Symptoms of toxoplasma in pregnancy
Toxoplasmosis | March of Dimes
Toxoplasmosis is an infection you can get from eating undercooked meat or touching cat poop.
Most times, there are no symptoms so you may not know that you have toxoplasmosis.
If you get toxoplasmosis just before or during pregnancy, you may pass it to your baby.
Toxoplasmosis can cause problems during pregnancy, including miscarriage, preterm birth or stillbirth.
Most babies born with toxoplasmosis have no symptoms. Symptoms can include eye infections, swollen glands, liver or spleen, or jaundice.
Toxoplasmosis is an infection you can get from eating undercooked meat or touching cat poop or a litter box. It’s caused by a very common parasite called Toxoplasma gondii. The parasite is so tiny you can’t see it.
More than 40 million people in the United States may have the parasite. Very few people have symptoms because a healthy immune system usually keeps the parasite from causing an infection. However, toxoplasmosis can cause health problems for you and your baby during pregnancy.
How do you get infected with toxoplasmosis?
You can come in contact with the parasite that causes the infection through:
- Eating raw or undercooked meat or shellfish
- Eating unwashed fruits and vegetables
- Touching cat litter or poop
- Touching kitchen utensils and cutting boards used to prepare raw or undercooked meat and fruits and vegetables
- Touching dirt or sand
- Touching stray cats
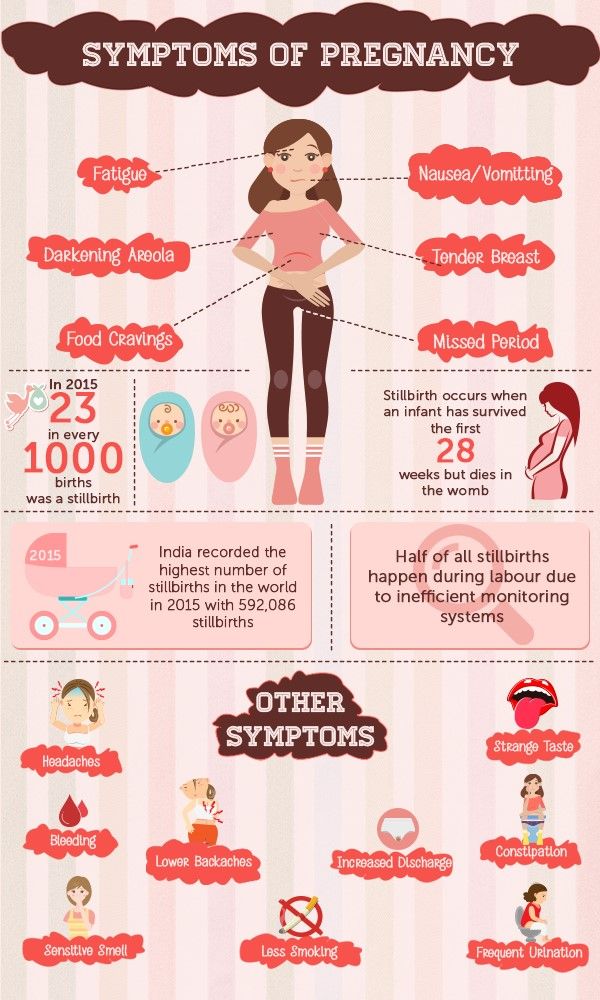
What are the signs and symptoms of toxoplasmosis?
You may not know if you have the infection. Many times there are no symptoms. For some people, it feels like the flu. Symptoms can include:
- Achy muscles
- Headache
- Fatigue (tiredness)
- Fever
- Swollen glands
- Blurry vision
- Eye redness
These symptoms can last for a month or longer. If you think you have toxoplasmosis, talk to your health care provider. Your provider can give you a blood test to find out if you have the infection. Even though blood tests are a regular part of prenatal care, you don’t usually get tested for toxoplasmosis. So be sure to talk to your provider if you think you have the infection.
Your provider can give you a blood test to find out if you have the infection. Even though blood tests are a regular part of prenatal care, you don’t usually get tested for toxoplasmosis. So be sure to talk to your provider if you think you have the infection.
Can toxoplasmosis cause problems before pregnancy?
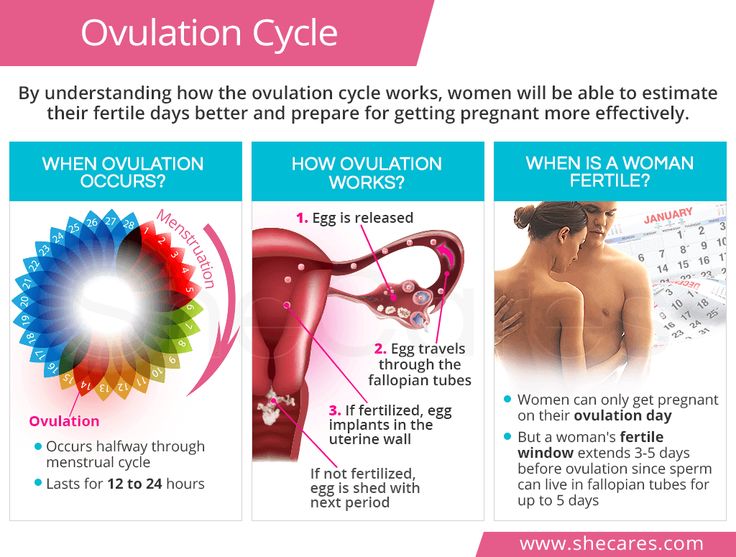
If you have toxoplasmosis within 6 months of getting pregnant, you may be able to pass it to your baby during pregnancy. Talk to your health care provider about being tested. Wait 6 months after a toxoplasmosis infection before trying to get pregnant.
Can toxoplasmosis cause problems during pregnancy?
Yes. Pregnancy complications caused by toxoplasmosis include:
- Preterm birth – Birth that happens before 37 weeks of pregnancy
- Stillbirth – When a baby dies after 20 weeks of pregnancy
- Miscarriage -- When a baby dies before 20 weeks of pregnancy
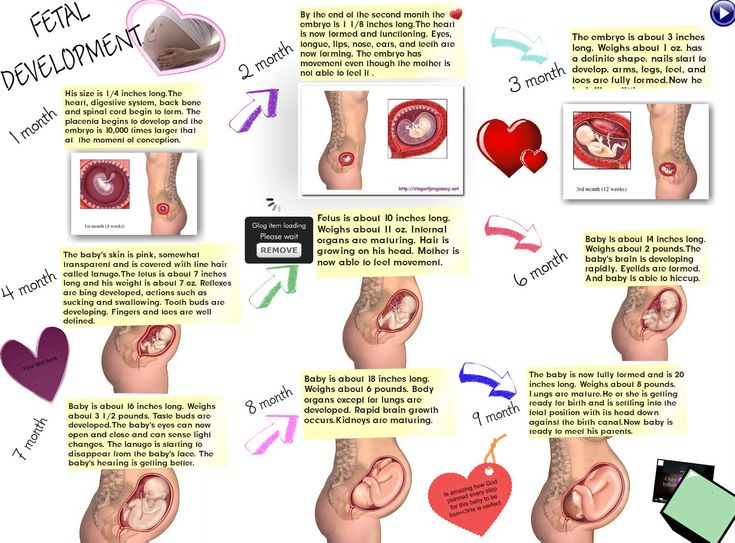
If you get toxoplasmosis just before or during pregnancy, you may pass the infection to your baby even if you don’t have any symptoms. The risk of passing the infection to your baby depends on how far along in your pregnancy you were when you were infected. The later in your pregnancy that you get infected (third trimester), the more likely it is that your baby will also get infected. But the earlier in pregnancy you get infected, the more serious the baby’s problems may be after birth. For example, your baby could have damage to the liver, brain and eyes. Up to 1 in 2 babies (50 percent) who are infected with toxoplasmosis during the pregnancy are born early (preterm). Some infected babies may die.
