Is sunlight good for babies
Knowledge and practice on adequate sunlight exposure of infants among mothers attending EPI unit of Aleta Wondo Health Center, SNNPR, Ethiopia | BMC Research Notes
- Research note
- Open Access
- Published:
- Asres Bedaso ORCID: orcid.org/0000-0001-7859-02641,
- Melese Gebrie1,
- Bedilu Deribe1,
- Mohammed Ayalew1 &
- …
- Bereket Duko1
BMC Research Notes volume 12, Article number: 183 (2019) Cite this article
-
68k Accesses
-
4 Citations
-
2 Altmetric
-
Metrics details
Abstract
Objective
The main objective of this study was to assess knowledge and practice of adequate sunlight exposure of infants among mothers attending EPI unit at Aleta Wondo Health Center, Sidama zone, SNNPR, Ethiopia. Institutional based descriptive cross sectional study design was used. 313 mothers who had under 1 year child and immunization follow-up were selected by simple random sampling technique using immunization registration book as sampling frame.
Result
Out of 313 respondents identified for the study 98.03% (n = 307) were responded for the interview. From the total respondents 279 (90.9%) of respondents exposed their infants to sunlight but only 62 (22%) of them exposed adequately. From 307 mothers, 191 (62.2%) are knowledgeable about sunlight exposure and 91 (32.6%) of mothers had good practice of exposing their infants to sunlight.
Introduction
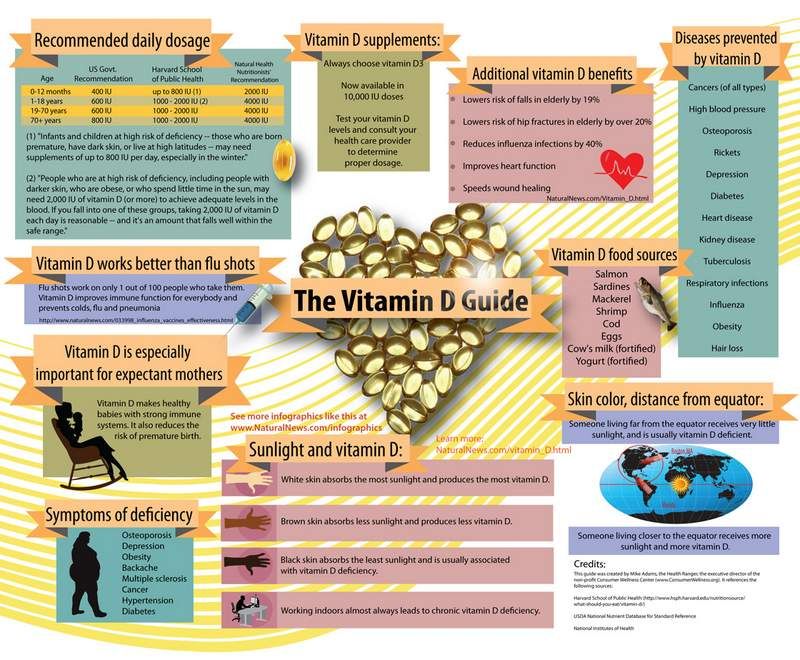
Sunlight exposure has a lots of health benefits for infants, it helps the body to produce vitamin D that helps the body to absorb calcium [1]. Also has a function of strengthening bones thereby preventing rickets in children and osteomalacia in adults and possibly inhibiting growth of some cancers [2]. Visible sunlight to the eyes gives health benefits through its association with timing of melatonin synthesis; maintenance of normal and robust cardiac rhythms and reduce the risk of seasonal affective disorder [3]. A daily requirement of vitamin D can be obtained by 30–60 min exposure to sunlight in the morning [4].
Visible sunlight to the eyes gives health benefits through its association with timing of melatonin synthesis; maintenance of normal and robust cardiac rhythms and reduce the risk of seasonal affective disorder [3]. A daily requirement of vitamin D can be obtained by 30–60 min exposure to sunlight in the morning [4].
It is important to limit the sun exposure between the hours of 10 a.m. and 4 p.m. for infants. In infants 1 week after birth the level of vitamin D is related to the level in their mothers during pregnancy [5]. The other source of vitamin D is from ingested diet and from supplements [6]. Adequate supplementation of vitamin D prevents low birth weight (LBW), birth asphyxia and deafness due to premature birth [7]. Studies worldwide identify lack of sun exposure as the main cause of rickets [8].
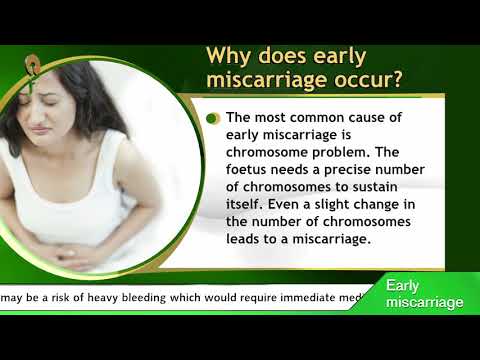
Rickets is a major public health problem in many countries of the world and it is common in children in Sub-Saharan African countries. Infants at risk of rickets are those whose mothers had poor vitamin D status during pregnancy and those exclusively breast-fed for a prolonged period with little skin exposure to ultraviolet B (UVB) [9]. Rickets is usually manifests as skeletal abnormalities, including frontal bossing, craniotabes, widening wrist, bowed legs and rachitic rosary [10]. The major causes of nutritional rickets in Ethiopia is lack of exposure to sunshine and inadequate intake of vitamin D [11].
Rickets is usually manifests as skeletal abnormalities, including frontal bossing, craniotabes, widening wrist, bowed legs and rachitic rosary [10]. The major causes of nutritional rickets in Ethiopia is lack of exposure to sunshine and inadequate intake of vitamin D [11].
Inadequate sunlight exposure of infants combined with nutritional rickets continues to be an evolving problem with several causes [12]. Nutritional rickets has received considerable attention from public health specialists in a number of developed countries. In developing countries, attention has been focused on rickets because of its effect on bone growth and mineral homeostasis and because of its association with increased infant and childhood mortality especially when accompanying lower respiratory tract infections [13, 14].
Primary deficiency is highly prevalent, even in countries with abundant sunshine, when skin exposure to UVB sunlight is limited by lifestyle and other factors. In Ethiopia, a review of rickets stated that the prevalence of rickets was highly as 40%, making it one of the highest in the world [15]. A study conducted in Kenyatta National Hospital showed that 58.8% of children aged 6 months develop rickets [16]. A recent study conducted in Kiambu District Hospital states that the prevalence of rickets in children 0–59 months to be 3.4% [17].
