Trisomy test in pregnancy
First trimester screening - Mayo Clinic
Overview
Nuchal translucency measurement
Nuchal translucency measurement
First trimester screening includes an ultrasound exam to measure the size of the clear space in the tissue at the back of a baby's neck (nuchal translucency). In Down syndrome, the nuchal translucency measurement is abnormally large — as shown on the left in the ultrasound image of an 11-week fetus. For comparison, the ultrasound image on the right shows an 11-week fetus with a normal nuchal translucency measurement.
First trimester screening is a prenatal test that offers early information about a baby's risk of certain chromosomal conditions, specifically, Down syndrome (trisomy 21) and extra sequences of chromosome 18 (trisomy 18).
First trimester screening, also called the first trimester combined test, has two steps:
- A blood test to measure levels of two pregnancy-specific substances in the mother's blood — pregnancy-associated plasma protein-A (PAPP-A) and human chorionic gonadotropin (HCG)
- An ultrasound exam to measure the size of the clear space in the tissue at the back of the baby's neck (nuchal translucency)
Typically, first trimester screening is done between weeks 11 and 14 of pregnancy.
Using your age and the results of the blood test and the ultrasound, your health care provider can gauge your risk of carrying a baby with Down syndrome or trisomy 18.
If results show that your risk level is moderate or high, you might choose to follow first trimester screening with another test that's more definitive.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Obstetricks
Why it's done
First trimester screening is done to evaluate your risk of carrying a baby with Down syndrome. The test also provides information about the risk of trisomy 18.
Down syndrome causes lifelong impairments in mental and social development, as well as various physical concerns. Trisomy 18 causes more severe delays and is often fatal by age 1.
First trimester screening doesn't evaluate the risk of neural tube defects, such as spina bifida.
Because first trimester screening can be done earlier than most other prenatal screening tests, you'll have the results early in your pregnancy.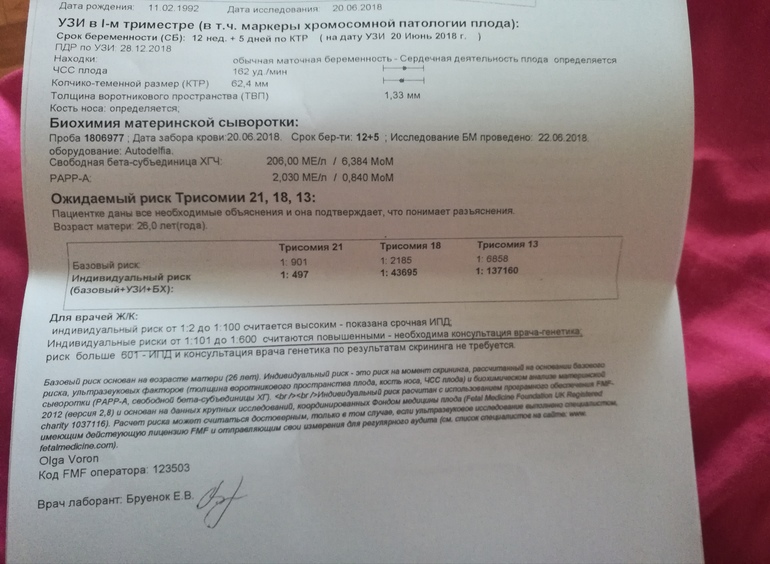 This will give you more time to make decisions about further diagnostic tests, the course of the pregnancy, medical treatment and management during and after delivery. If your baby has a higher risk of Down syndrome, you'll also have more time to prepare for the possibility of caring for a child who has special needs.
This will give you more time to make decisions about further diagnostic tests, the course of the pregnancy, medical treatment and management during and after delivery. If your baby has a higher risk of Down syndrome, you'll also have more time to prepare for the possibility of caring for a child who has special needs.
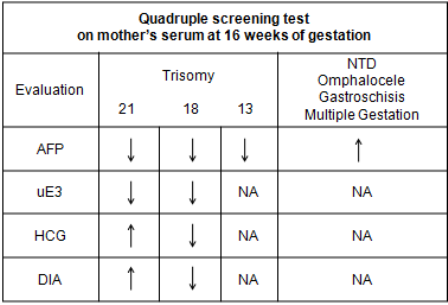
Other screening tests can be done later in pregnancy. An example is the quad screen, a blood test that's typically done between weeks 15 and 20 of pregnancy. The quad screen can evaluate your risk of carrying a baby with Down syndrome or trisomy 18, as well as neural tube defects, such as spina bifida. Some health care providers choose to combine the results of first trimester screening with the quad screen. This is called integrated screening. This can improve the detection rate of Down syndrome.
