Throwing up in last trimester
Vomiting in Third Trimester of Pregnancy
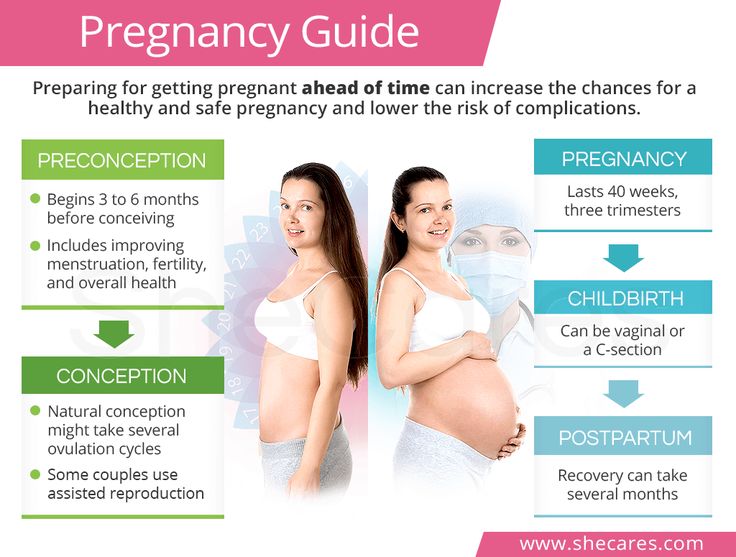
Nausea and vomiting are common in the first trimester of pregnancy; in fact, these are two of the very first symptoms that help you realise that you are pregnant. While it’s common to feel nauseated all the time in the first trimester of your pregnancy, if it continues in the second and third trimester of pregnancy, then it will obviously be taxing for you. If you are in your third trimester of pregnancy, it is essential that you know whether you should be concerned about vomiting at this stage.
Also Read: Complications during Third Trimester
Reasons for Vomiting in the 3rd Trimester of Pregnancy
Of the several symptoms that you go through while you are pregnant, vomiting in the third trimester of pregnancy is a concern that is bound to leave you worried. However, please remember that you are not the only one going through this and hence, it is not unnatural or abnormal. Some of the possible reasons for vomiting in the third trimester are as follows:
1.
One very obvious reason for vomiting in the final trimester of pregnancy is morning sickness. It is a common phenomenon and might result in vomiting even in the last trimester of pregnancy.
Also Read: 3rd Trimester Pregnancy Checklist
2. Heartburn or Acid Reflux
This is also a common occurrence in the advanced stages of pregnancy. When the muscles of the valve between the stomach and the oesophagus relax due to hormonal changes in pregnancy, it allows the stomach acids to move back up into the oesophagus. Also, as the size of the uterus gradually increases, it exerts pressure on the stomach, forcing acids upwards. This can then lead to vomiting.
3. Dehydration
Not drinking adequate amounts of water can lead to dehydration in the body which, in turn, can result in nausea and vomiting.
Also Read: Sex during Third Trimester
4. Food Poisoning
Food poisoning results in vomiting whether you are pregnant or not; however, it can be more severe and harmful when you’re carrying your baby. Infectious organisms in your food basically lead to a stomach bug or food poisoning, causing you to feel nauseated and vomit.
Infectious organisms in your food basically lead to a stomach bug or food poisoning, causing you to feel nauseated and vomit.
5. Preeclampsia
Vomiting might also be because of preeclampsia which is a complicated condition that can affect the baby. However, vomiting is a symptom that occurs only at a very late stage of the condition which is usually detected earlier itself.
Also Read: Diet during 3rd Trimester
Vomiting during the third trimester of pregnancy is not a rare or unusual symptom. However, you should try to find out the reason behind this condition in order to cross out any serious issues that may be causing it. If vomiting is because of reasons like morning sickness, food poisoning, acidity, etc., the baby will not be harmed and simple medications can treat such problems. However, it is always better to be safe and consult a doctor if you are experiencing any such symptom which you feel is unusual or detrimental to your health.