A study conducted in Kenyatta National Hospital showed that 58.8% of children aged 6 months develop rickets [16]. A recent study conducted in Kiambu District Hospital states that the prevalence of rickets in children 0–59 months to be 3.4% [17].
Until recently, little attention has been paid to the prevalence of rickets in most countries, but it is clear that rickets has been and remains a problem in Northern Asian countries, Middle East and in a number of countries in Africa [18]. A study done in Debre Markos 93% of mothers exposed their infants to sunlight but only 57.9% of them exposed daily [19]. A review of pediatric admissions in Jimma hospital, south western Ethiopia indicated that about 10% of children were diagnosed has rickets [20].
Mothers’ plays a key role in prevention of rickets by exposing their infants to sunlight adequately. Therefore, the objective of this study was to assess the knowledge and practice of adequate sunlight exposure of infants among mothers attending EPI unit at Aleta Wondo Health Center, Sidama zone, SNNPR, Ethiopia and fill the gap in these areas of concern.
Main text
Methods
Study design, area and period
An institutional based descriptive cross sectional study design was employed. Aleta Wondo is a town which is found in Sidama zone, SNNPR, Ethiopia. The town is located about 345 km away from Addis Ababa and 64 km from the regional capital city, Hawassa. This study was conducted from February 1 to April 30, 2018.
Source population and study participants
All mothers who attend EPI unit of Aleta Wondo health center for under one children EPI service were source population. All mothers who attend EPI unit of Aleta Wondo health center for under one children EPI service during the study period and fulfill the inclusion criterion were considered as study population.
Sample size determination and sampling technique
The sample size was calculated using a single population proportion formula by estimated prevalence of 54% taken from the study conducted in Debre Markos Town [19], with 5% marginal error (d) and confidence interval of 95% (Z α/2 = 1. 96). Based on these assumptions and adding 10% non-response rate, the total estimated sample size was 312.
96). Based on these assumptions and adding 10% non-response rate, the total estimated sample size was 312.
Regarding sampling, first, we selected one health center among all health centers through simple random sampling technique. Finally, simple random sampling technique was used to select the required number of participants among those who fulfill the inclusion criteria.
Inclusion and exclusion criteria
Mothers who attend EPI unit of Aleta Wondo health center for under one children EPI service were included in the study. Mothers who have difficulty of communication (hearing problem) were excluded from the study.
Data collection
Structured and pre-tested questionnaires were used to collect data. The questionnaire had four parts such as socio demographic related question, knowledge related question, practice related question and other determinant factors. The data was collected by trained nurses.
Data analysis
Data was entered and statistical analysis was carried out using SPSS version 20. The collected data were presented by frequency and percentage using tables, bar graph and pie charts. Mean and standard deviation was computed for numerical variables.
The collected data were presented by frequency and percentage using tables, bar graph and pie charts. Mean and standard deviation was computed for numerical variables.
Operational definitions
Adequate sunlight exposure: Those mothers who exposed their infants to sunshine at morning 8–10 a.m. for 15–30 min. Knowledgeable: those mothers who scored more than the mean value of response for knowledge related questions. Good Practice: Those mothers who scored more than the mean value of response for practice related questions.
Result
Socio demographic characteristics
All the required 313 study participants who came for EPI service at Aleta Wendo health center immunization clinic were interviewed with the response rate 100%. 144 (46.2%) of the respondents were between the ages of 22–27 years and 256 (82.1%) of their infants age were below 6 months. The mean age of the mothers and infants were 24 years and 4 months respectively (Table 1).
Table 1 Socio-demographic characteristics of mothers who attend EPI service in Aleta Wendo Health Center, Aleta Wondo Town, Southern Ethiopia, 2018 (N = 312)Full size table
Maternal information about the need of sunlight exposure of infants
Among the total respondents, majority 288 (92. 3%) of the mothers had information about the need of sunlight exposure for their infants and out of those mother who had information, half 148 (51.0%) of mothers got the information from neighbors/elders (Fig. 1).
3%) of the mothers had information about the need of sunlight exposure for their infants and out of those mother who had information, half 148 (51.0%) of mothers got the information from neighbors/elders (Fig. 1).
source of information about the need of sunlight exposure of infants among who attend EPI service in Aleta Wendo Health Center, Aleta Wondo Town, Sidama zone, SNNPR, Ethiopia, 2018 (n = 288)
Maternal
Full size image
Maternal knowledge about sunlight exposure of infants
From total respondents, 265 (84.9%) of mothers reported that sunlight exposure had positive benefit for infants and from those mothers. Majority, 157 (59.3%) of women’s indicated that sunlight exposure was useful to strength bone. In the other side, nearly half 152 (48.7%) of the study subjects indicated that sunlight exposure had negative or harmful effect on infant (Table 2).
Table 2 Knowledge status of mothers about sunlight exposure of their infants among who attend EPI service in Aleta Wendo Health Center, Aleta Wondo Town, Southern Ethiopia, 2018 (N = 312)Full size table
Mothers general knowledge about adequate sunlight exposure of infants
The mean score value of mothers who had knowledge about sunlight exposure was 6 out of the total score 10. More than half 196 (62.8%) of the study participants were knowledgeable about sunlight exposure (Additional file 1).
More than half 196 (62.8%) of the study participants were knowledgeable about sunlight exposure (Additional file 1).
Practice of mothers about sunlight exposure of infants
Out of the total respondents, 250 (80.1%) of mothers exposed their infants to sunlight. Among the reasons for not exposing their infants to sunlight, 62 (19.9%) of mothers said it is due to fear of cold and 19 (30.7%) responded due to fear of evil eyes (Additional file 2).
Age of infants for first sunlight exposure
From all mothers who exposed their infants to sunlight, 75 (30%) of mothers started exposing their infant to sun light at age of 45 days and above (Additional file 3).
Mothers general practice level about adequate sunlight exposure of infants
The mean score value of mothers who had practice of sunlight exposure of infants was 5 of the total score 10. More than half 145 (58%) of the study participants had good practice about adequate sunlight exposure (Additional file 4).
Discussion
In the current study, more than half (62.8%) of the mothers were knowledgeable about of sunlight exposure for infants. In addition most of mothers (84.9%) had awareness of the positive health benefit of sunlight exposure for infant and majority of them (59.3%) indicated sunlight exposure as the most important source of vitamin D used for growth and strength of bone through mobilization of calcium in the body. Also, 65.4% of the mother had awareness about the effect of inadequate or absence of sunlight exposure in health status that leads to rickets. This finding was consistent with the study done in Turkey which indicated that exposure of infant for sunlight was beneficial for bone development, diaper rash and neonatal jaundice [21].
