How much alcohol can you drink while pregnant
Drinking while pregnant: What we know and what we don’t | Your Pregnancy Matters
Will an occasional drink during pregnancy harm a baby? While we’ve long known that heavy alcohol consumption during pregnancy can cause these problems, the effects of an occasional glass of wine is less understood.“It’s our anniversary Saturday. Would it be OK to have a glass of wine?” “Can I have an occasional beer with dinner?” “I just found out I’m pregnant – but I had a couple drinks last weekend. Is my baby going to be OK?”
Pregnant women often have questions like these. Unfortunately, the advice they get can be confusing. Almost all national health organizations recommend complete abstinence when it comes to drinking during pregnancy, while some obstetricians – including myself – say it’s OK to have a drink now and then.
Still, we can’t ignore the potentially devastating effects of fetal alcohol spectrum disorders (FASDs): low birthweight, developmental delays, behavioral problems, and health problems such as seizures and visual or hearing impairment. Statistics show that as many as 2-5% of children born in Texas may have an FASD, and a 2017 study suggests that number is most likely underreported.
While we’ve long known that heavy alcohol consumption during pregnancy can cause these problems, the effects of an occasional glass of wine is less understood. Because we’re just not sure, there has been a push for women to refrain from consuming any alcohol while trying to get pregnant and during pregnancy.
Pregnancy, drinking, and the COVID-19 pandemic
During the pandemic, people in the U.S. purchased markedly higher amounts of alcohol. A report out of Columbia University found that Americans bought nearly $42 billion worth of alcohol from March to September 2020 – an increase of 20% compared to the same seven months in 2019.
The CDC reports that there was no change in the number of pregnant patients who report drinking from 2019 (pre-pandemic) to 2020 (the first year of pandemic). In both years, approximately 14-15% of pregnant women reported consuming alcohol and 6% reported binge drinking.
A report from Canada describes similar results, but a smaller percentage (6.7%) of women consuming alcohol in pregnancy. However, they also observed an increased rate of cannabis and tobacco use, as well as increased depressive symptoms and financial difficulties in patients who consumed cannabis or tobacco during pregnancy.
While it is good to know that women did not use alcohol to deal with the stress of pandemic, the number of people consuming alcohol during pregnancy is concerning. And, with the national uptick in drinking, patients may have more questions about alcohol use and overuse before, during, and after pregnancy.
What studies say about drinking while pregnant
The research is conclusive: Binge drinking and heavy consumption of alcohol in pregnancy pose a definite risk to the developing fetus. The CDC defines binge drinking as four drinks or more in two hours for women (five drinks or more for men). However, we just don’t have the same level of conclusive information when talking about low-level alcohol consumption.
For example, a 2012 Danish study examined the effects on 5-year-olds whose mothers drank alcohol during pregnancy, categorized as follows:
- Low consumption: One to four drinks a week
- Moderate consumption: Five to eight drinks a week
- High consumption: Nine or more a week
- Binge drinking: Five or more drinks during a single occasion
Researchers who knew nothing about the maternal consumption of alcohol during the pregnancy examined the 5-year-old children of those pregnancies. They performed tests on IQ, attention span, and executive functions such as planning, organization, and self-control. They were unable to tell any difference between children whose mothers drank low to moderate amounts of alcohol and those who abstained completely during pregnancy.
While this would seem to suggest that low-level alcohol consumption is safe during pregnancy, there are other factors to consider. First, while the study included 1,600 women, that’s still a relatively small sample size. Second, children’s brains are still developing at age 5, and the full effects that alcohol may have had on them may not yet be measurable.
The authors of the study concluded that more large-scale studies are needed to investigate the effects of low and moderate alcohol consumption during pregnancy – and that for now it’s best for pregnant women to avoid alcohol.
National health organizations advise abstaining from alcohol
There have been a number of publicized statements on alcohol use and pregnancy in the past year.
In November 2015, the American Academy of Pediatrics (AAP) published a report that focused on recognizing, diagnosing, and treating FASD. The AAP reaffirmed their recommendation that no amount of alcohol should be consumed during any trimester of pregnancy with a video series in 2019.
This follows the advice of most health organizations focused on pregnancy, such as the American College of Obstetricians and Gynecologists.
The CDC caused controversy in February 2016 when it published a report intended to raise awareness of the risk of FASD due to drinking before a woman realizes she is pregnant. The report recommended that women who are sexually active and want to get pregnant should avoid alcohol, and women who are sexually active and don’t want to get pregnant should use an effective birth control method. The report noted that half of pregnancies are unplanned, and even for women trying to conceive, most won’t know they’re pregnant until four to six weeks into the pregnancy.
In a press release announcing the report, a CDC official was quoted as saying: “It is critical for healthcare providers to assess a woman’s drinking habits during routine medical visits; advise her not to drink at all if she is pregnant, trying to get pregnant or sexually active and not using birth control; and recommend services if she needs help to stop drinking. ”
”
In January 2022, the CDC released a Frequently Asked Questions article about alcohol use and pregnancy, reaffirming that, “The best advice is to avoid any alcohol use when you start trying to get pregnant.”
Managing risks while preserving rights
Some pregnant women tell me they feel judged when they have a drink. I am not sure how we got to the point that in May 2016, New York City had to clarify guidelines prohibiting bars and restaurants from refusing to serve alcohol to pregnant women. The guidelines – which also apply to selling and serving foods such as soft cheeses and raw fish – are intended to discourage discrimination against pregnant women.
