When to do nuchal translucency
Nuchal translucency test Information | Mount Sinai
Nuchal translucency screening; NT; Nuchal fold test; Nuchal fold scan; Prenatal genetic screening; Down syndrome - nuchal translucency
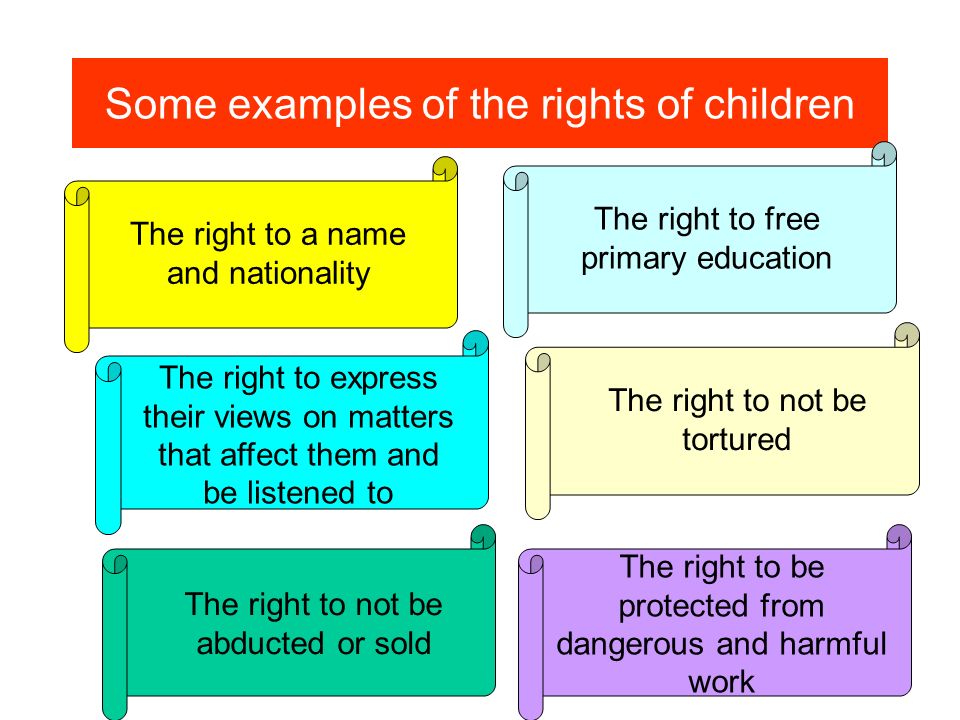
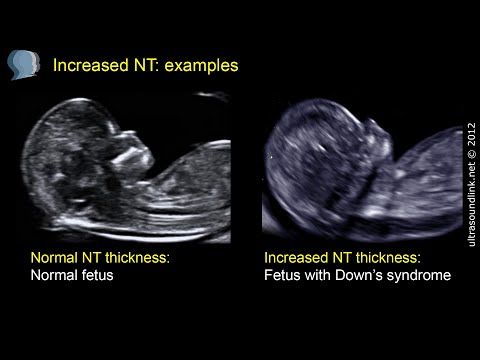
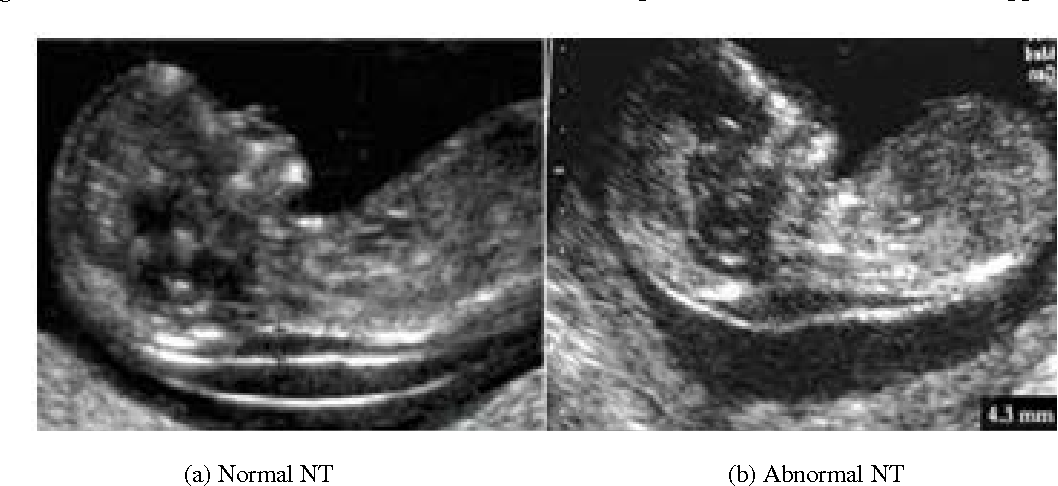
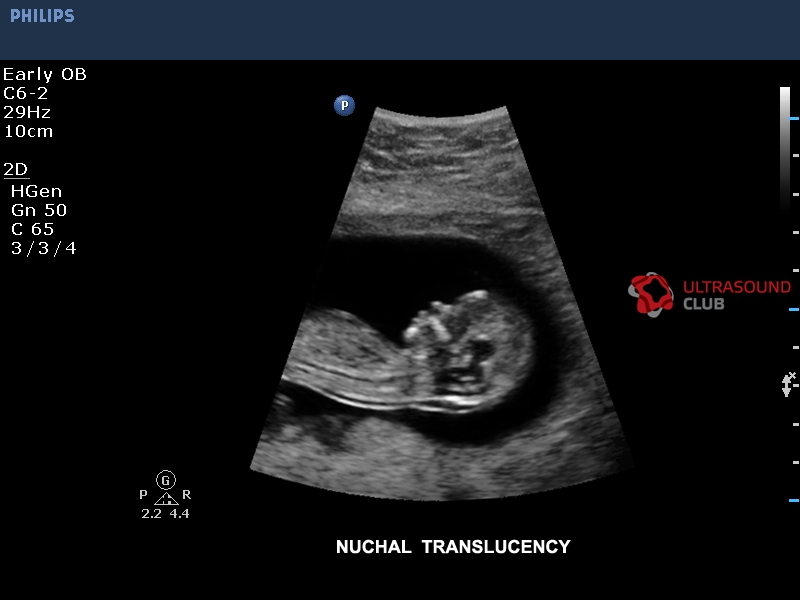
The nuchal translucency test measures the nuchal fold thickness. This is an area of tissue at the back of an unborn baby's neck. Measuring this thickness helps assess the risk for Down syndrome and other genetic problems in the baby.
How the Test is Performed
Your health care provider uses abdominal ultrasound (not vaginal) to measure the nuchal fold. All unborn babies have some fluid at the back of their neck. In a baby with Down syndrome or other genetic disorders, there is more fluid than normal. This makes the space look thicker.
A blood test of the mother is also done. Together, these two tests will tell if the baby could have Down syndrome or another genetic disorder.
How to Prepare for the Test
Having a full bladder will give the best ultrasound picture. You may be asked to drink 2 to 3 glasses of liquid an hour before the test. DO NOT urinate before your ultrasound.
How the Test will Feel
You may have some discomfort from pressure on your bladder during the ultrasound. The gel used during the test may feel slightly cold and wet. You will not feel the ultrasound waves.
The gel used during the test may feel slightly cold and wet. You will not feel the ultrasound waves.
Why the Test is Performed
Your provider may advise this test to screen your baby for Down syndrome. Many pregnant women decide to have this test.
Nuchal translucency is usually done between the 11th and 14th week of pregnancy. It can be done earlier in pregnancy than amniocentesis. This is another test that checks for birth defects.
Normal Results
A normal amount of fluid in the back of the neck during ultrasound means it is very unlikely your baby has Down syndrome or another genetic disorder.
Nuchal translucency measurement increases with gestational age. This is the period between conception and birth. The higher the measurement compared to babies the same gestational age, the higher the risk is for certain genetic disorders.
The measurements below are considered low risk for genetic disorders:
- At 11 weeks -- up to 2 mm
- At 13 weeks, 6 days -- up to 2.8 mm
What Abnormal Results Mean
More fluid than normal in the back of the neck means there is a higher risk for Down syndrome, trisomy 18, trisomy 13, Turner syndrome, or congenital heart disease. But it does not tell for certain that the baby has Down syndrome or another genetic disorder.
If the result is abnormal, other tests can be done. Most of the time, the other test done is amniocentesis.
Risks
There are no known risks from ultrasound.
Driscoll DA, Simpson JL. Genetic screening and diagnosis. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 10.
Walsh JM, D'Alton ME. Nuchal translucency. In: Copel JA, D'Alton ME, Feltovich H, et al, eds. Obstetric Imaging: Fetal Diagnosis and Care. 2nd ed. Philadelphia, PA: Elsevier; 2018:chap 45.
2nd ed. Philadelphia, PA: Elsevier; 2018:chap 45.
Last reviewed on: 3/31/2020
Reviewed by: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
First Trimester Ultrasound and Nuchal Translucency – San Diego Perinatal Center
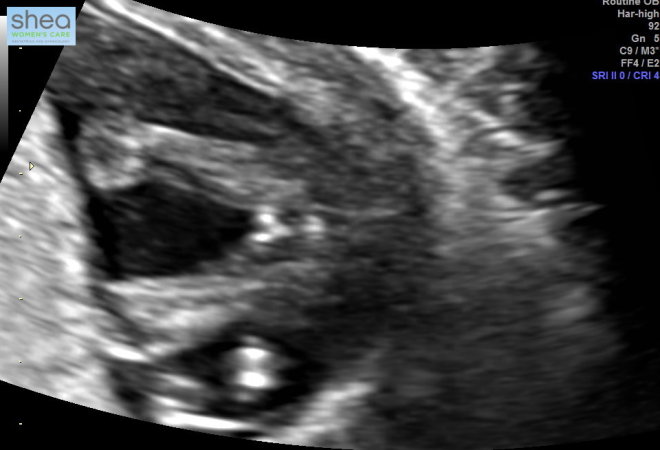
First trimester ultrasound performed between 11 and 14 weeks is an important early assessment of your pregnancy. This scan can be used to accurately date your pregnancy, to evaluate abnormalities in your ovaries and cervix, to accurately determine chorionicity in twins, to assess for placental abnormalities and to perform a nuchal translucency screen. In addition, at San Diego Perinatal Center, with our high resolution equipment, we are able to detect 40% of major fetal anomalies such as neural tube defects, abdominal wall defects, renal, limb and cardiac abnormalities on this early scan.
Nuchal translucency/First trimester screening – this blood test screens for Down Syndrome (Trisomy 21) and Trisomy 18. It is part of the California Prenatal Screening Program and is a free service to all pregnant women. Additional testing and counseling would be recommended if the test is positive. This test has about an 85 % detection rate for Down Syndrome.
Nuchal Translucency Screening for Detecting Trisomy 21 (Down Syndrome) and Trisomy 18.
During development of the embryo, there is a clear space beneath the skin at the back of the neck which we call the nuchal translucency. Between 11 and 14 weeks of pregnancy, this space can be measured by ultrasound and the size of this space is associated with the risk for fetal chromosome abnormalities and the risk for fetal heart defects. We use this measurement as an early screening tool to identify pregnancies at higher risk for these conditions.
If we can accurately measure the nuchal translucency, then a computer program can be used to calculate the risk for Down Syndrome and Trisomy 18 using the mother’s age and blood hormone markers. Women who screen positive at increased risk would then be offered further testing. The nuchal translucency screen will identify 85-90 percent of Down syndrome cases and 80-85 percent of Trisomy 18 cases. Approximately 5-10% of the time, we are unable to obtain this measurement either because the baby does not cooperate or there are other technical factors like abdominal wall scarring, fibroids or maternal obesity.
Women who screen positive at increased risk would then be offered further testing. The nuchal translucency screen will identify 85-90 percent of Down syndrome cases and 80-85 percent of Trisomy 18 cases. Approximately 5-10% of the time, we are unable to obtain this measurement either because the baby does not cooperate or there are other technical factors like abdominal wall scarring, fibroids or maternal obesity.