The risk of passing the infection to your baby depends on how far along in your pregnancy you were when you were infected. The later in your pregnancy that you get infected (third trimester), the more likely it is that your baby will also get infected. But the earlier in pregnancy you get infected, the more serious the baby’s problems may be after birth. For example, your baby could have damage to the liver, brain and eyes. Up to 1 in 2 babies (50 percent) who are infected with toxoplasmosis during the pregnancy are born early (preterm). Some infected babies may die.
If you have toxoplasmosis during pregnancy, there are several ways your health care provider can check to see if your baby is infected:
Amniocentesis. An amniocentesis (also called amnio) can test the fluid around your baby for infection. You can get this test at 15 to 20 weeks of pregnancy. It also can be tested for other problems with the baby, like birth defects or genetic problems.
Ultrasound. About 1 in 3 babies infected with toxoplasmosis have a problem that can be seen on an ultrasound. Ultrasound (also called sonogram) is a prenatal test that uses sound waves to show a picture of your baby before they are born. Ultrasound helps your provider check on your baby’s health and development. Most pregnant people get an ultrasound in their second trimester at 18 to 20 weeks of pregnancy.
About 1 in 3 babies infected with toxoplasmosis have a problem that can be seen on an ultrasound. Ultrasound (also called sonogram) is a prenatal test that uses sound waves to show a picture of your baby before they are born. Ultrasound helps your provider check on your baby’s health and development. Most pregnant people get an ultrasound in their second trimester at 18 to 20 weeks of pregnancy.
Blood test. Your baby’s blood can be tested for toxoplasmosis after birth.
How can toxoplasmosis during pregnancy harm your baby?
Most babies born with toxoplasmosis have no symptoms. But about 1 in 10 babies (10 percent) with the infection are born with problems, including:
- Eye infections or eye inflammation
- Swollen liver and spleen
- Jaundice (when a baby's eyes and skin look yellow.)
- Seizures or convulsions
- Fluid on the brain (hydrocephalus)
- Swollen lymph nodes
- Large head size (macrocephaly) or smaller-than-normal head size (microcephaly)
- Feeding problems
- Low birthweight
- Skin rash or bruising
Without treatment, newborns may develop problems later in life, even if they show no symptoms earlier. This can happen even 20 or 30 years later. These problems include:
This can happen even 20 or 30 years later. These problems include:
- Intellectual and developmental disabilities (problems with how the brain works that can cause your baby trouble or delays in physical development, learning, communicating, taking care of themselves or getting along with others).
- Eye infections and vision problems
- Pneumonia
- Cerebral palsy (a group of conditions that affects the parts of the brain that control the muscles. It can cause problems with movement, posture,standing up straight and balance).
- Seizures or convulsions
- Hearing loss
Each year, between 800 and 4,400 babies in the United States are born with toxoplasmosis. If you think you had toxoplasmosis during pregnancy, be sure your baby is tested.
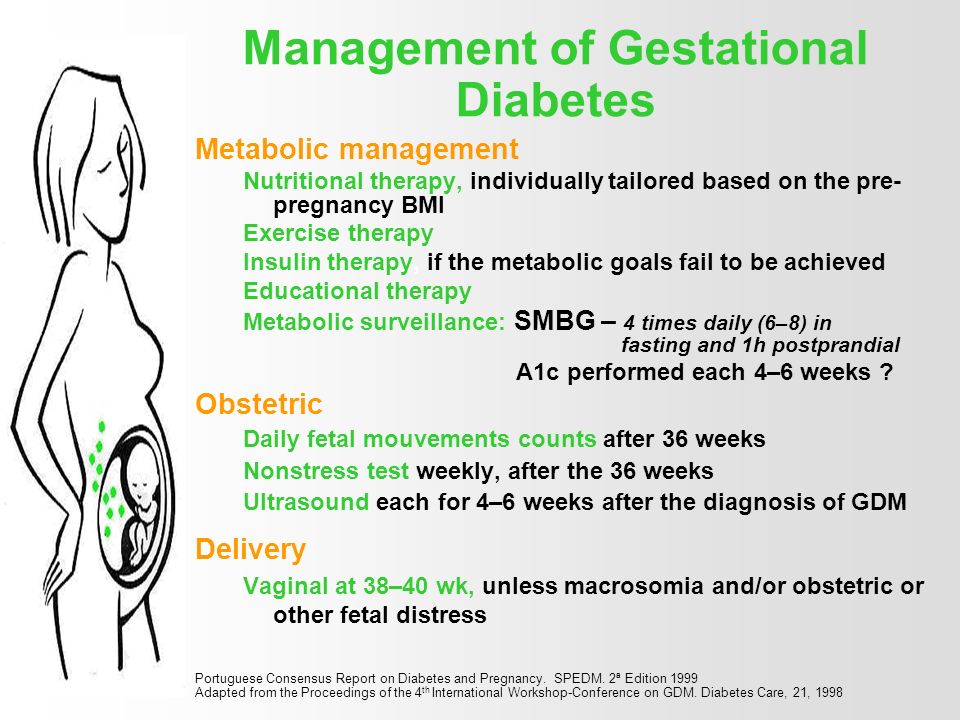
How is toxoplasmosis treated during pregnancy?
If you are infected during pregnancy, both you and your baby should be closely monitored during your pregnancy and after the baby is born. Getting treated with certain antibiotics helps reduce the chance of your baby getting toxoplasmosis. Antibiotics are medicines that treat certain types of infections. This treatment also helps reduce the seriousness of any symptoms your baby may have.
Getting treated with certain antibiotics helps reduce the chance of your baby getting toxoplasmosis. Antibiotics are medicines that treat certain types of infections. This treatment also helps reduce the seriousness of any symptoms your baby may have.
If you’re infected before 18 weeks of pregnancy, your provider may give you an antibiotic called spiramycin. This medicine helps reduce the chance of your baby getting the infection.
