, and exercising when it's safe for you to do so.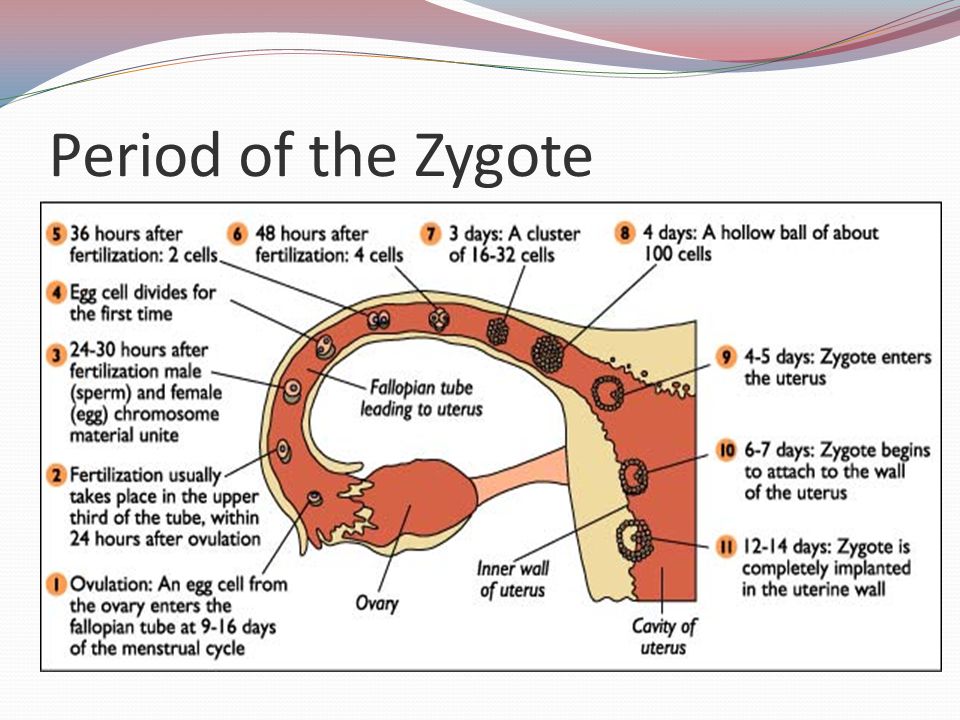 But good postpartum care also includes your mental health.
But good postpartum care also includes your mental health.
To take good care of your mental health:
- Develop a support system. Make sure you have other new parents to talk to and make a point of talking to them or seeing them at least once a week. Accept help and an empathetic ear from family and friends.
- Express and accept your negative feelings. The baby blues are very common, affecting up to 80 percent of moms right after birth. These feelings of sadness, exhaustion, and/or overwhelm often subside in a couple of weeks. In the meantime, don't bottle them up.
- Focus on your positive feelings. Look for ways in which you do feel good and pay attention to those, too.
- Take breaks by yourself, with your partner, or with another adult. No one can work at a job nonstop without some time off every day.
- Keep your expectations realistic. You can't do it all, let alone do it perfectly. Work toward reasonable, achievable goals, whether dealing with feelings, doing housework or losing your pre-baby weight.
- Nurture your sense of humor. Try to laugh daily, whether at yourself, your situation, or something outside of all this.
- Structure your day. Plan loosely how you'll spend your day, designating time for all the items on this list. Keep the plan flexible and realistic so you can stick to it.
- Postpone other major life changes. Avoid taking on a new job, a new home, or a new partner until you feel more settled in your new role of mother.
- If you have intense feelings of sadness or severe mood swings, are crying often, having trouble sleeping, or having overwhelming feelings of worthlessness or guilt, contact your provider. These are some of the signs of postpartum depression (PPD). PPD requires treatment, and the sooner you get help the better.
When will I get my first postpartum period?
The date of your first postpartum period depends in part on when (and how much) you're breastfeeding. When you nurse your baby, your body produces the hormones prolactin and oxytocin, which typically suppress ovulation.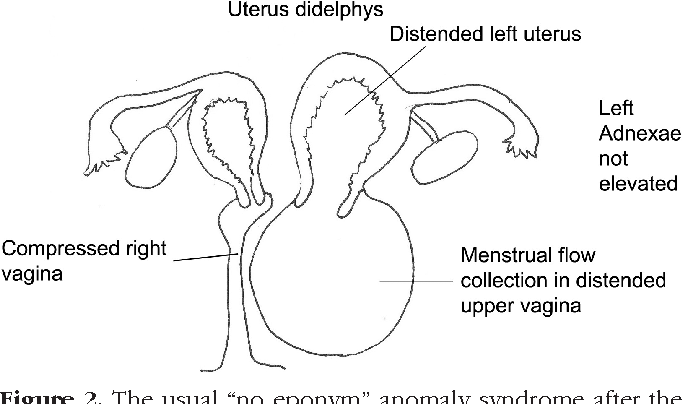 (And if you don't ovulate, you probably won't have a period – though it's possible.)
(And if you don't ovulate, you probably won't have a period – though it's possible.)