In the State of California, there is a prenatal screening program which is used for risk calculations. The state requires that all first and second trimester blood specimens are performed in the state laboratory system. https://www.cdph.ca.gov/Programs/CFH/DGDS/Pages/pns/
It is important to realize that the only way to be certain that a baby does not have a numeric chromosome abnormality like Down syndrome is by means of Amniocentesis or Chorionic Villous sampling.
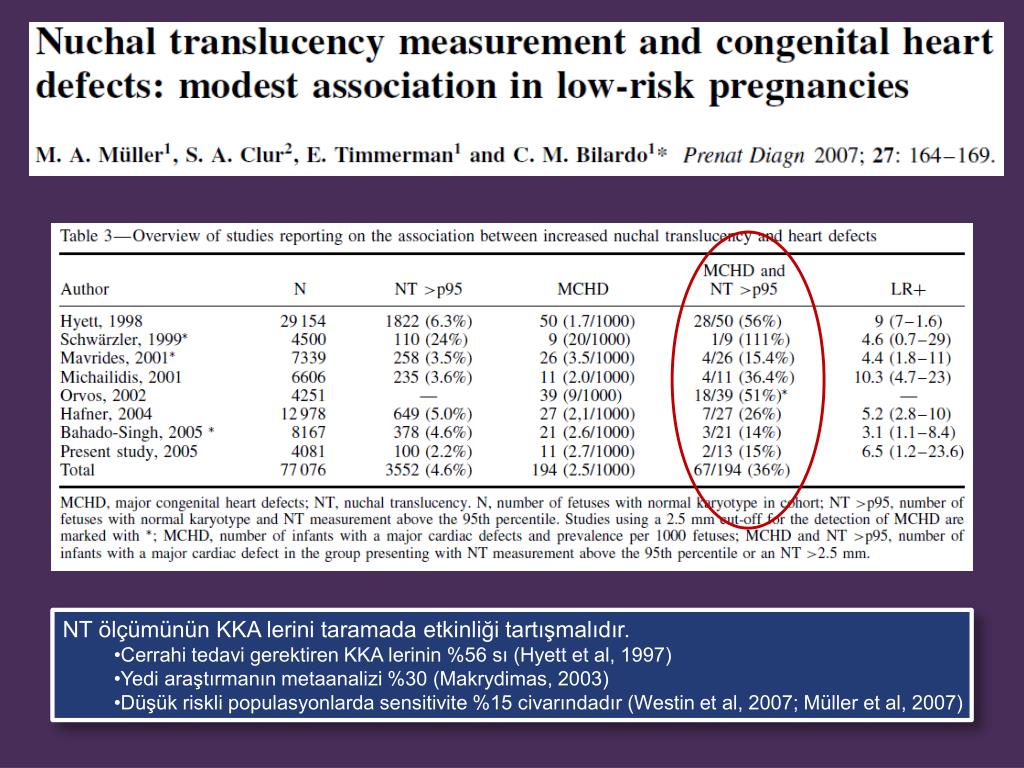
Risk for Other Birth Defects
The nuchal translucency measurement is more than just a screening for Down syndrome. A very small nuchal translucency measurement – less than 2.5 mm – places the pregnancy in a low-risk group for problems, such as fetal heart abnormalities. Pregnancies where the nuchal translucency measurement is between about 2.5 and 3.5 mm are in an intermediate-risk group, and for these women, a genetic sonogram at about 18 weeks into the pregnancy plus a detailed sonogram of the heart (called a fetal echocardiogram) at about 22 weeks are recommended. Women with a nuchal translucency measurement of 3.5 mm or more have pregnancies at increased risk for chromosome problems, for abnormalities of the fetal heart, and for other birth defects, ranging from abnormalities of the skeletal system to the baby’s diaphragm. For these pregnancies, genetic counseling and a genetic sonogram at 18 weeks, and a fetal echocardiogram and a detailed scan at about 22 weeks, are recommended.
A very small nuchal translucency measurement – less than 2.5 mm – places the pregnancy in a low-risk group for problems, such as fetal heart abnormalities. Pregnancies where the nuchal translucency measurement is between about 2.5 and 3.5 mm are in an intermediate-risk group, and for these women, a genetic sonogram at about 18 weeks into the pregnancy plus a detailed sonogram of the heart (called a fetal echocardiogram) at about 22 weeks are recommended. Women with a nuchal translucency measurement of 3.5 mm or more have pregnancies at increased risk for chromosome problems, for abnormalities of the fetal heart, and for other birth defects, ranging from abnormalities of the skeletal system to the baby’s diaphragm. For these pregnancies, genetic counseling and a genetic sonogram at 18 weeks, and a fetal echocardiogram and a detailed scan at about 22 weeks, are recommended.
In the past, sonography at 11 to 14 weeks was not an effective way to screen for birth defects of the baby. The embryo at that stage was just too small to evaluate well. As time has gone on, the ultrasound equipment and our ability to interpret the images have both improved. Now, at the 11 to 14-week scan, we are able to identify many major central nervous system, cardiac, abdominal, and limb abnormalities. Our center’s goal is to identify 40 percent of major structural malformations at the time of the nuchal translucency scan.
The embryo at that stage was just too small to evaluate well. As time has gone on, the ultrasound equipment and our ability to interpret the images have both improved. Now, at the 11 to 14-week scan, we are able to identify many major central nervous system, cardiac, abdominal, and limb abnormalities. Our center’s goal is to identify 40 percent of major structural malformations at the time of the nuchal translucency scan.
When is the best time to schedule a nuchal translucency scan?
The accuracy is highest when the lab work is done between 10 and 11 weeks into the pregnancy, and we recommend scheduling the nuchal scan between 12 and 13 weeks. As long as the lab test has been done more than a week before, we should be able to provide you with the Down syndrome and trisomy 18 risk calculations at the time of your ultrasound scan.
Prenatal screening - the most complete information
The Center for Immunology and Reproduction has been successfully operating for many years the prenatal screening program . Our specialists are invited to give lectures at specialized conferences and in other clinics. Our laboratory receives consistently good marks in the quality control system. Specially trained specialists carry out risk assessment.
Our specialists are invited to give lectures at specialized conferences and in other clinics. Our laboratory receives consistently good marks in the quality control system. Specially trained specialists carry out risk assessment.
Prenatal Screening Program at CIR
Contents
What is prenatal diagnosis?
The word prenatal means prenatal. Therefore, the term "prenatal diagnosis" means any research that allows you to clarify the condition of the fetus. Since human life begins from the moment of conception, various health problems can occur not only after birth, but also before birth. Problems can be different:
- fairly harmless, which the fetus can handle on its own,
- more serious, when timely medical care will save the health and life of the intrauterine patient,
- are heavy enough that modern medicine cannot handle.
To determine the state of health of the fetus, prenatal diagnostic methods are used, which include ultrasound, cardiotocography, various biochemical studies, etc.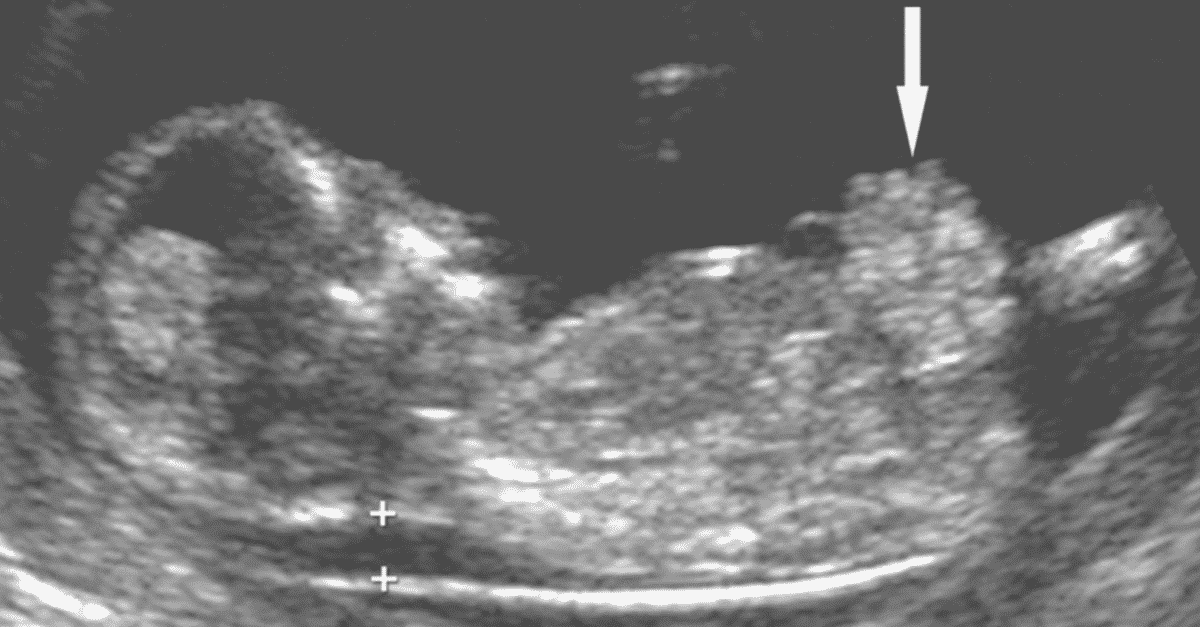 All these methods have different capabilities and limitations. Some methods are quite safe, such as ultrasound. Some carry some risk to the fetus, such as amniocentesis (amniotic fluid sampling) or chorionic villus sampling.
All these methods have different capabilities and limitations. Some methods are quite safe, such as ultrasound. Some carry some risk to the fetus, such as amniocentesis (amniotic fluid sampling) or chorionic villus sampling.
It is understood that prenatal diagnostic methods that carry the risk of pregnancy complications should only be used when there are strong indications for their use. In order to narrow the circle of patients who need invasive (i.e., those associated with intervention in the body) methods of prenatal diagnosis as much as possible, risk groups are used to identify risk groups for the development of certain problems in the fetus.
What are risk groups?
Risk groups are such groups of patients among whom the probability of detecting a particular pathology of pregnancy is higher than in the entire population (among all women in a given region). There are risk groups for the development of miscarriage, gestosis (late toxicosis), various complications in childbirth, etc.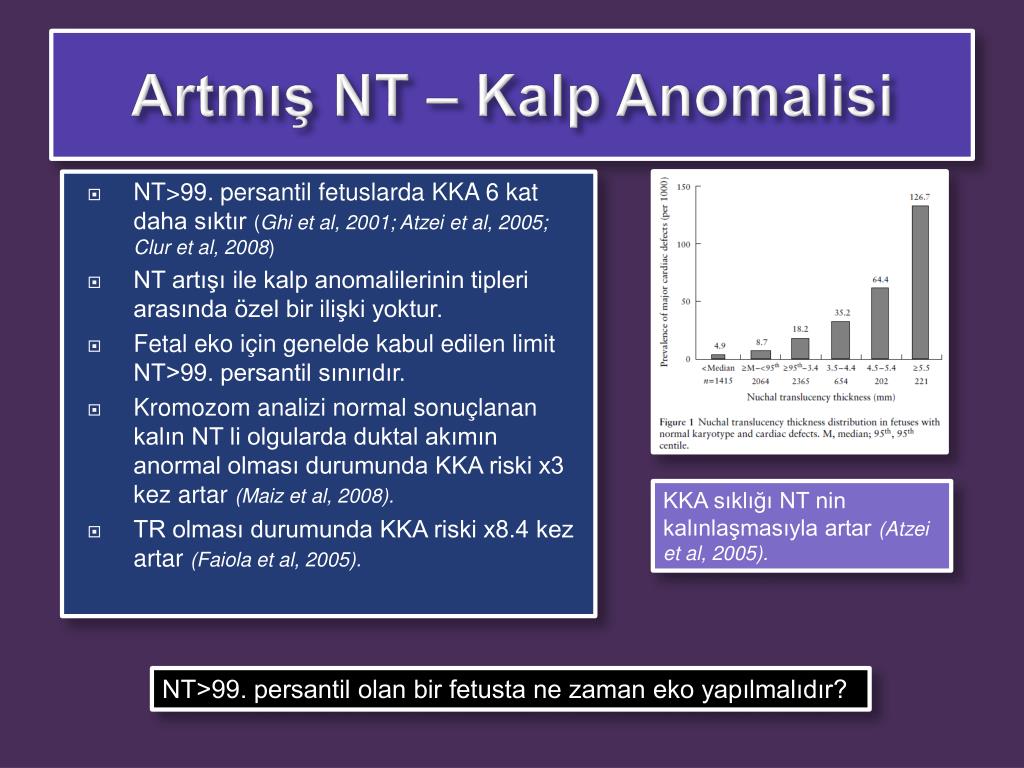 If a woman, as a result of an examination, is at risk for a particular pathology, this does not mean that this pathology will necessarily develop. This only means that in this patient one or another type of pathology may occur with a greater probability than in other women. Thus, the risk group is not identical to the diagnosis. A woman may be at risk, but there may not be any problems during pregnancy. And vice versa, a woman may not be at risk, but she may have a problem. Diagnosis means that this or that pathological condition has already been detected in this patient.
