Teenage pregnancy labor and delivery
Teenage Pregnancy: Labor and Delivery
Labor is the process of giving birth. Delivery is the birth itself.
There are 3 Stages of Labor
Stage One
Stage Two
-
Starts when your cervix is 10 cm dilated.
-
Pushing the baby through the birth canal can take anywhere from 15 minutes to 2 hours.
-
This stage ends when the baby is delivered.
Stage Three
Things to Remember About Labor
-
Remember that no two labors are alike. Most women having their first baby are in labor anywhere from 14 to 19 hours.
-
If you think you are in labor, get in a comfortable position, drink a big glass of water and empty your bladder.
-
Keep track of how far apart your contractions are (from the start of one to the start of the next). You can use the last sheet of this Helping Hand.
-
If contractions do not get better within 30 minutes: call the Teen and Pregnant Clinic at 614-722-2450 and select option 2, OR CALL YOUR DELIVERY HOSPITAL.
True Labor
Contractions happen when the muscles of your uterus tighten. That causes pain. In true labor, contractions will help your baby through the birth canal.
True labor means your water has broken or your cervix is at least 4 cm dilated and changing with regular contractions.
When you are in true labor your contractions:
-
Get longer, stronger and closer together.
-
Are 60 to 120 seconds long (1 to 2 minutes). Contractions continue or increase with walking.
-
Can be felt in your back or entire abdomen.
-
Cause your cervix to soften, open and change.
You may have a “bloody show” (a pink tinged discharge from your vagina).
False Labor
When you are in false labor your contractions:
-
Are irregular.
 They do not get longer, stronger, or closer together.
They do not get longer, stronger, or closer together. -
Are 30 to 60 seconds long.
-
Decrease with walking or taking a bath.
-
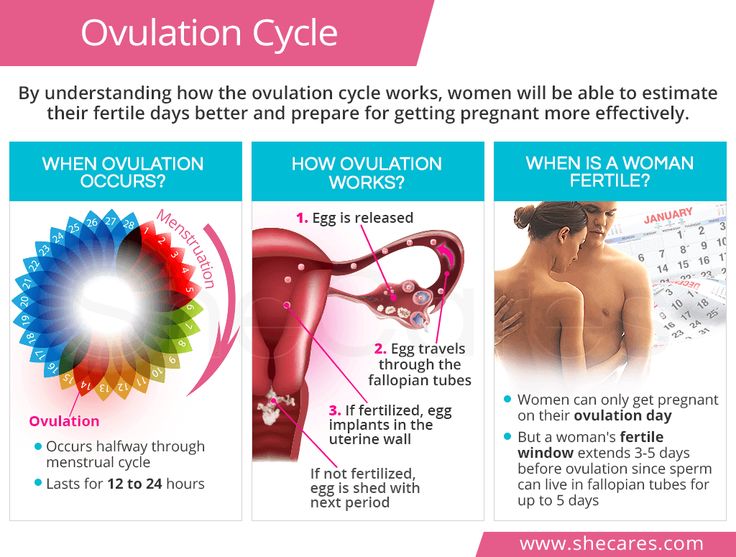
Sometimes feel like menstrual cramps.
-
Do not cause your cervix to change.
Braxton Hicks contractions are a mild tightening of your abdomen that comes and goes.
You should go to the Labor and Delivery area of your planned delivery hospital if you think you are in labor and you feel or see one or more of the following:
-
Contractions every 5 minutes, lasting at least a minute, and you have to stop to breathe to get through it.
-
Continuous leaking fluid or you think your water has broken.
-
More than a teaspoon of bright red blood.
-
Severe, constant pain or pressure in your abdomen or pelvic area.
-
Fewer than four fetal movements in an hour.

What Happens When You Go to the Hospital
-
If you think you have gone into labor, go directly to Labor and Delivery at your delivery hospital. DO NOT GO TO THE EMERGENCY ROOM FIRST.
-
If you are in active labor, the nurse will monitor the baby by putting a special belt on your belly. The belt “hears” and transmits the baby’s heartbeat. It will monitor your contractions, too. If the nurse cannot hear the baby well enough, a small internal wire monitor that attaches to the baby’s head will be placed. The monitor is easily removed after delivery and is safe for the baby.
-
The nurse will watch your contraction pattern and the baby’s heartbeat on a screen. This tells the doctors and nurses what is happening with your labor.
-
The nurse will check your cervix by doing a vaginal exam with her fingers. During most of your pregnancy, your cervix is closed. Your cervix will go from closed to 10 cm dilated (opened) as you have contractions.
 You may begin pushing when your cervix is 10 cm dilated and you have the urge to push.
You may begin pushing when your cervix is 10 cm dilated and you have the urge to push.
Warning Signs of Complications
-
A constant low backache that happens with contractions.
