Trouble pooping while pregnant
Causes, treatments, and home remedies
Constipation is a very common symptom that many women experience during pregnancy.
Some women have constipation at an early stage of their pregnancy, while it does not affect other women until much later on.
In this article, we explain why constipation is common in pregnancy and discuss safe treatments and home remedies that women can use to relieve the discomfort.
The cause of constipation during pregnancy depends on the stage at which it occurs. Possible causes include:
- Hormones: Changing hormone levels in early pregnancy cause the intestines to slow down the movement of stool through the bowel. This delay increases the amount of water that the colon absorbs from the stool, which makes it more solid and difficult to pass.
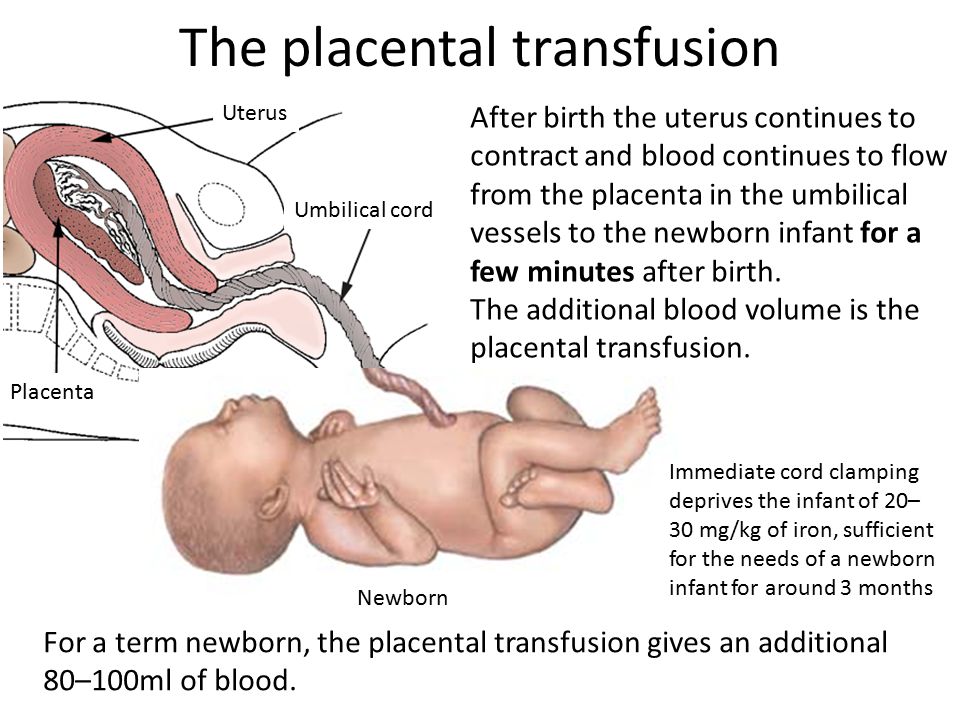
- Prenatal vitamins: Prenatal vitamins are chock-full of iron, a crucial mineral that can sometimes be deficient during pregnancy. Iron can cause constipation and hard, black stools.
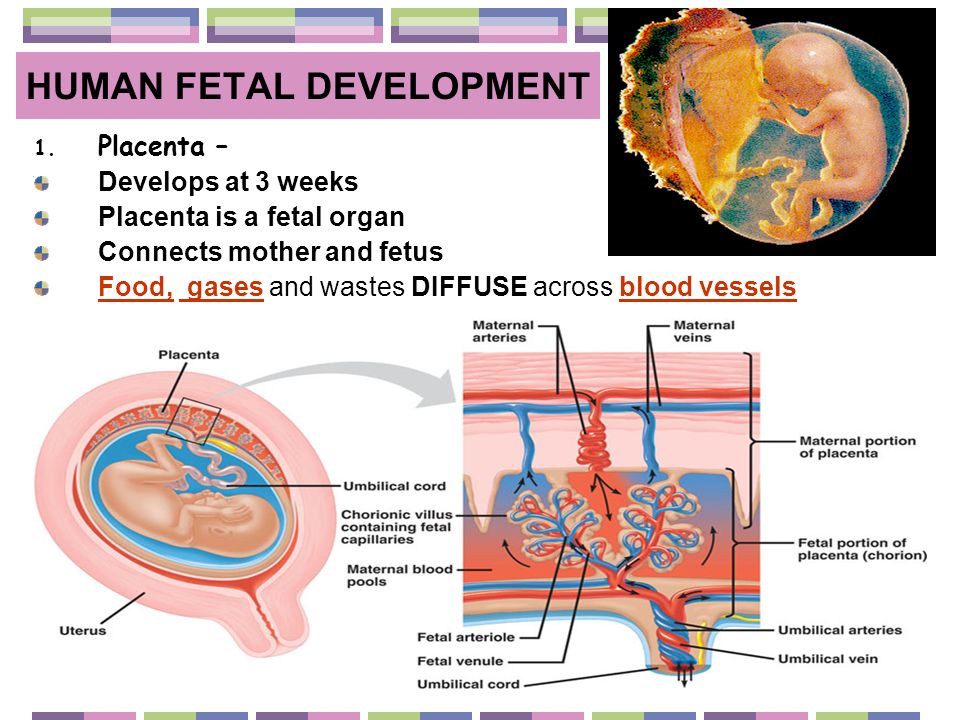
- Pressure from the uterus: In later pregnancy, the growing uterus can put pressure on the bowel, making it harder to move stool through the intestines.