If a woman, as a result of an examination, is at risk for a particular pathology, this does not mean that this pathology will necessarily develop. This only means that in this patient one or another type of pathology may occur with a greater probability than in other women. Thus, the risk group is not identical to the diagnosis. A woman may be at risk, but there may not be any problems during pregnancy. And vice versa, a woman may not be at risk, but she may have a problem. Diagnosis means that this or that pathological condition has already been detected in this patient.
Why are risk groups needed?
Knowing that the patient is in a particular risk group helps the doctor to plan the tactics of pregnancy and childbirth. Identification of risk groups helps protect patients who are not at risk from unnecessary medical interventions, and vice versa, allows you to justify the appointment of certain procedures or studies for patients at risk.
What is screening?
The word screening means "sifting". In medicine, screening is understood as the conduct of simple and safe studies of large groups of the population in order to identify risk groups for the development of a particular pathology. Prenatal screening refers to studies conducted on pregnant women to identify risk groups for pregnancy complications. A special case of prenatal screening is screening to identify risk groups for the development of congenital malformations in the fetus. Screening does not allow to identify all women who may have a particular problem, but it makes it possible to identify a relatively small group of patients, within which most of the people with this type of pathology will be concentrated.
In medicine, screening is understood as the conduct of simple and safe studies of large groups of the population in order to identify risk groups for the development of a particular pathology. Prenatal screening refers to studies conducted on pregnant women to identify risk groups for pregnancy complications. A special case of prenatal screening is screening to identify risk groups for the development of congenital malformations in the fetus. Screening does not allow to identify all women who may have a particular problem, but it makes it possible to identify a relatively small group of patients, within which most of the people with this type of pathology will be concentrated.
Why screening for fetal malformations?
Some types of congenital malformations in the fetus are quite common, for example, Down's syndrome (trisomy 21 or trisomy 21) - in one case in 600 - 800 newborns. This disease, as well as some other congenital diseases, occurs at the moment of conception or at the earliest stages of embryonic development, and with the help of invasive methods of prenatal diagnosis (chorionic villus biopsy and amniocentesis) can be diagnosed at a fairly early stage of pregnancy. However, such methods are associated with a risk of a number of pregnancy complications: miscarriage, the development of a conflict according to the Rh factor and blood type, infection of the fetus, the development of hearing loss in a child, etc. In particular, the risk of miscarriage after such studies is 1:200. Therefore, these studies should be prescribed only to women in high risk groups. Risk groups include women over 35 and especially over 40, as well as patients with the birth of children with malformations in the past. However, children with Down syndrome can also be born to very young women. Screening methods - completely safe studies conducted at certain stages of pregnancy - allow with a very high degree of probability to identify groups of women at risk of Down syndrome who may be indicated for a chorionic villus biopsy or amniocentesis. Women who are not at risk do not need additional invasive studies. Finding an increased risk of fetal malformations through screening methods is not a diagnosis.
However, such methods are associated with a risk of a number of pregnancy complications: miscarriage, the development of a conflict according to the Rh factor and blood type, infection of the fetus, the development of hearing loss in a child, etc. In particular, the risk of miscarriage after such studies is 1:200. Therefore, these studies should be prescribed only to women in high risk groups. Risk groups include women over 35 and especially over 40, as well as patients with the birth of children with malformations in the past. However, children with Down syndrome can also be born to very young women. Screening methods - completely safe studies conducted at certain stages of pregnancy - allow with a very high degree of probability to identify groups of women at risk of Down syndrome who may be indicated for a chorionic villus biopsy or amniocentesis. Women who are not at risk do not need additional invasive studies. Finding an increased risk of fetal malformations through screening methods is not a diagnosis.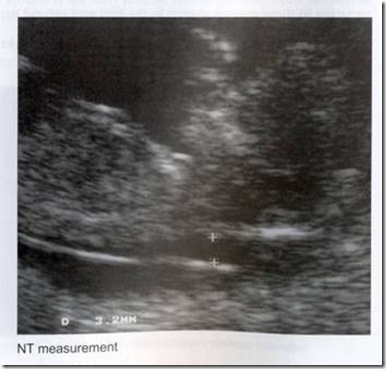 The diagnosis can be made or rejected with additional tests.
The diagnosis can be made or rejected with additional tests.
What types of birth defects are screened for?
Screening for the following types of birth defects in fetuses is currently recommended:
- Down syndrome (trisomy twenty-first pair of chromosomes)
- Edwards syndrome (trisomy eighteenth pair)
- Neural tube defects (spina bifida and anencephaly)
- Risk of trisomy 13 (Patau syndrome)
- Maternal triploidy
- Shereshevsky-Turner syndrome without dropsy
- Smith-Lemli-Opitz syndrome
- Corneli de Lange Syndrome
What types of testing are done to screen for the risk of fetal malformations?
According to types of research allocate:
- Biochemical screening : blood test for various indicators
- Ultrasound screening : detection of signs of developmental anomalies using ultrasound.

- Combined screening : Combination of biochemical and ultrasound screenings.
The general trend in the development of prenatal screening is the desire to obtain reliable information about the risk of developing certain disorders as early as possible in pregnancy. It turned out that the combined screening at the end of the first trimester of pregnancy (terms of 10–13 weeks) makes it possible to approach the effectiveness of classical biochemical screening of the second trimester of pregnancy.
Ultrasound screening, used for mathematical treatment of the risks of fetal anomalies, is performed only 1 time: at the end of the first trimester of pregnancy.
As for biochemical screening , the set of indicators will be different at different stages of pregnancy. During pregnancy 10-13 weeks the following indicators are checked:
- free β-subunit of human chorionic hormone (free β-hCG)
- PAPP-A (pregnancy associated plasma protein A), pregnancy-associated plasma protein A
The calculation of the risk of measuring fetal abnormalities based on the measurement of these parameters is called the first trimester double biochemistry test .
Using a double test in the first trimester, the risk of detecting Down syndrome (T21) and Edwards syndrome (T18) , trisomy 13 chromosome (Patau syndrome), triploidy of maternal origin, Shereshevsky-Turner syndrome without hydrocele is calculated. The risk of neural tube defects cannot be calculated using the dual test, since the key indicator for determining this risk is α-fetoprotein, which begins to be determined only from the second trimester of pregnancy.
Special computer programs allow calculating the combined risk of fetal abnormalities, taking into account the biochemical parameters determined in the double test of the first trimester and the results of an ultrasound done at 10-13 weeks of pregnancy. This test is called combined with TVP first trimester double test or first trimester triple test. The results of risk calculations obtained using a combined double test are much more accurate than risk calculations based only on biochemical parameters or only on the basis of ultrasound.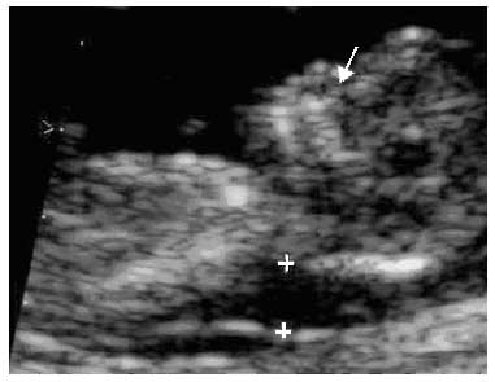
If the results of the test in the first trimester indicate a risk group for chromosomal abnormalities of the fetus, a chorionic villus biopsy can be performed to exclude the diagnosis of chromosomal abnormalities.
During pregnancy 14 - 20 weeks after the last menstruation ( recommended period: 16-18 weeks ) the following biochemical parameters are determined:
- Total hCG or free β-subunit of hCG
- α-fetoprotein (AFP)
- Free (unconjugated) estriol
- Inhibin A
Based on these indicators, the following risks are calculated:
- Down syndrome (trisomy 21)
- Edwards syndrome (trisomy 18)
- neural tube defects (non-closure of the spinal canal (spina bifida) and anencephaly).
- Risk of trisomy 13 (Patau syndrome)
- Maternal triploidy
- Shereshevsky-Turner syndrome without dropsy
- Smith-Lemli-Opitz syndrome
- Corneli de Lange Syndrome
This test is called Second Trimester Quadruple Test or Second Trimester Quadruple Biochemical Screening . A truncated version of the test is the so-called triple or double tests of the second trimester, which includes 2 or indicators: hCG or free hCG β-subunit, AFP, free estriol. It is clear that the accuracy of the double or double II trimester test is lower than the accuracy of the quadruple II trimester test.
A truncated version of the test is the so-called triple or double tests of the second trimester, which includes 2 or indicators: hCG or free hCG β-subunit, AFP, free estriol. It is clear that the accuracy of the double or double II trimester test is lower than the accuracy of the quadruple II trimester test.
Another option for biochemical prenatal screening is biochemical screening for the risk of second trimester neural tube defects only . In this case, only one biochemical marker is determined: α-fetoprotein
At what time of pregnancy is the second trimester screening performed?
At 14 to 20 weeks pregnant. The optimal period is 16 - 18 weeks of pregnancy.
What is a 2nd trimester quad test?
The main option for biochemical screening of the second trimester in the CIR is the so-called quadruple test, when the determination of inhibin A is added to the determination of the three above indicators.
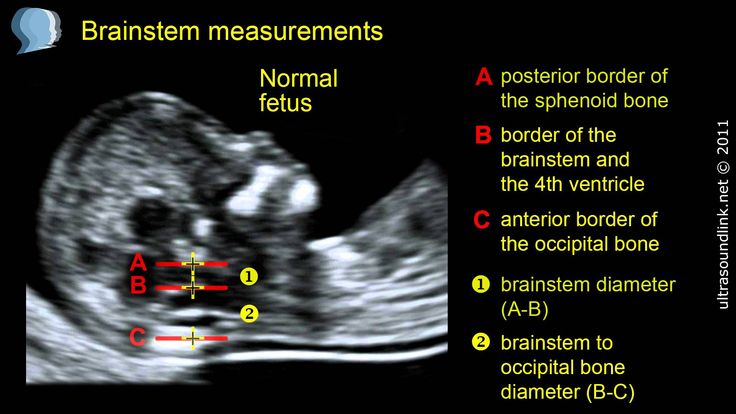
Ultrasound screening in the first trimester of pregnancy.