I understand the messages can seem mixed. For example, venues in New York City that serve alcohol are required by law to post a sign warning of the dangers that alcohol can pose to a developing fetus, but employees of that bar or restaurant must serve pregnant women alcohol if they order it.
Obviously, this is a complex issue.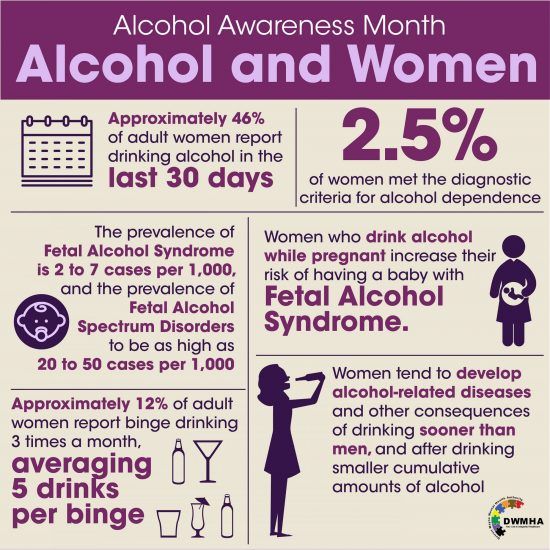 The debate that the New York City guidelines renewed over the risks of drinking while pregnant and preserving a woman’s right to make her own decisions followed the backlash a few months before to the CDC recommendation that women avoid drinking unless they were using birth control. Some women felt that the CDC was being condescending and interfering in their right to make decisions about how they live their lives.
The debate that the New York City guidelines renewed over the risks of drinking while pregnant and preserving a woman’s right to make her own decisions followed the backlash a few months before to the CDC recommendation that women avoid drinking unless they were using birth control. Some women felt that the CDC was being condescending and interfering in their right to make decisions about how they live their lives.
Having a drink during pregnancy is a personal decision
We know drinking heavily during pregnancy is not safe for the baby. We are less sure about the risks of low to moderate drinking, and until we have better information, it’s understandable that health organizations and providers would advise complete abstinence from alcohol.
Women make decisions about risks and outcomes for our health and the health of our children all the time. We decide what contraception to use based on our acceptance of the risk of an unintended pregnancy. We weigh risks and benefits of using anti-nausea medications or other drugs during pregnancy.
Healthcare providers must educate women about what we know regarding alcohol consumption during pregnancy. Women must be allowed to make their own decisions based on the amount of risk they are willing to accept. Many will say, “If there is any risk, I will follow the guidelines and not drink at all.” Others may examine the risks and choose to have an occasional drink.
The trouble with guidelines that recommend total abstinence is they don’t involve nuance. There are certainly women who truly have a problem with alcohol and whose drinking puts their babies at risk. We need to identify those women early and get them help. For women who do not have an unhealthy relationship with alcohol and who want to have a drink on a special occasion, they shouldn’t fear being judged or have others make that decision for them. However, pregnant patients who choose to drink should understand that any alcohol consumption – not just binge drinking – increases specific risks during pregnancy.
Proven risks of any alcohol consumption in pregnancy
Two studies from 2021 support the idea that alcohol consumption during pregnancy isn’t a good idea – both for the overall outcome of the pregnancy and for fetal neurodevelopment.
Increased risk of miscarriage is associated with any alcohol use in the first trimester. A study published in January 2021, which recruited patients prior to becoming pregnant and patients up to 7 weeks of pregnancy, showed an 8% increased risk of pregnancy loss each week between 5 and 10 weeks of gestation in patients who consumed alcohol compared to those who abstained.
To reduce the risk of miscarriage, women who are trying to conceive should consider avoiding alcohol. For those unwilling to do that or those with an unplanned pregnancy, stopping drinking as soon as a pregnancy test is positive may improve the likelihood of successful outcomes.
