Jaundice in pregnancy
Hepatobiliary diseases during pregnancy and their management: An update
1. Ch’ng CL, Morgan M, Hainsworth I, Kingham JG. Prospective study of liver dysfunction in pregnancy in Southwest Wales. Gut. 2002;51:876–80. [PMC free article] [PubMed] [Google Scholar]
2. Tamay AG, Kuşçu NK. Hyperemesis gravidarum: Current aspect. J ObstetGynaecol. 2011;31:708–12. [PubMed] [Google Scholar]
3. Goodwin TM. Hyperemesis gravidarum. ObstetGynecolClin North Am. 2008;35:401–17. [PubMed] [Google Scholar]
4. Kaplan PB, Gücer F, Sayin NC, Yüksel M, Yüce MA, Yardim T. Maternal serum cytokine levels in women withhyperemesis gravidarum in the first trimester of pregnancy. FertilSteril. 2003;79:498–502. [PubMed] [Google Scholar]
5. Jewell D, Young G. Withdrawn: Interventions for nausea and vomiting in early pregnancy. Cochrane Database Syst Rev. 2010;8 [PubMed] [Google Scholar]
6. Glantz A, Marschall HU, Mattsson LA. Intrahepatic cholestasis of pregnancy: Relationships between bile acid levels and fetal complication rates. Hepatology. 2004;40:467–74. [PubMed] [Google Scholar]
7. Kondrackiene J, Kupcinskas L. Intrahepatic cholestasis of pregnancy-current achievements and unsolved problems. World J Gastroenterol. 2008;14:5781–8. [PMC free article] [PubMed] [Google Scholar]
8. Marciniak B, Kimber-Trojnar Z, Leszczyńska-Gorzelak B, Patro-Małysza J, Trojnar M, Oleszczuk J. [Treatmentof obstetriccholestasiswith polyunsaturated phosphatidylcholineandursodeoxycholic acid] Ginekol Pol. 2011;82:26–31. [PubMed] [Google Scholar]
9. Ropponen A, Sund R, Riikonen S, Ylikorkala O, Aittomäki K. Intrahepatic cholestasis of pregnancy as an indicator of liver and biliary diease: Apopulation-based study. Hepatology. 2006;43:723–8. [PubMed] [Google Scholar]
10. Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376:631–44. [PubMed] [Google Scholar]
11. Barton JR, Sibai BM. Prediction and prevention of recurrent preeclampsia. ObstetGynecol. 2008;112:359–72. [PubMed] [Google Scholar]
12. Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al. Methods of prediction and prevention of pre-eclampsia: Systematic reviews of accuracy and effectiveness literature with economic modelling. Health Technol Assess. 2008;12:1–270. [PubMed] [Google Scholar]
Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al. Methods of prediction and prevention of pre-eclampsia: Systematic reviews of accuracy and effectiveness literature with economic modelling. Health Technol Assess. 2008;12:1–270. [PubMed] [Google Scholar]
13. Duley L, Henderson-Smart DJ, Meher S. Drugs for treatment of very high blood pressure during pregnancy (Cochrane Review) The Cochrane Database of Systematic Reviews. 2006;(3) [PubMed] [Google Scholar]
14. Pryde PG, Mittendorf R. Contemporary usage of obstetric magnesium sulfate: Indication, contraindication, and relevance of dose. Obstet Gynecol. 2009;114:669–73. [PubMed] [Google Scholar]
15. Kulikov AV, Spirin SV, Blauman SI. [Clinicopathologic characteristics of HELLP-syndrome].[Article in Russian] AnesteziolReanimatol. 2010;6:87–91. [PubMed] [Google Scholar]
16. Ducarme G, Bernuau J, Luton D. [Liver and preeclampsia] Ann FrAnesthReanim. 2010;29:e97–e103. [PubMed] [Google Scholar]
17. Salahuddin S, Lee Y, Vadnais M, Sachs BP, Karumanchi SA, Lim KH. Diagnostic utility of soluble fms-like tyrosine kinase 1 and soluble endoglin in hypertensive diseases of pregnancy. Am J ObstetGynecol. 2007;197:28.e1–6. [PubMed] [Google Scholar]
Salahuddin S, Lee Y, Vadnais M, Sachs BP, Karumanchi SA, Lim KH. Diagnostic utility of soluble fms-like tyrosine kinase 1 and soluble endoglin in hypertensive diseases of pregnancy. Am J ObstetGynecol. 2007;197:28.e1–6. [PubMed] [Google Scholar]
18. Mihu D, Costin N, Mihu CM, Seicean A, Ciortea R. HELLP syndrome–a multisystemic disorder. J Gastrointestin Liver Dis. 2007;16:419–24. [PubMed] [Google Scholar]
19. Onyangunga OA, Moodley J. Managing pregnancy with HIV, HELLP syndrome and low platelets. Best Pract Res Clin Obstet Gynaecol. 2012;26(1):133–47. [PubMed] [Google Scholar]
20. Martin JN, Jr, Rose CH, Briery CM. Understanding and managing HELLP syndrome: The integral role of aggressive glucocorticoids for mother and child. Am J Obstet Gynecol. 2006;195:914–34. [PubMed] [Google Scholar]
21. Woudstra DM, Chandra S, Hofmeyr GJ, Dowswell T. Corticosteroids for HELLP (hemolysis, elevated liver enzymes, low platelets) syndrome in pregnancy. Cochrane Database Syst Rev. 2010;9 [PMC free article] [PubMed] [Google Scholar]
2010;9 [PMC free article] [PubMed] [Google Scholar]
22. Ibdah JA. Acute fatty liver of pregnancy: An update on pathogenesis and clinical implications. World J Gastroenterol. 2006;12:7397–404. [PMC free article] [PubMed] [Google Scholar]
23. Williams J, Mozurkewich E, Chilimigras J, Van De Ven C. Critical care in obstetrics: Pregnancy-specific conditions. Best Pract Res ClinObstetGynaecol. 2008;22:825–46. [PubMed] [Google Scholar]
24. Hay JE. Liver disease in pregnancy. Hepatology. 2008;47:1067–76. [PubMed] [Google Scholar]
25. Devarbhavi H, Kremers WK, Dierkhising R, Padmanabhan L. Pregnancy-associated acute liver disease and acute viral hepatitis: Differentiation, course and outcome. J Hepatol. 2008;49:930–5. [PubMed] [Google Scholar]
26. vanZonneveld M, van Nunen AB, Niesters HG, de Man RA, Schalm SW, Janssen HL. Lamivudine treatment during pregnancy to prevent perinatal transmission of hepatitis B virus infection. J Viral Hepat. 2003;10:294–7. [PubMed] [Google Scholar]
27. US Food and Drug Administration, FDA. Available from: http://www.fda.gov.Drugs/DrugsSafety/Postmarket Drug Safety Information for Patientsand Providers/ucm111085 .
US Food and Drug Administration, FDA. Available from: http://www.fda.gov.Drugs/DrugsSafety/Postmarket Drug Safety Information for Patientsand Providers/ucm111085 .