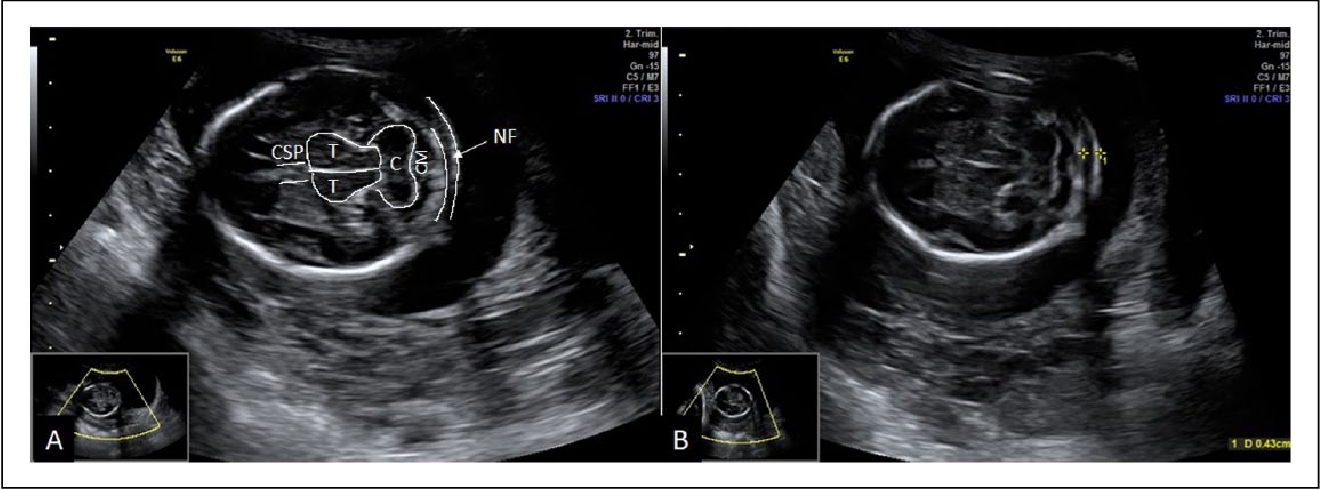
In the first trimester of pregnancy, the main measurement used in calculating risks is the width of the cervical translucency (English "nuchal translucency" (NT) , French "clarté nuchale"). In Russian medical usage, this term is often translated as "collar space" (TVP) or "neck fold". Cervical transparency, nuchal space and cervical fold are full synonyms that can be found in various medical texts and mean the same thing.
Cervical transparency - definition
- Cervical transparency is the ultrasound appearance of the accumulation of subcutaneous fluid on the back of the neck of the fetus in the first trimester of pregnancy
- The term "cervical transparency" is used regardless of whether it has septa or whether it is limited to the cervical region or surrounds the entire fetus
- The frequency of chromosomal and other anomalies is primarily related to the width of the transparency, and not how it looks in general
- During the second trimester, the transparency usually resolves, but in some cases it can turn into either cervical edema or cystic hygromas with or without generalized edema.

Cervical translucency measurement
Gestational age and coccyx-parietal size
The optimal gestational age for cervical translucency measurement is between 11 weeks and 13 weeks 6 days. The minimum size of the KTP is 45 mm, the maximum is 84 mm.
There are two reasons for choosing 11 weeks as the earliest time to measure CVP:
- Screening requires the ability to perform chorionic villus biopsy before the test can be complicated by fetal limb amputation.
- On the other hand, many gross fetal defects can only be detected after 11 weeks of gestation.
- The diagnosis of omphalocele is only possible after 12 weeks.
- Diagnosis of anencephaly is possible only after 11 weeks of pregnancy, since only from this period do ultrasound signs of ossification of the fetal skull appear.
- Evaluation of the four-chambered heart and great vessels is possible only after 10 weeks of pregnancy.
- The bladder is visualized in 50% of healthy fetuses at 10 weeks, in 80% at 11 weeks, and in all fetuses at 12 weeks.
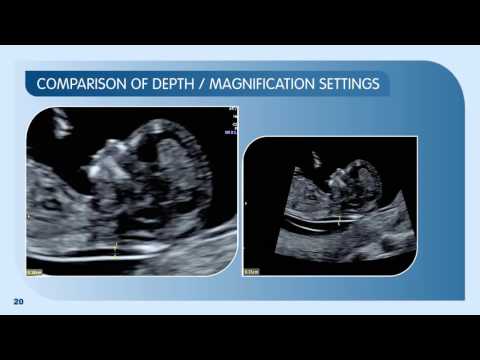
Imaging and measurement
To measure FN, the ultrasonic machine must have a high resolution with video loop function and calibrators that can measure the size to tenths of a millimeter. SP can be measured with an abdominal probe in 95% of cases, in cases where this cannot be done, a vaginal probe should be used.
Only the fetal head and upper thorax should be included in the image when measuring the NB. The magnification should be maximum, so that a small shift of the markers gives a change in measurement of no more than 0.1 mm. When zooming in on an image, either before or after fixing the image, it is important to reduce the gain. This avoids a measurement error when the marker falls into a blurred area and thus the size of the NR will be underestimated.
A good sagittal section should be obtained, of the same quality as the CTE measurement. The measurement should be made in the neutral position of the fetal head: extension of the head can increase the value of TBP by 0.6 mm, flexion of the head can decrease the value by 0.4 mm.
The measurement should be made in the neutral position of the fetal head: extension of the head can increase the value of TBP by 0.6 mm, flexion of the head can decrease the value by 0.4 mm.
It is important not to confuse the skin of the fetus with the amnion, because at this stage of pregnancy, both formations look like thin membranes. If in doubt, you should wait for the moment when the fetus makes a movement and moves away from the amnion. An alternative way is to ask the pregnant woman to cough or lightly tap on the pregnant woman's abdominal wall.
The largest perpendicular distance between the inner contours of the cervical translucency is measured (see figure below). Measurements are taken three times, the largest value of the size is used for the calculation. In 5-10% of cases, the umbilical cord is found wrapped around the fetal neck, which can greatly complicate measurement. In such cases, 2 measurements are used: above and below the cord entanglement, the average of these two measurements is used to calculate the risks.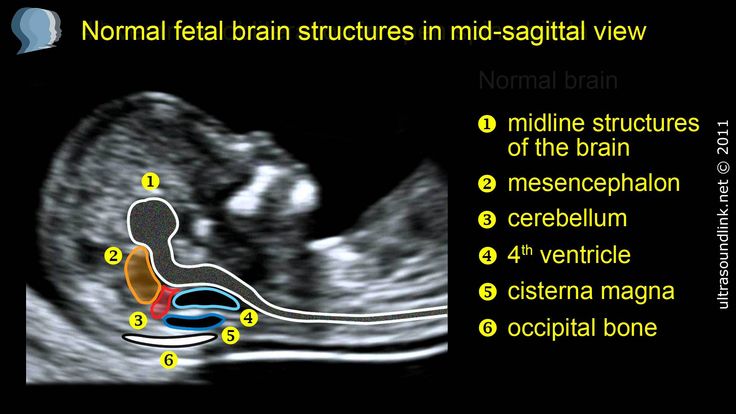
End-trimester ultrasound scanning standards are being developed by the England-based Fetal Medicine Foundation (FMF). In the CIR group of companies, ultrasound is performed according to the FMF protocol.
Additional ultrasound signs of the risk of Down's syndrome
Recently, in addition to the measurement of SP for the diagnosis of Down's syndrome at the end of the first trimester of pregnancy, the following ultrasound signs are used:
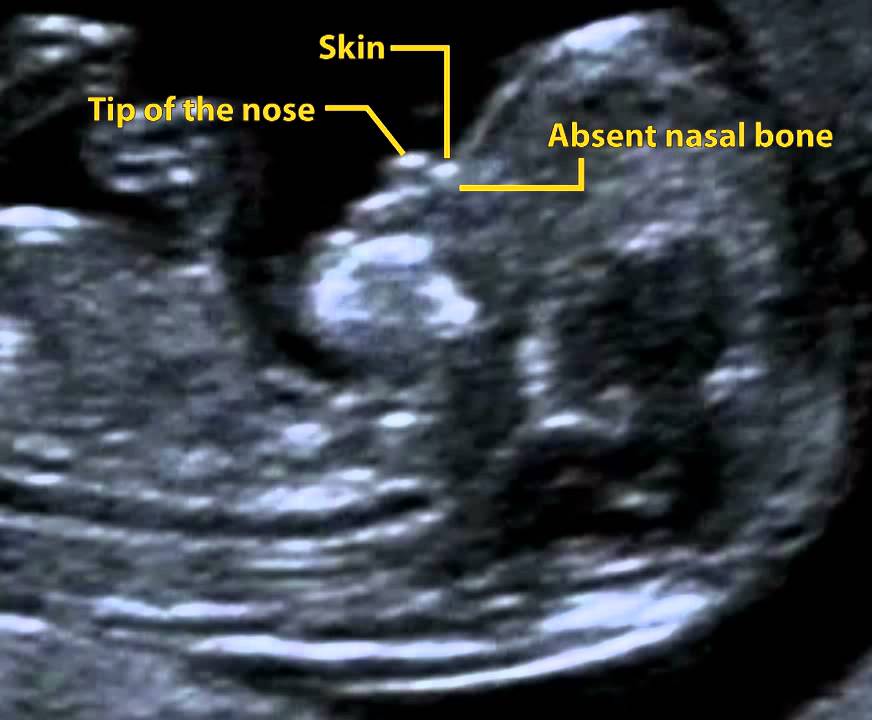
- Determination of the nasal bone . At the end of the first trimester, the nasal bone is not detected by ultrasound in 60-70% of fetuses with Down syndrome and only in 2% of healthy fetuses.
- Evaluation of blood flow in the duct of Arantia (venous) . Abnormalities in the waveform of blood flow in the duct of Arantia are found in 80% of fetuses with Down syndrome and only in 5% of chromosomally normal fetuses
- Maxillary bone reduction
- Bladder enlargement (“megacystitis”)
- Moderate fetal tachycardia
Doppler flow pattern in the duct of Arantia.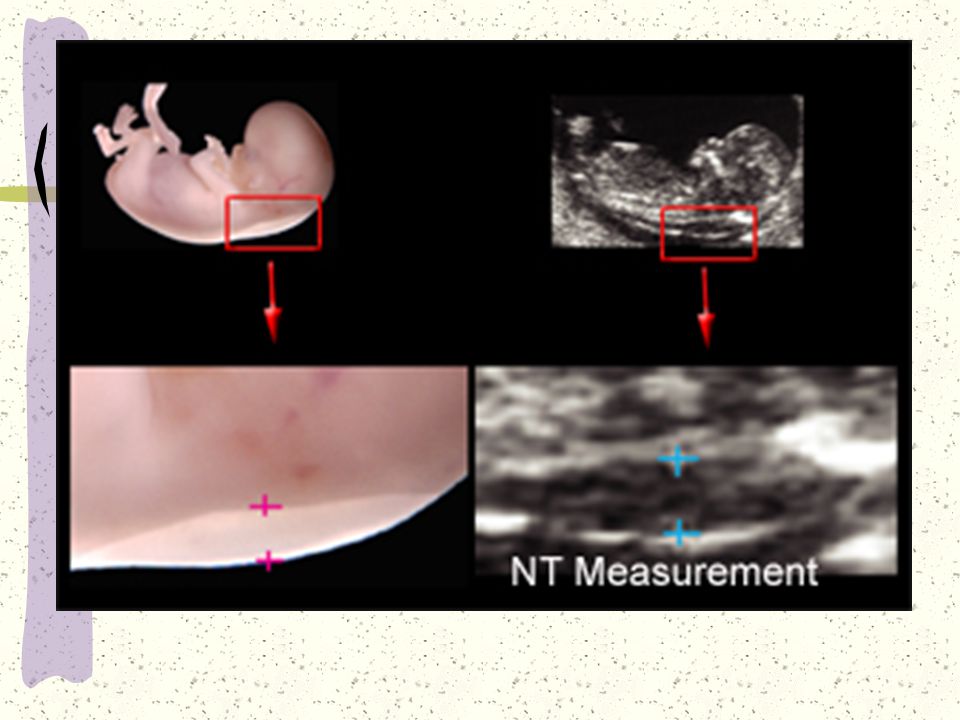 Top: normal; bottom: trisomy 21.
Top: normal; bottom: trisomy 21.
Not only Down syndrome!
During ultrasound at the end of the first trimester, the assessment of the fetal contour also reveals the following fetal anomalies:
- Exencephaly - anencephaly
- Cystic hygroma (swelling at the level of the neck and back of the fetus), more than half of the cases due to chromosomal abnormalities
- Omphalocele and gastroschisis. The diagnosis of omphalocele can only be made after 12 weeks of pregnancy, since before this period the physiological umbilical hernia, quite often detected, has no clinical significance
- The only umbilical artery (in a large percentage of cases it is associated with chromosomal abnormalities in the fetus)
How are risks calculated?