First trimester screening is optional. Test results indicate only whether you have an increased risk of carrying a baby with Down syndrome or trisomy 18, not whether your baby actually has one of these conditions.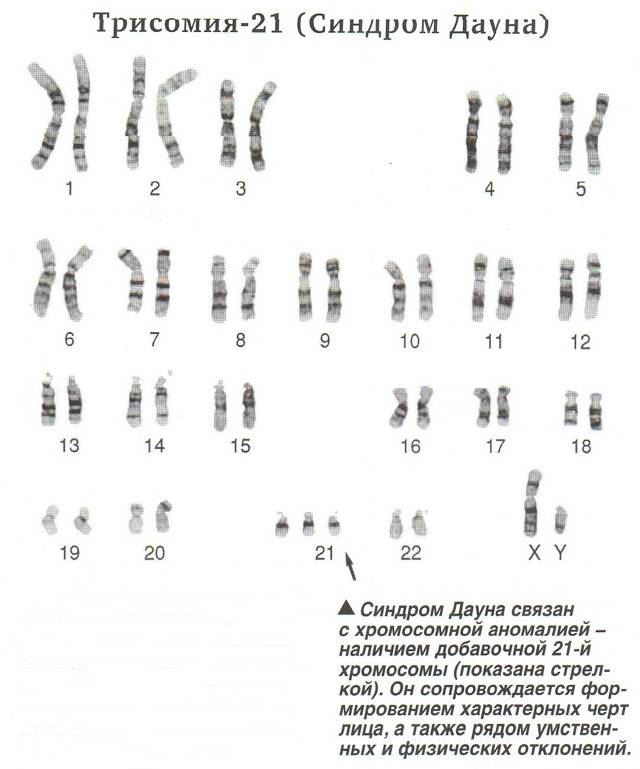
Before the screening, think about what the results will mean to you. Consider whether the screening will be worth any anxiety it might cause, or whether you'll manage your pregnancy differently depending on the results. You might also consider what level of risk would be enough for you to choose a more invasive follow-up test.
More Information
- Prenatal testing: Quick guide to common tests
Request an Appointment at Mayo Clinic
Risks
First trimester screening is a routine prenatal screening test. The screening poses no risk of miscarriage or other pregnancy complications.
How you prepare
You don't need to do anything special to prepare for first trimester screening. You can eat and drink normally before both the blood test and the ultrasound exam.
What you can expect
First trimester screening includes a blood draw and an ultrasound exam.
During the blood test, a member of your health care team takes a sample of blood by inserting a needle into a vein in your arm.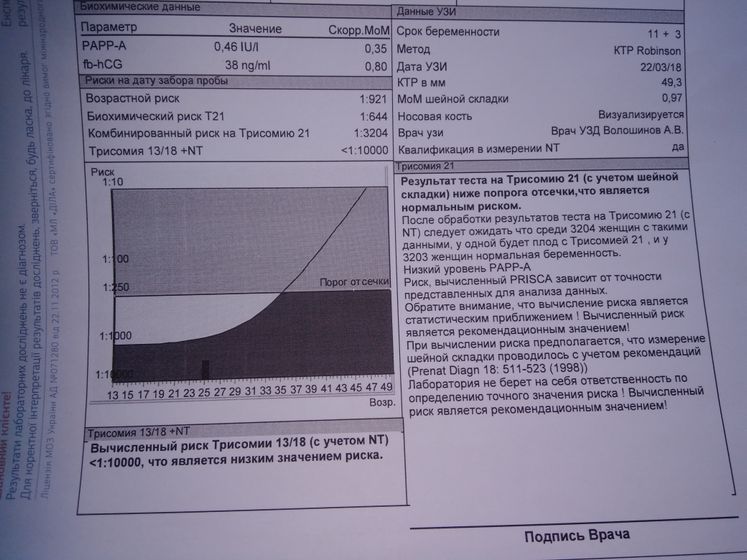 The blood sample is sent to a lab for analysis. You can return to your usual activities immediately.
The blood sample is sent to a lab for analysis. You can return to your usual activities immediately.
For the ultrasound exam, you'll lie on your back on an exam table. Your health care provider or an ultrasound technician will place a transducer — a small plastic device that sends and receives sound waves — over your abdomen. The reflected sound waves will be digitally converted into images on a monitor. Your health care provider or the technician will use these images to measure the size of the clear space in the tissue at the back of your baby's neck.