Concerning the health risk of solar UV radiation exposure, nearly half (48.7%) of mothers believed that sunlight exposure had negative health effect as a result of improper time and duration of exposure, such as skin cancer and sun burn. This idea was also supported with a review of research done in Germany on the challenges resulting from positive and negative effects of sunlight [22]. This indicated that most of the mothers do not have enough information about healthy sun bathing and its effect since sun bathing might be also useful for treating neonatal jaundice, dipper rash and prevention of vitamin D deficiency related conditions like hypertensions, cardiovascular disease and bone disease etc [23].
This idea was also supported with a review of research done in Germany on the challenges resulting from positive and negative effects of sunlight [22]. This indicated that most of the mothers do not have enough information about healthy sun bathing and its effect since sun bathing might be also useful for treating neonatal jaundice, dipper rash and prevention of vitamin D deficiency related conditions like hypertensions, cardiovascular disease and bone disease etc [23].
Regarding practice of sunlight exposure, 58.0% of the study participants had good practice about adequate sunlight exposure who score more than or equal to mean score value. However, majority (80.1%) of mothers were exposed their infants to sunlight. This finding was lower than similar study done in Debre Markos Town of Ethiopia which was 93% [19]. The reason for the difference might be the difference in socio cultural factors like fear of illness, fear of evil eyes and witchcraft and level of appropriate information concerning sunning the baby.
In this study, only 17.6% of mothers were started sun light exposure of their infants between 0–15 days of neonatal life, which was lower than similar study done in Debre Markos town of Ethiopia which was 24% [19]. However, 67.6% of mothers of this study were sunning their babies at daily which was better than the study done at Debre Markos town of Ethiopia which was 57.9% [19]. In addition, more than half (63.6%) of the mothers exposed their babies in outdoor which were lower than the similar study done previously at Debre Markos town which was 89.4% [19].
Most of mothers (90.0%) were exposed their babies between the time range of 8–10 a.m. in this study, but 54.8% and 26.8% of mothers were sunning their babies without sun screening or clothing and with time duration of 15–30 min as recommended, respectively. This finding was slightly lower than the study done at Debre Markos on exposing without sun screening and time of exposure which accounts 57.3% and 99.1%, respectively; whereas, its higher on duration of exposure which accounts 25. 5% [19]. This study finding was also incomparable with similar study done in Dale woreda of Southern Ethiopia as shown that 41.1% of the mothers exposed their child to sunlight within 1 month of birth [24].
5% [19]. This study finding was also incomparable with similar study done in Dale woreda of Southern Ethiopia as shown that 41.1% of the mothers exposed their child to sunlight within 1 month of birth [24].
Most of the children were exposed to sunlight for 20 to 30 min per day. About 49.4% were exposed to sunlight for 7 days in a week and 90.0% children were exposed to sunlight without clothing.
In this study, most of the mothers (90.8%) were used lubricants to be applied on their infant’s body when exposed to sunlight. Beside this, 41.4% of mothers were applied lubricants during the time of sunlight exposure, and followed by mothers who were applied lubricant after sunlight exposure which accounts 38.7%. This finding was lower than the same study done at Debre Markos town as shown that most (98.4%) of respondents applied lubricants on the baby’s body at the time of sunlight exposure and majority (70.6%) of mothers apply during sunlight exposure [19].
Conclusion
Although majority of the respondents have good knowledge about importance of sunlight exposure for the infants but there is a gap on time to start sunlight exposure and time to stay on sunlight while exposing.
Limitation of the study
Since the study is cross sectional it does not show cause and effect relationship between dependent and independent variables.
Abbreviations
- CI:
-
confidence interval
- EPI:
-
expanded program immunization
- LBW:
-
low birth weight
- SNNPR:
-
Southern Nations Nationality and Peoples Region
- SPSS:
-
Statistical Package for Social Science
- UV:
-
ultra violet
References
Reed K. 7 health benefits of direct sunlight to new born babies. Positive health wellness.
 2017. https://www.positivehealthwellness.com/diet-nutrition/7-health-benefits-direct-sunlight-newborn-babies/.
2017. https://www.positivehealthwellness.com/diet-nutrition/7-health-benefits-direct-sunlight-newborn-babies/.Horsley T, Cranney A, Donnel SO, Weiler H, Puil L, Ooi D. Effectiveness and safety of vitamin D in relation to bone health. Agency Healthc Res Qual. 2007;158:1–235.
Google Scholar
Mead MN. Benefits of sunlight a bright spot for human health. Environ Health Perspect. 2008;116:160–7.
Google Scholar
Teotia M, Teotia PS. Endemic flourosis and calcium deficiency interaction syndromes. In: Teotia PS, Teotia M, editors. Nutritional and metabolic bone and stone disease, 1st edition. New Delhi: CBS publisher and distributions; 2008. p. 361–67.
Nesby OD. Hypovitaminosis D prevalence and determinants among africanamerican and white women of a reproductive age. Am J Clin Nutr.
 2002;76:3–4.
2002;76:3–4.Article Google Scholar
Calvo SM, Whiting J, Barton NS. Vitamin D intake: global perspective of current status. J Nutr. 2005;135:310–6.
Article CAS Google Scholar
Mahendra TK, Vivek T. Roll of vitamin D prevention of deafness. Indian J Otol. 2012;18:55–7.
Article Google Scholar
Holick MH. Vitamin D deficiency. N Eng J Med. 2007;357:266–81.
Article CAS Google Scholar
Anthony N, Roger BDB. Nutritional rickets around the world. J Steroid Biochem Mol Biol. 2013;136:201–6.
Article Google Scholar
Fukumoto S, Ozono K, Michigami T, Mingawa M, Okazaki R, Sugimoto T, Matsumoto T.
 Pathogenesis and diagnostic criteria for rickets and osteomalacia—proposal by an expert panel supported by ministry of health, labour and welfare. Jpn Endocr Soc Endocr J. 2015;62(8):665–71.
Pathogenesis and diagnostic criteria for rickets and osteomalacia—proposal by an expert panel supported by ministry of health, labour and welfare. Jpn Endocr Soc Endocr J. 2015;62(8):665–71.CAS Google Scholar
Woldemichael K, Berhanu N. Magnitude and pattern of injury in Jimma University Specialized Hospital, South West Ethiopia. Ethiop J Health Sci. 2011;21(3):155–65.
PubMed PubMed Central Google Scholar
Creo AL, Thacher TD, Pettifor JM, Strand MA, Fischer P. Nutritional rickets around the world: an update. Paediatr Int Child Health. 2017;37(2):84–988.
