Using tens unit while pregnant
TENS (Transcutaneous electrical nerve stimulation)
TENS (Transcutaneous electrical nerve stimulation) | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Key facts
- Transcutaneous electrical nerve stimulation, or TENS, is a form of pain relief without medicine that can be used during labour.
- It is not clear how TENS works to reduce pain. It is thought to reduce pain by stimulating different nerves in the spinal cord, blocking pain signals.
- There is not a lot of evidence that TENS works to reduce pain, but some people find it helpful.
- Most people can safely use TENS, but it’s a good idea to discuss it with your doctor or midwife before your labour begins.
- If you want to use TENS for pain relief during labour, ask your doctor, midwife or hospital in advance about where you can borrow or rent a machine.
What is TENS?
Transcutaneous electrical nerve stimulation, or TENS, is a form of pain relief without medicine. It can be used in labour to help with the pain.
Two electrodes are stuck to your skin and connected to a battery-powered machine. The machine delivers small pulses of electrical current to the body. You can adjust the amount of electricity delivered to your body. The pulses feel like tingling sensations on your skin.
How can I use TENS to relieve pain?
It is not clear how TENS works to relieve pain.
It's possible that it blocks pain signals by stimulating different nerves in your spinal cord. It might also cause the release of endorphins, the body's natural pain relievers.
There is not a lot of evidence to show that TENS works to reduce pain, but some people find it helpful.
What are the advantages of TENS in labour?
The advantages of TENS are that:
- it doesn't require medicines or injections
- it may give you some control over pain relief
- you are able to move around
- you can use other methods if TENS does not give you enough pain relief
- there is no harm to you or your baby
- it can be used at home during early labour
What are the disadvantages of TENS in labour?
TENS doesn’t work for everybody. It can be uncomfortable but shouldn’t be painful. You may experience skin irritation where the electrodes are stuck on. TENS can’t be used in the bath or shower.
It can be uncomfortable but shouldn’t be painful. You may experience skin irritation where the electrodes are stuck on. TENS can’t be used in the bath or shower.
When should I not use TENS?
TENS is thought to be very safe, but it shouldn't be used:
- if you are pregnant but not in labour
- before 37 weeks gestation
- by people who have a pacemaker
- by some people with epilepsy
Where can I get a TENS machine?
Not all hospitals and birthing centres have TENS machines. If you’re interested in using one, it's best to discuss it with your doctor or midwife before you go into labour. You may wish to ask about whether it is safe for you to use a TENS machine, where you can get one and about any costs involved.
You can find more information about other methods of pain relief during labour here.
Sources:
Cochrane Library (Transcutaneous electrical nerve stimulation (TENS) for pain management in labour), King Edward Memorial Hospital Obstetrics & Gynaecology (Clinical practice guideline, Pain management), SA Health (TENS in labour), Royal Women's Hospital (Managing pain in labour)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Related pages
- Epidural
- Gas (Entonox)
- Non-medical pain relief during labour
- Pain relief during labour
- Making a birth plan
- Giving birth - stages of labour
Need more information?
Pain relief during labour
Learn what options are available to you to relieve pain during labour pain, and how your birth support partner can help you.
Read more on Pregnancy, Birth & Baby website
Non-medical pain relief during labour
There are many ways to relieve labour pain without medicines. Each method has advantages and disadvantages. Learn about the different options to help choose one or more that suit you.
Learn about the different options to help choose one or more that suit you.
Read more on Pregnancy, Birth & Baby website
Pain Relief in Labour and Childbirth
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Childbirth - pain relief options - Better Health Channel
Understanding your pain relief options can help you cope better with the pain of childbirth.
Read more on Better Health Channel website
Pain during childbirth | HealthEngine Blog
Almost all women experience pain during childbirth which varies in severity. There are different pharmacological and non-pharmacological approaches to treatment of pain during childbirth.
Read more on HealthEngine website
Glossary of pregnancy and labour
Glossary of common terms and abbreviations used in pregnancy and labour.
Read more on Pregnancy, Birth & Baby website
Assisted Birth
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Going to hospital or birthing centre
Whether you're planning to have your baby at home, in hospital or at a midwifery-led birth centre, you should get a few things ready at least two weeks before your due date.
Read more on Pregnancy, Birth & Baby website
Having a baby in hospital
Both public and private hospitals provide high-quality care for you and your baby. They both have advantages and disadvantages – find out more here.