The ultrasound doesn't hurt, and you can return to your usual activities immediately.
Results
Your health care provider will use your age and the results of the blood test and ultrasound exam to gauge your risk of carrying a baby with Down syndrome or trisomy 18. Other factors — such as a prior Down syndrome pregnancy — also might affect your risk.
First trimester screening results are given as positive or negative and also as a probability, such as a 1 in 250 risk of carrying a baby with Down syndrome.
First trimester screening correctly identifies about 85 percent of women who are carrying a baby with Down syndrome. About 5 percent of women have a false-positive result, meaning that the test result is positive but the baby doesn't actually have Down syndrome.
When you consider your test results, remember that first trimester screening indicates only your overall risk of carrying a baby with Down syndrome or trisomy 18. A low-risk result doesn't guarantee that your baby won't have one of these conditions. Likewise, a high-risk result doesn't guarantee that your baby will be born with one of these conditions.
If you have a positive test result, your health care provider and a genetics professional will discuss your options, including additional testing. For example:
- Prenatal cell-free DNA (cfDNA) screening. This is a sophisticated blood test that examines fetal DNA in the maternal bloodstream to determine whether your baby is at risk of Down syndrome, extra sequences of chromosome 13 (trisomy 13) or extra sequences of chromosome 18 (trisomy 18).
 Some forms of cfDNA screening also screen for other chromosome problems and provide information about fetal sex. A normal result might eliminate the need for a more invasive prenatal diagnostic test.
Some forms of cfDNA screening also screen for other chromosome problems and provide information about fetal sex. A normal result might eliminate the need for a more invasive prenatal diagnostic test. - Chorionic villus sampling (CVS). CVS can be used to diagnose chromosomal conditions, such as Down syndrome. During CVS, which is usually done during the first trimester, a sample of tissue from the placenta is removed for testing. CVS poses a small risk of miscarriage.
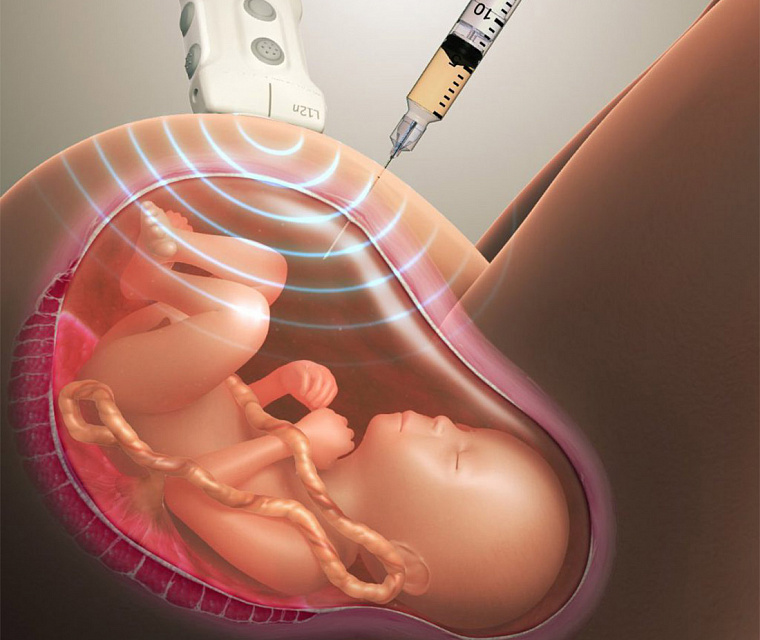
- Amniocentesis. Amniocentesis can be used to diagnose both chromosomal conditions, such as Down syndrome, and neural tube defects, such as spina bifida. During amniocentesis, which is usually done during the second trimester, a sample of amniotic fluid is removed from the uterus for testing. Like CVS, amniocentesis poses a small risk of miscarriage.

Your health care provider or a genetic counselor will help you understand your test results and what the results mean for your pregnancy.
By Mayo Clinic Staff
Related
Products & Services
Prenatal Testing for Down Syndrome | Patient Education
Down syndrome is a genetic condition caused by extra genes from the 21st chromosome. It results in certain characteristics, including some degree of cognitive disability and other developmental delays. Common physical traits include an upward slant of the eyes; flattened bridge of the nose; single, deep crease on the palm of the hand; and decreased muscle tone. A child with Down syndrome, however, may not have all these traits.
The incidence of Down syndrome in the United States is about 1 in 1,000 births. There is no association between Down syndrome and culture, ethnic group, socioeconomic status or geographic region.