Special software is used to calculate risks. Simply determining the level of indicators in the blood is not enough to decide whether the risk of developmental anomalies is increased or not.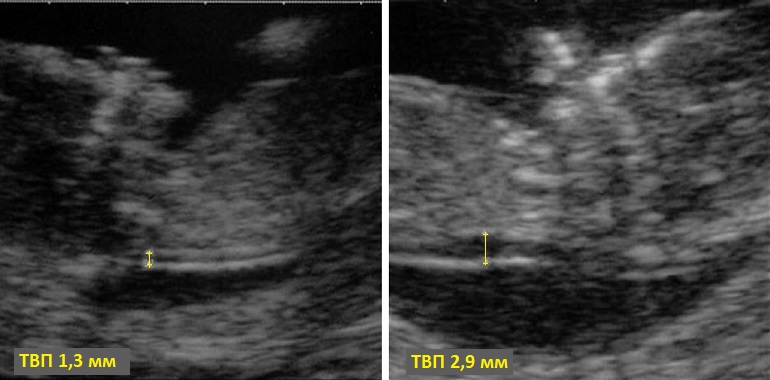 The software must be certified for use with prenatal screening. At the first stage of computer calculation, the figures of indicators obtained during laboratory diagnostics are converted into the so-called MoM (multiple of median, a multiple of the median), characterizing the degree of deviation of one or another indicator from the median. At the next stage of the calculation, the MoM is adjusted for various factors (a woman's body weight, race, the presence of certain diseases, smoking, multiple pregnancy, etc.). The result is the so-called adjusted MoM. In the third step of the calculation, the adjusted MoMs are used to calculate the risks. The software is specially configured for the methods used in the laboratory for determining indicators and reagents. It is unacceptable to calculate risks using analyzes made in another laboratory. The most accurate calculation of the risks of fetal anomalies is when using data from an ultrasound scan performed at 10-13 weeks of gestation.
The software must be certified for use with prenatal screening. At the first stage of computer calculation, the figures of indicators obtained during laboratory diagnostics are converted into the so-called MoM (multiple of median, a multiple of the median), characterizing the degree of deviation of one or another indicator from the median. At the next stage of the calculation, the MoM is adjusted for various factors (a woman's body weight, race, the presence of certain diseases, smoking, multiple pregnancy, etc.). The result is the so-called adjusted MoM. In the third step of the calculation, the adjusted MoMs are used to calculate the risks. The software is specially configured for the methods used in the laboratory for determining indicators and reagents. It is unacceptable to calculate risks using analyzes made in another laboratory. The most accurate calculation of the risks of fetal anomalies is when using data from an ultrasound scan performed at 10-13 weeks of gestation.
What is MoM?
MoM is the English abbreviation for the term “multiple of median”, which means “multiple of the median”.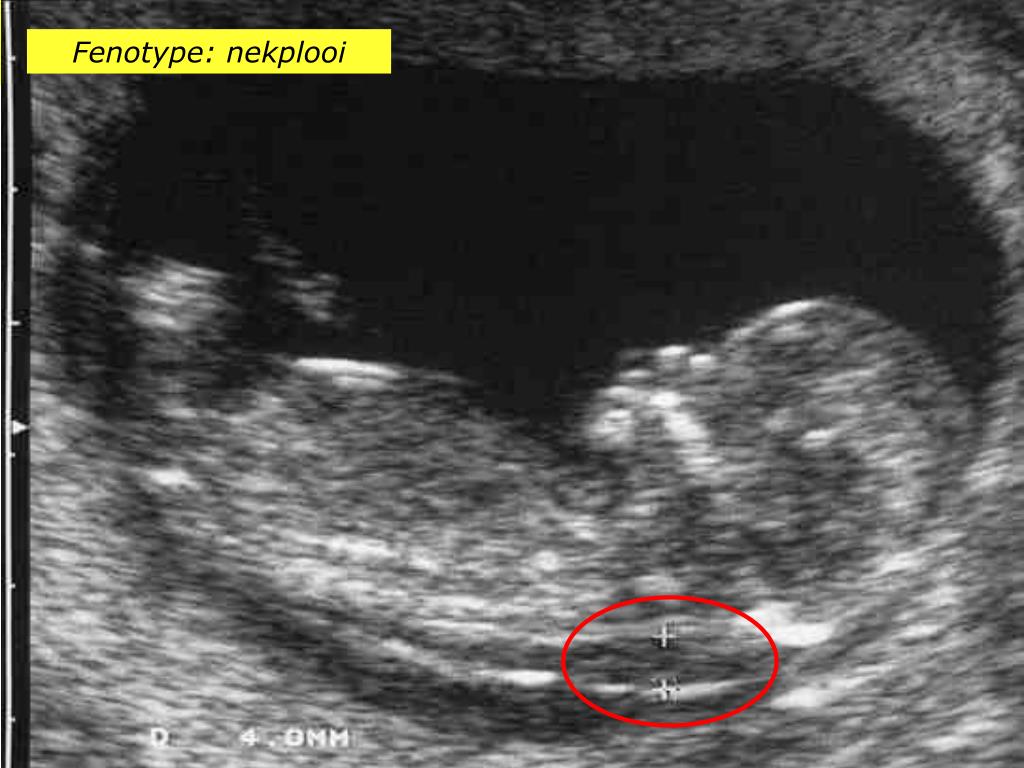 This is a coefficient showing the degree of deviation of the value of one or another indicator of prenatal screening from the average value for the gestational age (median). MoM is calculated using the following formula:
This is a coefficient showing the degree of deviation of the value of one or another indicator of prenatal screening from the average value for the gestational age (median). MoM is calculated using the following formula:
MoM = [Patient Serum Value] / [Median Value for Pregnancy]
. If the value of MoM in a patient is close to one, then the value of the indicator is close to the average in the population; if it is above one, it is above the average in the population; if it is below one, it is below the average in the population. With congenital malformations of the fetus, there may be statistically significant deviations of MoM markers. However, in its pure form, MoMs are almost never used in calculating the risk of fetal anomalies. The fact is that in the presence of a number of factors, the average values of MoM deviate from the average in the population. Such factors include the patient's body weight, smoking, race, pregnancy as a result of IVF, etc. Therefore, after obtaining the MoM values, the risk calculation program makes an adjustment for all these factors, resulting in the so-called “adjusted MoM value”, which used in risk calculation formulas. Therefore, in the conclusion forms based on the results of the analysis, next to the absolute values of the indicators, the adjusted MoM values for each indicator are indicated.
Therefore, after obtaining the MoM values, the risk calculation program makes an adjustment for all these factors, resulting in the so-called “adjusted MoM value”, which used in risk calculation formulas. Therefore, in the conclusion forms based on the results of the analysis, next to the absolute values of the indicators, the adjusted MoM values for each indicator are indicated.
Typical MoM profiles in pathology of pregnancy
In various fetal anomalies, MoM values are combined deviated from the norm. Such combinations of MoM deviations are called MoM profiles for a particular pathology. The tables below show typical MoM profiles at different gestational ages.
| Anomaly | PAPP-A | Free β-hCG |
|---|---|---|
| Tr.21 (Down syndrome) | 0.41 | 1.98 |
| tr. 18 (Edwards Syndrome) | 0.16 | 0.34 |
| Typloidy type i/II | 0.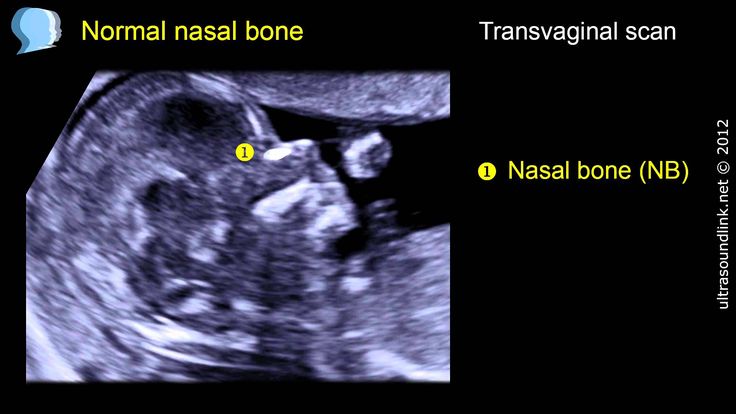 06 06 | |
| 0.49 | 1.11 | |
| Cleinfelter syndrome | 0.88 | 1.07 |
MOMENTER
| 0292 | AFP | Gen. HCG | St. Estriol | Ingin A | ||
|---|---|---|---|---|---|---|
| TR.21 (Down Syndrome) | 0.75 9030 | 2,79 9029 9029 9029 9029 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 902 90AR (Edwards Syndrome) | 0.65 | 0.36 9030 | 0.43 | 0.88 |
| Type I/II | 6.97 | 13 | 0.69 | 0.69 0.69 0.69 9030 0.69 9030 90309030 90AREL0301 | ||
| Shereshevsky-Terner Syndrome | 0.99 | 1.98 | 0.68 | |||
| Syndrome Syndrome Syndrome Syndrome Syndrome Syndrome Syndrome Syndrome Syndrome Clinfelter | 90-9 902 902 902 902 902 902 902 902 902 902 902 902 902 902 90AM 902 906 902 90AM 902 906 902 90EAL .
Typical MoM profiles - Second trimester
Indications for 1st and 2nd trimester prenatal screening for risk of fetal abnormalities
Prenatal screening is now recommended for all pregnant women. The order of the Ministry of Health of the Russian Federation of 2000 obliges antenatal clinics to conduct biochemical prenatal screening for all pregnant patients in the second trimester of pregnancy for two indicators (AFP and hCG).
Order No. 457 dated December 28, 2000 “On improving prenatal diagnostics in the prevention of hereditary and congenital diseases in children”:
The importance of monitoring congenital diseases on a regular basis in Moscow is also discussed in the Moscow Government Decree on the establishment of the city program “Children's Health” for 2003-2005.
Decree of the Government of Moscow dated July 23, 2002 No. 572-PP
572-PP
On the other hand, prenatal screening should be purely voluntary. In most Western countries, it is the physician's responsibility to inform the patient about the possibility of such studies and about the goals, possibilities and limitations of prenatal screening. The patient herself decides whether to do her tests or not. The same point of view is shared by the CIR group of companies. The main problem is that there is no cure for the detected anomalies. If the presence of anomalies is confirmed, the couple is faced with a choice: terminate the pregnancy or keep it. It's not an easy choice.
What is Edwards syndrome?
This is a condition caused by the presence of an extra 18th chromosome in the karyotype (trisomy 18). The syndrome is characterized by gross physical anomalies and mental retardation. This is a lethal condition: 50% of sick children die in the first 2 months of life, 95% - during the first year of life. Girls are affected 3-4 times more often than boys. The frequency in the population ranges from 1 case per 6,000 births to 1 case per 10,000 births (about 10 times less than Down syndrome).
This is a lethal condition: 50% of sick children die in the first 2 months of life, 95% - during the first year of life. Girls are affected 3-4 times more often than boys. The frequency in the population ranges from 1 case per 6,000 births to 1 case per 10,000 births (about 10 times less than Down syndrome).
What is the free β-subunit of hCG?
A number of pituitary and placental hormones (thyroid stimulating hormone (TSH), follicle stimulating hormone (FSH), luteinizing hormone (LH) and human chorionic hormone (hCG)) have a similar structure and consist of α and β subunits. The alpha subunits of these hormones are very similar and the main differences between the hormones are in the structure of the β subunits. LH and hCG are very similar not only in the structure of the α-subunits, but also in the structure of the β-subunits. That is why they are hormones with the same action. During pregnancy, LH production by the pituitary gland drops to almost zero, and hCG concentrations are very high. The placenta produces very large amounts of hCG, and although this hormone mainly enters the blood in an assembled form (a dimeric molecule consisting of both subunits), a small amount of free (not bound to the α-subunit) β-hCG subunit also enters the bloodstream. Its concentration in the blood is many times less than the concentration of total hCG, but this indicator can more reliably indicate the risk of problems in the fetus in the early stages of pregnancy. The determination of the free β-subunit of hCG in the blood is also important for the diagnosis of trophoblastic disease (molar mole and chorionepithelioma), some testicular tumors in men, and monitoring the success of in vitro fertilization procedures.
The placenta produces very large amounts of hCG, and although this hormone mainly enters the blood in an assembled form (a dimeric molecule consisting of both subunits), a small amount of free (not bound to the α-subunit) β-hCG subunit also enters the bloodstream. Its concentration in the blood is many times less than the concentration of total hCG, but this indicator can more reliably indicate the risk of problems in the fetus in the early stages of pregnancy. The determination of the free β-subunit of hCG in the blood is also important for the diagnosis of trophoblastic disease (molar mole and chorionepithelioma), some testicular tumors in men, and monitoring the success of in vitro fertilization procedures.