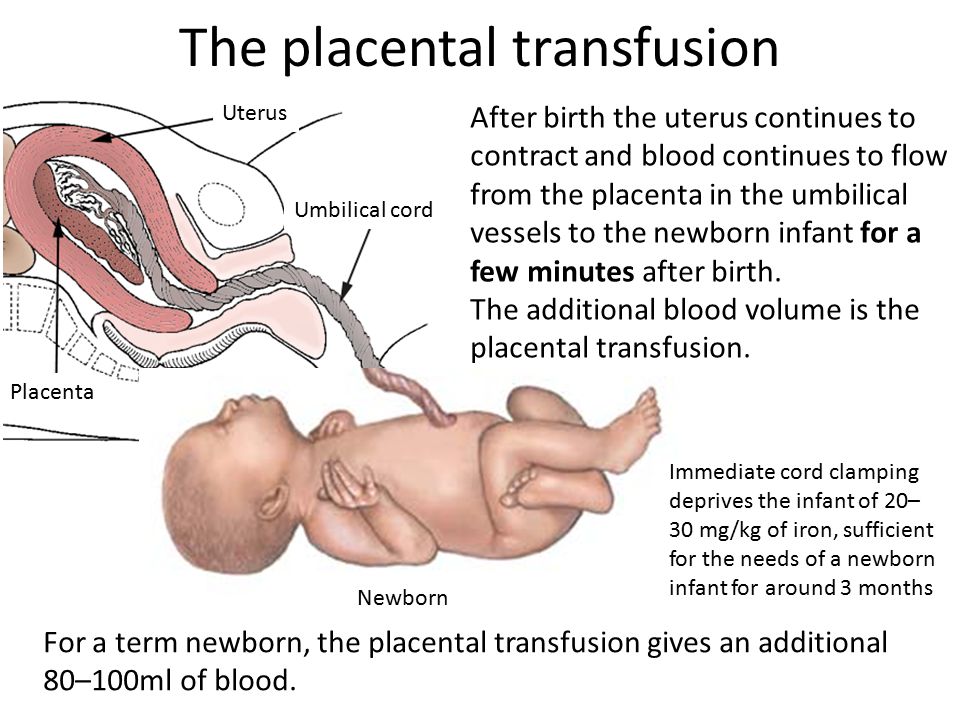
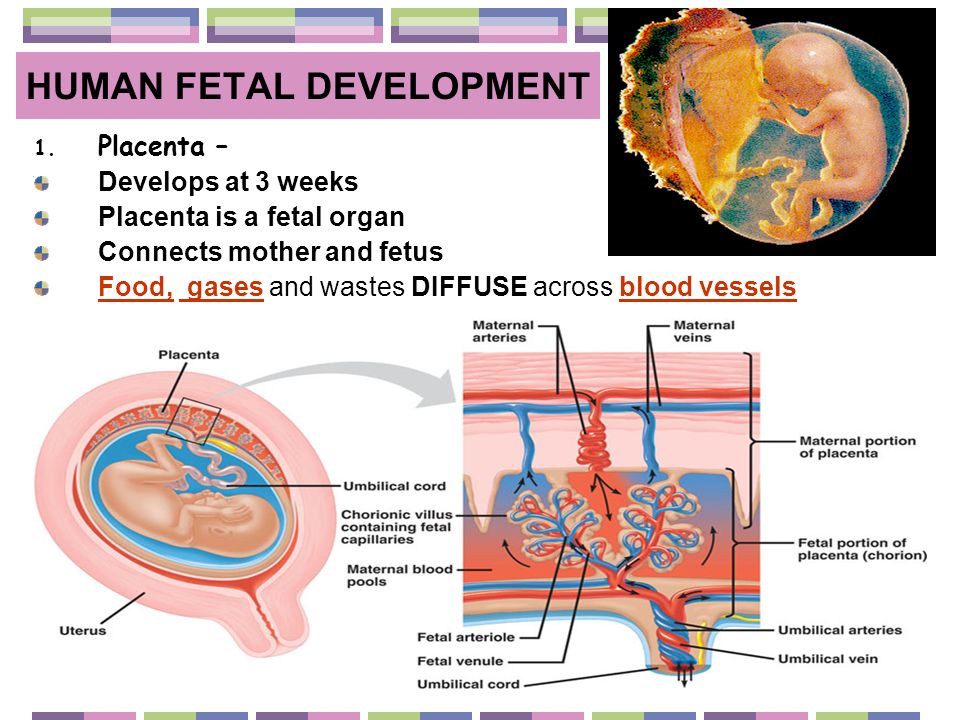
Stillbirth and fetal growth restriction also are associated with prenatal alcohol exposure.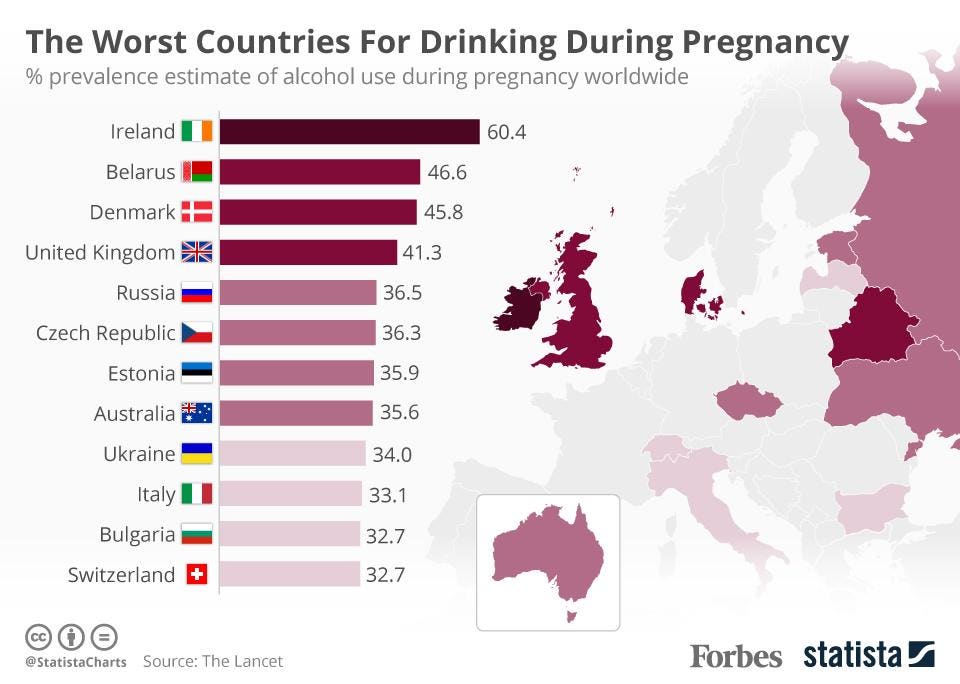 Results from a December 2021 study suggest that alcohol consumption in pregnancy leads to smaller placentas with abnormal blood vessels and abnormal function on the molecular level.