Age-Related Risks
Generally, the chance of having a Down syndrome birth is related to the mother's age.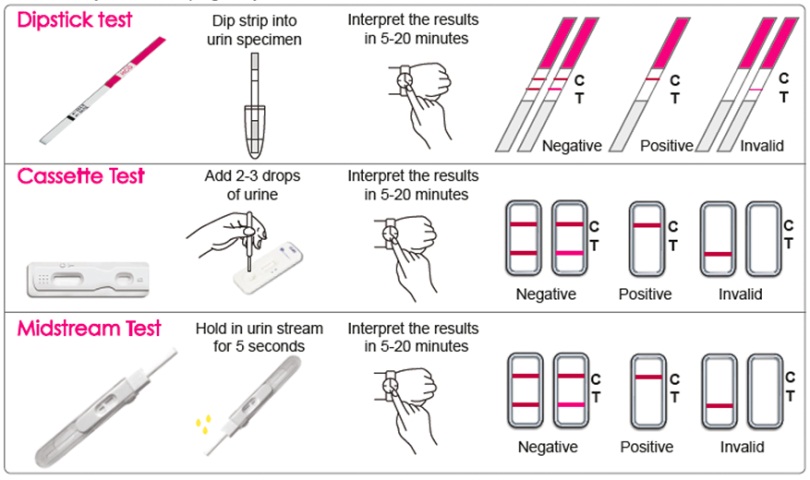 Under age 25, the odds of having a child with Down syndrome are about 1 in 1,400. At age 35, the odds are about 1 in 350. At age 40, the odds are about 1 in 100.
Under age 25, the odds of having a child with Down syndrome are about 1 in 1,400. At age 35, the odds are about 1 in 350. At age 40, the odds are about 1 in 100.
Causes of Down Syndrome
There are three causes of Down syndrome:
Trisomy 21
An estimated 95 percent of people with Down syndrome have trisomy 21, meaning they have three number 21 chromosomes instead of two. We normally have 23 pairs of chromosomes, each made up of genes. During the formation of the egg and the sperm, a woman's or a man's pair of chromosomes normally split so that only one chromosome is in each egg or sperm. In trisomy 21, the 21st chromosome pair does not split and a double dose goes to the egg or sperm. An estimated 95 to 97 percent of the extra chromosome is of maternal origin.
Translocation
Translocation occurs in about 3 to 4 percent of people with Down syndrome. In this type, an extra part of the 21st chromosome gets stuck onto another chromosome. In about half of these situations, one parent carries the extra 21st chromosome material in a "balanced" or hidden form.
Mosaicism
In mosaicism, the person with Down syndrome has an extra 21st chromosome in some of the cells but not all of them. The other cells have the usual pair of 21st chromosomes. About 1 to 2 percent of people with Down syndrome have this type.
Prenatal Testing
Screening tests can identify women at increased risk of having a baby with Down syndrome. These tests have no risks of miscarriage, but can't determine with certainty whether a fetus is affected. Diagnostic tests, on the other hand, are extremely accurate at identifying certain abnormalities in the fetus, but carry a small — generally less than 1 percent — risk of miscarriage. We offer options for both screening and diagnostic testing.
Continue reading
Screening Tests
Sequential Integrated Screening — Sequential integrated screening is offered to all pregnant women by the state of California. This non-invasive screening is performed in two steps.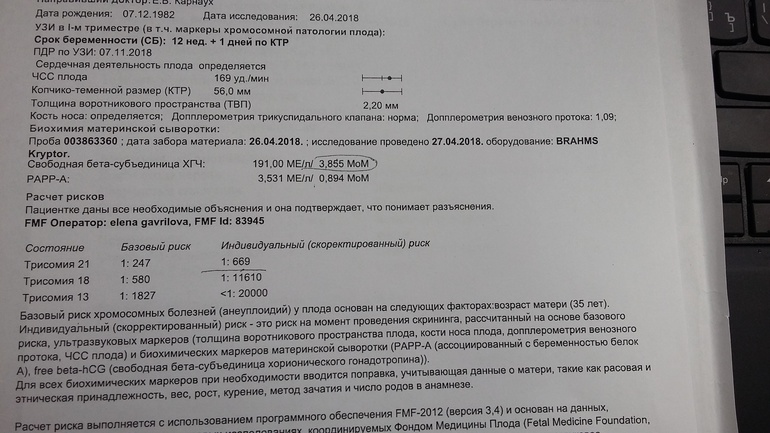
In the first step, which is performed between 10 and 14 weeks of pregnancy, a blood sample is taken from the mother and a nuchal translucency ultrasound is performed to measure the amount of fluid at the back of the baby's neck. If the blood test is scheduled prior to the ultrasound, we can provide the results at the end of the ultrasound appointment. The results of the blood test, the nuchal translucency measurement and the mother's age are used to estimate the risk for Down syndrome and trisomy 18.