If you’re infected after 18 weeks of pregnancy, your provider may give you different antibiotics called pyrimethamine, sulfadiazine or leucovorin. These medicines are recommended for use after 18 weeks of pregnancy. If you take them before 18 weeks of pregnancy, they may cause birth defects in your baby.
How is toxoplasmosis treated in your baby after birth?
If your baby shows symptoms of toxoplasmosis, the provider may treat your baby with antibiotics. Your baby may continue these antibiotic treatments until their first birthday, sometimes even longer.
Should you nurse your baby if you had toxoplasmosis during pregnancy?
Yes. Your provider can give you a blood test to find out if you are still infected. If you are healthy and no longer infected, the chances of giving your baby toxoplasmosis while nursing is very small. Don’t nurse your baby if you have cracked and bleeding nipples or breast inflammation if you were infected recently.
How can you prevent toxoplasmosis?
Here’s how to protect yourself from toxoplasmosis:
- Don’t eat raw, undercooked or contaminated meat, especially lamb, pork or venison. Cooked meat should not look pink, and the juices should be clear. Use a meat thermometer to check the temperature of the meat before you eat it.
- Don’t eat raw, undercooked or contaminated shellfish, such as oysters, clams or mussels.
- Do not drink raw milk, especially goat’s milk.
- Wash your hands with soap and water after handling fruits, vegetables or raw meat, poultry (such as chicken or turkey) or shellfish.
- Don’t touch your eyes, nose or mouth when handling raw meat.
- Clean cutting boards, work surfaces and utensils with hot, soapy water after using them with fruits, vegetables or raw meat.
- Peel or thoroughly wash all raw fruits and vegetables before eating.
- Use work gloves when you’re gardening. Wash your hands afterward.
If you have a cat:
- Don’t let your cat go outside your home, where it may eat spoiled food or come in contact with the parasite.
- Change your cat’s litter box daily. Ask someone else to clean the litter box. If you have to do it yourself, wear gloves. Wash your hands thoroughly when you’re done emptying the litter.
- Only feed your cat canned or dried cat food from the store or well-cooked table food. Don’t feed your cat raw or uncooked meat.
- Stay away from children’s sandboxes. Cats like to use them as litter boxes.
- Don’t touch stray cats or kittens.
Last updated August 2021
CDC - Toxoplasmosis - General Information
On This Page
- When should I be concerned about toxoplasmosis?
- How can Toxoplasma affect my baby?
- How do I know if I have been infected with Toxoplasma?
- How is toxoplasmosis spread?
- Do I have to give up my cat if I’m pregnant or planning on becoming pregnant?
- Is there treatment available for toxoplasmosis?
- What are the best ways to protect myself or my baby against toxoplasmosis?
- Can I breastfeed my baby if I contracted a Toxoplasma infection during pregnancy?
When should I be concerned about toxoplasmosis?
Generally, if you were infected with Toxoplasma before becoming pregnant your baby is protected by your immunity.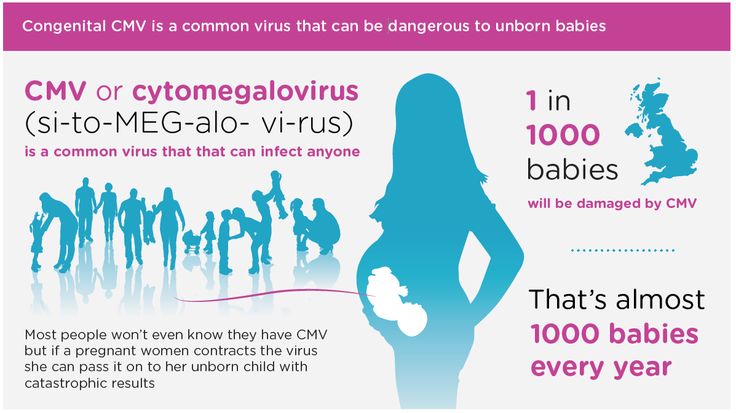 Some experts suggest waiting for 6 months after a recent infection to become pregnant.
Some experts suggest waiting for 6 months after a recent infection to become pregnant.
How can
Toxoplasma affect my baby?If you are newly infected with Toxoplasma while you are pregnant, or just before pregnancy, then you can pass the infection on to your baby. You may not have any symptoms from the infection. Most infected infants do not have symptoms at birth but can develop serious symptoms later in life, such as blindness or mental disability. Occasionally, infected newborns have serious eye or brain damage at birth.
How do I know if I have been infected with
Toxoplasma?Your health care provider may suggest one or more varieties of blood tests to check for antibodies to Toxoplasma.
How is toxoplasmosis spread?
Cats play an important role in the spread of toxoplasmosis. They become infected by eating infected rodents, birds, or other small animals. The parasite is then passed in the cat’s feces. Kittens and cats can shed millions of parasites in their feces for as long as 3 weeks after infection.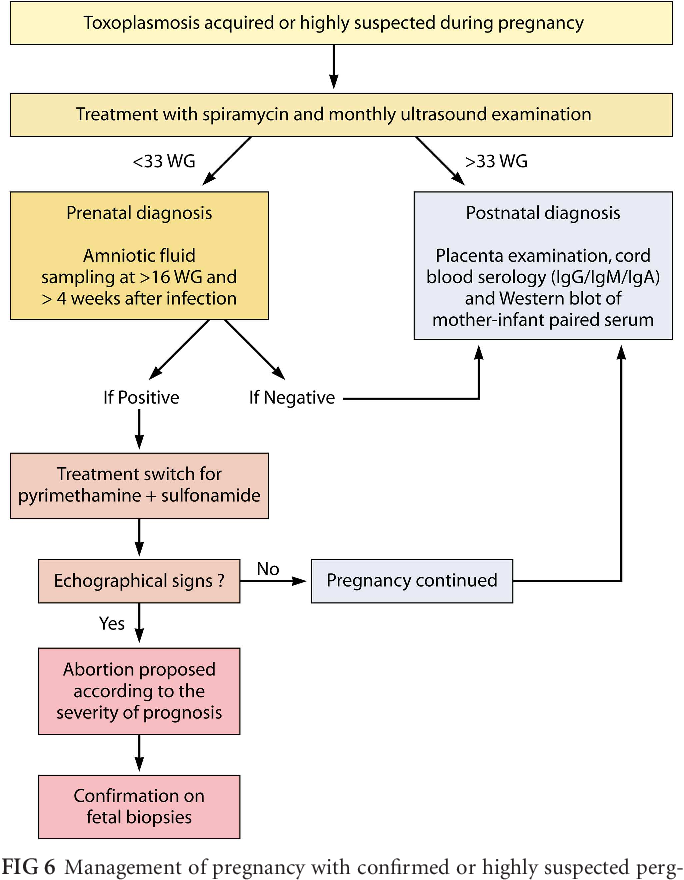 Mature cats are less likely to shed Toxoplasma if they have been previously infected. Cats and kittens prefer litter boxes, garden soils, and sandboxes for elimination, and you may be exposed unintentionally by touching your mouth after changing a litter box, or after gardening without gloves. Fruits and vegetables may have contact with contaminated soil or water also, and you can be infected by eating fruits and vegetables if they are not cooked, washed, or peeled.
