Thigh pain during pregnancy first trimester
Pregnancy: Pain in Groin and Inner Thigh – What Can I Do?
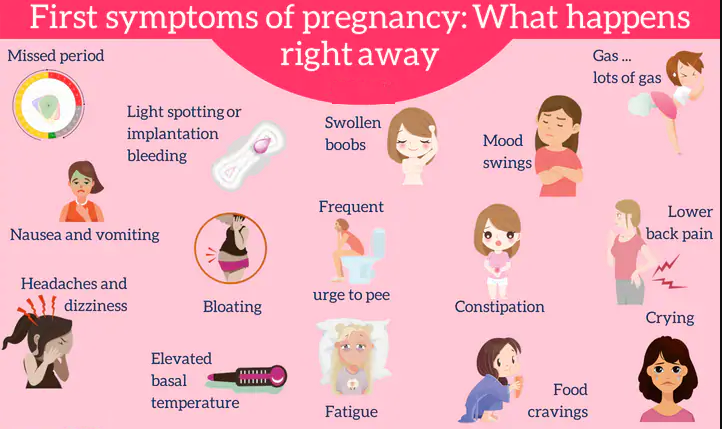
Pregnancy can be a beautiful time as you get ready to bring a new life into the world. However, many pregnancies also bring discomfort, pain, and other unwanted symptoms.
One example of an uncomfortable symptom during pregnancy is pain in the groin and inner thigh, particularly during the later months of pregnancy. This pelvic pain during pregnancy may be symphysis pubis dysfunction (SPD), which causes stiffness in the pelvic joints or uneven movements, such as when you walk.
What Causes SPD?
Symphysis pubis dysfunction happens when the ligaments responsible for keeping the pelvis aligned loosen up too much. When a ligament loosens beyond its normal range, the pelvic joint becomes unstable and can cause pain in the groin and inner thigh.
This loosening of ligaments is caused by a hormone called relaxin. Relaxin is an important hormone that is released from the placenta during pregnancy. It relaxes the wall of the uterus and prepares the uterus’ lining for pregnancy, and it also causes the cervix to dilate. Relaxin also prevents premature childbirth and regulates the mother’s and child’s health in a variety of ways.
However, during pregnancy, too much relaxin can be released into the system. When this happens, the excess of relaxin causes the ligaments responsible for stabilizing the pelvis to loosen up too much. This can cause pain in the inner thigh and groin area.
SPD Symptoms During Pregnancy
SPD can cause a variety of symptoms, including:
- Pain or difficulty walking
- Pain in the pubic or pelvic area
- Radiating pain that travels to the upper thighs
While some women experience SPD only when moving around too much, some feel it when doing normal daily activities. SPD pain is often felt when you perform any activity that requires weight-bearing or putting weight on one leg at a time. Examples include climbing stairs or even getting in and out of bed.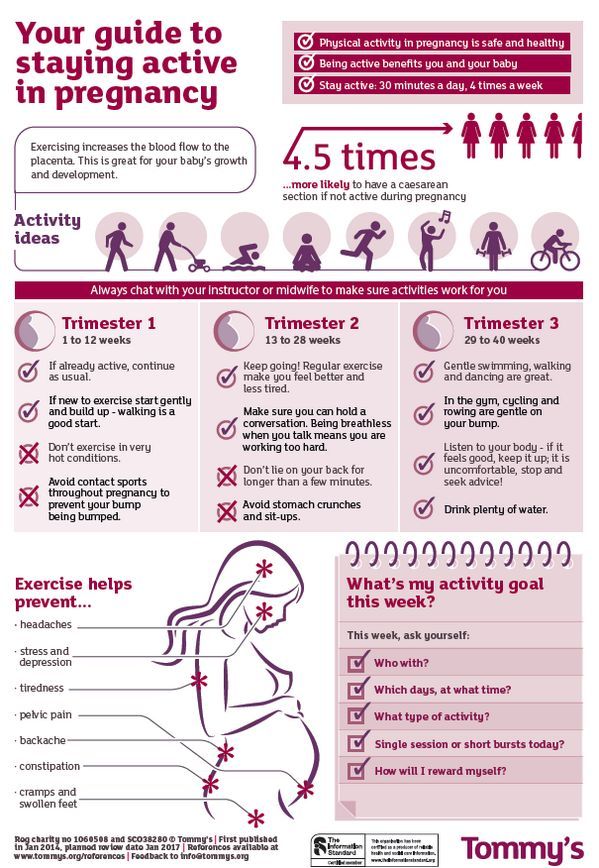
How to Deal with Pelvic Pain While Pregnant
If you experience SPD, there are a few things you can do to make your pregnancy more comfortable:
Pelvic Support Belt
Pelvic support belts help stabilize the pelvis better during pregnancy. If you experience SPD, a pelvic support belt may be able to reduce or eliminate significant SPD pain by supporting the pelvis. Talk to your OB/GYN about which pelvic support belt is right for your body.