-
Change in color or odor of your vaginal discharge.
-
More than 6 contractions in an hour if you are less than 37 weeks pregnant.
-
The baby is moving less than usual.
-
Pain when you urinate (pee).
-
Headaches that do not go away when you take Tylenol® (acetaminophen).
-
Blurred vision or vision changes.
Common Reasons for C-Sections
-
The baby is not tolerating the stress of labor well.
-
The baby is in the wrong position for birth (like breech).
-
You are not making progress in labor (your cervix is not dilating).
Pain Management in Labor
Epidural
An epidural contains medicine that will make your body numb from your breasts down. A small needle is placed in your lower back followed by a small catheter (a very small tube). The catheter is left in your back, and the needle is removed while you are in labor. The medication is given to you through this catheter. The medication never “runs out.”
Pros of Epidurals
Cons of Epidurals
-
The medicine can cause your blood pressure to drop which can cause changes in the baby’s heart rate. This is usually easily corrected.
-
You may not have the urge to push, and you may not push as effectively.
-
Labor may slow or stop; therefore, you might need medicine to restart your labor.
Spinal
This is very similar to an epidural but is used in a c-section. The medicine is given through a small needle into your spinal fluid which provides fast pain relief. The medicine lasts long enough for you to have your C-section.
The medicine lasts long enough for you to have your C-section.
General anesthesia
This is when you are given medicine to make you lose consciousness during a c-section. It is only used in emergencies and is generally avoided.
IV medicine
These medicines are given to you through an IV at the hospital. These medicines go into your bloodstream, but are safe for the baby. They can be tried first if you aren’t sure that you want an epidural. These medicines will not take the pain away, but they will “take the edge off.” These medicines can cause sedation and may affect breastfeeding.
Labor Log Worksheet
If you think you are in labor, record when contractions start and end below. Use the “Comments” area to write the strength of your contractions. This will help you decide if you should go to the hospital.
| Time Contraction Began | How long did it last? | How long from the beginning of one contraction to the beginning of the next | Comments (mile, moderate, sever) |
| Examples | |||
| 9:00 a. | 30 seconds | - | Massage helps |
| 9:08 a.m. | 45 seconds | 8 minutes | It was a hard one |
| When your labor begins, record your contractions below | |||
Teenage Pregnancy: Labor and Delivery (PDF)
HH-IV-142 6/14 Copyright 2014, Nationwide Children’s Hospital
When Your Teen Is Having a Baby (for Parents)
If your daughter is pregnant and planning to have the baby, many changes await your family. And though it's certainly not what most parents expect, it happens every day: nearly 250,000 teenage girls in the United States give birth every year.
And though it's certainly not what most parents expect, it happens every day: nearly 250,000 teenage girls in the United States give birth every year.
If your teen is about to become a mother (or your son has fathered a child), it can be overwhelming for all of you. How can you support your child through the challenges that lie ahead?
What You May Be Feeling
If you have just learned that your teen is having a baby, you're probably experiencing a wide range of emotions, from shock and disappointment to grief and worry about the future.
Some parents feel a sense of guilt, thinking that if only they'd done more to protect their child this wouldn't have happened. And although some parents are embarrassed by their teen's pregnancy and worried about how family, friends, and neighbors will react, others are happy about the news of a soon-to-be grandchild — especially if the teen is older and in a mature relationship.
Whatever feelings you're experiencing, this is likely to be a difficult time for your family. The important thing is that your teen needs you now more than ever. Being able to communicate with each other — especially when emotions are running high — is essential. Teens who carry a baby to term have special health concerns, and your daughter will have a healthier pregnancy — emotionally and physically — if she knows she doesn't have to go it alone.
The important thing is that your teen needs you now more than ever. Being able to communicate with each other — especially when emotions are running high — is essential. Teens who carry a baby to term have special health concerns, and your daughter will have a healthier pregnancy — emotionally and physically — if she knows she doesn't have to go it alone.
So what can you do as the parent of a teen having a baby? Recognize your feelings and work through them so that you can accept and support her. Does that mean you don't have the right to feel disappointed and even angry? No. Such reactions are common. You might have a strong flood of emotions to deal with, especially at first. But the reality of the upcoming baby means that you'll have to get beyond your initial feelings for the sake of your daughter and her child.
If you need help coping with your feelings about the situation, talk to someone you trust or seek professional counseling. A neutral third party can be a great resource at a time like this.
Page 1
What Your Teen May Be Feeling
Just a short time ago your teen's biggest concerns might have been hanging out with her friends and wondering what clothes to wear. Now she's dealing with morning sickness and scheduling prenatal visits. Her world has been turned upside down.