28. Heneghan MA, Norris SM, O’Grady JG, Harrison PM, McFarlane IG. Management and outcome of pregnancy in autoimmune hepatitis. Gut. 2001;48:97–102. [PMC free article] [PubMed] [Google Scholar]
29. Schramm C, Herkel J, Beuers U, Kanzler S, Galle PR, Lohse AW. Pregnancy in autoimmune hepatitis: Outcome and risk factors. Am J Gastroenterol. 2006;101:556–60. [PubMed] [Google Scholar]
30. Poupon R, Chrétien Y, Chazouillères O, Poupon RE. Pregnancy in women with ursodeoxycholic acid-treated primary biliary cirrhosis. J Hepatol. 2005;42:418–9. [PubMed] [Google Scholar]
31. Sternlieb I. Wilson's disease and pregnancy. Hepatology. 2000;31:531–2. [PubMed] [Google Scholar]
32. Elinav E, Ben-Dov IZ, Sharpia Y, Daudi N, Adler R, Shouval D, et al. Acute hepatitis A infection in pregnancy is associated with high rates of gestational complications and preterm labor. Gastroenterology. 2006;130(4):1129–34. [PubMed] [Google Scholar]
Gastroenterology. 2006;130(4):1129–34. [PubMed] [Google Scholar]
33. Banait VS, Sandur V, Parikh F, Murugesh M, Ranka P, Ramesh VS, et al. Outcome of acute liver failure due to acute hepatitis E in pregnant women. Indian J Gastroenterol. 2007;26:6–10. [PubMed] [Google Scholar]
34. Bhatia V, Singhal A, Panda SK, Acharya SK. A 20-year single-center experience with acute liver failure during pregnancy: Is the prognosis really worse? Hepatology. 2008;48:1577–85. [PubMed] [Google Scholar]
35. Mushahwar IK. Hepatitis E virus: Molecular virology, clinical features, diagnosis, transmission, epidemiology, and prevention. J Med Virol. 2008;80:646–58. [PubMed] [Google Scholar]
36. Gilat T, Konikoff F. Pregnancy and the biliary tract. Can J Gastroenterol. 2000;14(Suppl D):55D–59D. [PubMed] [Google Scholar]
37. Lu EJ, Curet MJ, El-Sayed YY, Kirkwood KS. Medical versus surgical management of biliary tract disease in pregnancy. Am J Surg. 2004;188:755–9. [PubMed] [Google Scholar]
38. Rautou PE, Plessier A, Bernuau J, Denninger MH, Moucari R, Valla D. Pregnancy: A risk factor for Budd-Chiari syndrome? Gut. 2009;58:606–8. [PubMed] [Google Scholar]
Rautou PE, Plessier A, Bernuau J, Denninger MH, Moucari R, Valla D. Pregnancy: A risk factor for Budd-Chiari syndrome? Gut. 2009;58:606–8. [PubMed] [Google Scholar]
Jaundice in Pregnancy | Patient
Jaundice in Pregnancy
In this article
- Acute viral hepatitis
- Cholelithiasis in pregnancy
- Chronic liver disease
- Autoimmune hepatitis
- Pre-eclamptic liver disease and HELLP
- Acute fatty liver of pregnancy
- Intrahepatic cholestasis of pregnancy
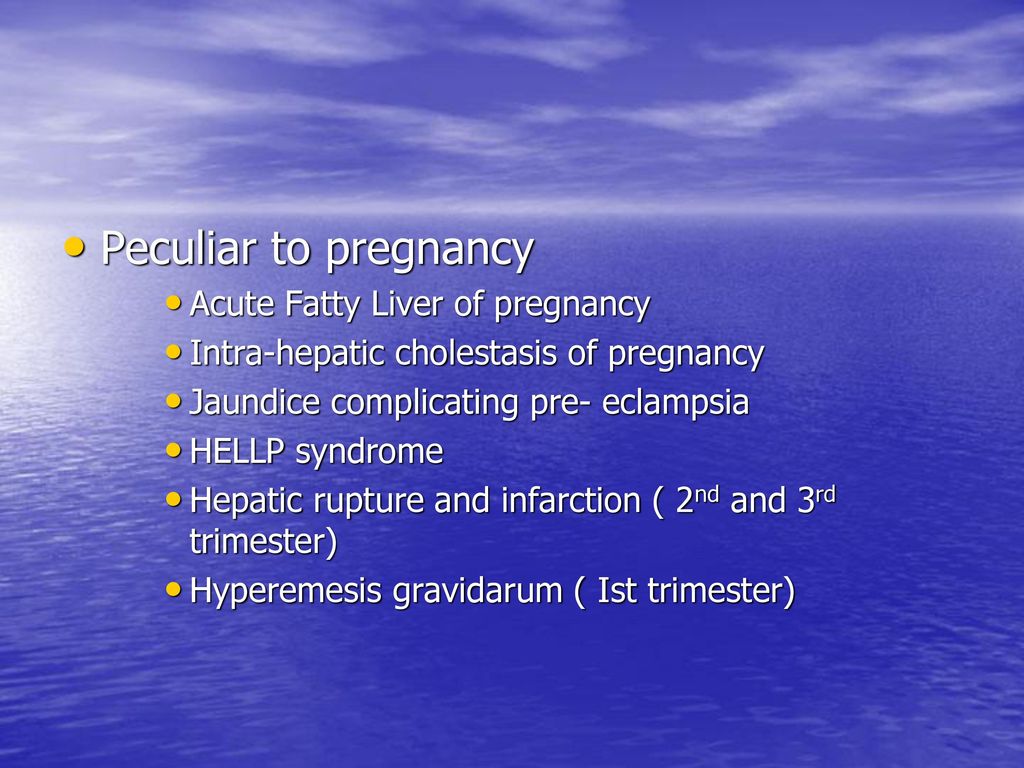
Jaundice in pregnancy, whilst relatively rare, has potentially serious consequences for maternal and fetal health. It can be caused by pregnancy or occur intercurrently. Causes of jaundice specific to pregnancy include:
- Pre-eclampsia associated with HELLP syndrome (= haemolysis, elevated liver enzymes and low platelet count).

- Acute fatty liver of pregnancy.
- Hyperemesis gravidarum.
- Intrahepatic cholestasis of pregnancy.
The presenting clinical features of liver disease in pregnancy are often nonspecific and consist of jaundice, nausea, vomiting and abdominal pain. All liver diseases occurring during pregnancy can lead to increased maternal and fetal morbidity and mortality[1].
Acute viral hepatitis
[2]Viral hepatitis is the most common cause of jaundice in pregnancy with infections due to hepatitis A, hepatitis B, hepatitis C, hepatitis D and hepatitis E viruses.
The incidence of hepatitis in pregnancy varies greatly around the world; in developed countries the incidence is around 0.1%, whilst in developing countries it can range from 3-20% or higher.
- Hepatitis A is most prevalent in developing countries. 1:1,000 pregnant women are infected with acute hepatitis A virus (HAV). The disease is mostly self-limited, with mortality of 0.
 3% to 0.6%.
3% to 0.6%. - Hepatitis B affects more than 250 million individuals worldwide and is the most common cause of chronic hepatitis worldwide. Sixty-five million women of childbearing age are infected with chronic hepatitis B virus (HBV). About 800,000 to 1.4 million people are infected with HBV in the USA. There is a 0.7% to 0.9% prevalence of chronic HBV infection among pregnant women in the USA.
- Hepatitis C virus (HCV) affects more than 170 million people worldwide. About 8% of pregnant women are infected with HCV. The estimated prevalence of antenatal HCV infection in the USA is 1% to 2.5%.
- Hepatitis D virus (HDV) affects 15-20 million people worldwide with HBV carriers. New studies estimate the prevalence of hepatitis D to be closer to 62-72 million. The prevalence of HDV in the USA is estimated to range from 2% to 50%, depending on the patient population. The prevalence of HDV in a study in Pakistan revealed an estimated 20.63% in pregnant women with chronic HBV infection.

- Hepatitis E virus (HEV) affects about 20.1 million new infections. HEV infection is prevalent in developing countries. The course of most viral hepatitis infections is unaltered by pregnancy - the exception is hepatitis E, where pregnant women who contract the disease exhibit fatality rates of 10-20%.
Hepatitis A
See the separate Hepatitis A article for further information.
- Isolate the infected patient to prevent spread.
- Symptomatic treatment includes maintenance of adequate hydration and nutrition.
- Pregnant women exposed to the virus can be given immune globulin within two weeks of exposure, together with vaccine.
- It is not clear if the virus is transmitted from mother to baby but, if the illness has occurred in the final month of pregnancy, the neonate should receive immune globulin.
Hepatitis B
See the separate Hepatitis B article for further information.
- This is the most common cause of acute viral hepatitis in pregnancy and can occur in acute, subclinical or chronic form.

