Bloody nose that won t stop
Nosebleed | NHS inform
About nosebleeds
Nosebleeds can be frightening, but they aren't usually a sign of anything serious and can often be treated at home.
The medical name for a nosebleed is epistaxis.
During a nosebleed, blood flows from one or both nostrils. It can be heavy or light and last from a few seconds to 15 minutes or more.
What to do
To stop a nosebleed:
- sit down and firmly pinch the soft part of your nose, just above your nostrils, for at least 10 to 15 minutes
- lean forward and breathe through your mouth – this will drain blood into your nose instead of down the back of your throat
- place an ice pack or bag of frozen vegetables covered by a towel on the bridge of your nose
- stay upright, rather than lying down, as this reduces the blood pressure in the blood vessels of your nose and will discourage further bleeding
If the bleeding eventually stops, you won't usually need to seek medical advice. However, in some cases you may need further treatment from your GP or in hospital.
Read more about treating nosebleeds
When to seek medical advice
Non-urgent advice: Contact your GP practice if:
- you're taking a blood-thinning medicine (anticoagulant) such as warfarin or have a clotting disorder such as haemophilia and the bleeding doesn't stop
- you have symptoms of anaemia such as heart palpitations, shortness of breath and a pale complexion
- a child under 2 years of age has a nosebleed
- you have nosebleeds that come and go regularly
If your GP practice is closed, phone 111.
Immediate action required: Go to your nearest accident and emergency (A&E) or phone 999 if:
- the bleeding continues for longer than 20 minutes
- the bleeding is heavy and you've lost a lot of blood
- you're having difficulty breathing
- you swallow a large amount of blood that makes you vomit
- the nosebleed developed after a serious injury, such as a car crash
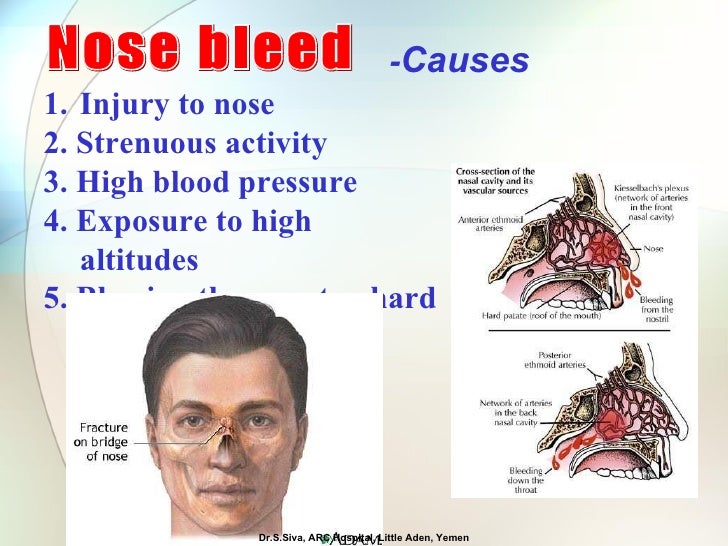
What causes nosebleeds?
The inside of your nose is full of tiny, delicate blood vessels that can become damaged and bleed relatively easily.
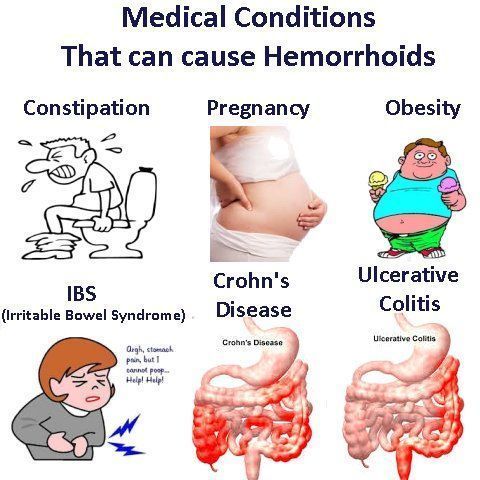
Common causes of nosebleeds include:
- picking your nose
- blowing your nose very hard
- a minor injury to your nose
- changes in humidity or temperature causing the inside of the nose to become dry and cracked
Occasionally, bleeding can come from the blood vessels deeper within the nose. This can be caused by a blow to the head, recent nasal surgery and hardened arteries (atherosclerosis).