How to Avoid Vomiting in the Third Trimester
Some small precautions taken beforehand can reduce the symptoms of nausea and vomiting, if not eliminate them completely. So, if you are worried about vomiting in or around the 8th month of pregnancy, you can take the following measures to keep nausea at bay:
So, if you are worried about vomiting in or around the 8th month of pregnancy, you can take the following measures to keep nausea at bay:
1. Drink lots of water.
Water helps you feel refreshed and keeps your bowel movements consistent. Drinking enough water would also decrease the chances of vomiting in the third trimester to a great extent. However, avoid drinking a lot of fluids in one go; rather, keep sipping a bottle of water every few hours. If you don’t like the taste of plain water, you can always add a lemon wedge or a piece of fruit to it to improve its taste. You can also opt for ice chips or clear fruit juices to ensure that you maintain your fluid intake.
2. Opt for small meals.
A pregnant woman is often advised to ‘eat for two’ since she is carrying a baby, but this is not true or required. Too much food on your plate might make you lose your appetite, especially if you are vomiting frequently. So, do not eat too much at a time; instead, have small meals spread throughout the day. Eat less but eat often, as this ensures smooth digestion. If foods with strong odours trigger nausea, you can choose to have such foods that can be eaten at room temperature (without any side effects).
Eat less but eat often, as this ensures smooth digestion. If foods with strong odours trigger nausea, you can choose to have such foods that can be eaten at room temperature (without any side effects).
3. Maintain a healthy diet.
A proper diet would decrease the chances of food poisoning or help prevent any kind of infection in the stomach for that matter.
4. Do not go to bed immediately after a meal.
It is always advisable to walk or rest for some time after a meal, rather than going to bed immediately, as this ensures that the process of digestion takes place sooner and better.
5. Make sure you’re well-rested.
Get plenty of rest during your pregnancy, be it through a good night’s sleep or by fitting in naps throughout the day (but not immediately after a meal, as mentioned!). This will alleviate a lot of problems you face while pregnant, nausea included.
Vomiting during pregnancy is not something very abnormal or unusual. Still, if you experience vomiting in the later stages of pregnancy even after trying out these measures, it is recommended that you consult a doctor.
Also Read: What Body Changes Occur during the Third Trimester of Pregnancy?
Nausea and Vomiting In The Third Trimester of Pregnancy
Posted at 05:12h in Inform by Guest Contributer
Associate Professor Steve Robson explains why women can experience nausea and vomiting late in their pregnancy, and what to do when this occurs.
Most women will experience nausea, and possibly vomiting (commonly referred to as ‘morning sickness’) in early pregnancy. While ‘nausea and vomiting of pregnancy’ (NVP) is common and distressing, the severe condition called hyperemesis gravidarum is fortunately rare.
For the unlucky few who suffer unremitting morning sickness through to the latter stages of pregnancy, the condition can be exhausting and debilitating. And then there are some women who have a complete recovery, and assume they are in the clear, only to have the problems return towards the end of pregnancy.
Reasons for Nausea During Pregnancy
As the uterus increases in size, the other abdominal organs (the bowel, in particular) are compressed in the upper part of the abdomen, against the diaphragm. Also, the hormones of pregnancy have some important effects. These hormones act to relax the valve, or ‘sphincter,’ that normally holds the junction between the oesophagus (gullet) and stomach closed.
Also, the hormones of pregnancy have some important effects. These hormones act to relax the valve, or ‘sphincter,’ that normally holds the junction between the oesophagus (gullet) and stomach closed.
At the same time, the movement of food onward from the stomach into the small bowel can be very slow, a condition known as ‘gastroparesis.’
This means that there can be a lot of food in the stomach that is pressed from below by the pregnant uterus.
Due to the laxity of the sphincter, the food flows back upwards, and sometimes out. This can cause painful heartburn, nausea, and sometimes vomiting.
Relief Measures
Eating smaller meals, avoiding lots of fluid with meals, taking antacids, and not eating too close to bedtime can help. Some women sleep with their head elevated to help reduce the reflux.
In severe cases, for which these measures do not provide relief, doctors sometimes prescribe medication that reduces acidity in the stomach and increases the movement of the stomach to help empty it. Fortunately, these symptoms usually resolve as soon as the baby is born.
Fortunately, these symptoms usually resolve as soon as the baby is born.