Results from a December 2021 study suggest that alcohol consumption in pregnancy leads to smaller placentas with abnormal blood vessels and abnormal function on the molecular level.
What if I drank before I realized I was pregnant?
Women frequently come to us worried because they had a few drinks before they noticed a missed period. I assure them there is little evidence to suggest that they harmed their pregnancy.
And I emphasize that stopping now that they’ve found out they’re pregnant can still improve pregnancy and fetal outcomes.
I also use this opportunity to discuss how much they normally drink and to educate them about the risks of drinking during pregnancy. If they don’t want to stop drinking entirely, we discuss what might be a reasonable limit. I tell patients I think one to two drinks a week is unlikely to be harmful – but that I can’t guarantee that there are no possible risks. Most of the time, patients just want to know it’s OK to have a glass of wine to celebrate a special occasion.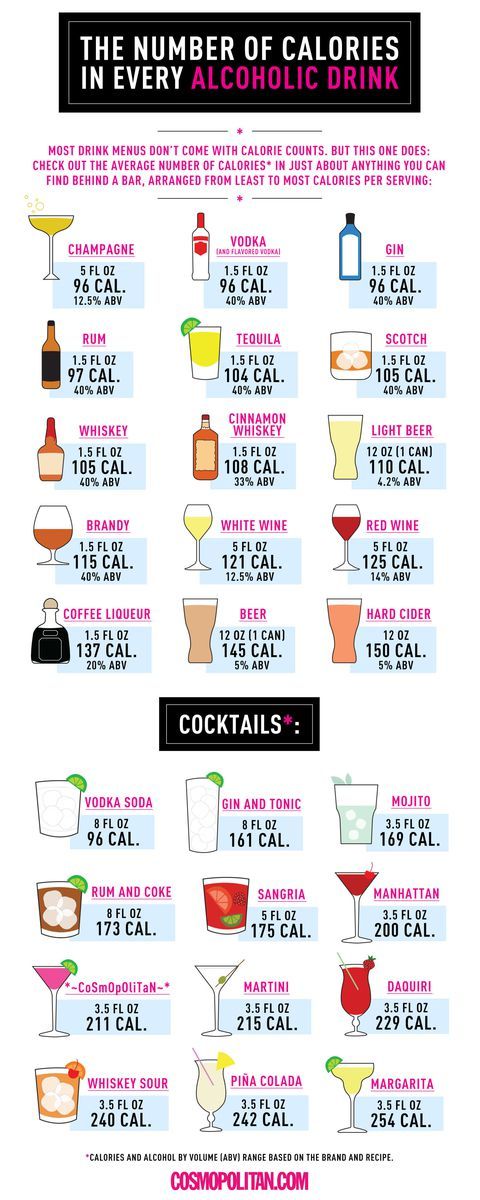
If you have a problem with alcohol, don’t be ashamed to ask for help. Addiction is a disease, and most people can’t manage it on their own. Your doctor can refer you to a therapist or program that may be able to help. We are here to help you, and we will not judge you. The sooner you get help, the better life will be for you and your baby.
To visit with a doctor, request an appointment online or call 214-645-8300.
Drinking alcohol while pregnant - NHS
Experts are still unsure exactly how much – if any – alcohol is completely safe for you to have while you're pregnant, so the safest approach is not to drink at all while you're expecting.
Is it safe to drink alcohol when pregnant?
The Chief Medical Officers for the UK recommend that if you're pregnant or planning to become pregnant, the safest approach is not to drink alcohol at all to keep risks to your baby to a minimum.
Drinking in pregnancy can lead to long-term harm to the baby, with the more you drink, the greater the risk.
How does alcohol affect my unborn baby?
When you drink, alcohol passes from your blood through the placenta to your baby.
A baby's liver is one of the last organs to develop and does not mature until the later stages of pregnancy.
Your baby cannot process alcohol well, and exposure to alcohol can seriously affect their development.
Drinking alcohol during pregnancy increases the risk of miscarriage, premature birth and your baby having a low birthweight. It can also affect your baby after they're born.
Drinking during pregnancy can cause your baby to develop a serious condition called foetal alcohol spectrum disorder (FASD).