Most unmarried teens don't plan on becoming pregnant, and they're often terrified when it happens. Many, particularly younger teens, keep the news of their pregnancies secret because they fear the anger and disappointment of their parents. Some might even deny to themselves that they are pregnant — which makes it even more important for parents to step in and find medical care for their teen as early in the pregnancy as possible. Younger teens' pregnancies, in particular, are considered high risk because their bodies haven't finished growing and are not yet fully mature.
Teen boys who are going to become fathers also need the involvement of their parents. Although some boys may welcome the chance to be involved with their children, others feel frightened and guilty and may need to be encouraged to face their responsibilities (the father is legally responsible for child support in every state).
That doesn't mean, however, that you should pressure your teen son or daughter into an unwanted marriage. Offer advice, but remember that forcing your opinions on your teen or using threats is likely to backfire in the long run. There's no "one size fits all" solution here. Open communication between you and your teen will help as you consider the future.
Page 2
Special Concerns of Pregnant Teens
Even though most teen girls are biologically able to produce healthy babies, whether they do often depends on whether they receive adequate medical care — especially in those critical early months of pregnancy.
Teens who receive proper medical care and take care of themselves are more likely to have healthy babies. Those who don't receive medical care are at greater risk for:
- fetal death
- high blood pressure
- anemia
- labor and delivery complications (such as premature labor and stillbirth)
- low birth-weight infant
The earlier your teen gets prenatal care, the better her chances for a healthy pregnancy, so bring her to the doctor as soon as possible after finding out she's pregnant. If you need help finding medical care, check with social service groups in the community or at your child's school.
If you need help finding medical care, check with social service groups in the community or at your child's school.
Your teen's health care provider can tell her what to expect during her pregnancy, how to take care of herself and her growing baby, and how to prepare for life as a parent.
Some topics that will be addressed include:
Medical Care
At her first prenatal visit, your teen will probably be given a full physical exam, including blood and urine tests. She'll be screened for sexually transmitted diseases (STDs) and for exposure to certain diseases, such as measles, mumps, and rubella.
Her health care provider also will discuss:
- how often prenatal visits should be scheduled
- what she may be feeling physically and emotionally
- what changes she can expect in her body
- how to deal with some of the uncomfortable side effects of pregnancy, like nausea and vomiting
Knowing what to expect can help alleviate some of the fears your daughter may have about being pregnant. Her health care provider will probably prescribe a daily prenatal vitamin to make sure she gets enough folic acid, iron, and calcium. Folic acid is especially important during the early weeks of pregnancy, when it plays a role in the healthy development of the neural tube (the structure that develops into the brain and spinal cord).
Her health care provider will probably prescribe a daily prenatal vitamin to make sure she gets enough folic acid, iron, and calcium. Folic acid is especially important during the early weeks of pregnancy, when it plays a role in the healthy development of the neural tube (the structure that develops into the brain and spinal cord).
Page 3
Lifestyle Changes
Your teen's health care provider will talk about the lifestyle changes she'll have to make for the health of her baby, including:
- not smoking (smoking while pregnant increases the risk of miscarriage, stillbirth, low birth weight, and sudden infant death syndrome)
- not drinking (alcohol causes mental and physical birth defects)
- not using drugs (drugs are associated with pregnancy complications and fetal death)
- not taking in more than 200 mg per day of caffeine (the amount in a 12-ounce cup of coffee)
- eating right
- getting enough rest
- avoiding risky sexual behaviors (such as having unsafe sex)
If your daughter smokes or uses alcohol or other drugs, her health care provider can offer ways to help her quit.
Nutrition
Fast food, soft drinks, sweets — teen diets are notoriously unbalanced. Eating well greatly increases your teen's chances of having a healthy baby, so encourage her to maintain a well-balanced diet that includes plenty of fruits, vegetables, and whole-grain breads (use the U.S. Department of Agriculture's MyPlate as a guide).
Important nutrients include:
- proteins (lean meat, fish, poultry, egg whites, beans, peanut butter, tofu)
- calcium (milk and other dairy products)
- iron (lean red meats, spinach, iron-fortified cereals)
- folic acid (green leafy vegetables, beans, peas, fortified cereals)
Drinking plenty of water is essential, too.
Pregnancy is not the time for your daughter to go on a diet. When pregnant, some teens might be tempted to counter normal pregnancy weight gain by cutting calories or exercising excessively — both of which can seriously harm their babies.
If you suspect that your teen has an unhealthy preoccupation with her weight, talk to her health care provider.
Page 4
Exercise
If your teen was physically fit before getting pregnant and is not experiencing any pregnancy complications, her health care provider will probably encourage her to continue exercising.
Most women benefit from getting some exercise during pregnancy, although they might have to modify their activity. Low-impact exercises, such as walking and swimming, are best. Have your daughter discuss her exercise plans with her health care provider early on.
