Chloasma during pregnancy
Changes to your skin during pregnancy
beginning of content3-minute read
Listen
As your pregnancy develops, you may find that you experience changes to your skin and hair. Some women can develop dark patches on their face and hormonal changes can make your skin a little darker.
You may also develop stretch marks on your body, particularly around your stomach where your skin is stretching to accommodate your growing baby.
Chloasma - dark patches on the face
Some pregnant women develop dark irregular patches on their face most commonly on the upper cheek, nose, lips, and forehead. This is called 'chloasma'. It is also sometimes known as 'melasma' or the 'mask of pregnancy'.
Chloasma is thought to be due to stimulation of pigment-producing cells by female sex hormones so that they produce more melanin pigments (dark coloured pigments) when the skin is exposed to sun. Some women develop these patches when they take oral contraceptives (the pill).
Women with a light brown skin type who are living in regions with intense sun exposure are more likely to develop these patches. The patches usually fade over a period of several months after giving birth, though they may last for several years for some women.
Careful protection of the skin using broad spectrum sunscreens every day during pregnancy and while taking the pill may make it less likely that chloasma will develop. It is necessary to continue to use sunscreen after pregnancy as sun exposure may cause the patches to reappear. Some creams that need to be prescribed by doctors may help to fade the patches.
Skin and hair changes
Hormonal changes taking place in pregnancy will make your nipples and the area around them go darker. Your skin colour may also darken a little, either in patches or all over. Birthmarks, moles and freckles may also darken. Some women develop a dark line down the middle of their stomach, called 'linea nigra'. These changes will gradually fade after the baby is born, although your nipples may remain a little darker.
These changes will gradually fade after the baby is born, although your nipples may remain a little darker.
If you sunbathe while you are pregnant, you may burn more easily. Protect your skin with a good high-factor sunscreen and don't stay in the sun for a long time.
Hair growth can also increase in pregnancy, and your hair may be greasier. After the baby is born, it may seem as if you are losing a lot of hair but you are simply losing the extra hair.
Stretch marks
Many women develop stretch marks during their pregnancy, usually in the last 3 months.
They usually appear on your stomach or sometimes on your upper thighs or breasts. Stretch marks are not harmful and over time, your skin will shrink and the stretch marks will fade into white-coloured scars.
Find out more on stretch marks.
Sources:
Royal Women's Hospital Victoria (Common concerns in early pregnancy - itching and skin), The Australasian College of Dermatologists (Striae), The Australasian College of Dermatologists (Melasma)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: January 2020
Back To Top
Related pages
- Common discomforts during pregnancy
- Stretch marks
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Chloasma--the mask of pregnancy - PubMed
Review
. 2008 Oct;32 Suppl 2:139-41.
Ivan Bolanca 1 , Zeljana Bolanca, Krunoslav Kuna, Ante Vuković, Neven Tuckar, Radoslav Herman, Goran Grubisić
Affiliations
Affiliation
- 1 University Department of Obstetrics and Gynecology, University Hospital Sestre milosrdnice, Zagreb, Croatia.
 [email protected]
[email protected]
- PMID: 19140277
Review
Ivan Bolanca et al. Coll Antropol. 2008 Oct.
. 2008 Oct;32 Suppl 2:139-41.
Authors
Ivan Bolanca 1 , Zeljana Bolanca, Krunoslav Kuna, Ante Vuković, Neven Tuckar, Radoslav Herman, Goran Grubisić
Affiliation
- 1 University Department of Obstetrics and Gynecology, University Hospital Sestre milosrdnice, Zagreb, Croatia. [email protected]
- PMID: 19140277
Abstract
Chloasma is a required hypermelanosis of sun-exposed areas occurred during pregnancy and it can affect 50-70% of pregnant women. It presents as symmetric hyperpigmented macules, which can confluent or punctuate. The most common locations are the cheeks, the upper lip, the chin and the forehead. The exact mechanism by which pregnancy affects the process of melanogenesis is unknown. Estrogen, progesterone, and melanocyte-stimulating hormone (MSH) levels are normally increased during the third trimester of pregnancy. However, nulliparous patients with chloasma have no increased levels of estrogen or MSH. In addition, the occurrence of melasma with estrogen- and progesterone-containing oral contraceptive pills has been reported. The observation that postmenopausal woman who are given progesterone develop melasma, while those who are given only estrogen do not, implicates progesterone as playing a critical role in the development of melasma. UV-B, UV-A, and visible light are all capable of stimulating melanogenesis. The condition is self-limited; however spontaneous resolution is time-consuming and may take months to resolve normal pigmentation.