Article Google Scholar
Ganmaa D, Stuart JJ, Sumberzul N, Ninjin B, Giovannuci E, Kleinman K, Rich-Edwards JW. Vitamin D supplementation and growth in urban Mongol school children: results from two randomized clinical trials.
 PLoS ONE. 2017;12(5):e0175237.
PLoS ONE. 2017;12(5):e0175237.Article Google Scholar
Thacher TD, Fischer PR, Strand MA, Pettifor J. Nutritional rickets around the world: causes and future directions. Ann Trop Paediatr. 2006;26:1–16.
Article Google Scholar
Prentice A. Vitamin D deficiency: a global perspective. Nutr Rev. 2008;66:S153–S164164.
Article Google Scholar
Oyatsi DP, Musoke RN, Wasunna A. Incidence of rickets of prematurity at Kenyattav National Hospital, Nairobi. East Afr Med J. 1999;76(2):63–6.
CAS PubMed Google Scholar
Theuri Alice W. Factors associated with rickets among children aged 0-59 months at Kiambu District Hospital. Kenya: University of Nairobi research archive; 2012.
 p. 16–22. http://erepository.uonbi.ac.ke:8080/xmlui/handle/123456789/6793.
p. 16–22. http://erepository.uonbi.ac.ke:8080/xmlui/handle/123456789/6793.Pettifor MJ. Nutritional rickets and vitamin D deficiency in nutrition and health in developing countries. 2nd ed. Totowa: Humana Press; 2008. p. 435–454.
Book Google Scholar
Abate A, Murugan R, Gualu T. Assessment of practice and factors affecting sunlight exposure of infants among mothers attending governmental health facilities in Debre Markos town, East Gojjam, Ethiopia. Am J Nurs Sci. 2015;5(1):30–6.
Article Google Scholar
Kenenisa C, Ewnetu H, Sime H. Retrospective analysis of prevalence of rickets and associated factors among children admitted to pediatric ward in Jimma University specialized hospital. J Pediatr Neonatal Care. 2014;1(7):00044.
Google Scholar
Aladag N, Filiz TM, Topsever P, Gorpelioglu S. Parents' knowledge and behaviour concerning sunning their babies; a cross-sectional, descriptive study. BMC Pediatr. 2006;6(27):1–6.
Google Scholar
Reichrath J. The challenge resulting from positive and negative effects of sunlight: how much solar UV exposure is appropriate to balance between risks of vitamin D deficiency and skin cancer? Progress Biophys Mol Biol. 2006;92:9–16.
Article CAS Google Scholar
Zhang X, Ding F, Li H, Zhao W, Jing H, Yan Y, Chen Y. Low serum levels of vitamin D and are associated with recurrent respiratory tract infections in children living in northern China: a case control study. PLoS ONE. 2016;11(12):e0167689.
Article Google Scholar
Tezera F, Whiting SJ, Gebremedhin S.
 Dietary calcium intake and sunlight exposure among children aged 6–23 month Sin Dale Woreda, Southern Ethiopia. Afr J Food Agric Nutr Dev. 2017;17(3):12427–400.
Dietary calcium intake and sunlight exposure among children aged 6–23 month Sin Dale Woreda, Southern Ethiopia. Afr J Food Agric Nutr Dev. 2017;17(3):12427–400.Article CAS Google Scholar
Download references
Authors’ contributions
AB, MG participated in the conception, design of the study, reviewing proposal and data analysis. AB, MG, BD, MA and BD participated in reviewing proposal and writing the research report. AB prepared the manuscript for publication. MG and BD have participated in supervising and editing manuscript. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank study participants and data collectors for their unreserved contribution.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data are included in this article and its supporting document.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Ethical clearance was obtained from ethical review board of Hawassa University, College of Medicine and health sciences. All participants of the study provided with a written consent, clearly stating the objectives of the study and the right of study participants. All participants were randomly selected without any discrimination and filled out questionnaires were carefully handled and all access to results kept strictly.
Funding
No funding was received for this research work.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
College of Medicine and Health Sciences, School of Nursing, Hawassa University, Hawassa, Ethiopia
Asres Bedaso, Melese Gebrie, Bedilu Deribe, Mohammed Ayalew & Bereket Duko
Authors
- Asres Bedaso
View author publications
You can also search for this author in PubMed Google Scholar
- Melese Gebrie
View author publications
You can also search for this author in PubMed Google Scholar
- Bedilu Deribe
View author publications
You can also search for this author in PubMed Google Scholar
- Mohammed Ayalew
View author publications
You can also search for this author in PubMed Google Scholar
- Bereket Duko
View author publications
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Asres Bedaso.
Additional files
Additional file 1.Distribution of maternal general level of knowledge about sunlight exposure of their infants based of knowledge score among who attend EPI service in Aleta Wendo Health Center, Aleta Wondo Town, Southern Ethiopia , 2018 (n = 312).
Additional file 2.Practice of mothers on adequate sunlight exposure of their infants among who attend EPI service in Aleta Wendo Health Center, Aleta Wondo Town, Southern Ethiopia, 2018 (N = 250).
Additional file 3.Age of infants who sunlight exposure among mothers who attend EPI service in Aleta Wondo Health Center, Aleta Wondo Town, Southern Ethiopia , 2018 (N = 250).
Additional file 4General Practice of mothers among who expose their infants to sunlight and who attend EPI service in Aleta Wendo Health Center, Aleta Wondo Town, Sidama Zone, Southern Ethiopia, 2018 (n = 250).
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4. 0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Reprints and Permissions
About this article
Sun Safety for Children and Babies | Patient Education
Melanoma is among the most common forms of cancer for young adults 15-29. Some experts blame the inappropriate use of sunscreen, saying that people do not apply enough lotion (a golf ball-size dollop) or do not reapply it as frequently as required. Products can no longer claim to be waterproof, only water-resistant, and labels must note a time limit of either 40 or 80 minutes before the sunscreen is ineffective.
Sunscreen is just one of the defenses against the harmful effect of UV radiation. Strategies such as seeking shade and dressing children in sun-protective clothing are just as important. A bad sunburn in childhood or adolescence doubles the risk of melanoma later in life, according to the Skin Cancer Foundation.
Rates of skin cancer—including melanoma, the most serious form of skin cancer—continue to rise, even in young people. Parents need to be extra vigilant about sun protection all the time. Just one blistering sunburn in childhood more than doubles a person's chances of developing melanoma later in life. Young skin is delicate, thinner, and produces less melanin, a skin protecting pigment. Ultra violet (UV) rays reach the skin’s pigment producing melanin cells, called melanocytes, and cause DNA damage to the skin.