Stress
Most teens enter parenthood unprepared for the stress a new baby brings, and many experience frustration, resentment, and even anger toward their newborns — which may explain why teen parents are at higher risk for abusing and neglecting their babies.
You may want to talk with your teen's doctor to discuss ways you can help her manage her stress levels so that she can better cope with changes in her life. She also may want to spend some time with other parents of newborns to get a better sense of what caring for a baby involves.
Prenatal Classes
Your daughter's health care provider will probably recommend that she take classes on pregnancy, giving birth, and parenting. These classes (some of which are held just for teens) can help prepare her for the practical side of parenthood by teaching skills such as feeding, diapering, child safety, and other basic baby care techniques.
Page 5
Preparing for New Responsibilities
Many practical issues must be considered. Will your teen keep the baby or consider adoption? If she keeps it, will she raise the baby herself? Will she continue to go to school? Will the father be involved in the baby's life? Who will be financially responsible for the baby?
The answers to these questions often depend on the support your daughter receives. Some teens raise their child alone, some have the involvement of the baby's father, and some rely on their families for support.
As a parent, you need to think about your own level of involvement and commitment and discuss it with your teen. How much support — financial and otherwise — are you willing and able to offer? Will your daughter and her child live with you? Will you help pay for food, clothing, doctor visits, and necessary items like a car seat and stroller? Can you assist with childcare while your she's at school and/or work? A social worker or counselor can help you and your teen sort through some of these issues.
How much support — financial and otherwise — are you willing and able to offer? Will your daughter and her child live with you? Will you help pay for food, clothing, doctor visits, and necessary items like a car seat and stroller? Can you assist with childcare while your she's at school and/or work? A social worker or counselor can help you and your teen sort through some of these issues.
If at all possible, it's best for girls who are pregnant to finish school so they can get better jobs and create a better life for themselves and their babies. This is no easy task — 60% to 70% of all pregnant teens drop out of school. And going back after quitting is especially hard, so try to offer your daughter the support she needs to stay in school — both she and the baby will benefit. Check for school and community programs that offer special services for teen mothers, such as childcare, transportation, or tutoring.
Help your teen understand that as rewarding as having a child is, it isn't always fun — caring for a baby is a huge responsibility and a lifelong commitment. Prepare her for the reality that she won't have as much time for the things she used to do — that her life is about change and the baby will take priority.
Prepare her for the reality that she won't have as much time for the things she used to do — that her life is about change and the baby will take priority.
As a parent, you can have a great impact on your teen's life and on her baby's. You may still wish that she had made different choices. But by supporting your daughter, making sure she gets good prenatal care, and listening as she shares her fears and anxieties, both of you may find that you're better parents in the long run.
Reviewed by: Steven Dowshen, MD
Date reviewed: September 2016
Pregnancy and childbirth in adolescence - Adolesmed
About 16 million women aged 15-19 give birth each year, accounting for about 11% of all births worldwide. 95% of these births occur in middle- and low-income countries. The average adolescent birth rate in middle-income countries is more than twice that of high-income countries, and five times higher in low-income countries.
Adolescent birth rate
in Eastern Europe and Central Asia
(number of live births per 1,000 women aged 15-19)
Source: Database TransMonEE http://www.
transmonee.org/ 2014,
* World Bank database http :// data . worldbank . org / indicators
While rates of teenage pregnancy are declining globally, there are significant regional and national variances. Early pregnancy occurs more frequently among the poorest and least educated adolescents. For some of these girls, pregnancy and childbirth is an expected and desired event, but not for everyone.
Risks for mother and child
According to the World Health Organization (WHO), pregnancy, abortion and childbirth during adolescence are among the leading causes of maternal and child mortality worldwide. The probability of stillbirth and death of newborns in adolescent mothers is 1.5 times higher than in women aged 20–29 years.
Most adolescent girls are not yet physically developed enough for safe pregnancy and childbirth. In early adolescence, girls are still growing, and their pelvises do not reach the size of adult women's pelvises. As a result, there is a high probability of disruption of normal labor activity. During pregnancy, nutrient requirements increase, which, in turn, can lead to slower growth of the girl. Finally, even if a pregnant teenage girl is physically ready for pregnancy, she most often lacks social and emotional maturity. Often a young mother has a negative attitude towards her unborn child, she refuses to breastfeed her baby and cannot provide him with proper care.
In early adolescence, girls are still growing, and their pelvises do not reach the size of adult women's pelvises. As a result, there is a high probability of disruption of normal labor activity. During pregnancy, nutrient requirements increase, which, in turn, can lead to slower growth of the girl. Finally, even if a pregnant teenage girl is physically ready for pregnancy, she most often lacks social and emotional maturity. Often a young mother has a negative attitude towards her unborn child, she refuses to breastfeed her baby and cannot provide him with proper care.