It presents as symmetric hyperpigmented macules, which can confluent or punctuate. The most common locations are the cheeks, the upper lip, the chin and the forehead. The exact mechanism by which pregnancy affects the process of melanogenesis is unknown. Estrogen, progesterone, and melanocyte-stimulating hormone (MSH) levels are normally increased during the third trimester of pregnancy. However, nulliparous patients with chloasma have no increased levels of estrogen or MSH. In addition, the occurrence of melasma with estrogen- and progesterone-containing oral contraceptive pills has been reported. The observation that postmenopausal woman who are given progesterone develop melasma, while those who are given only estrogen do not, implicates progesterone as playing a critical role in the development of melasma. UV-B, UV-A, and visible light are all capable of stimulating melanogenesis. The condition is self-limited; however spontaneous resolution is time-consuming and may take months to resolve normal pigmentation. Therefore, it is worthwhile to prevent the onset of chloasma, by strict photoprotection. Prudent measures to avoid sun exposure include hats and other forms of shade combined with the application of a broad-spectrum sunscreen at least daily. Sunscreens containing physical blockers, such as titanium dioxide and zinc oxide, are preferred over chemical blockers because of their broader protection. Chloasma can be difficult to treat. Quick fixes with destructive modalities (eg, cryotherapy, medium-depth chemical peels, lasers) yield unpredictable results and are associated with a number of potential adverse effects. The mainstay of treatment remains topical depigmenting agents. Hydroquinone (HQ) is most commonly used.
Therefore, it is worthwhile to prevent the onset of chloasma, by strict photoprotection. Prudent measures to avoid sun exposure include hats and other forms of shade combined with the application of a broad-spectrum sunscreen at least daily. Sunscreens containing physical blockers, such as titanium dioxide and zinc oxide, are preferred over chemical blockers because of their broader protection. Chloasma can be difficult to treat. Quick fixes with destructive modalities (eg, cryotherapy, medium-depth chemical peels, lasers) yield unpredictable results and are associated with a number of potential adverse effects. The mainstay of treatment remains topical depigmenting agents. Hydroquinone (HQ) is most commonly used.
Similar articles
-
Evaluation of the effectiveness of a broad-spectrum sunscreen in the prevention of chloasma in pregnant women.
Lakhdar H, Zouhair K, Khadir K, Essari A, Richard A, Seité S, Rougier A.
 Lakhdar H, et al. J Eur Acad Dermatol Venereol. 2007 Jul;21(6):738-42. doi: 10.1111/j.1468-3083.2007.02185.x. J Eur Acad Dermatol Venereol. 2007. PMID: 17567299 Clinical Trial.
Lakhdar H, et al. J Eur Acad Dermatol Venereol. 2007 Jul;21(6):738-42. doi: 10.1111/j.1468-3083.2007.02185.x. J Eur Acad Dermatol Venereol. 2007. PMID: 17567299 Clinical Trial. -
[Facial melanosis (melasma)].
Witkiewicz IM, Neering H. Witkiewicz IM, et al. Ned Tijdschr Geneeskd. 1981 Apr 18;125(16):609-11. Ned Tijdschr Geneeskd. 1981. PMID: 7242709 Dutch.
-
Near-visible light and UV photoprotection in the treatment of melasma: a double-blind randomized trial.
Castanedo-Cazares JP, Hernandez-Blanco D, Carlos-Ortega B, Fuentes-Ahumada C, Torres-Álvarez B. Castanedo-Cazares JP, et al. Photodermatol Photoimmunol Photomed. 2014 Feb;30(1):35-42. doi: 10.1111/phpp.12086. Epub 2013 Dec 3.
 Photodermatol Photoimmunol Photomed. 2014. PMID: 24313385 Clinical Trial.
Photodermatol Photoimmunol Photomed. 2014. PMID: 24313385 Clinical Trial. -
Advances in the treatment of melasma: a review of the recent literature.