FASD can cause problems with:
- learning and behaviour
- joints, bones, muscles and some organs
- managing emotions and developing social skills
- hyperactivity and impulse control
- communication, such as problems with speech
The risk is likely to be greater the more you drink.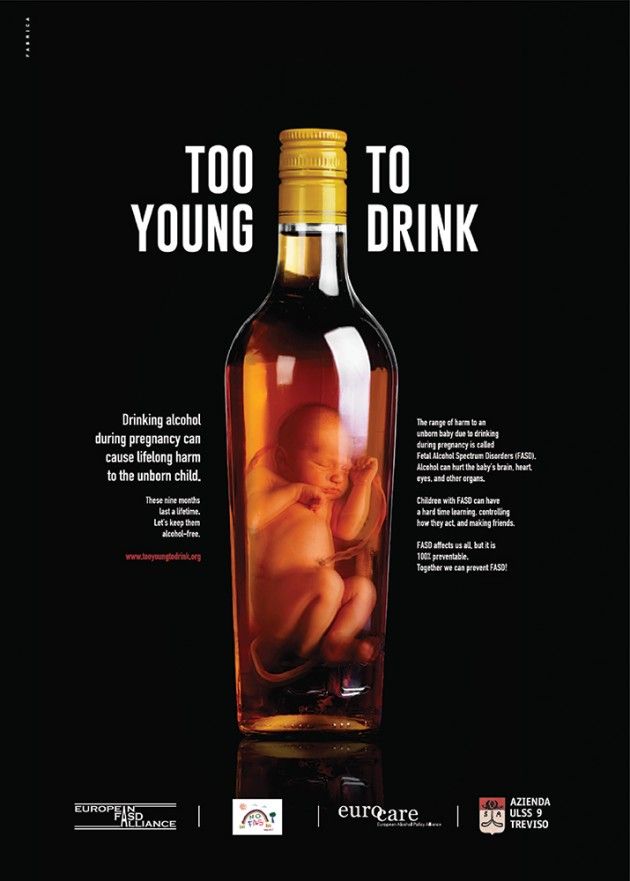
How to avoid alcohol in pregnancy
It may not be as difficult as you think to avoid alcohol completely during pregnancy, as many women go off the taste of alcohol early in pregnancy.
Most women do give up alcohol once they know they're pregnant or when they're planning to become pregnant.
Women who find out they're pregnant after already having drunk in early pregnancy should avoid further drinking.
However, they should not worry unnecessarily, as the risks of their baby being affected are likely to be low.
If you're concerned, talk to a midwife or doctor.
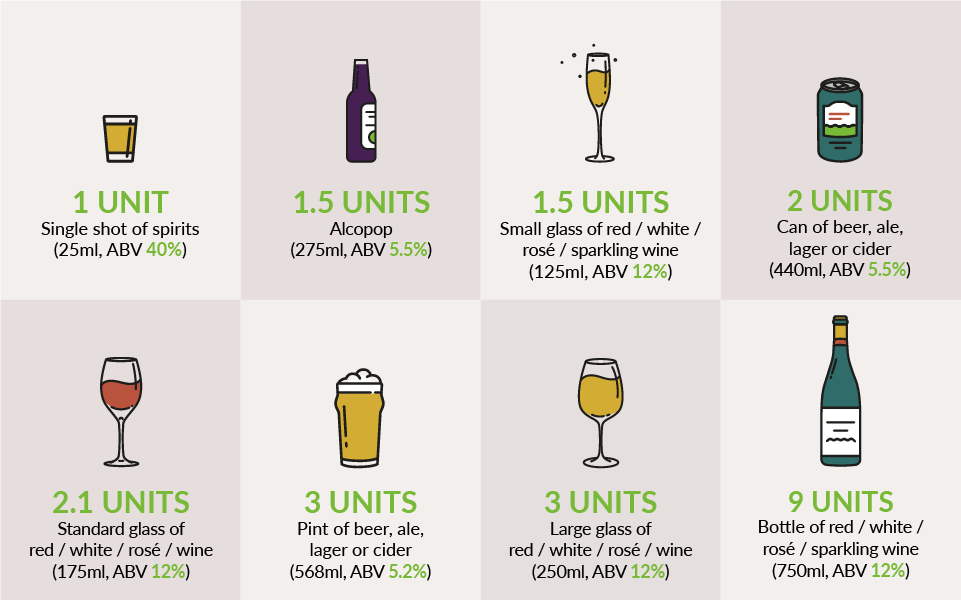
What is a unit of alcohol?
If you do decide to drink when you're pregnant, it's important to know how many units you are consuming.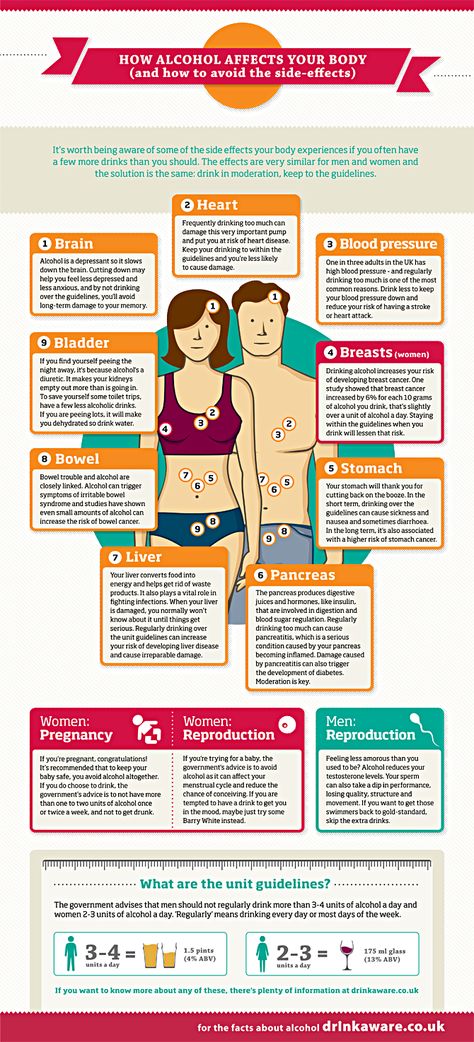
One UK unit is 10 millilitres (ml) – or 8 grams – of pure alcohol. This is equal to:
- just under half a pint of cider (218ml) at 4.5% alcohol by volume (ABV: you can find this on the label)
- just under half a pint of beer (250ml) at 4% ABV
- a single measure of spirit (25ml), such as whisky, gin, rum or vodka, at 40% ABV
- just under half a standard glass of wine (76ml) at 13% ABV
You can find out how many units there are in different types and brands of drinks with the Drinkaware unit and calorie calculator.