Pregnancy and childbirth in women under 18–20 years of age often occur with complications such as early and late gestosis, miscarriage, the threat of spontaneous abortion (miscarriage), impaired uterine contractility during childbirth, the birth of underweight children, fetal hypoxia during pregnancy and childbirth. The complicated course of childbirth occurs in most young women in labor.
Pregnant teenage girls are more likely to smoke and drink alcohol than older women, which can lead to many problems for the baby after birth. Children born to teenage mothers are more likely to have low birth weight and more likely to experience health problems compared to children born to older mothers. Children of adolescent mothers often have an age delay in the development of psychomotor skills, a high level of diseases of the central nervous system.
Children born to teenage mothers are more likely to have low birth weight and more likely to experience health problems compared to children born to older mothers. Children of adolescent mothers often have an age delay in the development of psychomotor skills, a high level of diseases of the central nervous system.
Social consequences of pregnancy for the adolescent mother
Even if the birth ended without harm to the reproductive and somatic health of the young mother, the psychological and social consequences can be very undesirable. Pregnancy can leave a girl out of school and prevent her from continuing her education after giving birth, which can lead to long-term unemployment or limit opportunities for well-paid and decent work.
A pregnant teenage girl and a young mother often find themselves in a difficult life situation due to the partner's refusal to share responsibility for the child and the lack of support from parents and other loved ones. Unable to support themselves and their children, young mothers often leave their children in the care of the state.
Unable to support themselves and their children, young mothers often leave their children in the care of the state.
Young mothers are more likely than older mothers to develop postpartum depression, and may experience mental health problems due to lack of support from family and friends, isolation from friends and family members, financial difficulties.
Most teenagers do not plan or expect pregnancy. Therefore, the very suspicion of a possible pregnancy can cause psychological shock. A girl may be faced with a difficult choice to keep or terminate the pregnancy, and this, with any decision, can lead to depression, and under the most unfavorable circumstances, suicide.
Pregnancy during adolescence can be the cause of an unplanned marriage. Often, persons entering into marriage as teenagers are characterized by a lower level of education, social status, and official position. Incomes in such families are low, and the families themselves often break up due to various reasons, including socio-economic ones.
Based on WHO materials, UNICEF manual "Adolescents at risk of HIV infection: A participant's book" Kyiv. 2012., and UNFPA manuals “Reproductive health counseling for adolescents and youth” Minsk, 2011.
Teenage pregnancy. What is Teen Pregnancy?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Teenage pregnancy is the state of carrying a developing embryo and fetus by an underage teenage girl. Clinically manifested by the same signs as gestation in adults: the absence of regular menstruation, causeless nausea and vomiting, changes in taste habits, engorgement of the mammary glands, hyperpigmentation of the areola and nipples, weight gain, and an increase in abdominal circumference. When making a diagnosis, they use the data of a gynecological examination, the results of a pregnancy test and ultrasound of the uterus. When the patient decides to keep the child, management tactics are aimed at the timely detection and correction of complications, the choice of an appropriate method of delivery.
- Causes of teenage pregnancy
- Pathogenesis
- Classification
- Symptoms of teenage pregnancy
- Complications
- Diagnostics
- Management of teenage pregnancy
- Prognosis and prevention
- Prices for treatment
General
Teenage pregnancy is not only a medical problem, but also a social one. In developed countries, its prevalence reaches 12 cases per 1,000 adolescents, in Russia this figure is 8-9times higher. According to WHO, about 16 million girls aged 15-19 years old give birth to children every year, which is up to 11% of all births in the world. 95% of such cases are detected in countries with low and middle incomes. The level of teenage pregnancy is largely influenced by national and religious traditions - in Islamic states it is much less common. According to statistics, up to 30% of pregnancies in girls end in artificial interruption, 14% in miscarriage, and 56% in childbirth. Two thirds of minors give birth out of wedlock. According to the social status, 72% of patients study at school, vocational schools or are housewives.
95% of such cases are detected in countries with low and middle incomes. The level of teenage pregnancy is largely influenced by national and religious traditions - in Islamic states it is much less common. According to statistics, up to 30% of pregnancies in girls end in artificial interruption, 14% in miscarriage, and 56% in childbirth. Two thirds of minors give birth out of wedlock. According to the social status, 72% of patients study at school, vocational schools or are housewives.
