Stillbirth and miscarriage
What is Stillbirth? | CDC
The loss of a baby due to stillbirth remains a sad reality for many families and takes a serious toll on families’ health and well-being. Learn more about stillbirth below.
A stillbirth is the death or loss of a baby before or during delivery. Both miscarriage and stillbirth describe pregnancy loss, but they differ according to when the loss occurs. In the United States, a miscarriage is usually defined as loss of a baby before the 20th week of pregnancy, and a stillbirth is loss of a baby at or after 20 weeks of pregnancy.
Stillbirth is further classified as either early, late, or term.
- An early stillbirth is a fetal death occurring between 20 and 27 completed weeks of pregnancy.
- A late stillbirth occurs between 28 and 36 completed pregnancy weeks.
- A term stillbirth occurs between 37 or more completed pregnancy weeks.
View and print fact sheet » [482 KB / 2 pages]
How Many Babies Are Stillborn?
Stillbirth affects about 1 in 175 births, and each year about 21,000 babies are stillborn in the United States. 1 That is about the same as the number of babies that die during the first year of life. Because of advances in medical technology over the last 30 years, prenatal care (medical care during pregnancy) has improved, which has dramatically reduced the number of late and term stillbirths. However, the rate of early stillbirth has remained about the same over time.
What Increases the Risk of Stillbirth?
Stillbirth with an unknown cause is called “unexplained stillbirth.” The further along a woman is in her pregnancy the more likely it is that the stillbirth will be unexplained. Having an autopsy on the baby and other laboratory tests is important in trying to understand why the baby died before birth. Your health care provider can share more information about this.
Stillbirth occurs in families of all races, ethnicities, and income levels, and to women of all ages. However, stillbirth occurs more commonly among certain groups of people including women who:
- are of black race
- are 35 years of age or older
- are of low socioeconomic status
- smoke cigarettes during pregnancy
- have certain medical conditions, such as high blood pressure, diabetes and obesity
- have multiple pregnancies such as triplets or quadruplets
- have had a previous pregnancy loss
This does not mean that every individual of black race or older age is at higher risk for having a stillbirth. It simply means that overall as a group, more stillbirths occur among all mothers of black race or older age when compared to white mothers and mothers under 35 years of age. Some factors that might contribute to these stillbirth disparities include differences in maternal preconception health, socioeconomic status, access to quality health care, and stress.2 More research is needed to determine what is underlying reason why some of these factors are associated with stillbirths.
It simply means that overall as a group, more stillbirths occur among all mothers of black race or older age when compared to white mothers and mothers under 35 years of age. Some factors that might contribute to these stillbirth disparities include differences in maternal preconception health, socioeconomic status, access to quality health care, and stress.2 More research is needed to determine what is underlying reason why some of these factors are associated with stillbirths.
Many of these factors are also associated with other poor pregnancy outcomes, such as preterm birth.
What Can Be Done?
CDC works to learn more about who might have a stillbirth and why. CDC does this by tracking how often stillbirth occurs and researching what causes stillbirth and how to prevent it. Knowledge about the potential causes of stillbirth can be used to develop recommendations, policies, and services to help prevent stillbirth. While we continue to learn more about stillbirth, much work remains. To learn more about CDC’s activities, visit the Stillbirth CDC Activities page.
To learn more about CDC’s activities, visit the Stillbirth CDC Activities page.
References
- Gregory ECW, Valenzuela CP, Hoyert DL. Fetal mortality: United States, 2020. National Vital Statistics Reports; vol 71 no 4. Hyattsville, MD: National Center for Health Statistics. 2022. [Read report]
- Pruitt SM, Hoyert DL, Anderson KN, et al. Racial and Ethnic Disparities in Fetal Deaths — United States, 2015–2017. MMWR Morb Mortal Wkly Rep 2020;69:1277–1282.