Mature cats are less likely to shed Toxoplasma if they have been previously infected. Cats and kittens prefer litter boxes, garden soils, and sandboxes for elimination, and you may be exposed unintentionally by touching your mouth after changing a litter box, or after gardening without gloves. Fruits and vegetables may have contact with contaminated soil or water also, and you can be infected by eating fruits and vegetables if they are not cooked, washed, or peeled.
Cats play an important role in the spread of toxoplasmosis.
Do I have to give up my cat if I’m pregnant or planning on becoming pregnant?
No. You should follow these helpful tips to reduce your risk of environmental exposure to Toxoplasma:
- Avoid changing cat litter if possible. If no one else can perform the task, wear disposable gloves and wash your hands with soap and water afterwards.
- Ensure that the cat litter box is changed daily. The Toxoplasma parasite does not become infectious until 1 to 5 days after it is shed in a cat’s feces.

- Feed your cat commercial dry or canned food, not raw or undercooked meats.
- Keep cats indoors.
- Avoid stray cats, especially kittens. Do not get a new cat while you are pregnant.
- Keep outdoor sandboxes covered.
- Wear gloves when gardening and during contact with soil or sand because it might be contaminated with cat feces that contain Toxoplasma. Wash hands with soap and water after gardening or contact with soil or sand.
More on: Handwashing
Is there treatment available for toxoplasmosis?
If you are infected during pregnancy, medication is available. You and your baby should be closely monitored during your pregnancy and after your baby is born.
What are the best ways to protect myself or my baby against toxoplasmosis?
Cat owners and women who are exposed to cats should follow these tips to reduce exposure to Toxoplasma.
- Avoid changing cat litter if possible.
 If no one else can perform the task, wear disposable gloves and wash your hands with soap and water afterwards.
If no one else can perform the task, wear disposable gloves and wash your hands with soap and water afterwards. - Ensure that the cat litter box is changed daily. The Toxoplasma parasite does not become infectious until 1 to 5 days after it is shed in a cat’s feces.
- Feed your cat commercial dry or canned food, not raw or undercooked meats.
- Keep cats indoors.
- Avoid stray cats, especially kittens. Do not get a new cat while you are pregnant.
- Keep outdoor sandboxes covered.
- Wear gloves when gardening and during contact with soil or sand because it might be contaminated with cat feces that contain Toxoplasma. Wash hands with soap and water after gardening or contact with soil or sand.
- Wash your hands and safely diaper and feed your baby.
Along with washing your hands, you should also:
- Cook food to an internal temperatures high enough to kill harmful pathogens like Toxoplasma. The only way to tell if food is safely cooked is to use a food thermometer.
 You can’t tell if food is safely cooked by checking its color and texture (except for seafood).
You can’t tell if food is safely cooked by checking its color and texture (except for seafood). - Use a food thermometer to ensure foods are cooked to a safe internal temperature. Learn how to place the thermometer correctlyin different food to get an accurate reading.
- Whole cuts of beef, veal, lamb, and pork, including fresh ham: 145°F (then allow the meat to rest for 3 minutes before carving or eating)
- Fish with fins: 145°F or cook until the flesh is opaque and separates easily with a fork
- Ground meats, such as beef and pork: 160°F
- All poultry, including ground chicken and turkey: 165°F
- Leftovers and casseroles: 165°F
- Check this chart for a detailed list of temperatures and foods
- Freeze meat for several days at sub-zero (below 0° F) temperatures before cooking to greatly reduce chance of infection. *Freezing does not reliably kill other parasites that may be found in meat (like certain species of Trichinella) or harmful bacteria.

- Avoid drinking untreated water.
- Do not drink unpasteurized goat’s milk.
- Do not eat raw or undercooked oysters, mussels, or clams (these may be contaminated with Toxoplasma that has washed into seawater).
- For more information on safe food handling to help reduce foodborne illness visit the Food Safety website.
Can I breastfeed my baby if I contracted a
Toxoplasma infection during pregnancy?Yes. Breast milk transmission of Toxoplasma infection is not likely. While Toxoplasma infection has been associated with infants who consumed unpasteurized goat’s milk, there are no studies documenting breast milk transmission of Toxoplasma infection in humans. If a nursing woman were to experience cracked and bleeding nipples or breast inflammation within several weeks following recent Toxoplasma infection (when the organism is still in her bloodstream), it is theoretically possible that she could transmit Toxoplasma to the infant through her breast milk. Immune suppressed women could have Toxoplasma in their bloodstream for longer periods of time. However, the likelihood of human milk transmission is still very small.
Immune suppressed women could have Toxoplasma in their bloodstream for longer periods of time. However, the likelihood of human milk transmission is still very small.
External
Back To Top
Toxoplasmosis during pregnancy - Juno
Contents of the article
How you can get toxoplasmosis
The causative agent is Toxoplasma (the simplest intracellular parasite). Its carriers are mostly domestic animals. Toxoplasma finally settles in the body of cats, but can choose birds and mammals as an intermediate place of residence. Sick animals infect the soil, grass, vegetable gardens.
The main ways of infection with toxoplasmosis during pregnancy:
- eating undercooked or raw meat, as well as unwashed vegetables, herbs;
- work with the earth, for example in a vegetable garden;
- interaction with cat waste products;
- organ transplant, blood transfusion;
- in utero - from mother to fetus.

The causative agent is not transmitted from a sick person through sexual or airborne droplets. During pregnancy, 1% of women become infected with toxoplasmosis, while 20% pass the infection to the fetus.
Causes of toxoplasmosis during pregnancy
If a woman had an infection long before pregnancy - in childhood or adolescence, then the disease is not dangerous for her. After suffering toxoplasmosis, antibodies are formed that protect the mother and baby.
However, if the infection occurred within six months before conception, the health of the mother and child may be at risk. It takes time for the formation of antibodies - at least 6 months after the disease. Accordingly, when they are not there yet, the pathogen can re-penetrate and harm the fetus.
There are also cases of chronic toxoplasmosis - when the infection proceeds in a latent form and is activated when immunity is reduced in pregnant women.
During pregnancy, experts recommend avoiding contact with animals, and, if possible, avoid visiting regions with a high prevalence of toxoplasma: Africa, the Middle East, and Latin America.
Symptoms of toxoplasmosis in pregnant women
The infection has no pronounced manifestations. The most severe signs of toxoplasmosis in pregnant women appear in case of reduced immunity. In the acute course of the disease, the symptoms are similar to a viral disease (flu, SARS): the temperature rises to 38‒39degrees, the lymph nodes are enlarged, the woman feels weak and weak. Headaches and muscle pain may also join.
In most cases, the entry of the pathogen into the body does not cause the development of the disease. Toxoplasmosis manifests itself in a mild form, sometimes goes unnoticed, and a person learns about the disease from tests.