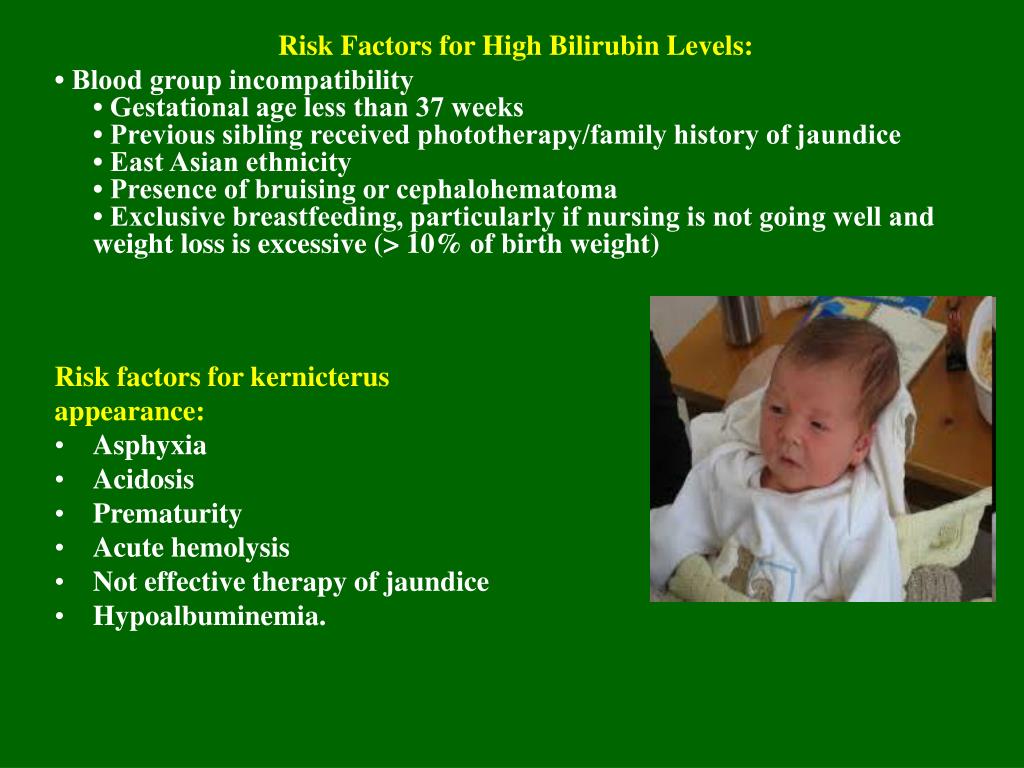
- The presence of HBeAg is associated with a very high risk of neonatal infection.
- All women should now be offered hepatitis B screening as part of routine antenatal screening.
- Infants of HBsAg-positive women should receive hepatitis B immune globulin immunoprophylaxis at birth and hepatitis B vaccine at 1 week, 1 month and 6 months of age. This regime reduces the incidence of hepatitis B vertical transmission to less than 3%.
- The prevalence of neonatal infection depends on the time during gestation that maternal infection takes place: rare in the first trimester, 6% in the second trimester and 67% of those in the third trimester.
Hepatitis C
See the separate Hepatitis C article for further information.
- No therapy has been shown to influence the neonatal transmission of HCV.
- Interferon should not be used during pregnancy because of possible adverse effects on the fetus.
Hepatitis D
This develops as a co-infection with hepatitis B. When present, it increases the incidence of acute hepatic failure.
When present, it increases the incidence of acute hepatic failure.
Hepatitis E
- This is rare in the developed world but, in developing countries (where it is more common), it is responsible for a high level of fulminant hepatic failure and mortality in pregnant women.
- In India it appears to be associated with a higher maternal mortality rate and worse obstetric and fetal outcomes compared with other causes of acute viral hepatitis in pregnancy.
Cholelithiasis in pregnancy
Symptomatic gallstone disease occurs in approximately 1 in 2,000 pregnancies[3].
Pregnancy alters bile composition and gallbladder emptying slows in the second trimester, increasing the risk of gallstones.
Individual risk factors are multiparity and previous gallbladder disease.
Presentation
Symptoms are similar in pregnant and non-pregnant women:
- Pain in the right upper quadrant or epigastrium, peaking at 12-24 hours.
- Pain may radiate towards the back and there may be epigastric or right upper-quadrant tenderness.
 Murphy's sign (right-sided tenderness at the tip of the 9th costal cartilage as the patient breathes in) is much less common in pregnancy.
Murphy's sign (right-sided tenderness at the tip of the 9th costal cartilage as the patient breathes in) is much less common in pregnancy.
Management
Obstructive jaundice requires surgical intervention, usually via laparoscopic cholecystectomy. There is an associated fetal loss of approximately 6%.
Chronic liver disease
Chronic liver disease in pregnancy is associated with an increased risk of fetal loss:
- In patients with primary biliary cirrhosis (PBC), ursodeoxycholic acid can be safely continued. Cholestasis may worsen during pregnancy with PBC[4].
- Infants of patients with marked hyperbilirubinaemia during pregnancy may require exchange transfusion at birth.
Autoimmune hepatitis
[5]Autoimmune hepatitis (AIH) in pregnancy is associated with an increased risk of fetal complications and maternal complications. However, data show that the number of pregnancies reported in women with AIH is becoming more frequent due to better clinical management and high-quality prenatal and antenatal care. Currently, pregnancy and childbirth in AIH appear to be safe for both mother and child. Azathioprine treatment has been used during pregnancy.
Currently, pregnancy and childbirth in AIH appear to be safe for both mother and child. Azathioprine treatment has been used during pregnancy.
Pre-eclamptic liver disease and HELLP
See the separate HELLP Syndrome article for further details.
This complicates 3-10% of pre-eclamptic pregnancies and the risk of recurrence in future pregnancies is 3-4%.
The most effective treatment for HELLP is prompt delivery.
Acute fatty liver of pregnancy
[6]Epidemiology
- It is a rare condition with a prevalence of 0.005 - 0.01%.
- Acute fatty liver of pregnancy (AFLP) tends to occur in late pregnancy.
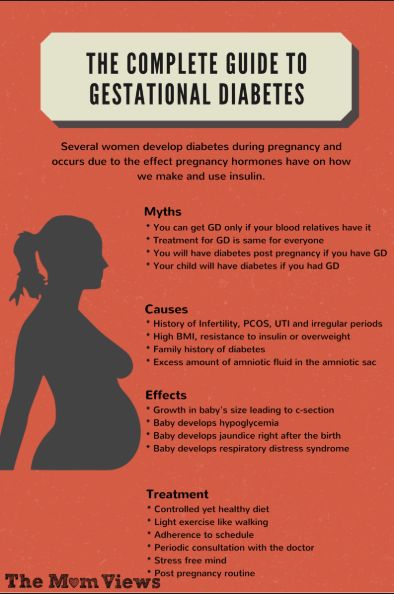
- Risk factors include first pregnancies, pre-eclampsia, twin pregnancies and male fetuses.
- It may be associated with a mutant gene producing a defect in mitochondrial fatty acid oxidation and infants born to mothers with AFLP should be screened for defects in this system.
Presentation
This usually presents acutely with nausea, vomiting and abdominal pain, fevers, headache and pruritus, beginning typically at about 35 weeks of gestation but can occur much earlier. It may also appear immediately after delivery.
It may also appear immediately after delivery.
Jaundice appears soon after onset of symptoms and can become intense in a large proportion of patients. Fulminant liver failure may follow.
Investigations
- The white cell count is often elevated. There may also be neutrophilia and thrombocytopenia.
- Liver transaminases are moderately high.
- Raised serum bilirubin.
- Abnormal clotting with coagulopathy (prolongation of prothrombin and partial thromboplastin times with depression of fibrinogen levels).
Biopsy would be diagnostic but coagulation problems often preclude it. CT/MRI scanning may show reduced attenuation in the liver.
Management
Consider early delivery, as the condition usually resolves afterwards with complete recovery. Supportive ITU care is frequently required.
Complications
AFLP is a life-threatening condition. To date, there are no reports of spontaneous remission of AFL prior to delivery of the infant. The characteristic course is progression to acute liver failure within one or two weeks, which is characterised by increasing jaundice, hypoglycaemia, development of coagulopathy, ascites/pleural effusions, encephalopathy and acute kidney failure in up to 90% of affected women.
The characteristic course is progression to acute liver failure within one or two weeks, which is characterised by increasing jaundice, hypoglycaemia, development of coagulopathy, ascites/pleural effusions, encephalopathy and acute kidney failure in up to 90% of affected women.