Ball Arefiev KL, Hantash BM. Ball Arefiev KL, et al. Dermatol Surg. 2012 Jul;38(7 Pt 1):971-84. doi: 10.1111/j.1524-4725.2012.02435.x. Epub 2012 May 14. Dermatol Surg. 2012. PMID: 22583339 Review.
-
Melasma--updated treatments.
Situm M, Kolić M, Bolanca Z, Ljubicić I, Misanović B. Situm M, et al. Coll Antropol. 2011 Sep;35 Suppl 2:315-8. Coll Antropol. 2011. PMID: 22220462 Review.
See all similar articles
Cited by
-
Loss of EMP2 Inhibits Melanogenesis of MNT1 Melanoma Cells via Regulation of TRP-2.

Enkhtaivan E, Kim HJ, Kim B, Byun HJ, Yu L, Nguyen TM, Nguyen TH, Do PA, Kim EJ, Kim KS, Huy HP, Rahman M, Jang JY, Rho SB, Lee H, Kang GJ, Park MK, Kim NH, Choi CI, Lee K, Han HK, Cho J, Lee AY, Lee CH. Enkhtaivan E, et al. Biomol Ther (Seoul). 2022 Mar 1;30(2):203-211. doi: 10.4062/biomolther.2022.001. Biomol Ther (Seoul). 2022. PMID: 35221300 Free PMC article.
-
Sex Hormones and Optic Nerve Disorders: A Review.
Nuzzi R, Scalabrin S, Becco A, Panzica G. Nuzzi R, et al. Front Neurosci. 2019 Feb 11;13:57. doi: 10.3389/fnins.2019.00057. eCollection 2019. Front Neurosci. 2019. PMID: 30804741 Free PMC article. Review.
-
Ocular changes during pregnancy.
Naderan M. Naderan M. J Curr Ophthalmol.
 2018 Jan 3;30(3):202-210. doi: 10.1016/j.joco.2017.11.012. eCollection 2018 Sep. J Curr Ophthalmol. 2018. PMID: 30197948 Free PMC article. Review.
2018 Jan 3;30(3):202-210. doi: 10.1016/j.joco.2017.11.012. eCollection 2018 Sep. J Curr Ophthalmol. 2018. PMID: 30197948 Free PMC article. Review. -
Lack of pregnancy warnings on over-the-counter dermatologic products containing potentially harmful hydroquinone.
Bio LL, Cies JJ. Bio LL, et al. J Perinatol. 2017 Jul;37(7):778-781. doi: 10.1038/jp.2017.35. Epub 2017 Mar 30. J Perinatol. 2017. PMID: 28358386
-
Melasma: a clinical and epidemiological review.
Handel AC, Miot LD, Miot HA. Handel AC, et al. An Bras Dermatol. 2014 Sep-Oct;89(5):771-82. doi: 10.1590/abd1806-4841.20143063. An Bras Dermatol. 2014. PMID: 25184917 Free PMC article. Review.
See all "Cited by" articles
Publication types
MeSH terms
Substances
causes, symptoms, diagnosis and treatment
- INVITRO
- Library
- Directory of Diseases
- Chloasma
ECO
Menopause
Hepatitis
6465 24 November nine0013
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes. nine0013
nine0013
Chloasma: causes, symptoms, diagnosis and treatment.
Definition
Chloasma is an acquired limited hypermelanosis, or hyperpigmentation of the skin (violation of the formation of melanin pigment in the direction of strengthening). Melanin grains accumulate in the cells of the basal and prickly layers of the epidermis, and the number of melanosomes in the superficial layers of the dermis increases. Spots of dark yellow or dark brown color appear more often in women aged 20 to 50 years, have an irregular shape and are usually localized on the skin of the face - in the cheeks, upper lip, around the eyes, on the temples and bridge of the nose. nine0013
Chloasma occurs in pregnant women, patients with chronic liver disease, women diagnosed with inflammatory processes in the gynecological area, or using oral contraceptive drugs.