The second step is a maternal blood test between 15 to 20 weeks of pregnancy. When the results of this blood test are combined with the results from the first trimester blood test and nuchal translucency ultrasound, the detection rate for Down syndrome increases. This test also provides a personal risk assessment for having a fetus with trisomy 18, Smith-Lemli-Opitz syndrome, an open neural tube defect or an abdominal wall defect.
Diagnostic Tests
Amniocentesis, chorionic villus sampling (CVS) and ultrasound are the three primary procedures for diagnostic testing.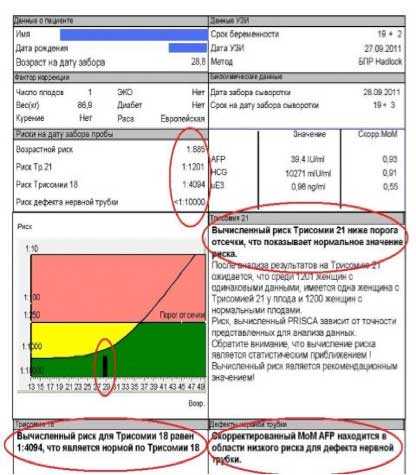
Amniocentesis — Amniocentesis is used most commonly to identify chromosomal problems such as Down syndrome. When the fetus is known to be at risk, it can detect other genetic diseases like cystic fibrosis, Tay-Sachs disease and sickle cell disease.
An amniocentesis procedure for genetic testing is typically performed between 15 and 20 weeks of pregnancy. Under ultrasound guidance, a needle is inserted through the abdomen to remove a small amount of amniotic fluid. The cells from the fluid are then cultured and a karyotype analysis — an analysis of the chromosomal make-up of the cells — is performed. It takes about two weeks to receive the results of the test.
Amniocentesis detects most chromosomal disorders, such as Down syndrome, with a high degree of accuracy. Testing for other genetic diseases, such as Tay-Sachs disease, is not routinely performed but can be detected through specialized testing if your fetus is known to be at risk. Testing for neural tube defects, such as spina bifida, also can be performed.
There is a small risk of miscarriage as a result of amniocentesis — about 1 in 100 or less. Miscarriage rates for procedures performed at UCSF Medical Center are less than 1 in 350.
Chorionic Villus Sampling (CVS) — Like amniocentesis, chorionic villus sampling is used most commonly to identify chromosomal problems such as Down syndrome. It can detect other genetic diseases like cystic fibrosis, Tay-Sachs disease and sickle cell disease in at-risk fetuses. The main advantage of CVS over amniocentesis is that it is done much earlier in pregnancy, at 10 to 12 weeks rather than 15 to 20 weeks.
CVS involves removing a tiny piece of tissue from the placenta. Under ultrasound guidance, the tissue is obtained either with a needle inserted through the abdomen or a catheter inserted through the cervix. The tissue is then cultured and a karyotype analysis of the chromosomal make-up of the cells is performed. It takes about two weeks to receive the results.
The advantage of CVS over amniocentesis is that the test is performed much earlier in pregnancy, so results are typically available by the end of the third month.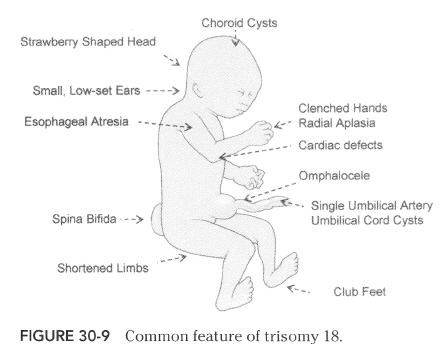 A disadvantage is that spinal cord defects cannot be detected. Expanded alpha fetoprotein (AFP) blood testing or ultrasound can be performed later in the pregnancy to screen for spinal cord defects.
A disadvantage is that spinal cord defects cannot be detected. Expanded alpha fetoprotein (AFP) blood testing or ultrasound can be performed later in the pregnancy to screen for spinal cord defects.