Teenage pregnancy
Causes of teenage pregnancy
Physiological opportunities for fertilization of the egg arise in the girl after the onset of the first menstruation (menarche). However, the real causes of early pregnancy are not related to the biological, but to the social aspect. The provocative factors differ in different countries and are largely determined by the level of economic development, the organization of education and medical care, local norms and traditions. According to experts in the field of obstetrics and gynecology, the onset of pregnancy in adolescence is facilitated by:
According to experts in the field of obstetrics and gynecology, the onset of pregnancy in adolescence is facilitated by:
- Insufficient sexual education and education. Adolescents are not always fully aware of the consequences of unprotected sex, the need and rules for contraception. This is due to the lack of targeted programs for the sexual education of schoolchildren, the sanctimonious attitude of adults, and examples of the asocial lifestyle that parents lead.
- Sexual emancipation. 9 out of 10 girls have their first sexual experience before the age of 20. This is facilitated by the availability of low-alcohol drinks, narcotic substances, and pornographic materials. Studies have shown that teens who watch TV shows and movies with sex scenes are at twice the risk of early pregnancy.
- Contraceptive prejudice. There is still a persistent stereotype in society that the use of male barrier contraceptives reduces the severity of pleasure and affects the romanticism of relationships.
As a result, some girls and young women, in fear of losing their partners, are embarrassed to ask them for condom protection.
- Sexual abuse. About 10% of pregnant adolescents under the age of 15 report the forced nature of their first sexual relationship. Often, coercion to have sex is caused by the girl's being in an unfavorable social environment, much less often it is an element of blackmail by a partner who threatens to end the romantic relationship.
- Poor socio-economic situation. This reason is one of the most significant for low-income countries. For some adolescents, the financial allowance at the birth of a child and social assistance provided until they reach a certain age become a significant argument in favor of early motherhood, and sometimes the only source of income.
Some of these reasons are relevant for poor countries with high unemployment, inaccessibility of educational and medical services, and low incomes. However, the increase in the frequency of early pregnancy in developed countries indicates the shortcomings of the implemented state policy and the lack of targeted efforts aimed at solving this problem.
Pathogenesis
Although, in general, the development of teenage pregnancy is based on the same mechanisms as normal, it has a number of features that affect the course of the gestational period and childbirth. First of all, these features are associated with the functional immaturity of the genital organs and endocrine regulation systems. In adolescence, complications of pregnancy are more often noted, and the likelihood of traumatism in childbirth increases. The onset of gestation in a teenager leads to an acceleration of the processes of puberty and somatic maturation - the size of the bone pelvis increases to typical for 16-18-year-old girls, which, combined with sufficient hydrophilicity and elasticity of the ligamentous apparatus, makes the bone ring more pliable.
Classification
In order to predict the development and choose the optimal tactics for supporting teenage pregnancy, it is advisable to systematize, taking into account a number of medical, physiological and social factors. Such a classification allows you to identify the risks of the gestational period in advance, prevent possible complications and determine the optimal delivery option. The main criteria for systematizing teenage pregnancy are:
Such a classification allows you to identify the risks of the gestational period in advance, prevent possible complications and determine the optimal delivery option. The main criteria for systematizing teenage pregnancy are:
- Menstrual age (MW). Taking into account the time of onset of menarche, groups of pregnant adolescents with a menstrual age of up to 1 year, 2 years, 3 years and more are distinguished. The lower the MV, the more likely the pathological course of pregnancy, childbirth and the postpartum period.
- Age of the pregnant woman. Girls under 9 years of age with accelerated sexual development are called "super-young primiparas", at the age of 9-15 years with incomplete puberty - "young primiparas", at 15-18 years old - adolescents ready for the implementation of childbearing function.
- State of health. Depending on the presence of concomitant pathology, there are categories of completely healthy pregnant adolescents, young pregnant women suffering from extragenital diseases, and adolescent girls with complications of the gestational period.

- Circumstances of pregnancy. There are primiparous girls with a desired pregnancy from prosperous and complete families, young pregnant women with an unwanted pregnancy from dysfunctional and single-parent families, adolescents who become pregnant due to rape.
Symptoms of teenage pregnancy
The key sign of onset gestation is the absence of another menstruation, although girls with an irregular monthly cycle may underestimate the significance of this symptom. A possible pregnancy is evidenced by the appearance of unreasonable nausea and vomiting, a change in taste and food preferences, breast engorgement, soreness in the nipple-areolar zone. As the uterus grows, the urge to urinate becomes more frequent, weight gain and an increase in the circumference of the abdomen are observed. Adolescent pregnancies are characterized by sudden mood swings with emotional lability, tearfulness, and tantrums. Often girls complain of unusual drowsiness, general weakness and fatigue.
Complications
Pregnancy and childbirth put an increased burden on the immature teenage body. In addition, in recent years there has been a significant deterioration in the somatic and reproductive health of girls - up to 75-86% of adolescents suffer from chronic somatic diseases, from 10 to 15% have genital pathology that affects fertility. As a result, teenage pregnancy often has a complicated course. Underage pregnant women are three times more likely to suffer from treatment-resistant anemia. Every second girl has preeclampsia, which manifests on average 12-14 days earlier, mostly has a moderate or severe course. Due to the presence of concomitant genital infections in the adolescent age group, the likelihood of developing an ectopic pregnancy increases.
