Stds in babies
Sexually transmitted infections, pregnancy, and breastfeeding
Sexually transmitted infections (STIs) are also called sexually transmitted diseases, or STDs. STIs include chlamydia, gonorrhea, trichomoniasis, genital herpes, genital warts, HIV, and syphilis. Some STIs can pass from mother to baby during pregnancy and through breastfeeding.
How do STIs affect pregnant women?
STIs can cause many of the same health problems in pregnant women as in women who are not pregnant. But having an STI also can hurt the unborn baby's health.
Having an STI during pregnancy can cause:
- Premature labor (labor before 37 weeks of pregnancy). Early (preterm) birth is the number one cause of infant death and can lead to long-term developmental and health problems in children.1
- Infection in the uterus (womb) after birth
Can I pass an STI to my baby?
Yes. Some STIs can be passed from a pregnant woman to the baby before and during the baby's birth.
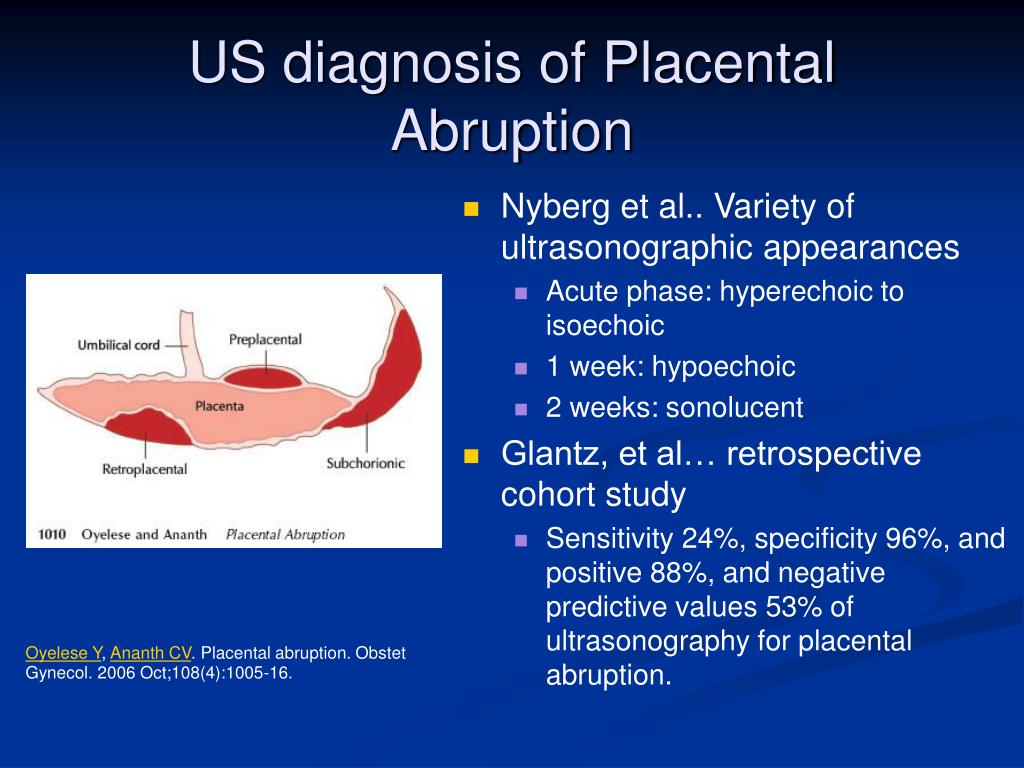
- Some STIs, such as syphilis, cross the placenta and infect the baby in the womb.
- Other STIs, like gonorrhea, chlamydia, hepatitis B, and genital herpes, can pass from the mother to the baby as the baby passes through the birth canal.
- HIV can cross the placenta during pregnancy and infect the baby during delivery.
What are the harmful effects of passing an STI to a baby?
The harmful effects to babies may include:
- Low birth weight (less than 5 pounds)
- Eye infection
- Pneumonia
- Infection in the baby's blood
- Brain damage
- Lack of coordination in body movements
- Blindness
- Deafness
- Acute hepatitis
- Meningitis
- Chronic liver disease, which can lead to scarring of the liver (cirrhosis)
- Stillbirth
I'm pregnant. What can I do to prevent problems from STIs?