Kegels and Pelvic Tilts
Kegels and pelvic tilts will help strengthen the pelvis’ muscles. These exercises can help stabilize the pelvis better and reduce the pain you’re feeling during your pregnancy. Talk to your OB/GYN about which types of strengthening exercises are best for you.
Rest
Sometimes, there is no better way of dealing with SPD than simply taking it easy. If you are experiencing a lot of pelvic pain, it’s time to relax.
Don’t take part in activities that will cause you pain, and make small changes to your routine to reduce the SPD pain. For example, change your clothes while sitting down instead of standing up, don’t lift heavy objects, and take the elevator or escalator instead of the stairs when possible.
For example, change your clothes while sitting down instead of standing up, don’t lift heavy objects, and take the elevator or escalator instead of the stairs when possible.
Pain Relief Medicine
Your OB/GYN may recommend pain relievers if your pain in the inner thigh and groin is severe. Talk to your doctor about your symptoms and whether pain relievers are a safe option for you and your baby.
OB/GYN Clinic in Syracuse
A supportive and knowledgeable obstetrician can help make your pregnancy a memorable, pleasant, and safe journey. If you are searching for an excellent OB/GYN center, University OB/GYN Associates is the place for you.
Our physicians have a wealth of experience dealing with a wide range of common and uncommon obstetric and gynecological issues, so you will be in safe hands. To schedule an appointment, call us at (315) 464-5162 or request an appointment online. We look forward to taking care of you.
Filed Under: Pregnancy Tagged With: groin pain, pregnancy, pregnant pain
Aching, Painful, Or Heavy Legs During Pregnancy
Having aching legs during pregnancy is the icing on the cake of all of your physical ailments. But contrary to cake, heavy or aching legs are not something to be desired. While things like morning sickness and fatigue can be expected, when leg pain hits, it might catch you off guard.
But contrary to cake, heavy or aching legs are not something to be desired. While things like morning sickness and fatigue can be expected, when leg pain hits, it might catch you off guard.
To help make your leg troubles a little more bearable, we’ll give you some basic information and help you identify the signs, causes, and treatments for your aching and heavy legs.
Blood Circulation And Heavy Or Aching Legs During Pregnancy
Pregnancy is a period during which the risk of circulatory disruptions becomes particularly high. These disruptions are the consequence of the related increase in body weight and hormonal changes, as seen below:
- As early as the first trimester, the increase in hormones creates circumstances in which the blood in the veins can easily stagnate, weakening vein walls and the firmness of blood vessels. Estrogen levels can lead to inflammation (edema), and progesterone modifies the vein walls and vessel dilation.
- Throughout pregnancy, the increased volume of the uterus leads to increased pressure on the main vein responsible for returning blood to the heart.

- Finally, an increase in blood weight and volume (of 20% to 30%) contributes to increased pressure on the leg veins, which is doubled or tripled. The valves are separated further from each other by distension of the veins and no longer play their role of impeding blood return.
Blood circulation in the leg veins can be considerably disrupted. The symptoms vary significantly from woman to woman and pregnancy to pregnancy, ranging from simple discomfort to disabling pain.
After delivery, these impairments most often go away on their own within a few weeks.
The Role Of Veins And Vascular Insufficiency
In their normal state, arteries supply the body’s tissues and organs with essential substances for their healthy functioning, such as oxygen. Veins, on the other hand, return blood to the heart.
Blood pressure and the firmness of vein walls allow blood to flow from the lower to the upper portion of the legs. This blood flow through the veins and back up to the heart is called venous return.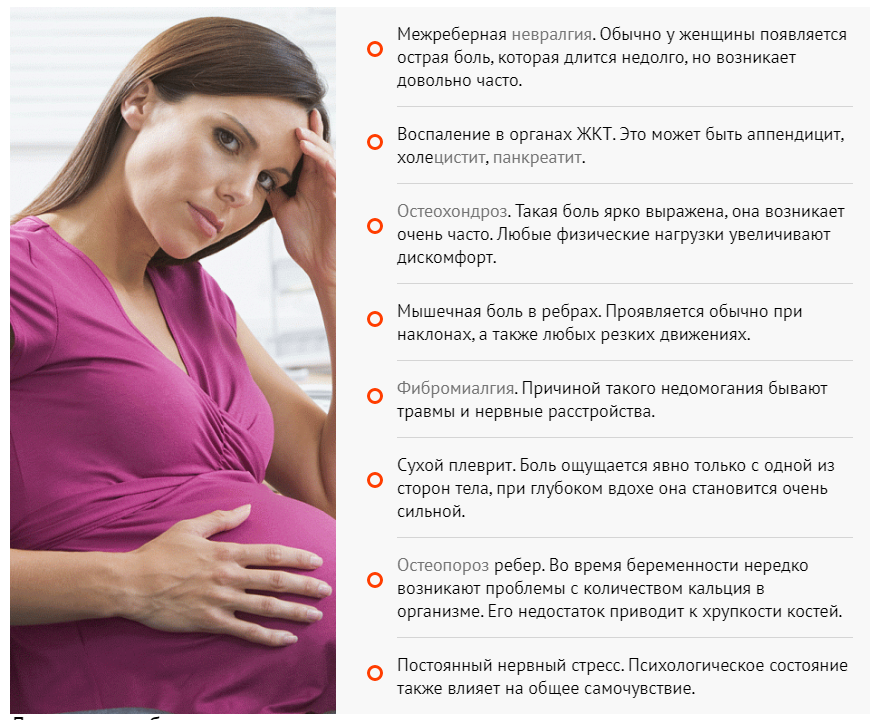
Valves, acting as small flaps, are positioned every 2 to 5 centimeters (0.8 to 2 inches) in the veins. These valves ensure that blood always flows in the same direction without ever “falling” back down the other way.