Read more about the causes of nosebleeds
Who gets nosebleeds?
Nosebleeds are fairly common and most people will experience them every now and again. Anyone can get a nosebleed, but they most often affect:
- children between 2 and 10 years of age
- elderly people
- pregnant women
- people who take blood thinning medication such as aspirin or anticoagulants, such as warfarin
- people with blood clotting disorders, such as haemophilia
Bleeding may also be heavier or last longer if you take anticoagulants, have a blood clotting disorder, or have high blood pressure (hypertension).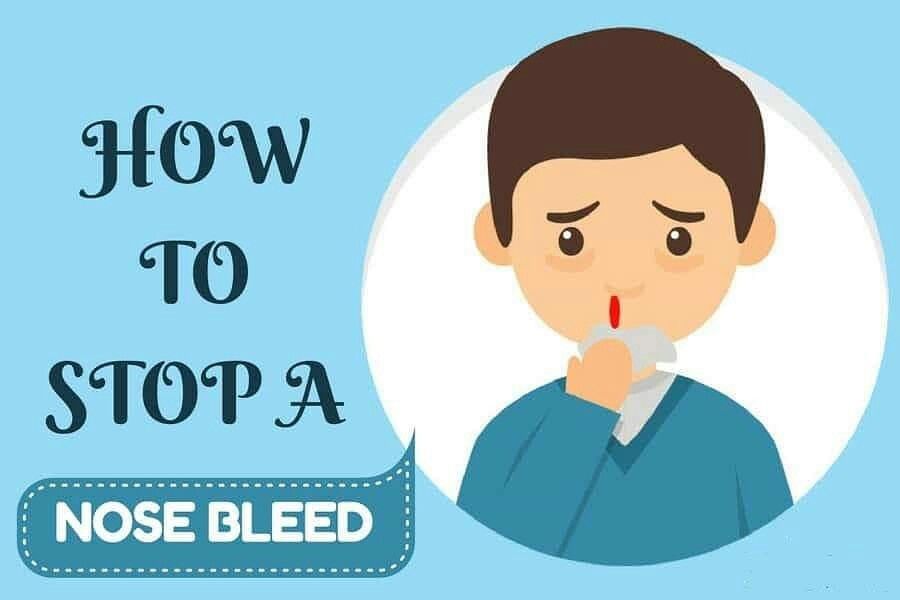
Are nosebleeds serious?
Nosebleeds aren't usually serious. However, frequent or heavy nosebleeds may indicate more serious health problems, such as high blood pressure or a blood clotting disorder, and should be checked.
Excessive bleeding over a prolonged period of time can also lead to further problems such as anaemia.
If your GP suspects a more serious problem is causing your nosebleeds, they may refer you to an ear, nose and throat (ENT) specialist for further tests.
Preventing nosebleeds
There are things you can do to prevent nosebleeds.
Do
- avoid picking your nose and keep your fingernails short
- blow your nose as little as possible and only very gently
- keep your home humidified
- wear a head guard during activities in which your nose or head could get injured
- always follow the instructions that come with nasal decongestants – overusing these can cause nosebleeds
Talk to your GP if you experience nosebleeds frequently and aren't able to prevent them. They may refer you to an ENT specialist for an assessment.
They may refer you to an ENT specialist for an assessment.
Causes of nosebleeds
Nosebleeds can be caused by a number of different things. It's not always possible to identify the exact reason why one occurs.
Nosebleeds can start just inside your nostrils (anterior) or at the back of your nose (posterior). These different types of nosebleeds tend to have different causes.
Anterior nosebleeds
The vast majority of nosebleeds are anterior nosebleeds, which means the bleeding comes from the wall between the two nose channels (the lower septum), just inside your nose. This part of the nose, known as Little's area, contains many delicate blood vessels that can be easily damaged.
The cause of anterior nosebleeds is sometimes unknown, but they can be caused by a number of things, including:
- picking your nose, particularly if you scratch the inside of your nose with a sharp fingernail
- blowing your nose very hard
- a minor injury to your nose
- a blocked or stuffy nose often caused by an infection such as a cold or flu
- sinusitis – an infection of the small, air-filled cavities inside your cheekbones and forehead
- dry air or an increase in temperature drying out the inside of your nose
- hay fever or other allergies
- high altitude
- excessive use of nasal decongestants
- a crooked nasal septum that's either present from birth (congenital) or the result of an injury (a deviated septum)
Anterior nosebleeds are more common in children and are not usually a sign of anything serious. They can often be treated easily at home.