Other Conditions That Can Cause Nausea and Vomiting
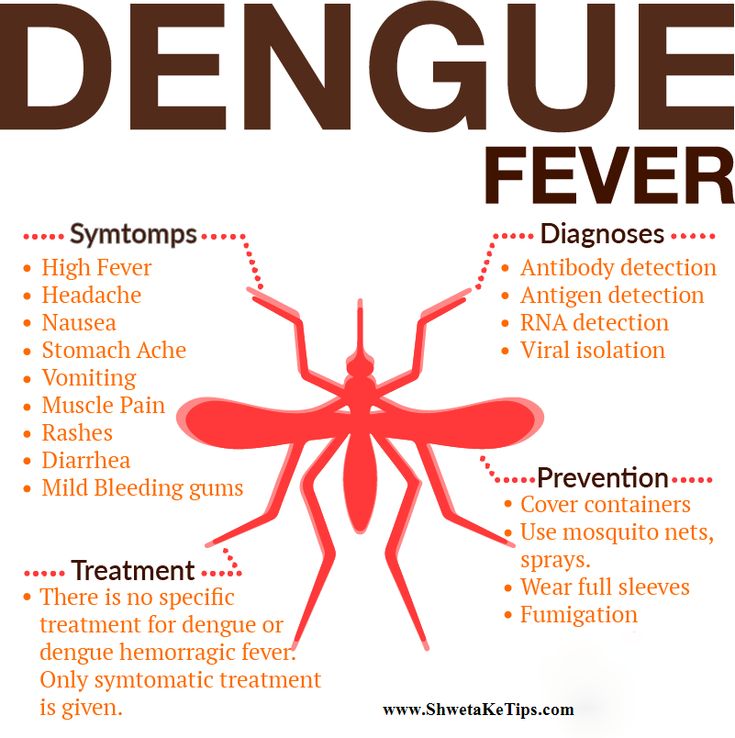
There are some other important conditions that can cause nausea and vomiting in late pregnancy, and if you are in any doubt about what is causing it, contact your doctor or midwife. Food poisoning, for example with salmonella or E coli, can cause a sudden onset of vomiting, but usually with diarrhoea as well.
Similarly, contagious episodes of gastroenteritis (such as caused by Norovirus) can also make women ill.
Vomiting and diarrhoea can last for several days, leading to dehydration, and these can pose risks for both mother and baby, including miscarriage. For these reasons, it is important to be very conscious of food safety, and to avoid other people if an epidemic of gastroenteritis is occurring.
Finally, some important complications of pregnancy can sometimes lead to the onset of upper abdominal pain, nausea and vomiting. Fortunately, they are very rare, but women should always alert their doctor or midwife if they have concerns.
Fortunately, they are very rare, but women should always alert their doctor or midwife if they have concerns.
Pre-eclampsia most commonly occurs in a woman’s first pregnancy.
It can cause high blood pressure, swelling, and the presence of protein in the urine. In very severe cases, pre-eclampsia can cause a woman to feel acutely unwell, with pain in the upper abdomen, nausea and vomiting.
The other condition is acute fatty liver, which is extremely rare and can be difficult to diagnose as sometimes the initial signs are very vague. Acute fatty liver can be so severe it can lead to loss of the baby. And sometimes a liver transplant is the only treatment – thankfully we rarely see this.
In summary, women who have nausea and vomiting in the third trimester will often feel better with simple measures.
If the condition doesn’t respond, becomes severe, or is associated with other problems, make sure you let your doctor or midwife know straight away.
Associate Professor Steve Robson is vice-president of the Royal Australian and New Zealand College of Obstetricians and Gynaecologists and a practising obstetrician.
Words by Dr S. Robson
What is preeclampsia? - ADONIS Medical Center in Kyiv
Preeclampsia, or late toxicosis, is a complication of pregnancy that develops in the 2nd and 3rd trimesters. It is possible to suspect its development in the early stages by the formation of edema and increased pressure. At the same time, the diagnosis can be confirmed or refuted only by the results of blood and urine tests.
Late toxicosis, compared with early, develops infrequently. According to the World Health Organization, its symptoms occur in an average of 8% of pregnant women. At the same time, in the territory of the CIS countries, this figure reaches 10-17%.
Severe forms of preeclampsia are rare, but the risk of such complications cannot be ignored. Unlike early toxicosis, late toxicosis poses a serious threat to the life of the mother and child. It is one of the main causes of perinatal morbidity and maternal mortality.