If you have an Android smartphone, iPhone, iPad or iPod touch, you can download the free One You Drinks Tracker from Google Play or the iTunes App Store. It allows you to keep a drinks diary and get feedback on your drinking.
Read more about alcohol units.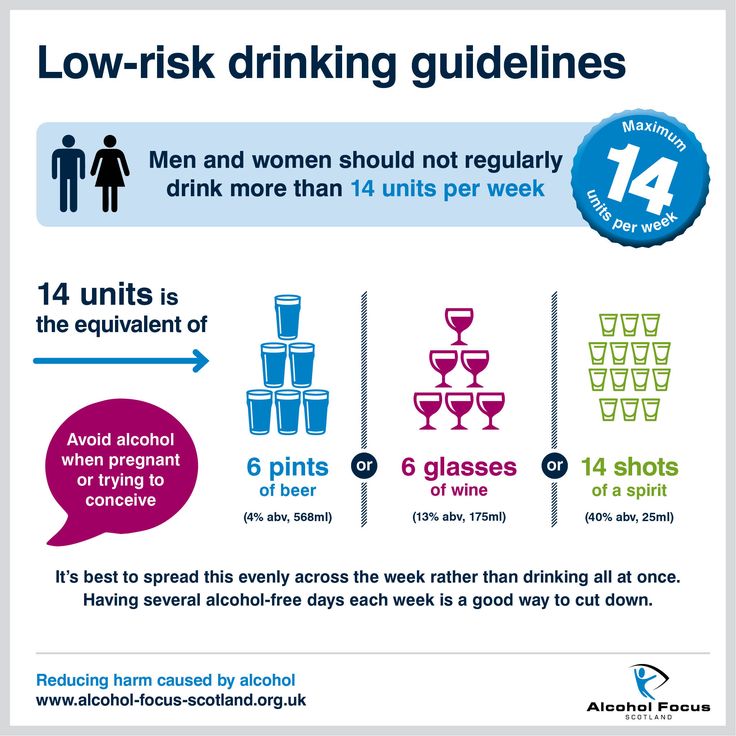
Alcohol support services
If you have difficulty cutting down what you drink, talk to a midwife, doctor or pharmacist.
Confidential help and support is also available from local counselling services:
- Drinkline – the national alcohol helpline; if you're worried about your own or someone else's drinking, call this free helpline on 0300 123 1110 (weekdays 9am to 8pm, weekends 11am to 4pm)
- We Are With You – a UK-wide treatment agency that helps individuals, families and communities manage the effects of alcohol and drug misuse
- Alcoholics Anonymous (AA) – a free self-help group; its "12-step" programme involves getting sober with the help of regular support groups
Find your nearest alcohol support services.
Read more advice on cutting down your drinking.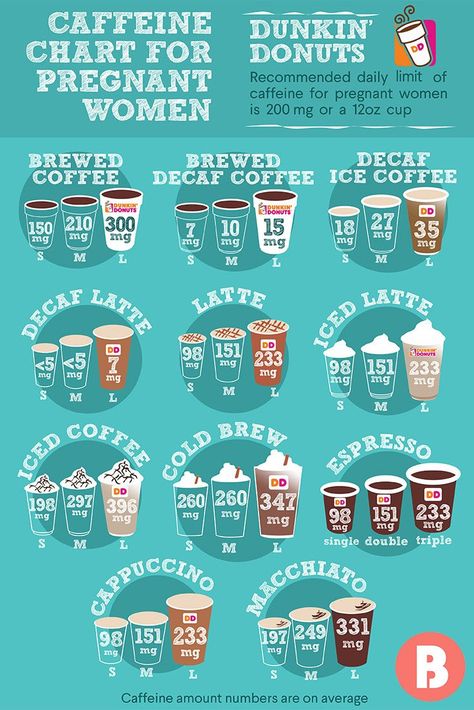
Find maternity services near you.
Page last reviewed: 29 January 2020
Next review due: 29 January 2023
What happens to the child if the mother drinks alcohol?
03.12.2019
Alcohol and pregnancy are incompatible - doctors do not get tired of talking about this to expectant mothers. But pregnant women sometimes allow themselves to skip a glass of wine, thinking that nothing bad will come of such an amount. However, alcohol can interfere with fetal development at any stage of pregnancy, even very early.
Studies show that excessive (four or more drinks at a time) and/or regular drinking by an expectant mother puts the fetus at the greatest risk of serious problems. But even a smaller amount of alcohol can be harmful, since there is no safe dose. nine0003
Alcohol easily passes from the mother's bloodstream into the child's bloodstream, which can affect the development of the brain and other vital organs, structures and physiological systems of the baby's body, leading to malformations that can begin in a child in early childhood and last a lifetime. The most profound effects of prenatal alcohol exposure are brain damage and associated behavioral and cognitive impairment.