The likelihood of a more severe course increases if the body is weakened. Therefore, with toxoplasmosis in pregnant women, the likelihood of clinical complications is higher.
Fetal effects
In the first trimester, the greatest risk of severe consequences is when the fetus is infected, since the laying of organs and systems in the baby occurs. However, the risk of infection is lower. And at a later date, toxoplasmosis is less dangerous for the fetus, but it is easier for a woman to get infected with it.
However, the risk of infection is lower. And at a later date, toxoplasmosis is less dangerous for the fetus, but it is easier for a woman to get infected with it.
The severity of the consequences depends on the gestational age:
- Up to 8-9 weeks, the risk is no more than 20%, but leads to severe malformations and even intrauterine death. Among the frequent consequences: stillbirth, absence of a brain in a child, hydrocephalus, liver enlargement, severe organic pathologies.
- At 9-18 weeks, the risk of infection is approximately 25%. The danger is in severe damage to the brain, liver, eyes, as well as the appearance of convulsive syndrome and fever in an infant.
- At 18–25 weeks, the risk is approximately 65%. Infection leads to dysfunction of organs in a child. Jaundice, anemia, enlargement of the liver, spleen are possible.
- At 26-40 weeks, the risk of infection of the fetus from the mother is high - up to 80%. Subsequently, the child may develop deafness, epileptic seizures, mental retardation.
If a child had an acute infection in the 2nd trimester, then more often at birth, chronic or overt (with severe clinical symptoms) toxoplasmosis is diagnosed. In the first case, complications may appear a few months after birth or already in adolescence.
If infected in the last weeks of pregnancy, a child is likely to be born with signs of acute congenital toxoplasmosis, accompanied by fever, rash, jaundice, pneumonia, and gastrointestinal upset.
Diagnosis of toxoplasmosis during pregnancy
To reliably determine the infection, it is necessary to take tests. Laboratory diagnosis of toxoplasmosis is carried out by the methods of RNIF and ELISA. In the blood of a pregnant woman, the presence or absence of antibodies of class M and G is determined:
- If no antibodies are found, then the woman was not infected at all. This means that there is a risk of infection entering the body during pregnancy.
- If class G antibodies less than 40 U / ml are detected, it is possible to speak about the carriage of Toxoplasma without the risk of infection of the fetus.

- With G values over 200 U/ml and absence of M antibodies, the diagnosis is chronic acquired toxoplasmosis. In this case, specific treatment is not required.
- If both types of antibodies increase, the situation indicates an acute infection.
If there is no suspicion of pathology, the examination is carried out 1-2 times during pregnancy. If there are warning signs, the doctor may prescribe to donate blood regularly. To detect intrauterine toxoplasmosis in children, amniocentesis (analysis of amniotic fluid), as well as cordocentesis (examination of umbilical cord blood), assess the likely signs of pathology on ultrasound. If an infection is detected in the fetus in combination with signs of damage on ultrasound, it is recommended to terminate the pregnancy.
Treatment of toxoplasmosis in pregnant women
Treatment of pregnant women for the prevention of congenital toxoplasmosis in the fetus is not carried out. With proven infection of the expectant mother in the first trimester, it is recommended to terminate the pregnancy, and if there is a threat of miscarriage, preservation therapy is not carried out.
Starting from the second trimester, the question is whether to treat the pregnant woman:
- After 12 weeks, with a reliably accurate test result, an additional examination is carried out. In this case, interruption according to indications is also possible. But at such times, if a woman refuses to interrupt, the disease can be treated with specific drugs against Toxoplasma.
- Treatment is provided by a gynecologist and an infectious disease specialist. Therapy involves taking strong antibacterial drugs, in some cases, antimalarial and antiparasitic drugs are used. You can start drinking such medicines no earlier than 12-16 weeks.
- The treatment has side effects, so the doctor individually determines the dosage, correlates the risk and benefit, and makes important recommendations. Therapy has been shown to reduce the risk of infant mortality and neurological damage from congenital toxoplasmosis.
- Chronic toxoplasmosis is treated before or after pregnancy.
 In the absence of complaints and clinical manifestations in the mother and fetus, the woman is observed, but specific therapy is not prescribed.
In the absence of complaints and clinical manifestations in the mother and fetus, the woman is observed, but specific therapy is not prescribed.
Toxoplasmosis in pregnant women is not an indication for caesarean section. A woman can give birth naturally.
Prophylaxis
Tips to help reduce the chance of infection during pregnancy:
- Maintain personal hygiene. Wash your hands before and after eating, and especially after interacting with any pets and visiting public places.
- Eat only well-done or long-cooked meat, wash vegetables and fruits thoroughly with boiled water.
- Avoid close contact with cats, especially outdoor cats, and do not clean the litter box.
- Regularly undergo examinations: screenings, tests, ultrasound.
- Wear gloves when working on the ground or in sand.
The danger of infection is not so great, but if you are planning a pregnancy or are already in happy expectation, keep your finger on the pulse.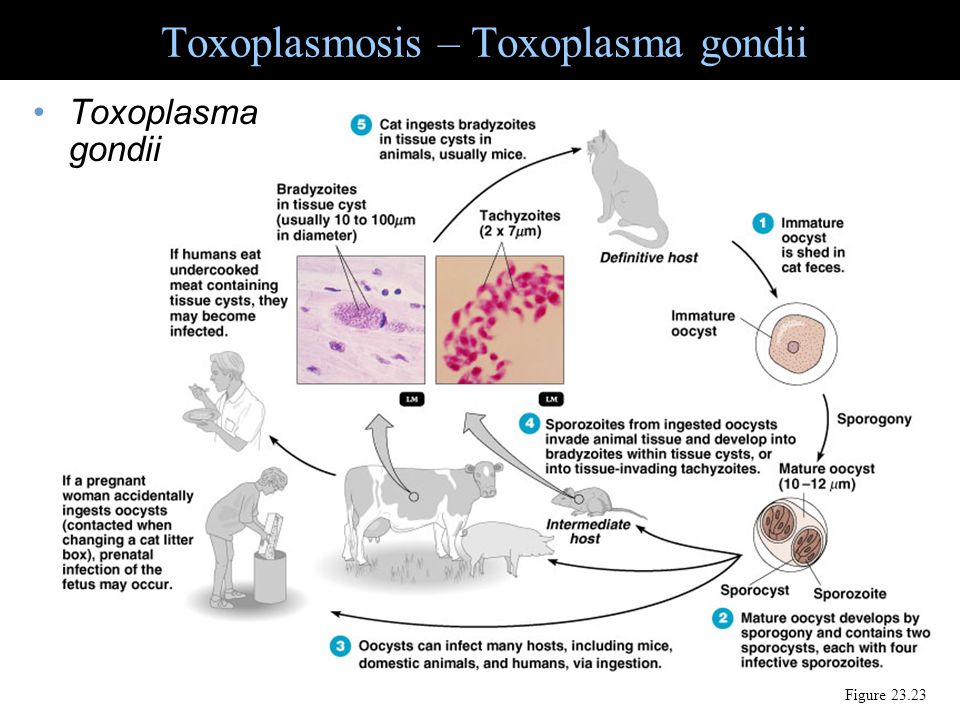 It is much easier to take the proper steps to avoid contracting a dangerous infection than to try to treat it during pregnancy. Take care of yourself and your future baby!