The calf muscles and compression of the instep also play a role in blood flow, particularly when walking.
Contributing Factors
Several factors can increase the risk of vascular insufficiency during pregnancy:
- Heredity: If your mom has had circulatory issues, you run a higher risk of experiencing them yourself.
- Working in a standing position and shuffling. Prolonged sitting can also disrupt venous return.
- A sedentary lifestyle and lack of physical exercise.
- Excess body weight prior to pregnancy, or significant weight gain during pregnancy.
- Previous pregnancies: The risk of venous insufficiency increases with the number of previous pregnancies carried to term — 23 percent for the first pregnancy and 31 percent for the fourth.
Healthy Habits
To avoid circulatory impairments during pregnancy, prevention is essential. If you need to, try to lose weight before getting pregnant and then limit your weight gain during pregnancy.
Here are some other healthy habits to help you avoid vascular insufficiency:
- Take walks or do light exercise, which boosts blood flow
- Wear shoes with a small heel that is neither too high nor too flat (3 to 4 cm or 1 to 1.5 inches)
- Avoid tight-fitting clothes and constricting socks
- If you suffer from any plantar arch problems, wear corrective insoles
- In certain cases, wearing compression stockings and taking venotonics may be recommended during pregnancy, starting in the second month
If you experience the sensation of heavy legs despite these measures, try some of these tips to help ease the discomfort:
- Raise your feet from the foot of your bed
- At the end of each shower, spray cold water over your legs in an upward motion from the ankles to the thighs
- Avoid sources of heat (prolonged exposure to the sun, high-temperature baths, underfloor heating, etc.
 )
) - Massage your legs every day, from the ankles to the knees, using a specific treatment cream to increase blood return and stimulate blood flow
Signs Of Heavy Or Aching Legs
Aching or heavy legs first appear as a sensation of discomfort, fatigue, and heaviness in the legs. These sensations can be the first sign of an actual circulation impairment alongside other characteristics, such as having pain:
- In the interior and posterior area of the calf that radiates up the leg toward the inside of the knee
- Most often felt towards the end of the day
- If you remain standing for a long time or if you are in contact with heat (summer temperatures, hot baths, hot-wax treatments, etc.)
- Increase as the pregnancy progresses
- Relieved by cold temperatures, winter climates, rest, elevation of the legs, and walking
- Accompanied by cramps at night, restlessness of the legs (painful discomfort that requires that one move one’s legs for relief), inflammation (edema of the ankles), varicosities, and even varicose veins
If you are experiencing any of these symptoms, talk about it with your doctor at your next visit. Your doctor may be able to prescribe a suitable treatment for you.
Your doctor may be able to prescribe a suitable treatment for you.
Causes Of Aching Or Heavy Legs
Like most expecting moms, you’re probably wondering what’s causing your aching or heavy legs. The sensation of heavy or aching legs is related to a loss of firmness and elasticity of the vein walls, which causes a slowing of blood circulation in the veins. Because of this, the veins dilate and blood pressure increases.
Valves — the small flaps that normally keep blood from flowing back down the leg veins — have difficulty maintaining this pressure and progressively become deficient.
Resistance to leaks weakens and blood stagnates in the lower portion of the veins, which further impairs vein walls. A vicious cycle takes hold.
On top of this, other factors could be causing your aching legs, such as:
- Nerve pressure: When your uterus expands, it puts pressure on certain nerves, which can trigger spasms and cause pain in your legs.
- Dehydration: If your body doesn’t get the right amount of hydration during your pregnancy — and it needs a lot! — it can really suffer.
 Whether you’re dealing with morning sickness, stress, or cramps, drinking water can be the easy answer to all your pregnancy woes. When in doubt, take the water route!
Whether you’re dealing with morning sickness, stress, or cramps, drinking water can be the easy answer to all your pregnancy woes. When in doubt, take the water route! - Increase in your weight: Your legs are carrying around more weight than they’re used to. They’re having to work a little harder each day, so at the end of the day, they’re tired just like you.