Which indicator: total hCG or free β-hCG subunit - is it preferable to use in the second trimester triple test?
The use of free hCG β-subunit determination compared to total hCG determination gives a more accurate estimate of the risk of Down syndrome, however, maternal total hCG levels have been used in classic population risk estimates for Edwards syndrome.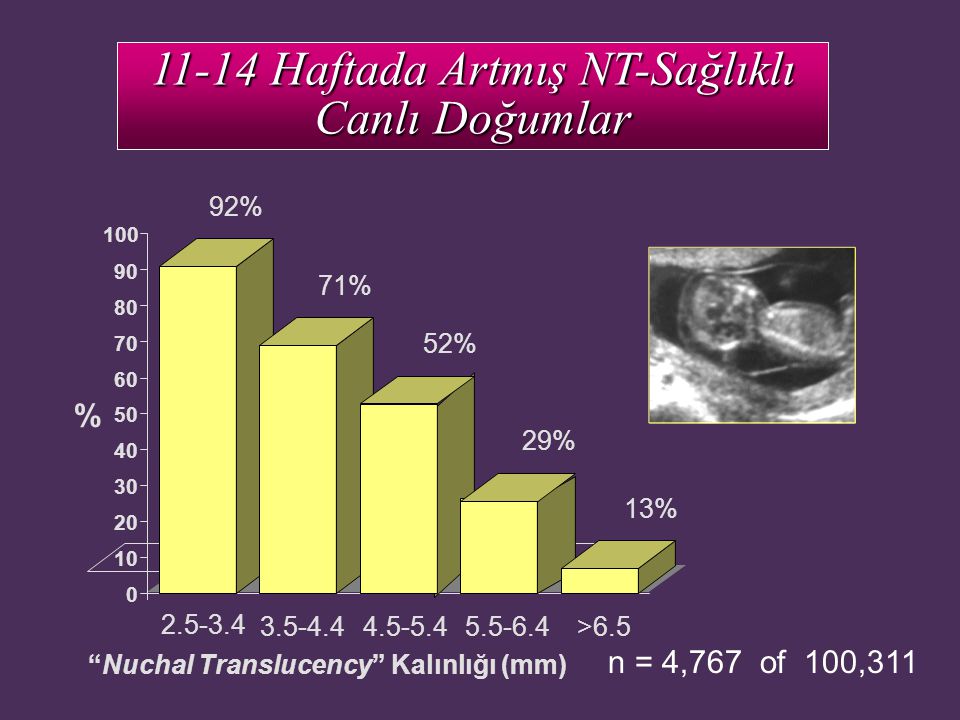 For the β-subunit of hCG, no such calculations have been made. Therefore, a choice must be made between a more accurate calculation of the risk of Down syndrome (in the case of the β-subunit) and the possibility of calculating the risk of Edwards syndrome (in the case of total hCG). Recall that in the first trimester, only free β-subunit hCG is used to calculate the risk of Edwards syndrome, but not total hCG. Edwards syndrome is characterized by low numbers of all 3 indicators of the triple test, therefore, in such cases, both variants of the triple test (with total hCG and with free β-subunit) can be done.
For the β-subunit of hCG, no such calculations have been made. Therefore, a choice must be made between a more accurate calculation of the risk of Down syndrome (in the case of the β-subunit) and the possibility of calculating the risk of Edwards syndrome (in the case of total hCG). Recall that in the first trimester, only free β-subunit hCG is used to calculate the risk of Edwards syndrome, but not total hCG. Edwards syndrome is characterized by low numbers of all 3 indicators of the triple test, therefore, in such cases, both variants of the triple test (with total hCG and with free β-subunit) can be done.
What is PAPP-A?
Pregnancy-associated plasma protein-A (PAPP-A) was first described in 1974 as a high molecular weight protein fraction in the serum of women in late pregnancy. It turned out to be a large zinc-containing metalglycoprotein with a molecular weight of about 800 kDa. During pregnancy, PAPP-A is produced by syncytiotrophoblast (the tissue that makes up the outer layer of the placenta) and extravillous cytotrophoblast (islets of fetal cells in the lining of the uterus) and enters the mother's bloodstream
The biological significance of this protein is not fully understood. It has been shown to bind heparin and is an inhibitor of granulocyte elastase (an enzyme induced by inflammation), so it is suggested that PAPP-A modulates the maternal immune response and is one of the factors that ensures the development and survival of the placenta. In addition, it was found that it is a protease that cleaves protein 4 that binds insulin-like growth factor. There are serious reasons to believe that PAPP-A is one of the factors of paracrine regulation not only in the placenta, but also in some other tissues, in particular, in atherosclerotic plaques. It is proposed to use this marker as one of the risk factors for coronary heart disease.
It has been shown to bind heparin and is an inhibitor of granulocyte elastase (an enzyme induced by inflammation), so it is suggested that PAPP-A modulates the maternal immune response and is one of the factors that ensures the development and survival of the placenta. In addition, it was found that it is a protease that cleaves protein 4 that binds insulin-like growth factor. There are serious reasons to believe that PAPP-A is one of the factors of paracrine regulation not only in the placenta, but also in some other tissues, in particular, in atherosclerotic plaques. It is proposed to use this marker as one of the risk factors for coronary heart disease.
Maternal blood concentrations of PAPP-A increase steadily with increasing gestational age. The greatest increase in this indicator is observed at the end of pregnancy.
Over the past 15 years, PAPP-A has been studied as one of three risk markers for trisomy 21 (Down syndrome) (together with free hCG β-subunit and nuchal thickness). It turned out that the level of this marker at the end of the first trimester of pregnancy (8-14 weeks) is significantly reduced if the fetus has trisomy 21 or trisomy 18 (Edwards syndrome). The uniqueness of this indicator is that its significance as a marker of Down syndrome disappears after 14 weeks of pregnancy. In the second trimester, its levels in maternal blood in the presence of trisomy 21 in the fetus do not differ from those in pregnant women with a healthy fetus. If we consider PAPP-A as an isolated marker of the risk of Down syndrome in the first trimester of pregnancy, the most significant would be its determination in terms of 8–9weeks. However, the free β-subunit of hCG is a stable marker of the risk of Down syndrome at 10–18 weeks, i.e. later than PAPP-A. Therefore, the optimal time for donating blood for a double test in the first trimester of pregnancy is 10-12 weeks.
It turned out that the level of this marker at the end of the first trimester of pregnancy (8-14 weeks) is significantly reduced if the fetus has trisomy 21 or trisomy 18 (Edwards syndrome). The uniqueness of this indicator is that its significance as a marker of Down syndrome disappears after 14 weeks of pregnancy. In the second trimester, its levels in maternal blood in the presence of trisomy 21 in the fetus do not differ from those in pregnant women with a healthy fetus. If we consider PAPP-A as an isolated marker of the risk of Down syndrome in the first trimester of pregnancy, the most significant would be its determination in terms of 8–9weeks. However, the free β-subunit of hCG is a stable marker of the risk of Down syndrome at 10–18 weeks, i.e. later than PAPP-A. Therefore, the optimal time for donating blood for a double test in the first trimester of pregnancy is 10-12 weeks.
The combination of PAPP-A measurement with free β-hCG blood concentration and TTP by ultrasound at the end of the first trimester of pregnancy can identify up to 90% of women at risk of developing Down syndrome in the older age group (after 35 years). The probability of false positive results is about 5%.
The probability of false positive results is about 5%.
In addition to prenatal screening for the risk of Down syndrome and Edwards syndrome, in obstetrics, PAPP-A determination is also used for the following types of pathologies:
- Threatened miscarriage and early pregnancy arrest
- Cornelia de Lange syndrome.
Diagnosis of the risk of fetal arrest in early pregnancy was historically the first clinical application of serum PAPP-A determination proposed in the early 1980s. Women with low levels of PAPP-A in early pregnancy have been shown to be at risk for subsequent pregnancy loss and severe late toxicosis. Therefore, it is recommended that this indicator be determined within 7–8 weeks for women with a history of severe pregnancy complications.
Cornelia de Lange syndrome is a rare form of congenital malformation of the fetus, found in 1 in 40,000 births. The syndrome is characterized by mental and physical retardation, heart and limb defects, and characteristic facial features.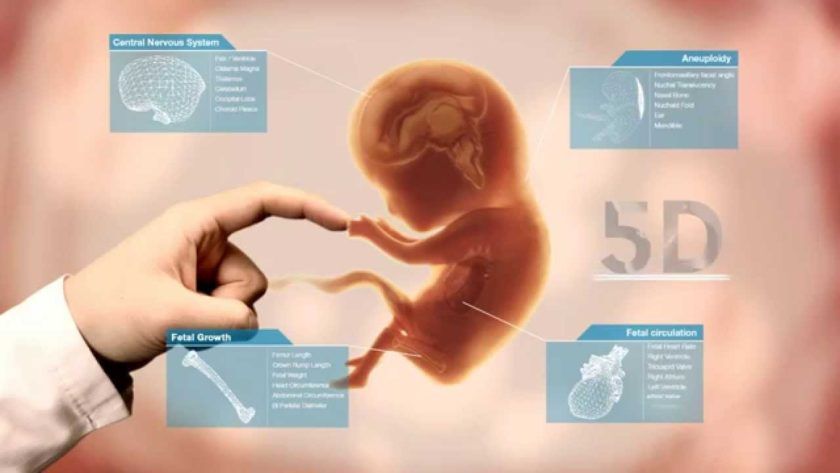 It has been shown that in this condition, the levels of PAPP-A in the blood at 20-35 weeks are significantly lower than normal. Study of Aitken's group at 1999 showed that this marker can be used for screening for Cornelia de Lange syndrome in the second trimester of pregnancy, since the levels of the indicator in such pregnant women were on average 5 times lower than normal.
It has been shown that in this condition, the levels of PAPP-A in the blood at 20-35 weeks are significantly lower than normal. Study of Aitken's group at 1999 showed that this marker can be used for screening for Cornelia de Lange syndrome in the second trimester of pregnancy, since the levels of the indicator in such pregnant women were on average 5 times lower than normal.
The reagents used to determine PAPP-A and free β-hCG subunit are an order of magnitude more expensive than those used for most hormonal parameters, making this test more expensive than most reproductive hormones.
What is α-fetoprotein?
It is a fetal glycoprotein produced first in the yolk sac and then in the liver and gastrointestinal tract of the fetus. It is a transport protein in the blood of the fetus that binds a number of different factors (bilirubin, fatty acids, steroid hormones). It is a dual fetus growth regulator. In an adult, AFP does not perform any known functions, although it can increase in the blood in liver diseases (cirrhosis, hepatitis) and in some tumors (hepatocellular carcinoma and germinal carcinoma). In the mother's blood, the level of AFP gradually increases with increasing gestational age and reaches a maximum by 30 weeks. The level of AFP in the mother's blood increases with neural tube defects in the fetus and with multiple pregnancies, and decreases with Down syndrome and Edwards syndrome.
In the mother's blood, the level of AFP gradually increases with increasing gestational age and reaches a maximum by 30 weeks. The level of AFP in the mother's blood increases with neural tube defects in the fetus and with multiple pregnancies, and decreases with Down syndrome and Edwards syndrome.
What is free estriol?
Estriol is synthesized in the placenta from 16α-hydroxy-dehydroepiantrosterone sulfate supplied by the fetus. The main source of estriol precursors is the fetal adrenal glands. Estriol is the main estrogenic hormone of pregnancy and ensures the growth of the uterus and the preparation of the mammary glands for lactation.
90% of estriol after 20 weeks of gestation is derived from fetal DEA-C. A large output of DEA-C from the adrenal gland of the fetus is associated with low activity of 3β-hydroxysteroid dehydrogenase in the fetus. A protective mechanism that protects the fetus from excess androgenic activity is the rapid conjugation of steroids with sulfate. The fetus produces more than 200 mg of DEA-C per day, 10 times more than the mother. In the maternal liver, estriol is rapidly conjugated with acids, mainly hyaluronic acid, and thus inactivated. The most accurate method for determining the activity of the fetal adrenal glands is to determine the level of free (unconjugated) estriol.