There is a small risk of miscarriage as a result of CVS — 1 in 100 or less. Miscarriage rates for procedures performed at UCSF Medical Center are less than 1 in 350.
Ultrasound — The primary purpose of ultrasound is to determine the status of a pregnancy — the due date, size of the fetus and if the mother is carrying multiples. Ultrasound also can provide some information about possible birth defects in a fetus. All patients at UCSF Medical Center undergo a comprehensive ultrasound examination before any invasive tests are performed. Results of the ultrasound are explained at the time of the visit.
In some patients, an ultrasound raises concern of a possible abnormality in the fetus. We have extensive experience in performing and interpreting ultrasounds in pregnancy.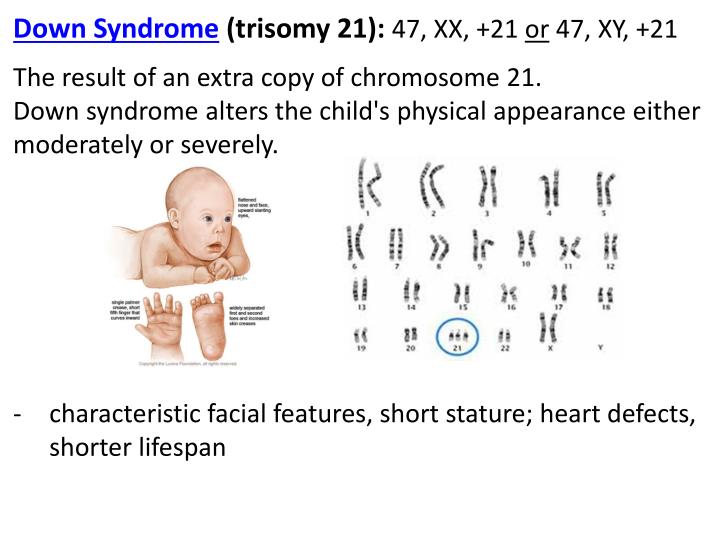
If You Receive a Positive Result
If you receive positive results on a screening test, we recommend that you discuss this with your doctor and a genetic counselor. Options for further diagnostic testing will be explained. The decision as to whether to have invasive genetic testing is up to you.
If a diagnostic test finds a genetic abnormality, the significance of such results should be discussed with experts familiar with the condition, including a medical geneticist and a genetic counselor, as well as your own doctor.
Screening tests for Down syndrome in the first 24 weeks of pregnancy
Relevance
Down's syndrome (also known as Down's disease or Trisomy 21) is an incurable genetic disorder that causes significant physical and mental health problems and disability. However, Down syndrome affects people in completely different ways. Some have significant symptoms, while others have minor health problems and are able to lead relatively normal lives. There is no way to predict how badly a child might be affected.
There is no way to predict how badly a child might be affected.
Expectant parents during pregnancy are given the opportunity to have a screening test for Down syndrome in their baby to help them make a decision. If a mother is carrying a child with Down syndrome, then a decision should be made whether to terminate the pregnancy or keep it. The information gives parents the opportunity to plan life with a child with Down syndrome.
The most accurate screening tests for Down syndrome include amniotic fluid (amniocentesis) or placental tissue (chorionic villus biopsy (CVS)) to identify abnormal chromosomes associated with Down syndrome. Both of these tests involve inserting a needle into the mother's abdomen, which is known to increase the risk of miscarriage. Thus, screening tests are not suitable for all pregnant women. Therefore, more often take blood and urine tests of the mother, and also conduct an ultrasound examination of the child. These screening tests are not perfect because they can miss cases of Down syndrome and are also at high risk of being positive when the child does not have Down syndrome.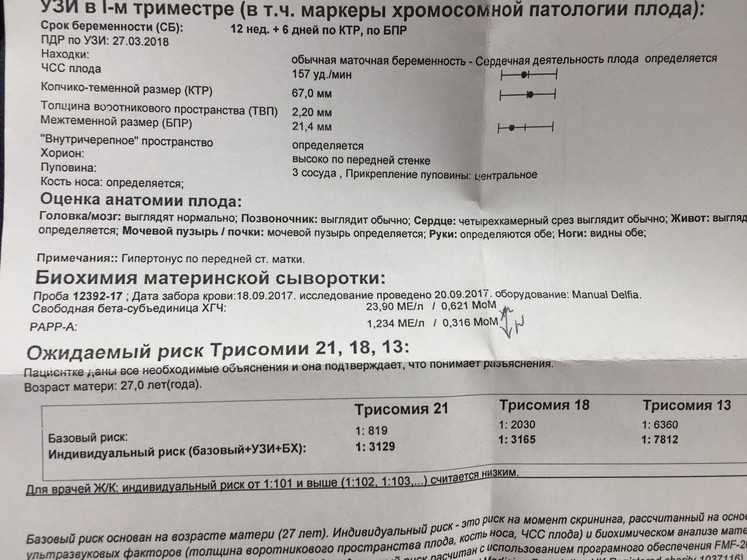 Thus, if a high risk is identified using these screening tests, further amniocentesis or CVS is required to confirm the diagnosis of Down syndrome.