- Swelling: Swelling is no stranger to pregnancy, especially in the heat. When your ankles and feet start to swell in the heat, as we’ve mentioned above, circulation gets restricted. This is when your legs start to ache and get heavy. (Note: If you notice consistent swelling in your legs and feet, or your leg starts to feel warm, reach out to your obstetrician right away.)
- Changes in your posture as your baby grows: Throughout stages of your pregnancy, your baby has taken different positions inside your uterus. This can take a toll on your body, especially your back.
 Your posture starts to change throughout your pregnancy without you even noticing at times, but your legs are sure to take notice of the change. Your legs have to support you throughout these different stages, and it can impact them.
Your posture starts to change throughout your pregnancy without you even noticing at times, but your legs are sure to take notice of the change. Your legs have to support you throughout these different stages, and it can impact them. - Fluid retention: Your growing uterus puts pressure on the veins that carry blood back from your lower body, which partially blocks blood flow. As a result, fluid remains in your legs and feet.
- Joint laxity: As we’ve discussed, when you’re carrying the extra weight from your precious baby, it’s a lot for your legs — but it’s also a lot for your joints. Your joints can easily become stressed from the added pressure. Your joints may seem a little loose and you might even waddle when you walk!
At-Home Treatment
Most often, your leg aches can be relieved at home. That’s something to shout about because we know leg aches can really be a Debby Downer as you wrap up your day!
Here are a few ideas to relieve your leg aches and heavy legs at the end of the day:
- Stretch your calf muscles by flexing and releasing each foot a few times
- Take short walks throughout the day to boost blood flow
- Avoid standing or sitting with your legs crossed for long periods
- Take a warm bath before bed (After getting out of a relaxing bath, don’t forget to apply Stretch Marks Oil to help limit the appearance of stretch marks! It leaves your skin restored, refreshed, and noticeably smoother.
 )
) - Massage your legs throughout the day and especially before bed (Try using our Body Firming Gel to give your legs a little massage. It hydrates your skin, giving it a firmer look and overall feel.)
- Take a calcium supplement (with the go-ahead from your doctor)
- Drink a glass of milk before bed
- Prop your legs up on a pillow (make sure your legs are elevated above your heart)
- Wear compression leggings or socks
- Increase your potassium intake
Medical Treatment
If your legs are painful and you see no improvement after trying the recommended measures outlined in the previous section, do not hesitate to see a doctor. They can prescribe suitable treatment for your condition.
Various methods — from medicinal to physical to surgical — may be considered, depending on the severity of your circulatory impairments:
- Compression via pantyhose, stockings, or socks is the basic treatment for anyone experiencing venous insufficiency.
 Different models are available depending on the strength of compression necessary. Significant progress has been made in improving the esthetics of these garments. The cost of some of these compression methods may be eligible for Social Security reimbursement.
Different models are available depending on the strength of compression necessary. Significant progress has been made in improving the esthetics of these garments. The cost of some of these compression methods may be eligible for Social Security reimbursement. - Venotonics have anti-inflammatory properties, stimulating muscle tone and protecting the elasticity of the vein walls. They must be taken for an extended period of time in order to be effective.
- Kinesitherapy and exercises to build up the leg muscle also have a role to play. Walking, swimming and biking are the best types of activity. Spa treatments, massages, and manual lymphatic drainage can also provide valuable relief.
- If varicose veins developed during your pregnancy and are still present after delivery, vein sclerotherapy or surgery may be considered. These techniques can be performed under local anesthesia, requiring neither an epidural nor general anesthesia, and the patient can go home the same day as treatment, or the following day.
A Comfortable Pregnancy
Aching and heavy legs can be caused by a variety of factors, as we listed above. Although these unpleasant sensations usually disappear on their own after delivery, they should not be taken lightly.
Heavy legs can turn into vascular pathologies that can sometimes be disabling. Monitor your heavy legs closely and give them the appropriate care from the very first signs to limit the risk of complications.
But keep in mind that most often, it’s not a cause for concern or harmful to your baby. Use at-home treatments to ease your leg aches and heavy legs. You may have to try a few before you find what works for you.
And while you’re at it, continue taking care of yourself during your pregnancy by treating your skin. Using the right products that have been clinically proven to effectively help expecting mothers, like our Stretch Marks Cream, will make for one comfortable pregnancy!
home remedies, causes, prevention
content
Share on Pinterest
If you are experiencing hip pain during pregnancy, you are not alone. Eye 20 place woman experiences some kind of pain in the hip during pregnancy. The pain may be directed to the thigh or back of the thigh, or to the area of the general pelvic girdle. It may feel dull or sharp, appear gradually or suddenly.
Eye 20 place woman experiences some kind of pain in the hip during pregnancy. The pain may be directed to the thigh or back of the thigh, or to the area of the general pelvic girdle. It may feel dull or sharp, appear gradually or suddenly.
Hip pain can start at any time during pregnancy but is more common during the second and third trimesters as the baby grows and your body prepares for birth. nine0003
Read on to learn how to manage and prevent hip pain during pregnancy.