The fetus produces more than 200 mg of DEA-C per day, 10 times more than the mother. In the maternal liver, estriol is rapidly conjugated with acids, mainly hyaluronic acid, and thus inactivated. The most accurate method for determining the activity of the fetal adrenal glands is to determine the level of free (unconjugated) estriol.
Free estriol levels gradually increase as pregnancy progresses and in the third trimester of pregnancy can be used to diagnose fetal well-being. With a deterioration in the condition of the fetus in the third trimester of pregnancy, a sharp drop in the level of free estriol can be observed. Free estriol levels are often low in Down syndrome and Edwards syndrome. Taking dexamethasone, prednisolone or metipred during pregnancy suppresses the function of the fetal adrenal glands, so the level of free estriol in such patients is often reduced (decrease in the supply of estriol from the fetus). When taking antibiotics, the rate of estriol conjugation in the mother's liver increases and the reabsorption of conjugates from the intestine decreases, so the level of estriol also decreases, but by accelerating its inactivation in the mother's body.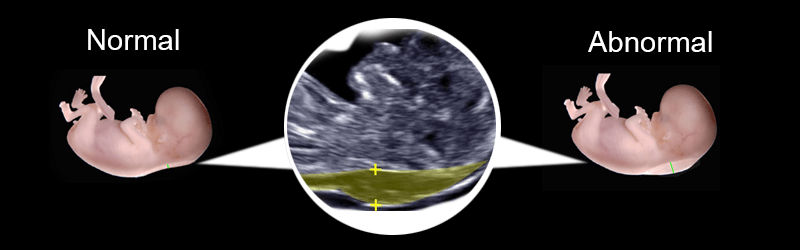 For an accurate interpretation of the triple test data, it is very important that the patient provides a complete list of drugs taken or taken during pregnancy with doses and timing of use.
For an accurate interpretation of the triple test data, it is very important that the patient provides a complete list of drugs taken or taken during pregnancy with doses and timing of use.
Prenatal screening algorithm for I and II trimester of pregnancy.
1. We calculate the duration of pregnancy, preferably after consultation with a doctor or with the help of a consultant.
First trimester screening has its own characteristics. It is carried out in terms of 10 - 13 weeks of pregnancy and is quite strictly limited in terms of time. If you donate blood too early or too late, if you make a mistake in calculating the gestational age at the time of donating blood, the accuracy of the calculation will decrease dramatically. Pregnancy terms in obstetrics are usually calculated on the first day of the last menstruation, although conception occurs on the day of ovulation, that is, with a 28-day cycle - 2 weeks after the first day of menstruation. Therefore, the terms of 10 - 13 weeks on the day of menstruation correspond to 8 - 11 weeks of conception.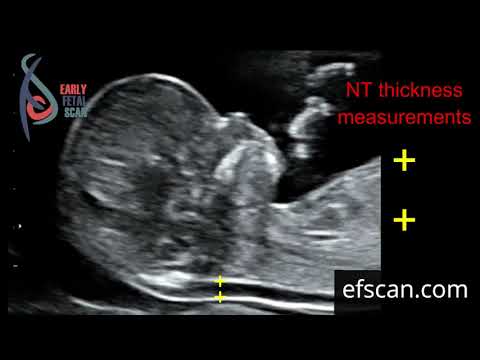
To calculate the gestational age, we recommend using the obstetric calendar available on our website. Difficulties in calculating the timing of pregnancy can be with an irregular menstrual cycle, with pregnancy that occurs shortly after childbirth, with a cycle that deviates more than a week from 28 days. Therefore, it is best to trust professionals, and to calculate the duration of pregnancy, conduct an ultrasound scan and donate blood, consult a doctor.
2. We do ultrasound.
The next step should be an ultrasound scan at 10-13 weeks of gestation. The data from this study will be used by the risk calculation program in both the first and second trimesters. It is necessary to start the examination with ultrasound, since during the study problems with the development of pregnancy (for example, a stop or lag in development), a multiple pregnancy, the timing of conception will be accurately calculated. The doctor conducting the ultrasound will help the patient calculate the timing of blood donation for biochemical screening.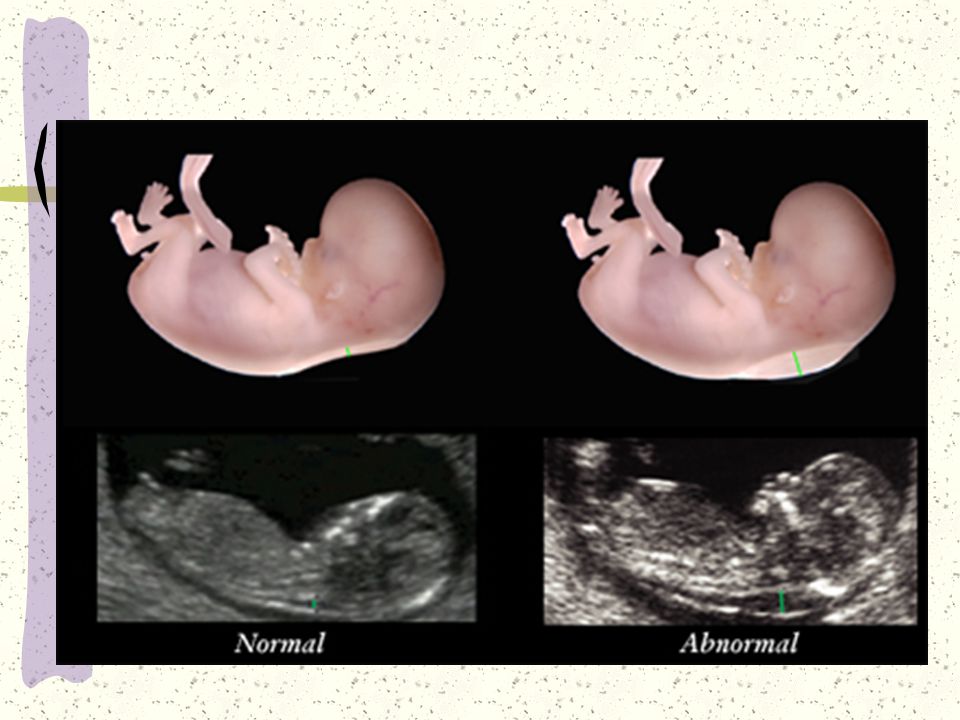 If the ultrasound is done too early in terms of pregnancy, then the doctor may recommend repeating the study after some time.
If the ultrasound is done too early in terms of pregnancy, then the doctor may recommend repeating the study after some time.
The following data from the ultrasound report will be used to calculate risks: ultrasound date, coccygeal-parietal size (CTE) and collar space thickness (NTT) (English abbreviations CRL and NT, respectively), as well as visualization of the nasal bones.
3. Donate blood.
Having the ultrasound results and knowing the exact gestational age, you can come to donate blood. Blood sampling for analysis for prenatal screening in the CIR group of companies is carried out daily, including weekends. On weekdays, blood sampling is carried out from 7:45 to 21:00, on weekends and holidays: from 8:45 to 17:00. Blood sampling is carried out 3-4 hours after the last meal.
At 14-20 weeks of gestation from the last menstrual period (recommended 16-18 weeks), the following biochemical parameters are determined:
- Total hCG or free β-subunit of hCG
- α-fetoprotein (AFP)
- Free (unconjugated) estriol
- Inhibin A
4. We get the result.
We get the result.
Now you need to get the results of the analysis. The turnaround time for the results of prenatal screening analysis in the CIR group of companies is one business day (except for the fourth test). This means that tests taken from Monday to Friday will be ready on the same day, and those taken from Saturday to Sunday on Monday.
The results of the study are issued to the patient in Russian.
Table. Explanation of terms and abbreviations
| Date of report | Date of computerized results | |
| Gestational age | Weeks + days | |
| Date of ultrasound | Date of ultrasound | Usually does not coincide with the date of blood donation. |
| Fruits | Number of fruits. 1 - singleton pregnancy; 2 - twins; 3 - triplets | |
| ECO | Pregnancy occurred as a result of IVF | |
| KTR | Copchic-Dark size, determined during ultrasound | |
| multiple medians (multiple of Median), degree gestational age | ||
Corr. MoM MoM | Adjusted MoM. MoM value after adjustment for body weight, age, race, number of fetuses, diabetes, smoking, IVF infertility treatment. | |
| NT | Nuchal translucency. Synonym: neck fold. In various versions of reports, either absolute values in mm or the degree of deviation from the median (MoM) can be given | |
| Age risk | Average risk for this age group No factors other than age are taken into account. | |
| Tr. 21 | Trisomy 21, Down syndrome | |
| Tr. 18 | Trisomy 18, Edwards syndrome | |
| Biochemical risk | Risk of fetal abnormalities after computer processing of blood test data without ultrasound data | |
| Combined risk of processing with consideration of fetal blood data with ultrasound data | . The most accurate indicator of the degree of risk. | |
| fb-HCG | Free hCG β-subunit | ng/ml |
| IU/ml | IU/ml |
Additional information.
Information for patients: please note that if you plan to undergo prenatal screening in the CIR group of companies, then the ultrasound data made in other institutions will be taken into account only if there is a special agreement between the CIR group of companies and these institutions.
Information for physicians
Dear colleagues! In accordance with the Order of the Ministry of Health No. 457 and Decree of the Government of Moscow No. 572, the CIR group of companies provides services to other medical institutions for prenatal screening for the risk of chromosomal abnormalities. You can invite our staff to come to you with a lecture on this program. To refer a patient for screening, the attending physician must complete a special referral. The patient can come to donate blood on her own, but it is also possible to take blood in other institutions with subsequent delivery to our laboratory, including by our courier. If you want to receive the results of double, triple and quadruple tests of the first and second trimesters of pregnancy, combined with ultrasound data, the patient must come to us for an ultrasound scan, or we must sign a special agreement with your institution and include your ultrasound specialists in the program, but only after departure of our expert in functional diagnostics to your institution and familiarization with the quality of the equipment and the qualifications of specialists.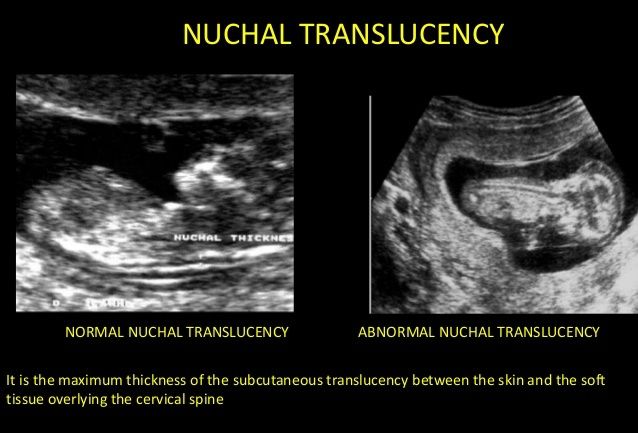
Tags: prenatal diagnostics
Cervical-collar zone massage: technique of performing
Contents of the article
- Danger of improper use of the cervical-collar zone massage technique
- Movements characteristic of the technique of performing massage in the cervical-collar zone
- Method of performing cervical zone massage 906
- Peculiarities of performing a therapeutic massage of the cervical-collar zone
- How to properly massage the collar zone for children?
- How is a neck massage for babies done?
- How to massage the cervico-collar area using the intensive technique?
- Cervical area massage technique to get rid of cellulite and unwanted fat deposits
- Neck area massage techniques using devices ShVZ is one of the demanded methods of the XXI century.
Use the massage technique in case of injuries in the cervical-collar area, intervertebral hernias after a doctor's prescription.
 Before this, it is important to first familiarize yourself with the diagnosis, study the medical history, analyze the indications and contraindications.
Before this, it is important to first familiarize yourself with the diagnosis, study the medical history, analyze the indications and contraindications. Danger of improper use of massage technique of the cervical-collar area
- increased frequency of headaches, migraines
- exacerbation of chronic diseases
- deterioration in general well-being
- hypertensive or hypotensive crisis
It is important to take into account all contraindications of the client before the session!
Movements typical for the technique of performing massage in the neck and collar area
Stroking.