They both have advantages and disadvantages – find out more here.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Using a TENS Machine for Labor Pain: Is It For You?
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Reducing pain during labor is a top priority for most moms-to-be. But given the limited options for managing pain, some pregnant people seek a more natural approach that doesn’t involve the use of medications.
And that’s why some parents-to-be are curious about the safety and effectiveness of a transcutaneous electrical nerve stimulation (TENS) unit.
A TENS machine or unit is a small device, often battery operated, that is used to manage both acute and chronic pain.
The unit has wires connected to electrodes that are placed on the skin. The electrodes deliver low voltage electrical currents to targeted body parts to control pain signals in the body.
A practitioner familiar with TENS therapy places the electrodes at or near the nerves where the pain is located. These electrical currents or impulses can create short-term or long-term relief from pain.
Experts say TENS therapy works in a couple of different ways. The first belief is that the electrical impulses affect the nervous system reducing its ability to transmit pain signals to the spinal cord and brain. But they also say that electrical impulses can stimulate the body to produce endorphins, a neurotransmitter that can help relieve pain.
“TENS unit use has been known to alleviate period, joint, back, endometriosis, arthritis, fibromyalgia, sports injuries, and postoperative pain,” says Sherry Ross, MD, OB-GYN and women’s health expert at Providence Saint John’s Health Center.
It’s essential that you do your homework when choosing a TENS unit. Ross recommends looking for one that has a reliable and good track record with a strong output intensity and with sufficient electrical impulses.
“The higher the numbers, the more helpful it will be to alleviate the pain,” Ross says.
Ideally, Ross says you’ll want to buy a pharmaceutical-grade TENS unit, going with a reputable brand. You can buy a TENS unit online through Amazon, at a CVS or Walgreens pharmacy, or through an online retailer that sells medical supplies and devices.
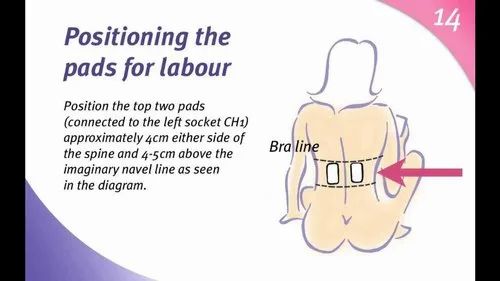
According to a review of the evidence, when using a TENS machine for labor pains, the electrodes are typically placed on your lower back, on specific acupuncture points, or on your head.
If you’re operating the unit yourself, you’ll regulate the intensity of the impulses during painful contractions. Most TENS units are small and battery operated, so you should be able to hold it in your hand or clip it to your clothing during contractions.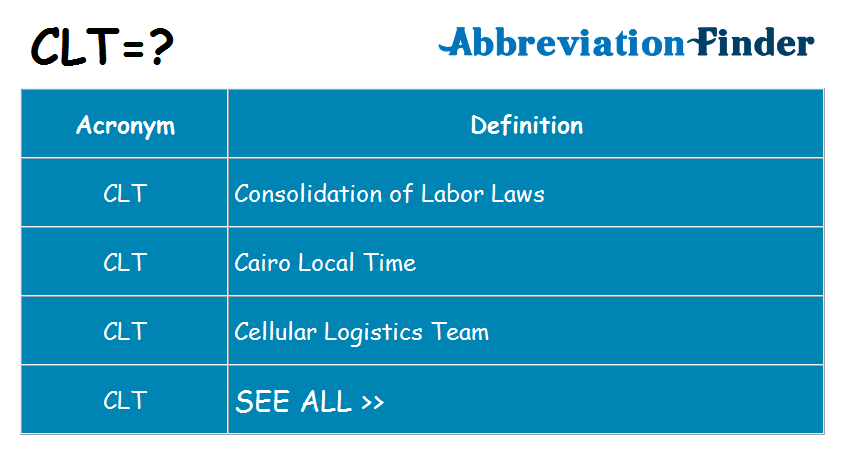
But if you’re not familiar with a TENS machine, it’s a good idea to consult with a physical therapist, midwife, or doctor who regularly uses this therapy. They’ll be able to show you how to place the electrodes on the skin as well as how to operate the machine to get the best results.
You can also hire a doula or midwife familiar with this method to operate the machine during labor. They’ll be able to place the electrodes and control the frequency of the currents coming from the TENS unit.