They can often be treated easily at home.
Read more about treating nosebleeds
Posterior nosebleeds
A small number of nosebleeds are posterior nosebleeds, which means the bleeding originates from branches of arteries that supply blood to the space inside your nose between the roof of your mouth and your brain (nasal cavity).
These nosebleeds are more common in adults than children. They can be more serious than anterior nosebleeds and bleed more heavily. Medical attention may be required.
Causes of posterior nosebleeds include:
- a blow to your head, or a fall
- a broken nose
- recent nasal surgery
- hardened arteries (atherosclerosis)
- medicines that cause you to bleed more easily, including aspirin and anticoagulants such as warfarin and heparin
- a tumour in the nasal cavity
- a blood clotting abnormality – such as haemophilia or von Willebrand disease
- hereditary haemorrhagic telangiectasia (HHT) – an inherited genetic condition that affects the blood vessels
- leukaemia (although this is rare and you're likely to have other symptoms as well)
High blood pressure (hypertension) is also more common in people with nosebleeds and may make it harder to stop the bleeding, but it's not clear whether this directly causes nosebleeds.
Treating nosebleeds
Most nosebleeds can be stopped without the need for medical attention, but occasionally further treatment may be required.
What to do
To stop a nosebleed:
- sit down and firmly pinch the soft part of your nose, just above your nostrils, for at least 10-15 minutes
- lean forward and breathe through your mouth – this will drain blood into your nose instead of down the back of your throat
- place an ice pack or bag of frozen vegetables covered by a towel on the bridge of your nose
- stay upright, rather than lying down as this reduces the blood pressure in the blood vessels of your nose and will discourage further bleeding
If the bleeding eventually stops, you won't usually need to seek medical advice. However, you should still follow our recovery advice.
Non-urgent advice: Contact your GP practice if:
- you're taking a blood-thinning medicine (anticoagulant) such as warfarin or have a clotting disorder such as haemophilia and the bleeding doesn't stop
- you have symptoms of anaemia such as heart palpitations, shortness of breath and a pale complexion
- a child under 2 years of age has a nosebleed
- you have nosebleeds that come and go regularly
If your GP practice is closed, phone 111.
Immediate action required: Go to your nearest accident and emergency (A&E) or phone 999 if:
- the bleeding continues for longer than 20 minutes
- the bleeding is heavy and you've lost a lot of blood
- you're having difficulty breathing
- you swallow a large amount of blood that makes you vomit
- the nosebleed developed after a serious injury, such as a car crash
Find your nearest A&E department
Medical treatment
If you see your GP or go to hospital with a nosebleed, you will be assessed to determine how serious your condition is and what's likely to have caused it. This may involve looking inside your nose, measuring your pulse and blood pressure, carrying out blood tests and asking about any other symptoms you have.
These are the main treatments that your GP or hospital doctor may use to stop your nose bleeding.
Antibiotic ointment
Your doctor may prescribe an antibiotic ointment. This should be applied by squeezing a pea-sized amount onto the front of the nasal septum (wall between the nostrils).
This can reduce the inflammation and crusting in the nose and reduce the severity and frequency of nosebleeds.
Antibiotic ointment is particularly effective in children.
Cautery
If your doctor is able to identify exactly where the bleeding is coming from, they may carry out a minor procedure to seal the bleeding blood vessel by cauterising (burning) it.
This is normally done using a stick of a chemical called silver nitrate. A local anaesthetic will be sprayed into your nose to numb it and the silver nitrate stick will be held against the bleeding point for up to 10 seconds.
Nasal packing
If cautery is ineffective or your doctor is unable to identify a specific bleeding point, they may recommend packing your nose with gauze or special nasal sponges to stop the flow of blood by applying pressure to the source of the bleeding.
Packing will usually be carried out after local anaesthetic has been sprayed into your nose. The gauze or sponges often need to be left in place for 24-48 hours before being removed by a health professional. You'll usually need to be admitted to hospital to be monitored during this time.