It is one of the main causes of perinatal morbidity and maternal mortality.
Although the consequences of preeclampsia seem frightening, do not worry ahead of time. First, edema and hypertension can occur for other reasons. Secondly, with the timely diagnosis of late toxicosis and the selection of the correct therapy, a woman can fully bear the pregnancy and give birth to a healthy baby.
At what time does late toxicosis begin? It is believed that the early onset of preeclampsia is associated with a severe course and often leads to premature birth, including by caesarean section.
Causes of late toxicosis in pregnant women
What exactly provokes the development of preeclampsia in pregnant women has not been established. There are several theories that have a different number of supporters, but none of them allows you to accurately determine which woman will develop late toxicosis and which will not.
At risk are pregnant women with:
- Hypertension;
- Diseases of the kidneys, liver, biliary tract, thyroid gland, adrenal glands, lungs and/or heart;
- Violation of fat metabolism and obesity;
- Anemia;
- Fetal growth retardation;
- Rh incompatibility;
- Multiple pregnancy;
- Birth or abortion within the last two years;
- Under the age of 19 or over 36.

The likelihood of developing late toxicosis increases against the background of chronic diseases. However, even if there are several risk factors, it cannot be said with certainty that there will be a complication.
How preeclampsia manifests itself
When preeclampsia develops in a woman, first there is a spasm of all vessels and a violation of blood circulation, as well as its clotting and fluidity. Because of this, hypoxia can develop, affecting the functioning of the heart, kidneys, liver, brain and placenta. As a result, dystrophic changes may occur in these organs.
There are 4 stages of preeclampsia:
- Edema;
- Nephropathy;
- Preeclampsia;
- Eclampsia.
At the first stage, late toxicosis is manifested by edema on the legs, arms, abdomen and in the face and neck. Most often, they do not provoke a significant deterioration in the well-being of a pregnant woman or the development of severe complications in her. In addition, with timely therapy, the following forms of preeclampsia develop in no more than 20% of cases.
In addition, with timely therapy, the following forms of preeclampsia develop in no more than 20% of cases.
With nephropathy, in addition to edema, hypertension and impaired renal function appear, which is determined by the release of protein in the urine.
Preeclampsia is the third stage of preeclampsia, which develops in only 5% of pregnant women. It is characterized by changes in the central nervous system that cause nausea, vomiting, headache, and other symptoms.
The most difficult stage of late toxicosis is eclampsia. With its development, pathological disorders are aggravated, and, in addition to the listed symptoms, the woman also has convulsions, a sharp increase in pressure and the risk of stroke.
Late toxicosis may result in:
- Severe edema;
- High blood pressure;
- Disorders of the functions of the kidneys, liver and other organs;
- Detachment of the placenta, leading to fetal hypoxia, slowing down its development, premature birth and perinatal pathologies.

In severe preeclampsia, the condition of a pregnant woman may become critical.
Features of preeclampsia treatment
For the diagnosis of preeclampsia, a number of laboratory blood and urine tests are prescribed, ultrasound is performed, an examination of the fundus and, if necessary, other examinations.
In case of mild late toxicosis of pregnant women, which is manifested only by edema, obstetrician-gynecologists recommend treatment in a day hospital or at home. If a pregnant woman also develops hypertension, protein is excreted in the urine, or other symptoms of pathologies appear, she may need to be hospitalized in an obstetric hospital.
Preeclampsia (Late toxicosis)
Gynecology
Preeclampsia or late toxicosis is a fairly common complication of pregnancy that occurs in the second half, is characterized by dysfunction of vital organs and systems and is the most common cause of severe complications for the mother, fetus and newborn. The causes of preeclampsia are varied, but in general they are explained by reflex changes in the vascular system and circulatory disorders - due to a violation of the hormonal regulation of the functions of vital organs and immunological incompatibility of maternal and fetal tissues.
The causes of preeclampsia are varied, but in general they are explained by reflex changes in the vascular system and circulatory disorders - due to a violation of the hormonal regulation of the functions of vital organs and immunological incompatibility of maternal and fetal tissues.