- MacDorman MF, Kirmeyer SE, Wilson EC. Fetal and perinatal mortality, United States, 2006. National vital statistics reports; vol 60 no 8. Hyattsville, MD: National Center for Health Statistics. 2012. [Read data brief pdf icon[432 KB / 23 pages]
Pregnancy and Infant Loss | CDC
The loss of a baby during pregnancy remains a sad reality for many families. Learn what the Centers for Disease Control and Prevention (CDC) is doing to understand the preventable causes of stillbirth. Read Milan’s story, as told by his mother Karina, about their family’s experience with the loss of a child through stillbirth.
Read Milan’s story, as told by his mother Karina, about their family’s experience with the loss of a child through stillbirth.
What is Stillbirth?
A stillbirth is the death of a baby before or during delivery. Both miscarriage and stillbirth describe pregnancy loss, but they differ according to when the loss occurs. In the United States, a miscarriage is usually defined as loss of a baby before the 20th week of pregnancy, and a stillbirth is loss of a baby at 20 weeks of pregnancy and later.
How Many Babies Are Stillborn?
About 1 pregnancy in 100 at 20 weeks of pregnancy and later is affected by stillbirth, and each year about 24,000 babies are stillborn in the United States.1
Each year about 24,000 babies are stillborn in the United States.
Milan’s Story
Karina was 39 weeks pregnant, expecting to give birth to her baby Milan.
Karina was healthy throughout her pregnancy. She saw a doctor regularly and did all of the normal testing and ultrasounds. Both the doctor and head midwife thought everything was fine.
Both the doctor and head midwife thought everything was fine.
During a check-up, one of Karina’s midwives listened for Milan’s heartbeat. Karina was in a room with her two midwives, her husband, a nurse, and an ultrasound technician. It was quiet as they listened for a heartbeat. They could not hear anything. Her husband and healthcare providers sat with Karina as she cried. Karina was 39 weeks pregnant when she learned that her baby had died. Karina was scared, but she knew that she had to deliver the baby or she risked her own life as well.
Karina was induced and she gave birth at home. She was grateful to give birth at home with people who loved her and treated her with great kindness.
Karina and her husband went on to have another child, named Phoenix, who gives their family great joy.
CDC thanks Karina and her family for sharing this personal story.
What Can Be Done?
The causes of many stillbirths are unknown. Stillbirth occurs in families of all races, ethnicities, and income levels, and to women of all ages. But there are things that a woman can do before and during pregnancy to increase her chance of having a healthy baby:
But there are things that a woman can do before and during pregnancy to increase her chance of having a healthy baby:
- Be sure that medical conditions, such as high blood pressure and diabetes, are under control before and during pregnancy.
- Avoid smoking cigarettes during pregnancy.
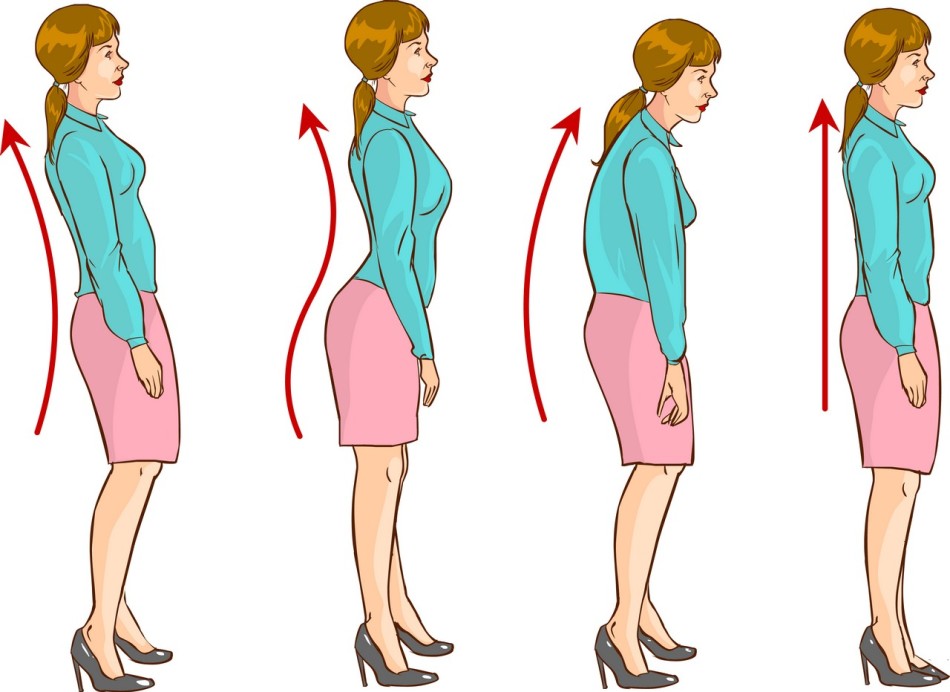
- Strive to reach and maintain a healthy weight before pregnancy.