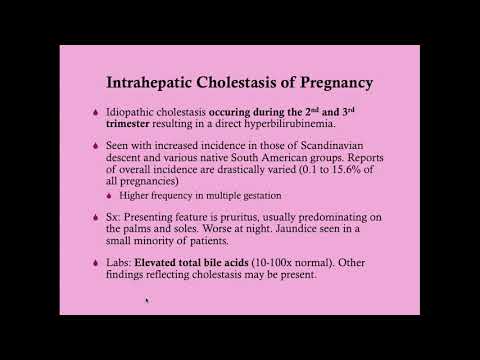
Intrahepatic cholestasis of pregnancy
Intrahepatic cholestasis is defined as pruritus with elevated serum bile acids occurring in the second half of pregnancy, which resolves after delivery.
See also the separate Obstetric Cholestasis article.
Epidemiology
ICP incidence rate is between 0.2% to 2% of pregnancies[7]. It is more common in South American and northern European continents. Research has described ICP in 0.2% to 0.3% of pregnancies in the USA.
Presentation
The main symptom is pruritus, especially of the palms and soles, which is followed by generalised symptoms. This usually occurs from week 25 of gestation.
Jaundice is uncommon. However, when present, it arises 2-4 weeks after the onset of pruritus.
Investigations
- Aminotransferase activity can be increased by 20 times the normal level.
- Raised gamma-glutamyltransferase activity is unusual but is indicative of MDR3 mutation or underlying liver disease unrelated to pregnancy. The key diagnostic test is a fasting serum bile acid concentration of greater than 10 mmol/L.
Management
Ursodeoxycholic acid is the mainstay of medical management, but it has not been shown to reduce adverse perinatal outcomes in women with ICP. Therefore, some call for its routine use for this condition be reconsidered[8].
Complications
Maternal morbidity results from pruritus and insomnia. The importance of this disorder is the effects on the fetus which can lead to prematurity, perinatal death, fetal distress and stillbirth. ICP often recurs in subsequent pregnancies[9].
Ibrahimi S, Mroue AA, Francois E, et al; Jaundice in a pregnant woman. Acta Gastroenterol Belg.
 2017 Jul-Sep80(3):422-424.
2017 Jul-Sep80(3):422-424.Gupta A, Tiwari P, Sachdeva P; A Case of Dubin-Johnson Syndrome in Pregnancy. Cureus. 2019 Feb 1111(2):e4048. doi: 10.7759/cureus.4048.
Lata I; Hepatobiliary diseases during pregnancy and their management: An update. Int J Crit Illn Inj Sci. 2013 Jul3(3):175-82. doi: 10.4103/2229-5151.119196.
Asafo-Agyei KO, Samant H; Pregnancy And Viral Hepatitis
Mukherjee R, Samanta S; Surgical emergencies in pregnancy in the era of modern diagnostics and treatment. Taiwan J Obstet Gynecol. 2019 Mar58(2):177-182. doi: 10.1016/j.tjog.2019.01.001.
Ducarme G, Bernuau J, Luton D; [Primary biliary cirrhosis and pregnancy]. J Gynecol Obstet Biol Reprod (Paris). 2014 May43(5):335-41. doi: 10.1016/j.jgyn.2013.03.016. Epub 2013 Apr 28.
Kothadia JP, Shah JM; Autoimmune Hepatitis and Pregnancy
Rath W, Tsikouras P, Stelzl P; HELLP Syndrome or Acute Fatty Liver of Pregnancy: A Differential Diagnostic Challenge: Common Features and Differences.
 Geburtshilfe Frauenheilkd. 2020 May80(5):499-507. doi: 10.1055/a-1091-8630. Epub 2020 May 18.
Geburtshilfe Frauenheilkd. 2020 May80(5):499-507. doi: 10.1055/a-1091-8630. Epub 2020 May 18.Pillarisetty LS, Sharma A; Pregnancy Intrahepatic Cholestasis. StatPearls Publishing 2021.
Chappell LC, Bell JL, Smith A, et al; Ursodeoxycholic acid versus placebo in women with intrahepatic cholestasis of pregnancy (PITCHES): a randomised controlled trial. Lancet. 2019 Sep 7394(10201):849-860. doi: 10.1016/S0140-6736(19)31270-X. Epub 2019 Aug 1.
Ovadia C, Seed PT, Sklavounos A, et al; Association of adverse perinatal outcomes of intrahepatic cholestasis of pregnancy with biochemical markers: results of aggregate and individual patient data meta-analyses. Lancet. 2019 Mar 2393(10174):899-909. doi: 10.1016/S0140-6736(18)31877-4. Epub 2019 Feb 14.
Cholestasis of pregnancy - Into-Sana
Cholestasis of pregnancy (CP) - a syndrome characterized by stagnation of bile in the gallbladder and bile ducts of a woman during pregnancy, which is manifested by skin itching and jaundice. Usually this syndrome completely regresses after childbirth.
Usually this syndrome completely regresses after childbirth.
Contents:
- Types of cholestasis of pregnancy
- Causes of cholestasis of pregnancy
- Symptoms of cholestasis of pregnancy
- Diagnosis of cholestasis of pregnancy
- Methods of treatment of cholestasis of pregnancy
- Sequelae of cholestasis of pregnancy
Types of cholestasis of pregnancy
Cholestasis of pregnancy is divided into extrahepatic and intrahepatic depending on the localization of bile outflow disorders. Icteric and anicteric forms of the course of this disease are also possible.
Causes of cholestasis of pregnancy
The frequency of chronic bronchitis is due to ethnic and geographical characteristics: in Latin America it is more common than among representatives of the Scandinavian countries. In Europe, the prevalence of this pathology is 1-2% of all pregnant women. In addition, cholestasis is a syndrome, the likelihood of which in a woman increases if one of her relatives in the female line has suffered this pathology, that is, we can talk about a genetic predisposition to cholestasis of pregnant women.
In addition, cholestasis is a syndrome, the likelihood of which in a woman increases if one of her relatives in the female line has suffered this pathology, that is, we can talk about a genetic predisposition to cholestasis of pregnant women.
The cause of extrahepatic cholestasis is mechanical compression of the gallbladder (multiple pregnancy contributes to this, as well as deformation of the gallbladder: bends / bends, etc.). As a result, there is a violation of the outflow of bile and the absorption of bile pigments into the blood.
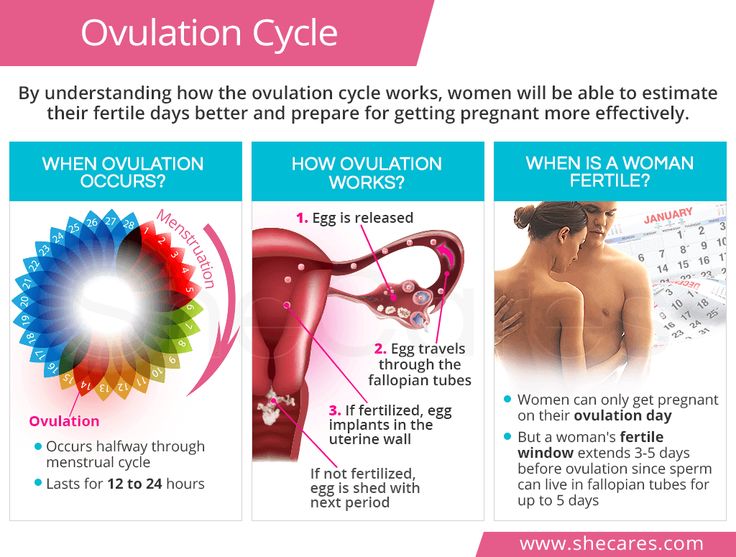
Intrahepatic cholestasis (idiopathic jaundice of pregnancy) is a benign disease that occurs during pregnancy, the main manifestations of which are pruritus and/or jaundice. This condition is one of the most common pathologies in pregnant women. As a rule, it manifests itself in the III trimester of pregnancy, in 20-30% of cases - in the II trimester, in very rare cases from the 6th week of pregnancy. Symptoms usually regress 1-3 weeks after delivery.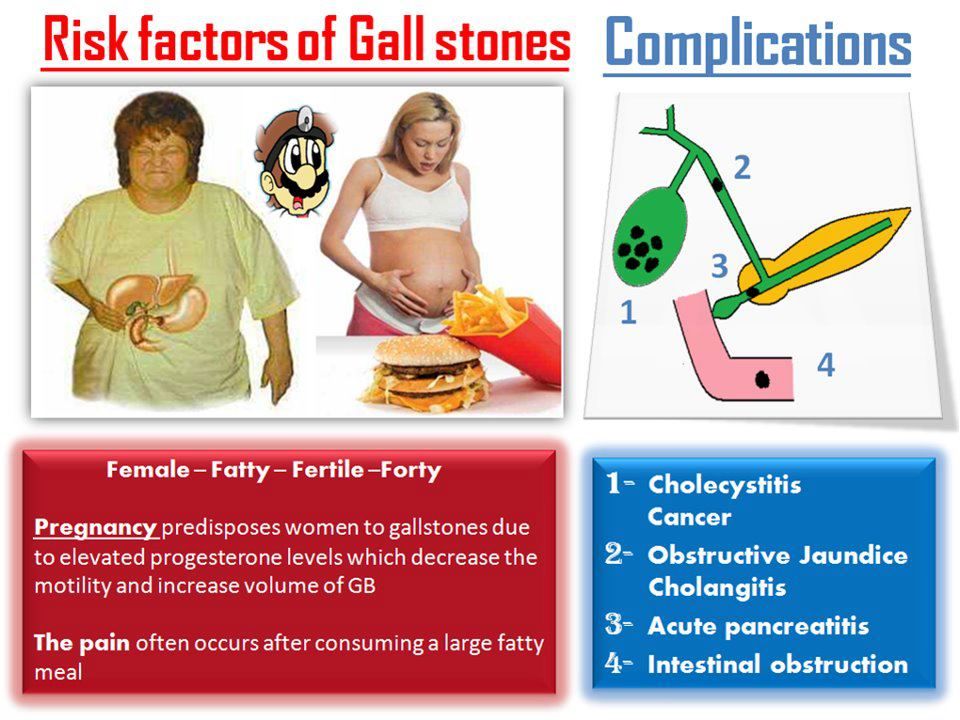
Cause of intrahepatic cholestasis - genetically determined hypersensitivity to estrogens. Pregnancy in this case plays the role of a trigger: changes in the hormonal background of a woman provoke violations of bile formation and bile secretion. Due to the hereditary nature of the disease, symptoms will usually recur in subsequent pregnancies.