The most profound effects of prenatal alcohol exposure are brain damage and associated behavioral and cognitive impairment.
Scientists define a wide range of effects and symptoms caused by prenatal alcohol exposure, termed "fetal alcohol spectrum disorders". These include conditions such as intrauterine alcohol syndrome, alcohol-related nervous system disorder, and alcohol-associated birth defects. All these cases have one common feature - damage to the central nervous system (CNS) as a result of prenatal alcohol exposure to the fetus. nine0003
The effect of alcohol on the CNS may be structural (eg, reduction in brain size, changes in certain areas of the brain) or functional (eg, cognitive and behavioral deficits, motor and coordination problems). Extended studies using modern imaging techniques (MRI, CT, etc.) have revealed differences in the structure and activity of the brain that are consistent with neuropsychological testing data, including a disorder in processing information from the senses, changes in cognitive processes and behavior in adults with the disorder alcohol spectrum of the fetus compared to healthy people. nine0003
nine0003
The most profound effects of prenatal alcohol exposure are brain damage and associated impairments in behavioral and cognitive functioning.
How are the disorders different?
Fetal alcohol syndrome was the first form of alcohol spectrum disorder and is still the most well-known syndrome. It manifests itself with excessive alcohol consumption by the expectant mother during the first trimester of pregnancy. The impact of harmful substances on the fetus can disrupt the normal development of not only the brain, but also the face. Thus, in addition to CNS developmental anomalies, the child will have a specific pattern of three facial anomalies: narrow eye openings, a smooth area between the lip and nose (compared to a normal ridge), and a thin upper lip. Also, the baby may experience growth deficiency in utero and (or) after birth. nine0003
Partial fetal alcohol syndrome includes only some of the characteristics listed above.
An alcohol-related disorder of the nervous system is characterized by disorders of the central nervous system, which may be structural or functional. Functional impairments include a complex pattern of cognitive (mental) or behavioral problems that do not correspond to the standard level of development at any given age in a child. At the same time, the reasons for this discrepancy cannot be explained by factors other than prenatal alcohol exposure. Facial abnormalities and growth retardation should not be present. nine0003
Alcohol-related birth defects include heart, kidney, bone, and other malformations; difficulties with vision and hearing; decreased function of the immune system. They are rarely considered separately, but rather are a secondary disorder that accompanies other fetal alcohol spectrum disorders.
What will happen to the baby in the future?
Every person whose mother may have abused alcohol during pregnancy experiences a combination of everyday turmoil that includes medical, behavioral, educational, or social problems in the following areas: nine0003
- learning and memorization;
- understanding and following directions;
- ability to keep attention;
- the ability to control emotions;
- communication and socialization;
- performing daily life skills (eg, eating, bathing, counting money, taking care of personal safety).

People with fetal alcohol spectrum disorder are more likely than others to make bad decisions, repeat the same mistakes, trust the wrong people, and have difficulty understanding the consequences of their actions. They are also more prone to disorders such as attention deficit hyperactivity disorder, depression, impulse control problems, alcoholism and drug addiction. nine0003
People with fetal alcohol spectrum disorder are more likely than others to make bad decisions, repeat the same mistakes, trust the wrong people, and have difficulty understanding the consequences of their actions.
Risk factors
Of course, it is impossible to argue that just one sip of champagne during pregnancy can provoke many anomalies in the development of the fetus and affect the psyche of the unborn child. But the medical community recommends completely avoiding any dose of alcohol during pregnancy. nine0003
There are risk factors that contribute to the development of undesirable consequences:
- the amount of alcohol a pregnant woman drinks at a time;
- frequency of drinking by a pregnant woman;
- the stage of pregnancy at which a woman drinks alcohol, and how much she drinks during the formation of one or another body system in the fetus.
Prenatal alcohol exposure to children can be exacerbated if their mothers are malnourished, overweight, underweight, or smoke…
In addition, studies show that prenatal alcohol exposure affects children more if their mothers live in unfavorable conditions and experience high levels of stress. These may include, for example, social isolation, living in a society where excessive drinking is common and acceptable, and living in a society where resources for prenatal care are limited.
The prenatal effects of alcohol on children can be exacerbated if their mothers are malnourished, overweight, underweight, smoke… nine0003
How to help a child?
First aid for a child is the refusal of the expectant mother from alcohol. But if during pregnancy a woman allowed herself to drink alcohol and the child has symptoms of a fetal alcohol spectrum disorder, special tactics of education and training should be applied. For example, a school may want to use specialized learning strategies that provide a consistent routine and allow children to continually practice learning skills. This will allow students to study better, remember lessons faster and keep up with the class. nine0003
For example, a school may want to use specialized learning strategies that provide a consistent routine and allow children to continually practice learning skills. This will allow students to study better, remember lessons faster and keep up with the class. nine0003
First aid for a child is the refusal of the expectant mother from alcohol.
Other ways to help include family support groups and classes to help parents take better care of their baby, prenatal and postpartum supplements for their babies, mental health interventions for children that include social skills training, problem solving, and personal safety.
Of course, all these measures can be taken by specialists. You should not take dietary supplements and medications unless prescribed by a doctor. nine0003
A child whose mother drank alcohol during pregnancy may develop both physiological and mental disorders, which will affect his life. A woman's refusal to drink alcohol will help her child grow up healthy and happy.