Causes of chloasma
The exact cause of chloasma is unknown. There are observations that speak of a genetic predisposition to excessive formation of melanin - there are known cases of the disease in several family members at once. Exposure to sunlight plays a significant role in the development of chloasma - exacerbations occur after prolonged exposure to the sun and fade away when there is no insolation. nine0013
There are observations that speak of a genetic predisposition to excessive formation of melanin - there are known cases of the disease in several family members at once. Exposure to sunlight plays a significant role in the development of chloasma - exacerbations occur after prolonged exposure to the sun and fade away when there is no insolation. nine0013
Often chloasma appears during pregnancy, so its other name is “pregnancy mask”. This type of dyschromia partially or completely disappears in the postpartum period after the resumption of menstruation. However, residual effects can persist for quite a long period.
Chloasma can manifest itself while taking hormonal contraceptives, in patients with ovarian tumors, since there is an association between increased melanin production and changes in the level of sex hormones estrogen and progesterone. nine0013
The risk factors provoking the formation of chloasma include:
- pregnancy, menopause;
- viral hepatitis, liver cirrhosis, tuberculosis;
- inflammatory diseases of the genital organs in women;
- taking oral contraceptives;
- excessive sun exposure, including artificial tanning.
Classification of the disease
Depending on the localization of lesions on the face, the following clinical forms of the disease are distinguished:
- centrofacial chloasma - located in the center of the forehead, on the nose, in the region of the upper lip, chin;
- molar chloasma - located on the cheeks and wings of the nose;
- mandibular (mandibular) chloasma - located on the skin of the lower jaw.
According to the clinical course allocate:
- passing forms - the spots disappear on their own, without treatment;
- persistent forms - the spots decrease during treatment, the progress of the disease slows down, but the hyperpigmentation does not completely disappear. nine0004
Depending on the level of deposition of melanin pigment , there are:
- epidermal type;
- dermal type;
- mixed type.
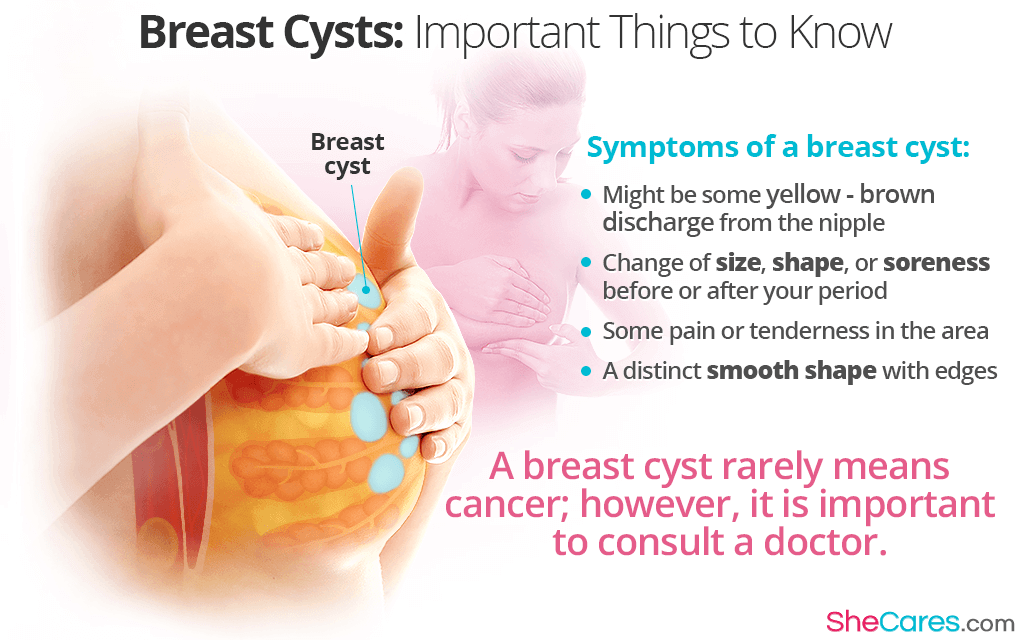
Symptoms of chloasma
Chloasma is characterized by various sizes of light brown, dark brown or heterogeneously colored spots of irregular shape, single or multiple. As a rule, they are located symmetrically on open areas of the skin of the face, less often - on the neck, in the décolleté area. The spots have clear uneven boundaries, are not raised above the surface of the skin, and can merge with each other. Chloasma does not cause physical discomfort, because it is not accompanied by peeling, itching and soreness. nine0013
In pregnant women, chloasma spots can be localized on the midline of the abdomen, in the nipples and vulva.