One of the main reasons parents-to-be consider a TENS machine is because it’s a drug-free alternative for pain management during labor.
According to Ross, the TENS unit’s ability to reduce pain sensation may be helpful in alleviating mild pain during labor. Some evidence points to the control it allows women to feel, which consequently reduces pain. It also provides a distraction from the contractions.
TENS therapy may also help reduce the dreaded low back pain that seems to strike so many women during the third trimester.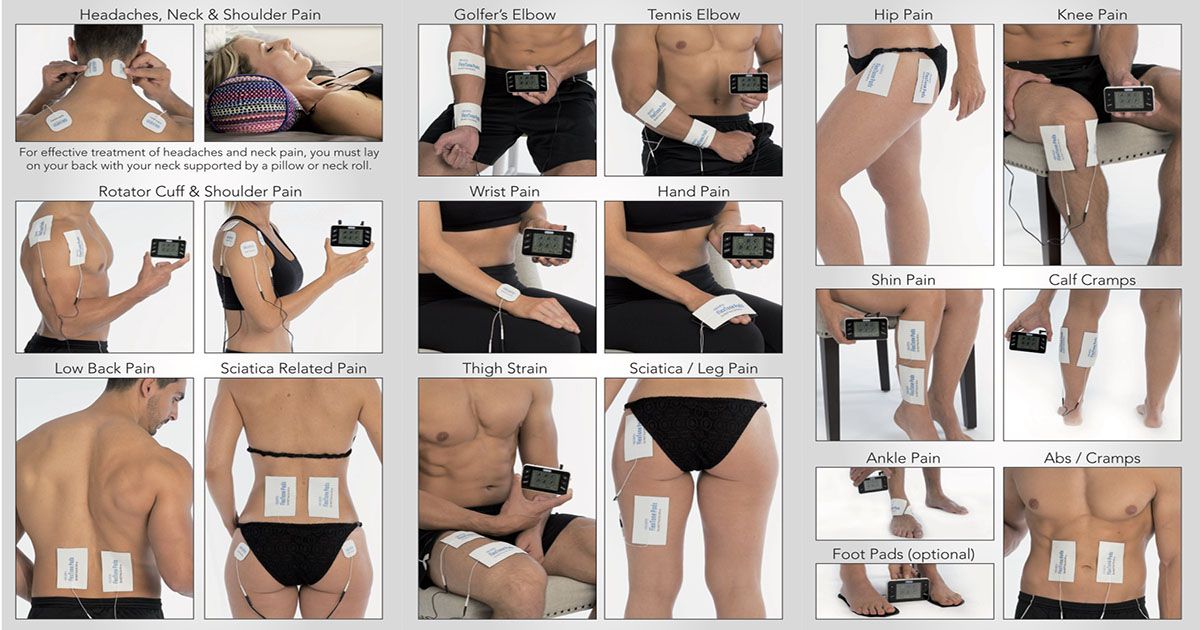
One 2012 study looked at the effectiveness of TENS in reducing low back pain during this period. Researchers divided 79 subjects into four groups: a control group and three treatment groups — one using acetaminophen, one using exercise, and the final group using TENS for pain management.
During the study period, researchers found that 57 percent of the control group experienced an increase in low back pain, while the TENS application reduced low back pain more effectively than exercise and acetaminophen.
In general, TENS therapy is considered mostly safe. That said, research involving the use of a TENS until during labor is minimal, at best.
Ross says some of the things you may notice when using the TENS unit in labor include:
- muscle twitching
- tingling
- buzzing sensation
- allergic reaction
- irritation and skin redness from the adhesive pads on the skin
- burn marks as a side effect from the electrode pads
- lower blood pressure
- muscle spasms
TENS units are used to manage pain for a variety of conditions, including painful contractions during labor. But if this is your first time receiving treatment from a TENS machine, and you plan on using it for labor pains, Ross says to proceed with caution.
But if this is your first time receiving treatment from a TENS machine, and you plan on using it for labor pains, Ross says to proceed with caution.
“Women who have never used the TENS unit for other pain conditions should not use it during labor for the first time,” says Ross. However, she does say the TENS unit may be useful for pain relief for women in labor if they have had success in the past using it for other painful symptoms — just don’t use it in conjunction with water immersion.
For all women, Ross says that since there are inconsistent results for women using the TENS unit, it should not be the only relied upon method for labor pains.