Infants
0-6 months:
- Infants under 6 months of age should be kept out of direct sunlight.
- Avoid using sunscreen.
 Baby’s young skin doesn’t have the ability to metabolize and excrete chemicals often found in sunscreens.
Baby’s young skin doesn’t have the ability to metabolize and excrete chemicals often found in sunscreens. - Dress baby in lightweight sun—protective clothing that breathes and covers the arms and legs.
- Always protect your baby’s head, face, ears, and neck with a wide-brimmed hat. A baby who wears a hat during the first few months will get used to having it on.
- Use stroller shades and umbrellas.
- Use removable mesh window shields to keep direct sunlight from coming in through the windows of your car or invest in UV window film, which can screen almost 100 % of ultraviolet radiation without reducing visibility.
- Use sunglasses with UVA/UVB protection. Eyes are affected by exposure to the rays of UV radiation. Overexposure to UV light contributes to the development of cataracts, retinal damage and other eye problems. Experts report that as much as 80% of UV damage to our eyes is done before the age of 18, making it even more important all of us to start protecting our eyes at an early age.

- Take walks early in the morning before 10 AM or after 4 PM and use a stroller with a sun—protective cover.
Babies
6-12 months:
- It's now safe to use sunscreen on babies. Choose sunscreen designated for infant skin, and one that won't sting baby's eye.
- All the protection methods explained above still apply, however now sunscreen use should be incorporated.
- Apply broad-spectrum sunscreen with a minimum SPF of 30, with UVA/UVB protection particularly to areas left uncovered such as baby's hands. Some children experience allergic reactions to various sunscreen ingredients. Test a product first by applying a small amount to a limited area of skin. Choose a product that is hypoallergenic and fragrance-free.
- Most importantly, sunscreen must be applied 30 minutes before going outside and reapplied every two hours or after swimming or excessive sweating. Products can no longer claim to be waterproof, only water-resistant, and labels must note a time limit of either 40 or 80 minutes before the sunscreen is ineffective.

Toddlers/Pre-School Age
- Protecting toddlers from the sun requires a little more thought and effort. It is important to educate your child and caregivers.
- All the protection methods explained above still apply, including how sunscreen use should be incorporated
- Make sure your child seeks the shade between 10 AM and 4 PM. Check the outdoor area where your child plays to make sure there is adequate shade.
- Make sure toddlers are covered. Long-sleeved, unbleached cotton clothing is cool and comfortable, while also highly protective. Clothing with an Ultraviolet Protection Factor (UPF) listing on the label offers extra security. The Skin Cancer Foundation recommends clothing with a UPF of 30 or higher.
- Don't forget hats and sunglasses. Choose a wide—brimmed hat that protects face, neck, and ears.
Pigmentation
Whatever our skin color, we're all potentially susceptible to sunburn and other harmful effects of exposure to UV radiation. Although we all need to take precautions to protect our skin, people who need to be especially careful in the sun are those who have.
Although we all need to take precautions to protect our skin, people who need to be especially careful in the sun are those who have.
- pale skin
- blond, red, or light brown hair
- been treated for skin cancer
- a family member who's had skin cancer
Sunglasses
Children under age 10 are at a high risk for skin and eye damage from UVR. The skin on their eyelids and around their eyes is more delicate and vulnerable than adult skin. And until about age 10, the lens of a child's eye is clear, allowing greater solar penetration and thus greater UVR—induced ocular changes.
Retinal exposure to UVR is associated with cataracts and macular degeneration, both causes of vision impairment. UVR damage builds over time, so the sooner you start protecting your children's eyes from the sun, the lower their risk will be of ever developing future eye problems.
Fortunately, good sunglasses protect both the skin around the eye and the eye itself. While children under 6 months old should never be exposed to the sun, once they reach 6 months, they should wear sunglasses outside. If they require prescription glasses, they should also wear prescription sunglasses.
While children under 6 months old should never be exposed to the sun, once they reach 6 months, they should wear sunglasses outside. If they require prescription glasses, they should also wear prescription sunglasses.
Keep these rules in mind when buying sunglasses for children:
- Find glasses that block 99-100 percent of both UVA and UVB rays. Buy ones that indicate the percentage of UVR protection they provide. The more skin covered, the better, so look for large, wraparound styles.
- Use playground-proof lenses. Kids run, trip, fall, and bounce off objects at alarming speed. Their sunglasses should match this active lifestyle. Find impact-resistant, scratch-proof lenses that don't pop out of the frames. Avoid glass lenses, unless recommended by a doctor; plastic is safer. Frames should be bendable but unbreakable. Make sure the glasses fit snugly, close to the face.
"Sun Protective” Clothing
Clothing is the single most effective form of sun protection. It is our first line of defense against the sun’s harmful ultraviolet rays.
It is our first line of defense against the sun’s harmful ultraviolet rays.
Clothing made with sun-protective fabrics differs from typical summer fabrics in several ways. They typically have a tighter weave or knit and are usually darker in color. Sun-protective clothes have a label listing the garment's Ultraviolet Protection Factor (UPF) value. The UPF label will help you identify sun-protective garments. The number on the label indicates what fraction of the sun’s rays can penetrate the fabric. The higher the UPF, the higher the protection.
A fabric with the minimum recommended UPF rating of 20 allows 1/20th of the sun's UV radiation to pass through it. This means that this fabric will reduce your skin's UV radiation exposure by 20 times where it's protected by the fabric. The more intense the hue, the better the UV defense—dark or bright colors, like red or black, absorb more UVR than white.
What is SPF?
SPF, or Sun Protection Factor, is the amount of UV radiation required to cause sunburn on skin with the sunscreen on, relative to the amount required without the sunscreen. SPF protection doesn't increase proportionally. For example, SPF 2 absorbs 50% of UV radiation, SPF 15 absorbs 93%, and SPF 34 absorbs 97%.
SPF protection doesn't increase proportionally. For example, SPF 2 absorbs 50% of UV radiation, SPF 15 absorbs 93%, and SPF 34 absorbs 97%.
What is UVA & UVB?
UVA and UVB refer to different kinds of ultraviolet radiation. Exposure to UVA and UVB can be harmful and cause cancer. Sunscreens protect from UVB rays, but not all sunscreen product screens out all UVA rays. Some may advertise UVA protection, but no criteria exist in the U.S. for measuring and labeling the amount of UVA defense a sunscreen provides yet.
What is Broad-spectrum protection?