It is much easier to take the proper steps to avoid contracting a dangerous infection than to try to treat it during pregnancy. Take care of yourself and your future baby!
Obstetrician-gynecologist of the first qualification category -
Panasenko Irina Gennadievna
Toxoplasmosis during pregnancy. What is toxoplasmosis during pregnancy?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Toxoplasmosis during pregnancy is a parasitic disease caused by the penetration of T. gondii into the body of a pregnant woman. In most cases, this pathology is asymptomatic, rarely accompanied by a flu-like symptom complex. Diagnosis of toxoplasmosis during pregnancy includes a serological study with the determination of IgM and IgG, ultrasound examination of the fetus and amniocentesis, followed by PCR of amniotic fluid. The medical treatment option depends on the infection of the fetus and may consist of macrolide antibiotics or a combination of a sulfanilamide and a folic acid antagonist.
The medical treatment option depends on the infection of the fetus and may consist of macrolide antibiotics or a combination of a sulfanilamide and a folic acid antagonist.
- Causes of toxoplasmosis during pregnancy
- Symptoms of toxoplasmosis during pregnancy
- Diagnosis of toxoplasmosis during pregnancy
- Treatment of toxoplasmosis during pregnancy
- Prognosis and prevention of toxoplasmosis during pregnancy
- Prices for treatment
General
Toxoplasmosis during pregnancy is an infectious disease caused by toxoplasma, which is of great importance in obstetrics and gynecology due to the transplacental transmission route. According to statistics, about 15-25% of women aged 15 to 45 are infected with T. gondii. The general frequency of congenital toxoplasmosis is from 1 to 10 cases per 10,000 newborns, of which 3-10% have severe developmental anomalies. At the same time, about 55% of women who gave birth to infected children did not notice any signs of the disease.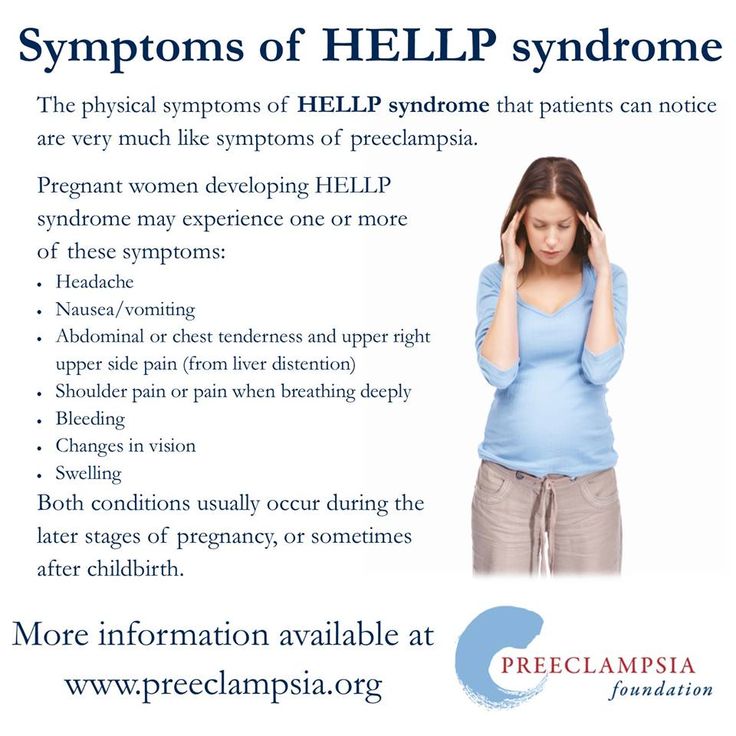 As a rule, women with immunodeficiency and living or traveling in endemic areas: France, Latin America and southern Africa are at a higher risk of developing toxoplasmosis during pregnancy.
As a rule, women with immunodeficiency and living or traveling in endemic areas: France, Latin America and southern Africa are at a higher risk of developing toxoplasmosis during pregnancy.
Toxoplasmosis during pregnancy
Causes of toxoplasmosis during pregnancy
The causative agent of toxoplasmosis during pregnancy is Toxoplasma gondii. It is an obligate intracellular parasite with a size of 4 to 8 microns. Depending on the environment, Toxoplasma can be found in three forms: oocyst, tissue cyst and tachyzoite. The first two are invasive to humans. Infection with cysts occurs when using contaminated meat products, oocytes - when in contact with the ground during gardening or eating unwashed vegetables and fruits. Toxoplasma in the form of oocysts is able to remain viable for a long time, especially being in warm and humid conditions, which significantly increases the risk of their transmission. When entering the body, parasites from invasive forms are transformed into tachyzoites, which cause the clinic of the disease and infection of the fetus against the background of toxoplasmosis during pregnancy.
There are several options for the way of human infection with T. gondii - eating raw minced meat or poorly thermally processed meat, contact with cat feces or earth containing oocysts, transplacental transmission from mother to child, and transfusion of infected blood. A significant part of cases (up to 65%) of toxoplasmosis during pregnancy occurs against the background of the use of infected food and water, passes in the form of primary infection. When in contact with cats, the main danger is pets that live on the street or eat raw meat.
An infected person can only be a source in the case of blood or organ donation. The risk of developing toxoplasmosis during pregnancy increases significantly when visiting regions with a high prevalence of toxoplasma: France, Latin America and southern Africa. It is generally accepted that even with a single ingestion of T. gondii, a person remains infected for life, and the disease itself proceeds in a subclinical form.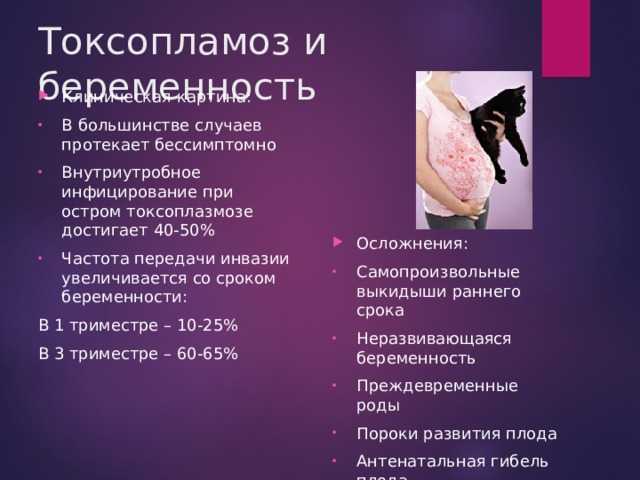 However, only in individual cases, toxoplasmosis during pregnancy is caused by the activation of a persistent infection.
However, only in individual cases, toxoplasmosis during pregnancy is caused by the activation of a persistent infection.