Symptoms of cholestasis of pregnancy
For extrahepatic cholestasis is characterized by heaviness in the right hypochondrium, skin itching, some lightening of feces, darkening of urine. There may be jaundice. Constipation is also observed, which may be associated with intestinal compression.
Manifestations of intrahepatic cholestasis are more varied. The mild form is manifested by skin itching, more often at night. In this case, changes in the skin are not determined. Sometimes this is the only symptom. More often, after 1-2 weeks, yellowing of the skin joins. Darkening of urine is possible, occasionally - lightening of feces.
Darkening of urine is possible, occasionally - lightening of feces.
In more severe forms of intrahepatic cholestasis of pregnancy, digestive disorders may join: nausea, feeling of fullness in the stomach, heaviness after eating, loss of appetite. Perhaps the appearance of dull pain in the right hypochondrium, sometimes vomiting. Patients become lethargic, lethargic, apathetic. The extreme manifestation is hepatic encephalopathy. On the skin, traces of scratching can be found.
With prolonged existence of the disease, such manifestations as weight loss, weight loss, as well as symptoms of vitamin D deficiency (bone pain, increased fragility), E (general weakness, muscle weakness), K (appearance of small hemorrhagic lesions on the skin) appear. rashes), A (impaired vision at dusk, dry skin and mucous membranes).
Diagnosis х
olestasis of pregnant women Since the load on the woman's liver increases significantly during childbearing, even in the physiological course of pregnancy, changes in laboratory tests can be detected in the absence of clinical manifestations. Therefore, the doctor needs to focus not only on the test data, but also on the overall clinical picture.
Therefore, the doctor needs to focus not only on the test data, but also on the overall clinical picture.
In addition to anamnesis data, examination of complaints and examination of patients, laboratory and instrumental methods . The necessary laboratory parameters for evaluation are: complete blood count, liver tests (bilirubin fractions, ALT, AST, alkaline phosphatase, gamma-glutamyl transpeptidase), the level of bile acids in the blood, blood cholesterol, coagulogram.
Ultrasound diagnostics makes it possible to confirm the diagnosis or to identify other concomitant diseases of the liver and biliary tract. In difficult cases, as well as in cases of severe comorbidity, it is possible to perform a liver biopsy. MRI diagnostics is not used.
Differential diagnosis is carried out with such diseases as acute viral hepatitis, acute fatty degeneration of the liver of pregnant women, late preeclampsia. In view of possible complications for the fetus, dynamic monitoring of its condition is carried out, if there are signs of fetal hypoxia, the issue of emergency delivery is resolved.
Methods of treatment x
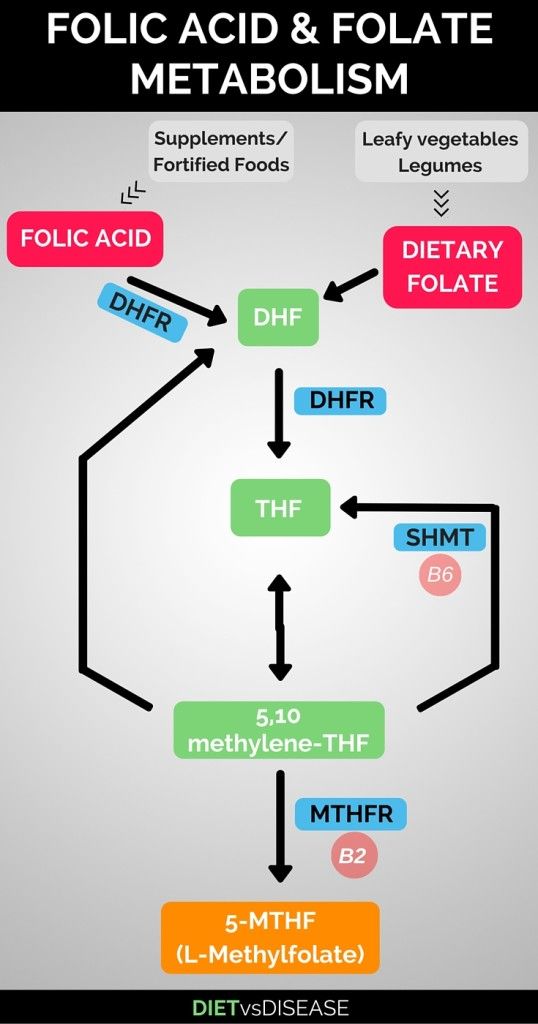
olestasis of pregnancyDrug and non-drug methods of therapy are used to treat cholestasis of pregnancy. The most important of the non-drug methods is diet therapy. Patients are prescribed a balanced diet with limited fat and increased protein intake. It is advisable to include in the diet foods rich in lipotropic enzymes (cottage cheese, buckwheat and oatmeal), B vitamins, folic acid.
Drug therapy is prescribed by the doctor individually, taking into account the severity of the patient's condition and the characteristics of the course of the pathology.
Consequences х
pregnancy olestasis Despite the fact that the disease is benign, the lack of treatment can lead to sad consequences. For the mother, severe forms of intrahepatic cholestasis and associated disorders of vitamin K synthesis can cause severe postpartum bleeding, and the risk of inflammatory postpartum diseases also increases.
Intrahepatic cholestasis also has an extremely unfavorable effect on the child. The placental blood flow worsens, as a result of which the fetus receives less nutrients. A high concentration of bile acids in the mother's blood can provoke the onset of premature birth, fetal hypoxia, respiratory distress syndrome, cardiac arrhythmias in newborns, and the presence of meconium amniotic fluid. In severe cases, intrauterine fetal death is possible.
Among the long-term consequences for the mother, it is worth mentioning the increased risk of developing cholelithiasis, cholecystitis, non-alcoholic hepatitis and cirrhosis of the liver, non-alcoholic pancreatitis.
Pregnant women with a diagnosis of cholestasis are observed by a general practitioner and an obstetrician-gynecologist in order to dynamically monitor and conduct adequate treatment, as well as prevent complications. It should be noted that if cholestasis occurred at least once during pregnancy, then in future pregnancies it will be present in 90% of cases.
Intrahepatic cholestasis of pregnancy. Kuzmin V.N.
Oksana Mikhailovna Drapkina Professor, Doctor of Medical Sciences:
- Professor Kuzmin Vladimir Nikolaevich will tell us about intrahepatic cholestasis of pregnant women.