“Broad-spectrum” indicates that a product shields against UVA and UVB. It does not guarantee protection against all UVA wavelengths, however. Most broad-spectrum sunscreens and sunblocks with an SPF of 30 or higher do a good job against UVB and short UVA rays. If they also contain avobenzone, zinc oxide, or titanium dioxide, they should be more effective against the entire UVA spectrum.
Tips on Applying Sunscreen
- Water and perspiration reduce the SPF value of many sunscreens—even those that are water-resistant—so be sure to reapply the product often.

- Sunscreen sprays may not work as well to prevent sunburn. The concern is twofold: that not enough sunscreen makes it onto the skin, and that the spray may be inhaled into the lungs.
- If your baby is taking medication, ask your doctor or pharmacist if the medications increase your baby’s skin sensitivity to the sun or aggravate sunburns or rashes. Certain antibiotics, diuretics, antihistamines, and antidepressants are among the commonly used drugs that can increase sensitivity to the sun's rays.
- Experts estimate that about half of the recommended amount of sunscreen is applied on their children. Read the product’s usage instructions to make sure you are using the proper amount.
- Apply sunscreen at least 30 minutes before your child will be exposed to the sun.
- Reapply sunscreen regularly and at least every 2 hours. Repeat application more often if your child is swimming or sweating.
- Use sunscreen even if it is cloudy outside. Clouds don't absorb or block UV radiation.

Sun Exposure & Vitamin D
Some sunlight is good for you and is needed for bone health. It has been suggested by some vitamin D researchers that approximately 5 to 30 minutes of sun exposure at least twice a week to the face, arms, legs, or back without sunscreen usually lead to sufficient vitamin D. Individuals with limited sun exposure need to include good sources of vitamin D in their diet or take a supplement to achieve recommended levels of intake.
sunbathing precautions
The question of the effect of sunlight on the children's body traditionally arises in the period of late spring - early summer. We will not stay away from heated discussions and try to figure out once again what the benefits and harms of the sun are for humans.
The level of solar radiation has been increasing in the last few decades due to the thinning of the ozone layer. This leads to general health problems and even to the development of serious diseases. At the same time, it is widely believed that sunbathing has a positive effect on immunity and increases the child's resistance to colds. So how exactly is the sun useful, and what is the harm? Let's figure it out.
So how exactly is the sun useful, and what is the harm? Let's figure it out.
Benefits of the sun for children and adults
- The positive effect of sunlight on humans has been scientifically proven. The sun contributes to the production of serotonin - the “hormone of happiness”, which is responsible for raising mood, reducing stress levels.
- Antiseptic properties of sunlight - the skin becomes cleaner under their influence, acne and dermatoses of various origins decrease (or disappear altogether).
- Sleep normalization. The sun regulates the production of a special substance - melatonin, which is responsible for maintaining the human biological rhythm.
- The sun triggers the synthesis of vitamin D, an extremely useful trace element for the healthy development of a child. It participates in mineral metabolism and “directs” calcium to connective bone tissue. Vitamin D deficiency increases the risk of rickets.
- Vitamin D Boosts Immunity: Pediatricians often note a link between low levels of the vitamin in children and frequent illnesses during the fall and winter.

However, you don't have to spend too much time in the sun to get enough vitamin D. In summer, spending a few minutes a day outdoors is enough. In less sunny seasons - a little longer. You don't have to sunbathe. Playing ball in the yard or a walk in the park will raise your vitamin D levels just as well.
Sun damage to humans
The sun is harmful to health with ultraviolet radiation - UVA and UVB rays. They affect the skin in different ways. More harmful UVA (long) rays cause premature aging and neoplasms on the skin, UVB (medium) is the main cause of burns.
Eyes
Excessive UV radiation causes damage to the cornea of \u200b\u200bthe eye (photokeratitis), which destroys the skin of the eyelids, the ocular mucosa, the iris, and the lens. Possible loss of visual acuity. It is worth remembering that the eyes of a child are more vulnerable than those of an adult - a child's lens transmits up to 75% of harmful UVA rays, while in an adult no more than 10% of the rays "pass" through the lens.
Overheating
Children, playing on the beach or chasing a ball in the yard, do not immediately notice the poor health caused by overheating. This is a failure in the life of the body due to a violation of water and salt metabolism. The malaise is accompanied by fever, sweating, headache, dizziness, weakness, nausea.
The extreme degree of overheating is heat stroke with an extremely high body temperature (up to 41 ◦ C), with loss of consciousness, confused speech. In our article on heat stroke in a child, we talk in detail about the causes of this condition, the symptoms, and how to provide first aid for heat stroke.
Sunburn
The child, due to the unformed light-protective layer of the skin, is especially sensitive to sunlight and can get burned - an inflammatory reaction of the skin to thermal energy. The burn is accompanied by reddening of the skin, burning, and with a strong lesion, blisters appear.
Heat rash (prickly heat)
With strong heating of the body, clogging of the pores on the skin and sweating delay provoke the appearance of a rash (pimples, blisters). The rash usually appears on the neck, elbows, chest, in the area between the shoulder blades, in the groin area. Infants and children are more prone to prickly heat because the pores on their skin are not as enlarged as in adults. Special powders help relieve symptoms and return the skin to a healthy state. For example, Powder-cream My Sunshine® will dry the skin, relieve itching and redness.
The rash usually appears on the neck, elbows, chest, in the area between the shoulder blades, in the groin area. Infants and children are more prone to prickly heat because the pores on their skin are not as enlarged as in adults. Special powders help relieve symptoms and return the skin to a healthy state. For example, Powder-cream My Sunshine® will dry the skin, relieve itching and redness.
Melanoma
The sun interferes with the functioning of skin cells. Especially heavy damage is caused by UV rays to children's thin skin, it has a lot of actively dividing stem cells. They are the main target for damage by ultraviolet rays. Sunburn in childhood significantly (according to some sources, almost twice) increases the risk of developing melanoma throughout life.
Precautions to take while sunbathing
It turns out that in order to get the maximum benefit from the sun, you need to properly protect yourself. We remember this paradox, as well as recommendations that are universal for adults and children:
Safe time for sunbathing
Refrain from walking during the hours of maximum solar activity. Older children and prudent adults should avoid the sun from 11:00 am to 4:00 pm. At this time, it is better to hide in the shade or just stay at home. And babies up to six months (and sometimes up to a year) should not be in direct sunlight at all.
Older children and prudent adults should avoid the sun from 11:00 am to 4:00 pm. At this time, it is better to hide in the shade or just stay at home. And babies up to six months (and sometimes up to a year) should not be in direct sunlight at all.