Symptoms of toxoplasmosis during pregnancy
More than 90% of cases of toxoplasmosis during pregnancy are asymptomatic, in the form of a healthy carriage. The development of a pronounced clinic is more likely in immunocompromised pregnant women - against the background of concomitant infectious or bacterial diseases, the use of corticosteroids, the early stages of AIDS, etc. The incubation period in such cases can vary from 1 to 3 weeks after the parasite enters the body. For acute toxoplasmosis during pregnancy, a flu-like variant of the course is characteristic: a rise in body temperature to 37.5-38 ° C, general weakness and malaise, headache, swollen lymph nodes, less often - hepatosplenomegaly. Pregnant women rarely develop toxoplasmic chorioretinitis, and even more rarely, conjunctivitis, keratitis, or iridocyclitis. Only against the background of a pronounced deficiency of immunity, toxoplasmosis during pregnancy can cause severe complications in the form of encephalitis, hepatitis, myocarditis or pneumonia.
Toxoplasmosis belongs to the group of TORCH infections, which includes infectious diseases that can have a teratogenic effect. Basically, the danger to the fetus is the primary infection of the mother, chronic toxoplasmosis during pregnancy rarely causes intrauterine transmission. Infection occurs between 1 and 4 months after penetration of tachyzoites into the placenta, the risk of infection increases with gestational age. According to statistics, the frequency of transmission of parasites to the fetus in the absence of treatment for toxoplasmosis during pregnancy in the third trimester is 10-12 times higher than in the first. Despite this, the earlier the infection of the fetus, the worse the prognosis. With the penetration of toxoplasma into the fetus in the first trimester, spontaneous abortions, severe developmental anomalies can be observed. Later congenital toxoplasmosis is manifested by Sabin's tetrad: chorioretinitis, dropsy of the brain, convulsive syndrome, intracranial calcification.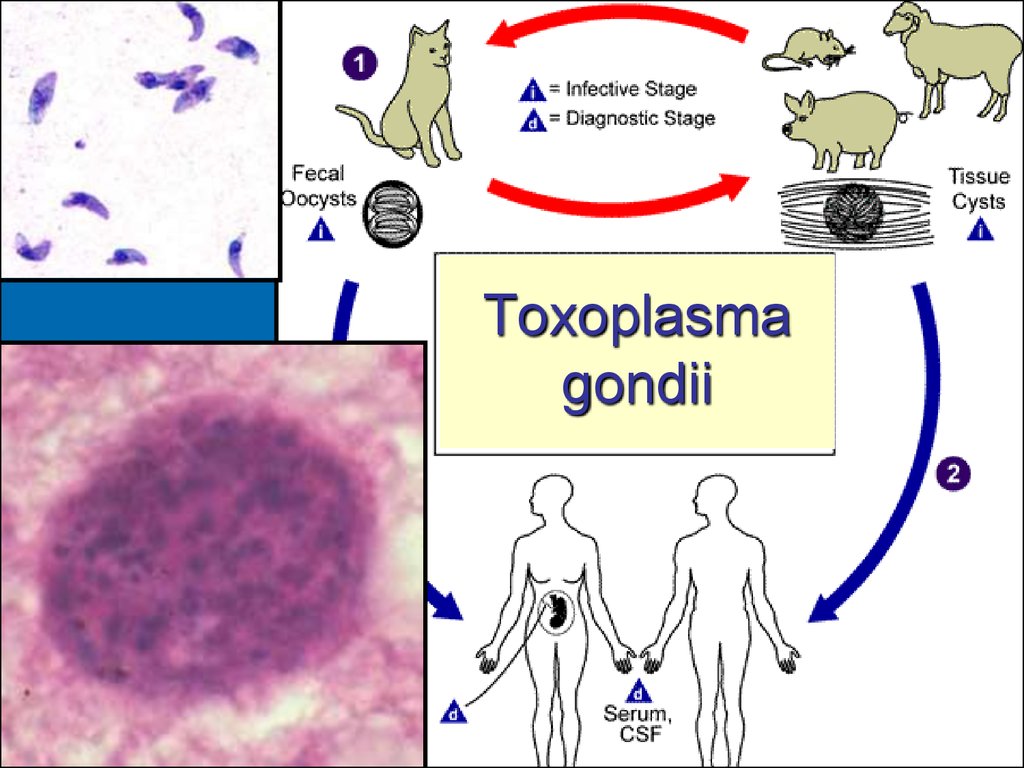 Severe intrauterine growth retardation and microcephaly may also be present. Their presence indicates the transferred acute toxoplasmosis during pregnancy.
Severe intrauterine growth retardation and microcephaly may also be present. Their presence indicates the transferred acute toxoplasmosis during pregnancy.
Diagnosis of toxoplasmosis during pregnancy
The diagnosis of toxoplasmosis during pregnancy is based on anamnestic data, identified symptoms, and the results of laboratory and instrumental studies. When collecting an anamnesis, an obstetrician-gynecologist or infectious disease specialist finds out all the circumstances under which toxoplasma infection could occur: eating raw meat, unwashed vegetables or fruits, contact with street cats, working with soil in the garden, staying in endemic areas. Physical examination in women with toxoplasmosis during pregnancy may reveal a flu-like symptom complex, but in the vast majority of cases it is of little information.
The leading place in the diagnosis of toxoplasmosis during pregnancy is played by serological tests, ultrasound scanning and puncture of the amniotic membrane of the fetus.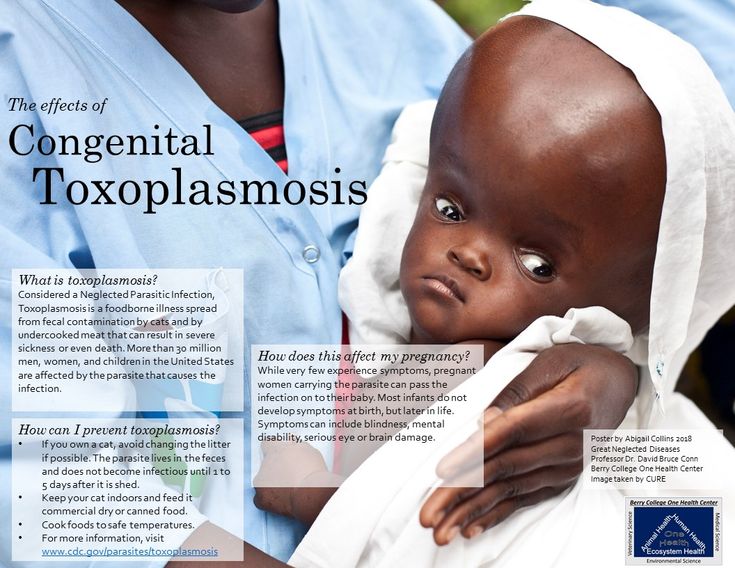 Laboratory diagnostics is often the first step and is carried out by enzyme immunoassay (ELISA) or special test systems. The essence of this study is to determine the immunoglobulins of class M (IgM) and G (IgG). Their complete absence refutes the diagnosis of toxoplasmosis during pregnancy. The presence of IgM and its increase by 4 times or more indicates a primary infection with T. gondii. Further, the titer gradually continues to increase and reaches a maximum 5-20 days after the invasion. The first manifestation of IgG in the mother's blood occurs after 7-14 days and reaches a maximum concentration in the interval from 3 to 6 months. In most cases, a high level of IgG indicates a latent course of toxoplasmosis during pregnancy. If positive results are obtained, the study should be repeated 3-4 times within 2-3 weeks.