Most moms who don't breastfeed will get their first postpartum period in 6 to 8 weeks, while breastfeeding moms typically resume their periods between 9 and 18 months after childbirth.
Generally, the more you breastfeed, the more likely your period is to be delayed. Some moms who exclusively breastfeed don't get a period until they stop nursing. Other nursing moms get a period once their baby starts sleeping through the night, which cuts back on feeding times. Supplementing with formula or introducing solids is also likely to have an effect.
Don't depend on breastfeeding for birth control. You can get pregnant while breastfeeding. And keep in mind – breastfeeding or not – you can get pregnant before you have your first period (ovulation usually comes first!). If you get your period sooner than 6 weeks, don't use tampons. These can introduce bacteria and increase the chances of infection while your body is still healing.
When is it safe to exercise postpartum?
Check with your healthcare provider for individual guidelines. Your return to exercise will depend in part on how your pregnancy and delivery went.
Some pregnancy complications will affect your return to exercise. For example, if you had preeclampsia, your provider will want you to take it slowly because strenuous exercise can worsen your blood pressure.
If you had an uncomplicated vaginal delivery and exercised throughout your pregnancy, your practitioner may give you the go ahead to do light exercise – such as walks, postpartum yoga, modified push-ups and stretching – within days of delivery, as long as you're not in any pain. If you had complications, though, or you weren't active throughout your pregnancy, your provider will give you other guidelines for exercising. If you had a severe tear, for example, your provider may refer you to a physical therapist and urogynecologist before you jump back into exercise.
If you had a c-section, you can probably ease back into exercise six to eight weeks after delivery. Your provider will examine you – to make sure your incision is healed – and give you the go-ahead at your postpartum visit if all is well. Before that, you can walk for exercise and do stretches.
Whenever you start exercising postpartum, you may want to begin slowly, with 10 minutes or so of low-impact activity. You can increase the length of time or number of activities as you regain strength.
Read more:
C-section recovery
Postpartum warning signs
Diet for a healthy breastfeeding mom
advertisement | page continues below
Postpartum - recovery, nutrition, sex after childbirth
Yulia Novitsyuk, an obstetrician-gynecologist at the ISIDA clinic, talks about the basic rules of behavior in the postpartum period.
The postpartum period is divided into two parts: the early postpartum period (lasts about two hours from the moment the baby is born) and the late postpartum period (up to 8 weeks after birth).
In the early postpartum period, women in childbirth are in the delivery room, the baby is laid out on the mother's stomach, he is first applied to the breast. The condition of the woman is being closely monitored.
Two hours later, the mother and child are transferred to the postpartum ward, the late postpartum period begins, during which the woman's body is restored. What does it mean?
Restoration of physiological functions. Approximately four hours after delivery, the patient is asked to empty her bladder. Difficulties can arise with this, which can be overcome by trying to relax while sitting on the toilet. You can open the water, its murmur helps to empty the bladder. If this does not work, the doctor, having assessed the fullness of the bladder, may suggest the use of a catheter.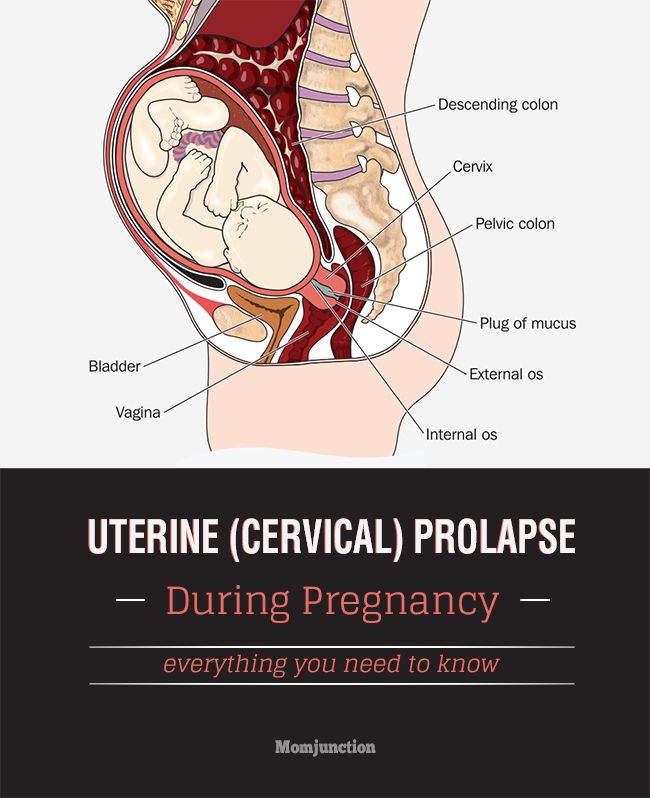
On the second day you need to empty the intestines. There can also be difficulties with this, since the intestines are compressed during childbirth, and after childbirth it changes its location in the abdominal cavity. But it is very important to start the work of the intestines in the first few days after childbirth. For this purpose, the correct diet is drawn up (foods high in pectins - apples, bananas, etc.). If the rhythmic work of the intestines is not restored, the doctor recommends resorting to microclysters. These are small tubes of medicine that are injected into the rectum and cause a bowel movement.