With gestosis, the functions of the brain, liver, and, especially, the kidneys are disturbed: from the appearance of protein in the urine to the development of acute renal failure. There are also pronounced changes in the placenta, which are the cause of a decrease in fetal-placental blood flow with the formation of chronic hypoxia and delayed fetal development.
Preeclampsia develops in several variants - as dropsy of pregnant women, nephropathy of pregnant women, preeclampsia and eclampsia. If it occurs in the absence of any other diseases, they speak of "pure preeclampsia". Against the background of already existing diseases (hypertension, diseases of the kidneys, liver, pathology of the endocrine system, disorders of fat metabolism), we are talking about combined preeclampsia.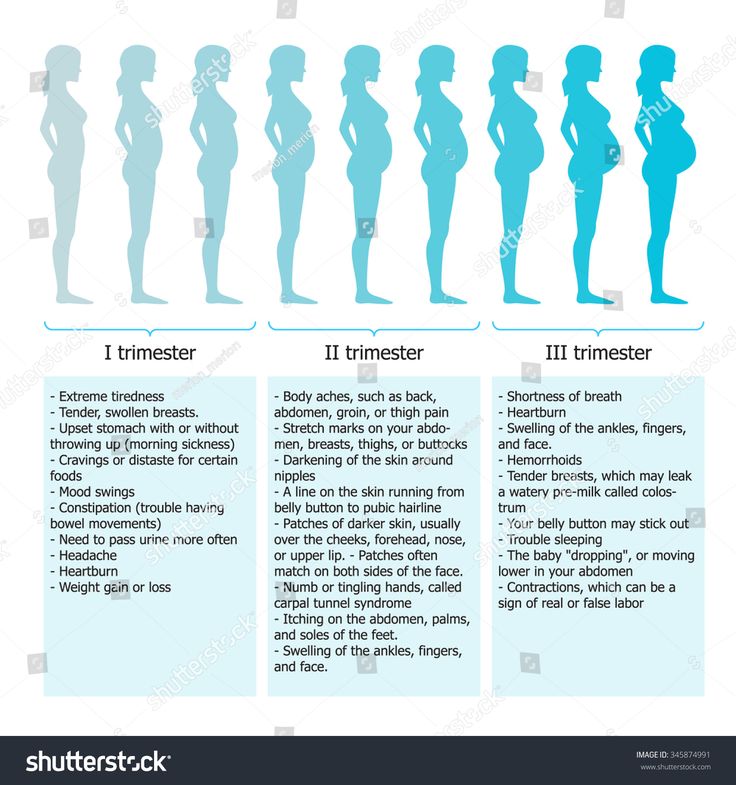
Dropsy of pregnancy, formed due to fluid retention in the body, is characterized by persistent edema and is one of the early manifestations of preeclampsia. Distinguish between hidden and obvious edema. Excessive or uneven weekly weight gain of a pregnant woman signals about hidden ones. Explicit (visible) edema is divided into degrees according to their prevalence: I degree - swelling of the legs, II degree - swelling of the legs and abdomen, III degree - swelling of the legs, anterior wall of the abdomen and face, IV degree - all the previous and the appearance of free fluid in the abdominal cavity (anasarca). Usually, swelling begins to form in the ankle area, gradually spreading higher. In the morning, they are less noticeable: during the night's rest, the fluid is redistributed throughout the body. Unfortunately, even with severe edema, the well-being of pregnant women often remains good, which is why a woman is in no hurry to see a doctor.
Nephropathy of pregnancy is characterized by a combination of three symptoms: the above-described edema, increased blood pressure (BP) and the presence of protein in the urine. However, only two of the three symptoms may be noted, in various combinations. Nephropathy usually develops against the background of dropsy preceding it. An increase in systolic blood pressure by 30 points from the initial one, and diastolic blood pressure by 15 and more points (on average, more than 140/95 mm Hg) testifies to arterial hypertension in pregnant women. Of particular importance is the increase in diastolic pressure and especially its sharp fluctuations. It is also necessary to assess the condition of the fundus vessels, which reflect the nature of cerebral circulation. A progressive increase in protein in the urine indicates a deterioration in the course of the disease, especially with a simultaneous decrease in the volume of urine excreted. The less urine is excreted and the longer the nephropathy, the worse the prognosis of the condition of both the pregnant woman and the outcome of her pregnancy. Nephropathy can progress to pre-eclampsia and then to eclampsia and cause severe dysfunction of vital organs.