Vladimir Nikolayevich Kuzmin Professor, Doctor of Medical Sciences:
- I would like to dwell on an important problem - the problem of liver pathologies in pregnant women and, in particular, intrahepatic cholestasis of pregnant women. I would like to say that in general there is an increase in various liver pathologies in the population, and pregnant women are no exception. Unfortunately, various related specialists deal with this problem: both gastroenterologists and infectious disease specialists, and, of course, obstetrician-gynecologists deal with this problem.
...about the fact that there are quite severe complications in various forms of liver pathologies. Unfortunately, patients who already have liver disease before pregnancy exacerbate the pregnancy situation. And vice versa, sometimes pregnancy can contribute to some kind of disruption of adaptation processes, liver diseases, liver pathologies, causing severe obstetric pathology and pregnancy complications.
And vice versa, sometimes pregnancy can contribute to some kind of disruption of adaptation processes, liver diseases, liver pathologies, causing severe obstetric pathology and pregnancy complications.
In general, what are we afraid of for the mother and fetus when there is one or another pathology of the liver? First of all, the development of complications of liver failure due to the high load on the liver during pregnancy, especially when the patient has various chronic liver diseases.
Also dangerous is the disruption of adaptive processes with the development of obstetric pathology, such as the development of preeclampsia, preeclampsia, intrahepatic cholestasis, more severe forms of complications in the form of HELLP-syndrome and the development of placental insufficiency. There are also problems of infectious genesis - first of all, infection with hepatitis B and C viruses, both during pregnancy and during childbirth. And complications of various chronic volumetric lesions and formations of the liver or complications associated with the course of a malignant tumor process of the liver, which can be aggravated by pregnancy itself.
Today, according to the classification of liver disease, it is customary to divide it into liver pathologies caused by pregnancy, that is, directly related to pregnancy. First of all, it is intrahepatic cholestasis of pregnancy, these are such serious conditions as acute fatty hepatosis of pregnant women, and various forms of gestosis, preeclampsia, severe forms in the form of HELLP syndrome. The second part is liver diseases not associated with pregnancy. This huge group is represented by viral hepatitis, other sexually transmitted infections, HIV infections, herpes infection, as well as general somatic diseases - primarily cholelithiasis. There are also chronic liver diseases during pregnancy, mainly due to either diffuse liver diseases or some various volumetric formations in the liver area.
The appearance of such a factor as jaundice in pregnant women is often classified only in one direction - this is the development of viral hepatitis. But, unfortunately, the reasons can be different, and the concept of jaundice cannot be reduced only to the development of viral hepatitis.
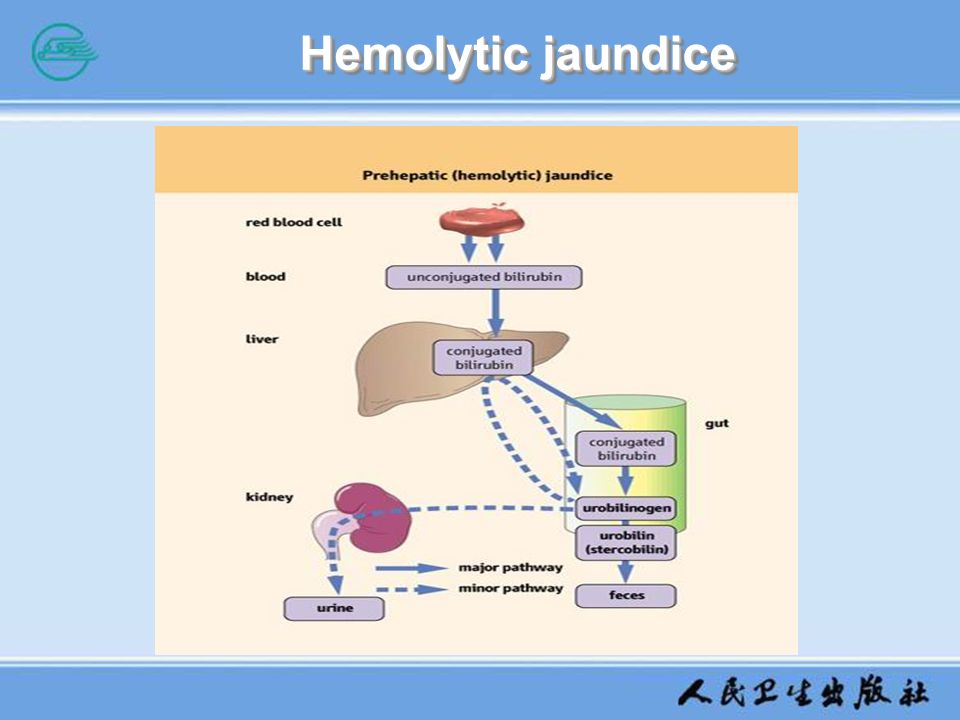
First of all, this is due to suprahepatic factors, mainly with the development of hemolysis, HELLP syndrome as a severe complication, DIC. Due to an increase in bilirubin, other indicators. Of course, such severe complications, in the first place, from the point of view of obstetric tactics, are aimed at emergency delivery.
The second category of factors that can cause jaundice during pregnancy is associated with hepatic factors. These include just hepatitis, and liver dystrophy, as well as intrahepatic cholestasis of pregnancy, as well as various forms of fermentopathy. Basically, they are associated with a change in the level of liver enzymes: bilirubin, and other functional tests, which entails different tactics for managing such patients.
The third group is subhepatic factors associated mainly with cholelithiasis and obstruction of the biliary tract, which are stopped, mainly, either by surgical or conservative removal of bile from the body.
Today, among the causes of liver dysfunction in pregnant women, there are two main causes: these are viral hepatitis, as well as cholestasis of pregnant women. Of course, these two causes basically form the entire pathology of liver function in pregnant women, and basically it is necessary to differentiate between these components. Therefore, the mandatory complex of examination of pregnant women should include a more extended concept of examination, primarily for viral hepatitis. Not only on the Hbs antigen, which is more used and for which pregnant women are examined, but a more detailed situation, because, unfortunately, it is not always possible to develop tactics for managing pregnant women simply by common markers of both hepatitis B and hepatitis C, as during pregnancy, and the solution of the issue of delivery.
Of course, these two causes basically form the entire pathology of liver function in pregnant women, and basically it is necessary to differentiate between these components. Therefore, the mandatory complex of examination of pregnant women should include a more extended concept of examination, primarily for viral hepatitis. Not only on the Hbs antigen, which is more used and for which pregnant women are examined, but a more detailed situation, because, unfortunately, it is not always possible to develop tactics for managing pregnant women simply by common markers of both hepatitis B and hepatitis C, as during pregnancy, and the solution of the issue of delivery.
It is also necessary to expand the questions about the examination of pregnant patients in terms of biochemical research associated with the determination of various indicators of the biochemical composition of the blood. But here I want to say that some changes in biochemical parameters sometimes change depending on the duration of pregnancy or against the background of pregnancy. We are talking about the following indicators: albumin can decrease by about 20%, this should also be borne in mind; it is an alkaline phosphatase that may be elevated; it's cholesterol. Of the various forms of globulins, gamma globulins may decrease somewhat. Invariable indicators, which, we believe, should be generalized and emphasized in pregnant women: first of all, these are bilirubin indicators; these are indicators of liver enzymes ALT and AST; these are various forms of triglycerides, which, by the way, can also increase, but slightly with an increase in the duration of pregnancy; and other indicators of the biochemical composition of the blood, on the basis of which it is possible to suspect or diagnose various changes in liver function.
We are talking about the following indicators: albumin can decrease by about 20%, this should also be borne in mind; it is an alkaline phosphatase that may be elevated; it's cholesterol. Of the various forms of globulins, gamma globulins may decrease somewhat. Invariable indicators, which, we believe, should be generalized and emphasized in pregnant women: first of all, these are bilirubin indicators; these are indicators of liver enzymes ALT and AST; these are various forms of triglycerides, which, by the way, can also increase, but slightly with an increase in the duration of pregnancy; and other indicators of the biochemical composition of the blood, on the basis of which it is possible to suspect or diagnose various changes in liver function.