CDC works to learn more about who might have a stillbirth and why. CDC tracks how often stillbirth occurs and looks at the causes of stillbirth. Knowledge about the potential causes of stillbirth can be used to create recommendations, policies, and services to help prevent stillbirth.
To learn more about CDC’s activities, visit the Stillbirth CDC Activities page.
- MacDorman MF, Gregory EC. Fetal and perinatal mortality: United States, 2013. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System.
 2015; 64(8):1-24.
2015; 64(8):1-24.
Miscarriages and stillbirths: why paracetamol is dangerous during pregnancy
Taking ibuprofen and paracetamol during pregnancy increases the risk of miscarriage and death in the first month of life by 50%, British experts have found. What else can be dangerous to take painkillers during pregnancy, under what conditions they are relatively harmless and how to reduce the likelihood of a situation where such medications may be needed, Gazeta.Ru was told by an obstetrician-gynecologist at the SM-Clinic Reproductive Health Center Victoria Fisyuk .
Taking painkillers and antipyretics during pregnancy, in particular ibuprofen and paracetamol, can cause miscarriages and stillbirths, British doctors from the University of Aberdeen reported in an article for the medical journal BMJ Open.
Researchers collected data from more than 151,000 pregnancies between 1985 and 2015. Some of the women took painkillers and antipyretic drugs - paracetamol, aspirin, ibuprofen, diclofenac and naproxen.
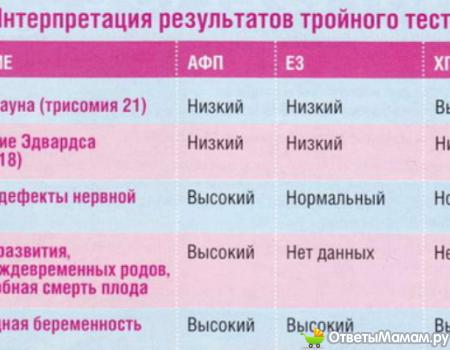
Women who took painkillers were more likely to suffer from pregnancy complications. Thus, the risk of having a child with low body weight was 28% higher, 64% more common were defects in the development of the neural tube, which is necessary for the formation of the brain and spine, congenital defects of the penis in boys were observed 27% more often.
33% higher risk of stillbirth, 50% higher risk of miscarriage or preterm birth. Also, the risk of infant death in the first month of life was 50% higher.
Paracetamol is considered safe during pregnancy. Other non-steroidal anti-inflammatory drugs can affect the circulation and kidney function of a child, especially if used frequently, so their use is considered undesirable.
An average of 3 out of 10 women took over-the-counter pain medication during pregnancy. At the same time, in 2008-2015, this happened twice as often as before, which indicates a rapid increase in the frequency of painkiller use.
However, it is not known how often and in what dosage women took painkillers, the authors of the work admit.
“Detailed information on the exact dose and timing of administration during pregnancy was not available in our dataset,” they write.
“According to WHO recommendations, taking paracetamol and ibuprofen during pregnancy is permissible once, without systemic use,” Victoria Fisyuk, an obstetrician-gynecologist at the SM-Clinic Reproductive Health Center, told Gazeta.Ru. - At the same time, it is highly recommended not to take them in the first and third trimester. But significant contraindications for the use of these drugs by pregnant women in the second trimester have not been identified. They can also be taken during lactation. There is no convincing evidence that non-systematic use of these drugs increases the risk of miscarriage or preterm birth, as well as evidence that it leads to autism or hyperactivity. Probably, this can be observed when they are taken systemically.