In addition to infrequent bowel movements, constipation can cause bloating, stomach discomfort, and hard, dry stools that are painful to pass. It can also result in a feeling that not all the stool has passed.
Constipation can be particularly uncomfortable during pregnancy.
During pregnancy, women can often relieve constipation using gentle, safe home remedies:
- Fiber: Taking fiber supplements or eating more fibrous foods, such as fruits, vegetables, and whole grains, can increase the number of stools and facilitate their passage through the intestines. Adults should eat between 28 and 34 grams of fiber each day.
- Fluid: Drinking enough water is important to keep stool soft and easy to pass. If a person feels that water is not helping, they can try adding clear soups, teas, and naturally sweetened fruit or vegetable juices to their diet.

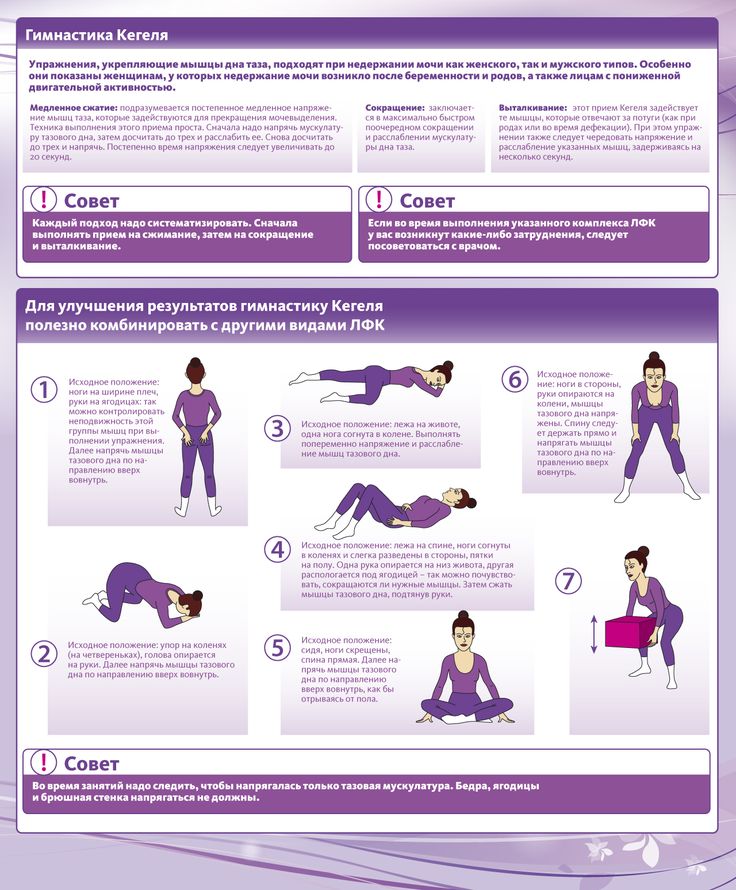
- Activity: Being active helps stool move through the intestines. Getting regular exercise, with a doctor’s approval, can help relieve constipation. If exercising is not a priority or possibility, try to fit in a gentle walk each day.
- Probiotics: Millions of healthy bacteria live in the gut and help it function correctly. Probiotics may help repopulate the gut bacteria with healthy strains that encourage normal and regular bowel movements. Foods high in probiotics include yogurt, sauerkraut, and kimchi.
If the home remedies above do not work, it may be time to discuss other options with a doctor.
For women taking prenatal vitamins that are high in iron, doctors may recommend trying a vitamin that contains less iron.
The primary medical treatment for constipation in pregnancy is a medication called a laxative, which makes it easier and more comfortable to go to the bathroom.
It is generally safe to use gentle laxatives, but it is best to avoid stimulant laxatives because they can induce uterine contractions.