Lactation. Milk usually arrives on the third day. In ISIDA, already on the first day after childbirth, a breastfeeding specialist comes to the patients and tells in great detail and in a popular way how to apply the baby to the breast. Proper attachment to the breast is 90% of the success of breastfeeding.
Nutrition during breastfeeding. Nutrition after childbirth should be varied and balanced. The diet of a nursing woman should include meat, fish, vegetables, fruits, cereals, dairy products. During the first 10 days, it is necessary to start the rhythmic work of the mother's intestines, so the basis of the diet should be foods high in pectin. On the table of a nursing woman should be baked apples, bananas, cereals, vegetable soups, dried fruit soups, birch sap.
The diet of a nursing woman should include meat, fish, vegetables, fruits, cereals, dairy products. During the first 10 days, it is necessary to start the rhythmic work of the mother's intestines, so the basis of the diet should be foods high in pectin. On the table of a nursing woman should be baked apples, bananas, cereals, vegetable soups, dried fruit soups, birch sap.
New products should be introduced carefully. You can eat stewed vegetables - broccoli, cauliflower, carrots, beets, onions, zucchini, pumpkin. For snacks, you can use prunes, dried apricots, biscuit cookies, bagels, croutons without raisins. Butter - no more than 15 g per day, chicken, pork are not recommended. Eat rabbit, turkey. 10 days after birth, fermented milk products, boiled fish, black bread, boiled or baked potatoes, pasta from durum wheat are introduced. A little later, you can introduce hard cheese, but its fat content should not exceed 45%.
During breastfeeding, you should not eat raisins, mayonnaise, semi-finished products, sausages, sausages, smoked meats, fast food is unacceptable, alcohol is strictly prohibited.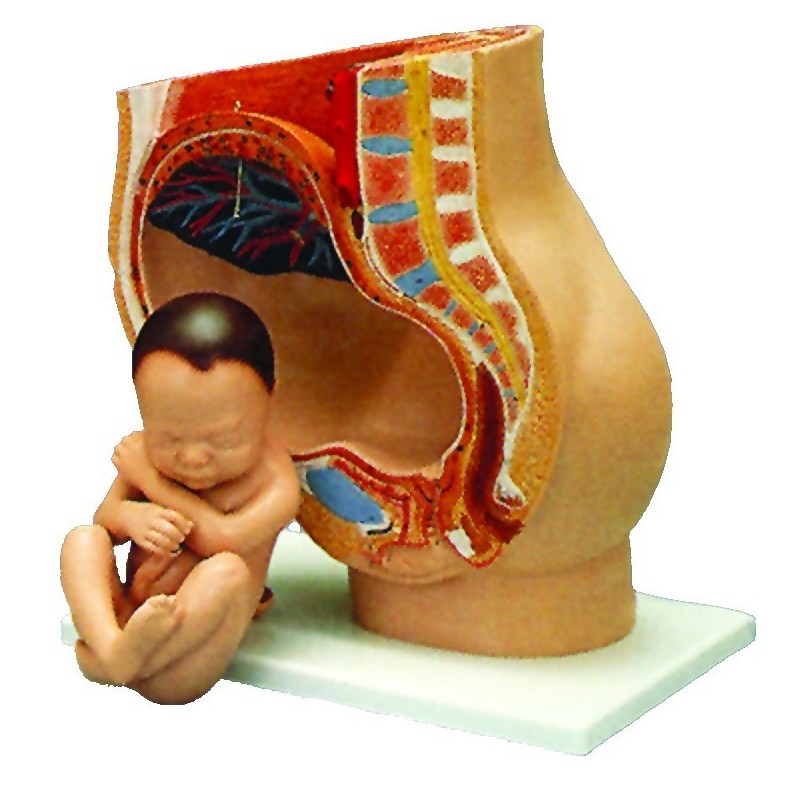 Also exclude sweet carbonated drinks, everything fatty and fried, strong broth is unacceptable. It is also not recommended to eat raw tomatoes, white cabbage - this can cause bloating in both you and the baby. If you can’t wake up without coffee, allow yourself one (maximum two) cups of a weak drink with milk.
Also exclude sweet carbonated drinks, everything fatty and fried, strong broth is unacceptable. It is also not recommended to eat raw tomatoes, white cabbage - this can cause bloating in both you and the baby. If you can’t wake up without coffee, allow yourself one (maximum two) cups of a weak drink with milk.
It is necessary to monitor the condition of the baby's skin, it is advisable to keep a food diary.
Drinking regimen during breastfeeding. Do not force yourself to drink through force. The amount of milk does not depend on the amount of liquid drunk, lactation is a hormone-dependent process. Drink as thirst arises, excess fluid is an extra burden on the kidneys and nothing more.