Further treatment
If the treatments above don't help, you may be referred to a hospital specialist such as an ear, nose and throat (ENT) doctor for further treatment.
Additional treatments that may be used in hospital include:
- electrocautery – an electric current running through a wire is used to cauterise the blood vessel where the bleeding is coming from
- blood transfusions – a procedure to replace the blood you've lost
- tranexamic acid – medication that can reduce bleeding by helping your blood to clot
- packing under anaesthetic – your nose is carefully packed with gauze while you are unconscious from general anaesthetic
- ligation – an operation using small instruments to tie off bleeding blood vessels in the back of your nose
Recovery
Once your nose has stopped bleeding, you should follow the advice below to reduce the risk of your nose bleeding again and to stop you picking up an infection:
- avoid blowing or picking your nose, heavy lifting, strenuous exercise, lying flat, and drinking alcohol or hot drinks for 24 hours
- don't remove any crusts that form inside your nose – these may be unpleasant, but they're a useful part of the healing process
- if you need to sneeze, try to sneeze with your mouth open to reduce the pressure in your nose
- avoid people with coughs and colds
If you see a GP or a hospital doctor about your nosebleed, they may give you a prescription for an antiseptic nasal cream once the bleeding stops. This should be applied to the inside of your nostrils several times a day for up to two weeks to help prevent further bleeding.
This should be applied to the inside of your nostrils several times a day for up to two weeks to help prevent further bleeding.
If your nose does start to bleed again, follow the first aid advice above and seek medical advice if the bleeding doesn't stop.
Vasomotor Rhinitis: Symptoms, Causes & Treatment
Overview
What is vasomotor rhinitis?
Vasomotor rhinitis happens when the tissues inside of your nose become inflamed (swollen). The inflammation causes unpleasant symptoms most people associate with allergies, like a stuffy or runny nose.
However, unlike allergies (allergic rhinitis), vasomotor rhinitis doesn’t result from exposure to allergens, like pollen, mold, pet dander, etc. It’s not caused by viruses or bacteria either. Instead, you may experience symptoms because of weather changes, certain smells, eating, exercise, medications or other triggers that irritate your nose.
Vasomotor is also called idiopathic rhinitis. It’s a type of nonallergic rhinitis.
Who is likely to have vasomotor rhinitis?
Anyone can develop vasomotor rhinitis, but most people get diagnosed after age 20. The majority of diagnoses occur between ages 30 and 60. It’s more common in women and people assigned female at birth.
How common is vasomotor rhinitis?
Allergic and nonallergic rhinitis (including vasomotor rhinitis) affects up to half of the population in industrialized countries. Vasomotor rhinitis accounts for anywhere from 15% to half of these cases.
Symptoms and Causes
Vasomotor rhinitis may result from multiple triggers, including medications and changes in your environment.What causes vasomotor rhinitis?
Vasomotor rhinitis, unlike allergic rhinitis, doesn’t happen because you’re sensitive to a specific allergen, like tree pollen, dust mites or mold. Instead, various triggers may cause symptoms. It’s likely people with vasomotor rhinitis have heightened sensitivity to various substances and environmental changes that would trigger a response in most people — just in higher amounts.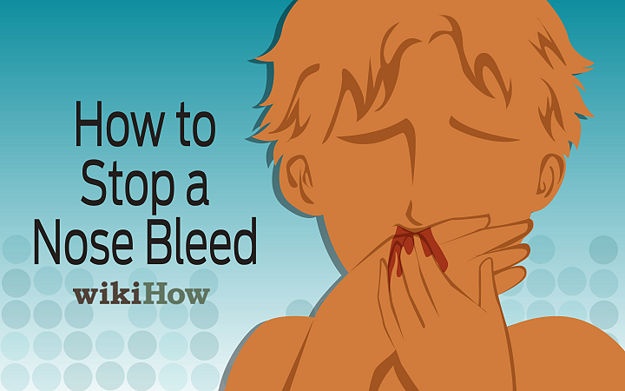
If you have nasal inflammation and related symptoms resulting from an unknown cause, you might receive this diagnosis.
What triggers vasomotor rhinitis?
Triggers related to your environment, medicines you’re taking and even hormone changes can cause a reaction.