Although many laxatives are available over the counter, it is important to check with a doctor which one is safe to use. Limited information is available about using some of these medications during pregnancy.
Women can usually safely use the following types of laxative during pregnancy:
Bulk-forming agents
Bulk-forming agents mimic fiber by adding material to the stool and helping it absorb more water. By doing this, they make the stool larger, softer, and easier to pass.
These types of laxative can cause some cramping or discomfort, so people should start with the lowest dosage and ensure that they drink lots of water.
Examples of bulk-forming agents include psyllium, methylcellulose, and polycarbophil.
Stool softeners
Stool softeners add water to the stool to help make it softer and more comfortable to pass.
The stool softener that doctors most commonly recommend to pregnant women is docusate (Colace).
Lubricant laxatives
Lubricant laxatives add a slippery coating to either the stool or the inside of the intestinal tract to aid the passage of stool out of the body.
Glycerin suppositories are one type of lubricant laxative. It is essential to always speak to a healthcare professional before using suppositories, especially when pregnant.
Osmotic laxatives
By drawing more water into the intestines, these laxatives help soften the stool. They also allow the bowel to contract more to move the stool along. These types of laxative can also cause cramping and bloating in the abdomen.
Examples of osmotic laxatives include polyethylene glycol and magnesium hydroxide.
In most cases, constipation in pregnancy is short-lived and resolves with no or minimal treatment. In rare cases, however, prolonged constipation can cause fecal impaction, which may need removal by a doctor.
Continued use of certain types of laxative can cause the bowel to “forget” how to push stool through the intestines.
These drugs can also cause electrolyte or fluid imbalances in some people. Such issues usually affect people who have other health problems, such as diabetes or kidney disease.
It is best to speak to a doctor about the types of laxative to take and how often to take them.
It is vital that pregnant women speak with their doctor before taking any medication, including laxatives or other constipation remedies.
Seeing a doctor is also advisable if any additional symptoms occur, including:
- nausea
- stomach pain
- vomiting
- constipation that lasts for longer than 1–2 weeks
- bleeding from the rectum
- no relief after using a laxative
As always, mention any other symptoms or concerns to the doctor for more specific information and advice.
Causes, treatments, and home remedies
Constipation is a very common symptom that many women experience during pregnancy.
Some women have constipation at an early stage of their pregnancy, while it does not affect other women until much later on.
In this article, we explain why constipation is common in pregnancy and discuss safe treatments and home remedies that women can use to relieve the discomfort.
The cause of constipation during pregnancy depends on the stage at which it occurs. Possible causes include:
- Hormones: Changing hormone levels in early pregnancy cause the intestines to slow down the movement of stool through the bowel. This delay increases the amount of water that the colon absorbs from the stool, which makes it more solid and difficult to pass.
- Prenatal vitamins: Prenatal vitamins are chock-full of iron, a crucial mineral that can sometimes be deficient during pregnancy. Iron can cause constipation and hard, black stools.
- Pressure from the uterus: In later pregnancy, the growing uterus can put pressure on the bowel, making it harder to move stool through the intestines.
In addition to infrequent bowel movements, constipation can cause bloating, stomach discomfort, and hard, dry stools that are painful to pass. It can also result in a feeling that not all the stool has passed.
Constipation can be particularly uncomfortable during pregnancy.
During pregnancy, women can often relieve constipation using gentle, safe home remedies:
- Fiber: Taking fiber supplements or eating more fibrous foods, such as fruits, vegetables, and whole grains, can increase the number of stools and facilitate their passage through the intestines. Adults should eat between 28 and 34 grams of fiber each day.
- Fluid: Drinking enough water is important to keep stool soft and easy to pass. If a person feels that water is not helping, they can try adding clear soups, teas, and naturally sweetened fruit or vegetable juices to their diet.
- Activity: Being active helps stool move through the intestines. Getting regular exercise, with a doctor’s approval, can help relieve constipation. If exercising is not a priority or possibility, try to fit in a gentle walk each day.
- Probiotics: Millions of healthy bacteria live in the gut and help it function correctly.
 Probiotics may help repopulate the gut bacteria with healthy strains that encourage normal and regular bowel movements. Foods high in probiotics include yogurt, sauerkraut, and kimchi.
Probiotics may help repopulate the gut bacteria with healthy strains that encourage normal and regular bowel movements. Foods high in probiotics include yogurt, sauerkraut, and kimchi.
If the home remedies above do not work, it may be time to discuss other options with a doctor.
For women taking prenatal vitamins that are high in iron, doctors may recommend trying a vitamin that contains less iron.