Chloasma diagnostics
The diagnosis of "chloasma" is established by the doctor on the basis of examination and history taking - to exclude the congenital or post-inflammatory nature of hyperpigmentation.
A more detailed study of age spots is carried out by a specialist using the dermatoscopy method. A dermatoscope is a device designed to examine the superficial and deep layers of the skin under 10x (sometimes more) magnification. Dermatoscopy is widely used in modern dermatology and cosmetology and makes it possible to detect malignant changes in the early stages, as well as to observe age spots in dynamics to assess the effectiveness of treatment. nine0013
A dermatoscope is a device designed to examine the superficial and deep layers of the skin under 10x (sometimes more) magnification. Dermatoscopy is widely used in modern dermatology and cosmetology and makes it possible to detect malignant changes in the early stages, as well as to observe age spots in dynamics to assess the effectiveness of treatment. nine0013
The use of a Wood's lamp (ultraviolet lamp) helps to distinguish between epidermal and dermal types of chloasma.
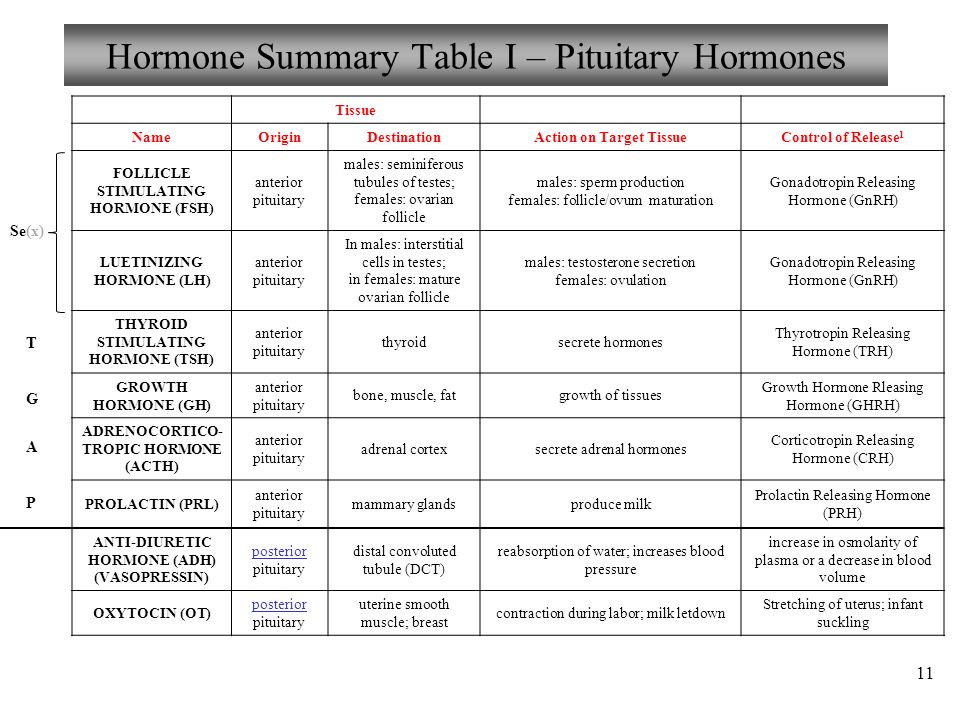
Laboratory diagnostics includes determining the level of sex hormones in the blood: estradiol, progesterone, luteinizing hormone, testosterone.
Estradiol (E2, Estradiol)
Synonyms: Blood test for estradiol. 17-beta-estradiol. Brief description of the analyte Estradiol Estradiol is a steroid hormone with maximum estr...
Up to 1 business day
Available with home visit
715 RUB
In garbage
Progesterone
Synonyms: Progestin; Gestagen. P4; Pregn-4-ene-3,20-dione. Brief description of the analyte Progesterone Progesterone is produced in the ovaries and in a small cell...
P4; Pregn-4-ene-3,20-dione. Brief description of the analyte Progesterone Progesterone is produced in the ovaries and in a small cell...
Up to 1 business day
Available with home visit
705 RUB
In garbage
Luteinizing Hormone (LH)
Synonyms: Glycoprotein gonadotropic hormone; luteotropin; Lutropin. luteinizing hormone; LH; Lutropin; Interstitial cell stimulating hormone; ICSH. Brief characteristic determined ...