You can prevent some of the health problems caused by STIs and pregnancy with regular prenatal care. Your doctor will test you for STIs early in your pregnancy and again closer to childbirth, if needed.
Your doctor will test you for STIs early in your pregnancy and again closer to childbirth, if needed.
- STIs caused by bacteria, such as chlamydia and gonorrhea, can be cured with antibiotics. Some antibiotics are safe to take during pregnancy. Your doctor can prescribe antibiotics for chlamydia, gonorrhea, syphilis, and trichomoniasis during pregnancy.
- STIs caused by viruses, such as genital herpes and HIV, have no cure.
- If you have herpes, antiviral medicine may help reduce symptoms. If you have symptoms of herpes or active genital herpes sores at the start of labor, you may need a cesarean section (C-section). This can help lower the risk of passing the infection to your baby.
- If you have HIV, antiviral medicines can lower the risk of giving HIV to your baby to less than 1%.2 You also may need to have a C-section.
You also can take steps to lower your risk of getting an STI during pregnancy.
Can I breastfeed if I have an STI?
Maybe. Some STIs affect breastfeeding, and some don't. The following are some general guidelines, but talk to your doctor, nurse, or a lactation consultant about the risk of passing the STI to your baby while breastfeeding:
- If you have HIV, do not breastfeed. You can pass the virus to your baby. In countries like the United States where clean water is available, using a breastmilk substitute like formula is recommended.
- If you have chlamydia, gonorrhea, or HPV, you can breastfeed your baby.
- If you have trichomoniasis, you can take the antibiotic metronidazole if you are breastfeeding. You may need to wait 12 to 24 hours after taking the medicine to breastfeed.
- If you have syphilis or herpes, you can breastfeed as long as your baby or pumping equipment does not touch a sore. It is possible to spread syphilis or herpes to any part of your breast, including your nipple and areola.
 If you have sores on your breast, pump or hand-express your milk until the sores heal. Pumping will help keep up your milk supply and prevent your breast from getting overly full and painful. You can store your milk to give to your baby in a bottle for another feeding. But if parts of your breast pump also touch the sore(s) while pumping, you should throw the milk away.
If you have sores on your breast, pump or hand-express your milk until the sores heal. Pumping will help keep up your milk supply and prevent your breast from getting overly full and painful. You can store your milk to give to your baby in a bottle for another feeding. But if parts of your breast pump also touch the sore(s) while pumping, you should throw the milk away.
Are STI treatments safe to use while breastfeeding?
If you are being treated for an STI, ask your doctor about the possible effects of the medicine on your breastfeeding baby. Most treatments for STIs are safe to take while breastfeeding.
Did we answer your question about STIs, pregnancy, and breastfeeding?
For more information about STIs, pregnancy, and breastfeeding, call the OWH Helpline at 1-800-994-9662 or contact the following organizations:
- Food and Drug Administration (FDA), HHS
Phone Number: 888-463-6332 - National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), CDC, HHS
Phone Number: 800-232-4636 - National Institute of Allergy and Infectious Diseases (NIAID), NIH, HHS
Phone Number: 866-284-4107 (TDD: 800-877-8339) - American Sexual Health Association
Phone Number: 800-227-8922
Sources
- Centers for Disease Control and Prevention.
 (2015). Preterm Birth.
(2015). Preterm Birth. - Centers for Disease Control and Prevention. (2015). HIV Among Pregnant Women, Infants, and Children.
The Office on Women's Health is grateful for the medical review by:
- Jill E. Long, M.D., M.P.H., FACOG, Commander, U.S. Public Health Service Commissioned Corps, Medical Officer, Sexually Transmitted Diseases Branch, Division of Microbiology and Infectious Diseases, National Institute of Allergy and Infectious Diseases
- Centers for Disease Control and Prevention (CDC) staff
All material contained on these pages are free of copyright restrictions and maybe copied, reproduced, or duplicated without permission of the Office on Women’s Health in the U.S. Department of Health and Human Services. Citation of the source is appreciated.
Page last updated: February 22, 2021
STD Facts - STDs & Pregnancy
If you are pregnant, you can become infected with the same sexually transmitted diseases (STDs) as women who are not pregnant.
 Pregnant women should ask their doctors about getting tested for STDs, since some doctors do not routinely perform these tests. This fact sheet answers basic questions about STDs during pregnancy.