The reception must be performed with the inner surfaces of both hands, using very light and smooth massage movements with the palms along the central line of the neck. Stroking the cervical-collar zone is useful to do along the lymph nodes. With the help of strokes, the effect of relaxation is achieved, getting rid of dead skin cells, relaxing the body and preparing the client for the massage procedure itself.

Types of stroking used to massage the neck and back:
- Planar surface stroking. Slightly perceptible for the client movement in the collar section with a relaxed hand. Before performing planar surface stroking in the massage of the cervical-collar zone, it is useful for the massage therapist to shake and relax his hands.
- Flat deep stroke. Similar to planar surface stroking, but done with more effort.
- Continuous stroking. The massage therapist's brush slowly and firmly wraps around the treated area and slides towards the center. The movement of the hand(s) should be slow.
- Intermittent stroking. Similar to embracing continuous stroking. Grasp and squeezing is done with short intermittent, rhythmic massage movements.
Ironing
Palm bent at a right angle. The movement is done by the back surface of the phalanges of the fingers.
Rake-like movements
The massage therapist makes movements with spread rake-like fingers.
Drills
During the reception, the palm should be on the selected part of the spine so that it is between the thumb and forefinger. Emphasis is placed with the thumb on the back, and the rest are made in circular motions along the spine.
Rubbing
Reception is based on the displacement of the skin under the masseur's hands, they are similar to rubbing, but have a more intense character. This technique allows you to warm up tissues, muscles, joints, improve blood circulation, blood flow, accelerate the removal of toxins from the body, and have a preventive effect against the development of osteochondrosis and other diseases. The use of rubbing will increase the tone, contractile function of the muscles of the massaged section. It must be remembered that massage oils and gels reduce the force of rubbing, its warming effect.
 The masseur should apply the same pressure during the application of the movement to each point of the cervical or collar zone, but be careful in places with delicate skin so as not to provoke pain. Rubbing is an intense and strong movement, but it should not cause pain in the massaged area. If you want to increase the effect of rubbing, increase the angle between your palm and your back or neck. Rubbing is useful to alternate with stroking.
The masseur should apply the same pressure during the application of the movement to each point of the cervical or collar zone, but be careful in places with delicate skin so as not to provoke pain. Rubbing is an intense and strong movement, but it should not cause pain in the massaged area. If you want to increase the effect of rubbing, increase the angle between your palm and your back or neck. Rubbing is useful to alternate with stroking. Rubbing is divided into superficial and deep, continuous and intermittent.
Types of rubbing that are used to massage the neck and back:
- Rectilinear - rubbing with the pads of four fingers of the massage therapist along the spine and neck.
- Circular - displacement of the skin with circular massage movements using fingers or the base of the palm.
- Spiral Spiral rubbing with one or both hands. The spiral rubbing technique is useful for massaging the trapezius, paravertebral, and supraspinatus muscles.
An effective method is combined rubbing in the cervical-collar area. The technique involves combining longitudinal rubbing with the edge of the palm (one hand), fingers (the other hand).
Kneading
Successive gripping, lifting, squeezing, kneading, rolling muscles. There are longitudinal kneading (along the muscle), transverse kneading (across the muscle). The movement can be made with pads, phalanges of fingers, palms. Kneading should be done at a slow pace. Massage gel and oil weaken the effect of the reception, as well as when performing rubbing. With each session, it is worth increasing the intensity of kneading. This technique occupies the largest part of the massage of the cervical-collar zone.
Types of rubbing used to massage the neck and back:
- Longitudinal - carried out with straightened fingers along the muscle fibers.
- Transverse - performed across the muscle fibers.
Auxiliary techniques. Felting, pressing, rolling, shifting.
Vibration
This massage technique can be applied with the masseuse's fingertips, hand, base of palms, fist. Reception of vibration consists in the implementation of continuous or intermittent oscillatory movements. Intensive performance of movements allows you to achieve benefits in the form of an increase in muscle tone in the neck-collar zone, calm vibration gives the effect of relaxation. To enhance the effect of vibration, it is worth reducing the angle between the fingers, palm and massaged area.
Vibration can be continuous, intermittent, stable, superficial, deep, labile.
Types of vibration used to massage the neck and back:
- Continuous - during the movement, the hand, edge of the palm, tips or phalanges of the fingers do not come off the massaged surface.
- Intermittent - rhythmic strokes on the massaged surface.
 Chopping is performed along the muscle fibers. It is important not to perform chopping with closed fingers, this can lead to pain for the client.
Chopping is performed along the muscle fibers. It is important not to perform chopping with closed fingers, this can lead to pain for the client.
Additional techniques: shaking, shaking, patting.
Percussion techniques
Percussion massage techniques are usually used after vibration.
- The simplest technique used for back and neck massage is tapping with the fingers of both hands.
- Chopping with the edge of the palm (one or two at the same time) in the collar area.
- Popping fists. The cam should consist of 4 fingers, and the little finger should be taken away.
How to massage the neck zone- Before starting the session, always ask the client about the contraindications to the procedure
- Place the client on a chair in front of the massage table with a pillow
- pillows, and chin chest. Hands in front of you.
- Perform 7 strokes between the head and shoulders
- Perform 7 rubs
- Perform push-ups, gradually increasing pressure with the edge of the palm of your hand.

- Perform kneading, 5-7 times.
- Massage the trapezius muscle with the entire surface of the palm, 5-10 times.
- Gentle circular massage of the shoulder joints 5-7 times.
- Perform vibration reception - up to 15 sec.
- Stroke the entire collar area, 5-7 times.
Peculiarities of therapeutic massage of the neck and collar zone
- The procedure must be carried out in a comfortable environment for the client and the master.
- Oil is used for good glide.
- SHVZ for children - up to 15 minutes. For adults - up to 30 minutes.
- For maximum effect and benefit, a course of 15 sessions is recommended.
- The frequency of sessions depends on the problem and purpose: after 1, 2, 3 days.
- The procedure should not cause acute pain or discomfort. It is necessary to monitor the reaction, requests of the client.
- After the procedure, help the client to stand up smoothly, without making sudden movements
How to properly massage the collar zone for children?
The treatment procedure is shown for children starting from infants, as an effective remedy for:
- Weakening of the muscle corset of the back and neck
- Insomnia
- headaches, migraines
- development
How is baby collar massage done?
- sessions are performed on a child who has reached 2 months.
 The procedure is contraindicated for children under this age
The procedure is contraindicated for children under this age - put the child in the prone position
- apply baby cream or massage oil to the child’s skin
- use stroking, gentle kneading techniques
- make slow, smooth movements
- massage the neck area from top to bottom
- massage the collar area in the direction from the spine to the shoulder blades
- the session should not exceed a quarter of an hour
How to massage the cervical-collar zone in intensive technique?
Before the session, make sure that the client does not have subluxations, mobility of the cervical vertebrae, problems with the spine, pronounced wounds and irritation. Check for contraindications to the procedure!
- strokes 10-15 times
- stroking the periosteal fossa (depression on the posterior surface of the shoulder blade)
- vibration, patting (10-15 times) of the periosteal fossa
- stroking (10-15 times) in the direction from the spine to the armpits
- rubbing, kneading the trapezius muscle (10 -15 times)
- vibration with the fingers and the edge of the palm (10-15 times)
- stroking the entire surface of the back
After a session of intensive healing technique, it is useful to cover the client with a warm towel and let him rest for 3-5 minutes.

Cervical collar massage technique to get rid of cellulite and unwanted fat deposits
- During the procedure, it is useful to use not a traditional massage agent, but a warming, anti-cellulite gel or oil.
- Stroking. With the help of strokes, the effect of relaxation is achieved, getting rid of dead skin cells, relaxing the body, and preparing the client for the procedure of the cervical-collar zone.
- Make rubbing movements with widely spaced fingers, as if trying to “squeeze out” excess fat, fluid from the body. The use of rubbing will increase the tone, contractile function of the muscles of the back and neck. It must be remembered that massage oils and gels reduce the force of rubbing, its warming effect, so do not use a large amount of funds during rubbing. should apply the same pressure during the application of the movement to each point of the cervical-collar zone, but be careful in places with delicate skin so as not to provoke pain.
 Rubbing is an intense, strong movement, but it should not cause pain. If you want to enhance the effect of rubbing, increase the angle between the palm of your hand and the back or neck area. Rubbing during massage of the cervical-collar zone is useful to alternate with stroking.
Rubbing is an intense, strong movement, but it should not cause pain. If you want to enhance the effect of rubbing, increase the angle between the palm of your hand and the back or neck area. Rubbing during massage of the cervical-collar zone is useful to alternate with stroking. - Do intense kneading, rolling, tapping movements that should “break up” excess subcutaneous fat. These anti-cellulite massage techniques occupy the largest part of the cervical-collar zone procedure.
- We return to stroking again to calm the client's body.
Massage against cellulite of the cervical-collar zone will allow not only to get rid of excess fat deposits, speed up blood circulation and lymph flow, but also to remove puffiness from the face, improve skin color, and the patient's well-being.
Techniques for performing massage of the collar zone using devices
A significant part of people of the 21st century work in offices and spend at least 8 hours every day in a sitting position, which does not give the body health and well-being.
 Neck and back massage is indicated for almost every office worker in the absence of contraindications. Ideally, SHVZ massage should be done once a week to relieve tension, prevent the development of osteochondrosis and other diseases. This will help home appliances for self-massage of the cervical-collar zone, which everyone can use.
Neck and back massage is indicated for almost every office worker in the absence of contraindications. Ideally, SHVZ massage should be done once a week to relieve tension, prevent the development of osteochondrosis and other diseases. This will help home appliances for self-massage of the cervical-collar zone, which everyone can use. Butterfly is a compact device that stimulates nerve contractions with harmless electrical impulses. Butterfly allows not only to relieve tension from the areas of the back, neck and shoulders, but also to reduce the amount of body fat.
Handheld massager is a compact, inexpensive and easy-to-use device with a long handle, which facilitates the procedure in hard-to-reach places.
Belt-massager, like a massager - the collar is securely fastened in the area of the cervical region and covers the entire cervical-collar surface and effectively affects a person using various vibration modes.
Pillow - massager is convenient to use in the car, in the office, at home.
 A simple evening ritual of relaxing on the couch can be turned into a useful procedure that will allow you to relax after a hard day, warn against the development of osteochondrosis and other diseases of the spine.
A simple evening ritual of relaxing on the couch can be turned into a useful procedure that will allow you to relax after a hard day, warn against the development of osteochondrosis and other diseases of the spine. Each of us saw Kuznetsov's applicator at his grandmother's. It is a rug with small roses with spikes that can be used for any part of the body. Perfectly improves blood circulation and accelerates lymph flow. The applicator is indicated for use by almost everyone and at any age.
Cervical collar massage technique is one of the most popular techniques of the 21st century, which is actively used for the health of adults and the proper development of children!
Author of the article:
Practicing: 15 years, Teaching: 8 years
Selivanov Pavel Vladimirovich
Teacher of classical, sports, reflex massage with medical education, author of unique massage techniques, specialist in acupuncture and acupuncture, expert in oriental medicine.
 Pavel gives deep, comprehensive knowledge on the subject, teaches students to work consciously, to bring maximum benefit to each client. Read more…
Pavel gives deep, comprehensive knowledge on the subject, teaches students to work consciously, to bring maximum benefit to each client. Read more… Basic education:
St. Petersburg Medical Institute. Academician I.P. Pavlova. Specialty: Dentistry
Additional and profile education:
2018 - International Training Center "Masseur of a wide profile"
Mechnikov cycle "Clinical Transfusiology"
2008 - St. Petersburg Medical Academy of Postgraduate Education of the Federal Agency for Health and Social Development "Actual Issues of Maxillofacial Surgery"
2004 - St. Petersburg Medical Academy of Postgraduate Education of the Ministry of Health of the Russian Federation. Specialty: Organization of healthcare and public health.
2004 - 2009 SPB Administration. Specialty: Maxillofacial surgery for category I.
2003 – MAPO certified cycle Topical issues of maxillofacial surgery.
2000 - Certification at the Health Committee
1998 - Postgraduate Medical Academy (MAPO).
- sessions are performed on a child who has reached 2 months.
 64-3.91
64-3.91