Up to 1 business day
Available with home visit
715 RUB
In garbage
Testosterone
Testosterone is the main androgenic hormone. The test is used in the diagnosis of disorders of sexual development and hypogonadism in men; cycle disorders, infertility, virus...
The test is used in the diagnosis of disorders of sexual development and hypogonadism in men; cycle disorders, infertility, virus...
Up to 1 business day
Available with home visit
715 RUB
In garbage
Since in some cases hyperpigmentation may be one of the manifestations of an ovarian tumor, an ultrasound examination (ultrasound) of the pelvic organs is performed.
US examination of pelvic organs (uterus, adnexa)
Ultrasound scanning of the organs of the female reproductive system to assess the shape and size, as well as exclude pathology.
RUB 2,390 Sign up
If a malignant nature of the neoplasm is suspected, a blood test is prescribed for the ovarian tumor marker - SA.
Antinuclear antibodies, IgG, screening, ELISA (Antinuclear antibodies, ANAs, EIA)
Synonyms: Antinuclear antibodies, Antinuclear factor; ANF. Antinuclear Antibody; ANA; antinuclear factor; ANF. Brief description of the test "Antinuclear antibodies, IgG, screening, I...
Up to 3 business days
Available with home visit
RUB 915
In garbage nine0013
CA-125 (Cancer Antigen 125)
Synonyms: Blood test for CA-125; Carbohydrate antigen-125; Tumor antigen CA 125; Cancer antigen CA 125; Tumor marker for ovarian cancer. CA-125 tumor marker, Cancer Antigen - 125; Carbohydrate antige...
Up to 1 business day
Available with home visit
1 010 RUB nine0013
In garbage
Which doctors to contact
Dermatologists are involved in the examination and treatment of patients with hyperpigmentation. Since the development of the disease may be associated with hormonal imbalances, it is often involved in the process of examination and treatment.
Since the development of the disease may be associated with hormonal imbalances, it is often involved in the process of examination and treatment.
gynecologist
.
Treatment of chloasma
Benign hyperpigmentation does not affect health in general, does not degenerate into malignant neoplasms, but their appearance on the face often brings psychological discomfort. nine0013
For effective treatment of chloasma, first of all, it is necessary to eliminate the cause that provoked the development of this disease. For example, if chloasma arose as a result of a liver disease, then the function of this organ is restored first of all. In cases where chloasma is the result of hormonal disorders, drugs are prescribed that correct this condition, change or completely cancel oral contraceptives, etc.
Before proceeding with the cosmetic removal of chloasma spots, it is necessary to make sure that the composition of skin care products used on a regular basis does not include photosensitizing ingredients - retinoids, alpha and beta hydroxy acids, etc. nine0013
nine0013
In the arsenal of modern cosmetology there are many methods aimed at correcting age spots. Their appointment is the competence of a dermatologist. In cases where chloasma is localized in the epidermis, it is often possible to limit oneself to depigmenting cosmetic preparations, which include arbutin, kojic, ascorbic and azelaic acids, hydroquinone, rucinol and other active substances with whitening properties. In addition, mesotherapeutic procedures are performed, as well as chemical peels (phytic, retinoic, pyruvic, azelaic, glycolic, etc.). In case of treatment failure, hardware procedures are used - microdermabrasion, laser resurfacing or laser peeling. nine0013
Treatments with fractional or neodymium lasers are recommended for dermal chloasma.
Complications
Chloasma has no complications that could affect a person's life, but it brings considerable psychological discomfort.
Chloasma prophylaxis
The main preventive measure is the restriction of exposure to the open sun, the exclusion of visits to solariums and the use of sunscreen even in cloudy weather. nine0013
nine0013
When using hormonal contraceptives, it is necessary to discuss with the gynecologist the possibility of their cancellation.
A number of drugs and cosmetics have a photosensitizing effect - they increase the sensitivity of the skin to sunlight. The doctor will help you choose their analogues, which will minimize the risk of further development of chloasma.