Thus, if a high risk is identified using these screening tests, further amniocentesis or CVS is required to confirm the diagnosis of Down syndrome.
What we did
We analyzed combinations of serum screening tests in the first (up to 14 weeks) and second (up to 24 weeks) trimesters of pregnancy with or without ultrasound screening in the first trimester. Our goal was to identify the most accurate tests for predicting the risk of Down syndrome during pregnancy. One ultrasound index (neckfold thickness) and seven different serological indexes (PAPP-A, total hCG, free beta-hCG, unbound estriol, alpha-fetoprotein, inhibin A, ADAM 12) were studied, which can be used separately, in ratios or in combination with each other, obtained before 24 weeks of gestation, thereby obtaining 32 screening tests for the detection of Down's syndrome. We found 22 studies involving 228615 pregnant women (including 1067 fetuses with Down syndrome).
What we found
During Down Syndrome screening, which included tests during the first and second trimesters that combined to determine overall risk, we found that a test that included neckfold measurement and PAPP- A in the first trimester, as well as the determination of total hCG, unbound estriol, alpha-fetoprotein and inhibin A in the second trimester, turned out to be the most sensitive, as it allowed to determine 9out of 10 pregnancies associated with Down syndrome. Five percent of pregnant women who were determined to be at high risk on this combination of tests would not have a child with Down syndrome. There have been relatively few studies evaluating these tests, so we cannot draw firm conclusions or recommendations about which test is best.
Five percent of pregnant women who were determined to be at high risk on this combination of tests would not have a child with Down syndrome. There have been relatively few studies evaluating these tests, so we cannot draw firm conclusions or recommendations about which test is best.
Other important information to consider
Ultrasounds by themselves have no adverse effects on women, and blood tests can cause discomfort, bruising, and, in rare cases, infection. However, some women who have a high-risk Down syndrome baby on screening and who have had an amniocentesis or CVS are at risk of miscarriage of a non-Down syndrome baby. Parents will need to weigh this risk when deciding whether to perform amniocentesis or CVS after a "high risk" screening test is identified.
Translation notes:
Translation: Abuzyarova Daria Leonidovna. Editing: Prosyukova Ksenia Olegovna, Yudina Ekaterina Viktorovna. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University).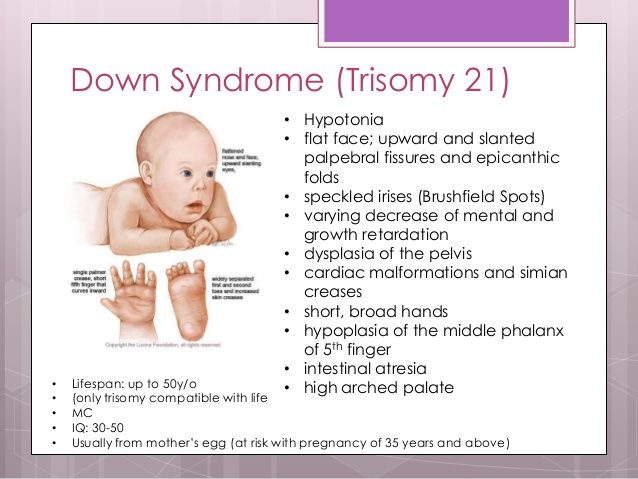 For questions related to this translation, please contact us at: [email protected]; [email protected]
For questions related to this translation, please contact us at: [email protected]; [email protected]
Prenatal screening for trisomy in the second trimester of pregnancy (triple test)
Prenatal screening for trisomy of the second trimester of pregnancy is also called a triple test - this is a study that allows you to determine the likely risk of developing chromosomal diseases such as Down's disease, Edwards syndrome, Patau syndrome, neural tube defects, and other fetal anomalies.