Environmental triggers
Your surroundings can trigger your senses and cause a reaction. Common environmental triggers include:
- A drop in temperature.
- Air pollution or smog.
- Cold or dry air.
- Perfume or cologne.
- Cigarette smoke.
- Paint fumes.
- Spicy food.
- Stress.
Medication triggers
Certain medications can trigger nasal inflammation and swelling or make it worse. Triggers include:
- Nasal decongestant sprays (when they’re overused).
- ACE inhibitors to treat high blood pressure.
- Alpha-blockers and beta-blockers to treat high blood pressure.
- Nonsteroidal anti-inflammatory drugs (NSAIDs).

- Hormone medications, like birth control pills.
- Medicines that treat erectile dysfunction (ED).
- Antidepressants.
- Sedatives.
Hormone imbalances
Hormone changes can trigger a reaction. You may experience symptoms during times when hormones are in flux, including:
- Menopause.
- Puberty.
- Pregnancy.
Nonallergic rhinitis may also result from using nonprescription drugs, like cocaine.
What are the symptoms of vasomotor rhinitis?
Unlike allergic rhinitis, symptoms of vasomotor rhinitis usually occur year-round. Instead of being seasonal — as is the case with seasonal allergies — symptoms flare up whenever you’re exposed to a trigger.
Symptoms of vasomotor rhinitis include:
- Stuffy nose.
- Runny nose.
- Postnasal drip.
- Sneezing.
- Diminished sense of smell.
Rarely, vasomotor rhinitis causes a foul-smelling crust to form inside your nose. The interior nasal tissues may bleed when you attempt to remove the crust.
The interior nasal tissues may bleed when you attempt to remove the crust.
Is vasomotor rhinitis contagious?
No. It’s unrelated to germs that cause infections, like viruses and bacteria, which means you can’t catch it or spread it to someone else.
Diagnosis and Tests
How is nonallergic rhinitis diagnosed?
A healthcare provider can diagnose vasomotor rhinitis with a physical exam of your nose and throat and a review of your medical history. In some cases, further testing helps confirm your diagnosis.
- Allergy testing: Your provider may recommend allergy testing to rule out the possibility that allergies are causing your symptoms. Allergy tests use a blood sample or a skin prick, which exposes your body to small amounts of specific allergens. Then, it tests for antibodies in your blood made in response to those allergens. You may need a referral to an allergy expert for this test.
- Nasal endoscopy: In rare cases, providers examine the inside of your nose and nasal passages with a long, flexible tube called an endoscope.
 During the exam, a provider can identify other problems that may cause your symptoms, such as nasal polyps. Nasal polyps are noncancerous growths of tissue occurring in your sinuses or nasal passages.
During the exam, a provider can identify other problems that may cause your symptoms, such as nasal polyps. Nasal polyps are noncancerous growths of tissue occurring in your sinuses or nasal passages. - Computed tomography (CT) scan: Your provider may recommend a CT scan. This test uses X-rays to create detailed pictures of the inside of your nose. They can show if structural irregularities, like nasal polyps or a deviated septum, are causing your symptoms.
- Nasal inspiratory flow test: Your provider may order a nasal inspiratory flow test to measure how much air enters your lungs when you inhale. It can detect blockages in your nasal passages that may be causing your symptoms.
Management and Treatment
Is vasomotor rhinitis curable?
There isn’t a cure for nonallergic rhinitis. Most people manage symptoms with self-care measures, changes to their environment and medicine.
How is vasomotor rhinitis treated?
If your condition results from exposure to triggers like perfumes, treatment may be as simple as avoiding the trigger. In those cases where avoiding the trigger is impossible, you can put measures in place to ease symptoms, try over-the-counter medications or get a prescription from a healthcare provider.
In those cases where avoiding the trigger is impossible, you can put measures in place to ease symptoms, try over-the-counter medications or get a prescription from a healthcare provider.
Using a humidifier at home or at work may ease symptoms. It may be helpful to rinse your nasal passages with a saline (salt water) solution to clean out your nose and nasal cavities (nasal irrigation).
Prescribed medications can decrease nasal inflammation and manage your symptoms. These medications may include:
- Decongestant nasal sprays to relieve nasal congestion.