Sources:
- Melasma - European recommendations. nine0009 Kurbanova D.Ch. The problem of the prevalence of chloasma and melasma in women. Bulletin of science and practice, journal. Vol.5, No.7. 2019.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes. nine0013
nine0013
Recommendations
-
Schizotypal disorder
13379 21 December
-
Lactase deficiency
13382 21 December
nine0009
Swine Flu (Influenza A/h2N1pdm09, California 04/2009, Mexican Flu, Swine Flu, Influenza A Subtype h2N1)
13424 December 20
Show more
Acne (acne)
nine0012 ThyrotoxicosisGastritis
Menopause
Encephalitis
Hypercholesterolemia
nine0012 HepatitisDermatitis
Dermatitis: causes, symptoms, diagnosis and treatment.
More
ECO
Diabetes mellitus
Thrush
Mastopathy
Mastopathy: causes, symptoms, diagnosis and treatment.
More
Thyrotoxicosis
Menopause
Acne (acne)
nine0012 Diabetes mellitusHirsutism
Hirsutism: causes, symptoms, diagnosis and treatment.
More
Hepatitis
Jaundice
Viral Hepatitis D (Hepatitis D, Hepatitis Delta, Hepatitis delta virus, HDV)
Viral hepatitis D: causes, symptoms, diagnosis and treatment.
More
Loss of consciousness
Convulsions
Respiratory arrest
nine0012 StrokeDiabetes mellitus
Cirrhosis
Hepatitis
Pyelonephritis
Coma or coma
Coma: causes, symptoms, diagnosis and treatment.
More
Nothing found
Try editing your query or select a doctor or service from the list.
Doctor not found
Try changing your query or select doctor from the list
Medical office not found
Try changing your query or select medical office from list
Therapist Traumatologist-orthopedist Endocrinologist Urologist Gynecologist Ultrasound doctor Cardiologist Pediatrician
Nothing found
Please try editing your query
Thank you!
You have successfully made an appointment
Detailed information has been sent to your e-mail
Pigmentation during pregnancy: how to get rid of it - Parents.ru
Pregnancy
- Photo
- DiMedia/Shutterstock
Pigmentation is the darkening or, conversely, lightening of skin areas, which occurs due to failures in the production of melanin, the pigment responsible for the color of the skin. The appearance of such signs suggests that a woman is pregnant. Whether the spots appear dark or light, depends on the original skin color. Such marks, characterized by sharp edges and irregular shape, are called melasma or chloasma by doctors. nine0013
The appearance of such signs suggests that a woman is pregnant. Whether the spots appear dark or light, depends on the original skin color. Such marks, characterized by sharp edges and irregular shape, are called melasma or chloasma by doctors. nine0013
During pregnancy, they can appear both on the face (on the forehead, chin, around the eyes, on the upper part of the cheeks, on the upper lip), and on other parts of the body: on the inner thighs, areolas of the mammary glands, on the abdomen.
"Pregnancy mask" on the face: what is it
In some areas, the skin begins to darken in the very early stages of pregnancy. Sometimes the manifestation of this particular symptom prompts a woman to think about pregnancy. First, the nipples and areolas around them, the area of the labia and the clitoris darken. nine0013
In the second trimester, pigmentation becomes brighter and some expectant mothers get the so-called “pregnancy mask” - pigmentation occurs on the face during pregnancy. The spots appear on the cheeks, on the nose, on the forehead, cheekbones, under the eyes, above the upper lip and on the chin and can be arranged symmetrically. If a woman is prone to the appearance of freckles, then you need to be prepared for the fact that during the bearing of the baby they will become brighter, and their number will increase.
The spots appear on the cheeks, on the nose, on the forehead, cheekbones, under the eyes, above the upper lip and on the chin and can be arranged symmetrically. If a woman is prone to the appearance of freckles, then you need to be prepared for the fact that during the bearing of the baby they will become brighter, and their number will increase.
Pigmentation during pregnancy on the abdomen appears at about the same time. This brown stripe, which stretches from the navel to the pubis, the so-called Alba stripe, exists in every woman, it just becomes more noticeable during the bearing of the baby. nine0013
Why pigmentation occurs
The color of human skin depends on many circumstances, but the most important is the concentration of coloring substances, or pigments, one of which is melanin. It accumulates in special molecules called "melanosomes", which act as a natural filter that protects the top layer of the skin from the harmful effects of ultraviolet rays.