If your pain is particularly severe or limiting, consider visiting a chiropractor or physical therapist for a professional evaluation. Be sure to tell them that you are pregnant. By the way, here are a few things you can do at home to feel better.
1. yoga
Stretching can help loosen tight hips and relieve pain. Yoga can also be a good exercise during pregnancy because it is gentle and ineffective. nine0003
Some forms of yoga, including hot yoga, are not recommended during pregnancy.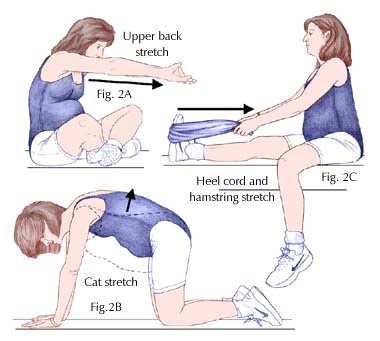 Be sure and tell your instructor that you are pregnant if you choose to attend yoga classes.
Be sure and tell your instructor that you are pregnant if you choose to attend yoga classes.
You can find many free online videos with a series of poses specially designed to help with hip and back problems during pregnancy.
For example, Yoga Seedsel shares this 20 minute hip and lower back session. It focuses on the following poses:
Cow pose
Active body. Creative mind.
Optional: You can also move slowly on all fours because you feel good.
Childish pose
Active body. Creative mind.
Optional: you can also move forward and backward in this position.
Bound Angle Pose
Active Body. Creative mind.
2. Other Exercises
There are also physical therapy techniques you can try at home to get relief. Jane Sa myPhysioSA for her details of several prostheses suitable for pregnant women:
Figure 4 stretch
Active body. Creative mind.
Figure 4 (sitting)
Active body. Creative mind.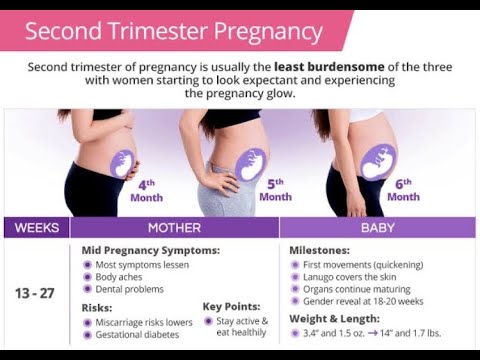
3. OTC Painkillers
In addition to exercising and stretching, you may find relief with non-alcoholic (OTC) pain medication. Ask your doctor what might be best for you, as well as the dose you should be taking.
For example, acetaminophen (Tylenol) is a category B drug and is generally considered safe during pregnancy. nine0003
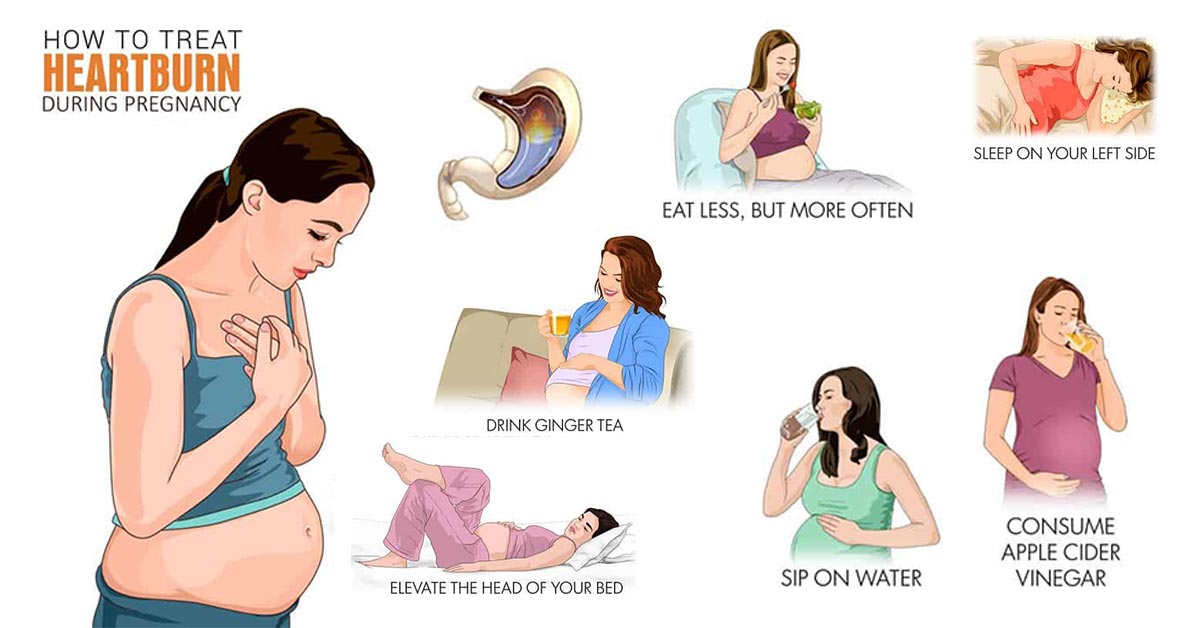
4. Warm bath or compress
If you are using temperature treatment for hip pain, you need to use heat, not cold. The heat helps ensure blood flow to the area. It also reduces joint stiffness and muscle spasms.