- Antihistamine nasal sprays that reduce nasal inflammation.
- Corticosteroid nasal sprays (like fluticasone) to reduce nasal inflammation (first-line treatment for nasal congestion).
- Anticholinergic nasal sprays (like ipratropium bromide) to help with a runny nose.
Surgery may be an option if the medications aren’t helping or if another condition is intensifying the problem, like a deviated septum or nasal polyps.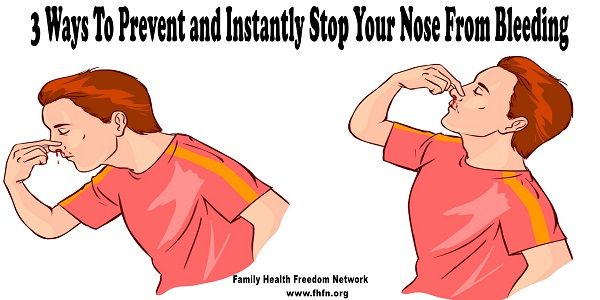
What complications are associated with vasomotor rhinitis?
Left untreated, vasomotor rhinitis may cause persistently blocked nasal passages or a constantly runny nose. These conditions can cause complications, including:
- Middle ear infections.
- Nasal polyps.
- Sinusitis, inflammation of your sinus cavities.
- Difficulty sleeping and a tired feeling during the day.
- Difficulty concentrating.
- Irritability.
Prevention
Can vasomotor rhinitis be prevented?
There’s no way to prevent vasomotor rhinitis. You can lower your risk by avoiding triggers known to cause rhinitis.
Outlook / Prognosis
What is the prognosis (outlook) for people with vasomotor rhinitis?
For many people, vasomotor rhinitis is a chronic, or long-term, condition. It may come and go over time.
Living With
When should I contact my doctor?
If you have a runny nose, stuffy nose or postnasal drip that won’t go away, talk to a healthcare provider. They can help determine what’s triggering your symptoms. They can recommend treatments that can help.
They can help determine what’s triggering your symptoms. They can recommend treatments that can help.
A note from Cleveland Clinic
The symptoms associated with vasomotor rhinitis — runny nose, nasal congestion and postnasal drip — are unpleasant, regardless of the cause. If you’re experiencing these symptoms, and they don’t improve, see a healthcare provider. They can determine whether the cause is related to allergies, an infection or something else (as is the case with vasomotor rhinitis). They can recommend or prescribe medicines that can help.
Nosebleed: what to do?
Is your city Moscow?
- Pharmacies
- Catalog
- Discounts and promotions nine0006
- Loyalty program
- Jobs
- Help nine0006
- Rent
- Contacts
- COVID-19
September 1, 2021
Nosebleed, or epistaxis, is an unexpected and even frightening phenomenon.
Should one be alert when such an unpleasant symptom appears, what factors provoke it and how can one help in such a situation? Let's figure it out further. nine0003
Why does the nose bleed?
Bleeding from the nose is classified into "anterior" and "posterior". In the first case, the cause is damage to small blood vessels, this type is usually easy to stop. The second case is considered more dangerous, bleeding occurs due to injury to large vessels located deeper in the nose, so it cannot be dealt with at home. If the blood is "in full swing" - this is a reason for an urgent call for an ambulance.
Causes of nosebleeds include:
- nose injury;
- thinning of the mucous membrane;
- inflammatory processes in the nasal cavity;
- vascular fragility, diseases of the heart and blood;
- sudden increase in blood pressure;
- uncontrolled intake of certain drugs (anticoagulants, NSAIDs, vasoconstrictor drops for the common cold).

What should I do if my nose bleeds?
At the moment when the bleeding starts, it is important to try not to be nervous, because the excitement makes our heart beat faster, which leads to more blood loss. nine0003
The bleeding stop algorithm is as follows:
- Sit straight, tilt your head forward.
- You should be comfortable: loosen the belt and collar, if necessary, open the window.
- Place a cold, wet towel or ice on your nose and a warm heating pad on your feet. This will help constrict the vessels in your nose and dilate them in your legs, which will reduce bleeding.