Pregnant women should ask their doctors about getting tested for STDs, since some doctors do not routinely perform these tests. This fact sheet answers basic questions about STDs during pregnancy.I’m pregnant. Can I get an STD?
Yes, you can. Women who are pregnant can become infected with the same STDs as women who are not pregnant. Pregnancy does not provide women or their babies any additional protection against STDs. Many STDs are ‘silent,’ or have no symptoms, so you may not know if you are infected. If you are pregnant, you should be tested for STDs, including HIV (the virus that causes AIDS), as a part of your medical care during pregnancy. The results of an STD can be more serious, even life-threatening, for you and your baby if you become infected while pregnant. It is important that you are aware of the harmful effects of STDs and how to protect yourself and your unborn baby against infection. If you are diagnosed with an STD while pregnant, your sex partner(s) should also be tested and treated.
How can STDs affect me and my unborn baby?
STDs can complicate your pregnancy and may have serious effects on both you and your developing baby. Some of these problems may be seen at birth; others may not be discovered until months or years later. In addition, it is well known that infection with an STD can make it easier for a person to get infected with HIV. Most of these problems can be prevented if you receive regular medical care during pregnancy. This includes tests for STDs starting early in pregnancy and repeated close to delivery, as needed.
Should I be tested for STDs during my pregnancy?
Yes. Testing and treating pregnant women for STDs is a vital way to prevent serious health complications to both mother and baby that may otherwise happen with infection. The sooner you begin receiving medical care during pregnancy, the better the health outcomes will be for you and your unborn baby. The Centers for Disease Control and Prevention’s 2015 STD Treatment Guidelines recommend screening pregnant women for STDs. The CDC screening recommendations that your health care provider should follow are incorporated into the table on the STDs during Pregnancy – Detailed CDC Fact Sheet.
The CDC screening recommendations that your health care provider should follow are incorporated into the table on the STDs during Pregnancy – Detailed CDC Fact Sheet.
Be sure to ask your doctor about getting tested for STDs. It is also important that you have an open, honest conversation with your provider and discuss any symptoms you are experiencing and any high-risk sexual behavior that you engage in, since some doctors do not routinely perform these tests. Even if you have been tested in the past, you should be tested again when you become pregnant.
Can I get treated for an STD while I’m pregnant?
It depends. STDs, such as chlamydia, gonorrhea, syphilis, trichomoniasis and BV can all be treated and cured with antibiotics that are safe to take during pregnancy. STDs that are caused by viruses, like genital herpes, hepatitis B, or HIV cannot be cured. However, in some cases these infections can be treated with antiviral medications or other preventive measures to reduce the risk of passing the infection to your baby. If you are pregnant or considering pregnancy, you should be tested so you can take steps to protect yourself and your baby.
If you are pregnant or considering pregnancy, you should be tested so you can take steps to protect yourself and your baby.
How can I reduce my risk of getting an STD while pregnant?
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting chlamydia:
- Being in a long-term mutually monogamous relationship with a partner who has been tested and has negative STD test results;
- Using latex condoms the right way every time you have sex.
You can add this content to your website by syndicating.
STDs during Pregnancy - CDC Detailed Fact Sheet
Detailed fact sheets are intended for physicians and individuals with specific questions about sexually transmitted diseases. Detailed fact sheets include specific testing and treatment recommendations as well as citations so the reader can research the topic more in depth.
STDs (sexually transmitted diseases)
Ask a question or make an appointment
Nowadays, the most common STDs are: chlamydia, trichomoniasis, thrush (candidiasis), gardenelosis, ureaplasmosis, mycoplasmosis, cytomegalovirus, papilloma virus, herpes simplex virus human (HPV) and some others (there are more than 20 pathogens of these diseases). STDs are among the most common infectious diseases worldwide. According to statistics, about 75% of women have had an episode of urogenital candidiasis at least once in their lives, and in 40% of them the disease recurs. Trichomoniasis affects 60-70% of women with excessive discharge.
STDs are among the most common infectious diseases worldwide. According to statistics, about 75% of women have had an episode of urogenital candidiasis at least once in their lives, and in 40% of them the disease recurs. Trichomoniasis affects 60-70% of women with excessive discharge.