As a warm compress, you can use a heating pad or home compress (damp towel soaked in warm water). Apply for 10-15 minutes at a time. Do not apply a heating pad directly to your stomach.
Do not apply a heating pad directly to your stomach.
When using a warm bath to relieve pain during pregnancy, make sure the water is not too hot. It should be warm enough that you do not feel cold, but not so hot that your body temperature rises. Try adding a cup of Epsom salts (magnesium sulfate) to relieve muscle tension. nine0003
5. Massage
Your partner may massage certain parts around the thighs to relieve pain and pressure. Certified massage therapist Isis Arieta explains that lateral thigh and leg massages can be done safely at home.
Here's how:
 nine0029
nine0029 Note: During the massage, your partner should focus on opening the torso and stretching the muscles back towards the spine.
There are several reasons why you may feel pain in your hips during pregnancy. Often this is not a sign of complications or that you have done something wrong. Here are five common reasons:
1. Relax
The hormone relaxin increases during pregnancy. As the name suggests, it relaxes the tissues that connect bones throughout the body. This can lead to pelvic discomfort, especially back or hip pain.
2. Weight gain
As you and your child gain weight, the stress on your bones and joints increases. Excessive weight gain can lead to hip pain and other discomfort. nine0003
Doctors recommend gaining 11 and 40 pounds in total with a single blood pregnancy. The recommended amount depends on the starting weight. Women with a healthy pre-pregnancy weight should be between 25 and 35 pounds.
The recommended amount depends on the starting weight. Women with a healthy pre-pregnancy weight should be between 25 and 35 pounds.
Follow your doctor's advice to gain weight during pregnancy, and never try to lose weight during pregnancy unless your doctor specifically recommends and supervises.
3. Poor posture
Your posture can change with weight gain and redistribution around your belly. Not only that, but putting your baby on one side more than the other can also cause pain. nine0003
Holding an older child on their side or carrying other heavy objects without proper posture is another fasting problem that can lead to hip pain.
To practice good posture, focus on wearing supportive shoes during pregnancy. If possible, reduce the number of heavy objects you lift or carry. Take breaks while walking so you don't lose your posture as a result of fatigue.
If your doctor does not recommend it, avoid sitting for a long time. Instead, get up and move around to avoid putting extra stress on your joints and muscles. nine0003
nine0003
4. Transient osteoporosis
Some pain in the hip joint may be due to demineralization of the pelvic bones or a phenomenon known as transient osteoporosis. This condition usually begins sometime during the second or third trimester and may be related to calcium and potassium levels.
You may feel pain in your hips or groin. An MRI will be required to make a correct diagnosis.
Transient osteoporosis usually improves shortly after birth, but in rare cases, longer lasting hip fractures may occur. nine0003
5. sleeping position
Sleeping on your side can contribute to hip pain by putting pressure on your joints. With fewer sleeping positions during pregnancy, sleeping on your side may be the most comfortable option.
If this position on your hips bothers you, consider sleeping with a pillow between your knees to better position your legs. A standard pillow will do, but special maternity pillows like the Snoogle are also helpful and provide full-body support.
Although hip pain during pregnancy can be normal, you may want to see a doctor if the pain is interfering with your daily life. For example, talk to your healthcare provider if you are avoiding certain activities, such as walking, because of pain.
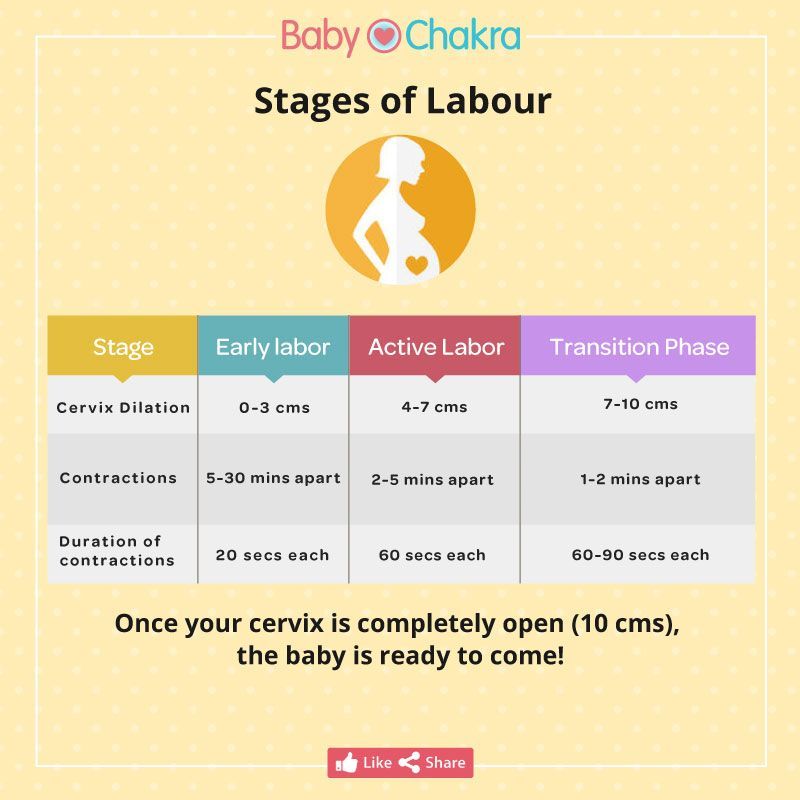
If the pain becomes severe, pay attention. Pain and pressure can be signs of preterm labor, especially if you feel contractions. Contractions may feel like abdominal cramps. 10 to 12 minutes apart (or closer). Another sign is clear pink or brown vaginal discharge. nine0003
Want to prevent hip pain before it starts? Here are a few things you can try. Keep in mind that preventative measures may not work for everyone.