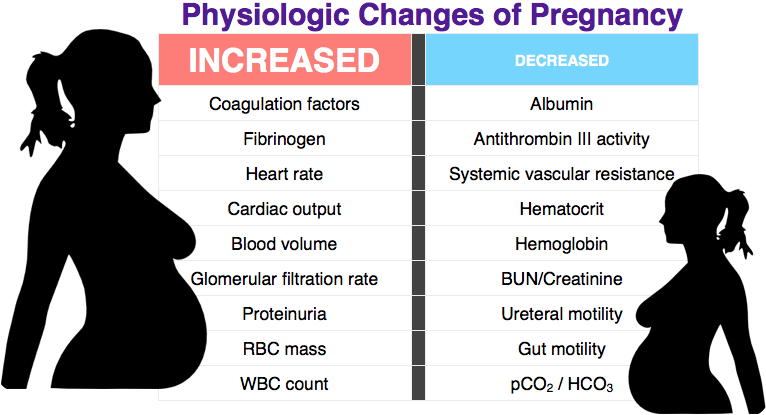
During pregnancy, the production of melanin changes, because the adrenal glands begin to synthesize more estrogens, progesterone and melanocyte-stimulating hormone. Because of this, more melanin is released, which is concentrated in certain areas of the skin. As a result, the woman develops hyperpigmentation. nine0013
Because of this, more melanin is released, which is concentrated in certain areas of the skin. As a result, the woman develops hyperpigmentation. nine0013
Occasionally, chloasma is caused by taking oral contraceptives before pregnancy or a lack of folic acid. Pigmentation can also indicate problems in the functioning of the liver, pituitary gland, ovaries, incorrect cosmetic procedures, the use of low-quality cosmetics or perfumes. Stress also plays an important role in the appearance of spots on the skin.
Genetics also matter. If the mother had such a problem during pregnancy, then it is possible that age spots during the period of bearing the baby will appear in her daughter. nine0013
Expectant mothers often ask how pregnancy pigmentation affects the baby. If its cause is not an exacerbation of chronic ailments, then age spots will not have any effect on the unborn child.
- Photo
- Konstantin Aksenov/Shutterstock
Age spots during pregnancy: a boy or a girl?
There is a popular belief that age spots during pregnancy appear more often in expectant mothers of girls. This is justified: a girl developing in her stomach takes estrogens from her future mother, and their level in the woman's body decreases. But how then to explain that age spots appear in expectant mothers of boys? In a word, than to guess according to folk signs, it is better to do an ultrasound. It definitely won't go wrong. nine0013
This is justified: a girl developing in her stomach takes estrogens from her future mother, and their level in the woman's body decreases. But how then to explain that age spots appear in expectant mothers of boys? In a word, than to guess according to folk signs, it is better to do an ultrasound. It definitely won't go wrong. nine0013
How to reduce the risk of age spots
Age spots are a temporary phenomenon, but not so pleasant. What rules should the expectant mother follow in order to reduce the likelihood of their occurrence?
-
Since pigmentation becomes more noticeable under the influence of ultraviolet rays, protect the skin from the sun: in summer, wear wide-brimmed hats, sunglasses, use sunscreen intended for children;
-
Carefully read the ingredients list of cosmetic products and choose those that do not contain vitamin A, which stimulates the formation of age spots: : green leafy vegetables, cabbage, quality vegetable oil, cereals, fish, liver and beets;
-
But fatty foods are best avoided, because they make the liver work in an enhanced mode, and this threatens with hyperpigmentation.
 nine0013
nine0013 -
Do not disregard the recommendation of the gynecologist to visit an endocrinologist. This is necessary to check the functioning of the thyroid gland.
Will we be treated?
Many experts believe that during pregnancy you should not take any drastic measures to combat hyperpigmentation, and advise you to calmly wait until it disappears by itself some time after childbirth. But among the doctors there are those who do not mind the use of traditional medicine. In that case , the expectant mother should understand that it is unlikely that it will be possible to completely get rid of this problem during the bearing of the baby, the pigmentation will only become less noticeable. And most importantly, before using any remedy, you must always consult a doctor.
These tips, of course, do not apply to cases where chloasma is caused by an exacerbation of chronic diseases. If this is the reason, serious attention should be paid to the treatment of the disease and strictly follow the recommendations of the attending doctor.