The primary medical treatment for constipation in pregnancy is a medication called a laxative, which makes it easier and more comfortable to go to the bathroom.
It is generally safe to use gentle laxatives, but it is best to avoid stimulant laxatives because they can induce uterine contractions.
Although many laxatives are available over the counter, it is important to check with a doctor which one is safe to use. Limited information is available about using some of these medications during pregnancy.
Women can usually safely use the following types of laxative during pregnancy:
Bulk-forming agents
Bulk-forming agents mimic fiber by adding material to the stool and helping it absorb more water. By doing this, they make the stool larger, softer, and easier to pass.
By doing this, they make the stool larger, softer, and easier to pass.
These types of laxative can cause some cramping or discomfort, so people should start with the lowest dosage and ensure that they drink lots of water.
Examples of bulk-forming agents include psyllium, methylcellulose, and polycarbophil.
Stool softeners
Stool softeners add water to the stool to help make it softer and more comfortable to pass.
The stool softener that doctors most commonly recommend to pregnant women is docusate (Colace).
Lubricant laxatives
Lubricant laxatives add a slippery coating to either the stool or the inside of the intestinal tract to aid the passage of stool out of the body.
Glycerin suppositories are one type of lubricant laxative. It is essential to always speak to a healthcare professional before using suppositories, especially when pregnant.
Osmotic laxatives
By drawing more water into the intestines, these laxatives help soften the stool. They also allow the bowel to contract more to move the stool along. These types of laxative can also cause cramping and bloating in the abdomen.
They also allow the bowel to contract more to move the stool along. These types of laxative can also cause cramping and bloating in the abdomen.
Examples of osmotic laxatives include polyethylene glycol and magnesium hydroxide.
In most cases, constipation in pregnancy is short-lived and resolves with no or minimal treatment. In rare cases, however, prolonged constipation can cause fecal impaction, which may need removal by a doctor.
Continued use of certain types of laxative can cause the bowel to “forget” how to push stool through the intestines.
These drugs can also cause electrolyte or fluid imbalances in some people. Such issues usually affect people who have other health problems, such as diabetes or kidney disease.
It is best to speak to a doctor about the types of laxative to take and how often to take them.
It is vital that pregnant women speak with their doctor before taking any medication, including laxatives or other constipation remedies.
Seeing a doctor is also advisable if any additional symptoms occur, including:
- nausea
- stomach pain
- vomiting
- constipation that lasts for longer than 1–2 weeks
- bleeding from the rectum
- no relief after using a laxative
As always, mention any other symptoms or concerns to the doctor for more specific information and advice.
Frequent urination during pregnancy - Juno
Article content
When is considered frequent
Urges are frequent if they occur more than 9 times a day. Usually only a small amount of urine is passed at a time. Pregnant women may have about 20 visits to the toilet per day, while the daily amount of urine can also increase to 2 liters.
Is it an early sign of pregnancy?
HCG slightly increases the volume of urine excreted, so frequent urination begins already in the first weeks of pregnancy. The symptom does not 100% indicate the onset of fertilization - it should be considered in conjunction with other manifestations - primarily with a positive test. nine0008
nine0008
However, keep in mind that with an increase in the daily volume of urine at a very early date, a false negative result is possible. Also, the symptom is less pronounced in ectopic pregnancy due to lower hCG levels, so an examination is required in any case.
If you began to frequent the toilet and there is a delay, then pregnancy is very likely.
Physiological causes of frequent urination in pregnant women
In healthy women, this phenomenon is associated with the body getting used to carrying a baby, as well as with other physiological reasons. nine0008
In the first half of pregnancy
The main causes of frequent urination during early pregnancy:
- Increased progesterone production. This hormone relaxes muscle tissue, helping to maintain pregnancy. As a result, urine is retained worse, the urge to void becomes more frequent due to the reduced tone of the bladder.
- Increased blood supply in the pelvis.
 Due to the proximity of the bladder to the uterus, its increased sensitivity occurs - filling receptors react more strongly. nine0027
Due to the proximity of the bladder to the uterus, its increased sensitivity occurs - filling receptors react more strongly. nine0027 - Active work of the kidneys. During the bearing of a child, the renal blood flow increases 1.5 times for the constant renewal of amniotic fluid and the timely removal of metabolic products. Accordingly, more urine begins to be produced.
Physiological increase in urination does not cause pain and discomfort, itching and burning. In the presence of negative symptoms, you need to consult a doctor to rule out pathologies.