In other words, you may need to use other forms of pain management in combination with a TENS unit. Techniques like massage, relaxation, and breath exercises are all proven ways to help moms-to-be move through labor and childbirth with less pain.
Using a TENS unit during labor may help to manage pain. The effectiveness of the currents depends on the placement of the pads and the frequency of the currents coming from the machine.
There is minimal research regarding the effectiveness of TENS during childbirth. That’s why it’s essential that you consult with your doctor and other healthcare professionals familiar with this protocol. They can help you decide if using a TENS machine during labor is right for you.
the effect of hypovitaminosis on the intelligence of a child
Vitamin D plays a special role in a woman's fertility. The influence of vitamin D on the regulation of the menstrual cycle, namely its participation in the maturation of follicles, ovulation and the formation of the corpus luteum 1 was shown. Therefore, maintaining normal levels of Vitamin D is important at all stages: preparation for pregnancy, pregnancy and lactation.
Vitamin D in pregnancy
During pregnancy, vitamin D deficiency is associated with the risk of developing preeclampsia (preeclampsia is defined as a multisystem pathological condition that occurs after the 20th week of pregnancy, characterized by arterial hypertension in combination with proteinuria (0. 3 g / l in daily urine), often, edema, and manifestations of multiple organ failure), diabetes mellitus in pregnancy, premature birth, the birth of small children, as well as the development of skeletal disorders in them due to rickets. Vitamin D deficiency is associated with an increased risk of cardiovascular disease, diabetes, cancer 2
3 g / l in daily urine), often, edema, and manifestations of multiple organ failure), diabetes mellitus in pregnancy, premature birth, the birth of small children, as well as the development of skeletal disorders in them due to rickets. Vitamin D deficiency is associated with an increased risk of cardiovascular disease, diabetes, cancer 2
Vitamin D during breastfeeding
During lactation, the mother loses vitamin D and other substances in breast milk, taking even small doses of vitamin D before and after childbirth can have a beneficial effect on the provision of vitamin D to mother and baby 3 .
How much vitamin D should pregnant women take?
Since Russia belongs to an endemic region for vitamin D deficiency, it is advisable for all women preparing to conceive to receive vitamin D in prophylactic doses. In order to prevent vitamin D deficiency, women aged 18-50 years are recommended to take at least 600-800 IU of vitamin D per day, when pregnancy occurs, the dose is increased to 800-1200 IU / day 2 . The decision on the need to take vitamin D and its dosing regimen is made by a specialist based on clinical examination data and laboratory diagnostics. Hypovitaminosis D requires mandatory correction 2 .
The decision on the need to take vitamin D and its dosing regimen is made by a specialist based on clinical examination data and laboratory diagnostics. Hypovitaminosis D requires mandatory correction 2 .
What foods contain vitamin D?
Dietary sources of vitamin D are fatty fish, liver, egg yolk, some cereals, vitamin D is also synthesized in the body when the skin is exposed to ultraviolet sunlight. For the synthesis of vitamin D in physiological quantities, it is necessary to expose the extremities to sunlight (from 10.00 am to 15.00 pm) at least 2 times a week, according to the recommendations of the US National Institutes of Health 2 .
Insufficient intake of vitamin D from food can be compensated by the intake of the vitamin as part of dietary supplements or vitamin-mineral complexes. 4
References:
- Yazykova OI, Khilkevich EG Pregnancy planning. Vitamin D deficiency – infertility, correction of vitamin D deficiency // Medical Council.
 – 2017. – no. 2.
– 2017. – no. 2. - Pregravid preparation: clinical protocol / [ed.-dev. V.E. Radzinsky and others]. - M .: Editorial staff of the Status Praesens magazine, 2016. - 80 from
- McDermott C.M., Beitz D.C., Littledike E.T., Horst R.L. Effects of dietary vitamin D3 on concentrations of vitamin D and its metabolites in blood plasma and milk of dairy cows. J Dairy Sci. 1985; 68:1959–67
- National program "Vitamin D deficiency in children and adolescents of the Russian Federation: modern approaches to correction", 2018
Arterial hypertension in pregnancy | Shchelkovsky Perinatal Center
Arterial hypertension during pregnancy
Rise in blood pressure during pregnancy. What is preeclampsia?