- Clamp the bleeding vessel: squeeze the wings of the nose with your fingers for 3-5 minutes, the blood should stop. Also for this purpose, you can enter a gauze swab previously moistened with hydrogen peroxide into the nostril. nine0006
If you have completed all of the above and the blood continues to flow, call an ambulance immediately, as even a small loss of blood can lead to fainting.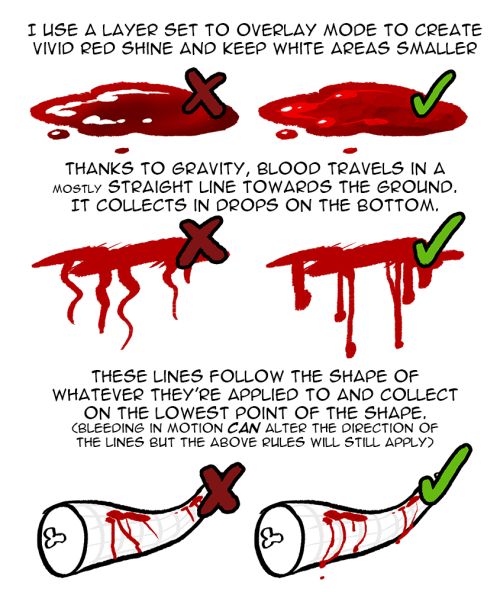
What to remember about nosebleeds?
- Do not lie down and do not let your feet be above your head - this will increase bleeding;
- Do not tilt your head: a large amount of blood in the stomach can cause vomiting, and blood can flow into the windpipe and make breathing difficult. nine0006
- After the bleeding has stopped, refrain from eating and caffeinated drinks to avoid high blood pressure and new bleeding.
Prevention of nosebleeds
Remember, frequent nosebleeds are a reason to see a doctor. The specialist will identify the cause of the problem and prescribe treatment, which may include the use of hemostatic agents, as well as drugs that improve blood circulation.
To prevent rebleeding, your specialist may recommend:
- Taking medications and vitamins to strengthen blood vessels.
- Proper diet. Adding foods rich in vitamin K and C to the menu. Vitamin K is responsible for blood clotting, they are rich in parsley, spinach, basil, bananas, avocados, broccoli, bran, etc.
 Vitamin C strengthens the walls of blood vessels, it is found in large quantities in rose hips, sweet peppers, currants, citrus fruits, etc.
Vitamin C strengthens the walls of blood vessels, it is found in large quantities in rose hips, sweet peppers, currants, citrus fruits, etc. - Activity and moderate physical activity: light exercise in the morning, daily walks in the fresh air, swimming pool, etc.
Be healthy!
- General
- Interesting
- Health
Popular
You may be interested
nine0002 Disclaimer This blog is not intended to provide diagnosis, treatment or medical advice. The information on this block is provided for informational purposes only. Please consult your physician for any medical and health-related diagnoses and treatments. The information on this blog should not be considered a substitute for consulting a physician.
The information on this blog should not be considered a substitute for consulting a physician.
Frequent nosebleeds: what are the causes and what to do?
Other related articles: otolaryngologist, therapist
-
"Sedentary" diseases
-
10 examinations
-
COVID-19
-
adenovirus infection
-
Adenoids
- nine0128 Angina
-
Anemia
-
Meniere's disease
-
Bronchitis
-
Bronchoscopy
-
Types of ELI tests nine0129
-
All about flu
-
Sinusitis
-
Nasal hemangioma
-
Hypertension
-
Flu and SARS
- nine0128 flu during pregnancy
-
Diarrhea (diarrhea)
-
Eustachitis
-
iron deficiency
-
Ear diseases
-
immunity to coronavirus nine0129
-
Nose curvature
-
Nosebleeds
-
Nosebleed
-
Laryngitis
-
Lungs after COVID
nine0005 -
Lymphadenitis
-
ENT diseases in children
-
mastoiditis
-
Medical examinations
-
Uric acid nine0129
-
Runny nose
-
Nasal septum
-
Surveys in autumn
-
Complications after angina
-
Pneumonia
nine0006 -
Defeat the Flu
-
Items in the nose
-
Taking antibiotics
-
Signs of COVID-19
-
Application of ozone
- nine0128 Washing lacunae
-
Rheumatism
-
Sinusitis
-
Vaccine testing
-
Tonsillitis
-
Tuberculosis nine0129
-
Sulfur Plug Removal
-
Tick bite
-
Bed bug bites
-
Pharyngitis
-
ferritin
- nine0128 Chronic fatigue
-
nasal endoscopy
Treatment of adenoids
Bleeding from the nose due to trauma usually does not raise questions, but if it occurs without any mechanical impact, and even often, this should alert
What can be the causes of frequent nosebleeds and how they can be cured - tells otorhinolaryngologist of the clinic "Semeynaya" Olga Pavlovna Soloshenko. nine0003
nine0003
If the bleeding does not occur from trauma and recurs periodically, it is better not to delay the visit to the ENT. After all, bleeding can be anterior and posterior - the second happens less often, but it is much more dangerous. With anterior bleeding, blood only goes out, with posterior bleeding, it flows into the mouth or stomach along the back of the pharynx. Posterior is usually caused by damage to larger vessels that are located deep in the nasal cavity. It is very difficult to stop back bleeding without a doctor.