Second half of pregnancy
The main reason for frequent urge to urinate in the second and third trimester is the increased pressure of the uterus on the bladder. However, diseases can also be the cause:
- Infections. Changes in the pelvis in pregnant women and a decrease in protective forces increase the risk of developing urethritis, cystitis, pyelonephritis. Such pathologies are accompanied not only by frequent urination, but also by pain, discomfort in the area of inflammation, and a burning sensation.
 The woman's health is deteriorating; nine0027
The woman's health is deteriorating; nine0027 - Gestational diabetes. An increase in blood glucose in violation of carbohydrate metabolism. The amount of urine separated increases significantly.
Other pathologies include neoplasms in the small pelvis, endocrine and neurological disorders.
Soreness with frequent urination in pregnant women - is it normal or not?
Painful urination is not normal. Unpleasant sensations indicate the development of a pathological process. Pain and discomfort are a sign of urinary tract irritation. Cystitis is very likely if a woman has severely reduced immunity or has chronic diseases of the pelvic organs. Sometimes it can be accompanied by a temperature and requires a mandatory visit to the doctor. nine0008
Calls at night
Pregnant women often complain about how tired they are at night "hiking". The situation is explained by the fact that the work of the kidneys depends on the position of the body. In the later stages, the female body is prone to fluid retention and edema, especially when in an upright position. When the expectant mother lies down, the renal blood flow and the outflow of fluid from the tissues increase. As a result, the kidneys excrete more urine.
In the later stages, the female body is prone to fluid retention and edema, especially when in an upright position. When the expectant mother lies down, the renal blood flow and the outflow of fluid from the tissues increase. As a result, the kidneys excrete more urine.
What is the duration of frequent urination during pregnancy? nine0003
The phenomenon begins already from the first days of pregnancy and is especially pronounced up to about 12 weeks. Later, the number of emptyings gradually decreases, because by 4-5 months the body adapts to new conditions. The diaphragm rises, creating more space for the growing uterus and "unloading" the pelvic organs.
Frequent urination during pregnancy in the second trimester may indicate the addition of an infection or the development of inflammation, but it is also possible as a manifestation of the individual characteristics of the body. You can find out more precisely this moment from your doctor, who is involved in pregnancy management. nine0008
nine0008
In the third trimester, the opposite phenomenon is possible - fluid retention. However, the closer the birth, the more often the urge to urinate becomes. In the last month of gestation, the uterus descends and puts pressure on the organs of the urinary system.
How likely is miscarriage in the absence of frequent urination?
A woman does not always immediately find out about a missed pregnancy. Fetal movements are not felt in the early stages, so pregnant women "listen" to other signs. In the first weeks, the abrupt cessation of toxicosis and frequent urge to urinate are alarming. These symptoms can indeed indicate the death or developmental delay of the fetus, as well as an ectopic pregnancy, but not always. Toward the end of the first trimester, the kidneys excrete less urine, in some this has been observed since 9‒10 weeks.
How to deal with frequent urination during pregnancy: tips
In the absence of pathologies, the discomfort caused by physiological frequent urination can be reduced as follows:
- Stay hydrated.
 Drink enough, but don't overdo it. Give preference to water over sugary drinks like coffee.
Drink enough, but don't overdo it. Give preference to water over sugary drinks like coffee. - Eat rationally. Eliminate diuretic foods (citrus fruits, spicy foods), as well as things that cause constipation. nine0027
- Exercise. Strengthen your pelvic muscles by training your vaginal and anus sphincters.
- Get more rest. Sleep during the day is very useful, especially in the later stages - after being in a horizontal position, the bladder empties faster, as a result, the load on the kidneys during night rest is reduced.
- Maintain immunity. Avoid hypothermia, take vitamin complexes as prescribed by the doctor.
- Empty your bladder as much as possible. Do not hold back the urge and try to make sure that all the urine comes out completely. In this regard, it is easier to urinate in the shower. nine0027
Control your condition. If other symptoms (pain, fever, burning sensation) appear in addition to frequent urination, tell your doctor immediately.
Cystitis during pregnancy: description of the disease, causes, symptoms, diagnosis and treatment
What not to do with cystitis in early pregnancy
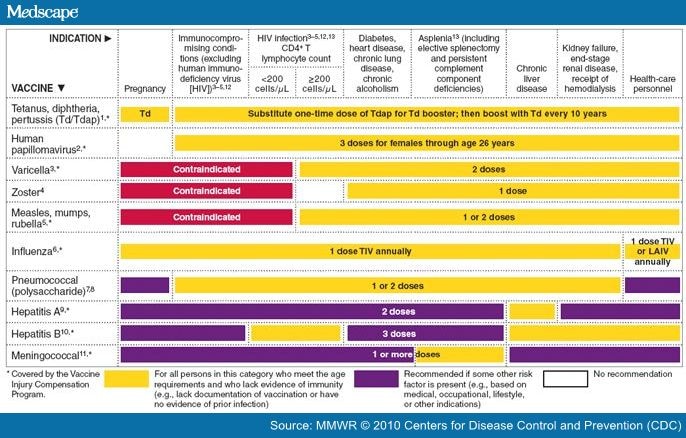
1. Take antibiotics unless prescribed by a doctor. Self-medication can lead to the development of fetal abnormalities. It is especially forbidden to take tetracycline, ofloxacin, norfloxacin, aminoglycosides. nine0008
2. Carrying out instillations. This procedure, during which an antibacterial drug is injected into the bladder, can cause an early miscarriage.