"Care" of the abdomen. Women giving birth for the first time usually cherish the dream that the belly will disappear once after childbirth. Unfortunately, they are disappointed. The abdomen cannot immediately decrease, because immediately after childbirth, the uterus weighs 800-1000 g.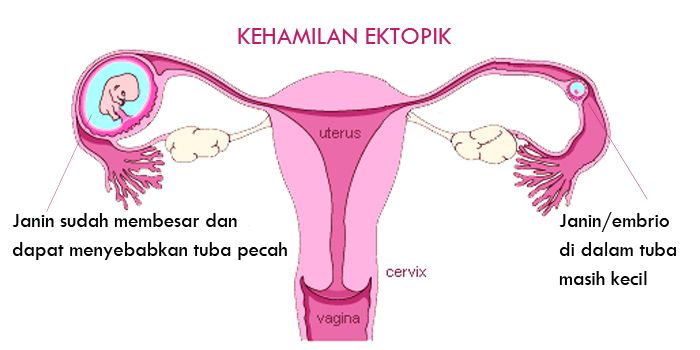 But already seven days after childbirth, the uterus weighs 400-500 g. And every day until the 12th day after childbirth, the height of the fundus of the uterus decreases by 2 cm. In the future, it decreases less intensively, but by about 6-8 weeks after birth, the uterus has its prenatal weight, which is 50-60 g. It should be noted that the active contraction of the uterus stimulates the frequent attachment of the baby to the breast.
But already seven days after childbirth, the uterus weighs 400-500 g. And every day until the 12th day after childbirth, the height of the fundus of the uterus decreases by 2 cm. In the future, it decreases less intensively, but by about 6-8 weeks after birth, the uterus has its prenatal weight, which is 50-60 g. It should be noted that the active contraction of the uterus stimulates the frequent attachment of the baby to the breast.
Postpartum discharge - lochia. Frequent application of the child to the breast also contributes to the expulsion of the postpartum secret from the uterus - lochia. A few days after childbirth, the discharge is abundant, often with clots, and may have a specific smell. By day 5-6, their number decreases, and the appearance also changes: a mucous component is added. After a few more days, the blood in the discharge becomes even less, the discharge becomes brownish, then yellowish, and finally - mucous. As a rule, by 6-8 weeks after birth, lochia disappear.
An important point: if within two weeks the discharge is abundant, but suddenly decreases or disappears sharply, you should consult a doctor. This is a very dangerous symptom!
Episiotomy . An episiotomy is a surgical incision in the perineum along the back wall of the vagina in order to prevent deep vaginal tears and also protect the baby from traumatic brain injury. This manipulation is usually resorted to in rapid labor, childbirth with a large fetus, labor with pelvic diligence, or preterm labor.
After the episiotomy, the sutures are sutured with a synthetic thread, which is completely absorbed after one and a half to two months. The seam must be kept clean and dry, treated with an antiseptic (ordinary brilliant green). Sometimes in the area of the seam, and then the scar, there is a violation of sensitivity. This is normal and will pass in 6-9 months.
Delivery by caesarean section. On the first day after the caesarean section, the woman is in intensive care, on the second day she is transferred to the postpartum department.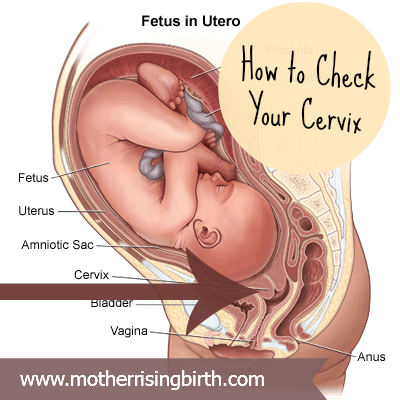 Seam care is normal, that is, brilliant green and air baths. To reduce the load, after a caesarean section, wearing a bandage is recommended. It is strictly forbidden to strain the press, physical education and sports are permissible no earlier than 6 months after childbirth. And it should be moderate physical activity - dancing, Pilates, yoga. Strength training equipment, tennis, active running are not recommended.
Seam care is normal, that is, brilliant green and air baths. To reduce the load, after a caesarean section, wearing a bandage is recommended. It is strictly forbidden to strain the press, physical education and sports are permissible no earlier than 6 months after childbirth. And it should be moderate physical activity - dancing, Pilates, yoga. Strength training equipment, tennis, active running are not recommended.
The next pregnancy after delivery by caesarean section is recommended no earlier than two years later. In this case, it is necessary to look at the scar on the uterus, if there is a niche there. These niches can be the cause of an inconsistent scar on the uterus - an indication for the next delivery by caesarean section.
Sex after childbirth. The uterus recovers within 6-8 weeks after childbirth, the vaginal mucosa is about the same. Therefore, you should not start an intimate life earlier than 6-8 weeks after childbirth. It is important to note that women often experience a decrease in libido, sometimes vaginal dryness. This is how the hormone estrogen works. His influence will soon decline. To eliminate dryness, you can use candles with hyaluronic acid, lubricants. It improves the quality of sexual life.
This is how the hormone estrogen works. His influence will soon decline. To eliminate dryness, you can use candles with hyaluronic acid, lubricants. It improves the quality of sexual life.
A “stretched” vagina after childbirth is another unpleasant moment from the point of view of sexual sensations. Wumbling helps to cope with this (in particular, Kegel exercises, vaginal cones). These classes can begin approximately 2 months after childbirth.
Postpartum contraception is a must! There is a stereotype that if a woman is breastfeeding, then she cannot become pregnant. This is not true. Contraceptives after childbirth are necessary, even if menstruation has not yet recovered.