But it is important to take into account that the prescription of any drugs is resorted to only if it is really necessary, and only as directed by a doctor.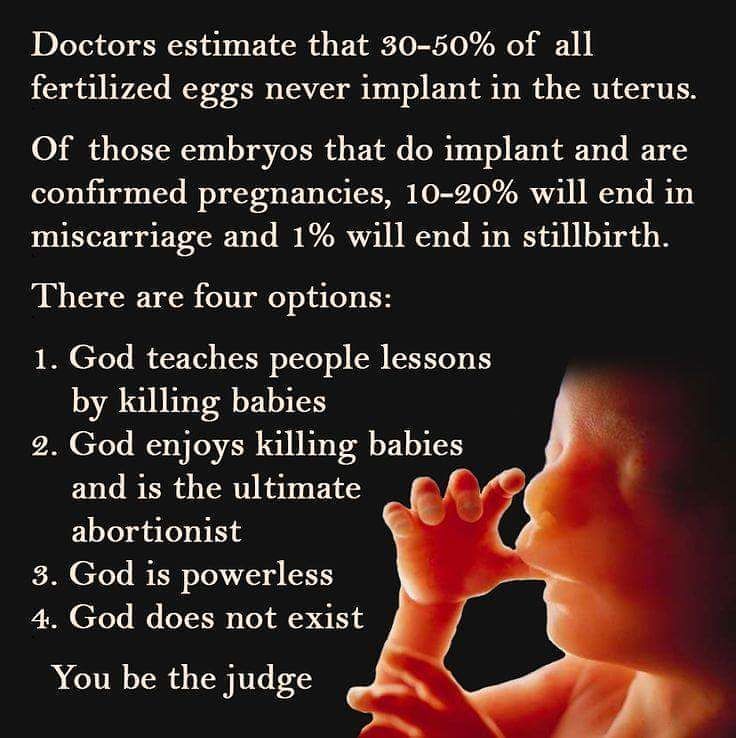 ”
”
Paracetamol is one of two antipyretic and analgesic drugs approved for use by pregnant and lactating women. The mechanism of action and safety of paracetamol has been clinically confirmed, and therefore paracetamol is on the WHO list of essential medicines, the doctor noted. Another drug that is allowed during pregnancy is ibuprofen.
“However, a number of articles have recently been published discussing the possibility of harm to the fetus when taking ibuprofen. We are talking about a negative impact on the egg reserve in girls in the future, the formation of a factor in reducing the ovarian reserve and possible infertility. In relation to boys, we are talking about a negative effect on the testicles in the fetus due to the possible development of cryptorchidism - undescended testicles into the scrotum. However, these experiments were carried out in laboratories where a direct effect on cells was considered and the factor that the human body has a so-called “utilizing” function that can neutralize many negative effects of one nature or another was not taken into account. Nevertheless, it has been proven that the use of ibuprofen after 22–24 weeks can lead to the development of cardiovascular diseases in the fetus,” Fisyuk added.
Nevertheless, it has been proven that the use of ibuprofen after 22–24 weeks can lead to the development of cardiovascular diseases in the fetus,” Fisyuk added.
During pregnancy, the responsibility for gestation lies not only with the expectant mother, but also with doctors, Fisyuk pointed out. Ideally, pregnancy should proceed without taking any medications - only vitamin and mineral complexes are acceptable at the planning stage.
Before planning, it is necessary to visit an obstetrician-gynecologist. If necessary, he will prescribe folic acid and iodine preparations. It is also recommended to visit a dentist, ophthalmologist, neurologist and orthopedist.
“Such preventive measures before pregnancy will help to avoid many negative manifestations, including headache, back pain and toothache,” said Fisyuk. —
So, when a pregnant woman complains of a headache, one often has to resort to prescribing drugs such as paracetamol and ibuprofen. In case of untreated caries, these drugs may also be required. This also includes various viral infections, which are accompanied by an increase in body temperature.
This also includes various viral infections, which are accompanied by an increase in body temperature.