3. You can not take non-steroidal anti-inflammatory drugs. This refers to the intake of nimesil, diclofenac, analgin, etc. Otherwise, the unborn child may experience severe pathologies.
4. Do not carry out physiotherapy procedures, so as not to provoke a miscarriage. nine0008
5. Do not take a hot bath, do not visit the sauna, bath. Avoid overheating to avoid uterine hypertonicity.
How does cystitis manifest during pregnancy
The inflammatory process in the bladder in a pregnant woman is manifested:
-
Frequent urination.
nine0027 This symptom does not always signal the appearance of cystitis. This is normal during pregnancy.
This symptom does not always signal the appearance of cystitis. This is normal during pregnancy. -
The appearance of itching and burning in the urethra. An increase in these symptoms is observed after urine has begun to stand out.
-
There is always a feeling that the bladder has not completely emptied.
-
False claims appear. The pregnant woman is in dire need of going to the toilet, but there is no urine output. nine0008
-
The stomach hurts, heaviness is felt in the lower part of the abdomen.
-
The color of the urine changes. It is cloudy, reddish in color. This is due to blood impurities.
-
After emptying the bladder, urine still leaks. The spread of the inflammatory process occurred on the sphincter. In this case, there was a violation of its functioning. nine0008
-
A woman observes that a purulent and mucous secretion has begun to be released from the urethra.

-
body intoxication. General weakness appears, the head often hurts, body temperature rises, there is no appetite.
Features of the treatment of cystitis in the later stages
Treatment of the disease in the third trimester of pregnancy is very similar to early treatment. However, there is a decrease in the risk of developing pathologies in the unborn child if the gestational age is more than 24 weeks. nine0008
At this time, the formation of the main organs, tissues and systems has already taken place. They just mature and develop. But at this stage of pregnancy, the likelihood of developing cystitis increases, which is dangerous for both the child and the pregnant woman with its complications.
Those medicines and procedures that were prohibited at an early date may be prescribed at a later date. It must be remembered that only the attending physician can prescribe this. It takes into account all the risks of treatment for the expectant mother and her child. nine0008
nine0008
Exemplary regimen for the treatment of disease in late pregnancy
1. Appointment of antibiotic therapy. They can prescribe amoxicillin, suprax, monural. If the disease is more severe, the doctor prescribes penicillins, macrolipids, and other cephalosporins.
2. Instillation is carried out. During the procedure, an antibacterial and anti-inflammatory drug is injected into the bladder. This method can be carried out only in late pregnancy and only in the chronic form of the disease. The procedure is carried out in a hospital. nine0008
3. Herbal preparations (canephron, urolesan, cystone) are prescribed.
4. Treatment with antispasmodics.
5. Use of physiotherapy. Pregnant women may be prescribed electrophoresis or galvanophoresis with no-shpa or papaverine, calcium chloride, acetylsalicylic acid, antiseptic and antibiotic. These methods are indicated up to 34 weeks of pregnancy. Physiotherapy is in most cases prescribed for chronic cystitis. Contraindication is increased uterine tone, bleeding, preeclampsia, etc. nine0008
Contraindication is increased uterine tone, bleeding, preeclampsia, etc. nine0008
6. The use of immunostimulating drugs (flavozid or viferon).
It should be remembered that any therapeutic measures should be prescribed exclusively by a qualified and experienced specialist. With any attempt at self-treatment, the most deplorable consequences for the unborn child can occur.
Varieties of cystitis during pregnancy
Cystitis in early pregnancy can have a different etiology. This means that there is no single method of treating pathology. Drawing up a treatment regimen and prescribing drugs depends on the results of the diagnosis. The disease may be: nine0008
-
Hemorrhagic. The provoking factor is an infectious agent. They mean Escherichia or Pseudomonas aeruginosa, enterobacteria, streptococci. This is the most common form of cystitis. In such a situation, treatment with an antibacterial drug is necessary. The choice of the drug is carried out strictly by the attending physician, since the intake of certain drugs is prohibited in the first trimester of pregnancy.