In particular, in terms of the frequency of development today among pregnant women, there are a large number of women who are diagnosed with such a thing as intrahepatic cholestasis of pregnancy - this is a degenerative liver damage caused precisely by the sensitivity of hepatocytes to sex hormones, mainly estrogen, during pregnancy. This situation occurs against the background of pregnancy, and after delivery, intrahepatic cholestasis and its symptoms gradually disappear. Basically, the incidence of intrahepatic cholestasis is more characteristic of development in the second half of pregnancy, and even after 30 weeks of pregnancy.
This situation occurs against the background of pregnancy, and after delivery, intrahepatic cholestasis and its symptoms gradually disappear. Basically, the incidence of intrahepatic cholestasis is more characteristic of development in the second half of pregnancy, and even after 30 weeks of pregnancy.
From the point of view of different spelling of diagnoses, it sometimes appears as the concept of intrahepatic cholestasis, as cholestatic hepatosis of pregnancy, as idiopathic intrahepatic jaundice in pregnancy. But according to the ICD-10 classification, all these are liver lesions during pregnancy, childbirth or the postpartum period.
To date, the various degrees of severity of intrahepatic cholestasis are classified mainly according to the severity of the disease: it is mild, moderate and severe. Doctors mainly have to deal with moderate or severe intrahepatic cholestasis.
I would like to talk about several factors that predispose the development of intrahepatic cholestasis and which sometimes need to be paid attention to when such women enter various hospitals, in particular, maternity hospitals. First of all, there is a genetically determined hypersensitivity of hepatocytes, and this is a genetically determined disease. Intrahepatic cholestasis is mainly transmitted through the maternal line, therefore, from the anamnesis, you can also pay attention to these factors. There may be a congenital defect in the synthesis of enzymes and a congenital defect in the synthesis of bile acids, as a result of which such an atypical reaction occurs.
First of all, there is a genetically determined hypersensitivity of hepatocytes, and this is a genetically determined disease. Intrahepatic cholestasis is mainly transmitted through the maternal line, therefore, from the anamnesis, you can also pay attention to these factors. There may be a congenital defect in the synthesis of enzymes and a congenital defect in the synthesis of bile acids, as a result of which such an atypical reaction occurs.
Next, I would like to draw the attention of doctors to the recurrent nature of intrahepatic cholestasis in repeated pregnancies. Therefore, if a woman is in a second pregnancy or is giving birth again, it is imperative to pay attention to whether there were similar clinical symptoms, manifestations of cholestasis in this pregnant woman in previous pregnancies.
Clinical manifestations are mainly characterized by the development of cholestasis in both the second and third trimesters of pregnancy. Moreover, there is a tendency to an increase in clinical manifestations closer to childbirth, and their complete disappearance after delivery.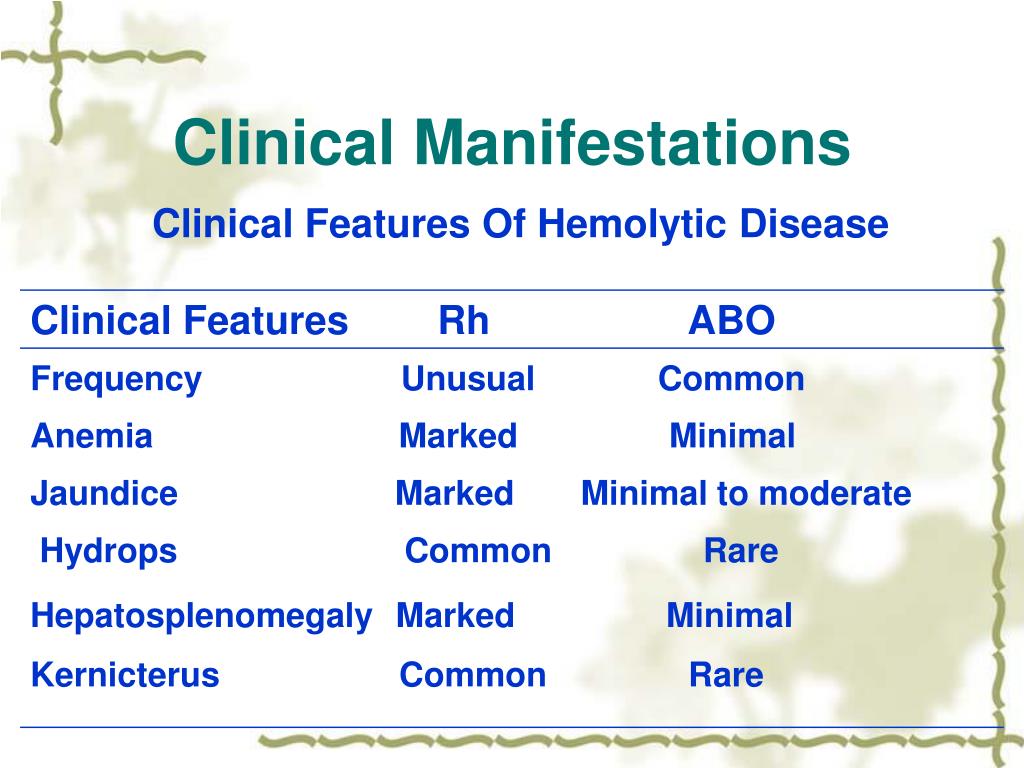
However, this pathology can also lead to complications in terms of obstetric pathology. This is, first of all, of course, the development of a large number of complications in the form of abortion, mainly at a later stage with the development of premature birth, with the development of a state of fetal distress syndrome, and the impact on the placental complex, and on pregnancy in general, can cause even late fetal death.
To assess the clinical manifestations, it is necessary to evaluate, first of all, situations associated with women after 20 weeks, but more often cholestatic hepatosis debuts after the 30th week of pregnancy. First of all, you need to pay attention to such a clinical manifestation as pruritus, which can be either a mild degree of intensity or a pronounced and severe intensity. Moreover, skin itching is much ahead of the development of jaundice, sometimes jaundice may not develop. We recommend focusing on the fact that cholestatic hepatosis of pregnant women is not characterized by an increase in the liver and spleen, various types of intoxication are not characteristic, and there are no dyspeptic syndrome and pain syndrome, and the general condition of the woman does not suffer. This imbalance, when there are pronounced manifestations, for example, skin itching, and at the same time the woman feels good, this is just one of the clinical manifestations of intrahepatic cholestasis of pregnant women. However, ICP must be differentiated from other forms of possible cholestatic reaction and development, including jaundice, primarily with the cholestatic form of acute viral hepatitis, with drug-induced hepatitis and various forms of chronic liver diseases.
This imbalance, when there are pronounced manifestations, for example, skin itching, and at the same time the woman feels good, this is just one of the clinical manifestations of intrahepatic cholestasis of pregnant women. However, ICP must be differentiated from other forms of possible cholestatic reaction and development, including jaundice, primarily with the cholestatic form of acute viral hepatitis, with drug-induced hepatitis and various forms of chronic liver diseases.