The greatest number of side effects in the study was observed with the simultaneous use of paracetamol and other drugs, but the mechanism of this is not yet fully clear. The researchers insist that more attention should be paid to studying the possible side effects of painkillers on the fetus during pregnancy, as well as to inform women more about the possible harm: pregnant women often take medications without doctor's recommendations, focusing, for example, on advice on the Internet.
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find the country »
- A
- B
- B
- g
- D
- E
- z 9002 L 9002 L 9002 L 9002 l
- K 9002 l 9002 l 9002 l 9002 l
- to 9002 l 9002 l
- to 9002 l
- to 9002 l
- to
- О
- П
- Р
- С
- Т
- У
- Ф
- Х
- Ц
- Ч
- Ш
- Щ
- Ъ
- Ы
- Ь
- Э
- Yu
- I
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Spotlight /
- Why is it so important for us to talk about the loss of a child
Why is it important for us to talk about the loss of a child
WHO/M. Purdie
Purdie
© A photo
The loss of a child during pregnancy due to miscarriage or stillbirth is still a taboo topic around the world, which is associated with condemnation or a sense of shame. Many women who lose a child during pregnancy or childbirth continue to receive neither the proper care nor the respect they deserve. In this material we want to share stories told by women from different countries.
Miscarriage is the most common cause of pregnancy loss. Estimates of the prevalence of this phenomenon vary somewhat, although according to the March of Dimes Foundation, an organization dedicated to maternal and child health, the prevalence of miscarriage in women who knew they were pregnant is 10-15%. Different countries around the world use different definitions of pregnancy loss, but as a rule, the death of a child before 28 weeks of gestation is considered a miscarriage, and death at or after 28 completed gestational weeks is considered a stillbirth. There are 2.6 million stillborn babies born each year, and many of these deaths could have been prevented. However, even in developed countries, miscarriages and stillbirths are not systematically recorded, so the actual figures may be even higher.
There are 2.6 million stillborn babies born each year, and many of these deaths could have been prevented. However, even in developed countries, miscarriages and stillbirths are not systematically recorded, so the actual figures may be even higher.
Worldwide, women's access to health services varies by country of residence, with hospitals and outpatient facilities very often under-resourced and understaffed in many countries. As varied as the experience of bereaved women, stigma, guilt and shame are common themes around the world. Women who have lost their children have shared personal experiences that they felt they had to keep their grief quiet, either because miscarriages or stillbirths remain common or because people perceive them as inevitable.
Jessica Zucker, Clinical Psychologist and Writer, USA
“I am a clinical psychologist specializing in mental health issues related to reproduction and motherhood. I have been doing this for over ten years. But when I myself had a miscarriage at 16 weeks, only then could I truly feel that heartache, that re-experienced feeling of grief and loss that my patients have been telling me about for so many years.
Jessica's story
All this has an extremely hard effect on women. Many women who lose a child during pregnancy may develop mental health problems that last for months or years, even if they later have healthy children.
Cultural and social views on the loss of a child in different parts of the world can be very different from each other. Thus, in sub-Saharan Africa, the prevailing opinion is that a baby can be born dead because of witchcraft or the machinations of evil spirits.
Larai, 44, pharmacist, Nigeria
“I took everything that happened after my miscarriage very hard. This was greatly facilitated by the medical workers themselves, despite the fact that I am also a doctor. Another issue is cultural representations. Here, the loss of a child brings shame to the woman, because there is a perception that if a woman has lost a child several times, something is wrong with her, and that she may have had extramarital affairs, and the loss of a child in that case, God's punishment.
Larai's story
Miscarriages or stillbirths have many possible causes, from fetal abnormalities, maternal age, to infections, many of which (such as malaria and syphilis) are preventable, although identifying the exact cause is often difficult.
General recommendations for preventing miscarriage include a healthy diet, physical activity, avoiding smoking, drug and alcohol use, limiting caffeine intake, managing stress, and maintaining a normal body weight. This approach focuses on lifestyle factors, and in the absence of specific explanations for what happened, this can lead to women feeling guilty that it was their behavior that caused the miscarriage.