Causes of nosebleeds:
- Injuries. Injury to the nose is often fraught with cartilage fractures. As a rule, this is accompanied by swelling and pain.
- High blood pressure. Very common cause. Due to a sharp jump, the walls of the capillaries easily burst. Pressure rises due to overload, as well as in the presence of diseases of the cardiovascular system.
- Sunstroke and any sudden increase in body temperature.
 nine0006
nine0006 - Overwork.
- Hormonal changes. Bleeding may occur in women during the months of pregnancy or menopause, and in adolescents at puberty.
- Dry air. It causes dryness of the mucous membranes.
- Poor blood clotting.
- ENT diseases. Sinusitis, sinusitis, rhinitis - all of them can cause bleeding, especially with the constant use of drugs that thin the mucosa. nine0006
- Vascular problems. Even infectious diseases such as chickenpox, measles, influenza, etc. can lead to them.
- Polyps, adenoids, tumors. In addition to occasional bleeding, they simply make breathing difficult.
- Foreign body - can damage the mucous membranes and blood vessels.
- Deficiency of vitamins K, C and calcium.
First aid rules for nosebleeds:
- Lie down (or position the patient) with legs down
- Tilt head forward
- Place a cold compress on the bridge of the nose for a few minutes
- Cover nose with hand or insert swab pre-moistened with hydrogen peroxide
- Drops can be instilled to constrict blood vessels
Attention, this must not be done!
- Throwing the head back (contrary to popular belief) - blood can enter the respiratory tract
- Blow your nose - so as not to increase bleeding without it.

Which cases require an immediate call to a doctor and an ambulance
- In case of loss of consciousness
- For excessive bleeding
- Blood flows with clear fluid (this may occur after trauma and indicate a skull fracture)
- If vomiting of blood occurs (possibly indicating bleeding in the esophagus or stomach)
- Foamy blood (possible with lung injury)
- In case of diabetes mellitus in a patient
- If the patient is known to have poor blood clotting
Treatment
Treatment of bleeding is carried out in a complex manner. Often, an otorhinolaryngologist works in conjunction with a general practitioner, neurologist, endocrinologist, and hematologist.
At the first examination, the doctor determines the type of bleeding - anterior or posterior. Also, the patient is required to pass a general blood test and a coagulogram (analysis of blood coagulation indicators). In addition, it is important to measure the pressure, because if it is above the norm (the absolute norm is 120/80 mm Hg, but these figures change depending on age), the blood will not stop until it decreases. nine0003
nine0003
In case of significant blood loss, the patient may be left in the hospital.
As a treatment for bleeding, it is possible to pack the nasal cavity, cauterize vessels (with drugs, laser, ultrasound, etc.), remove polyps. If there is no result, surgical ligation of vessels in problem areas is performed. In addition, drugs are prescribed that increase blood clotting.
Prevention
- Taking drugs that strengthen the walls of blood vessels
- Nutrition rich in vitamins and minerals
- Air humidification during the heating season
- Injury Prevention
- Monitoring blood pressure and taking medications to lower it
Nosebleeds are not only unpleasant, but also dangerous. Therefore, as soon as it begins to bother you regularly, it is important to see a doctor as soon as possible. It is better to exclude all the most terrible causes of such a phenomenon as soon as possible and then it is already calmer to engage in further treatment.