What are the dangers of genetic abnormalities for the fetus
Down syndrome is the most common genetic anomaly. Children with this diagnosis have serious physical and mental abnormalities, half of the newborns are diagnosed with heart disease. Immediately or over time, problems with vision, with the thyroid gland, with hearing may appear. Statistics say that every 700-800th child is born with this pathology. This fact does not depend on the lifestyle of the parents, their state of health or ecology.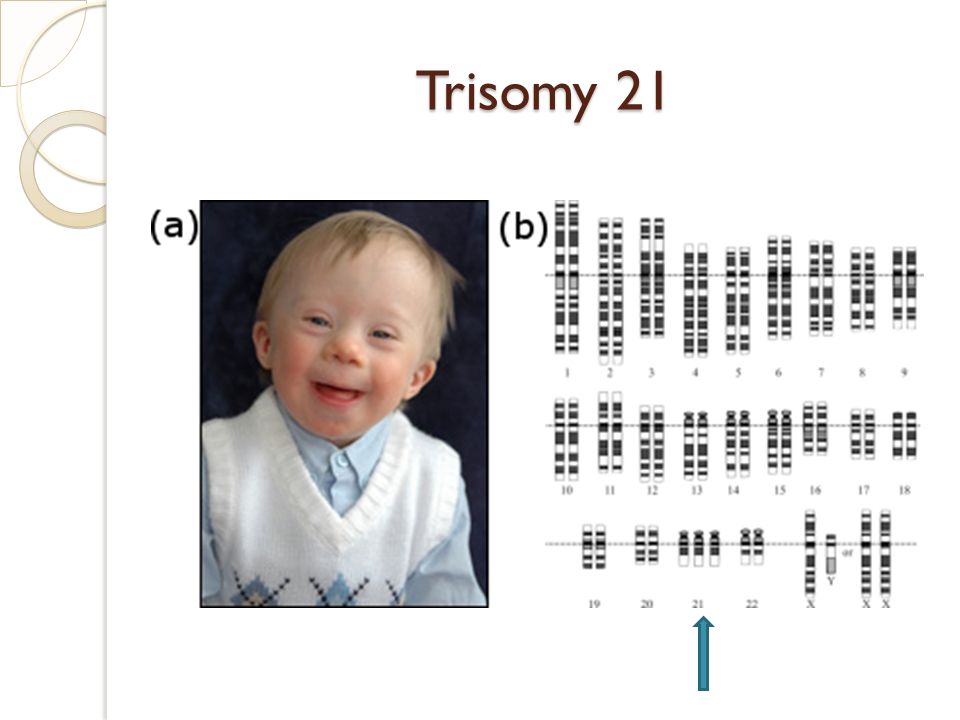 Scientists have found that the cause lies in the trisomy of the 21st chromosome (the presence of three homologous chromosomes instead of a pair).
Scientists have found that the cause lies in the trisomy of the 21st chromosome (the presence of three homologous chromosomes instead of a pair).
Edwards syndrome is also a chromosomal anomaly; with the full form of this disease, oligophrenia develops to a complicated degree; with a mosaic form, it may not manifest itself so clearly. In the case of this syndrome, the woman in labor has trisomy on the 18th chromosome.
Patau's syndrome is also characterized by physical defects and mental retardation. The disease is caused by trisomy on the 13th chromosome.
One of the most common causes of morbidity and mortality in newborns is neural tube defects (NTDs), including anencephaly and spina bifida. The first defect is a gross malformation of the brain, the second is a malformation of the spine, often combined with defects in the development of the spinal cord.
How is the triple test done?
To detect an anomaly at an early stage, screening is carried out between 14 and 22 weeks of gestation. Blood is taken from a woman in labor as a biomaterial. The day before, fatty foods are contraindicated for the patient, half an hour before the study, it is required to exclude physical and emotional overstrain, as well as smoking.
Blood is taken from a woman in labor as a biomaterial. The day before, fatty foods are contraindicated for the patient, half an hour before the study, it is required to exclude physical and emotional overstrain, as well as smoking.
During the test, the level of human chorionic gonadotropin (hCG), alpha-fetoprotein and free estriol is checked. According to these indicators, one can judge the successful course of pregnancy or identify violations of the development of the fetus.
The study takes into account age, weight, number of fetuses, race, bad habits, the presence of diabetes and medications taken. At the end of the test, the pregnant woman is prescribed a consultation with an obstetrician-gynecologist.
Important! Based on the results of screening, they do not make a diagnosis, nor are they a reason for artificial termination of pregnancy. The test makes it possible to determine the need for invasive methods for examining the fetus. If the risks of an anomaly are high, then a mandatory additional study is prescribed.