- nine0007 Interstitial. This type of cystitis is characterized by a non-infectious inflammatory process, that is, the cause of the disease is an allergen or medication. To eliminate this form of the disease, an antibiotic is not prescribed. For the treatment of interstitial cystitis, a pregnant woman is shown taking anti-inflammatory, sedative and analgesic drugs.
-
Luchev. Refers to a rarer occurrence during pregnancy. This is explained by the fact that the conduct of radiation therapy to a woman is prohibited during the bearing of a child. For the treatment of this form of cystitis, antispasmodics, sedatives and drugs are prescribed that help accelerate regenerative processes. nine0008
-
Sexual. An exacerbation of this form of cystitis during pregnancy occurs due to prior infection. Strengthening of the symptoms of the disease is observed after sexual intercourse, if there are no barrier means of protection. This can be easily explained.
 After intimacy, the microflora changes. If pathogenic or conditionally pathogenic microorganisms have entered the urethra, a woman will notice the appearance of signs of cystitis. Genital inflammation of the bladder needs to take antiseptics, sedatives, diuretics. nine0008
After intimacy, the microflora changes. If pathogenic or conditionally pathogenic microorganisms have entered the urethra, a woman will notice the appearance of signs of cystitis. Genital inflammation of the bladder needs to take antiseptics, sedatives, diuretics. nine0008
Why does cystitis appear
The development of cystitis during pregnancy occurs under the influence of several factors. An important point is the timely determination of the causes that led to the appearance of cystitis. This is necessary so that the doctor can prescribe effective treatment and draw up a list of medical recommendations that will help the pregnant woman avoid a relapse of the disease. Also, it helps to prevent the transition of the disease into a chronic form. nine0008
There are a number of factors that lead to cystitis:
-
Promiscuous sexual intercourse. The likelihood of infection during sexual contact increases, since the urethra and vagina are located in close proximity.
 It should be borne in mind that the penetration of infection into the urinary tract can occur, both from the mucous membrane of the vagina and the external genital organ of a woman. nine0026
It should be borne in mind that the penetration of infection into the urinary tract can occur, both from the mucous membrane of the vagina and the external genital organ of a woman. nine0026 -
Prolonged presence of dysbacteriosis or vaginal candidiasis. If the vaginal microflora is disturbed, pathogenic microorganisms multiply much faster. This can cause an inflammatory response. nine0008
-
Impaired immunity. If immunity is lowered or allergic local pathologies are present, a significant decrease in the protective properties of the body occurs. As a result, pathogenic or opportunistic microorganisms enter the bladder without any obstacles.
-
With infrequent urination.
 It is normal for a woman to empty her bladder at least 4 times a day. During pregnancy, this figure increases. There are various reasons why a timely trip to the toilet is not possible. And if it becomes regular, the structure of the urethra and the sphincter anatomically change. As a result of such changes, the normal emptying of the bladder is disrupted. In addition, if urine is in the bladder for a long time, optimal conditions are created for infectious development. nine0008
It is normal for a woman to empty her bladder at least 4 times a day. During pregnancy, this figure increases. There are various reasons why a timely trip to the toilet is not possible. And if it becomes regular, the structure of the urethra and the sphincter anatomically change. As a result of such changes, the normal emptying of the bladder is disrupted. In addition, if urine is in the bladder for a long time, optimal conditions are created for infectious development. nine0008 -
With regular hypothermia. If the body of a pregnant woman is often supercooled, its local protective properties are weakened, as a result of this, the likelihood of unhindered penetration of the infection into the bladder increases. Damaging factors contribute to the development of an inflammatory reaction in the walls of the bladder, as a result - the appearance of signs of cystitis.
Neglect of hygiene rules. It is necessary to wash the external genital organs daily, to wash after intimacy, to change underwear in a timely manner, to use daily pads. All this helps to reduce the likelihood of infection entering the urinary tract of a woman.
All causes of cystitis are divided into infectious and non-infectious. There are four routes of bladder infection: nine0008
1. Descending - the penetration of the infection occurs from the inflamed organ, that is, the kidney.
Descending - the penetration of the infection occurs from the inflamed organ, that is, the kidney.
2. Ascending - the initial localization of the infection that has entered the bladder is the external environment.
3. Lymphogenic - lymphatic vessels are involved in the movement of the infection. Basically, the focus of infection in the inflamed genital organ.
4. Hematogenous - the spread of infection occurs through the bloodstream from a distant purulent focus. nine0008
Noninfectious causes of cystitis:
-
An allergic reaction, which manifests itself in the form of an inflammatory process of the mucous membrane of the bladder.