- Be active during pregnancy. Low-impact exercises such as walking, cycling, and swimming may be the best for preventing hip pain.
- Make sure you are gaining weight. You usually just need to consume about 300 extra calories each day to support a healthy pregnancy. nine0029
- Wear comfortable flat shoes with good arch support during exercise and everyday activities.
 And give your leg a long rest if you start noticing pain.
And give your leg a long rest if you start noticing pain. - Maintain good posture when sitting, standing, lifting or carrying heavy objects.
- Avoid certain activities that can make pelvic pain worse, such as crossing your legs, standing for long periods of time, vacuuming, or lifting heavy objects.
- Purchase a pregnancy support belt to support your hips throughout the day.
- Consider scheduling a regular prenatal massage with a licensed therapist to keep your muscles relaxed.
Hip pain can be a reality of pregnancy, especially as your due date approaches. If these exercises, stretching, and other sedatives are not giving you relief, consider seeking medical help or seeking specialized help from a physical or chiropractor. Hip pain caused by pregnancy will most likely go away soon after delivery. nine0003
Pain in the pubic region during pregnancy
Subscribe to our Instagram! Useful information about pregnancy and childbirth from leading obstetrician-gynecologists in Moscow and foreign experts: https://www.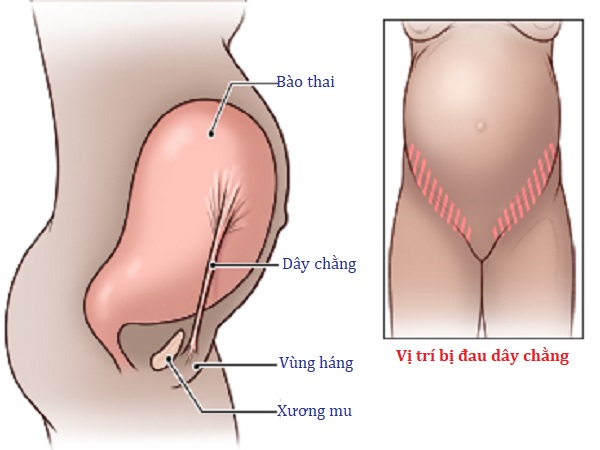 instagram.com/roddompravda/
instagram.com/roddompravda/
Tips and opinions from leading child professionals: https://www.instagram.com/emc.child/
The pubic bone is one of the three bones that make up the pelvic bone. Two pubic bones, forming the pubic articulation (symphysis), form the anterior wall of the pelvis. The pubic bone in women with a regular physique has the form of a roller about the thickness of the thumb, which is curved and forms a pubic eminence. This bone hangs in a kind of arch over the entrance to the vagina. nine0003
The main cause of pain in the pubic bone is the divergence and increased mobility of the pubic symphysis. To refer to pathological changes in the pubic symphysis of the pelvis during pregnancy and after childbirth, the following terms are used: symphysiopathy, symphysitis, arthropathy of pregnant women, divergence and rupture of the pubic symphysis, dysfunction of the pubic symphysis. The most commonly used terms are "symphysitis" or "symphysiopathy".
So, symphysiopathy is a disease associated with a pronounced softening of the pubic joint under the influence of the hormone relaxin, which is produced during pregnancy. The process of softening the interosseous joints is natural, it helps the child to pass more easily through the bone pelvis during childbirth. The diagnosis of "symphysiopathy" is made when severe pain appears, the pubic joint swells, greatly stretches, becomes mobile, and the pubic bones diverge excessively. One of the striking, characteristic symptoms of this pathology is that it is impossible to raise the leg in the prone position. In addition to acute pain in the pubis, there are difficulties when walking up the stairs, it becomes difficult to turn from side to side on the bed and get up from the sofa, and the gait changes and becomes like a "duck". According to most doctors, the cause of symphysiopathy is a lack of calcium, an increased concentration of the hormone relaxin, and increased physical activity on the bones of the pelvic region. In addition, the development of symphysiopathy can be provoked by a serious sports injury or a fracture of the pelvic bones. nine0003
In addition, the development of symphysiopathy can be provoked by a serious sports injury or a fracture of the pelvic bones. nine0003
At what stage of pregnancy do they occur?