What else are hidden infections dangerous for? STDs are the cause of male and female infertility. During pregnancy, during the development of the fetus, these infections lead to severe congenital diseases, deformities or death of the child in the womb. They are able to be transmitted to the child through mother's milk, through saliva during a kiss, during a blood transfusion, in the household way. In an adult, latent sexual infections often lead to pathology of internal organs.
STDs are mainly transmitted sexually through unprotected sex with an infected partner. It must be remembered that adolescents and young women are more susceptible to STDs than men.
Timely screening for sexually transmitted infections plays a key role in the prevention of latent infections. Prevention and treatment of STDs reduce the risk of HIV transmission, especially in people who have a large number of sexual partners. The most effective means of reducing the transmission of STDs is the male latex condom, however, even this does not guarantee 100% protection against infection, its reliability is 65% - 98%, depending on the infection.
Prevention and treatment of STDs reduce the risk of HIV transmission, especially in people who have a large number of sexual partners. The most effective means of reducing the transmission of STDs is the male latex condom, however, even this does not guarantee 100% protection against infection, its reliability is 65% - 98%, depending on the infection.
If casual sexual contact does occur, and there is no condom at hand, it is necessary to wash hands and external genitalia with soap (2 times). It is useful for women to douche the vagina using water with an antiseptic. Within 2 hours after intercourse, you can use the drug betadine, miramistin, etc. The minus of such prevention is that it does not give a 100% guarantee.
In any case, it is necessary to consult a specialist and to be tested for infections in 3-4 weeks.
The most important weapon against STDs, however, remains the prevention of sexual infections. Regularly visit a gynecologist and urologist-andrologist for examination and necessary tests.
Signs of infection may include:
- unusual discharge from the genitals (white, slimy, green, frothy), with or without odor;
- itching and burning in the vulva;
- appearance on the skin or mucous membranes of spots, sores, vesicles;
- frequent urge or painful urination;
- lower abdominal discomfort;
- pain in groin and scrotum;
- pain during intercourse;
- menstrual disorders;
- swollen lymph nodes.
If any of these symptoms are present, a woman should see a gynecologist, and a man should see a urologist or a dermatologist-venereologist. One hundred percent certainty that you are healthy can only be given by the results of laboratory tests for STDs. It is better to diagnose and treat STDs in the early stages, when nothing bothers you.
Do not forget that your health is the guarantee of the health of your loved ones and your children.
If the suspicions are confirmed and the test results are positive, it is recommended that your partner also be tested. We need to treat STDs together. During treatment, sexual intercourse is not recommended, although it is possible, but only with the use of condoms.
We need to treat STDs together. During treatment, sexual intercourse is not recommended, although it is possible, but only with the use of condoms.
Never self-medicate! With uncontrolled use of antibiotics, you will ensure that the disease is not cured, but becomes hidden. Moreover, microorganisms adapt to the drug, which greatly complicates the treatment.
Only a timely visit to a doctor is a guarantee of successful treatment.
When diagnosing and treating diseases, doctors take into account all the individual characteristics of the body, as well as strictly adhere to the standards accepted in medicine.
After a course of treatment, it is obligatory to carry out a control of the cure. Control tests should be performed no earlier than 3 weeks after the completion of the course of treatment (optimally - after 1 month). A re-examination is done after 4 months. More precisely, the attending physician will already tell you how long to take tests after STD treatment
Remember that your sexual and reproductive health depends on you. Do not put off the diagnosis and visit to the doctor. Take care of your health!
Do not put off the diagnosis and visit to the doctor. Take care of your health!
Non-childhood diseases of adolescence
01.01.2018
It is often difficult for adolescents to talk to their parents about intimate problems, and even more so to admit to their illness.
In order to minimize such situations in the Ryazan region, a special center for the prevention, diagnosis and treatment of sexually transmitted infections (STIs), "Trust", was created.
The curator of the organization, dermatovenereologist, deputy chief physician of the Regional Clinical Dermatovenerologic Dispensary, a member of the International Union Against Infections Transmitted by sexually Mikhail Zhuchkov .
— Mikhail Valeryevich, please tell us how urgent the problem of STIs among adolescents is today.
- STIs are a small but heterogeneous group of diseases. Despite the fact that in the last 10 years throughout the Russian Federation there has been a decrease in the incidence of sexually transmitted infections, the problem remains very relevant.
Despite the fact that in the last 10 years throughout the Russian Federation there has been a decrease in the incidence of sexually transmitted infections, the problem remains very relevant.