-
Disturbed work of the immune system, nervous system.
-
If the lower abdomen or pubis is undergoing radiation therapy.
nine0032 -
regular hypothermia of the body.

-
Constant use of tight underwear.
-
Non-compliance with hygiene rules.
-
Chronic disease of one or another internal organ. nine0008
-
Overwork, hypovitaminosis.
-
Impaired emptying of the bladder.
-
Reduced protective functions of the body.
-
The presence of a foreign body that is located in the bladder.
There are factors in the presence of which increases the likelihood of developing cystitis. This happens when:
Despite the fact that the most common cause of cystitis is a bacterial infection, the inflammatory process in the bladder can begin due to some non-infectious factors. nine0008
Under the influence of certain drugs, especially chemotherapy drugs, an inflammatory process in the bladder can begin. The cause of drug cystitis is the excretion of the decay products of medicines from the body.
With prolonged use of the catheter, there is an increase in susceptibility to bacterial infection. As a result, the likelihood of an inflammatory process increases. This is called foreign body cystitis. nine0008
This is called foreign body cystitis. nine0008
Some women may be hypersensitive to a particular substance found in personal care or household products. They mean bath foam, feminine hygiene spray, spermicidal gel. In some situations, the inflammatory process is a consequence of the reaction of the body - allergies.
Diagnostic measures
If any signs of cystitis appear, a woman should immediately consult a doctor. At the appointment, the patient is asked about how long ago she noticed the onset of symptoms, whether this happened before, and also what diseases were previously transferred and are present now. The patient must truthfully answer the questions. Otherwise, the doctor will not get a complete picture of what is happening to her. nine0008
To detect cystitis, the doctor sends for a laboratory examination. It consists in the delivery of a general analysis of blood and urine. Thanks to such studies, it is possible to detect inflammation, the level of leukocytes and the immature form of neutrophils, the level of erythrocyte sedimentation rate. In addition, protein in the urine, bacteria are detected. If the result of a general urinalysis showed that the content of leukocytes is increased, the patient is prescribed a urine test according to Nechiporenko.
In addition, protein in the urine, bacteria are detected. If the result of a general urinalysis showed that the content of leukocytes is increased, the patient is prescribed a urine test according to Nechiporenko.
Conducting such a urine test will help determine what was the causative agent of the disease. As a result, more effective treatment is prescribed. With this method of examination, an antibiogram can be performed and the sensitivity of the pathogen to various types of antibacterial drugs can be determined. nine0008
Also, special test strips are used, thanks to which nitrites and leukocytes are determined. Such special strips give a reaction if the products of the activity of pathogenic microorganisms are present in the urine.
Ultrasound examination of the bladder helps to exclude stones in the organ, and also, the doctor assesses the condition of the upper urinary tract and the organs adjacent to the bladder. Ultrasound will allow to exclude a volumetric neoplasm. nine0008
nine0008
How to prevent the development of cystitis
There are a number of recommendations, subject to which the likelihood of developing the disease decreases.
1. It is necessary to wash every day once a day. For these purposes, use soap, preferably for children. It does not contain fragrances and dyes.
2. Carefully monitor that the sexual partner observes the basic rules of personal hygiene. He must wash the external genitalia every day. nine0008
3. Before and after sexual intercourse, you should thoroughly wash yourself. Use soap. This rule must be respected by both sexual partners.
4. With stomatitis, tonsillitis, oral candidiasis and other infections, it is not recommended to have oral sex. This rule is easy to explain - with saliva, the infection is transmitted to the external genital organs, and then to the urethra.
5. Always dress for the weather. Hypothermia can cause chronic recurrent cystitis. It should be noted that cystitis is not the most terrible pathology that hypothermia can cause. In addition to cystitis, an inflammatory process develops in nearby organs, which can provoke a miscarriage. nine0008
In addition to cystitis, an inflammatory process develops in nearby organs, which can provoke a miscarriage. nine0008
6. Keep track of the state of your own immunity. If a woman often has a cold, it can be judged that the work of the immune system is reduced. To restore it, you need to contact a qualified specialist.
7. Try as much as possible not to hold back urination. With prolonged retention of urine in the bladder, an infection develops.
8. Drink enough fluids.
9. A man should change his underwear every day. Thanks to this rule, the risk of developing the disease is minimized.
10. After emptying the bowels, wipe from front to back. By no means the other way around. This tactic is easy to explain - if you wipe from back to front, you can transfer intestinal bacteria to the external genitalia. After that, pathogenic microorganisms will reach the urethra.
11. During an exacerbation of the disease, the patient should take about 2.