The disease begins gradually or suddenly during pregnancy, childbirth or after childbirth. Most often, women begin to feel pain in the area of the pubic joint in the third trimester of pregnancy. This is due to the fact that the places of adhesions of the pubic bones, their ligaments and cartilage, soften under the influence of the hormone relaxin. This hormone of pregnancy naturally softens the bony joints, which is necessary to facilitate the passage of the child's bone pelvis and birth canal at the time of childbirth. nine0003
Some women begin to complain of pain in the pelvic bones some time after giving birth. This may be the result of traumatic childbirth (imposition of obstetrical forceps, shoulder dystocia, excessive separation of the hips during childbirth, etc.) or physical exertion (lifting a heavy baby stroller up the stairs, prolonged motion sickness in the arms of a well-fed baby, etc. ). It is recommended to limit physical activity, wear an orthopedic bandage, consult a traumatologist. Complaints usually recur after the next pregnancy. In a small proportion of patients, pain persists for a long time. nine0003
). It is recommended to limit physical activity, wear an orthopedic bandage, consult a traumatologist. Complaints usually recur after the next pregnancy. In a small proportion of patients, pain persists for a long time. nine0003
When can this be considered the norm, and when not?
Obstetricians-gynecologists do not consider a slight soreness of the pubic joint to be a pathology, but if the pain is acute, restricting the movements of the pregnant woman, accompanied by edema, then we can talk about pathology. Pain can be quite strong and especially manifest itself while walking, turning the body to the right and left in a sitting position and even lying down. In this case, you need to urgently consult a doctor and undergo an ultrasound diagnosis (ultrasound) to determine the size of the divergence of the pubic bones. Magnetic resonance imaging (MRI) is also used, which allows assessing the state of the symphysis, the state of the bone tissue, as well as soft tissues. nine0003
nine0003
With ultrasound, the degree of divergence (diastasis) of the pubic bones is determined. The severity of the clinical picture largely depends on the degree of divergence of the pubic bones, and therefore there are three degrees of divergence of the pubic branches: in the first degree - by 6-9 mm, in the second - by 10-20 mm, in the third - more than 20 mm. The severity of the symptoms of the disease varies from mild discomfort to unbearable pain.
How can pain be relieved? nine0199
There are some recommendations that will help reduce bone pain during pregnancy, if the cause of its occurrence is the divergence of the pubic bones. Be sure to wear a bandage, especially in later pregnancy. The bandage takes on most of the load, thereby releasing pressure from the pubic joint. Limitation of heavy physical exertion is indicated for any manifestations of pain, lying down more often, walking less and being in a sitting position for no longer than 30-40 minutes. In severe cases, before and sometimes after childbirth, a woman may be shown strict bed rest. Moreover, the bed should not be hard and flat. nine0003
In severe cases, before and sometimes after childbirth, a woman may be shown strict bed rest. Moreover, the bed should not be hard and flat. nine0003
Since the appearance of symphysiopathy is associated not only with a large production of the hormone relaxin, but also with a lack of calcium in the body, the expectant mother is prescribed calcium preparations and complex vitamins for pregnant women, which contain all the necessary vitamins and trace elements in the right amount and proportions. There is evidence that pain is reduced during acupuncture and physiotherapy.
In especially severe cases of symphysiopathy, the pregnant woman is hospitalized. nine0003
What is the danger of this condition?
The occurrence of symphysiopathy is due to several reasons. This is a lack of calcium in the body of the future mother, and an excess amount of the hormone relaxin, and the individual structural features of the woman's body, and possible hereditary or acquired problems of the musculoskeletal system.
With an unexpressed clinical picture of the disease, with an expansion of the pubic fissure up to 10 mm, normal pelvic sizes, a small fetus, childbirth can be carried out through the birth canal, avoiding the use of physical force, such as the Christeller maneuver. With a pronounced stretching of the pubic symphysis, pain syndrome, especially with anatomical narrowing of the pelvis, a large fetus, there is a danger of rupture of the pubic symphysis, and the method of choice in this case is caesarean section. This is due to the fact that during natural delivery, the bones can disperse even more and the woman subsequently will not be able to walk at all. nine0003
Prevention
The body of a healthy woman is able to independently cope with all the difficulties of the pregnancy period. First of all, the expectant mother should include enough foods containing calcium in her diet, as well as take vitamins for pregnant women.
For the prevention of symphysiopathy, the use of a prenatal bandage is recommended, which supports the abdomen and prevents excessive stretching of the ligaments and muscles.