Fetoplacental insufficiency with hypoxia, antenatal distress and fetal growth retardation is more often formed in pregnant girls of menstrual age 1-2 years. Insufficient secretion of steroids by the fetoplacental system leads to anomalies in the birth forces. With a teenage pregnancy, the risk of spontaneous abortions and premature births increases. Hypoglobulinemia and insufficient reserve potential of phagocytes provoke immune failure, which is manifested by an increase in infectious and inflammatory processes at the gestational and postpartum stages.
With a teenage pregnancy, the risk of spontaneous abortions and premature births increases. Hypoglobulinemia and insufficient reserve potential of phagocytes provoke immune failure, which is manifested by an increase in infectious and inflammatory processes at the gestational and postpartum stages.
The course of childbirth directly depends on the menstrual age of the minor. With CF up to 1-2 years, anatomical or functional narrowing of the pelvis is observed in 50-66% of primiparas, breech presentation occurs more often, childbirth is complicated by spastic irregular contractions in the preliminary period, violent labor, primary weakness of the labor force, traumatization of soft tissues, hypotonic postpartum hemorrhage arising from pathological attachment of the placenta. Girls with 3-year-old CF often give birth quickly or rapidly, they have signs of primary weakness or incoordination of labor, there are ruptures of the birth canal, especially the perineum and cervix. After childbirth, postpartum endometritis, subinvolution of the uterus, hypogalactia and agalactia are detected twice as often in juvenile women in labor.
After childbirth, postpartum endometritis, subinvolution of the uterus, hypogalactia and agalactia are detected twice as often in juvenile women in labor.
Diagnostics
A feature of teenage pregnancy is its late diagnosis, due to the fact that up to 35-55% of girls do not suspect that they are carrying a child, or hide it. Often, adolescents turn to an obstetrician-gynecologist only at a later date, and 8-11% of underage pregnant women are not registered at all. The "gold" standard for diagnosing the condition is based on identifying the same presumptive, probable and reliable signs as in the adult reproductive group. To finally confirm pregnancy in a girl with a delay in menstruation, they carry out:
- Chair examination. With bimanual palpation, an increase in the uterus to the probable gestational age, softening of its isthmus, and increased mobility of the cervix are determined. Examination in the mirrors allows you to identify possible signs of a genital infection (inflammation of the vaginal mucosa, discharge from the cervical canal).

- Pregnancy test. Laboratory diagnostics is based on the determination of chorionic gonadotropin in the urine, a specific hormone that begins to be secreted from the time of implantation of a fertilized egg in the uterus. Modern inkjet tests are highly sensitive, and their reliability reaches 99%.
- Ultrasound of the uterus. Sonographic examination is the most popular and affordable method that reliably confirms the fact of pregnancy in a teenager. With the help of ultrasound in the uterine cavity, the fetus, placenta, membranes are detected. Regular screening allows you to dynamically monitor gestation, and fetometry - to assess the development of the fetus.
To exclude a possible infectious and inflammatory pathology of the genital organs, microscopy of a smear from the vagina, bacteriological seeding on nutrient media, TORCH-complex, RIF, ELISA, PCR diagnostics are performed. Subsequently, CTG is recommended for early detection of signs of fetoplacental insufficiency. Differential diagnosis is carried out with neoplasms of the abdominal cavity and small pelvis, malformations of the uterus, hypothalamic-pituitary disorders, primary ovarian insufficiency, metabolic and endocrine disorders in diabetes mellitus, hypofunction and hyperfunction of the thyroid gland, and other diseases accompanied by amenorrhea. According to the indications, the patient is consulted by an adolescent pediatrician, an endocrinologist, an infectious disease specialist, a dermatologist, a neuropathologist, a neurosurgeon, a psychologist, and a psychiatrist.
Differential diagnosis is carried out with neoplasms of the abdominal cavity and small pelvis, malformations of the uterus, hypothalamic-pituitary disorders, primary ovarian insufficiency, metabolic and endocrine disorders in diabetes mellitus, hypofunction and hyperfunction of the thyroid gland, and other diseases accompanied by amenorrhea. According to the indications, the patient is consulted by an adolescent pediatrician, an endocrinologist, an infectious disease specialist, a dermatologist, a neuropathologist, a neurosurgeon, a psychologist, and a psychiatrist.
Management of teenage pregnancy
After detecting gestation, a teenage girl, her relatives and employees of a medical institution need to decide on the advisability of bearing a child, patient management tactics and the optimal method of delivery. Possible options for solving the problem, taking into account all possible factors and the opinion of the pregnant woman, can be:
- Induced abortion.