Laboratory diagnostics is often the first step and is carried out by enzyme immunoassay (ELISA) or special test systems. The essence of this study is to determine the immunoglobulins of class M (IgM) and G (IgG). Their complete absence refutes the diagnosis of toxoplasmosis during pregnancy. The presence of IgM and its increase by 4 times or more indicates a primary infection with T. gondii. Further, the titer gradually continues to increase and reaches a maximum 5-20 days after the invasion. The first manifestation of IgG in the mother's blood occurs after 7-14 days and reaches a maximum concentration in the interval from 3 to 6 months. In most cases, a high level of IgG indicates a latent course of toxoplasmosis during pregnancy. If positive results are obtained, the study should be repeated 3-4 times within 2-3 weeks.
An ultrasound scan for women with suspected toxoplasmosis during pregnancy is necessary to assess the condition of the fetus. In most cases, it is not possible to identify any pronounced signs of congenital toxoplasmosis, or the changes present are not enough to confirm the diagnosis. The main manifestations of fetal infection against the background of toxoplasmosis during pregnancy include general intrauterine growth retardation and disorders of the central nervous system structure - hydro- or microcephaly, the formation of calcifications. Termination of pregnancy is recommended only if severe morphological abnormalities are detected.
The main manifestations of fetal infection against the background of toxoplasmosis during pregnancy include general intrauterine growth retardation and disorders of the central nervous system structure - hydro- or microcephaly, the formation of calcifications. Termination of pregnancy is recommended only if severe morphological abnormalities are detected.
A puncture of the amniotic membrane (amniocentesis) is required in cases of primary toxoplasmosis during pregnancy against the background of low information content of serological diagnostics and the presence of ultrasound signs of fetal damage. The decision on the advisability of puncturing the amniotic sac is made by the treating infectious disease specialist together with neonatologists and obstetrician-gynecologists. The bottom line is to take the amniotic fluid and determine the presence of T. gondii in it by polymerase chain reaction (PCR). The sensitivity and specificity of this procedure ranges from 90-95%. As a rule, amniocentesis in the presence of signs of toxoplasmosis during pregnancy is performed at a period not earlier than 18 obstetric weeks, which is associated with a high risk of obtaining false positive results. Also, this study is shown only 4 weeks after the alleged infection. Previously considered the “gold standard”, cordocentesis is now almost never used due to the risk to the fetus, the high information content of amniocentesis and PCR.
As a rule, amniocentesis in the presence of signs of toxoplasmosis during pregnancy is performed at a period not earlier than 18 obstetric weeks, which is associated with a high risk of obtaining false positive results. Also, this study is shown only 4 weeks after the alleged infection. Previously considered the “gold standard”, cordocentesis is now almost never used due to the risk to the fetus, the high information content of amniocentesis and PCR.
Treatment of toxoplasmosis during pregnancy
Treatment is necessary only in cases of acute toxoplasmosis during pregnancy, accompanied by clinical manifestations. In the absence of clinical symptoms of infection, recovery occurs on its own. Depending on the damage to the fetus, there are two directions of drug therapy for toxoplasmosis during pregnancy. In the absence of signs of infection of the fetus, according to the results of PCR of the amniotic fluid, macrolide antibiotics (spiramycin) are used. These funds are able to accumulate in the tissues of the placenta and prevent the vertical route of transmission.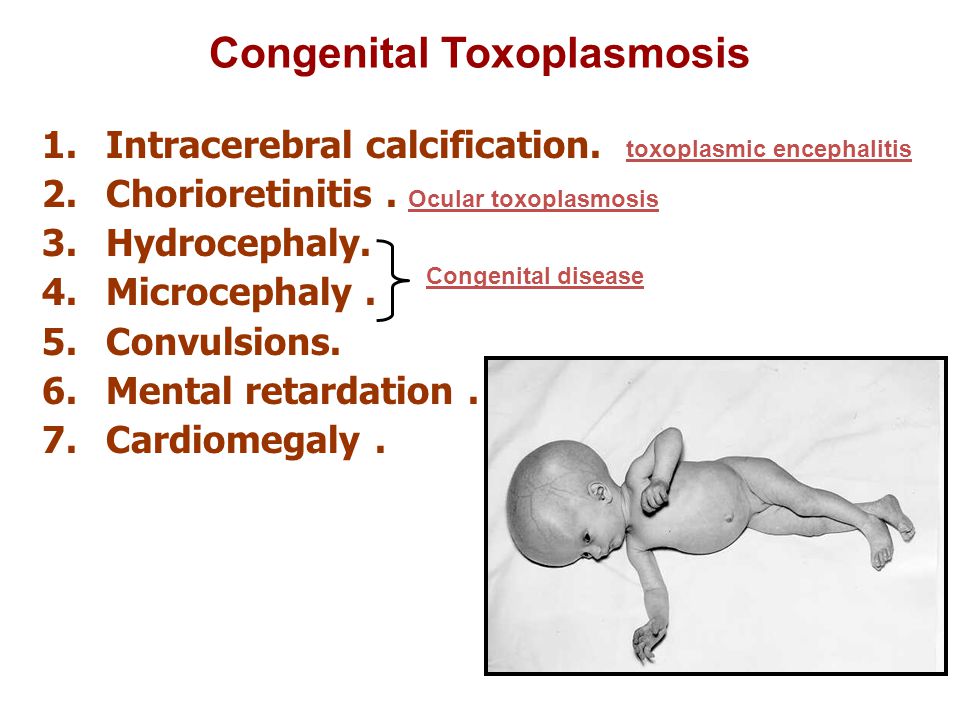
If infection of the fetus is confirmed or suspected against the background of toxoplasmosis during pregnancy, pharmacotherapy should consist of a folic acid antagonist (pyrimethamine) and a sulfanilamide (sulfadiazine). The first is able to suppress cell division in the bone marrow, so its purpose is always supplemented with folic acid preparations. Also, the use of the drug is contraindicated in the first trimester of pregnancy due to the potential teratogenic effect. This treatment option is aimed at reducing the severity of the disease in a child and improving the overall prognosis.
Prognosis and prevention of toxoplasmosis during pregnancy
The prognosis for a woman against the background of toxoplasmosis during pregnancy is favorable. Almost all cases end in clinical recovery. The prognosis for the unborn child directly depends on the trimester in which the infection occurred - the penetration of parasites into the fetus in the first trimester is associated with a high risk of spontaneous abortion or severe developmental anomalies.