Lisa, 40, Marketing Manager, UK
“I've had four miscarriages. Every time this happens, a part of you dies. The first time was the hardest. It was my very first pregnancy. We were so happy that we will soon have a baby. But when we went to our local hospital in the southeast of England at week 12 for a routine ultrasound, I was told that I had a miscarriage, or miscarriage, which meant that my baby had died long ago, although I did not feel no signs. "
"
Lisa's story
As with some other medical topics, such as mental health, which remain a huge taboo, many women report that, regardless of their cultural background, education and upbringing, their friends and families don't want to talk about their loss. Apparently, this is due to the general tradition to surround any grief with a veil of silence.
Susan, 34, writer, USA
“I've been dealing with infertility for almost five years now. After I decided to try IVF, I actually managed to get pregnant, but after a few weeks the baby stopped growing. It took doctors two and a half weeks to confirm this. It took another two weeks before I had a miscarriage that lasted 19days. I could not imagine that it could be so painful, for so long and with such heavy bleeding.
Susan's story
Stillbirths occur later in pregnancy, namely after 28 gestational weeks, as defined by the WHO. About 98% of stillbirths occur in low- and middle-income countries. Lack of proper care and supervision during labor results in one in two stillbirths occurring during delivery, many of which could have been prevented with quality care and proper supervision of the woman in labour.
Lack of proper care and supervision during labor results in one in two stillbirths occurring during delivery, many of which could have been prevented with quality care and proper supervision of the woman in labour.
Better care during pregnancy and childbirth could prevent more than half a million stillbirths globally. Even in high-income countries, non-compliance with standards of care is an important cause of stillbirths.
There are clear ways to reduce the number of children who die during pregnancy, namely: improving access to antenatal care (in some parts of the world, women do not see a health worker until they are several months pregnant), introducing continuous care models, provided by midwives, as well as community care where possible. Integrating infection management during pregnancy, fetal heart rate monitoring and birth monitoring into a comprehensive care package could save 1.3 million lives of otherwise stillborn babies.
Emilia, 36, shopkeeper, Colombia
“When my baby was stillborn at 32 weeks, we already gave him a name. The doctor referred me for an ultrasound examination, during which he told me that the child was not showing signs of life. I knew right away that my baby was dead. I know this could have been avoided. If from the very beginning I had been told everything about my condition in more detail, if the doctors had treated me more attentively during the critical periods of my pregnancy, my child could have been saved.
The doctor referred me for an ultrasound examination, during which he told me that the child was not showing signs of life. I knew right away that my baby was dead. I know this could have been avoided. If from the very beginning I had been told everything about my condition in more detail, if the doctors had treated me more attentively during the critical periods of my pregnancy, my child could have been saved.
Emilia's story
The attitude towards women during pregnancy is related to the extent to which their sexual and reproductive rights are generally realized; many women around the world do not have the ability to make autonomous decisions in this area.
In many parts of the world, the pressure of public opinion is forcing women to become pregnant when they are not yet physically or psychologically ready for it. Even in 2019, 200 million women who want to avoid pregnancy do not have access to modern methods of contraception. And when pregnancy does occur, 30 million women are forced to give birth outside of health facilities, and 45 million women do not receive adequate antenatal care or no antenatal care at all, greatly increasing the risk of complications and death for both the mother and the mother. child.
child.
Cultural practices, such as ritual female genital mutilation and child marriage, cause great harm to girls' sexual and reproductive health and the health of their children. Having children at a young age can be dangerous for both mother and child. Adolescent girls (aged 10–19 years) are significantly more likely to have eclampsia or intrauterine infections than women aged 20–24 years, increasing the risk of stillbirth in this age group. In addition, babies born to women younger than 20 are more likely to have low birth weight, prematurity, or severe health problems in the first month of life, which also increases the risk of stillbirth.
Female genital mutilation increases a woman's risk of protracted or difficult labour, bleeding, severe tears and increases the frequency of instrumental use in childbirth. At the same time, children of such mothers are much more likely to need resuscitation during childbirth and increase the risk of death during childbirth or after birth.