 The girl and her relatives need to be explained that medical or surgical abortion performed at adolescence is more often complicated by traumatic injuries of the uterus, inflammation of the reproductive organs, and a violation of the ovarian cycle. In the future, such patients increase the likelihood of miscarriage and infertility. If a girl insists on terminating a pregnancy, it is important to intervene at an earlier date.
The girl and her relatives need to be explained that medical or surgical abortion performed at adolescence is more often complicated by traumatic injuries of the uterus, inflammation of the reproductive organs, and a violation of the ovarian cycle. In the future, such patients increase the likelihood of miscarriage and infertility. If a girl insists on terminating a pregnancy, it is important to intervene at an earlier date. - Pregnancy with natural delivery. The management of young primiparas does not differ significantly from standard protocols and involves the timely correction of emerging complications. In more than 90% of cases, a teenage girl is able to give birth to a child on her own. Even with an anatomically narrow pelvis, a clinical discrepancy between the size of the fetal head and the mother's pelvis is observed in only 10% of patients, which is associated with the frequent onset of preterm birth.
- Pregnancy and caesarean section. The decision to operate in each case is made individually, and the young age of the patient should not be taken as an obstacle to timely surgical intervention.
 Indications for operative delivery in adolescent women in labor are the same as in adult women. A caesarean section is performed when anomalies of labor activity that are resistant to conservative therapy, a clinically narrow pelvis, and signs of intranatal fetal hypoxia are detected.
Indications for operative delivery in adolescent women in labor are the same as in adult women. A caesarean section is performed when anomalies of labor activity that are resistant to conservative therapy, a clinically narrow pelvis, and signs of intranatal fetal hypoxia are detected.
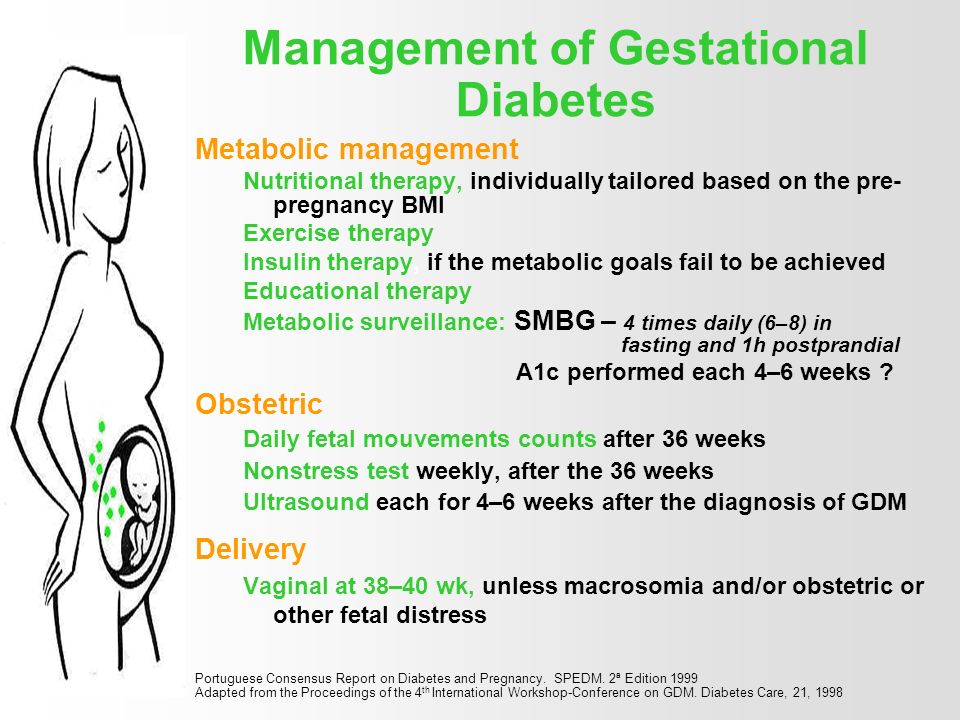
When managing a girl carrying a child, an obstetrician-gynecologist pays attention to both the medical aspects of pregnancy and the correction of the patient's lifestyle. Since the adolescent age group often eat irregular and unbalanced meals, the importance of rational diet and food intake is being educated. Particular attention is paid to the discussion of smoking, alcohol and drug use, prevention of sexually transmitted infections, psychoprophylactic preparation for the upcoming birth. Given the increased risk of complications in childbirth, pregnant adolescents are shown hospitalization in highly qualified obstetric hospitals for 37-39week of gestational age.
Prognosis and prevention
The prognosis with proper management of teenage pregnancy and the choice of the optimal method of delivery is favorable.
 m.
m.