The decline in the incidence of the most common sexually transmitted infections, according to the majority of reputable Russian epidemiologists, is "false", since it is entirely based on official statistics.
Meanwhile, both in the Ryazan region and in Russia as a whole, a huge number of private medical organizations are successfully operating. There is no doubt about the competence of the specialists working there, because most of them are also employees of state healthcare institutions. But the reliability of the information provided by private clinics on the number of patients with STDs is highly questionable. So, in 2012, only 7% of commercial medical organizations in the Ryazan region provided annual statistical reporting data to our dispensary.
Meanwhile, many patients who suspect that they have STDs, especially adolescents, always want to get advice in conditions of absolute anonymity, incorrectly believing that this is only possible in a private medical organization. Thus, the vicious circle closes.
Thus, the vicious circle closes.
— So how do you break this vicious cycle?
- Very simple. Today, everyone should understand that public health institutions that provide specialized medical care to those suffering from STDs operate in strict accordance with the law. A patient applying, for example, to a dermatovenerological dispensary, can count not only on receiving qualified assistance, but also on strict adherence to the principles of confidentiality by the medical staff of the organization. Gone are those distant Soviet times, when persons suffering from sexually transmitted diseases were “hung with social labels”, reported a case of illness at the place of work, with the help of police officers, and were examined forcibly. All these are crude, cruel and absolutely unjustified atavisms of the past. The past, for which, to be honest, we are a little ashamed, but still the past. STI today is not a “disease to be ashamed of”, it is a disease that needs to be treated effectively, quickly, efficiently and anonymously.
— Mikhail Valeryevich, it's no secret that teenagers are the most vulnerable category of people in relation to sexual infections. And not every one of them will decide to tell their parents about the symptoms that have arisen. Is there a place in our city where a "confused" teenager can come for an anonymous free consultation?
- On the basis of the Ryazan Regional Clinical Dermatovenerologic Dispensary, the teenage center for the prevention, diagnosis and treatment of sexually transmitted infections, "Doverie", has been successfully operating over the past few years. It was created as part of the implementation of the federal target program "Prevention and control of diseases of a social nature." The center's specialists every day provide qualified medical and psychological assistance to children and adolescents in the prevention, diagnosis and treatment of STIs.
— Is it true that the prevalence of STIs among adolescents continues to increase?
- Unfortunately, yes. Now in society there are a lot of socially unadapted children and adolescents, some of them take psychotropic drugs. And besides, over the past few years, the age of onset of sexual activity has significantly decreased. But the most important reason for the high incidence of sexually transmitted infections is still the lack of awareness of adolescents about the prevention of STIs and their adverse effects on reproductive health.
Now in society there are a lot of socially unadapted children and adolescents, some of them take psychotropic drugs. And besides, over the past few years, the age of onset of sexual activity has significantly decreased. But the most important reason for the high incidence of sexually transmitted infections is still the lack of awareness of adolescents about the prevention of STIs and their adverse effects on reproductive health.
— And how do teenagers themselves react to an offer to be tested for STIs or, for example, to listen to a lecture on proper sexual behavior?
- Oddly enough, the vast majority of them are very interested. Educational programs are aimed at making teenagers more attentive to sexual contacts, making them think about themselves and the person who is nearby. A huge merit of the doctors of the Dermatovenerologic Dispensary in general and the Trust Center in particular is the formation in young people of responsibility for their sexual health and the health of a person close to him. Fortunately, every year young people trust our center more and more. We see confirmation of this every day, observing more and more adolescents at outpatient appointments.
Fortunately, every year young people trust our center more and more. We see confirmation of this every day, observing more and more adolescents at outpatient appointments.
— Mikhail Valeryevich, tell me, in what cases and for what symptoms do teenagers need to contact the doctors of the center?
- General signs, characteristic of most genital infections, are discharge from the genital organs, pain during intercourse, sores and abrasions on the surface of the genitals. But the most important thing that every teenager should understand is that in the vast majority of cases, many sexually transmitted infections do not manifest themselves for the time being! And therefore, all young people who have an active sex life need to be regularly examined by a dermatovenereologist.
Persons and organizations of the article
Deputy chief physician for organizational and methodological work
Zhuchkov Mikhail Valerievich The highest qualification category,
The highest qualification category, Dermatovenereology, Health Organization and Public Health
Source: Portal UZRF.