The easiest method of contraception is condoms. The intrauterine device is very effective. If a woman has not yet menstruated, putting a spiral is more difficult, but possible.
The next method of contraception is hormonal contraceptives, the so-called mini-pills.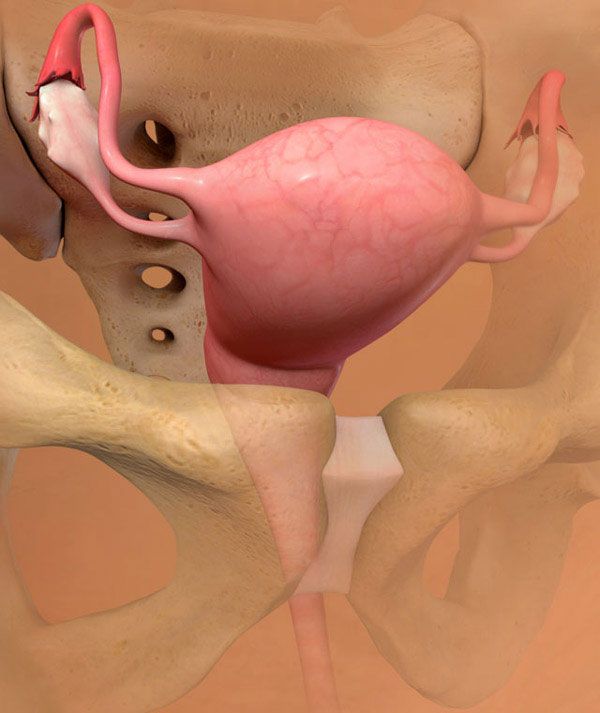 These are tablets with one hormone that acts at the level of the uterus and does not affect milk in any way. These pills are designed specifically for nursing mothers.
These are tablets with one hormone that acts at the level of the uterus and does not affect milk in any way. These pills are designed specifically for nursing mothers.
The next method is the use of spermicides - suppositories that are inserted into the vagina. They work well if done right.
The last method is sterilization. In women, this can occur during a caesarean section, with her consent. Sometimes men agree to sterilization.
Especially for those who want to know as much as possible about partner births, we have created a selection of materials on this topic. In the Partner Birth Toolkit , you'll find active links to video interviews with doctors, to flyer presentations with the most important logically structured information, and even an interesting celebrity birth interview.
For those who want to know as much as possible about childbirth, we have created a selection of materials on this topic. In the Childbirth Resource Kit you will find answers to most of your questions.
You can find out about the conditions of comprehensive pregnancy monitoring programs at the ISIDA clinic on our page Pregnancy management programs.
Are you looking for a clinic whose specialists you can trust with the birth of your baby? Trust the specialists of the ISIDA clinic: sign up for a consultation by calling 0800 60 80 80, +38 (044) 455 88 11. Or ask us your question and we will definitely answer it.
Share:
Recovery after childbirth
In most cases, the recovery of normal health is not rapid. The first sensation of incredible relief has passed, and now you notice that the stomach is still large, and even a little sore. To take its former size, the uterus must still be contracted for a long time and diligently. Its mass decreases from 1 kg to 50 g within 6-8 weeks.
Since the contraction of the uterus occurs due to the work of the muscles, this is accompanied by pain sensations of varying intensity, reminiscent of light contractions. You may notice an increase in pain while breastfeeding your baby. The thing is that stimulation of the nipple causes an increase in the level of oxytocin in the blood, which contributes to uterine contractions.
You may notice an increase in pain while breastfeeding your baby. The thing is that stimulation of the nipple causes an increase in the level of oxytocin in the blood, which contributes to uterine contractions.
For better uterine contraction, it is recommended to lie on your stomach after childbirth. If you feel good, try to move more and do gymnastics.
Another disturbing circumstance is pain in the perineum, which appears even if there were no tears and the doctor did not make an incision. This is due to the fact that the tissues have undergone a strong stretch during childbirth. Usually the pain is not very intense and disappears in 2-3 days. But if there were tears or a perineal incision, then it can hurt longer - 7-10 days. You should carefully monitor the seams, carry out hygiene after each visit to the toilet. In addition, it is necessary to treat the sutures daily with antiseptic solutions, you can not sit for 2 weeks.