Proper clothing and accessories for sun protection
The main summer accessory is a headdress. It can be a wide-brimmed hat or special baseball caps that cover not only the face, but also the ears with the neck and shoulders.
Another fashion accessory is sunglasses. Choose models with glasses that reflect UV rays (look for the corresponding mark on the glasses). And the choice of color, shape and design can be entrusted to the child.
From clothes, spacious T-shirts, shirts and trousers made of natural fabrics in light shades are perfect. Summer is the time to dress your baby in white and beige.
Recently, sun protection clothing has been gaining popularity. It provides additional protection against ultraviolet radiation due to special impregnation and special weaving of threads. Clothing made from such fabrics is marked with UPF marking - a letter designation on the label and a UPF coefficient of 30 and higher. Sun protection T-shirts and overalls are a great solution for playing in the water, they provide good protection for the back, shoulders and chest.
Clothing made from such fabrics is marked with UPF marking - a letter designation on the label and a UPF coefficient of 30 and higher. Sun protection T-shirts and overalls are a great solution for playing in the water, they provide good protection for the back, shoulders and chest.
Shoes are rarely seen as protection from the sun, and this is wrong. The sun threatens the upper surface of the foot no less than the nose. Therefore, it is better to choose sandals that will cover this sensitive area.
Special skin protection: how to choose the right product?
Sunscreens are a real summer must have, and you can’t do without them.
In no case do not use adult sunscreen cosmetics for children, choose only children's. Pay attention to age restrictions.
A good modern cosmetic should contain filters that block UVA and UVB rays. Pay attention to the following indicators, and do not confuse them, please:
- SPF is the main characteristic of the protective ability of a cosmetic product.
 But only from UVB rays! The higher the SPF, the stronger the UVB protection.
But only from UVB rays! The higher the SPF, the stronger the UVB protection. - PPD - UVA protection rating. The maximum value of this indicator is 42. The minimum value for serious protection is 8. Sometimes they also use the Japanese system and the PA scale with “+” signs after the letters (PA +++, at least three “+”).
Protection factor SPF choose products according to the phototype of the child. The lighter the skin and eyes, the more protection will be required. You can reduce the degree of protection after a few days of exposure to the sun, when the skin adapts. Blue-eyed blondes need a high protection factor, from SPF 50+. For them, a cream from the My Sunshine® series of sunscreens with protection factor SPF 50+, which was created specifically for children, is suitable. Allowed from 12 months.
Dark-eyed brunettes first need SPF 30, and after a week at the sea or in the country, twenty will do. Pay attention to Moe Sunshine® SPF 30 and 20 creams, SPF 30 spray.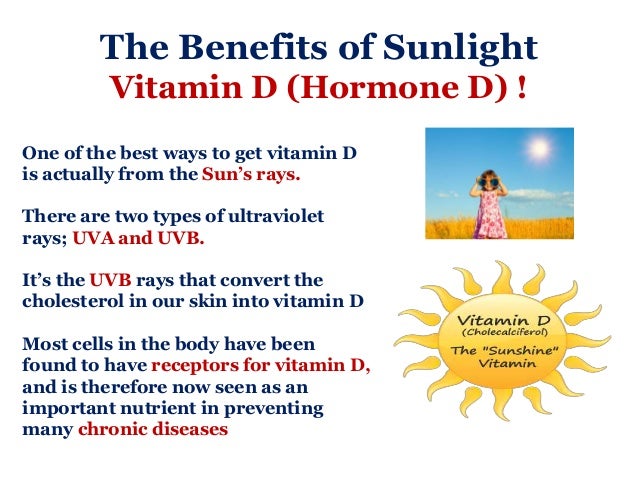 The products of this sunscreen series include safe sunscreens, natural plant ingredients and vitamin E, which carefully protect delicate baby skin from harmful UVA and UVB rays. For ease and convenience of application, sun spray SPF 30 is suitable, which is quickly absorbed and contains an additional moisturizing and protective component - D-panthenol.
The products of this sunscreen series include safe sunscreens, natural plant ingredients and vitamin E, which carefully protect delicate baby skin from harmful UVA and UVB rays. For ease and convenience of application, sun spray SPF 30 is suitable, which is quickly absorbed and contains an additional moisturizing and protective component - D-panthenol.
Choose waterproof products. Creams My Sunshine® will not wash off with water and will survive several baths. Do not forget to renew the product every two hours, and if the baby sweats or bathes for a long time, even more often. Apply the cream liberally, this is the case when the amount matters.
Creams are good, but don't forget the My Sunshine® sunscreen lip balm. It can be applied to the sensitive T-zone (forehead and nose) as well as to the top of the cheeks for extra protection.
If the child has been in the sun for too long or you notice the first signs of a sunburn (redness of the skin, soreness of damaged areas), use the gel and after-sun milk My Sunshine®. The gel contains aloe vera extract, panthenol and allantoin, which help to instantly cool the skin and relieve discomfort. Milk with the addition of plant extracts and a complex of vitamins softens and moisturizes the affected areas.
The gel contains aloe vera extract, panthenol and allantoin, which help to instantly cool the skin and relieve discomfort. Milk with the addition of plant extracts and a complex of vitamins softens and moisturizes the affected areas.
All products of the "solar" series are designed specifically to care for delicate baby skin and are recommended by pediatricians for use from 3 months or from 1 year.
Misconceptions about the properties of ultraviolet rays
- All sunbeams are the same.
- What is the use of the sun if sunscreen cosmetics block the production of vitamin D
- Even a small amount of sunscreen helps to effectively protect the skin.
- The higher the protection factor of the cream, the less often it needs to be renewed.
- Organic (mineral) sunscreens are not safe for children.
Well, in the end, we will dispel five common ideas about the effects of the sun on the human body, which are far from the truth.
The main negative effect of the sun on the human body comes from ultraviolet or UV rays, namely from UVA and UVB rays. They cause various skin problems. UVA provoke skin melanoma, enlargement and change of moles and premature aging, UVB cause skin burns. They need protection from them.
Sunscreen cosmetics prevent the harmful effects of UVA and UVB rays, and do not affect the synthesis of vitamin D. Under sunscreen, vitamin D is produced without any risk to the skin.
Under sunscreen, vitamin D is produced without any risk to the skin.
For effective protection, the skin of the child must be covered with such a layer of cream that there are no gaps and poorly treated areas. Apply enough cream. If you are using a spray, apply it several times to create a dense coverage on the skin.
Regardless of the level of SPF cream, it must be renewed every two hours, and if the child sweats a lot or bathes for a long time, even more often.