Pre-eclampsia is one of the most common complications of pregnancy, affecting both the mother and the unborn child. This condition occurs in 5-8% of pregnant women, is diagnosed based on the rise in blood pressure (BP) and the appearance of protein in the urine. That is why at every prenatal visit to the doctor in a pregnant woman, blood pressure is measured and urine is evaluated for the presence of protein. nine0005
That is why at every prenatal visit to the doctor in a pregnant woman, blood pressure is measured and urine is evaluated for the presence of protein. nine0005
In most cases, preeclampsia is relatively mild, occurs closer to full-term pregnancy, and ends with favorable outcomes. At the same time, some cases of preeclampsia progress or develop rapidly and can be extremely dangerous for a woman and her child.
What is "toxemia"?
During visits to the doctor or in the literature, you may come across other terms that define the rise in blood pressure during pregnancy: toxemia, preeclampsia, OPG-preeclampsia (edema, proteinuria, hypertension). However, the definition of "preeclampsia" is now accepted. nine0005
How is preeclampsia related to eclampsia or HELLP syndrome?
Eclampsia and HELLP syndrome are clinical variants of preeclampsia. The hallmark of eclampsia is seizures, which usually occur as a late complication of severe preeclampsia.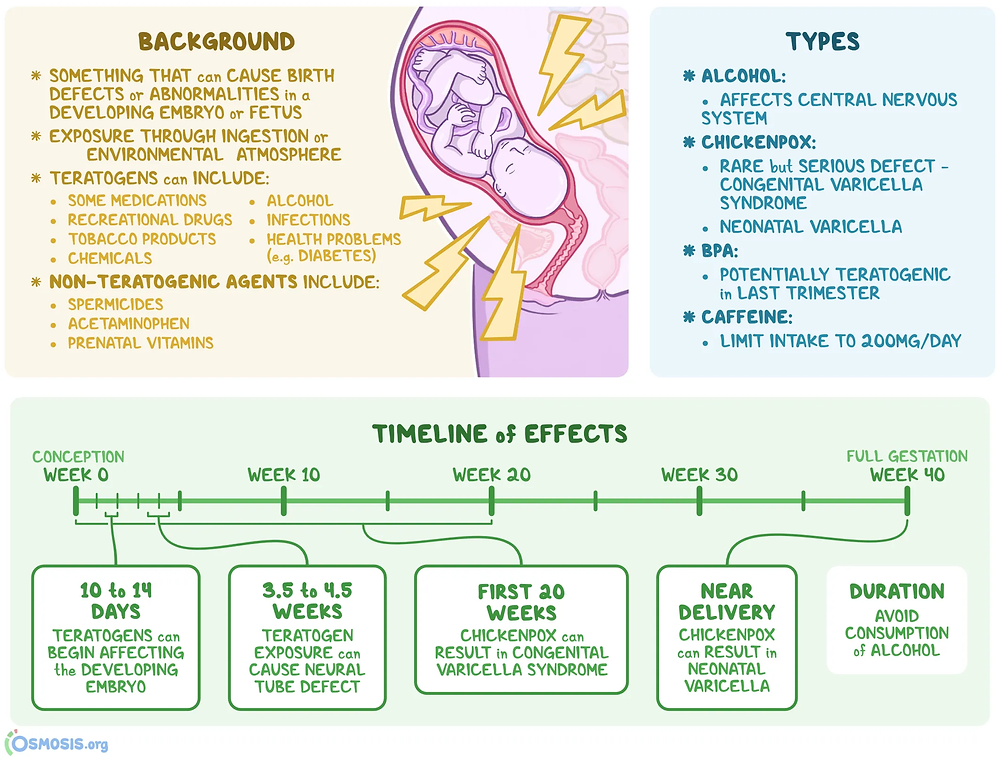 However, seizures can also develop without any previous signs of severe illness.
However, seizures can also develop without any previous signs of severe illness.
HELLP syndrome is one of the most severe forms of preeclampsia and occurs in approximately 15% of patients with preeclampsia. This condition is sometimes confused with a cold or gallbladder problems. HELLP syndrome can lead to significant liver damage in the mother, the breakdown of red blood cells (erythrocytes), and a decrease in platelets. nine0005
What are the causes of preeclampsia? Can it be prevented?
The causes of preeclampsia are not fully understood, so there is currently no reliable way to prevent this condition. Many theories have been proposed that describe various strategies for the prevention of preeclampsia, but none of them is completely successful.