Haemorrhoids often appear after childbirth.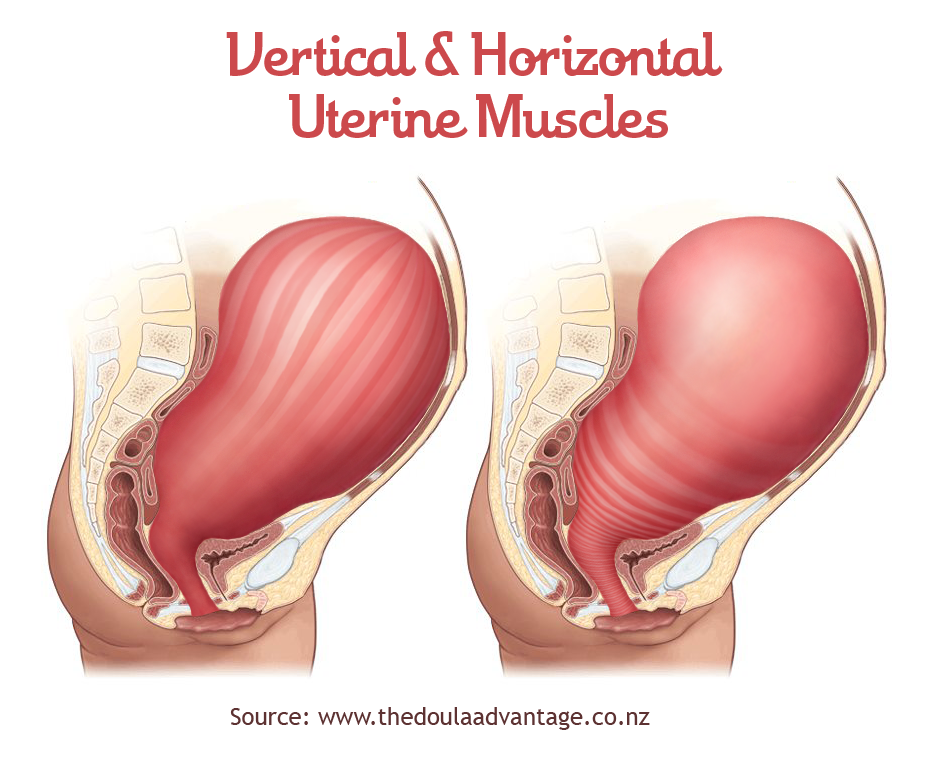 Careful hygiene and daily evening showers help reduce pain. Do not forget about the diet, include in your diet foods rich in fiber and with a slight laxative effect: seaweed, beets, baked apples, cauliflower, germinated cereals. Medications are usually not used because the inflammation usually goes away with time. If everything does not go away by itself and the woman continues to suffer from hemorrhoids, you need to consult a doctor and apply the medicines prescribed by him or take a course of physiotherapy procedures.
Careful hygiene and daily evening showers help reduce pain. Do not forget about the diet, include in your diet foods rich in fiber and with a slight laxative effect: seaweed, beets, baked apples, cauliflower, germinated cereals. Medications are usually not used because the inflammation usually goes away with time. If everything does not go away by itself and the woman continues to suffer from hemorrhoids, you need to consult a doctor and apply the medicines prescribed by him or take a course of physiotherapy procedures.
Constipation, which occurred during pregnancy, may also remind of itself in the postpartum period. They are, in particular, caused by the fear of damaging the seams in the perineum. However, such fear is unfounded. In addition, during a bowel movement, you can hold the area where the stitches are applied with a napkin, which will reduce the stretching of the tissues, and the bowel movement will be less painful. The chair usually does not happen immediately after childbirth, but after 2-3 days.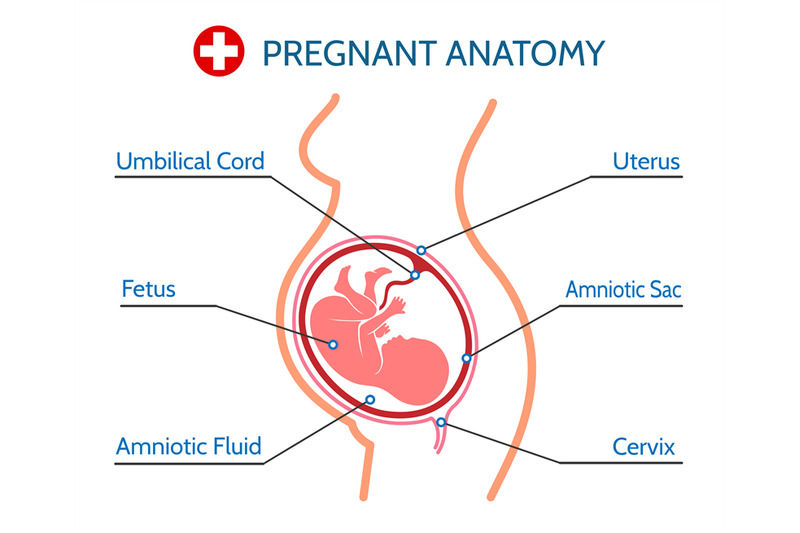 To prevent constipation, eat prunes and dried apricots, drink mineral water. And only if there was no bowel movement on the 3rd day, you can use a laxative candle.
To prevent constipation, eat prunes and dried apricots, drink mineral water. And only if there was no bowel movement on the 3rd day, you can use a laxative candle.
After childbirth, especially strong discharge from the uterus is observed on the first day, then it decreases. After 3 days, the discharge becomes muco-bloody. By the 5-6th week after birth, the discharge from the uterus stops altogether. During this period, hygiene must be carefully observed, because an infection that has entered the uterus can lead to endometritis (an inflammatory process of the uterine mucosa).