ALCOHOL AND PREGNANCY - Outpatient medical facility
The fact that you can not drink alcohol during pregnancy is known to most. However, different situations can arise in life: one woman is planning a pregnancy, continuing to drink alcohol on holidays in order to avoid uncomfortable questions; another drinks a glass of wine, unaware that she is already pregnant; the third during pregnancy cannot cope with the desire to drink beer, believing that "a little bit is possible." Let's look at these situations in more detail. nine0003
Alcohol consumption during pregnancy planning.
Alcohol is a toxin that adversely affects the human reproductive system. In women, alcohol consumption leads to disruption of the menstrual cycle and hormonal balance, which significantly affects the ability to conceive. There are also opinions that even episodic alcohol consumption can have a negative effect on the eggs, leading to their inferiority. Also, alcohol consumption affects the male reproductive system, significantly reducing the number of sperm capable of fertilization. Therefore, a couple planning a pregnancy should stop drinking alcohol at least 3 months in advance in order to increase the likelihood of conception. nine0003
Also, alcohol consumption affects the male reproductive system, significantly reducing the number of sperm capable of fertilization. Therefore, a couple planning a pregnancy should stop drinking alcohol at least 3 months in advance in order to increase the likelihood of conception. nine0003
Alcohol consumption in the first weeks after conception.
Without a special examination, a woman usually discovers the fact of pregnancy at 3 weeks after conception, when the next menstruation does not come. By this time, the embryo has already firmly attached to the uterine cavity and began to receive nutrition from the mother's blood. If negative factors, including alcohol, affect him before the moment of attachment, then this will lead to his rejection and death, and he will simply leave the uterus with the next menstruation. Thus, a woman may not know that she was pregnant. nine0003
According to most scientists, if alcohol did not disrupt the attachment process and the embryo continued to develop, then this would not lead to the formation of malformations in it.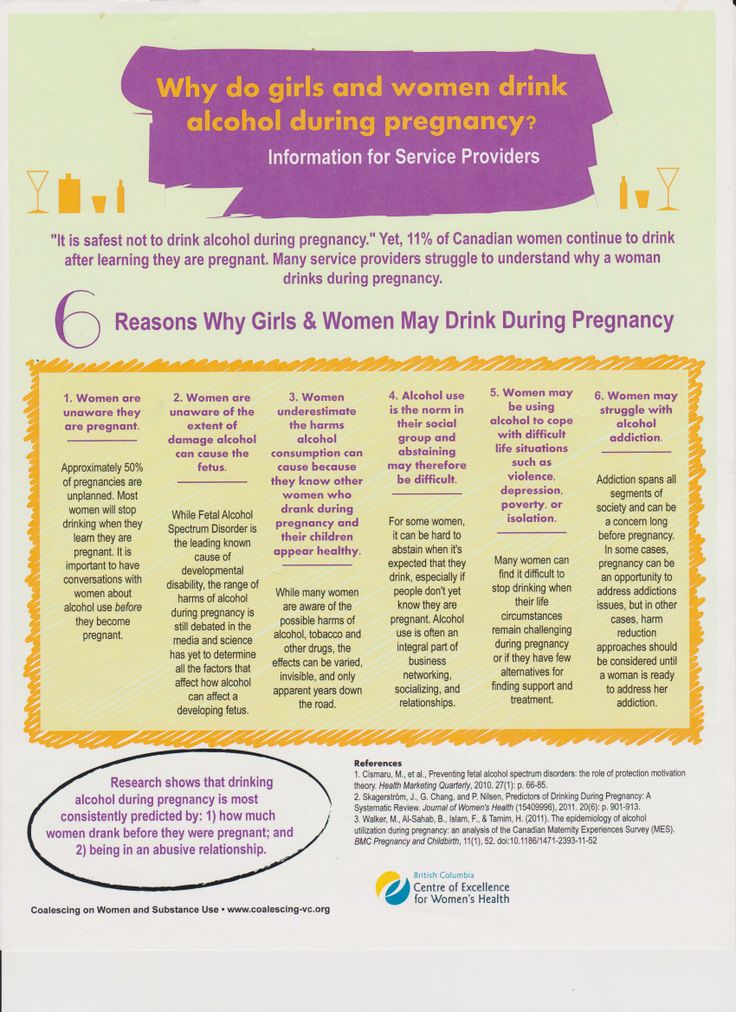 Thus, alcohol accidentally drunk during the first two weeks after conception will either lead to the termination of pregnancy or will not affect its further development.
Thus, alcohol accidentally drunk during the first two weeks after conception will either lead to the termination of pregnancy or will not affect its further development.
Alcohol use in early pregnancy.
As mentioned above, as early as the 3rd week after conception, the embryo begins to come into contact with maternal blood. This means that all the substances in the mother's blood come to him. including ethyl alcohol. From the 3rd to the 13th week of development, the laying of all the main systems of the body of the unborn child occurs and the effect of alcohol no longer leads to rejection and death of the embryo, but to the formation of malformations and deformities of the nervous, cardiovascular, and digestive systems. nine0003
Alcohol use in late pregnancy.
The negative impact of alcohol on the course of pregnancy is observed after the 13th week. Ethanol and its decay products lead to spasm of the vessels of the placenta and umbilical cord, impairing the delivery of oxygen and nutrients, leading to a delay in the development of the fetus, disruption of its nervous system and brain.