However, only two of the three symptoms may be noted, in various combinations. Nephropathy usually develops against the background of dropsy preceding it. An increase in systolic blood pressure by 30 points from the initial one, and diastolic blood pressure by 15 and more points (on average, more than 140/95 mm Hg) testifies to arterial hypertension in pregnant women. Of particular importance is the increase in diastolic pressure and especially its sharp fluctuations. It is also necessary to assess the condition of the fundus vessels, which reflect the nature of cerebral circulation. A progressive increase in protein in the urine indicates a deterioration in the course of the disease, especially with a simultaneous decrease in the volume of urine excreted. The less urine is excreted and the longer the nephropathy, the worse the prognosis of the condition of both the pregnant woman and the outcome of her pregnancy. Nephropathy can progress to pre-eclampsia and then to eclampsia and cause severe dysfunction of vital organs.
Preeclampsia, in addition to the above triad of symptoms, is manifested by a feeling of heaviness in the back of the head, headaches, abdominal pain, nausea and vomiting. At the same time, memory impairments, insomnia or drowsiness, irritability or indifference and lethargy occur. These symptoms are due to impaired cerebral circulation. There is also a weakening of vision, flickering of "flies" or sparks and a "veil" before the eyes due to damage to the retina. BP with preeclampsia - 160/110 mm Hg. Art. and higher; protein content in urine - from 5 g per day or more; excreted urine per day - less than 400 ml.
Eclampsia is the most severe stage of gestosis, which, in addition to the symptoms characteristic of nephropathy and preeclampsia, is also manifested by seizures. The appearance of a convulsive seizure in eclampsia is most often provoked by external stimuli: bright light, sharp sound, pain, stressful situation. After the seizure, the patient lies unconscious for some time, and when consciousness returns, she does not remember anything about what happened, complains of headache and general weakness. It is very bad if such an unconscious state is not interrupted, but goes into the next seizure, which indicates cerebral edema. Less commonly, there is a non-convulsive form of eclampsia, in which the patient complains of severe headaches, darkening of the eyes. With this form of eclampsia, a pregnant woman can suddenly fall into a coma, and at the same time, a fatal outcome from a cerebral hemorrhage is quite possible.
It is very bad if such an unconscious state is not interrupted, but goes into the next seizure, which indicates cerebral edema. Less commonly, there is a non-convulsive form of eclampsia, in which the patient complains of severe headaches, darkening of the eyes. With this form of eclampsia, a pregnant woman can suddenly fall into a coma, and at the same time, a fatal outcome from a cerebral hemorrhage is quite possible.
Complications of preeclampsia are varied and very dangerous: heart failure and pulmonary edema, renal failure, hemorrhages in the adrenal glands, intestines, pancreas, spleen. The most typical and frequent complications are placental abruption and fetoplacental insufficiency, fetal hypoxia, neonatal asphyxia (up to fetal death).
Diagnosis of preeclampsia in our Clinic is based on an assessment of the anamnesis and complaints of the patient, the results of clinical and laboratory examinations. Ultrasound is also of great importance, in which the doctor, using doplerometry, will determine the state of the uterine, placental and fetal-placental blood flow. If necessary, additional consultations are held: therapist, nephrologist, neuropathologist, oklista.
If necessary, additional consultations are held: therapist, nephrologist, neuropathologist, oklista.
Treatment of preeclampsia is based on the creation of a therapeutic and protective regimen, maintaining and restoring the functions of vital organs, preventing and treating intrauterine hypoxia of the fetus and delaying its development, quick and careful delivery.
With dropsy of the 1st degree and the initial stage of nephropathy, it is possible to carry out treatment on an outpatient basis, for example, in the day hospital of the LeVita Clinic. With more severe dropsy, treatment is carried out in a hospital. And it is advisable to hospitalize pregnant women with severe nephropathy, preeclampsia, eclampsia in those hospitals that have an intensive care unit and a department for nursing premature babies. The duration of treatment is determined by the severity of preeclampsia and the condition of the fetus. The patient can be discharged from the hospital with recommendations to continue treatment under the supervision of an obstetrician-gynecologist.