For 9 months, all the organs of the female body worked to ensure the child's proper development and good health. Now he was born and became quite "independent". However, the functions of a woman-mother did not end there. The main one - to provide the baby with food - is taken over by the mammary glands. In the body of a woman, hormonal changes continue, due to which significant changes occur in the mammary glands, and they begin to produce milk. In the first 2-3 days, colostrum is released, and already on the 3-4th day - transitional milk, which gradually turns into mature breast milk. Feeding your baby stimulates milk production. Therefore, in case of insufficient lactation, more frequent breastfeeding is recommended.
In the first 2-3 days, colostrum is released, and already on the 3-4th day - transitional milk, which gradually turns into mature breast milk. Feeding your baby stimulates milk production. Therefore, in case of insufficient lactation, more frequent breastfeeding is recommended.
However, women often face the opposite problem - an excess amount of milk and difficulty in its outflow. This, in turn, leads to its stagnation and engorgement of the mammary glands - they harden, increase in volume, and painful sensations appear in the chest area. It may even increase body temperature. How to prevent such occurrences?
First of all, try to breastfeed your baby regularly, and in the first 3-4 days after birth, limit fluid intake to 800 ml per day. Then the mammary glands will gradually become soft again. In addition, it is important to know that in the first days after childbirth, the skin of the nipples is very delicate and may crack. This makes them vulnerable to infection, the entry of which into the cracks is fraught with the development of mastopathy. Therefore, you need to take good care of the nipples and wear a comfortable bra, which will help the proper development of lactation.
Therefore, you need to take good care of the nipples and wear a comfortable bra, which will help the proper development of lactation.
To prevent cracks in the nipples, it is necessary to apply the baby to each breast in turn in the first 2-3 days after childbirth. First, give the baby one for 5-7 minutes, then another for 5-7 minutes. To prevent cracks, there is a special cream that needs to be used between feedings, and before them, carefully wash off its remnants.
That's all the troubles that are easily forgotten and seem not so significant against the background of new worries. Now your attention will be constantly occupied by the baby. However, it is very important not to forget about yourself, maintain your health and restore your former beauty. Not everyone succeeds, which contributes to the development of postpartum depression.
Lochiometer
After childbirth, under the influence of cellular enzymes secreted by the granulation shaft, blood clots and fragments of the decidua remaining on the walls of the uterus are liquefied.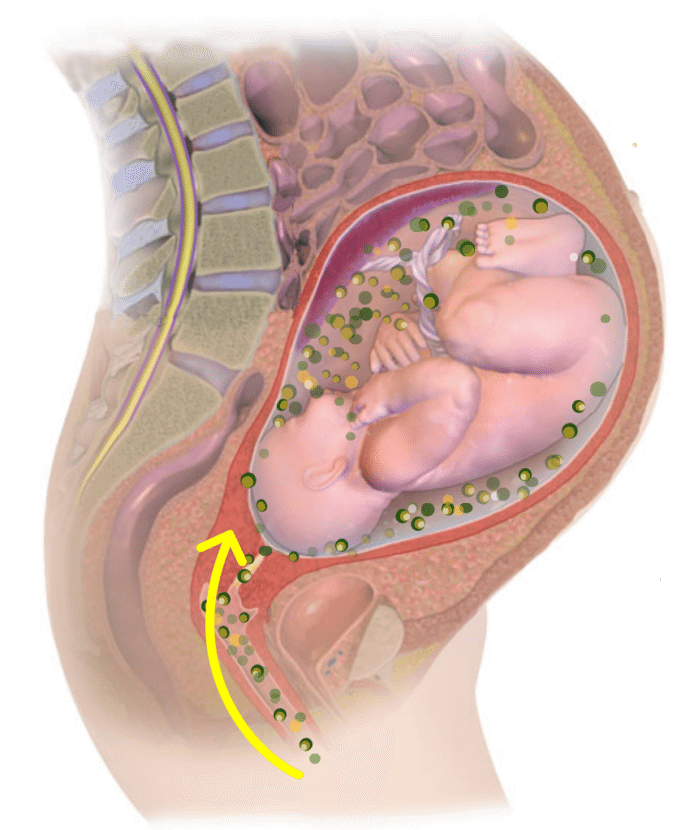 In addition, leukocytes, erythrocytes, plasma and lymph penetrate into the uterine cavity through the wound surface. All these elements form lochia - a postpartum wound secret, which normally actively flows from the uterine cavity through the cervical canal into the vagina.
In addition, leukocytes, erythrocytes, plasma and lymph penetrate into the uterine cavity through the wound surface. All these elements form lochia - a postpartum wound secret, which normally actively flows from the uterine cavity through the cervical canal into the vagina.
The first 2-3 days after birth, lochia have a bloody character, then, from the 4th-5th day, they acquire a dark red and brownish hue, and after a week they become yellowish-white due to the high content of leukocytes. From the 10th day, the discharge becomes light, watery, serous-mucous consistency. Gradually, the number of lochia decreases, and by the end of the 3rd week, the discharge practically stops and soon disappears completely.
With a delay in the outflow of postpartum secretions, they speak of a lochiometer - stagnation of lochia in the uterine cavity. The danger of developing lochiometers lies in the high probability of infection of the contents of the uterus, since lymph, serum, blood, and tissue remnants serve as the best nutrient medium for the reproduction of microbial flora. Most often, against the background of lochiometers, endometritis develops.