Putting women at the center of care is critical to creating a positive pregnancy experience—the biomedical and physiological aspects of health services need to be complemented by social, cultural, emotional and psychological support.
However, many women, even in developed countries with access to the best health care systems, do not receive adequate care after the loss of a child. Even the language used by medical professionals in relation to miscarriage and stillbirth can be traumatic in itself: the use of terms such as "cervical failure" or "dead gestational sac" can be painful.
Andrea, 28, stylist and singer, Colombia
“When I was 12 weeks pregnant, I went to a scheduled appointment with the doctor, where they did an ultrasound. The doctor told me that I was not doing well, but did not specify what exactly was wrong. The next day, when I woke up, I noticed blood stains on the sheets. I didn't get any information about why I had a miscarriage.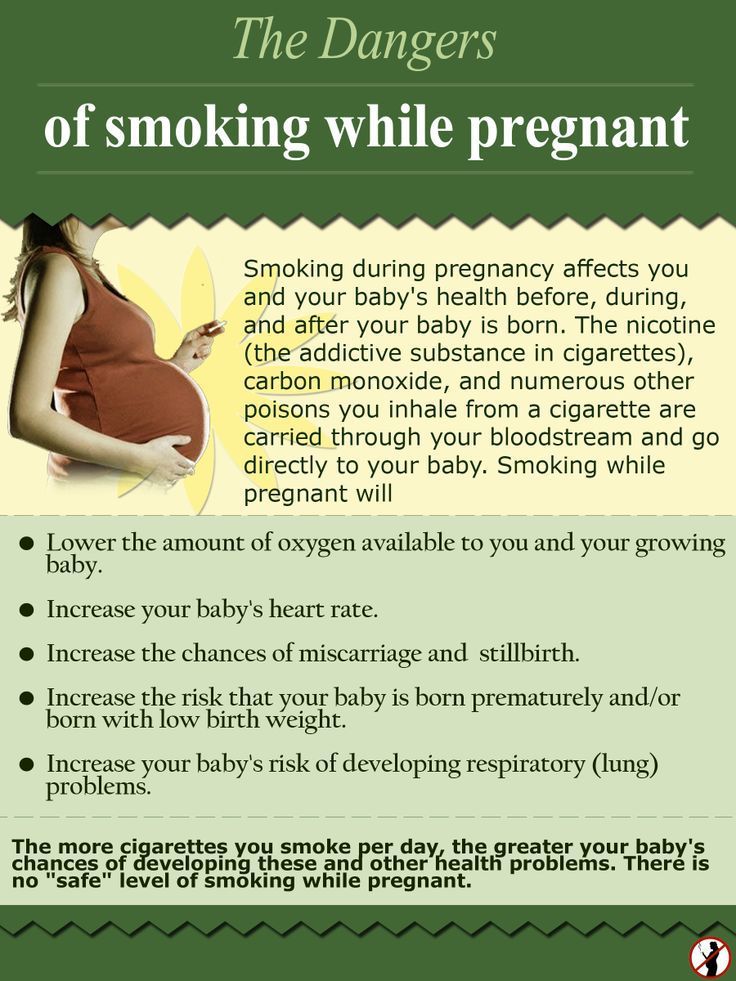 My doctor was very kind to me, but he didn't explain anything to me. But the nurses were completely indifferent and unfriendly and behaved as if I had undergone an ordinary medical procedure, and nothing more. No one gave me any support."
My doctor was very kind to me, but he didn't explain anything to me. But the nurses were completely indifferent and unfriendly and behaved as if I had undergone an ordinary medical procedure, and nothing more. No one gave me any support."
Depending on the rules of the particular medical facility, stillborn bodies may be treated as clinical waste and may be incinerated. It happens that when a woman learns that her child has died, she is forced to continue to carry the dead baby for several weeks before she can give birth. Even if this delay may be clinically justified, this situation is excruciating for both the woman and her partner. Even in developed countries, women may be forced to give birth to their dead babies in maternity wards, surrounded by women who have healthy children, which is very difficult from a psychological point of view and reminds the woman of her loss.
Not all inpatient or outpatient facilities can adopt a new care strategy or provide more services.