Differential diagnosis today, both on an outpatient basis and in a hospital, is mainly differentiated from viral hepatitis in pregnant women; with such a severe complication of pregnancy as acute fatty hepatosis of pregnant women, where an emergency permit is required; as well as with severe forms of preeclampsia, such as HELLP-syndrome. In general, I would like to emphasize that in the differential diagnosis for cholestatic hepatosis, unlike others, it is characteristic that the increase in the same enzymes is not too high.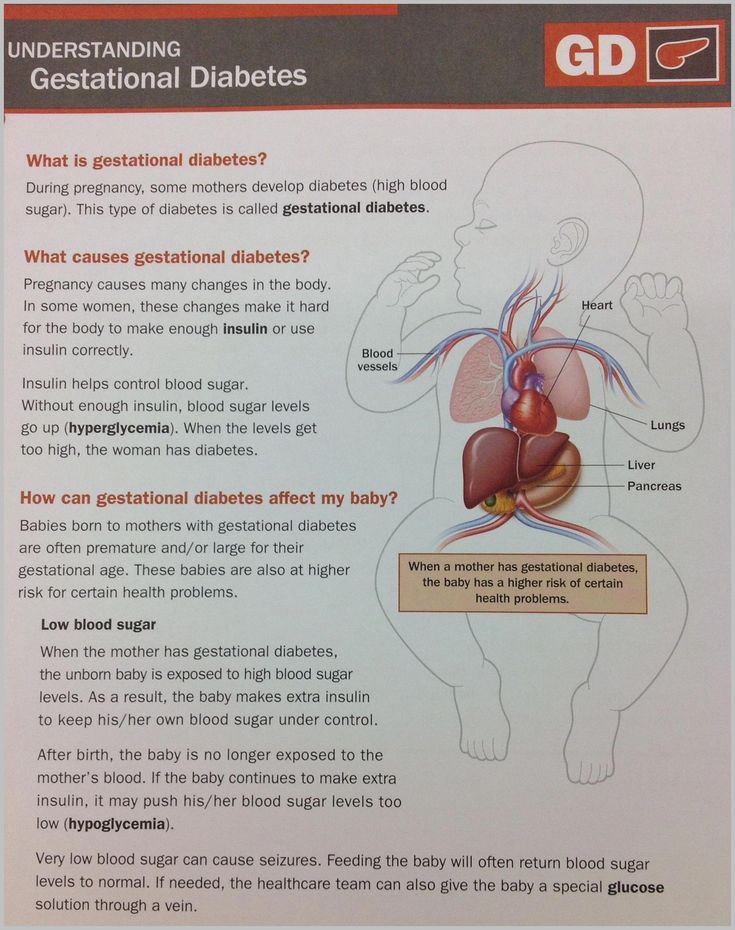 Yes, they rise, but not as high as, for example, with viral hepatitis. And also the differences are that changes in blood coagulability are more typical for other forms, first of all, for fatty hepatosis than for cholestatic hepatosis, and for cholestasis of pregnant women it prevails more towards the clinic of skin itching.
Yes, they rise, but not as high as, for example, with viral hepatitis. And also the differences are that changes in blood coagulability are more typical for other forms, first of all, for fatty hepatosis than for cholestatic hepatosis, and for cholestasis of pregnant women it prevails more towards the clinic of skin itching.
With the development of cholestasis in pregnant women after delivery, laboratory parameters usually normalize during the first day, sometimes during the first week, depending on the course of this disease. If cholestasis of pregnant women develops much earlier during pregnancy, then there is usually a tendency to worsen in the direction of some complications, primarily premature birth, as well as the possibility of a complication that is dangerous for us, obstetrician-gynecologists - this is bleeding during childbirth, mainly due to vitamin K deficiency. Therefore, such patients should be very carefully examined and evaluated from the point of view of both pregnancy management and childbirth, assessing the risk factors that are currently available, including not only anamnestic ones - multiple pregnancy can also give a complication in the form of cholestasis of pregnancy.
In terms of diagnosis, intrahepatic cholestasis allows us to make a diagnosis based on the concentration of serum bile acids. This is the most optimal marker for cholestasis of pregnancy, on the basis of which it is possible to make a diagnosis of intrahepatic cholestasis and then decide on the further management of such a patient. Also, markers of intrahepatic cholestasis include an increase in alkaline phosphatase, which is one of the markers of cholestasis; increase in gamma-glutamyltransferase; possible changes in alpha, beta globulins, increased bilirubin, triglycerides, and possibly a slight decrease in albumin; gamma-glutamyl transpeptidase may even remain within the normal range. In this regard, in our opinion, only a comprehensive laboratory examination allows us to clearly make this diagnosis. As for the increase in the activity of ALT, AST enzymes, there may be an increase from insignificant to significant. But with a significant increase in enzymes (more than 10 times the norm), it is necessary first of all to differentiate with acute viral hepatitis.
As I have already said, with a long course of cholestasis in pregnant women, a decrease in the content of vitamin K is possible, which directly correlates with a decrease in the concentration of prothrombin, which can cause or sometimes causes severe obstetric complications in the form of obstetric bleeding. Therefore, in the plan and tactics of managing such patients, a forecast must be made for possible complications not only in pregnancy, but also during childbirth, in particular, the development of postpartum hemorrhage; or certain steps must be taken to prevent bleeding during labor and the postpartum period.
As for additional methods of examination, in particular ultrasound examination of the liver and biliary tract, it is not possible to make this diagnosis due to the absence of any specific changes in ultrasound examination.
Treatment of intrahepatic cholestasis. Of course, the goal of treatment is, first of all, the relief of symptoms of cholestasis in pregnancy, the disappearance and relief of symptoms of a threatened abortion, and the improvement of uteroplacental blood flow. These are the main points for treatment, and due to the fact that cholestasis of pregnancy, which occurs during pregnancy, is due to pregnancy, it is not always possible to achieve the complete disappearance of possible symptoms. But to stop these symptoms as much as possible and, most importantly, to prolong pregnancy until the normal term of delivery is our main task.
These are the main points for treatment, and due to the fact that cholestasis of pregnancy, which occurs during pregnancy, is due to pregnancy, it is not always possible to achieve the complete disappearance of possible symptoms. But to stop these symptoms as much as possible and, most importantly, to prolong pregnancy until the normal term of delivery is our main task.
Methods of treatment. Of the non-drug methods of treatment, it is possible to use various efferent methods of treatment that allow the elimination of some compounds, but today the main methods of drug treatment are hepatoprotectors, choleretics, and antioxidants.
Evaluation of the effectiveness of treatment. First of all, it is the disappearance of pruritus or its intensity, or improvement in terms of reducing the intensity of pruritus as a clinical symptom, on the basis of which we can determine the effectiveness of the treatment. Secondly, this is a decrease in biochemical parameters: a decrease in the level of primary bile acids and the activity of alkaline phosphatase, gamma-glutamyl transferase, liver enzymes and bilirubin. Third: the disappearance of symptoms of the threat of abortion and its prolongation, as well as a decrease in the frequency of both miscarriage, a decrease in the frequency of premature birth and the birth of healthy children without any perinatal diseases and complications.
Third: the disappearance of symptoms of the threat of abortion and its prolongation, as well as a decrease in the frequency of both miscarriage, a decrease in the frequency of premature birth and the birth of healthy children without any perinatal diseases and complications.
To date, there is a widespread therapy using ursodeoxycholic acid, in particular the drug Ursosan, for the use of effective therapy for cholestasis, and in particular cholestasis of pregnancy. We have been using this drug in our clinic for a long time in pregnant women, it showed quite good results. This drug can be used specifically in pregnant women, it is not a contraindication for pregnancy, which, along with the limited use of drugs, in particular hepatoprotectors, allows us to deal with intrahepatic cholestasis of pregnant women. When using this drug for a certain time, both clinical symptoms decrease in terms of the development of skin itching, the disappearance of manifestations of skin itching, and the level of bile acids in the blood decreases.
The advantage of ursodeoxycholic acid preparations is still the possibility of use during pregnancy due to the low development of side effects and the absence of any lesions for the fetus. These drugs are in FDA category B, which shows a low risk of drug exposure to the development of fetal pathologies. Based on numerous experiences of clinics around the world, and in particular our clinic, ursodeoxycholic acid preparations (Ursosan, in particular) reduce skin itching, normalize biochemical parameters, which is very important for prolonging the pregnancy of such women and giving birth to children at a normal gestational age, as well as the possibility of adding drugs to the combination, including to improve the condition of the utero-placental complex.
The use of Ursosan in the third trimester of pregnancy did not cause any side effects based on our numerous experience, and also did not complicate the already difficult course of pregnancy in this patient, but only improved the additional prolongation of pregnancy and gave birth to full-term and healthy children more often.
In general, I would like to say that ursodeoxycholic acid preparations are currently optimal for the treatment of intrahepatic cholestasis. Also, in cases of severe cholestasis in pregnancy, even a long course of cholestasis in pregnancy, it is recommended to prevent complications from the administration of vitamin K a few days before delivery in order to reduce the risk of bleeding during childbirth and the postpartum period. It is also mandatory to treat feto-placental insufficiency during pregnancy with the inclusion of various drug complexes, including infusion therapy, on the basis of which there will be both a prolongation of pregnancy and a decrease in the frequency of perinatal complications. Given the fact that we switched to a new live birth criterion from 22 weeks, we should try to give birth to healthy children even at short terms.
In general, I would like to say that the prognosis for cholestatic hepatosis of pregnant women is favorable. This pathology completely disappears after childbirth, however, the risk of possible complications in the form of premature birth and bleeding, the doctor must remember when such a woman arrives or such a patient needs to be observed or treated and further carried out during pregnancy and childbirth.