The use of aspirin, calcium, and other therapeutic agents is beneficial in some situations, but studies do not support their widespread use. At the same time, there is a widespread belief that the placenta plays a key role in the development of preeclampsia, and that women with chronic hypertension and other risk factors are predisposed to developing preeclampsia. It is important to know the alarming symptoms, trust your feelings, visit the doctor regularly and strictly follow his recommendations. nine0005
It is important to know the alarming symptoms, trust your feelings, visit the doctor regularly and strictly follow his recommendations. nine0005
When does preeclampsia develop?
In most cases, preeclampsia develops after 20 weeks of pregnancy and usually stops with the birth of the baby. Sometimes preeclampsia continues for up to 6 weeks after delivery. Therefore, you should carefully monitor the symptoms even after childbirth.
Preeclampsia may progress slowly. But sometimes it comes suddenly. This usually happens in cases where a woman does not attach due importance to the manifestations and symptoms of the disease, as a result of which they remain unrecognized for a long time. nine0005
Signs and symptoms of pre-eclampsia:
- High blood pressure. 140/90 mm. rt. Art. and higher. An increase in blood pressure during pregnancy that is 30 or more units above your baseline is a cause for concern and requires medical attention.
- Protein in urine. 0.3 g in a 24 hour sample or mark 1+ on a paper test strip.
- Swelling of hands, feet or face. Particularly around the eyes if thumb marks remain or if these symptoms come on suddenly. nine0040
- Headache, which does not go away even after taking medication for it.
- Visual disturbances. Double vision, glow, "flickering flies", aura (a special condition preceding an attack).
- Nausea or pain in the upper abdomen (epigastrium). Sometimes confused with indigestion, gallbladder pain, or the flu, however, nausea in the second half of pregnancy is not a normal condition. nine0040
- Sudden weight gain, more than 500 g per week.
Risk factors
Personal history
- First pregnancy
- Pre-eclampsia during a previous pregnancy
- Age over 40 or under 18
- High blood pressure before pregnancy
- Diabetes before or during pregnancy
- Multiple pregnancy
- Obesity
- Systemic lupus erythematosus or other autoimmune diseases
- Polycystic ovary syndrome
- Long interval between pregnancies
- Pregnancy after IVF
- Sickle cell anemia
Family history
- Maternal or paternal preeclampsia in the family
- High blood pressure or heart disease
- Diabetes
Risk factors for premature babies include lung immaturity and many other potential problems. In severe cases, preeclampsia can cause fetal death.
In severe cases, preeclampsia can cause fetal death.
What is the treatment for preeclampsia?
Professionals need to consider many factors when deciding how to manage preeclampsia and when to deliver, including the condition of the baby, the condition and age of the mother, and the exact course of the disease. These include monitoring blood pressure, evaluating the results of laboratory tests that characterize the condition of the mother's kidneys, liver, or the ability of her blood to clot. Other tests monitor how the fetus grows and whether it is endangered while in the womb. Therapeutic agents include magnesium sulfate to prevent seizures, as well as medications to lower blood pressure. Sometimes a wait-and-see approach is used, both with and without medication. When the health of the mother or child is in serious danger, the only acceptable treatment for preeclampsia at any stage of pregnancy is delivery. nine0005
Can medicines harm me or my baby?
Blood pressure medication rarely causes any side effects for the mother. And if the doctor prescribed them for you, then this means that your pressure is high enough, and that the risk for you or your child from raising the pressure is much higher than from taking medication. Magnesium sulfate is generally safe for the baby, but can cause hot flashes, sweating, thirst, visual disturbances, drowsiness, mild confusion, muscle weakness, and shortness of breath in the mother. These side effects should completely disappear when the administration of the drug ends. nine0005
And if the doctor prescribed them for you, then this means that your pressure is high enough, and that the risk for you or your child from raising the pressure is much higher than from taking medication. Magnesium sulfate is generally safe for the baby, but can cause hot flashes, sweating, thirst, visual disturbances, drowsiness, mild confusion, muscle weakness, and shortness of breath in the mother. These side effects should completely disappear when the administration of the drug ends. nine0005
Can I stay at home?
Sometimes women with mild preeclampsia stay at home. In this case, more frequent visits to a specialist, monitoring of blood pressure and urine tests are necessary in order to timely identify signs of a progressive condition and prevent the adverse effects of preeclampsia on your health and the health of your child. The well-being of the child should be assessed by monitoring the nature of changes in heart rate, fetal growth and weight, blood flow in the vessels using ultrasound.