Organic filters absorb the sun's rays due to their chemical composition. Some of the components may be absorbed into the skin, however, there is no confirmed information about side effects.
In our article "Sunscreen Myths for Kids" we continue to uncover the topic, debunk fears and "blind spots" of ignorance about the effect of sunscreens.
#development #tips #skin protection from the sun
Share article
‹Previous ›Next
We also recommend reading
Myths about sunscreens
Heat stroke in a child: symptoms and first aid
Sunscreen: what and how to choose?
Best after sun product for kids
Related products
Sun cream SPF 50+
55 ml
Sun cream SPF 30
55 ml
After Sun Gel
100 ml
Sun Protection Lip Balm SPF 15
2. 8 g
8 g
The benefits and harms of the sun for children's skin
June 12, 2019
Due to the established hot and sunny weather in the Children's City Polyclinic No. 7, Anna Yuryevna Mykalo, a pediatrician from the office of a healthy child, conducted a lecture for 23 young mothers on the topic: do children need a tan ? The benefits and harms of the sun for children's skin.
On hot summer days, you want to walk with your baby for as long as possible. But at the same time, the mother must ensure that the child does not burn.
According to scientific research, about 80% of the total amount of solar exposure during a person's life occurs in the first 18 years of life. Since such damage to children's skin as photoaging, the destruction of collagen and elastin is irreversible, it is very important to protect the skin of a child from the sun from the very first days of his birth.
Sun protection for children
Research by scientists has also shown that children need sun protection not only on a clear, cloudless day.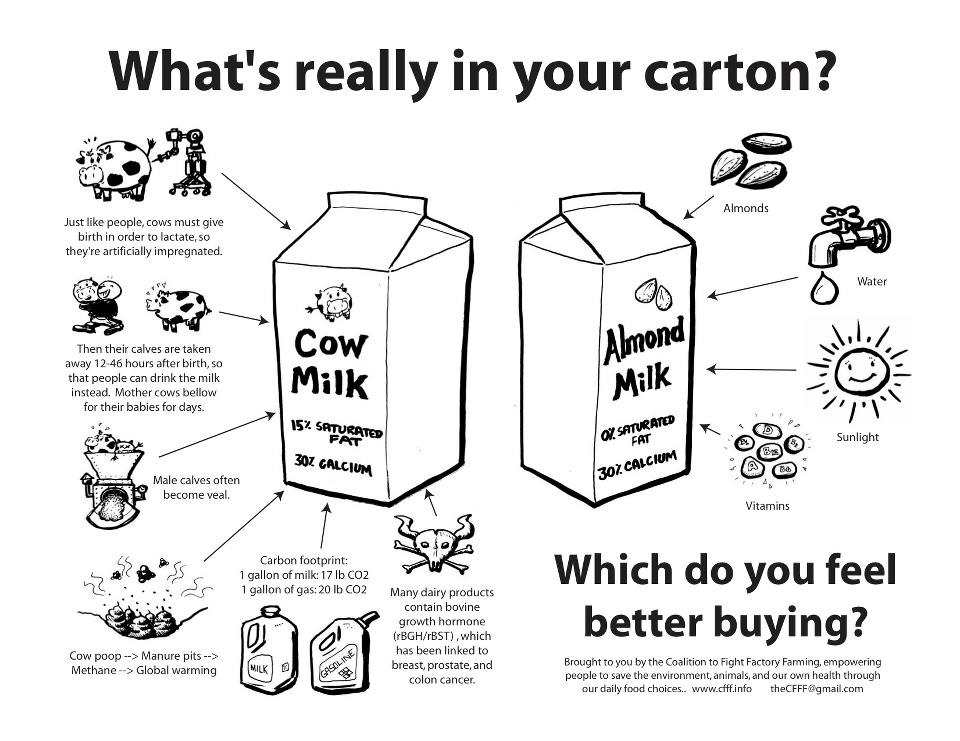 In cloudy weather, 80% of UV rays are active, in a building with transparent glass windows - 72% of the rays, and in the shade of trees - 40%.
In cloudy weather, 80% of UV rays are active, in a building with transparent glass windows - 72% of the rays, and in the shade of trees - 40%.
That's why it's important to use a sunscreen for children that provides protection against two types of UV rays - UVA and UVB. And for children under three years of age, the SPF factor should be very high - not lower than 50.
It is also necessary that moisturizing ingredients are included in the cosmetic product.
Vitamin D and the sun
You must have heard that walking in sunny weather is good for the child's body. This is mainly due to the fact that vitamin D is produced in the sun. So, the prevention of rickets to your baby in the summer season is provided. But at the same time, remember: everything is useful in moderation, so you need to be careful.
Do children need a tan
Dermatologists unanimously say that tanning is bad for children. The fact is that a child's skin is thinner and more sensitive than that of an adult, and therefore burns easily. But if you smear his body with sunscreen for children, ultraviolet rays will not harm him.
The fact is that a child's skin is thinner and more sensitive than that of an adult, and therefore burns easily. But if you smear his body with sunscreen for children, ultraviolet rays will not harm him.
Apply baby sunscreen to your baby half an hour before going outside. Don't forget your lips, nose, ears, neck, shoulders, hands and toes, and your feet if they're not wearing socks. After two hours, you still haven't returned from your walk? Then repeat the procedure.
But be aware that not every sunscreen is suitable for children. It must be chosen taking into account many characteristics. Buy a well-known brand that is labeled "children's" and "hypoallergenic." And if the baby is splashing in the street in the water, then sunscreen cosmetics should also be waterproof.
Life according to the sunny regime of the day
As a rule, summer makes adjustments to the usual daily routine. The main rule: on a clear sunny day, walk with a small child only until 11 am. Spend the hottest hours of the day indoors or, if possible, in a garden, park or forest. Usually after lunch, the children have a “quiet hour”, which means that there will be no special problems.
Spend the hottest hours of the day indoors or, if possible, in a garden, park or forest. Usually after lunch, the children have a “quiet hour”, which means that there will be no special problems.
Then go outside after 16-17:00. And get a special umbrella for the stroller, which will additionally protect the baby from direct sunlight.
Both land and sea
The sun is dangerous not only through direct contact with the skin. A child can also get sunburned under an awning (the rays are reflected from the surface of the water). Also, keep in mind that a baby who splashes in an inflatable pool in the country is more exposed to ultraviolet radiation than one that crawls on the grass. Therefore, he needs careful protection from the sun.
Dress your baby in light, light-coloured clothing made from natural fabrics. It must pass air well. Only no nets and fabrics with a sparse weave: although the skin breathes more freely, the sun's rays penetrate there.