Most often, against the background of lochiometers, endometritis develops.
Causes of the development of lochiometers
The development of lochiometers is due to mechanical obstacles to the outflow of secretions in the cervical canal or insufficient uterine contractility.
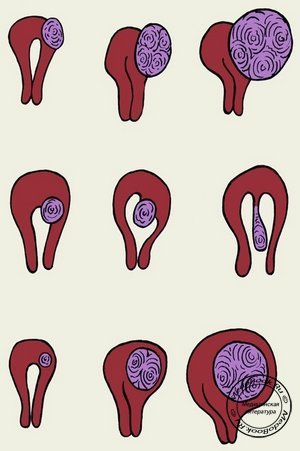
Mechanical obstruction may be due to kinking (hyperanteflexia) of the uterus or obstruction of the cervical canal by blood clots, remnants of the decidua and flaking uterine tissue.
Insufficient contractile activity of the uterus in the postpartum period usually develops as a result of overstretching of the uterus (with a large fetus, polyhydramnios or multiple pregnancy), weak or discoordinated labor, spasm of the internal os, caesarean section.
The development of lochiometers is facilitated by prolonged bed rest and low activity after childbirth.
Symptoms of lochiometer
Lochiometer develops on the 5th-7th day after childbirth, characterized by a noticeable decrease or cessation of postpartum discharge from the uterus.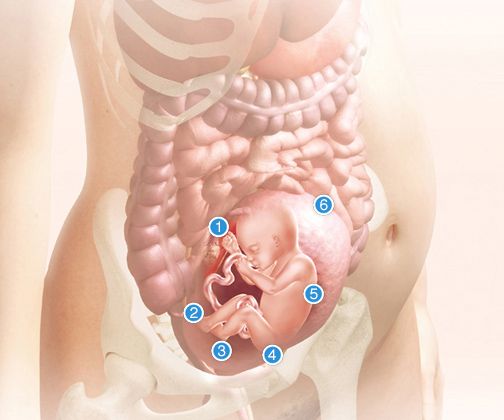 At the same time, there is an increase in the size of the uterus compared to the norm for the current postpartum day, its soreness on palpation. The general health and objective condition of a woman with a lochiometer does not suffer, body temperature is normal, tachycardia is absent.
At the same time, there is an increase in the size of the uterus compared to the norm for the current postpartum day, its soreness on palpation. The general health and objective condition of a woman with a lochiometer does not suffer, body temperature is normal, tachycardia is absent.
When delaying timely therapeutic tactics in relation to lochiometers, fever appears (body temperature 38-40 ° C), chills, cramping pains, turbid discharge with an unpleasant odor, tachycardia. After 1-2 days, the temperature drops critically with the simultaneous appearance of liquid purulent lochial discharge.
Diagnosis lochiometer
Lochiometer is diagnosed by characteristic clinical signs. With the help of a gynecological examination, an unevenly enlarged and painful uterus is determined, which has a densely elastic consistency, often - the closure of the internal pharynx, the bend of the uterus.
Clarifying lochiometer diagnostics includes ultrasound. during which the expansion of the uterine cavity is revealed, the presence of hyperechoic blood clots and liquid blood in it.
Treatment of lochiometers
Treatment of lochiometers consists in ensuring the free outflow of lochia, taking into account the cause that caused this condition.
When lochiometers are detected, the gynecologist prescribes injections of antispasmodics (papaverine, no-shpy) to relieve spasm of the uterine os. In the treatment of lochiometers, uterotonic (contracting the uterus) agents are used - oxytocin, methylergometrine. For a free outflow of secretions, the puerperal is recommended to lie on her stomach 2-3 times a day for 1-2 hours.
In case of hyperanteflexia of the uterus, the bend is eliminated during a bimanual examination; exercise therapy is prescribed. In the case of a lochiometer due to blockage of the cervical canal by clots, when viewed on a chair, digital dilatation of the cervical canal and careful removal of clots are performed.
Situations when the lochiometer is not allowed within 2-3 days are considered by clinical gynecology as an indication for instrumental removal of the contents of the uterus with a curette or vacuum apparatus under hysteroscopy control. For the prevention and treatment of postpartum infections against the background of lochiometers, antibiotics are prescribed, taking into account the results of a bacteriological smear.
For the prevention and treatment of postpartum infections against the background of lochiometers, antibiotics are prescribed, taking into account the results of a bacteriological smear.
Complications of lochiometers
If, after the elimination of lochiometers, uterine tenderness, its poor contraction, hyperthermia persist, one should think about the development of postpartum metroendometritis.
If the infection progresses, the condition of the puerperal may worsen due to the development of purulent-resorptive fever, manifested by intoxication, abdominal pain, purulent discharge with a putrid odor. Against this background, the transition of lochiometers to pyometra is noted.
Prophylaxis and prognosis with lochiometer
To prevent the development of lochiometers, competent management of pregnancy and preparation of the woman for childbirth are required, as well as careful monitoring of the puerperal during the postpartum period: regular monitoring of uterine contractions (daily palpation determination of its sensitivity, consistency, fundus height), volume and nature of discharge .